Abstract
Objective:
The current study examined the influence of early parental stress and positive parent personality during infancy on sleep in middle childhood. Further, the role of positive parent personality as a buffer of the association between parental stress and sleep was considered.
Methods:
Participants included 381 twins and their primary caregivers who were recruited from birth records in the United States. Primary caregivers completed survey assessments via phone when twins were 12 and 30 months of age to assess multiple dimensions of parental stress and positive parent personality. Approximately six years later (M=5.78, SD=0.42), twins participated in an intensive assessment that included wearing actigraph watches to provide an objective measurement of sleep, while primary caregivers completed daily diaries regarding twins’ sleep.
Results:
Positive parent personality was associated prospectively with longer actigraphy sleep duration and higher parent-reported sleep quality/daytime functioning. Parental stress was associated prospectively with greater variability in sleep duration. Positive parent personality moderated the parental stress—sleep-timing relation, such that greater parental stress was associated with a later midpoint of the sleep period only for children with parents low on positive personality (e.g., low optimism). All other findings were non-significant.
Conclusions:
Findings suggest that both positive attributes and stress may influence sleep in middle childhood, and that low parent positive personality may exacerbate associations between parental stress and later timing of sleep periods in children. Early interventions to promote healthy sleeping may consider focusing on decreasing parental stress and increasing parental empathy and optimism as early as infancy.
Keywords: pediatric sleep, parental stress, positive parent personality, resilience
Early-life experiences can impact physical and mental health across the lifespan. Adverse early-life experiences, such as neglect and violence, have been associated with later physiological and mental health problems (Johnson et al., 2013; Shonkoff et al., 2012). Other early promotive or protective factors, such as strong family relationships, have been associated with healthy development (Youngblade et al., 2007). Such promotive factors may have direct effects on child health, but also may serve as a source of resilience, by buffering the detrimental effects of early adversity (Masten, 2014). A host of mechanisms are likely to account for the links between early-life experiences and subsequent child health outcomes, but one key potential pathway is sleep, a restorative bioregulatory process that occupies roughly one-third of daily life (Mathur et al., 2018; Palagini et al., 2019). Many children and adolescents worldwide do not meet the recommended hours of sleep, which are 9–11 and 8–10 hours for school-aged children and adolescents, respectively (National Sleep Foundation, 2014; Gradisar, Gardner, & Dohnt, 2011), suggesting the importance of identifying factors that impact sleep in childhood, including the lasting influence of the early environment. Based on the ecobiodevelopmental framework (Shonkoff et al., 2012), the current study examined the potential influences of early-life experiences (i.e., parental stress and strain [hereafter parental stress] and positive parent personality) on sleep among twins in middle childhood.
Early Life Parental Stress and Strain
Early-life stress and adversity in childhood have been connected to physical and mental health problems in adulthood. This was exemplified by the Adverse Childhood Experiences (ACES) study conducted by Felitti and colleagues (1998), which was the first to connect negative childhood experiences to health conditions later in life. Continued research has linked early-life adversity with numerous negative health consequences in adulthood, including shorter sleeping periods, less physical activity, poorer diet, more depressive symptoms, and increased rates of substance use (e.g., Felitti et al., 1998; Windle et al., 2018). Further, it is proposed that early-life stress impacts sleep, which then may contribute to mental health problems later in life (Palagini et al., 2019), suggesting a life-long trajectory of poor consequences stemming from negative early-life experiences.
Prior research has connected adversity early in life to poor sleep (e.g. disturbances [trouble falling or staying asleep], insomnia) in adolescence and adulthood (Chapman et al., 2011; Chapman et al., 2013; Kajeepeta et al., 2015; Wang, Raffeld, Slopen, Hale, & Dunn, 2016), suggesting a link between the early environment and sleep later in life. Negative childhood experiences have been related to troubled sleep, defined as self-reports of difficulty falling or staying asleep, and an increased likelihood of poor sleep quality among adults (Baiden, Fallon, den Dunnen, & Boateng, 2015; Koskenvuo, Hublin, Partinen, Paunio, & Koskenvuo, 2010). Childhood stress across a wide range of contexts has also been associated with actigraphy-based shorter sleep duration, prolonged sleep latency, decreased sleep efficiency, and increased movements during sleep periods among adults (Schafer & Bader, 2013). The prior work offers a foundation for the connection between negative early-life experiences and sleep.
The bulk of the literature linking early adversity with health outcomes has focused on severe forms of adversity, including sexual and physical abuse; yet other forms of early-life stress may also impact sleep. The current study focused on early parental stress, reflected in a composite of parental depressive symptoms, parenting daily hassles, lack of social support, lack of parent-child emotional availability, chaos in the home, and use of punitive punishment. For example, early risky family environments (e.g., low warmth and support) have been associated with poor self-reported sleep quality among young adults (Counts, Grubin, & John-Henderson, 2018). Among college students, retrospective reports of family conflict and lack of affection in childhood as well as reports on parental warmth, moderated the associations between daily stress and physiological measures (i.e., sleep and cortisol; Hanson & Chen, 2010). For students who reported more difficult childhood environments (e.g. more conflict), greater or more severe amounts of stress were associated with less sleep and more cortisol secretion across the day, as indicated by greater area under the curve (Hanson & Chen, 2010). These studies exemplify that negative qualities of the family environment including low parental warmth have been linked to poor sleep. Further substantiating the link between parental factors and child sleep, early maternal postnatal depression has been prospectively related to self-reported sleep problems in adolescence (16 and 18 years of age; Taylor et al., 2017).
A small body of research has examined more proximal mechanisms of early-life stress on sleep in childhood. Early maternal psychosocial adversity, defined as higher depressive and anxious symptomology, has been associated with sleep disturbances (i.e., later bedtimes, more variability in bedtime and duration) in children at 18 months and 5 years of age (Cronin, Halligan, & Murray, 2008; Sheridan et al., 2013). Additionally, higher stress related to parenting and maternal anxiety and depressive symptoms have been associated with greater parent-reported night wakings among infants and young children (Coto, Garcia, Hart, & Graziano, 2018; Ystrom et al., 2017). This suggests that the effects of early-life stress may not only have lasting impacts throughout a person’s life trajectory, but also negative consequences may occur relatively soon after exposure to stress. However, most research linking early-life stress and adversity to sleep in children and adults relies on self- or parent-report of both sleep and adversity, leading to single method and report bias.
Promotive Factors and Positive Parent Personality
In contrast to numerous findings linking early adversity with health outcomes, few studies have examined positive parent personality as a promotive factor of children’s health outcomes. Parent personality can impact parenting which affects the environmental context in which a child develops (Prinzie, Stams, Dekovic, Rejintjes, & Belsky, 2009; Clark, Kochanska, & Ready, 2000). Therefore, the current study also examined the impact of positive parent personality as a promotive factor of positive development (i.e., healthy sleep) and the interaction of parental stress and positive parent personality as a factor of resilience. Here positive parent personality is reflected in a composite that includes optimism, hope, self-compassion, empathic concern and perspective taking, personal mastery, and positive emotional expressiveness.
Parent attributes such as internal locus of control, hardiness, and optimism have been associated with positive child outcomes (Johnson & McMahon, 2008; McDonald, Kehler, & Tough, 2016; Nowicki, Iles-Caven, Gregory, Ellis, & Golding, 2017). For example, for toddlers with mothers with mental health problems, maternal optimism was a protective factor in the development of behavioral problems (McDonald et al., 2016). Among single, African American mothers optimism has been linked to positive parenting and may buffer the impact of economic pressures on internalizing symptoms (Taylor et al., 2010). Self-compassion has also been linked to positive development in children. Higher levels of parent self-compassion have been associated with lower levels of criticism towards children, fewer distressed reactions towards children, and fewer reported internalizing and externalizing problems among children (Psychogiou et al., 2016). Together findings suggest optimism and self-compassion may be promotive factors for positive development.
Further, several parent personality traits including locus of control (Nowicki et al., 2017) and hardiness (Johnson & McMahon, 2008) have been specifically associated with child sleep outcomes. External locus of control among parents has been associated with poor child health behaviors, including more sleep problems and worse eating habits (Nowicki et al., 2017). More specifically, parents with an external locus of control had children with more sleep problems, including a lack of a bedtime routine, refusal to go to bed, and night wakings. Other research examining the effect of parental hardiness on sleep among preschoolers found that lower hardiness was associated with more problematic sleep-related cognitions among the parents (Johnson & McMahon, 2008). The negative cognitions predicted more bedtime interactions with the child, which then was associated with more child sleep problems. The same indirect association between maternal prenatal hardiness and child sleep problems was observed among 18-month olds (Johnson et al., 2014). Overall, prior research suggests aspects of parental personality may influence child sleep habits and health, with positive traits (e.g., optimism) being associated with positive child outcomes.
Implications of Poor Sleep for Health
Sleep in childhood has been connected to later health problems including obesity, cognitive problems, and mental health problems (Kurth, Olini, Huber, & Lebourgeois, 2015; Palagini et al., 2019). Sleep has been identified as one of three lifestyle behaviors that potentially predispose children to the development of non-communicable diseases (Wu et al., 2016), and has been related to metabolic disease in children and adults (Schmid, Hallschmid, & Schultes, 2015). Sleep problems among children have been found to persist into adolescence (Sivertsen, Harvey, Pallesen, & Hysing, 2017; Wang et al., 2016). Among adolescents, shorter durations have been associated with poorer self-rated health, more depressive symptoms, and increased odds of being overweight (Yeo et al., 2018). Prior research suggests a connection between poor sleep and poor mental and physical outcomes, with longitudinal trajectories of poor sleep starting in childhood.
While the literature consistently links sleep duration with health indicators, it is important to consider other parameters that characterize quality of sleep, including timing of the sleep period, sleep efficiency, and sleep latency. Sleep duration, efficiency, and timing have been differentially linked with health indicators, such as physical activity and adiposity (Chaput et al, 2015; McNeil et al., 2015). For example, later bedtimes and shorter durations have been associated with more sedentary time and unhealthy diet patterns (Chaput et al., 2015; Golley, Maher, Matricciani, & Olds, 2013); whereas sleep efficiency has only been related to unhealthy diet patterns (Chaput et al., 2015; Kjeldsen et al., 2014). Shorter sleep durations and objectively-assessed poor quality (e.g., efficiency, minutes awake after onset) also have been linked to mental health problems, including depressive symptoms, anxiety, and externalizing symptoms among children (Kelly & El-Sheikh, 2014). When considering variability in sleep, greater variability in sleep timing and duration have been related to increased odds of being overweight/obese and unhealthy diet patterns, respectively (Kjeldsen et al., 2014; Zhou, Lalani, Banda, & Robinson, 2018). Together these findings highlight differences in sleep-health relations in the literature and suggest that different aspects of the quality of sleep may be related to various physical and mental health indicators. Therefore, not only is it important to study influences on sleep in childhood, but also to examine different dimensions of sleep to get a holistic picture of children’s sleep behaviors.
Current Study
The current study extended the prior literature by examining the impact of both early-life parental stress and positive parent personality, as well as their interaction, on children’s sleep in middle childhood. Further, this study included both objective sleep parameters (i.e., mean sleep duration, mean sleep latency, midpoint of the sleep period, variability in duration) along with parent-reported subjective sleep quality (see Figure 1 for model) to obtain a well-rounded portrayal of the children’s actual sleep patterns. Parental stress and positive parent personality reports were assessed when the children were in their first few years of life; therefore, this study did not rely on retrospective reports of the early environment. Given recent findings from this sample illustrating early-life socioeconomic disparities in children’s sleep (see Doane, BreitensteiN, Beekman, Clifford, Smith, & Lemery-Chalfant, 2019), we proposed to examine indicators of parental stress from caregiver-related domains and also focused on promotive and potentially resilient indicators from early life that were associated with children’s sleep. Our focus on parent-related factors coincides with factors that have been identified as potentially modifiable to promote resilience in childhood in the face of other adversities (e.g., poverty; Traub & Boynton-Jarrett, 2017).
Figure 1. Conceptual Multilevel Model of Parent-Related Early Life Experiences Predicting Child Sleep at 8 Years of Age.
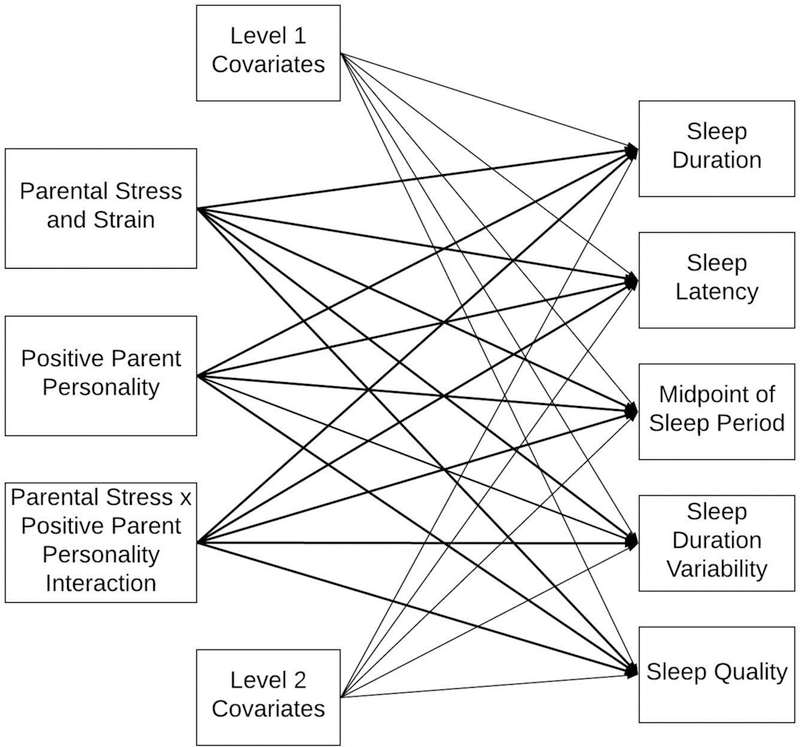
Note. Figure 1 is a conceptual model and does not depict any final results. All five sleep outcomes were estimated simultaneously. Sleep duration, sleep latency, midpoint of the sleep period, and sleep duration variability were derived from week-long actigraphy. Sleep quality includes daytime dysfunction and was derived from the caregiver daily diary reports. The main predictors were all at Level 2 (family level) and the outcomes were at Level 1 (child level). Level 1 covariates included child sex and child BMI. Level 2 covariates included child age (same for twin pairs), family SES, and whether the assessment took place during the summer or winter break versus during the school year.
This study aimed to 1) examine the main effects of early parental stress and positive parent personality on children’s sleep at 8 years of age and 2) examine the interaction between parental stress and positive parent personality as a predictor to investigate positive parent personality as a resilience factor. We hypothesized that early parental stress would be negatively associated with children’s sleep six years later (e.g., shorter duration) and that early positive parent personality would be positively associated with children’s later sleep. Additionally, we hypothesized that positive parent personality would buffer the effect of parental stress on children’s sleep.
Methods
Participants
Families were recruited through birth records as part of the longitudinal study and data for the current study were collected in 2009, 2011, and 2017 (The Arizona Twin Project; Lemery-Chalfant, Clifford, McDonald, O’Brien, & Valiente, 2013). Participants in the current study include 381 twins and their primary caregivers that are part of the longitudinal cohort (191 families; monozygotic or MZ families = 28.3%, same-sex dizygotic or DZ families = 37.7%, opposite-sex dizygotic or DZ families = 33.0%, unknown zygosity = 1.0%). Recruitment and response rate of the current sample have been previously described in detail (see Doane et al., 2019; Lemery-Chalfant et al., 2013). One twin was excluded from all analyses due to significant disabilities; all reports are on 381 twins. Twins were approximately 8 years of age (M = 8.45, SD = 0.45) and 50.4% were male, 56.4% were non-Hispanic White, and 25.2% were Hispanic. The majority of primary caregivers reported being the twins’ mother (94.8%). See Table 1 for participant demographics.
Table 1.
Twins and Primary Caregiver Demographics
| Demographic Items | Total Sample |
|---|---|
| Twins | N = 381 |
| Age, M years (SD) | 8.45 (0.45) |
| Sex (Female), n (%) | 189 (49.6) |
| Race/Ethnicity, n (%) | |
| Black/African American | 16 (4.2) |
| Hispanic/Latino | 96 (25.2) |
| Non-Hispanic White/European American | 215 (56.4) |
| Asian/Asian American | 20 (5.2) |
| Native American | 4 (1.0) |
| Native Hawaiian or Pacific Islander | 6 (1.6) |
| Multi-racial/ethnic or Unknown | 24 (6.3) |
| Caregiver | N = 191 |
| Relation to twins, n (%) | |
| Mother | 181 (94.8) |
| Father | 10 (5.2) |
| Relationship Status (at 12 months), n (%) | |
| Single/Never Married | 10 (5.2) |
| Married | 141 (73.8) |
| In a partnership | 12 (6.3) |
| Divorced | 3 (1.6) |
| Separated | 2 (1.0) |
| Widowed | 1 (0.5) |
| Other or Unknown | 22 (11.5) |
| Education (at 12 months), n (%) | |
| Less than a high school education | 4 (2.1) |
| High school degree | 17 (8.9) |
| Some college | 46 (24.1) |
| College degree (e.g., BS or BA) | 69 (36.1) |
| 2+ years of graduate school | 5 (2.6) |
| Graduate or professional degree | 28 (14.7) |
| Unknown | 22 (11.5) |
| Income-to-needs ratio (at 12 months), n (%) | |
| Below 1 (under poverty line) | 16 (9.8) |
| 1 – 2 (near the poverty line) | 34 (20.7) |
| 2 – 3 (lower middle class) | 40 (24.4) |
| Greater than 3 (middle to upper class) | 74 (45.1) |
| Household size (at 12 months), M (SD) | 4.85 (1.26) |
Note: percentages for income-to-needs ratios based on available data
Procedure
Institutional Review Board approval was obtained. Caregivers provided informed consent before all assessments; twins assented at the eight-year assessment. Caregivers completed questionnaires via phone when the twins were approximately 12 (M = 12.48, SD = 1.12) and 30 (M = 31.63, SD = 2.67) months. As the twins approached 8 years of age, families were contacted to participate in an intensive assessment of daily activities and home environment. The eight-year assessments included surveys, two home visits, and a week of daily assessments, including objective measurement of sleep and daily diaries. Two trained research assistants administered questionnaires, cognitive and interaction tasks, and took biological assessments of the twins and caregivers during the first home visit. Also, at this time the research assistants explained the actigraph and daily diary procedures to the families. Each twin was given an actigraph watch to wear for seven consecutive days (24 hours a day excluding bathing or swimming times) on their non-dominant wrist to assess daily sleep habits. Primary caregivers were instructed to complete a daily diary each night for seven consecutive days, which included a subjective assessment of the twins’ sleep quality. Parents reported on each twin separately in the diary..
During the assessment week, study staff contacted the families every evening to ensure the protocols were being followed and to address any concerns. Approximately a week later, two research assistants returned to the families’ homes for the second home visit in which the actigraph watches and any paper daily diaries were retrieved. Once actigraph watches were returned to the lab, data were retrieved and saved to the secure server. Actigraphy data were cleaned once and then checked by two other research team members to ensure data quality. Once all actigraphy data were secured on the server, watches were cleared and reset for the next family. Between assessments, families were mailed periodic newsletters and birthday cards to maintain contact and retrieve updated contact information. Families were compensated for their time at each assessment point.
Measures
Demographics.
Primary caregivers reported twins’ age, sex, and ethnicity. Information on socioeconomic status (SES) included household income, family size, and primary and secondary caregiver education were reported by caregivers. An income-to-needs ratio was calculated for each family based on income and family size, using the 2009 federal standards (U.S. Department of Health and Human Services, 2009). A composite measure of family SES, assessed when twins were 12 months old, was calculated from the income-to-needs ratio and both primary and secondary caregiver education. The 12-month SES composite was used in analyses to control for early adversity related to environment (e.g., poverty).
Actigraphy.
Objective sleep parameters were assessed via actigraph watches worn on the twins’ non-dominant wrist for seven consecutive nights (Motion Logger Micro Watch, Ambulatory Monitoring, Inc., Ardsley, NY USA). Motion is measured in one-minute epochs using a zero-crossing mode with these devices. The Sadeh algorithm in Action W-2 software version 2.7.1 (Ambulatory Monitoring) program was used to analyze the sleep data (Sadeh, Hauri, Kripke, & Lavie, 1995; Sadeh, Sharkey, & Carskadon, 1994). Actigraphy has been established as a reliable and valid assessment of sleep among children and adolescents (Acebo et al., 1999; Sadeh & Acebo, 2002). The following sleep parameters were assessed: 1) duration (total hours of sleep, excluding wake periods); 2) latency (minutes in bed before falling asleep); 3) efficiency (proportion of time asleep while in bed); and 4) midpoint of the sleep period (halfway mark between bed and wake time). The midpoint of the sleep period takes into account both the bed and wake time as assessed by the actigraph watches; therefore, it is a robust assessment of the timing of the sleep period. Twins’ bedtimes were determined by the cessation of light and activity as indicated by the actigraphy data. Wake times were determined by the resumption of activity and light. Of the 381 children, 33 (8.7%) had full missing actigraphy data. Otherwise, compliance was excellent, averaging 6.82 (SD = 0.66) of seven nights completed. Mean composites were calculated for duration, latency, efficiency, and midpoint. The standard deviations across the week were calculated for the duration and midpoint variability variables.
Daily Diaries.
Primary caregivers completed daily diary reports for the same seven days the children wore the actigraph watches. Approximately 49.7% of caregivers completed the diaries online, 47.5% completed the paper forms, and 2.8% completed both online and paper diaries. Subjective sleep quality and daytime functioning was assessed with the following four questions: “How did your twins sleep last night?”, “Did your twins seem refreshed after they woke up this morning?”, “How much energy did you twins have today?”, and “How awake did your twins seem today?”. All four questions were responded to on a one to five scale and were compiled to create a daily sleep quality/daytime functioning factor. Diary questions assessing sleep quality and daytime functioning were derived from the Sleep-Wake Diary (Manber, Bootzin, Acebo, & Carskadon, 1996). In general, sleep diaries have been established as a valid assessment of subjective sleep among adolescents and adults (Manber et al., 2006; Suh et al., 2012; Walker, Johnson, Miaskowski, Lee, & Gedaly-Duff, 2010) and parent-reported sleep diaries have also been used to report on children’s sleep behaviors (Price, Farrell, Donovan, & Waters, 2019; Wiggs, Montgomery, & Stores, 2005). However, there is not a universal sleep diary format (Buysse, Ancoli-Israel, Edinger, Lichstein, Morin, 2006). Additionally, self- or parent-reported sleep diaries are often used in conjunction with objective sleep assessments as multiple methods of sleep assessment are important for assessing various aspects of sleep (Doane, Gress-Smith, & Breitenstein, 2015; Gregory & Sadeh, 2012). The first principal component accounted for 59.28% of the variance (item loadings .67-.82) and regression values were retained as the daily diary composite; the weekly average was used in analyses. There were full missing data on 20 children (10 families) where primary caregivers completed neither electronic nor paper diaries. There was excellent compliance with daily diary procedures from caregivers for children without full missing data; an average of 6.78 (SD = 0.71) of seven days of diaries were completed.
12-Month Positive Parent Personality Composite.
Six measures (described in Lemery-Chalfant et al., 2013) were combined into the positive parent personality composite: Life Orientation Test – Revised—Optimism (α = .82; Scheier, Carver, & Bridges, 1994); Heath Hope Scale—Positive Readiness/Expectancy and Temporality (α = .89; Herth, 1991); Interpersonal Reactivity Index—Empathic Concern and Perspective Taking (α = .82; Davis, 1980; Davis, 1983); Self-Compassion Scale—Self Kindness and Mindfulness (α = .91; Neff, 2003); Pearlin Mastery Scale (α = .83; Pearlin & Schooler, 1978); and Self-Expressiveness in the Family Questionnaire—Positive (α = .88; Halberstadt, Cassidy, Stifter, Parke, & Fox, 1995). The first principal component explained 54.55% of the variance (scale loadings .50 −.91) and regression values were retained as the positive parent personality composite. Full information on the measures in the positive parent personality composite is in Supplementary Table 1.
30 Month Parental Stress and Strain Composite.
Six measures (described in Lemery-Chalfant et al., 2013) made up the parental stress composite: Parenting Daily Hassles frequency (α = .81; Crnic & Greenberg, 1990); MOS Social Support Survey (reverse scored; α = .83; Sherbourne & Stewart, 1991); Confusion, Hubbub, and Order Scale (α = .71; Matheny, Wachs, Ludwig, & Phillips, 1995); Center for Epidemiological Studies – Depression (α = .79; Radloff, 1977); Emotional Availability Scale (reverse scored; α = .74; Biringen, Robinson, and Emde, 2000); and Parent Responses to Child Misbehavior – Punitive Discipline (α = .59; Holden & Zambarabo, 1992). The first principal component explained 37.71% of the variance (scale loadings .46-.71) and regression values were retained as the parental stress composite. Full information on the measures in the parental stress composite is in Supplementary Table 2.
Data Analysis
Potential covariates (e.g., child sex, SES), skewness, and kurtosis of variables were examined prior to analyses. Sleep latency was skewed, such that the majority of children reported short latencies; therefore, a natural log transformation was conducted on this variable. Child sex, child age, child body mass index (BMI), family SES, and whether the assessment period took place during the school year versus when school was not in session (i.e., summer or winter break) were all assessed as potential covariates. Whether or not the assessment took place during the summer (or winter break) was dichotomized (summer/break period = 1, school year = 0). Child sex was also dichotomized (females = 1, males = 0). Seven facets of sleep were examined as correlates of the two early life experiences composites: mean sleep duration, mean sleep efficiency, mean sleep latency, mean midpoint time, mean sleep quality, duration variability, and midpoint variability.
A two-level (twins nested in families) multilevel analysis was conducted using Mplus 8.0 (Muthén & Muthén, 1998–2017). Continuous variables were grand-mean centered and robust maximum likelihood estimation was used to handle missing data. An interaction term was created between the parental stress and positive parent personality composites. Sleep quality/daytime functioning composite scores were standardized before entered into the model. Model fit was assessed with RMSEA and CFI. Simple slopes analysis for hierarchical linear modeling probed interactions (Preacher, Curran, & Bauer, 2006). Although the children are twins, this study focused on phenotypic associations across early development and not on genetic and environmental influences on sleep, an analysis that requires a larger sample size.
Results
On average, children slept 8.12 (SD = 0.71) hours a night, had a 90.37% (SD = 5.40) sleep efficiency, and took approximately 25.26 minutes (SD = 21.48) to fall asleep (latency) across the assessment week. The midpoint of the children’s sleep period averaged to 2:23 AM (SD = 0.73). Approximately 28% of children were assessed during the summer or holiday break, with summer participation included as a covariate.
Five of the seven facets of sleep were significantly correlated with the parental stress and/or positive parent personality composites and thus included in the multilevel model: duration, latency, midpoint, caregiver-reported quality, and duration variability (Table 2). The model testing early-life experiences as predictors of all five sleep indicators demonstrated good model fit, RMSEA = .00 and CFI = 1.00. Child sex, BMI, age, family SES, and summer participation were included in the model as covariates. A model constraint was added to the dichotomous Level 1 covariate (i.e., child sex) to constrain the variance of the parameter. Unstandardized regression coefficients are presented due to the restrictions of Mplus. See Table 3 for regression coefficient estimates.
Table 2.
Descriptive Statistics and Zero-Order Correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sleep Duration (hours) | - | |||||||||||||
| 2. Sleep Efficiency (%) | .61** | - | ||||||||||||
| 3. Sleep Latency (minutes)a | −.20** | −.12* | - | |||||||||||
| 4. Sleep Midpoint | −.19** | −.11* | .22** | - | ||||||||||
| 5. Sleep Duration Variability | −.28** | −.16** | .17** | .32** | - | |||||||||
| 6. Sleep Midpoint Variability | −.21** | −.03 | .12* | .39** | .38** | - | ||||||||
| 7. Sleep Quality Compositeb | .08 | −.03 | −.05 | .01 | −.11+ | .03 | - | |||||||
| 8. Parental Stress Composite – 30 months | −.15* | −.03 | .03 | .16* | .20** | .07 | −.22** | - | ||||||
| 9. Positive Parent Personality Composite – 12 months | .21** | .05 | −.12* | −.04 | −.10 | −.04 | .26** | −.32** | - | |||||
| 10. Socioeconomic Status Composite – 12 months | .21** | .13* | −.14* | −.21** | −.16** | −.16** | −.01 | −.21** | −.02 | - | ||||
| 11. Sex | .14* | .06 | .04 | .01 | −.05 | −.03 | −.09+ | −.15* | .09 | −.05 | - | |||
| 12. Age (years) | −.17** | .01 | −.05 | .16** | .03 | .17** | .02 | .06 | .07 | −.13* | .04 | - | ||
| 13. Body Mass Index | −.17** | −.13* | .03 | −.01 | −.07 | −.03 | −.03 | .07 | −.08 | −.14* | .03 | .09 | - | |
| 14. Summer Participation | −.05 | −.07 | .09 | .29** | .10+ | −.06 | .01 | .03 | .02 | −.12* | .002 | −.06 | .02 | - |
| Meanc | 8.12 | 90.37 | 25.26 | 2.23 | .86 | .59 | .01 | -.02 | .06 | .003 | .50 | 8.45 | 16.80 | .28 |
| Standard Deviation | .71 | 5.40 | 21.48 | .73 | .40 | .29 | .65 | .99 | .95 | .80 | - | .45 | 2.85 | - |
| Minimum | 5.62 | 67.18 | .86 | .35 | .15 | .08 | −3.08 | −2.13 | −2.64 | −2.06 | - | 7.58 | 13.19 | - |
| Maximum | 10.01 | 98.80 | 128.3 | 4.79 | 3.20 | 1.93 | .89 | 3.19 | 1.95 | 1.75 | - | 9.66 | 31.98 | - |
| Skewness | −.55 | −1.13 | 2.33 | .60 | 1.53 | 1.03 | −.90 | .69 | −.35 | −.17 | - | .62 | 1.90 | - |
| Kurtosis | .34 | 1.61 | 6.55 | .59 | 4.74 | 1.65 | 1.04 | 1.02 | −.12 | −.50 | - | -.15 | 4.84 | - |
Note. Sleep duration, efficiency, latency, midpoint, and variability indicators were actigraphy-based sleep measures. Sex: Female = 1, Male = 0; SES, socioeconomic status (mean composite of primary caregiver education, secondary caregiver education and income to needs ratio at 12 months); Summer Participation: participated in summer =1, participated during school year = 0.
p <. 10;
p< .05;
p< .01.
Log transformed values used in zero-order correlations and raw scores are presented in descriptive statistics.
Sleep quality and daytime functioning composite from parent reports in daily diaries
Mean for continuous variables and percentage of sample for dichotomous variables.
Table 3.
Multilevel regression coefficients estimating sleep from parental stress and positive parent personality composites as well as the interaction between the two and covariates.
| Duration (hrs) | Latency (mins)a | Midpoint | Duration Variability | Diary Sleepb | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | 95% CI | Est. | SE | 95% CI | Est. | SE | 95% CI | Est. | SE | 95% CI | Est. | SE | 95% CI | |
| Sex | .22** | .08 | 0.07, 0.37 | .06 | .07 | - | .09* | .04 | 0.01, 0.17 | .01 | .04 | - | −.13 | .08 | - |
| Body Mass Index | −.03** | .01 | −0.06, −0.01 | −.01 | .01 | - | −.01 | .01 | - | −.02* | .01 | −0.03, −0.002 | .004 | .01 | - |
| Age | −.28* | .11 | −0.49, −0.06 | −.06 | .09 | - | .29* | .12 | 0.06, 0.51 | .03 | .06 | - | .04 | .17 | - |
| Socioeconomic Status (12 months) | .17** | .06 | 0.05, 0.29 | −.14* | .06 | −0.25, −0.03 | −.11 | .07 | - | −.07* | .04 | −0.14, −0.003 | −.04 | .11 | - |
| Summer | −.06 | .10 | - | .08 | .11 | - | .42** | .12 | 0.18, 0.66 | .06 | .06 | - | .01 | .17 | - |
| Parental Stress (30 months) | −.02 | .05 | - | −..03 | .05 | - | .10 | .07 | - | .06* | .03 | 0.01, 0.12 | −.16 | .10 | - |
| Positive Parent Personality (12 months) | .15** | .06 | 0.04, 0.36 | −.12+ | .06 | -0.24, 0.01 | .002 | .06 | - | −.02 | .03 | - | .25** | .09 | 0.08, 0.42 |
| Interaction (Adversity × Positive Personality) | .002 | .04 | - | −.05 | .05 | - | −.10+ | .05 | −0.02, 0.005 | −.03 | .03 | - | −.04 | .09 | |
Note. N = 381. Unstandardized coefficients are presented due to Mplus restrictions. Sex (Female = 1, Male = 0) and body mass index are within family covariates. Age, summer participation, and SES are between family covariates. Parental stress and positive parent personality composites are between family predictors and sleep is measured at the child level. Est. = unstandardized partial regression coefficient. SE = standard error of the unstandardized coefficient. 95% CI = 95% confidence intervals. The 90% CI for the interaction term with midpoint time is (−0.19, −0.01) and does not contain 0. Sensitivity analyses were run removing children with less than 5 nights of actigraphy data and for children with fewer than 5 daily diaries. Results remained the same or effect sizes were slightly stronger.
p<.10;
p <.05;
p < .01.
Log transformed values used.
Diary sleep is a mean composite of parent reported sleep quality and daytime functioning items from the daily diaries.
Greater positive parent personality predicted longer average sleep duration and better caregiver-reported sleep quality. An approximately 1 SD increase in positive parent personality scores was associated with 0.15 hours increase in duration and 0.25 SD increase in sleep quality scores. Higher parental stress predicted more sleep duration variability. An approximately 1 SD change in parental stress scores was associated with a 0.15 SD increase in sleep duration variability. Child sex, specifically being female, was associated with longer average sleep durations and later midpoints times of the sleep period. Child age was also associated with duration and midpoint of the sleep period, such that younger children had longer durations and an earlier midpoint of their sleep period. Lower BMI was related to longer sleep durations and more variability in duration across the week. Having the assessment period take place in the summer was associated with later midpoint times of the sleep period. Lastly, higher SES was associated with longer sleep durations, shorter sleep latencies, and less variability in duration across the week.
Although not significant (p = .06), we probed the interaction between parental stress and positive parent personality on midpoint time of the sleep period. Simple slopes analysis indicated that parental stress and midpoint time were significantly associated at low levels of positive parent personality (b = .19, p = .03), but not at average (b = .10, p = .18) or high (b = .002, p = .98) levels. Greater parental stress was associated with later midpoint times of the sleep period for children who had caregivers with low positive parent personality. Approximately 22% of families fell into the region of significance for low positive parent personality (Figure 2).
Figure 2.
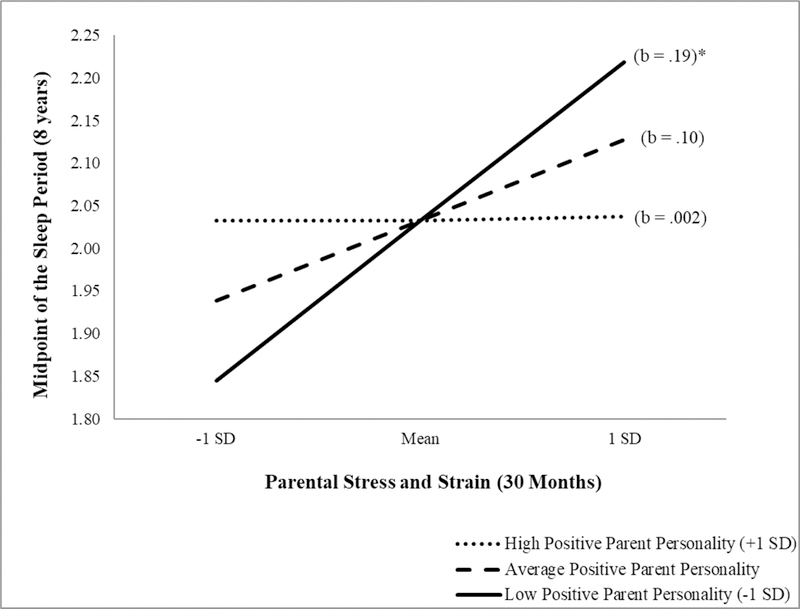
Simple slopes of the interaction between early parental stress and positive parent personality on children’s midpoint of the sleep period (i.e., the time of the midpoint; for example, 2.00 is 2:00 AM). Approximately 22% of families fell into the low positive parent personality group. b = unstandardized regression coefficient. *p<.05.
Discussion
Consistent with hypotheses, the current study found that parental stress was associated with more variability in sleep duration, and positive parent personality was a promotive factor that was associated with longer sleep duration and better parent-reported sleep quality/daytime functioning. Further, the association between parental stress and midpoint of the sleep period was exacerbated for children who had parents with low positive parent personality, such that greater parental stress was associated with later midpoint times for this subset of children. These relations were seen while controlling for early-life SES. Understanding the effects of parent-related factors (both positive and negative) in the context of other sources of vulnerability is important for identifying potentially modifiable risk factors within broader systemic experiences of adversity. Important to note is that all other findings were nonsignificant. In addition to examining early-life parental stress and promotive factors, the current study examined positive parent personality as a source of resilience for child outcomes. Resilience frameworks are important to examine because resilience factors take into account simultaneous negative experiences and promote positive outcomes despite these other ongoing negative influences.
The sleep behaviors of this sample are similar to recently provided guidelines for establishing actigraphy norms in children (see Galland et al., 2018). Our average sleep duration of 8.12 hours for the twins is slightly under pooled means of 6–8 year olds (8.98 hours) and 9–11 year olds (8.85), but does fall within the range of reported durations, which are 8.10 to 9.86 hours for the younger group and 7.87 to 9.52 hours for the older group. There is less information on actigraphy-based sleep efficiency and latency; therefore, our results can only be compared to means across all ages (Galland et al., 2018). Children in the current study had a 90.37% sleep efficiency, which is close to the mean of other studies including 3–14 year olds (i.e., 88.3%, range 79.2–97%). Sleep latency (25.26 minutes) also fell close to the mean of prior reported studies including 3–18 year olds of 19.40 minutes (range 3.8 to 45; Galland et al., 2018). While children in the current study are not meeting duration guidelines of 9–11 hours/night, they are sleeping efficiently.
Findings connecting higher levels of parental stress with greater sleep duration variability are consistent with the prior adult literature that has linked higher levels of adversity with poor sleep in adults (Kajeepeta et al., 2015). Variability in sleep duration among adolescents has been associated longitudinally with reductions in white matter integrity (Telzer, Goldenberg, Fuligni, Lieberman, & Gálvan, 2015). Telzer and colleagues’ (2015) findings held true regardless of total sleep time or bedtime variability, suggesting that day-to-day variation in duration may have detrimental effects on the developing brain in adolescents. However, our findings differ from that of Shafer and Bader (2013), who connected early-life stress to actigraphy-based sleep duration, latency, and efficiency. There are several important differences to note, including that Shafer and Bader (2013) included adult psychiatric outpatients, whereas the current study included a community sample of children. Additionally, we simultaneously estimated the effects of positive parent personality on all outcomes, which may be a more robust predictor of some sleep outcomes at this age. The current study findings extend prior work that has linked greater adversity with poor sleep in children (Sheridan et al., 2013) by including a more comprehensive composite of early-life parental stress and objective sleep in middle childhood.
Prior research suggests that personality traits may influence parenting; however, much of the research has focused on the Big Five personality traits (for review see Prinzie et al., 2009). Limited research has included attributes of personality outside these five dimensions, with optimism as the other main trait assessed. Specifically, socioeconomic adversity has been longitudinally associated with poor parenting practices (e.g., power assertion), except among parents that reported being optimistic and trusting (Kochanska, Aksan, Penney, & Boldt, 2007). Optimism and low neuroticism have also been linked to positive parenting (e.g., responsiveness, affectively positive interactions) of children with difficult temperaments (e.g., proneness to anger; Koeing, Barry, & Kochansha, 2010). Optimism has also been found to buffer the association between poor parenting and social competence among children (Castro-Schilo et al., 2013). Thus, positive parent personality may promote better parenting practices or buffer the impact of poor parenting practices on child outcomes. This study built upon prior work by combining several facets of positive personality into a composite score and relating parental personality in infancy to child health (i.e., sleep).
Positive parent personality was associated with longer sleep durations and better sleep quality/daytime functioning. These findings are in line with prior research that has connected positive parent personality traits, such as internal locus of control, with positive health behaviors among children (Nowicki et al., 2017). Sleep extension studies have found that even small extensions in sleep (e.g., ~30 minutes) are associated with better neurobehavioral functioning and improvements on cognitive tasks and working memory among children and adolescents (de Bruin, van Run, Staaks, & Meijer, 2017; Dewald-Kaufmann, Oort, & Meijer, 2013; Sadeh, Gruber, & Raviv, 2003). Longer sleep duration among children and adolescents has also been associated with better emotion regulation, better quality of life, greater academic achievements, and lower adiposity (see Chaput et al., 2016 for review). Promoting good sleep habits (e.g., longer duration, better quality) may have benefits for a host of other outcomes for children (e.g., cognitive performance, lower adiposity); therefore, it is important to understand factors associated with good sleep among children. Together the direct effects of the current study suggest that negative and positive parent-related early-life experiences may impact different facets of sleep among children. Specifically, parental stress may inhibit a child’s ability to get a consistent amount of sleep each night, while positive parent personality may promote both better quality and quantity of sleep.
Last, we found that for children with parents low on positive personality, higher levels of parental stress was associated with a later midpoint of the sleep period. This finding is consistent with prior literature that has found parental warmth to buffer the association between childhood adversity and allostatic load in adulthood, such that the association between adversity and allostatic load was significant only for those who reported low parental warmth (Carroll et al., 2013). Additionally, maternal nurturance has been found to buffer the association between low childhood SES and metabolic syndrome in adulthood (Miller et al., 2011) and maternal warmth in childhood buffered the association between low childhood SES and pro-inflammatory signaling among adults (e.g., increased inflammatory activity; Chen, Miller, Kobor, & Cole, 2011). The prior studies along with the current findings suggest that positive parental attributes may attenuate the effects of negative early-life experiences on health. The current study finding is also consistent with the theoretical framework put forth by Johnson and colleagues (2013) that the effects of the early environment can be buffered by supportive caregiving. This finding combined with the direct effects of positive parent personality on sleep, suggest that promoting positive attributes (e.g., more hope, optimism, self-compassion) among caregivers may have long-term beneficial effects on sleep behaviors among children.
Strengths and Limitations
Limitations of the current study include the reliance on parental report to assess early-life parental stress and positive parent personality, although we used objective measures of children’s sleep with excellent compliance and utilized a longitudinal design. The extensive assessment of these parent-reported composites likely reduced rater bias, as 12 different reliable and valid scales made up these two composites. Further, this study did not rely on retrospective reports of parental stress and positive parent personality. Other aspects of adversity, such as neglect, were not included in the composite score. However, this study focused on parent-related factors experienced in the first few years of life, and family SES from when the twins were 12 months old was included to control for early environmental adversity, such as living in poverty. The current study used complex modeling that estimated the effects of all predictors simultaneously on all five outcomes, which clarified which predictors influenced which outcomes while controlling for other related variables. In addition, the children were twins, a select group of the broader population of children. There is no evidence that sleep parameters in twin pairs are different from children in the general population, and our descriptive statistics are similar to those obtained in other community samples (El-Sheikh et al., 2013).
Future Directions and Clinical Implications
Future studies should examine potential mechanisms underlying identified associations between early-life experiences and sleep, including emotion regulation and stress responsivity (Hanson & Chen, 2010). Additionally, continued research should examine the effects of parent-related early-life experiences on sleep as the children approach adolescence to determine if the effects change as the children enter another developmental period. Specifically, the findings regarding the association between greater adversity and later midpoint times of the sleep period for children with parents low on positive personality need to be replicated. Associations between early-life experiences and timing of the sleep period have been studied less frequently and need further exploration in both community and clinical populations. Findings from this study suggest that exposure to early-life parental stress is a risk factor for sleep in children, whereas parent positive personality is promotive and could potentially be protective. Understanding these processes can help inform targets of future interventions. Decreasing factors such as parental stress and strain (e.g., daily hassles, depressive symptoms, hopelessness) to enhance positive attributes among caregivers could positively influence child sleep behaviors. For example, the Family Check-Up intervention has been found to be feasible for parents in high stress situations, and has produced improvements in children’s outcomes, including emotional problems, through changes in parent-related factors, such as reduced maternal depression (Reuben, Shaw, Brennan, Dishion, & Wilson, 2015; Smith et al., 2018). Finally, working to reduce the number of factors related to parent adversity, such as increasing social support or lowering depressive symptoms, among caregivers during infancy may have positive ramifications on the development of children’s sleep.
Supplementary Material
Acknowledgements:
This study was supported by two grants from the National Institute of Child Health and Human Development (NICHD R01HD079520; Doane & Lemery-Chalfant, PI and NICHD R01HD086085; Davis & Lemery-Chalfant, PIs). Additionally, the Institute for Mental Health Research (IMHR) funded the launch of the study in infancy.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson AR, Hafer A, & Carskadon MA (1999). Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? Sleep, 22, 95–103. [DOI] [PubMed] [Google Scholar]
- Baiden P, Fallon B, den Dunnen W, & Boateng GO (2015). The enduring effects of early-childhood adversities and troubled sleep among Canadian adults: a population-based study. Sleep Medicine, 16, 760–767. doi: 10.1016/j.sleep.2015.02.527. [DOI] [PubMed] [Google Scholar]
- Biringen Z, Robinson J, & Emde R (2000). Appendix B: The emotional availability scales (3rd ed.; an abridged Infancy/Early Childhood Version). Attachment & Human Development, 2, 256–270. doi: 10.1080/14616730050085626. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, & Morin CM (2006). Recommendations for a standard research assessment of insomnia. Sleep, 29, 1155–1173. [DOI] [PubMed] [Google Scholar]
- Carroll JE, Gruenewald TL, Taylor SE, Janicki-Deverts D, Matthews KA, & Seeman TE (2013). Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proceedings of the National Academy of Sciences, 110, 17149–17153. doi: 10.1073/pnas.1315458110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro-Schilo L, Ferrer E, Taylor ZE, Robins RW, Conger RD, & Widaman KF (2013). Parents’ optimism, positive parenting, and child peer competence in Mexican-origin families. Parenting, Science and Practice, 13, 95–112. doi: 10.1080/15295192.2012.709151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, & Croft JB (2013). Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: A retrospective cohort study. BMC Public Health, 13. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, … Perry GS (2011). Adverse childhood experiences and sleep disturbances in adults. Sleep Medicine, 12, 773–779. doi: 10.1016/j.sleep.2011.03.013 [DOI] [PubMed] [Google Scholar]
- Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T, … Tremblay MS (2016). Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41, S266–S282. doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Katzmarzyk PT, LeBlanc AG, Tremblay MS, Barreira TV, Broyles ST, … Olds T, ISCOLE Research Group. (2015). Associations between sleep patterns and lifestyle behaviors in children: an international comparison. International Journal of Obesity Supplements, 5(Suppl 2), S59–65. doi: 10.1038/ijosup.2015.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Miller GE, Kobor MS, & Cole SW (2011). Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Molecular Psychiatry, 16, 729–737. doi: 10.1038/mp.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Kochanska G, & Ready R (2000). Mothers’ personality and its interaction with child temperament as predictors of parenting behavior. Journal of Personality and Social Psychology, 79, 274–285. doi: 10.1037//0022-3514.79.2.274. [DOI] [PubMed] [Google Scholar]
- Coto J, Garcia A, Hart KC, & Graziano PA (2018). Associations Between Disruptive Behavior Problems, Parenting Factors, and Sleep Problems Among Young Children. Journal of Developmental and Behavioral Pediatrics, 39, 610–620. doi: 10.1097/DBP.0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counts CJ, Grubin FC, & John-Henderson NA (2018). Childhood socioeconomic status and risk in early family environments: predictors of global sleep quality in college students. Sleep Health, 4, 301–306. doi: 10.1016/j.sleh.2018.02.003. [DOI] [PubMed] [Google Scholar]
- Cronin A, Halligan SL, & Murray L (2008). Maternal psychosocial adversity and the longitudinal development of infant sleep. Infancy, 13, 469–495. doi: 10.1080/1525000080232940. [DOI] [Google Scholar]
- Crnic K & Greenberg M (1990). Minor parenting stresses with young children. Child Development, 61, 1628–1637. [DOI] [PubMed] [Google Scholar]
- Davis MH (1980). A multidimensional approach to individual differences in empathy.JSAS Catalog of Selected Documents in Psychology, 10, 85. [Google Scholar]
- Davis MH (1983). Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of Personality and Social Psychology, 44, 113,126. [Google Scholar]
- de Bruin EJ, van Run C, Staaks J, & Meijer AM (2017). Effects of sleep manipulation on cognitive functioning of adolescents: A systematic review. Sleep Medicine Reviews, 32, 45–57. doi: 10.1016/j.smrv.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Dewald-Kaufmann JF, Oort FJ, & Meijer AM (2013). The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: An experimental study. Sleep Medicine, 14, 510–517. doi: 10.1016/j.sleep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Doane LD, Breitenstein RS, Beekman C, Clifford S, Smith TJ, Lemery-Chalfant K (2019). Early life socioeconomic disparities in children’s sleep: The mediating role of the current home environment. Journal of Youth and Adolescence, [Epub ahead of print]. doi: 10.1007/s10964-018-0917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doane LD, Gress-Smith JL, & Breitenstein RS (2015). Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. Journal of Youth and Adolescence, 44, 389–404. doi: 10.1007/s10964-014-0150-7. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, & Buckhalt JA (2013). Economic adversity and children’s sleep problems: multiple indicators and moderation of effects. Health Psychology, 32, 849–859. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Galland BC, Short MA, Terrill P, Rigney G, Haszard JJ, Coussens S, … Biggs SN (2018). Establishing normal values for pediatric nighttime sleep measured by actigraphy: a systematic review and meta-analysis. Sleep, 41. doi: 10.1093/sleep/zsy017. [DOI] [PubMed] [Google Scholar]
- Golley RK, Maher CA, Matricciani L, & Olds TS (2013). Sleep duration or bedtime? exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. International Journal of Obesity, 37, 546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- Gradisar M, Gardner G, & Dohnt H (2011). Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Medicine, 12, 110–118. doi: 10.1016/j.sleep.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Gregory AM & Sadeh A (2012). Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews, 16, 129–36. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Halberstadt A, Cassidy J, Stifer C, Parke R, & Fox N (1995). Self-expressiveness within the family context: Psychometric support for a new measure. Psychological Assessment, 7, 93–103. [Google Scholar]
- Hanson MD & Chen E (2010). Daily stress, cortisol, and sleep: The moderating role of childhood psychosocial environments. Health Psychology, 29, 394–402. doi: 10.1037/a0019879. [DOI] [PubMed] [Google Scholar]
- Herth Kaye. (1991). Development and refinement of an instrument to measure hope. Scholarly Inquiry for Nursing Practice: An International Journal, 5, 39–56. [PubMed] [Google Scholar]
- Holden GW, & Zambarano RJ (1992). Passing the rod: Similarities between parents and their young children in orientations toward physical punishment In Sigel IE, McGillicuddy-DeLisi AV, & Goodnow JJ (Eds.), Parental belief systems: The psychological consequences for children (pp. 143–172). Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Johnson N, & McMahon C (2008). Preschoolers’ sleep behaviour: Associations with parental hardiness, sleep-related cognitions, and bedtime interactions. Journal of Child Psychology and Psychiatry, 49, 765–773. doi: 111/j.1469-7610.2007.01871.x. [DOI] [PubMed] [Google Scholar]
- Johnson N, McMahon C, & Gibson F (2014). Assisted conception, maternal personality, and parenting: Associations with toddler sleep behaviour. Journal of Paediatrics and Child Health, 50, 732–738. doi: 10.1111/jpc.12654. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Riley AW, Granger DA, & Riis J (2013). The science of early life toxic stress for pediatric practice and advocacy. Pediatrics, 131, 319–327. doi: 10.1542/peds.2012-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajeepeta S, Gelaye B, Jackson CL, & Williams MA (2015). Adverse childhood experiences are associated with adult sleep: A systematic review. Sleep Medicine, 16, 320–330. doi: 10.1016/j.sleep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly RJ, & El-Sheikh M (2014). Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology, 50, 1137–1147. doi: 10.1037/a0034501. [DOI] [PubMed] [Google Scholar]
- Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, … Sjödin A (2014). Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors in obesity in danish school children. International Journal of Obesity, 38, 32–39. doi: 10.1038/ijo.2013.147. [DOI] [PubMed] [Google Scholar]
- Koeing JL, Barry RA, Kochanska G (2010). Rearing difficult children: Parents’ personality and children’s proneness to anger as predictors of future parenting. Parenting, Science and Practice, 10, 258–273. doi: 10.1080/15295192.2010.492038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koskenvuo K, Hublin C, Partinen M, Paunio T, & Koskenvuo M (2010). Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Medicine, 11, 17–22. doi: 10.1016/j.sleep.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Kochanska G, Aksan N, Penney SJ & Boldt LJ (2007). Parental personality as an inner resource that moderates the impact of ecological adversity on parenting. Journal of Personality and Social Psychology, 92, 136–150. doi: 10.1037/0022-3514.92.1.13. [DOI] [PubMed] [Google Scholar]
- Kurth S, Olini N, Huber R, & LeBourgeois M (2015). Sleep and early cortical development. Current Sleep Medicine Reports, 1, 64–73. doi: 10.1007/s40675-014-0002-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemery-Chalfant K, Clifford S, McDonald K, O’Brien TC, & Valiente C (2013). Arizona Twin Project: A focus on early resilience. Twin Research and Human Genetics, 16, 404–411. doi: 10.1017/thg.2012.107. [DOI] [PubMed] [Google Scholar]
- Manber R, Bootzin RR, Acebo C & Carskadon MA (1996). The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep, 19, 432–441. [DOI] [PubMed] [Google Scholar]
- Masten AS (2014). Invited commentary: Resilience and positive youth development frameworks in developmental science. Journal of Youth and Adolescence, 43, 1018–1024. doi: 10.1007/s10964-014-0118-7. [DOI] [PubMed] [Google Scholar]
- Matheny AP, Wachs TD, Ludwig JL, & Phillips K (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology, 16, 429–444. [Google Scholar]
- Mathur A, Graham-Engeland J, Slavish DC, Smyth JM, Lipton RB, Katz MJ, & Sliwinski MJ (2018). Recalled early life adversity and pain: The role of mood, sleep, optimism, and control. Journal of Behavioral Medicine, 41, 504–515. doi: 10.1007/s10865-018-9917-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald SW, Kehler HL, & Tough SC (2016). Protective factors for child development at age 2 in the presence of poor maternal mental health: Results from the All Our Babies (AOB) pregnancy cohort. BMJ Open, 10, e012096. doi: 10.1136/bmjopen-2016-012096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcneil J, Tremblay MS, Leduc G, Boyer C, Bélanger P, Leblanc AG, … Chaput J (2015). Objectively‐measured sleep and its association with adiposity and physical activity in a sample of canadian children. Journal of Sleep Research, 24, 131–139. doi: 10.1111/jsr.12241. [DOI] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, & Seeman TE (2011). Pathways to resilience: Maternal nurturance as a buffer against the effects on childhood poverty on metabolic syndrome at midlife. Psychological Science, 22, 1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998-2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Sleep Foundation. (2014). Sleep in America Poll: Sleep in the Modern Family. Retrieved from: http://www.sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2014-sleep-in-the-modern-family.
- Neff K (2003). Development and validation of a scale to measure self- compassion. Self and Identity, 2, 223–250. [Google Scholar]
- Nowicki S, Iles-Caven Y, Gregory S, Ellis G, & Golding J (2017). The impact of prenatal parental locus of control on children’s psychological outcomes in infancy and early childhood: A prospective 5 year study. Frontiers in Psychology, 12; 8:546. doi: 10.3389/fpsyg.2017.00546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palagini L, Domschke K, Benedetti F, Foster RG, Wulff K, & Riemann D (2019). Developmental pathways towards mood disorders in adult life: Is there a role for sleep disturbances? Journal of Affective Disorders, 243, 121–132. doi: 10.1016/j.jad.2018.09.011. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, & Schooler C (1978). The structure of coping. Journal of Health and Social Behavior, 19, 2–21. [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. [Google Scholar]
- Price TE, Farrell LJ, Donovan CL, & Waters AM (2019). Behavioral sleep-related problems in clinically anxious children: A parent-report diary study. Child Psychiatry and Human Development, [Epub ahead of print]. doi: 10.1007/s10578-019-00878-5. [DOI] [PubMed] [Google Scholar]
- Prinzie P, Stams GJJM, Deković M, Reijntjes AHA, & Belsky J (2009). The relations between parents’ Big Five personality factors and parenting: A meta-analytic review. Journal of Personality and Social Psychology, 97, 351–362. doi: 10.1037/a0015823 [DOI] [PubMed] [Google Scholar]
- Psychogiou L, Legge K, Parry E, Mann J, Nath S, Ford T, & Kuyken W (2016). Self-compassion and parenting in mothers and fathers with depression. Mindfulness, 7, 896–908. doi: 10.1007/s12671-016-0528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Reuben JD, Shaw DS, Brennan LM, Dishion TJ, & Wilson MN (2015). A family-based intervention for improving children’s emotional problems through effects on maternal depressive symptoms. Journal of Consulting and Clinical Psychology, 83, 1142–1148. doi: 10.1037/ccp0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A & Acebo C (2002). The role of actigraphy in sleep medicine. Sleep Medicine Reviews, 6, 113–124, .doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Gruber R, & Raviv A (2003). The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Development, 74, 444–455. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Hauri PJ, Kripke DF, & Lavie P (1995). The role of actigraphy in the evaluation of sleep disorders. SLEEP, 18, 288–302. doi: 10.1093/sleep/18.4.288 [DOI] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, & Carskadon MA (1994). Activity-based sleep-wake identification: An empirical test of methodological issues. SLEEP, 17, 201–207. doi: 10.1093/sleep/17.3.201 [DOI] [PubMed] [Google Scholar]
- Schäfer V, & Bader K (2013). Relationship between early-life stress load and sleep in psychiatric outpatients: A sleep diary and actigraphy study. Stress and Health, 29, 177–189. doi: 10.1002/smi.2438. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A re-evaluation of the Life Orientation Test. Journal of Personality and Social Psychology, 67, 1063–1078. [DOI] [PubMed] [Google Scholar]
- Schmid SM, Hallschmid M, & Schultes B (2015). The metabolic burden of sleep loss. The Lancet: Diabetes & Endocrinology, 3, 52–62. doi: 10.1016/S2213-8587(14)70012-9. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS Social Support Survey. Social Science and Medicine, 32, 705–714. [DOI] [PubMed] [Google Scholar]
- Sheridan A, Murray L, Cooper PJ, Evangeli M, Byram V, & Halligan SL (2013). A longitudinal study of child sleep in high and low risk families: Relationship to early maternal settling strategies and child psychological functioning. Sleep Medicine, 14, 266–273. doi: 10.1016/j.sleep.2012.11.006. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129, e232–246. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Harvey AG, Pallesen S, & Hysing M (2017). Trajectories of sleep problems from childhood to adolescence: A population‐based longitudinal study from Norway. Journal of Sleep Research, 26, 55–63. doi: 10.1111/jsr.12443. [DOI] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Hails KA, Dishion TJ, Shaw DS, & Wilson MN (2018). Predictors of participation in the family check-up program: A randomized trial of yearly services from age 2 to 10 years. Prevention Science, 19, 652–662. doi: 10.1007/s11121-016-0679-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suh S, Nowakowski S, Bernert RA, Ong JC, Siebern AT, Dowdle CL, & Manber R (2012). Clinical significance of night-to-night sleep variability in insomnia. Sleep Medicine, 13, 469–75. doi: 10.1016/j.sleep.2011.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor ZE, Larsen-Rife D, Conger RD, Widaman KF, & Cutrona CE (2010). Life stress, maternal optimism, and adolescent competence in single mother, African American families. Journal of Family Psychology, 24, 468–477. doi: 10.1037/a0019870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AK, Netsi E, O’Mahen H, Stein A, Evans J, & Pearson RM (2017). The association between maternal postnatal depressive symptoms and offspring sleep problems in adolescence. Psychological Medicine, 47, 451–459. doi: 10.1017/S0033291716002427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telzer EH, Goldenberg D, Fuligni AJ, Lieberman MD, & Gálvan A (2015). Sleep variability in adolescence is associated with altered brain development. Developmental Cognitive Neuroscience, 14, 16–22. doi: 10.1016/j.dcn.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traub F, & Boynton-Jarrett R (2017). Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics, 139. doi: 10.1542/peds.2016-2569. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2009). The HHS Poverty Guidelines. Washington, DC: U.S. Department of Health and Human Services; Retrieved from https://aspe.hhs.gov/poverty-guidelines. [Google Scholar]
- Walker AJ, Johnson KP, Miaskowski C, Lee KA, & Gedaly-Duff V (2010). Sleep quality and sleep hygiene behaviors of adolescents during chemotherapy. Journal of Clinical Sleep Medicine, 6, 439–444. [PMC free article] [PubMed] [Google Scholar]
- Wang B, Isensee C, Becker A, Wong J, Eastwood PR, Huang R, … Rothenberger A (2016). Developmental trajectories of sleep problems from childhood to adolescence both predict and are predicted by emotional and behavioral problems. Frontiers in Psychology, 7, 1874. doi: 10.3389/fpsyg.2016.01874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Raffeld MR, Slopen N, Hale L, & Dunn EC (2016). Childhood adversity and insomnia in adolescence. Sleep Medicine, 21, 12–18. doi: 10.1016/j.sleep.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M, Haardörfer R, Getachew B, Shah J, Payne J, Pillai D, & Berg CJ (2018). A multivariate analysis of adverse childhood experiences and health behaviors and outcomes among college students. Journal of American College Health, [Epub ahead of print]. doi: 10.1080/07448481.2018.1431892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggs L, Montgomery P, & Stores G (2005). Actigraphic and parent reports of sleep patterns and sleep disorders in children with subtypes of attention-deficit hyperactivity disorder. Sleep, 28, 1437–1445. [DOI] [PubMed] [Google Scholar]
- Wu BW, Skidmore PM, Orta OR, Faulkner J, Lambrick D, Signal L, Williams MA, & Stoner L (2016). Genotype vs. Phenotype and the Rise of Non-Communicable Diseases: The Importance of Lifestyle Behaviors During Childhood. Cureus, 8, 458. doi: 10.7759/cureus.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngblade LM, Theokas C, Schulenberg J, Curry L, Huang IC, & Novak M (2007). Risk and promotive factors in families, schools, and communities: A contextual model of positive youth development in adolescence. Pediatrics, 119, S47–53. doi: 10.1542/peds.2006-2089H. [DOI] [PubMed] [Google Scholar]
- Yeo SC, Jos AM, Erwin C, Lee SM, Lee XK, Lo JC, … Gooley JJ (2018). Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: problems and possible solutions. Sleep Medicine, [Epub ahead of print]. doi: 10.1016/j.sleep.2018.10.041. [DOI] [PubMed] [Google Scholar]
- Ystrom E, Hysing M, Torgersen L, Ystrom H, Reichborn-Kjennerud T, & Sivertsen B (2017). Maternal symptoms of anxiety and depression and child nocturnal awakenings at 6 and 18 months. Journal of Pediatric Psychology, 42, 1156–1164. doi: 10.1093/jpepsy/jsx066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M, Lalani C, Banda JA, & Robinson TN (2018). Sleep duration, timing, variability and measures of adiposity among 8- to 12-year-old children with obesity. Obesity Science & Practice, 4, 535–544. doi: 10.1002/osp4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


