Abstract
Critical care medicine is far from the first medical field to come to mind when humanitarian action is mentioned, yet both critical care and humanitarian action share a fundamental purpose to save the lives and ease the suffering of people caught in acute crises. Critically ill children and adults will be present regardless of resource limitations and irrespective of geography, regional or cultural contexts, insecurity, or socioeconomic status, and they may be even more prevalent in a humanitarian crisis. Critical care is not limited to the walls of a hospital, and all hospitals will have critically ill patients regardless of designating a specific ward an ICU. Regular and consistent consideration of critical care principles in humanitarian settings provides crucial guidance to intensivists and nonintensivists alike. A multidisciplinary, systematic approach to patient care that encourages critical thinking, checklists that encourage communication among team members, and context-specific critical care rapid response teams are examples of critical care constructs that can provide high-quality critical care in all environments. Promoting critical care principles conveys the message that critical care is an integral part of health care and should be accessible to all, no matter the setting. These principles can be effectively adopted in humanitarian settings by normalizing them to everyday clinical practice. Equally, core humanitarian principles—dignity, accountability, impartiality, neutrality—can be applied to critical care. Applying principles of critical care in a context-specific manner and applying humanitarian principles to critical care can improve the quality of patient care and transcend barriers to resource limitations.
Keywords: critical care, intensive care, humanitarian action
Humanitarian Action and Critical Care
Criticized for being expensive, for requiring unavailable equipment and technology to be effective, for benefitting only a few when the needs of many are overwhelming in humanitarian settings, critical care medicine is far from the first medical field to come to mind when humanitarian action is mentioned. Yet both critical care and humanitarian action share a fundamental purpose “to save the lives and ease the suffering of people caught in acute crises, thereby restoring their ability to rebuild their lives and communities” (1). Too often underappreciated are the triage skills, the patient assessment skills to recognize those deteriorating from severe illnesses, as well as the critical thinking and practical approach that critical care teams bring to patient care. Such knowledge and skills are independent of specialized equipment and medications (Figure 1). Critically ill children and adults will, after all, be present regardless of resource limitations and irrespective of geography, cultural contexts, insecurity, or socioeconomic status, and they may be even more prevalent in a complex humanitarian emergency.1 As physicians in critical care, emergency medicine, anesthesia, and obstetrics, we have worked in various humanitarian settings—“a range of situations including natural disasters, conflict, slow- and rapid-onset events, rural and urban environments, and complex political emergencies” (2)—in multiple countries (Afghanistan, Haiti, Iraq, Laos, Nepal, Pakistan, and various countries throughout Africa). In this article we reflect on our personal experiences of the value and role of critical care medicine in the global context during our work with various humanitarian organizations, including Médecins Sans Frontières/Doctors Without Borders (MSF), to guide nonintensivists and intensivists in improving assessment and treatment of critically ill patients specifically in humanitarian settings. MSF is an independent medical humanitarian organization that brings medical care to people affected by armed conflict, epidemics, healthcare exclusion, and disasters. This article discusses how critical care can be provided and adapted to improve the quality of patient care in humanitarian settings, the practical lessons learned, and future directions to optimize the contributions of critical care to those in need. Examples from a recent MSF field mission to South Asia are discussed, although specific MSF projects, details about these projects, or specific analysis cannot and have not been identified in this article to mitigate operational risks.
Figure 1.
(A) Modified T-piece apparatus made with a 10-ml syringe. The shaft of the 10-ml syringe is cut and the endotracheal tube is inserted into the shaft. Oxygen tubing is applied to the needle end of the syringe. The plunger of the syringe is removed. The finger of a glove is cut (top and bottom) and placed on the plunger end of the syringe to create a one-way valve. (B) Monitors (top left), electricity (top right), fluid warmer (right), and suction equipment and oxygen concentrator (bottom) denote basic equipment for critical care.
Access Barriers
Once illness occurs, the initial challenge for critically ill patients in humanitarian settings is the ability to seek and access health care. Common access barriers include the lack of transportation methods, prehospital and hospital clinicians, and medical resources. These barriers are further exacerbated by insecurity, sudden population movements, outbreaks, natural disasters, and social or cultural challenges (Table 1). In a global society that values access to health care, such access should not exclude the knowledge and skill that critical care can bring to humanitarian efforts. Humanitarian settings differ from established environments in that doctors and teams are often not trained in critical care; the ability to monitor patients can be very limited; there can be overwhelming patient volumes, limited human resources, and limited critical care equipment; and transfers to higher levels of care may not be possible because they do not exist. Yet, as demonstrated in the 2014 to 2016 West African Ebola epidemic, critical care can save many lives in humanitarian settings (3–5).
Table 1.
Social and Cultural Challenges Unique to Humanitarian Settings
| Social and Cultural Challenges | Impact on Providing Critical Care |
|---|---|
| Gender constructs | • Male chaperones may need to be present for female patients to access health care and may be needed to provide consent for procedures |
| • Only female staff can assess female patients (e.g., perform an ECG, intramuscular gluteal injections, assessment of femoral pulse, pelvic examinations) | |
| • Female patients may not disclose their health issues to male staff | |
| • Limited number of female healthcare professionals available to work | |
| • Female staff dress in culturally appropriate attire when in view of public (outfits have to be changed when moving between emergency department and ward) | |
| Regional insecurity, violence, mistrust of nongovernmental organizations | • Attacks on healthcare workers |
| • Limited staff because of an undesirable work location | |
| • Restricted movements, curfews, limited ability of staff to remain at the field project, limited ability to transfer patients | |
| • Closure of field projects | |
| Private versus public healthcare systems and the perception of Western medicine | • Expectation of foreigners to provide expensive medical care |
| • Unjustified ordering of diagnostics due solely to newly acquired access | |
| • Defrayed costs to humanitarian teams | |
| Bureaucracy related to gaining approval of new activities | • Challenges to initiating new initiatives |
| • Challenges to procuring medications or equipment | |
| • Challenges to clinical practice to reflect latest evidence | |
| Job insecurity (temporary field projects), noncompetitive salaries | • Frequent staff turnover and recruitment necessary |
| • Loss of educational gains in the professional development of staff |
Critical care is not limited to the walls of a hospital, and all hospitals will have critically ill patients regardless of designating a specific ward an ICU for, “at its core, critical care is simply healthcare for very sick patients” (6). Few doctors in humanitarian settings are ICU trained, and those who are may find themselves working in environments and with considerations that are very different from those they are familiar with (Table 2). The ICU team is usually not just a consulting service but also the same team that triages patients on arrival and assesses them in the emergency room. In many humanitarian settings, critically ill patients are cared for in a relatively basic healthcare center, solely in the emergency department or postanesthesia recovery room. In some humanitarian settings, there may be an identified ICU with less equipment typically associated with such environments, such as central venous lines, intravenous pumps, or ventilators, and the only vasopressor reliably available is adrenaline. In some settings, the ICU is not defined geographically but rather it is the bed, no different from any other bed, in which the critically ill patient is placed. There may be limited access to oxygen and monitors. Bedside ultrasound has become increasingly available and may aid in diagnostics; however, clinicians are still limited in their skills in using it, and it provides limited therapeutic advantages without the appropriate treatment resources. The ability to perform X-rays varies, and laboratory support is commonly minimal. Clinicians must rely on their history and physical examination skills, the physical examination skills and their physiologic implications that are often forgotten or not taught (e.g., jugular venous pressure waveform assessments, pulsus paradoxus, quality of and presence of extra heart sounds, hepatojugular reflex) in resource-rich settings in an era of bedside ultrasound and widespread availability of computed tomography scans and magnetic resonance imaging. In many humanitarian settings, it is not about bringing the patient to the ICU; it is about bringing the ICU to the patient. Awareness of and application of critical care principles can reduce morbidity and mortality regardless of patient location and can be effectively achieved by normalizing these principles to everyday clinical practice.
Table 2.
Select Clinical Scenarios and Challenges in Humanitarian Settings Based on the Authors’ Personal Experiences in Various Humanitarian Settings
| Clinical Scenarios | Context-Specific Challenges in Humanitarian Settings |
|---|---|
| Trauma and other conditions requiring resuscitation | Airway |
| • Limited advanced airway equipment should not preclude basic airway management. Contrary to conventional teachings regarding the need to intubate patients with low GCS, the placement of an oral airway, oxygen, positioning, and suctioning can, at times, be sufficient to manage a patient successfully | |
| Breathing | |
| • Reliance on history and clinical examination if imaging modalities not available (e.g., pneumonia vs. pulmonary edema) | |
| • Lack of wall suction for chest tubes and pleural drains | |
| • Trial of bag-mask ventilation in lieu of NIV for conditions that benefit from NIV | |
| • Manual bagging with endotracheal tube in situ in lieu of mechanical ventilation because of limited or lack of ventilators | |
| • Need for prolonged manual bagging until recovery if ventilator not available for organophosphate toxicity (consideration of teaching family members bagging technique) | |
| Circulation | |
| • Lack of central venous lines and ensuring safe administration of vasoactive medications with peripheral IV cannulas | |
| • Insertion of multiple peripheral IV cannulas in series into the same vein in patients with poor venous access options in lieu of a multilumen central venous line when multiple medication infusions are required | |
| • Use of nebulized salbutamol for temporary management of symptomatic bradycardia when atropine or other vasoactive medications are not available | |
| • Limited availability of blood products and predominate use of whole blood | |
| • Limited reversal of coagulopathy from lack of fresh blood | |
| • Limited systems/processes in place for immediate blood transfusions and the need to anticipate in advance if transfusions will be required (e.g., need to call in donors, who are usually patient relatives, to obtain blood) | |
| • Limited IV line warmers and blood warmers | |
| • Reliance on urine output and mental status as markers of shock | |
| Disability (neurological) | |
| • Language barrier can make neurologic assessment challenging | |
| • Incomplete neurological assessments with lack of assessment of GCS, pupils, eye movements, gaze preference, cranial nerves, presence of motor and sensory levels | |
| • Limited imaging, monitoring, and advanced interventions for brain injuries | |
| • Limited stabilization in the field, assessment and monitoring skills, imaging, monitoring, and advanced interventions for spinal cord injuries | |
| • CT imaging guidelines based on prognosis and not necessarily severity | |
| • Lack of postoperative neuro–intensive care capabilities preclude interventions, resulting in referral of patients to other facilities if available | |
| Exposure (and other organ systems) | |
| • Reliance on physical examination with limited blood tests and imaging modalities | |
| • Casting/splinting and external fixation predominates with lack of resources for internal fixation for orthopedic fracture management | |
| • Limited burn care resources and treatment capabilities for thermal burns and electrical injuries | |
| • Considerations for special wound care management (e.g., rabies immunoglobulin, tetanus immunoglobulin, snake antivenom) | |
| • Lack of referral pathways, prehospital clinicians, and medically staffed ambulances | |
| Multiple causalities | |
| • Frequent occurrence of multiple-causality events or incidents alongside day-to-day operations using preestablished triage and disaster plans | |
| • Patients or family members may assist in procedures (e.g., hold chest tube after it is inserted while clinician sutures it to the chest) | |
| • Extubate stable open-abdomen patients (pragmatic to the situation) | |
| Perioperative and anesthesia | • Lack of complex ventilators and anesthetic machines for inhalational anesthesia |
| • Use of alternative (potentially unfamiliar) anesthesia delivery systems, such as draw-over anesthetic circuits | |
| • Unreliable supply of gases (either piped or bottled) | |
| • Unreliable supply of electricity | |
| • Predominate use of spinal anesthesia | |
| • Predominate use of ketamine and basic airway management | |
| • Anesthetic agents may differ significantly from high-income countries (e.g., halothane) | |
| • Limited anesthesia specialists and training of nonphysician anesthesia clinical staff | |
| • Lack of ventilators/lack of ICU results in overreliance of postanesthesia recovery room or the emergency department for postoperative ventilated patients who could not be extubated (or kept in the operating theater) | |
| • Common cultural low regard for the importance of postanesthesia recovery room | |
| • High proportion of clinically unwell children presenting for surgery; may strain the clinician (if unfamiliar with pediatrics) and the resources of equipment | |
| Obstetrics | • Unknown antenatal history and poor antenatal care |
| • High parity because of poor access to family planning (or due to cultural norms) | |
| • Complications of unsafe abortions | |
| • Uterine ruptures from oxytocin misuse and abuse | |
| • Postpartum hemorrhage often presents late (e.g., after home delivery) and in hemorrhagic shock, with limited or short supply of medical therapies (e.g., tranexamic acid or blood transfusion) | |
| • Populations with high prevalence of severe preeclampsia/eclampsia (seizures are seen as a spiritual event rather than a medical problem in some cultures, which results in late presentation after hours of uncontrolled hypertension and seizures possibly leading to an intracerebral hemorrhage) | |
| • Lack of access and understanding for preventive low-dose aspirin after severe preeclampsia or eclampsia, which could significantly reduce the risk of complications of future pregnancies | |
| • Preference for vaginal delivery to avoid complications after cesarean section in future pregnancies | |
| • Late presentation or referral of patients in obstructed labor with resulting difficult cesarean sections and risk of obstetric fistula | |
| • High incidence of female genital mutilation in some populations | |
| Pediatrics | • Clinicians need to be comfortable managing both adults and children, as pediatric specialists may not always be available |
| • A large number of patients presenting to hospital are children (e.g., traumatic injuries, burns, infections) | |
| • Large number of critically ill neonates presenting after home deliveries requiring resuscitation | |
| • Frequent cases of malnutrition and use of ready-to-use therapeutic foods | |
| Infections | • Endemic considerations: tuberculosis, HIV, malaria, typhoid, dengue, cholera, viral hemorrhagic fevers |
| • Minimal infection, prevention, control resources and limited ability for isolation rooms | |
| • Neonatal tetanus from cutting umbilical cord with dirty objects | |
| • Measles due to lack of immunization |
Definition of abbreviations: CT = computed tomography; GCS = Glasgow Coma Scale; NIV = noninvasive ventilation.
Applying Critical Care Principles to Humanitarian Settings
Critical Assessment Skills
Performing a primary survey—assessing airway, breathing, circulation, disability, and exposure (ABCDE)—is a fundamental skill that can be used to resuscitate all critically ill patients irrespective of injury or disease (7). The ABCDE approach is well known to many clinicians yet poorly performed in chaotic, busy humanitarian settings. Such an approach, however, should be used beyond the standard considerations of whether a patient has an airway, is breathing, and has a pulse. Simple modifications can foster critical thinking by including questions to help clinicians anticipate deteriorations, facilitate goal-directed resuscitation before the development of irreversible organ failure, build team communication, establish daily targets, and identify warning signs of problems for less-experienced teams to promote a preventative critical care approach (Figure 2). Such an approach with head-to-toe assessments can be used to reassess responses to treatments. These concepts are relatively new to humanitarian settings and can bring consistency and rigor to care, prevent tunnel vision, and foster treatment plans to improve outcomes. For example, in a recent field mission to a hospital that had a focus on promoting cardiac care, there was anchoring bias, wherein patients presenting with hypotension were perceived to be in cardiogenic shock, when in reality sepsis was the more common problem, especially in patients with no preceding history of chest pain (Médecins Sans Frontières–Operational Centre Brussels, unpublished results). The focus on cardiac care likely contributed to the team’s predisposition to misdiagnose cardiac disease and start to manage most patients who presented in shock accordingly, which resulted in failures to adequately fluid resuscitate patients and an increased incidence of multisystem organ failure. Promotion of critical thinking and the application of the quick Sepsis-related Organ Failure Assessment score improved the doctors’ recognition of sepsis and led to appropriate initiation of antibiotics and sepsis care bundles and improved outcomes (8).
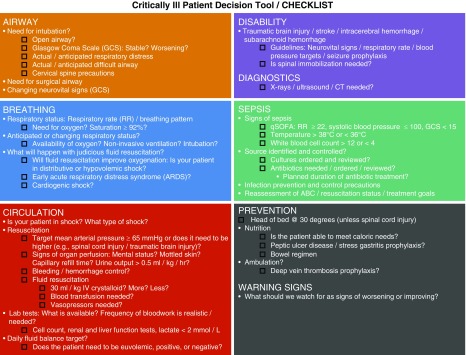
Figure 2.
Modified airway, breathing, circulation, disability (ABCD) assessment. CT = computed tomography; qSOFA = quick sepsis-related organ failure assessment.
Interprofessional Teaching and Team Approach to Care
Interprofessional education is infrequent in many humanitarian settings because of hierarchical social constructs, gender, and cultural issues. Multidisciplinary, low-fidelity simulation training with doctors and nurses together in field missions promotes the empowerment of nurses to actively discuss with doctors a patient’s treatment plan, rather than simply following orders. This can lead to the realization of the importance of frequent reassessment of patients’ vital signs (something we take for granted in a resource-rich ICU), closed-loop communication during resuscitation, and the need for a team approach to treatment. Although such an approach requires leadership and significant time commitment, it results in a more tightly knit team that communicates more effectively, anticipates potential complications, and understands risks, leading to better monitoring and more timely identification of deterioration, decreasing failures to rescue and improving patient safety.
Rational Testing and Treating
In humanitarian settings, careful consideration of resource allocation is needed, with a higher-than-usual threshold before advanced interventions are initiated. In some contexts, hospitals are a conglomerate of many small buildings, and obtaining diagnostic investigations (e.g., X-rays or computed tomography [CT] scans) requires transporting patients across busy streets. Patients are often sent unaccompanied by healthcare staff, in some instances because staff are so busy there is no one available and in others because staff do not understand the need to accompany. Even when accompanied, there are risks of transporting patients for tests in such settings, because safety equipment (e.g., end-tidal CO2 monitors as an example) is not available, and if problems develop during the transportation, the ability to stabilize en route is usually much more limited. Clinicians should weigh the risks versus benefits of investigations to not expose patients, or even themselves, to undue risks, and need to plan how patient safety can be maintained and risks mitigated when transportation for tests is needed. Similarly, a rational and transparent approach is needed to determine what treatments to offer, because the risk and benefit considerations change in humanitarian settings and there is a need to optimize and maintain resource availability. In consideration of all these issues, when in the field, we developed and pragmatically instituted two simple tools to systematically support such decisions: ITEST and ITREAT (Figure 3). A survey of local doctors before their introduction showed that the majority did not have a tool to help them decide which investigations (11/16) and treatments (12/16) to order. ITEST was used to promote rational use of investigations, and ITREAT was incorporated into the management of shock, antibiotic stewardship, and guided palliative treatment plans. A survey performed 6 weeks after their introduction showed the majority of doctors felt more supported in their clinical decision making (15/16), and a quarter of doctors said their initial plan was changed as a result (4/16).
Figure 3.
ITEST and ITREAT mnemonic tool.
Trauma from motor vehicle collisions, falls from heights, and interpersonal violence is a significant cause of mortality in many humanitarian settings. The decision to not intubate a patient with a severe head injury with a Glasgow Coma Scale score less than 8 because there are no resources to ventilate or nowhere to transport can be one of the most difficult decisions a clinician can make; however, resource limitations do not preclude basic airway management, such as keeping the head of the bed raised to 30 degrees, suctioning, and applying supplemental oxygen. Moreover, such maneuvers can at times be sufficient to manage a patient successfully.
Treating critically ill obstetrical patients is similarly an important component of humanitarian work, as many pregnant women present without prior prenatal care. A common presentation is severe preeclampsia/eclampsia with concurrent anemia, low platelets, and elevated liver enzymes (Médecins Sans Frontières–Operational Centre Brussels, unpublished results). HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome was suspected in some of these cases, with a differential diagnosis of fatty liver of pregnancy or thrombotic microangiopathies. A systematic approach to assessing such patients encourages clinicians to also consider other important endemic causes of anemia and thrombocytopenia, such as malaria and dengue, which require different investigations and treatment to achieve good outcomes. Making an accurate diagnosis in this context is very important and has long-term repercussions: if diagnosed with eclampsia, an intubated patient is generally destined for a cesarean section; however, in humanitarian settings, cesarean sections must be performed judiciously, because the ability to perform any repeat cesarean sections may not be available in the future and the risks of complications associated with a previous uterine scar with a subsequent vaginal birth need to be considered. Given these risks, a decision not to immediately intubate unresponsive, postictal patients with eclampsia to facilitate a vaginal birth is favored, but doing so requires close monitoring, with frequent reassessments.
Finally, many, if not all, humanitarian crises involve insecurity, which can affect the supply chain of medical resources, the ability of field teams to safely remain on site to provide care, and/or patient transfers to a higher level of care, if these exist at all. All treatment plans must account for such issues as much as possible. Local clinicians may remain on site when expatriate clinicians are mandated to return to safer environments by humanitarian agencies. Waiting to see how patients respond acutely to treatments is often a luxury. Instead, there is a need to think multiple steps ahead and anticipate and teach local clinicians to look for warning signs, signs of expected and successful response, and potential adjustments needed to any treatment plan. In addition, involving local clinicians in the decision making and implementation of new protocols is vital. In our experience from developing protocols for critically ill patients, the involvement of local clinicians at a multidisciplinary level led to ownership of any new protocols and sustainability after expatriate clinicians left.
Checklists and Treatment Bundles
Checklists and bundles of care are commonly used evidence-based critical care interventions that decrease morbidity (9). Evidence-based, best-practice treatment protocols for illnesses such as head injuries and strokes can be helpful as long as they are practical and set targets that are achievable and realistic for the setting. For example, regular vital signs can be challenging if there is only one blood pressure cuff, and neuro-vital signs may be difficult to obtain in a timely fashion when human resources are scarce. The question becomes what standard can be feasibly achieved and how can protocols be adapted to maintain patient safety and achieve the best possible outcomes. Treatment protocols must also be kept updated, and this can be challenging when staff are struggling to care for high volumes of patients and do not have time to explore or ability to access current literature. Internationally developed protocols, such as the World Health Organization (WHO) Trauma Care Checklist, when implemented in high-, middle-, and low-income countries, have been associated with improvements in patient care (10, 11). The WHO Trauma Care Checklist is performed immediately after the primary and secondary surveys and before the clinical team leaves the patient. From our experience in humanitarian settings, the WHO Trauma Care Checklist is an effective quality assurance tool and facilitates team communication, especially during the transfer process out of the resuscitation room.
In humanitarian settings, checklists can also have specific, yet perhaps unanticipated, cultural significance that can lead to important quality improvement. To improve safety of vasopressor administration, recognizing that central venous lines were not available and that infusion pumps were not always readily available, we developed a peripherally administered vasopressor checklist, which included an additional step that required both doctor and nurse to review and sign. In the particular cultural context, the signatures were seen as a contract between doctor and nurse in treating the patient. This encouraged communication, empowered nursing colleagues, and increased patient safety.
Rapid Response and Resuscitation Teams
Cardiac arrest teams and critical care rapid response teams are well-known constructs in resource-rich hospitals. Resource limitations may not permit the luxury of such teams, yet such teams can bring real value in carefully chosen humanitarian contexts. Reducing maternal mortality is a target within the United Nations Sustainable Development Goals, and critical care can play an important role in achieving this target (12). MSF provides emergency obstetrical services in many settings; however, cultural and gender barriers can create challenges for healthcare providers and access to women’s health in certain regions. In South Asia, the development of an all-female team to respond to obstetrical emergencies allowed for faster care of critically ill obstetrical patients in a culturally appropriate manner where only women can provide certain aspects of clinical care (Table 1). Such rapid response teams could be used more widely to mitigate barriers to care in many similar environments. Humanitarian settings are about bringing critical care to the patient; organizing this response into context-specific rapid response teams is another way to find and meet the needs of some of the sickest patients who present.
End-of-Life Care
It is a hard truth that the ability to save critically ill patients in humanitarian settings is often much more limited and that survivors may experience greater morbidity. Although most humanitarian settings provide free access to medications, the supply is limited in both its range and quantity. Oxygen supplies may be limited. It is very common for the only vasopressor to be adrenaline, which has to be administered in small amounts or mixed in a diluted manner and the drops counted to determine its dose, because intravenous pumps are lacking. The possibility of central line insertion is very rare. A decision to resuscitate a patient with septic or cardiogenic shock in humanitarian settings faces very grim odds of success. The risks are higher in terms of underdosing medications, the complications of too high doses, and the risks of extravasation. Transfer to another more advanced facility is often not possible, because one does not exist, the journey would be too long and patient stability cannot be maintained, or such a journey would involve crossing through unsafe conflict zones, placing everyone at risk. Despite all efforts, many critically ill patients die. Even if patients do survive, the ability to provide ongoing treatment for subsequent morbidities and the financial resources needed to live with chronic illness and to rehabilitate from critical illness can impact treatment, limiting decisions in humanitarian settings. Supporting patients and families facing such difficult realities is an important aspect of humanitarian medicine. End-of-life discussions (in a culturally respectful manner) are often needed. Asking how these topics are negotiated is important. Knowing that patients would have had better odds of surviving in different settings can be difficult to handle, particularly when the team tried everything they could. Initial bereavement support also requires cultural understanding that critical care physicians are accustomed to discussing. Acknowledging these realities while advocating to change them and providing support to clinical teams can improve humanitarian teams’ coping and resilience.
Applying Humanitarian Principles to Critical Care
Critical care principles can appear very scientific and detached because of the high stakes of decisions to allocate what are often the scarcest of resources in humanitarian settings. Rational testing and treatment decisions risk failing to convey the primary purpose—to humanely treat and try to save critically ill patients—unless some fundamental core humanitarian principles are consistently considered: dignity, accountability, impartiality, and neutrality (13). These principles can be applicable to critical care in both humanitarian and resource-rich settings.
Of these, the most important concept is that of dignity—of the patients, families, and clinicians. It has been said that the measure of society is how we treat our most vulnerable. Critically ill patients are among the most vulnerable worldwide. Patient education to first prevent severe illness and promote understanding of the diagnosis and context-appropriate treatments can convey respect for the patient as a person and help set expectations anywhere in the world. The engagement of patients/families in care decisions should be promoted in culturally appropriate ways, regardless of their level of education or socioeconomic status. In humanitarian settings, clinicians may feel dispirited that they do not have the tools necessary to achieve better outcomes and may feel devalued by those from resource-rich settings who come to help. Local clinicians may fail to appreciate their strong clinical diagnostic skills, the need to teach the meaning of these skills to those who may have forgotten or not been taught them, and the value they add to developing differential diagnoses that are independent of imaging modalities relied on elsewhere. Such clinicians can teach those from resource-rich settings by reminding them of the need for proper physical examinations and bedside assessments.
In humanitarian settings, expectations run high that field clinicians from resource-rich settings will be able to successfully treat those with critical illnesses. Although the same results are not always possible, accountability means that the highest standards of care achievable should be targeted. Care must be practical, grounded in scientific knowledge, and often creative. The risks and benefits of any proposed treatment plan must be weighed in ways that reflect the modified settings. Basic principles still apply, despite common patient expectations to receive intravenous medications or other advanced interventions. Not all febrile illnesses require antibiotics, not all medications need to be administered intravenously, and advanced interventions may not be appropriate, as they will not change the outcome. Promoting critical care principles conveys the message that critical care is an integral part of health care and should be accessible to all, no matter the setting. In many humanitarian settings, the use of critical care skills such as intubation or the administration of adrenaline will change the standard of care and require consideration of the consequences of such changes on sustainability, trust within the community, transparency in allocation of resources, and team burnout and resilience.
The concepts of impartiality and neutrality mean that assistance is offered to all patients on the basis of need and irrespective of race, religion, gender, political affiliation, or social status. It is crucial to demonstrate that these factors do not influence investigations or treatments, as many critical illnesses may be the result of socioeconomic issues, lifestyle choices, or predisposing illnesses that, for whatever reason, are viewed negatively in the cultural context. Triage on the basis of illness severity alone is poorly taught, and yet, grounded in impartiality and neutrality, it is life-saving.
Future Directions: Advancing Critical Care in Humanitarian Settings—Getting Involved
In humanitarian action, the attempt to rebuild lives and communities, an emphasis should be placed on local staff capacity building with critical care knowledge and skills. Critical care clinicians from resource-rich countries can build solidarity by working abroad or contributing from home. Professionalization of humanitarian assistance is a reality, and ensuring that standards in a humanitarian response are met is essential (2, 14).
Working in humanitarian settings, conversely, provides unique insights to all critical care physicians, through the honing of assessment skills, the development of more rational investigation and treatment plans, and improved use of ICU resources. The tenets of humanitarian medicine, those of dignity and accountability in particular, can provide a change in perspective to critical care physicians from resource-rich settings, prone to burnout and cynicism from the provision of inappropriate treatments, by reminding them of their purpose in helping critically ill patients who would have no chance at survival without a humanitarian response.
Academic institutions can engage humanitarian organizations to expose trainees to humanitarian settings through established field training facilities. Partnerships with academic institutions can enhance patient care. Expertise can be brought with education, research, knowledge translation, and updating clinical guidelines or protocols in an evidence-based, context-specific manner. In addition, the development of practice support tools can be a low-cost but high-yield critical care intervention.
Telemedicine presents a feasible opportunity to be involved with humanitarian action for those who do not have the opportunity to work abroad and can bring critical care expertise to any bedside worldwide. MSF recently implemented real-time telemedicine in South Asia as a quality-improvement initiative using a smartphone-based messenger application to provide remote neuro–critical care support (15). Local doctors were able to discuss indications for CT imaging, an expensive resource, and seek further management advice of these critically ill patients. Anonymous surveys completed by local doctors after the consultation showed that originally missed CT findings were identified (33/82), new knowledge on patient management was provided (31/82), patient management was changed (34/82), and clinicians felt better supported after the consultation (55/82). From the telemedicine consultants’ perspective, seeing the local doctors improve their knowledge, skill, and confidence in a short time frame was very rewarding. Real-time telemedicine consultations contributed to both satisfaction in the clinical environment and professional growth.
Conclusions
Critically ill children and adults will always be present in humanitarian settings. Humanitarian action and critical care medicine share a common pursuit of saving lives during times of acute crises. Applying principles of critical care in a context-specific manner and applying core humanitarian principles—dignity, accountability, impartiality, and neutrality—to critical care can improve the quality of patient care and transcend barriers to resource limitations.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank all field staff, local collaborators, patients, and families from all Médecins Sans Frontières (MSF) field projects that they have had the pleasure of participating in. They also thank Dr. Annick Antierens for her review of the manuscript, all departments from MSF–Operational Centre Brussels, and all referents/advisors they have communicated with for their guidance and support. They also thank Dr. Aziz Alali, Dr. James Maskalyk, Yogesh Jha, Fabien Schneider, and MSF Canada for their expertise and support with the real-time telemedicine initiative.
Footnotes
A complex humanitarian emergency is defined by the Inter-Agency Standing Committee as a humanitarian crisis in a country, region, or society where there is a total or considerable breakdown of authority resulting from internal or external conflict that requires an international response that goes beyond the mandate or capacity of any single and/or ongoing United Nations country program.
Author Contributions: All authors contributed to the conception or design of this work; acquisition, analysis, and interpretation of data; drafting the work or revising it critically for important intellectual content; and final approval of the version to be published.
Originally Published in Press as DOI: 10.1164/rccm.201806-1059CP on October 5, 2018
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Medecins Sans Frontieres International. Activities: humanitarian issues [accessed 2018 Apr 16]. Available from: http://www.msf.org/en/humanitarian-issues
- 2.The Sphere Project. Humanitarian charter and minimum standards in humanitarian response [accessed 2018 Apr 16]. Available from: http://www.spherehandbook.org.
- 3.Fowler RA, Fletcher T, Fischer WA, II, Lamontagne F, Jacob S, Brett-Major D, et al. Caring for critically ill patients with Ebola virus disease: perspectives from West Africa. Am J Respir Crit Care Med. 2014;190:733–737. doi: 10.1164/rccm.201408-1514CP. [DOI] [PubMed] [Google Scholar]
- 4.Hunt L, Lee JS. Empiric intravenous fluid and electrolyte therapy in patients with Ebola virus disease. Trop Doct. 2016;46:148–150. doi: 10.1177/0049475516644883. [DOI] [PubMed] [Google Scholar]
- 5.Dickson SJ, Clay KA, Adam M, Ardley C, Bailey MS, Burns DS, et al. Enhanced case management can be delivered for patients with EVD in Africa: experience from a UK military Ebola treatment centre in Sierra Leone. J Infect. 2018;76:383–392. doi: 10.1016/j.jinf.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riviello ED, Letchford S, Achieng L, Newton MW. Critical care in resource-poor settings: lessons learned and future directions. Crit Care Med. 2011;39:860–867. doi: 10.1097/CCM.0b013e318206d6d5. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons Committee on Trauma. Advanced Trauma Life Support ATLS student course manual. 9th ed. Chicago, IL: American College of Surgeons: 2012. Initial assessment and management; pp. 2–21. [Google Scholar]
- 8.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006;355:2725–2732. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. The WHO trauma care checklist. [accessed 2018 Apr 16]. Available from: http://www.who.int/emergencycare/publications/trauma-care-checklist.pdf?ua=1.
- 11.Lashoher A, Schneider EB, Juillard C, Stevens K, Colantuoni E, Berry WR, et al. Implementation of the World Health Organization Trauma Care Checklist program in 11 centers across multiple economic strata: effect on care process measures. World J Surg. 2017;41:954–962. doi: 10.1007/s00268-016-3759-8. [DOI] [PubMed] [Google Scholar]
- 12.United Nations. Sustainable development goals. [accessed 2018 Apr 20]. Available from: https://www.un.org/sustainabledevelopment/health/
- 13.Médecins Sans Frontières International. About MSF: charter and principles [accessed 2018 Apr 16]. Available from: http://www.msf.org/en/msf-charter-and-principles.
- 14.World Health Organization Classification and minimum standard for foreign medical teams in sudden onset disasters [accessed 2018 Apr 16]. Available from: http://www.who.int/hac/global_health_cluster/fmt_guidelines_september2013.pdf?ua=1.
- 15.Jha Y, Lee J, Hawryluck L, Alali A, Maskalyk J, Schneider F, et al. Smartphone based, real-time telemedicine for the management of neurological emergencies: a field-based quality improvement initiative [version 1; not peer reviewed] F1000Research. 2018;7:645. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.