Abstract
Background
Prevention of avoidable preterm birth in Aboriginal and Torres Strait Islander (Indigenous) families is a major public health priority in Australia. Evidence about effective, scalable strategies to improve maternal and infant outcomes is urgently needed. In 2013, a multiagency partnership between two Aboriginal Community Controlled Health Organisations and a tertiary maternity hospital co-designed a new service aimed at reducing preterm birth: ‘Birthing in Our Community’.
Methods
A prospective interventional cohort study compared outcomes for women with an Indigenous baby receiving care through a new service (n = 461) to women receiving standard care (n = 563), January 2013–December 2017. The primary outcome was preterm birth (< 37 weeks gestation). One to one propensity score matching was used to select equal sized standard care and new service cohorts with similar distribution of characteristics. Conditional logistic regression calculated the odds ratio with matched samples.
Findings
Women receiving the new service were less likely to give birth to a preterm infant than women receiving standard care (6·9% compared to 11.6%). After controlling for confounders, the new service significantly reduced the odds of having a preterm birth (unmatched, n = 1024: OR = 0·57, 95% CI 0·37, 0·89; matched, n = 690: OR = 0·50, 95% CI 0·31, 0·83).
Interpretation
The short-term results of this service redesign send a strong signal that the preterm birth gap can be reduced through targeted interventions that increase Indigenous governance of, and workforce in, maternity services and provide continuity of midwifery carer, an integrated approach to supportive family services and a community-based hub.
Keywords: Indigenous, Maternity, Midwifery, Continuity of midwifery care, Health services research, Co-design, Aboriginal and Torres Strait Islander, Community, Closing the gap, Health disparities, Birthing on Country, Birthing in Our Community, Prospective study, Propensity score matching, Birth cohort, Preterm birth, Child mortality, Community investment-ownership-activation, Aboriginal Community Controlled Health Organisations, The Indigenous Birthing in an Urban Setting (IBUS) study
Research in context
Evidence before this study
Indigenous community investment-ownership-activation in service design and delivery improves perinatal outcomes for Indigenous families. Continuity of midwifery carer reduces preterm birth in the non-Indigenous setting. Birthing on Country is a complex intervention incorporating these service characteristics but there is a dearth of evidence on this topic.
Added value of this study
This study provides evidence that an urban Birthing on Country Service has reduced preterm birth for Indigenous families. Established through local Indigenous community investment-ownership-activation and in partnership with a mainstream health service, key components of the Service include: a partnership Steering Committee, Indigenous governance, a co-designed sevice, local leadership, enhanced caseload midwifery service, increased Indigenous workforce focused on family wellbeing and strength-based approaches to birthing and parenting, and improving cultural capability of the non-Indigenous workforce. This Service has resulted in greater integration across Indigenous community-based and tertiary maternal infant health care and support service for families.
Implications of all the available evidence
Prevention of avoidable preterm birth in Aboriginal and Torres Strait Islander families is a major public health priority in Australia. Evidence for effective, scalable strategies to improve maternal and infant outcomes among Aboriginal and Torres Strait Islander families is urgently needed to inform policy and practice. Replication of this Birthing on Country Service should be tested in other settings as a key strategy to reduce Indigenous preterm birth rates in Australia.
Alt-text: Unlabelled Box
1. Introduction
Health disparities between Indigenous peoples and their non-Indigenous counterparts in colonised countries start early in life [1]. Strategies to address disparities are more likely to succeed if they are led by, or conducted in partnership with, Indigenous organisations and build Indigenous capacity and engagement. A realist review of services for antenatal and infant health promotion found local Indigenous community investment (collective understanding and valuing of a program), ownership (program is ‘ours’) and activation (high-level community participation) is associated with increased antenatal attendance and breastfeeding, a higher proportion of children meeting developmental milestones, and cultural benefits including exposure to Indigenous language and culture [2]. This paper describes the impact on preterm birth of a partnership approach to developing and evaluating a new Service co-designed and delivered by two Aboriginal Community Controlled Health Organisations and a tertiary maternity service in Australia. The Service is called: ‘Birthing in Our Community’ [3].
1.1. Reducing child mortality by targeting preterm birth
Since the Australian Government committed to ‘Closing the Gap’ between Indigenous and non-Indigenous disadvantage in 2007, the target to halve the gap in child mortality rates (< 5-years) is not on track [4]. Some health gains have been realised with a 10% reduction for Indigenous children from 182 per 100,000 in 2008 to 164 per 100,000 in 2017, however the non-Indigenous rate reduced by 33% (104 to 68 per 100,000) seeing an increase in the gap (2·4 times higher for Indigenous children) [4]. Most Indigenous child deaths (84%) occur in the first year of life and 56% of these are from perinatal conditions such as preterm birth [4]. In 2008, preterm birth rates were 13·3% for Indigenous women compared to 8·0% for non-Indigenous women [5] and almost unchanged at 13·6% and 8·4% in 2017 [6]. Not only is preterm birth an important contributor to childhood disability and mortality, it marks the genesis of preventable chronic diseases in adult life, including: diabetes, cardiovascular and renal disease [7]. Chronic diseases are overrepresented in the Indigenous population and are a major contributor to premature death [8]. Increasing term birth will impact all other Closing the Gap targets (e.g. life expectancy, literacy, year 12 completion and employment targets) as babies born preterm are at greater risk of dying in infancy and more likely to be diagnosed with developmental delays that impact school readiness and attainment [4]. The known modifiable causes of preterm birth include inadequate antenatal care, psychosocial stress, infections, smoking in pregnancy and teenage pregnancy [7]. The World Health Organisation recommends preterm birth be a priority area for research and program innovation [7].
1.2. Birthing on country
For four decades there has been a global movement led by Indigenous people to return birthing services to Indigenous communities. In Canada the community driven initiative to establish the Inuulitsivik Midwifery Service in a remote Inuit community meant women were no longer flown 8 h away for birth [9]. This change was seen as an important contributor to the cultural healing required to address the impact of colonisation which had weakened the health, strength and spirit of the community [9]. Evaluation data reported high community engagement, local training of Inuit midwives, improved birth outcomes and very low intervention rates with caesarean section facilities not available on site [9]. Subsequently there has been a return of birthing services and onsite midwifery training to other remote Inuit communities as they gain control of their health services and address the social determinants of health with holistic services and employment and education initiatives for First Nations women [10]; initiatives supported by the Society of Obstetrician and Gynaecologists of Canada [11]. In 2013, an Indigenous birth centre also opened in urban Toronto, Canada. New Zealand also has many small midwifery run birthing units, enabling Maori women to birth close to home, and practice cultural traditions, supported by family [12].
During the same period, Australia did not experience this progressive movement of returning birthing services to communities. On the contrary, maternity services closed and centralised, resulting in women travelling hundreds of miles from family and community for birth. This disproportionately impacts Indigenous women, particularly in rural and remote communities. Indigenous women regularly request the return of Birthing on Country which strengthens babies connection to their traditional lands in a deeply cultural way, affording both privileges and responsibilities for life [13], [14]. Following a review of maternity services in Australia in 2009 [15], Birthing on Country Services were defined as: “maternity services designed and delivered for Indigenous women that encompass some or all of the following elements: are community based and governed; allow for incorporation of traditional practice; involve a connection with land and country; incorporate a holistic definition of health; value Indigenous and non-Indigenous ways of knowing and learning, risk assessment and service delivery; are culturally competent and are developed by, or with, Indigenous people.” [14] Although national policy recommends these services be developed [16], implementation is limited by a lack of funding and mechanisms to support Indigenous control of maternity services [16]. No Indigenous birth centres exist in Australia today.
1.3. Study setting: the Birthing in Our Community Service
In 2013, the Birthing in Our Community Service was established in Brisbane, Australia. This was in response to the evaluation of an Indigenous-specific antenatal clinic operating since 2004 at a tertiary maternity hospital. The evaluation compared outcomes between Indigenous and non-Indigenous women, demonstrating a widening gap in preterm birth (relative increase of 51% 1998–2009) with the Indigenous rate at 16% [17]. At the stakeholder engagement workshop disseminating these results participants recommended the partnering of Aboriginal Community Controlled Health Organisations and the tertiary hospital in a concerted effort to improve cultural competence across the maternity journey and birthing outcomes for Indigenous families [3]. Reducing preterm birth was highlighted by participants as a priority area requiring intervention. This resulted in a multiagency partnership between three organisations.
The Institute for Urban Indigenous Health was established in 2009 by four Aboriginal and Torres Strait Islander Community Controlled services, with a vision for healthy, strong and vibrant Indigenous families and communities. It drives the development and implementation of transformational change in healthcare delivery for urban Indigenous Australians in South East Queensland, one of the largest, fastest growing Indigenous populations in Australia. Key to their approach has been the strategic use of data to drive system reform and continuous improvement; fostering partnerships to increase the responsiveness of tertiary services; and coordinating a regional approach to the modelling, training and development of a skilled urban Indigenous health workforce.
The Aboriginal and Torres Strait Islander Community Health Service Brisbane Limited was established in 1973 as one of the first four Aboriginal Community Controlled Health Services in Australia. They now provide care for around 10,000 Indigenous people across six multidisciplinary primary health care clinics; a large residential aged care facility; early childhood education facilities; and two maternal and child health care centers. The flagship clinic and head office are located in the inner-city suburb adjacent to the Hospital.
Mater Mothers' Hospital is a tertiary teaching hospital providing maternity services to approximately 5000 women accessing public services per annum; approximately 300 are Indigenous babies. Co-located with a similar sized private hospital it is one of the largest maternity facilities in Australia. They have multiple service models including Maternal Fetal Medicine (complex problems), shared care with general practitioners, midwifery and obstetric antenatal clinics and caseload midwifery group practices. The Indigenous antenatal clinic was co-located with the Indigenous liaison service which is well respected in the Indigenous community.
The partners co-designed the maternal infant health services with community stakeholders to enable greater Indigenous governance and control of the service [17]. The ‘active ingredients’ of this complex intervention have at times demonstrated reductions in preterm birth in either different population groups or smaller studies; yet they have never been combined and tested in this way. They were based on the importance of Indigenous community investment-ownership-activation in improving maternal and infant health outcomes [2], the Birthing on Country literature [14], the evidence showing continuity of carer through caseload (one-to-one) midwifery reduces preterm birth [18] and the importance of respectful, evidence-based, culturally capable care [19]. The new Service is a complex intervention with multiple inputs and a program logic to guide evaluation and further details are available in the research protocol [20]. The key components of the Birthing in Our Community Service are outlined below.
1.3.1. Indigenous governance and partnership Steering Committee
The Service is governed by a partnership Steering Committee underpinned by a Memorandum of Understanding (MOU) and Statement of Commitment, with clearly articulated shared goals and commitment. Strong Indigenous leadership has driven the design, development and implementation of the Service. The Steering Committee commenced with all three chief executive officers (CEOs) (two Indigenous) committing to the partnership and meeting regularly. The Steering Committee met monthly in the first few months prior to the launch then reduced gradually over five years and now meet twice a year. Although membership has changed over time, the CEOs (two have changed since inception with a renewed Statment of Committment and MOU soon to be signed) are still occasionally involved in the regular meetings that are attended by senior managers who have financial, clinical and managerial control of the services and are able to make changes directly in response to regular reports and monitoring. There is also a monthly senior managers meeting, with all partners represented, who are responsible for on the ground management, reporting and troubleshooting. The Institute is now the major funds holder for the Service, purchasing additional midwifery services from the Hospital, employing the Service Manager, and operating the community-based Hub facility.
1.3.2. Caseload midwifery
Available to women 24/7 throughout pregnancy, birth and up to six weeks postnatally by a known midwife and back-up midwives if the primary midwife is off duty (initially one group of four caseload midwives was established but this was increased to two groups of four midwives when partners received additional funding from government). Antenatal care is delivered according to women's preferences, including in the home, Community-Based Hub or hospital for women with complex needs or who live outside of the designated home visiting area.
1.3.3. Indigenous workforce strategy
The Indigneous workforce strategy meets the dual purpose of providing a culturally competent and responsive maternity services workforce and addresses key social determinants of health: education, income and career development for Indigenous women. Dedicated resources are allocated by the two Indigenous organisations to support Indigenous midwifery trainees through cadetships with an Indigenous new graduate midwifery position also being trialled. Indigenous staff are actively recruited and supported to identify pathways for training and career development. Frontline staff are provided access to regular clinical and cultural supervision, along with contextualised training in areas specific to need.
1.3.4. Indigenous-controlled community-based hub
The Hub was established in the early years when additional government funds were recieved. It serves as the base for the Service, with transport to facilitate access to the hospital, home and Hub. The Hub provides a culturally enabling environment, where women and families not only access multidisciplinary maternity and infant care, but also connect, interact, share and learn from each other and from elders with community drop in days, cook-ups and other activities.
1.3.5. Integrated family services
Maternity-specific services are centred around the family, offering a ‘one stop shop’ approach with multidisciplinary providers–employed or engaged by the Indigenous partner organisations–delivering a full range of primary maternity and infant health and related services. Indigenous Family Support Workers play a critical role in connecting and securing care pathways for women and families. There is a strong focus on social and emotional health and well-being, mother and infant attachment and ready access to social work, perinatal psychology and parenting support. Linkages with local family doctors at Aboriginal Community Controlled Health Organisations are actively fostered through shared electronic health records, phone and in-person communication. Active planning is undertaken well in advance for a transition of care beyond the 6-week postnatal period to primary providers and specialised child health and onsite paediatric services as needed.
2. Methods
2.1. Study design
A prospective cohort study using routinely collected hospital clinical data was conducted. In our setting, within the Indigenous context and respecting the view of the Steering Committee, an explanatory trial was not possible. The Steering Committee felt the need to provide services differently was urgent and did not want to delay implementation to apply for research funding to conduct a trial nor did not want to limit women's access to, or risk a lack of engagement in, this new Service.
2.2. Procedure
The Birthing in Our Community Service started with four caseload midwives providing care in an ‘all risk’ service to ~ 140 women carrying an Indigenous baby annually. The caseloads were reduced to ~ 120 per annum to account for higher than expected travel time and working hours identified in the first year. From January 2017, further government funding enabled scaling up of the Service to include an additional four midwives, increasing caseload care to ~ 240 women annually.
During the study, when a woman pregnant with an Indigenous baby was referred by her family doctor to the tertiary service, she was allocated by the Hospital General Practitioner liaison officer either to Birthing in Our Community or any other service available (referred to as Standard Care in this paper). Other services include: shared care with her family doctor; midwifery and medical antenatal clinics; specialised clinics (e.g. diabetes, drug and alcohol dependency; Maternal Fetal Medicine); caseload midwifery for non-Indigenous women including specialised services (e.g. Young Women's < 25 years). Women were not referred to the Service if: Indigenous status was not identified on referral form (most common and usually gets noted after the ‘booking-in’ visit and will be transferred into the service if places available); they requested another service (shared care with family doctor most common); no available places for the month their baby was due, or they were allocated to another specialised service (eg. drug and alcohol dependency clinic).
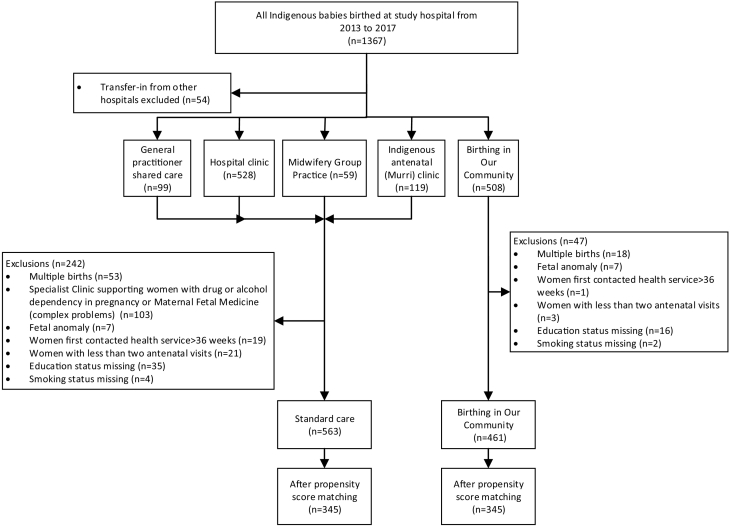
2.3. Participants
Birth records of all Indigenous babies born at the Mater Mothers Public Hospital between 1 January 2013–31 December 2017 were extracted (n = 1367). In total, n = 343 observations were excluded from the analysis if they were women: transferred in from other hospitals (n = 54); with a multiple birth (n = 71); attending the specialised clinics for drug and alcohol dependency in pregnancy (CHAMP) or for complex problems (Maternal Fetal Medicine) (n = 103); with a known fetal anomaly (n = 14); whose first contact with any health service was > 36 weeks (n = 20); were not exposed to either model defined as < 2 antenatal visits (n = 24); or missing key variables (n = 57) (Fig. 1). In total 1024 women were included in analysis, 563 received Standard Care and 461 received the Birthing in Our Community Service.
Fig. 1.
Study participants' flowchart.
2.4. Outcomes
Outcomes were defined a priori with four primary outcomes of interest, one being the proportion of women who had a preterm birth, at least 20-weeks' gestation or 400 g birthweight (Australian definition for viability), and < 37 completed weeks gestation. Regular audits showed a reduction in preterm birth faster than anticipated with full primary analysis due to occur at year five. Early analysis of data on preterm birth was proposed and is reported here.
2.5. Ethics
Ethical approval was granted by the Mater Health Services Human Research Ethics Committee (HREC/15/MHS/24) and University of Queensland Human Research Ethics Committee (2015000624).
2.6. Statistical analysis
The sample size required (n = 350 in each group) was calculated based on the preterm rate with an expected reduction from 16% to 9%, 80% power and a type 1 error of 5% (similar to a previously reported reduction in an Indigenous specific antenatal program [21]). Outcomes were presented as frequencies and odds ratios (ORs) for categorical variables, means and standard deviations for normally distributed continuous variables, and medians and interquartile ranges (IQR) for non-normally distributed continuous and ordinal variables. Propensity score matching analyses were performed to account for confounding bias in the estimation of the treatment effects using observational data. The study adjusted the following characteristics which were thought to potentially contribute to preterm birth, derived from the literature and well documented in our dataset: maternal age; body mass index; Indigenous mother, education, marital status; parity; smoking at booking; previous caesarean section, stillbirth or preterm birth; pre-existing hypertension, diabetes, liver disease, renal disease, thyroid disease, haematological disease or heart disease; pregnancy complications such as pregnancy induced hypertension, gestational diabetes, and antepartum haemorrhage. The Socioeconomic Index for Areas (SEIFA) quintiles were used to reflect socioeconomic status.
A logit regression model was performed to calculate the propensity score for each birth. The propensity score was the predicted probability of a woman accessing the Birthing in Our Community Service, given their profile in terms of the above risk factors. The births were matched on a one-to-one basis without replacement, using callipers of width of 0·2 standard deviation of the logit of the propensity score (calliper 0·18). The balance of the covariates before and after matching (Table 1) were checked using Rubin's B, Rubin's R and the standardised differences. Rubin's B summarise the overall model bias and less than 25% indicate the two groups have been adequately balanced, and Rubin's R is the ratio of variances between the two groups, and a value close to 1·0 indicate adequate balance [22]. The standardised difference for each covariate was also reported with less than 10% indicating a sufficient balancing in terms of the covariates being assessed [23]. Models were developed based on both unmatched and the matched samples. For the unmatched sample, the univariate model was developed with unadjusted odds ratios (OR) calculated. Conditional logistic regression was used for the matched sample to accommodate the 1:1 matching [23]. We used OR to interpret the relative measure of effect, which allowed the comparison between the intervention group and Standard Care. The intervention group had a higher proportion of Indigenous mothers who appear to be more disadvantaged when comparing the demographic characteristics between the groups. Indigenous mothers are known to experience higher rates of preterm birth. To test the potential impact of the Indigenous status of the mother, a number of Standard Care women recieving caseload midwifery carer and the robustness of our model and findings; two sensitivity analysis were conducted. One with only Indigenous mothers and the other excluding women in other caseload models, both using the same strategy described above. All analyses were performed with Stata software, version 14·1.
Table 1.
Demographic and baseline characteristics of BiOC and standard care before and after propensity score matching.
| Before matching |
After matching |
|||||
|---|---|---|---|---|---|---|
| Standard care (n = 563) |
BiOC (n = 461) |
Bias (%) |
Standard care (n = 345) |
BiOC (n = 345) |
Bias (%) |
|
| Age (Mean ± SD) | 27·3 ± 6·3 | 26·0 ± 6·2 | − 19·5 | 26·1 ± 6·2 | 26·0 ± 6·3 | 2·2 |
| BMI (Median, IQR) | 24·5 (20·8–30·9) | 24·4 (20·8–29·8) | − 8·6 | 24·4 (20·5–30·5) | 25·2 (20·8–30·5) | 3·7 |
| Indigenous mum | 375 (63·3%) | 432 (90·6%) | 71·7 | 296 (87·3%) | 294 (86·7%) | − 0·7 |
| Socioeconomic status (SEIFA) | ||||||
| Quintile 1 (most disadvantaged) | 109 (19·4%) | 119 (25·8%) | 15·5 | 77 (22·3%) | 74 (21·5%) | − 2·1 |
| Quintile 2 | 86 (15·3%) | 52 (11·3%) | − 11·8 | 43 (12·5%) | 46 (13·3%) | 2·6 |
| Quintile 3 | 86 (15·3%) | 82 (17·8%) | 6·8 | 57 (16·5%) | 54 (15·7%) | − 2·3 |
| Quintile 4 | 159 (28·4%) | 133 (28·9%) | 1·3 | 104 (30·1%) | 101 (29·3%) | − 1·9 |
| Quintile 5 (most advantaged) | 123 (21·9%) | 75 (16·3%) | − 14·2 | 64 (18·6%) | 70 (20·3%) | 4·4 |
| Education | ||||||
| < Grade 10 | 53 (9·4%) | 38 (8·2%) | − 4·1 | 31 (9·0%) | 38 (11·0%) | 7·1 |
| Grade 10–12 | 374 (66·4%) | 334 (72·5%) | 13·1 | 248 (71·9%) | 243 (70·4%) | − 3·1 |
| Tertiary | 136 (24·2%) | 89 (19·3%) | − 11·8 | 66 (19·1%) | 64 (18·6%) | − 1·4 |
| Marriage status | ||||||
| Married or de facto | 300 (53·3%) | 180 (39·1%) | − 28·8 | 150 (43·5%) | 158 (45·8%) | 4·7 |
| Not married or de facto | 255 (45·3%) | 273 (59·2%) | 28·1 | 189 (54·8%) | 179 (51·9%) | − 5·9 |
| Not stated | 8 (1·4%) | 8 (1·7%) | 2·5 | 6 (1·7%) | 8 (2·3%) | 4·6 |
| Parity (Median, IQR) | 1(0–2) | 1(0–2) | − 5·1 | 1(0–2) | 1(0–2) | 5·7 |
| Smoking at booking | 190 (33·8%) | 161 (34·9%) | 2·5 | 128 (37·1%) | 138 (40·0%) | 6·1 |
| Previous caesarean sections | 103 (18·3%) | 68 (14·8%) | − 9·5 | 53 (15·4%) | 61 (17·7%) | 6·2 |
| Previous stillbirths | 15 (2·7%) | 10 (2·2%) | − 3·2 | 9 (2·6%) | 10 (2·9%) | 1·9 |
| Previous preterm births | 11 (2·0%) | 8 (1·7%) | − 1·6 | 6 (1·7%) | 7 (2·0%) | 2·2 |
| Maternal comorbidities | ||||||
| Diabetes disease | 31 (5·5%) | 23 (5·0%) | − 2·3 | 19 (5·5%) | 19 (5·5%) | 0·0 |
| Liver disease | 15 (2·7%) | 14 (3·0%) | 2·2 | 9 (2·6%) | 12 (3·5%) | 5·2 |
| Heart disease | 35 (6·2%) | 31 (6·7%) | 2·1 | 25 (7·3%) | 24 (7·0%) | − 1·2 |
| Renal disease | 62 (11·0%) | 61 (13·2%) | 6·8 | 36 (10·4%) | 36 (10·4%) | 0·0 |
| Thyroid disease | 24 (4·3%) | 10 (2·2%) | − 11·9 | 8 (2·3%) | 10 (2·9%) | 3·3 |
| Haematological disease | 141 (25·0%) | 158 (34·3%) | 20·3 | 105 (30·4%) | 100 (29·0%) | − 3·2 |
| Essential hypertension | 37 (6·6%) | 17 (3·7%) | − 13·1 | 18 (5·2%) | 17 (4·9%) | − 1·3 |
| Current pregnancy complications | ||||||
| Gestational diabetes | 46 (8·2%) | 37 (8·0%) | − 0·5 | 29 (8·4%) | 28 (8·1%) | − 1·1 |
| Pregnancy induced hypertension, mild, moderate or severe preeclampsia | 12 (2·1%) | 15 (3·3%) | 6·9 | 10 (2·9%) | 6 (1·7%) | − 7·2 |
| Antepartum Haemorrhage (APH) | 12 (2·1%) | 15 (3·3%) | 6·9 | 10 (2·9%) | 6 (1·7%) | − 7·2 |
Note: BiOC = Birthing in Our Community.
Rubin's B: 84·9% before matching and 21·3% after matching.
Rubin's R: 0·5 before matching and 0·9 after matching.
2.7. Role of the funding source
Funding from partner organisations was used to establish the Service. The Queensland Government funded an increase in service capacity including several Indigenous specific positions and a Community-Based Hub. NHMRC grant was awarded following a peer review process and enabled the research. The NHMRC did not have any role in study design, data collection, data analysis, data interpretation, or writing of this paper. In-kind support from partner organisations and universities provides employment for those in the investigator team not paid directly from the grant. They also provide research support and infrastructure (e.g. computers, office space).
3. Results
During 2013–2017 a total of 1367 observations were Indigenous births at the study hospital. Of these, 343 (25·1%) were excluded, leaving 1024 observations for analysis: 461 from the Birthing in Our Community Service and 563 from Standard Care. On average women in the Birthing in Our Community Service had their first antenatal contact with any health provider at 9·5 weeks (Median 6, IQR 6–11) with 79.4% receiving care in the first trimester and women in Standard Care started at 10·9 weeks (Median 7, IQR 6–14) with 76.3% receiving care in the first trimester. Eighty-nine percent of women in the Birthing in Our Community Service had booked into the study hospital by second trimester (Median 16, IQR 12–20) compared to 80.2% for women in Standard Care (Median 18, IQR 14–25). The majority of women in both groups had a dating scan; 87.9% in the Birthing in Our Community Service and 89.2% in Standard Care having either a dating, morphology or nuchal scan in pregnancy.
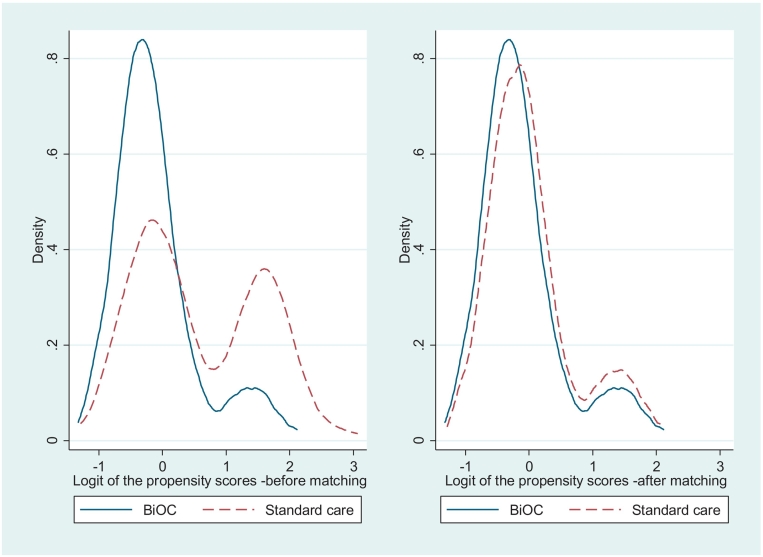
Before propensity score matching, the Birthing in Our Community and Standard Care cohorts had significantly different maternal and pregnancy characteristics. Women who received care through Birthing in Our Community were more likely: to be Indigenous mothers, younger, single, with lower levels of education, in the most disadvantaged SEIFA quintile, to have renal disease, haematological conditions, pregnancy induced hypertension, mild, moderate or severe preeclampsia, or to have an antepartum haemorrhage (Table 1). Women in Standard Care were more likely to have had a previous caesarean section or stillbirth, thyroid disease or essential hypertension. However, the propensity score matching process balanced these potential confounders between the cohorts. The Rubin's B was 84·9% before matching but it was reduced to 21·3% after matching. The Rubin's R was 0.5 before matching and 0·9 after matching. The standardised difference of covariates are all less than 10% and the largest one was 7·2% which suggests the matched cohorts are highly similar in terms of the covariates assessed (Table 1). Density distributions of the logit of the propensity scores for the two cohorts before and after matching also showed that after matching the propensity scores distribution are near-identical (Fig. 2). More than 74% of the women in the new Service were successfully matched with women in Standard Care by their propensity scores which resulted in a 345 equal-sized cohort pairs after matching.
Fig. 2.
Density distribution of the logit of the propensity score for BiOC and Standard care cohorts before and after propensity score matching.
Crude odds ratio estimates for the association of the Birthing in Our Community Service and preterm birth in the before matching cohort were significantly reduced (OR 0·57, 95% CI 0·37–0·89). After matching the odds of having preterm birth in the new Service remained significantly lower (OR 0·50, 95% CI 0·31–0·83), indicating women who underwent the new Service were less likely to have a preterm birth than those who received Standard Care (Table 2). Further analysis examining Indigenous mothers only showed a similar reduction with OR 0·51 (95% CI 0·30, 0·89); similiar to when women in Standard Care who received caseload midwifery were excluded OR 0·51 (95% CI 0·32, 0·83). Further details presented in the supplement Tables S1, S2, S3 and S4.
Table 2.
Frequency and rate of preterm births by model of care before and after propensity score matching.
| Outcomes | Before matching (n = 1024) |
|||
|---|---|---|---|---|
| Standard care (n = 563) | BioC (n = 461) | OR (95% CI) | P-value | |
| Preterm births | 65 (11·6%) | 32 (6·9%) | 0·57 (0·37, 0·89) | 0·013 |
| Term births | 498 (88·4%) | 429 (93·1%) | Reference | |
| Outcomes | After matching (n = 690) |
|||
|---|---|---|---|---|
| Standard care (n = 345) | BioC (n = 345) | OR (95% CI) | P-value | |
| Preterm births | 48 (13·9%) | 26 (7·5%) | 0·50 (0·31, 0·83) | 0·008 |
| Term births | 297 (86·1%) | 319 (92·5%) | Reference | |
4. Discussion
This study found that women having an Aboriginal or Torres Strait Islander baby who received the Birthing in Our Community Service had a significant reduction in the odds of having a preterm birth compared to women receiving Standard Care (reduced by half). This innovative, complex intervention has multiple embedded components which we hypothesised would work synergistically to improve birth outcomes and it did. A systematic review of continuity of midwifery care found a 24% reduction in preterm birth [18] yet a randomised trial of this model including women with risk factors did not reach a statistically significant level, despite improving other health outcomes at reduced cost [24]. There are mixed results in the Indigenous setting with no randomised trials, small numbers in most studies, a wide variation in methodological quality and very few services providing caseload midwifery care across the continuum [14], [25], [26], [27]. Three services with high levels of community investment-ownership-activation (without caseload midwifery) in urban settings found significant improvements in the quality of antenatal care and lower rates of preterm birth, when compared to controls, however authors noted selection bias as a potential confounder [21], [28]. Another statewide initiative that provides continuity of antenatal and postnatal (not birthing) care with a midwife and Aboriginal health worker working together to provide a culturally appropriate service found improved antenatal attendance and reduced preterm birth [29]. Our study builds on current evidence with a stronger design and analysis than many previous studies as we were able to reduce the risk of selection bias. Another service established for Indigenous women from remote communities relocating to an urban setting for birth where they received caseload midwifery found significant improvements in the quality of care, though no reduction in preterm birth. The authors hypothesised this was due to the limited changes that occurred in the remote communities where women received most of their antenatal care [30]. Additionally, little community investment-ownership-activation occurred in these sites.
Our results suggest reducing preterm birth is possible when targeting Indigenous women early for antenatal care and providing culturally safe continuity of carer within a holistic service with high levels of community investment-ownership-activation and health service leadership across partner organisations. We observed a 50% reduction in preterm birth which is similar to the observational study of caseload midwifery for young women (same setting), reporting a 41% reduction in preterm birth for caseload care in comparison to those receiving routine or community based antenatal care only [31]. It could be that greater gains are possible when targeting vulnerable women who may have more modifiable risk factors amenable to change. The study of young women determined that the service, community based and delivered in partnership with a non-government organisation providing additional support to vulnerable women, was exerting its effect by facilitating early engagement in pregnancy, enabling trusting relationships between women and care providers, and providing opportunities for early health and social support interventions that impacted positively on birth outcomes [32]. Similar mechanisms are likely to be impacting in our current study. The new Service is popular with families and in high demand without advertising. Women are reporting an increase in culturally capable care (unpublished data currently being analysed from the two month postnatal survey) with cultural supervision for midwives and family support workers aimed at ensuring the impact of colonisation and trauma is understood by all staff and supported by onsite perinatal psychologist with expertise in trauma-informed care. Similar to the First Nations services in Canada, this Service is also addressing the social determinants of health with holistic services alongside employment and education initiatives, including midwifery training, for Indigenous women. The addition of Indigenous family support workers, who work side-by-side with the midwives, strengthens the cultural capability of this Service and capacity for relationship-based care and support for stressors (e.g. financial, homelessness, violence, legal, child safety services and food insecurity). Family support workers lead a series of activities that strengthen women's families self-identified needs and aspirations and enhance their connection to culture and community. This is achieved through the community-based hub, with a design that is homelike and welcoming, where a majority of staff are Indigenous (e.g. reception, transport, manager, paediatric co-ordinator), well connected to the community and where women feel safe. Women access a large kitchen where they can make themselves tea or coffee and healthy fruit and other food is available. Weekly ‘Community Days’ provide opportunities for women to come together to learn and celebrate their cultural heritage and draw support from other women (peer support) and staff from their community. Senior women (Aunties and Elders) are also involved in some community days, sharing stories and ‘yarns’ of growing up kids and being culturally strong. Some days women participate in the preparation and consumption of nutritious meals overseen by a visiting dietician and the family support workers. Creative activities including visual diaries, belly casting and infant hand and feet casting (arts health) are facilitated by Indigenous staff trained in trauma informed techniques. Specialised social workers and psychologists support these interventions and also participate in the community days where women are able to develop relationships with them. This in turn enhances the acceptability of referral to these workers when more individual therapeutic support would be beneficial. Family support workers are also often visiting women in their homes or at the hospital as not all women attend the hub for care. The transfer of funds from government to an Aboriginal Community Controlled Health Organisation for the upscale contributed to a strengthening of community governance with this partner organisation controlling the majority of the resources for the Service. This Service redesign demonstrates a shift from the fragmented care delivered by multiple providers where women ‘fell through the cracks’ [33]. It has greater holistic and supportive integration of a multidisciplinary team: Indigenous family support workers strengthen women's networks and work alongside health professionals and hospital based Indigenous liaison officers who provide respectful clinical care as recommended in The Lancet papers on midwifery [34] and maternal health [19].
4.1. Strengths and limitations
This is the first paper reporting the efficacy of a complex intervention designed to implement the national Birthing on Country policy [16], [35]. Our study included all eligible Indigenous births and controlled for potential confounders through propensity score matching. The modelling is superior to conventional regression modelling when the number of events is low compared to the number of confounders (seven or fewer events per confounder), as in this study, because it produces less biased, more robust, precise estimates [36]. More than 70% of the women in the Birthing in Our Community Service were successfully matched to women in Standard Care. Data were collected from a large well-maintained clinical database with very few missing data. However, unlike randomised trials which aim to adequately balance both measured and unmeasured variables across treatment groups, the propensity score matching can only balance measured cofounders that were included in the calculation of the propensity score, so hidden bias is likely to remain. The two groups had different baseline characteristics which may be a random result related to our sample size. There was a higher number of Indigenous mothers in the intervention group whose socioeconomic demographic characteristics showed they were more disadvantaged. We believe this strengthens our findings and the potential generalisability of the study as our results changed little when we conducted the analysis on Indigenous mothers only compared to the analysis that included some non-Indigenous mothers with Indigenous partners. Some variables that could affect preterm birth outcomes were not included due to missing data such as drug and alcohol use, and mental illness. However, given that we have controlled for substantial social, economic and medical risk factors, the impact of unmeasured risk factors on preterm births is reduced. Also we assume that all included covariates are baseline confounding factors, and are not mediators lying on the causal pathway between exposure and outcome.
4.2. Generalisability
It is acknowledged that context, timing, governance, leadership and the commitment of partners are all pivotal to the intervention. However, it is likely that services set up with similar inputs [18] would see similar results for Indigenous women and babies across diverse Australian settings, and in other resource-rich colonised countries. In our matched sample (n = 345 in each arm), the preterm birth rate was 13.9% (48 preterm births) in Standard Care and 7.5% (26 preterm births) in the Birthing in Our Community Service, thus in absolute terms this equates to 22 preterm births avoided in the intervention arm. In 2016, there were over 16,479 Indigenous babies born in Australia. If the program was scaled up across the nation, approximately 1038 Aboriginal and Torres Strait Islander preterm births may be prevented each year. Not only would this have significate impact at a family and community level, but it would also have a reduction in excess hospital costs associate with the immediate admissions to a neonatal intensive care and costs of longer-term sequalae across the lifespan.
4.3. Future directions
Birthing in Our Community Service not only aims to provide clinically and culturally exceptional care, but also contributes to addressing the social and cultural determinants of health through employment and education, incorporation of cultural practices and addressing racism. This combination is likely to benefit throughout the life-course by improving health and outcomes and the social determinants. Health-economic analysis, full analysis of primary and secondary outcomes, infant assessments, survey and interview data up to six months postnatally and a realist process evaluation will provide further evidence for assessing impact of this complex intervention.
5. Conclusion
Our study found a significant reduction in preterm birth can be achieved with targeted innovation through a multi-agency partnership. The partnership has increased Indigenous community accessibility to, and governance of, the maternity services for Indigenous families, resulting in culturally responsive early intervention that would not otherwise be available through a hospital-based tertiary maternity service. Support for further research to test replication and scale-up should be considered as a strategy to improve health and wellbeing outcomes and accelerate progress towards reducing Indigenous child mortality. The team have developed the RISE Framework for implimentation to drive this health service reform: 1. Redesign the health service; 2. Invest in the workforce; 3. Strengthen families; and, 4. Embed Aboriginal and/or Torres Strait Islander community governance and control [37].
Author contributions
SKi was involved in developing the intervention, led the literature search, protocol development, successful funding application, study design, interpretation and writing of the manuscript. She oversaw data collection and contributed to key decisions in analysis. YG was involved in protocol and study design, writing the successful funding proposal, interpretation of results and writing of the manuscript. She conducted the data analysis leading key decisions in analysis and completed the tables and figures. SH contributed to the conduct and monitoring of the study, the collection of data, interpretation of results and writing of manuscript. SKr contributed to the protocol and study design, writing the successful funding proposal, interpretation of results and writing of the manuscript. CN was involved in developing the intervention, protocol and study design, writing the successful funding proposals, interpretation of results and writing of the manuscript. RB contributed to the delivery of the intervention, interpretation of results and writing of the manuscript. Skil, SKR, CN, RB were involved in monitoring intervention fidelity. ST was involved in developing the protocol, writing the successful funding proposal, study design, analysis plan, interpretation of results and writing of the manuscript. CH provided the biostatistical oversight and leadership for the analysis, also conducted some analysis. He was involved in interpretation of results and writing of the manuscript. DW was involved in study design, key decisions in analysis and interpretation of results. YR provided the Indigenous oversight of the study. She was involved in protocol development, study design, writing the successful funding proposal and Indigenous methodology, contributed to key decisions in analysis, interpretation of results and writing of the manuscript.
Funding
National Health and Medical Research Council (NHMRC) Funding (No. 1077036) matched by partners: Institute for Urban Indigenous Health, the Aboriginal and Torres Strait Islander Community Health Service Brisbane and the Mater Mothers Hospital. Additional funding from Queensland Government, University of Queensland and University of Sydney.
Acknowledgments
Acknowledgement
The authors acknowledge the Aboriginal and Torres Strait Islander families and all the staff who have contributed to, and participated in, the development and delivery of the Birthing in Our Community Service; in particular members of the Steering Committee and Indigenous Birthing in an Urban Setting (IBUS) investigators: Mr. Adrian Carson, Ms. Jody Currie, Ms. Maree Reynolds, Ms. Kay Wilson, Dr. Michael Beckmann, Ms. Shannon Watego, Ms. Machellee Kosiak, Professor Roianne West, Dr. Anton Clifford-Motopi, and Associate Professor Megan Passey.
Trial registration
Retrospectively registered, Australian New Zealand Clinical Trial Registry #ACTRN12618001365257.
Declaration of Competing Interest
We declare no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eclinm.2019.06.001.
Appendix A. Supplementary data
Supplementary tables
References
- 1.Stephens C., Porter J., Nettleton C., Willis R. Disappearing, displaced, and undervalued: a call to action for indigenous health worldwide. Lancet. 2006;367(9527):2019–2028. doi: 10.1016/S0140-6736(06)68892-2. [DOI] [PubMed] [Google Scholar]
- 2.Smylie J., Kirst M., McShane K., Firestone M., Wolfe S., O'Campo P. Understanding the role of indigenous community participation in indigenous prenatal and infant-toddler health promotion programs in Canada: a realist review. Soc Sci Med. 2016;150:128–143. doi: 10.1016/j.socscimed.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Kildea S., Hickey S., Nelson C. Birthing on country (in our community): a case study of engaging stakeholders and developing a best-practice indigenous maternity service in an urban setting. Aust Health Rev. 2018;42(2):230–238. doi: 10.1071/AH16218. [DOI] [PubMed] [Google Scholar]
- 4.Commonwealth of Australia . Department of the Prime Minister and Cabinet; Canberra: 2019. Closing the gap prime Minister's report 2019. [Google Scholar]
- 5.Laws P., Li Z., Sullivan E. vol. 2008. AIHW National Perinatal Statistics Unit; Sydney: 2010. Australia's mothers and babies. [Google Scholar]
- 6.Australian Institute of Health and Welfare. Australia mothers and babies 2015 - perinatal dynamic data displays. 26.10.16 2017. https://www.aihw.gov.au/reports/mothers-babies/perinatal-dynamic-data-displays/contents/dynamic-data-displaysCat. no. PER 91).
- 7.Howson C., Kinney M., Lawn J. March of Dimes, Partnership for Maternal, Newborn and Child Health, Save the Children, World Health Organisation; Geneva: 2012. Editors. The global action report on preterm birth, born too soon. [Google Scholar]
- 8.O'Dea K. Preventable chronic diseases among indigenous Australians: the need for a comprehensive national approach. Heart Lung Circ. 2005;14(3):167–171. doi: 10.1016/j.hlc.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Van Wagner V, Osepchook C, Harney E, Crosbie C, Tulugak M. Remote midwifery in Nunavik, Quebec, Canada: outcomes of perinatal care for the Inuulitsivik health centre, 2000-2007. Birth 2012; 39(3): 230–7. [DOI] [PubMed]
- 10.Douglas V.K. The Inuulitsivik maternities: culturally appropriate midwifery and epistemological accommodation. Nurs Inq. 2010;17(2):111–117. doi: 10.1111/j.1440-1800.2009.00479.x. [DOI] [PubMed] [Google Scholar]
- 11.Society of Obstetricians and Gynaecologists of Canada Returning birth to aboriginal, rural and remote communities. J Obstet Gynaecol Can. 2010;32(12):1186–1188. doi: 10.1016/s1701-2163(16)34744-2. [DOI] [PubMed] [Google Scholar]
- 12.Cairns J.B. Maori maternity in the land of the long white cloud. Br J Midwifery. 2005;13(2):74–77. [Google Scholar]
- 13.Felton-Busch C. Birthing on country: an elusive ideal? Contemp Nurse. 2009;33(2):161–162. doi: 10.5172/conu.2009.33.2.161. [DOI] [PubMed] [Google Scholar]
- 14.Kildea S, Van Wagner, V. 'Birthing on Country' maternity service delivery models: An evidence check rapid review brokered by the sax institute on behalf of the maternity services inter-jurisdictional committee. Sydney: Australian Health Ministers' Advisory Council; 2013.
- 15.Department of Health and Aging . Commonwealth of Australia; 2009. Improving maternity services in Australia: a discussion paper from the Australian Government. [Google Scholar]
- 16.Kildea S., Tracy S., Sherwood J., Magick-Dennis F., Barclay L. Improving maternity services for indigenous women in Australia: moving from policy to practice. Med J Aust. 2016;205(8):374–379. doi: 10.5694/mja16.00854. [DOI] [PubMed] [Google Scholar]
- 17.Kildea S., Stapleton H., Murphy R., Kosiak M., Gibbons K. The maternal and neonatal outcomes for an urban indigenous population compared with their non-indigenous counterparts and a trend analysis over four triennia. BMC Pregnancy Childbirth. 2013;13(1):167. doi: 10.1186/1471-2393-13-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016; 4: CD004667. [DOI] [PMC free article] [PubMed]
- 19.Miller S., Abalos E., Chamillard M. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–2192. doi: 10.1016/S0140-6736(16)31472-6. [DOI] [PubMed] [Google Scholar]
- 20.Hickey S., Roe Y., Gao Y. The indigenous birthing in an urban setting study: the IBUS study: a prospective birth cohort study comparing different models of care for women having aboriginal and Torres Strait islander babies at two major maternity hospitals in urban south East Queensland, Australia. BMC Pregnancy Childbirth. 2018;18(1):431. doi: 10.1186/s12884-018-2067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panaretto K.S., Mitchell M.R., Anderson L. Sustainable antenatal care services in an urban indigenous community: the Townsville experience. Med J Aust. 2007;187(1):18–22. doi: 10.5694/j.1326-5377.2007.tb01109.x. [DOI] [PubMed] [Google Scholar]
- 22.Rubin D.B. Using propensity scores to help design observational studies: application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2(3–4):169–188. [Google Scholar]
- 23.Austin P. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tracy S.K., Hartz D.L., Tracy M.B. Caseload midwifery care versus standard maternity care for women of any risk: M@NGO, a randomised controlled trial. The Lancet. 2013;382(9906):1723–1732. doi: 10.1016/S0140-6736(13)61406-3. [DOI] [PubMed] [Google Scholar]
- 25.Rumbold A.R., Cunningham J. A review of the impact of antenatal care for Australian indigenous women and attempts to strengthen these services. Matern Child Health J. 2008;12(1):83–100. doi: 10.1007/s10995-007-0216-1. [DOI] [PubMed] [Google Scholar]
- 26.Jongen C., McCalman J., Bainbridge R., Tsey K. Aboriginal and Torres Strait Islander maternal and child health and wellbeing: a systematic search of programs and services in Australian primary health care settings. BMC Pregnancy Childbirth. 2014;14(1):251. doi: 10.1186/1471-2393-14-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Herceg A. Canberra: Australian Government Department of Health and Ageing. 2005. Improving health in aboriginal and Torres Strait islander mothers, babies and young children: a literature review. [Google Scholar]
- 28.Bertilone C., McEvoy S. Success in closing the gap: favourable neonatal outcomes in a metropolitan aboriginal maternity group practice program. Med J Aust. 2015;203(6):262 e1–7. doi: 10.5694/mja14.01754. [DOI] [PubMed] [Google Scholar]
- 29.Murphy E., Best E. The aboriginal maternal and infant health service: a decade of achievement in the health of women and babies in NSW. NSW Public Health Bulletin. 2012;23(4):68–72. doi: 10.1071/NB11051. [DOI] [PubMed] [Google Scholar]
- 30.Gao Y., Gold L., Josif C. A cost-consequences analysis of a midwifery group practice for aboriginal mothers and infants in the top end of the Northern Territory, Australia. Midwifery. 2014;30(4):447–455. doi: 10.1016/j.midw.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Allen J., Gibbons K., Beckmann M., Tracy M., Stapleton H., Kildea S. Does model of maternity care make a difference to birth outcomes for young women? A retrospective cohort study. Int J Nurs Stud. 2015;52(8):1332–1342. doi: 10.1016/j.ijnurstu.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 32.Allen J., Kildea S., Stapleton H. How does group antenatal care function within a caseload midwifery model? A critical ethnographic analysis. Midwifery. 2015;31(5):489–497. doi: 10.1016/j.midw.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Kildea S., Stapleton H., Murphy R., Low N.B., Gibbons K. The Murri clinic: a comparative retrospective study of an antenatal clinic developed for aboriginal and Torres Strait islander women. BMC Pregnancy Childbirth. 2012;12(1):159. doi: 10.1186/1471-2393-12-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Renfrew M.J., McFadden A., Bastos M.H. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384(9948):1129–1145. doi: 10.1016/S0140-6736(14)60789-3. [DOI] [PubMed] [Google Scholar]
- 35.Australian Health Ministers Advisory Council (AHMAC) vol. 2011. AHMAC, Commonwealth of Australia; Canberra: 2011. National Maternity Services Plan. [Google Scholar]
- 36.Cepeda M.S., Boston R., Farrar J.T., Strom B.L. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158(3):280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
- 37.[37] Kildea, S., S. Hickey, L. Barclay, S. Kruske, C. Nelson, J. Sherwood, J. Allen, Y. Gao, R. Blackman and Y. Roe (In press). "Implementing Birthing on Country services for Aboriginal and Torres Strait Islander families: RISE Framework." Women and Birth Special Issue, Birthing on Country. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary tables