Abstract
Background
Although human-to-human transmission of severe fever with thrombocytopenia syndrome phlebovirus (SFTSV) via direct contact with body fluids has been reported, the role of specific body fluids from SFTSV-infected hosts has not been investigated in detail.
Methods
To demonstrate the virus transmission kinetics in SFTSV-infected hosts, we adapted the ferret infection model and evaluated the virus shedding periods, virus titers, and transmission modes from various specimens of infected ferrets.
Results
Large amounts of infectious SFTSV are shed through nasal discharge, saliva, and urine from SFTSV-infected ferrets. Virus could be detected from 2 dpi and persisted until 12 dpi in these specimens, compared with the relatively short virus-shedding period in sera. Further, transmission studies revealed that SFTSV can be transmitted to close direct and indirect contact naïve animals through various mediums, especially through contact with serum and urine. Further, ferrets contacted with human urine specimens from SFTSV-positive patients were successfully infected with SFTSV, suggesting that urine specimens could be a source of SFTSV infection in humans.
Conclusions
Our results demonstrate that the SFTSV can be shed in various body fluids for more than 12 days and that these specimens could be a source for direct or indirect transmission through close personal contact.
Keywords: body fluids, ferret, indirect transmission, SFTSV, virus shedding
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging zoonotic infectious disease caused by SFTS phelobovirus (SFTSV), a novel member of the family Phlevovirdae [1, 2]. Since the first report of this virus in rural areas of the Hubei and Henan provinces in Central China in 2009, SFTS has mainly been found in China, Japan, and South Korea, with growing annual incidence and high case fatality rates [1, 3, 4]. SFTSV is believed to be maintained in nature by an enzootic tick–animal cycle [5]. Of the tick species, Haemaphysalis longicornis are implicated as a main vector of SFTSV [6], and their active cycle from March through November is also the epidemic season of SFTSV [6–9]. Although SFTSV infection in humans is believed to be predominantly mediated through bites from virus-infected ticks, the first human-to-human transmission of SFTSV through contact or exposure to patient blood was reported in 2012 [10]. Since then, possible human-to-human transmissions of SFTS have been reported in families, co-residents of villages, and even in the hospital setting [11–14]. Further, some secondarily infected patients died with high viral loads and clinical symptoms, including high fever and low platelet counts [15]. Investigation of a cluster of SFTS cases provided evidence of person-to-person transmission through contact with blood from an index patient with a high serum virus load [10, 16]. However, detailed information regarding the kinetics of virus shedding in various body fluids and the manner of SFTSV transmission in vivo is quite limited due to the previous lack of an animal infection model.
Therefore, in this study, we performed direct and indirect contact transmission studies using a ferret model, which was recently characterized as a suitable model for SFTSV human infection [17]. In this model, we attempted to trace virus transmission and identify the specimens most likely mediating transmission from infected hosts. The virus-shedding periods and viral loads of various specimens were comparatively analyzed using real-time reverse transcription polymerase chain reaction (RT-PCR). In addition, the presence of infectious virus in collected ferret and human specimens was demonstrated through infection in sentinel ferrets.
METHODS
Study Design for Animal-to-Animal Transmission
To demonstrate animal-to-animal transmission of SFTSV, ferrets (≥4Y, n = 3) were inoculated with the CB1/2014 SFTSV strain [17] at a titer of 106.0 fifty percent of tissue culture infective dose (TCID50)/mL by the intramuscular (IM) route, and direct contact (DC) and indirect contact (IC) ferret groups (n = 6/group) were introduced into the cages at 2 days postinfection (dpi), which is the initial day postcontact (dpc). Inoculated and DC ferrets were kept in direct contact in the same cage, whereas IC ferrets were separated from inoculated animals by a partition, which allowed air to move but did not allow direct contact between animals. Blood, fecal, nasal wash, saliva, and urine samples were collected every other day for 22 days from each group of ferrets to detect CB1/2014 SFTSV. Further, to investigate whether each collected specimen contained infectious live virus, groups of ferrets (≥4Y, n = 3/group) were treated with specimens (serum, fecal, nasal washes, saliva, and urine) by the oro-nasal route. Ferrets were then monitored for clinical symptoms, platelet numbers, and viral titers in body secretions. In addition, 500-μL blood samples were collected in EDTA tubes (MEDISTAR, Seoul, Korea) followed by analysis of hematological parameters using a Celltac hematology analyzer (MEK-6550J/K, Nihon Kohden, Japan).
Quantitative Real-time RT-PCR to Detect SFTSV RNA
Collected ferret secretions were resuspended with cold phosphate-buffered saline (PBS) containing antibiotics (5% penicillin/streptomycin; Gibco). For virus titration, total RNA was extracted from the collected samples using the RNeasy Mini kit (QIAGEN, Hilden, Germany) according to the manufacturer’s instructions [18]. A cDNA synthesis kit (Omniscript Reverse Transcriptase, QIAGEN) was used to synthesize single-strand cDNA using total viral RNA. To quantitate viral RNA and viral copy number, quantitative real-time RT-PCR (qRT-PCR) was performed for the partial M gene with the SYBR Green kit (iQ SYBR Green Supermix kit, Bio-Rad, Hercules, CA), as described elsewhere [17]. The number of viral RNA copies was calculated as a ratio compared with the number of copies of the standard control [19].
Demonstration of Active SFTSV in Human Specimens
To determine whether SFTSV-confirmed human specimens had the ability to cause contact infections, groups of ferrets (≥4Y, n = 2/group) were oro-nasally treated with urine specimens (1 mL) from 2 SFTSV-confirmed patients. For this, patients’ urine samples were collected within 3 days of the first confirmation of SFTSV infection by RT-PCR assay. Ferrets were then monitored for clinical symptoms, platelet numbers, and viral titers in body secretions, as described above.
RESULTS
Clinical Features of SFTSV-Inoculated Ferrets Along With Direct and Indirect Contact Ferrets
To demonstrate ferret-to-ferret transmission in an experimental setting, animals (n = 3) were inoculated with 106.0 TCID50/mL of the strain CB1/2014 via an IM injection, and the DC and IC ferret groups (n = 2/group) were introduced into cages at 2 dpi. Clinical features of SFTSV infection were then compared between the ferret groups. This study was conducted in 3 independent trials. In CB1/2014-inoculated ferrets, there was a rapid increase in body temperature, from 39°C to 40.6°C, between 3 and 5 dpi, followed by a rapid drop in temperature at 7 dpi, which was when ferrets succumbed. Four of 6 DC and 2 of 6 IC ferrets also showed increased body temperatures (>39°C) from 6 to 10 dpi (4 to 8 dpc) (Figure 1A). Moreover, 2 of 6 DC ferrets had body temperatures >40°C from 9 to 11 dpc and succumbed to death at 12 dpc (Figure 1A). However, all surviving DC and IC ferrets recovered to their initial body temperature range between 9 and 12 dpc (Figure 1A).
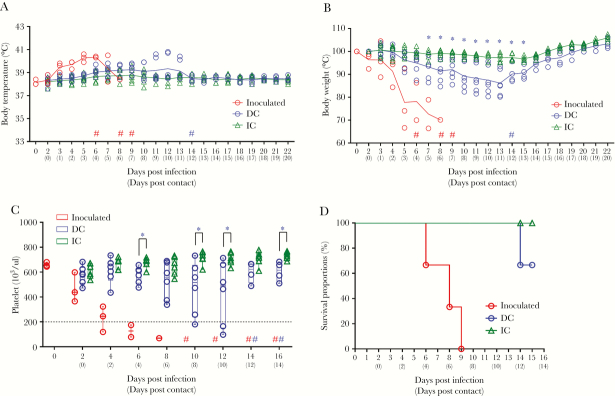
Figure 1.
Clinical symptoms in ferrets after inoculation with CB1/2014 severe fever with thrombocytopenia syndrome phlebovirus. Three ferrets were inoculated intramuscularly with 106.0 TCID50 of virus, and direct contact (DC) and indirect contact (IC) ferrets (n = 6/group) were introduced into the cage at 2 dpi. Body temperature (A), relative weight (B), platelet count (C), and survival rate (D) were assessed and are shown as means with standard deviations. The number indicates a reduced number of samples collected due to death of ferrets in this group. Red, blue, and green symbols represent the direct infected, DC, and IC ferrets, respectively. Data are presented with the horizontal dotted line as the minimum threshold values. The Mantel Cox method was used to assess survival. Asterisks indicate statistical significance between direct and indirect contact ferrets, as determined from the same dpi as in the 2-tailed, unpaired t test (*P < .05). This experiment was performed in 3 independent trials.
Significant weight loss was observed in all CB1/2014-inoculated ferrets starting at 5 dpi, with an average 30% weight decrease at 7 dpi. In DC ferrets, 4 of 6 ferrets showed 3%–15% weight loss between 3 and 11 dpc, but the fatal cases (n = 2) in the DC group showed a loss of morbidity and gradual weight loss up to 20% from 3 dpc until death (12 pdc). After 11 dpc, the surviving ferrets (n = 4) started recovering their body weight, reaching their initial weights by 18 dpc. In IC ferrets, body weight loss was <5%, and all ferrets recovered their body weight by 14 dpc (Figure 1B).
As indicated by the name, severe thrombocytopenia is one of the major clinical symptoms of SFTSV. Therefore, we collected blood from each group of ferrets and quantitated platelets. All infected ferrets exhibited thrombocytopenia, with platelet counts <69 ×103/uL at 8 dpi (the normal range for ferrets is 200–1280 ×103/µL [20]) (Figure 1C). In DC ferrets, platelet counts were only reduced by 10%, with the exception of the 2 fatal cases (Figure 1C). The 2 ferrets that succumbed showed slightly decreased platelet numbers until 4 dpc, and then a sharp decrease, 97 ×103/uL at 10 dpc, before dying at at 12 dpc (Figure 1C and D). This trend in platelet counts is similar to that of the infection group. In contrast, platelet counts remained within the normal range throughout the study without any fatal cases in the IC group (Figure 1C and D).
Detection of SFTSV in Various Ferret Specimens
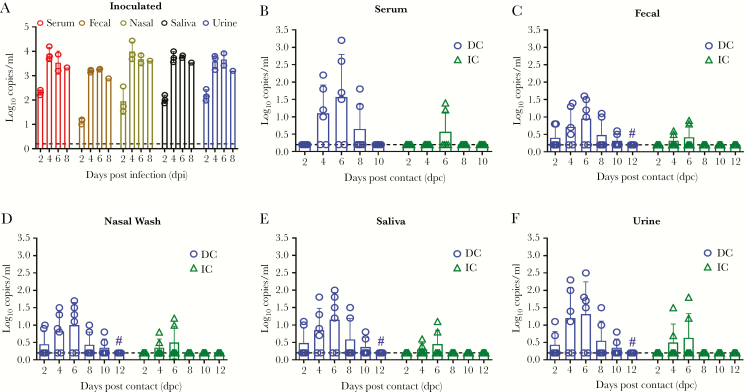
To investigate shedding of SFTSV from each group of animals, we collected body secretions every other day and measured the viral RNA copy numbers. In the inoculated group, viral RNA was detected at 1.20 and 2.56 log10 copies/mL in all specimens at 2 dpi. The highest amount of viral RNA was detected in nasal washes from inoculated ferrets at 4 dpi (4.44 log10 copies/mL) (Figure 2A). In the DC group, viral RNA was detected in sera from 4 to 8 dpc at 1.0 to 3.2 log10 copies/mL, and the highest titer was observed at 6 dpc (3.2 log10 copies/mL) in 4 out of 6 ferrets. In the IC group, viral RNA was only detected in sera at 6 dpc in 2 out of 6 ferrets, with a mean of 1.3 log10 copies/mL (Figure 2B). In fecal specimens, viral RNA gradually increased until 6 dpc, when it peaked at 1.6 (DC ferrets) and 0.9 (IC ferrets) log10 copies/mL and then decreased in the DC group until 10 dpc and disappeared in the IC group after 6 dpc (Figure 2C). In nasal wash specimens, the highest viral titers were detected at 6 dpc (1.7 and 1.2 log10 copies/mL in DC and IC ferrets, respectively); viral titers then decreased until 10 dpc in the DC group (Figure 2D). In saliva specimens, the highest titer was seen at 6 dpc (2.0 log10 copies/mL in DC ferrets and 1.1 log10 copies/mL in IC ferrets); titers then gradually decreased until 10 dpc in DC ferrets (Figure 2E). Urine specimens from DC ferrets showed viral RNA titers comparable to those seen in the serum with the highest viral RNA titer at 6 dpc in both DC (2.5 log10 copies/mL) and IC (1.8 log10 copies/mL) ferrets, which then decreased gradually until 10 dpc in the DC group (Figure 2F). No viral RNA was detected in any specimens (serum, fecal, nasal wash, saliva, or urine) after 6 dpc for IC ferrets and 10 dpc for DC ferrets.
Figure 2.
Viral titers in collected specimens from each group of ferrets. Specimens (fecal, nasal washes, saliva, and urine) were collected for 12 days, and blood samples were collected for 10 days (once every 2 days). All specimens from directly infected ferrets (A), and the serum (B), fecal (C), nasal washes (D), saliva (E), and urine (F) of direct contact (DC) and indirect contact (IC) ferrets were titered using real-time polymerase chain reaction. Blue circles and green triangles represent DC and IC ferrets, respectively. Each experiment was performed 3 separate times. The number indicates a reduced number of samples collected due to death of ferrets in this group. Data are presented with the horizontal dotted line as the minimum values (0.2 log10 copies/mL) observed.
To evaluate the virus titers and tissue distributions in the 2 fatal cases in DC ferrets, a qRT-PCR assay was conducted with various tissues taken on the day of death and compared with those of inoculated ferrets. The highest viral RNA titers were detected in the spleens of inoculated ferrets and DC ferrets, 5.42 and 3.71 log10 copies/mL, respectively (Table 1). Interestingly, the fatal cases in the DC group had virus titers in tissues that were overall lower than those seen in infected ferrets; however, the viral load in the spleen was significantly higher than in other organs (P < .05). These results demonstrate that SFTSV can replicate in multiple organs, causing systemic infection, and that it is transmitted by direct contact, which can lead to death, as well as by indirect contact.
Table 1.
Quantitation of Viral RNA in Organs of Deceased Ferrets in Each Group Using Real-Time RT-PCR
| Organs of Deceased Ferrets, Log10 Copies/mLa | |||||
|---|---|---|---|---|---|
| Group | Lung | Liver | Spleen | Intestine | Kidney |
| Infected | 4.02 ± 0.13 | 4.36 ± 0.58 | 5.28 ± 0.20 | 4.68 ± 0.45 | 3.04 ± 0.64 |
| Fatal cases in DC | 1.19 ± 0.08 | 2.63 ± 0.29 | 3.59 ± 0.18 | 1.14 ± 0.25 | 0.70 ± 0.15 |
Abbreviations: DC, direct contact; RT-PCR, reverse transcription polymerase chain reaction.
aThe virus RNA detection limit was 0.30 log10 copies/mL.
Demonstration of Direct Transmission Through Ferret Secretions
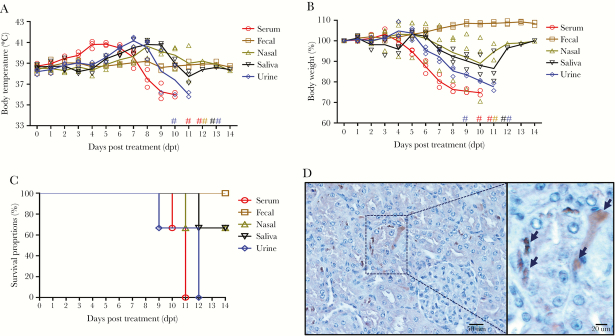
Next, to investigate which body secretions could cause infections in naïve ferrets, specimens collected from inoculated ferrets at 5 dpi were used to treat naïve ferrets (n = 3/group), and clinical symptoms and viral titers were monitored. Although ferrets treated with fecal specimens did not show SFTS-like clinical symptoms or mortality, serum- and urine-treated ferrets showed increased body temperatures (above 40°C) at 4 and 6 days post-treatment (dpt), respectively (Figure 3A), and they showed rapid body weight loss at 5 and 6 dpt (Figure 3B). These animals eventually succumbed by 9 and 10 dpt, respectively (Figure 3C). Ferrets treated with saliva and nasal washes also showed increased body temperatures (Figure 3A) and weight loss until 10 to 11 dpt, respectively (Figure 3B). One of 3 nasal- and saliva-treated ferrets succumbed by 11 and 12 dpt (Figure 3C), whereas the other ferrets showed signs of recovery from 12 dpt.
Figure 3.
Clinical symptoms in ferrets (n = 3) after inoculation with collected body secretions (serum, fecal, nasal washes, saliva, or urine) by the oro-nasal route. Body temperature (A), relative weight (B), and survival rate (C) were assessed and are shown as means with standard deviations. The number indicates a reduced number of samples collected due to death of ferrets in this group. The Mantel Cox method was used to assess survival. Blue circles (serum), dark brown squares (fecal), light brown triangles (nasal washes), black inverted triangles (saliva), and blue rhombi (urine) represent each group of specimen-treated ferrets, respectively.
To confirm that the observed clinical symptoms and mortality were associated with SFTSV infection, we collected body secretions and measured virus titers in each specimen. The qRT-PCR results revealed that serum, nasal wash, saliva, and urine specimen–treated ferrets showed relatively high virus sheading through most routes, with the exception of fecal specimens (Table 2). The fecal specimen–treated ferrets only shed virus through the serum, and at low levels (<2 log10 copies/mL) and for a short period of time (4–8 dpt). In contrast, SFTSV was detected in all specimens from the saliva and urine specimen–treated ferrets between 4 and 12 dpt. It is noteworthy that nasal washes, saliva, and urine specimens showed relatively long virus-shedding periods compared with the serum specimens, which shed between 4 and 8 dpt (Table 2). Nevertheless, these data show that a majority of body secretions from SFTSV-infected ferrets contain infectious virus at levels high enough to induce fatal infections in contact animals.
Table 2.
Quantitation of Viral RNA in Specimens (Serum, Feces, Nasal Wash, Saliva, and Urine) From Ferrets Treated With the Indicated Secretions From Inoculated Ferrets
| Days Post-treatment, Log10 Copies/mLa | |||||||
|---|---|---|---|---|---|---|---|
| Route | Specimen | 2 | 4 | 6 | 8 | 10 | 12 |
| Serum | Serum | - | - | 0.92 ± 0.38 | 1.59 ± 0.40 | - | - |
| Fecal | - | - | - | - | - | - | |
| Nasal | - | 1.16 ± 0.34 | 1.77 ± 0.49 | 2.28 ± 0.40 | - | - | |
| Saliva | - | 0.72 ± 0.30 | 1.31 ± 0.57 | 1.12 ± 0.52 | - | - | |
| Urine | - | 1.04 ± 0.33 | 1.93 ± 0.39 | 2.15 ± 0.39 | - | - | |
| Fecal | Serum | - | 0.33 ± 0.58 | 0.35 ± 0.60 | - | - | - |
| Fecal | - | - | - | - | - | - | |
| Nasal | - | - | - | - | - | - | |
| Saliva | - | - | - | - | - | - | |
| Urine | - | - | - | - | - | - | |
| Nasal | Serum | - | 0.49 ± 0.85 | 1.03 ± 0.91 | 1.45 ± 1.27 | - | - |
| Fecal | - | - | - | - | - | - | |
| Nasal | - | 0.85 ± 0.74 | 1.64 ± 0.66 | 1.99 ± 0.76 | 2.57 ± 0.82 | 0.47 ± 0.29 | |
| Saliva | - | 0.56 ± 0.65 | 0.94 ± 0.88 | 0.54 ± 0.93 | - | - | |
| Urine | - | 1.02 ± 0.25 | 1.45 ± 0.36 | 2.33 ± 0.56 | - | - | |
| Saliva | Serum | 0.75 ± 0.77 | 1.32 ± 0.69 | 2.02 ± 0.50 | - | - | |
| Fecal | - | 0.63 ± 0.75 | 0.95 ± 0.83 | 1.28 ± 1.11 | 1.11 ± 0.97 | - | |
| Nasal | - | 1.41 ± 0.55 | 1.73 ± 0.54 | 2.48 ± 1.64 | 2.53 ± 2.19 | - | |
| Saliva | - | - | 0.87 ± 0.86 | 1.68 ± 0.57 | 0.67 ± 1.16 | 0.37 ± 0.47 | |
| Urine | - | - | 1.19 ± 0.34 | 1.94 ± 0.44 | 3.01 ± 1.16 | 0.30 ± 0.53 | |
| Urine | Serum | - | 0.47 ± 0.82 | 1.18 ± 1.06 | 1.91 ± 1.76 | - | - |
| Fecal | 0.48 ± 0.84 | 1.39 ± 0.17 | 2.09 ± 0.41 | 2.82 ± 0.91 | 1.21 ± 0.69 | - | |
| Nasal | - | 0.49 ± 0.64 | 1.15 ± 1.00 | 1.94 ± 1.70 | 0.43 ± 0.91 | - | |
| Saliva | 0.37 ± 0.64 | 0.99 ± 0.33 | 1.50 ± 0.23 | 2.28 ± 0.55 | 0.30 ± 0.59 | - | |
| Urine | - | 0.80 ± 0.94 | 1.82 ± 0.52 | 2.61 ± 0.55 | 1.24 ± 0.42 | 0.35 ± 0.60 | |
aThe virus RNA detection limit was 0.30 log10 copies/mL.
Demonstration of Active SFTSV Transmission by Human Urine Specimens
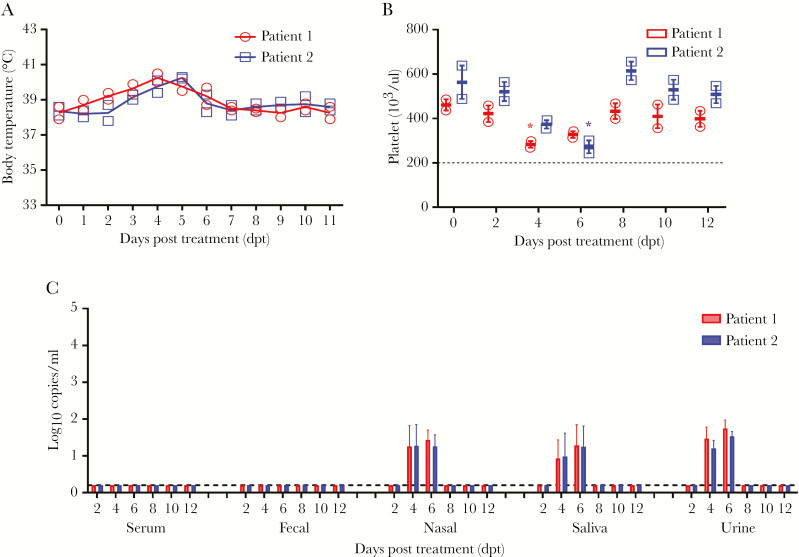
As shown above, urine specimens in particular exhibit relatively high virus titers for long periods of time (2–10 dpi) (Figure 2F). To demonstrate that SFTSV-positive urine specimens from human patients could be a source of infection for contact persons, we treated ferrets with 2 SFTSV-positive human urine specimens (viral titers of 1.2 and 1.8 copies/mL) by the oro-nasal route, which were collected from the SFTSV-confirmed patients at Chungbuk National University Hospital in September of 2018. Ferrets treated with the urine samples showed elevated body temperatures (39°C–40.5°C) (Figure 4A). Further gradual decreased platelet numbers were observed between 4 and 6 dpt compared with those of prior infections in both ferret groups, although they were still within the normal range and recovered by 8 dpt (Figure 4B). SFTSV RNA was detected in the nasal washes, saliva, and urine specimens from 4 to 6 dpt. It should be noted that overall virus titers were lower than 2 log10 copies/mL and no viral RNA was detected in serum and fecal specimens (Figure 4C). This result demonstrates that infectious SFTSV is transmitted through urine specimens from SFTS patients, which could be a transmission source through direct personal contact, such as to health care workers.
Figure 4.
Clinical symptoms in ferrets (n = 2) after inoculation with urine from human severe fever with thrombocytopenia syndrome phlebovirus–positive patients. Body temperature (A), platelet counts (B), and virus copy number in collected specimens (C) were assessed and are shown as means with standard deviations. Red circles and blue squares represent patient 1 and patient 2, respectively. Asterisks indicate statistical significance compared with the sample from the start day by 2-tailed, unpaired t test (*P < .05). Data are presented with the horizontal dotted line as the minimum threshold values in (B) and as the minimum values observed (0.2 log10 copies/mL) in (C).
DISCUSSION
Given the increased human-to-human transmission of SFTSV, including patient-associated transmission to health care professionals in the hospital setting [10, 12–16], we investigated SFTSV shedding in various body secretions and various modes of transmission of this virus in the ferret model, a previously demonstrated model of human SFTSV infection [17]. We found that a high amount of SFTSV was shed from inoculated ferrets through various body secretions and that ferrets placed in direct contact with infected ferrets were readily infected with SFTSV. Further, 2 of the DC ferrets showed severe clinical symptoms, including high body temperatures, deceased platelet numbers, and ~20% body weight loss, before succumbing. These data clearly demonstrate that SFTSV-infected hosts shed virus in various body secretions and can cause fatal infections in animals kept in close contact.
Recently, nosocomial transmission of SFTS through respiratory secretions was reported in South Korea indicating that human-to-human transmission does occur in the hospital setting [21]. Further, Jeong et al. reported detection of SFTSV RNA in patient's blood, trachea aspirate, gastric aspirate, and urine by semiquantitative RT-PCR [20]. However, the qRT-PCR cycle threshold (Ct) values were relatively low (up to 35), and the specimens were not assayed to determine if they contained virus titers sufficient to cause contact infection. Although the potential risk of infection from exposure to patient respiratory droplets is considered low, direct treatment of naïve ferrets with specimens from infected ferrets caused severe virus infections with clear clinical manifestations, including high fever, body weight loss, and even fatality in the case of serum-, respiratory secretion–, saliva-, and urine-treated groups. These results imply that there is risk of animal-to-human or human-to-human transmission through many secreted, and easily accessible, fluids from infected hosts.
In this study, ferrets treated with human urine specimens showed relatively attenuated clinical symptoms compared with those treated with infected ferret urine. This discrepancy might be explained by viral RNA titers in the specimens. Although the viral copy number in ferret urine was >2.0 log10 copies/mL, the viral copy number in human patient specimens was <1.8 log10 copies/mL. As a limitation of this study, we could not monitor sequential virus titers in urine specimens from human patients during active SFTSV infection; however, our data might suggest that the specimens utilized were collected during the recovery period (Figure 2 and Table 2). Nevertheless, the qRT-PCR results demonstrate that active infections occurred in human urine–treated ferrets. Therefore, we cannot rule out any bodily secretions from SFTSV patients as possible sources for virus transmission through close personal contact.
Taken together, our results demonstrate that SFTSV can be shed in various body fluids of infected hosts for more than 12 days and that these specimens are a source for direct and indirect transmission to those in close contact, including other patients or health care professionals. Therefore, we recommend that health care workers and family members caring for SFTS-suspected patients utilize proper personal equipment to protect against direct contact with patient blood, urine, and other body fluids. Further, the data in this study will be useful for updating the guidelines for the prevention and treatment of SFTSV patients to prevent the spread of SFTSV in the hospital setting.
Acknowledgments
All animal experiments were approved by the Medical Research Institute, a member of the Laboratory Animal Research Center of Chungbuk National University (Approval No. CBNUA-1083-18-02). The use of human specimens collected from SFTS-suspected patients at the Chungbuk National University Hospital was approved by the Institutional Review Board of Chungbuk National University Hospital (No. 2017-05-002-001). Animal management and sample analysis were undertaken in an enhanced Biosafety Level 3 (BSL-3) facility at the Chungbuk National University, as permitted by the Korea Centers for Disease Control & Prevention (K-CDC, Permit No. KCDC-14-3-07).
Financial support. This work was supported by grants from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (Grant No. HI15C2817) and the Government-wide R&D project funding for infectious disease research (Grant No. HG18C0029), Republic of Korea.
Potential conflicts of interest. All authors declare no competing interests. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Yu XJ, Liang MF, Zhang SY, et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med 2011; 364:1523–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adams MJ, Lefkowitz EJ, King AMQ, et al. Changes to taxonomy and the International Code of Virus Classification and Nomenclature ratified by the International Committee on Taxonomy of Viruses (2017). Arch Virol 2017; 162:2505–38. [DOI] [PubMed] [Google Scholar]
- 3. Kim K-H, Yi J, Kim G, et al. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerg Infect Dis 2013; 19:1892–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takahashi T, Maeda K, Suzuki T, et al. The first identification and retrospective study of severe fever with thrombocytopenia syndrome in Japan. J Infect Dis 2014; 209:816–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yamaji K, Aonuma H, Kanuka H. Distribution of tick-borne diseases in Japan: past patterns and implications for the future. J Infect Chemother 2018; 24:499–504. [DOI] [PubMed] [Google Scholar]
- 6. Luo LM, Zhao L, Wen HL, et al. Haemaphysalis longicornis ticks as reservoir and vector of severe fever with thrombocytopenia syndrome virus in China. Emerg Infect Dis 2015; 21:1770–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zheng H, Yu Z, Chen Z, et al. Development and biological characteristics of Haemaphysalis longicornis (Acari: Ixodidae) under field conditions. Exp Appl Acarol 2011; 53:377–88. [DOI] [PubMed] [Google Scholar]
- 8. Zheng H, Yu Z, Zhou L, et al. Seasonal abundance and activity of the hard tick Haemaphysalis longicornis (Acari: Ixodidae) in North China. Exp Appl Acarol 2012; 56:133–41. [DOI] [PubMed] [Google Scholar]
- 9. Li Z, Bao C, Hu J, et al. Ecology of the tick-borne phlebovirus causing severe fever with thrombocytopenia syndrome in an endemic area of China. PLoS Negl Trop Dis 2016; 10:e0004574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tang X, Wu W, Wang H, et al. Human-to-human transmission of severe fever with thrombocytopenia syndrome bunyavirus through contact with infectious blood. J Infect Dis 2013; 207:736–9. [DOI] [PubMed] [Google Scholar]
- 11. Zhu Y, Wu H, Gao J, et al. Two confirmed cases of severe fever with thrombocytopenia syndrome with pneumonia: implication for a family cluster in East China. BMC Infect Dis 2017; 17:537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hu J, Shi C, Li Z, et al. A cluster of cases of severe fever with thrombocytopenia syndrome bunyavirus infection in China, 1996: a retrospective serological study. PLoS Negl Trop Dis 2018; 12:e0006603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moon J, Lee H, Jeon JH, et al. Aerosol transmission of severe fever with thrombocytopenia syndrome virus during resuscitation. Infect Control Hosp Epidemiol 2019; 40:238–41. [DOI] [PubMed] [Google Scholar]
- 14. Bao C-j, Guo X-l, Qi X, et al. A family cluster of infections by a newly recognized bunyavirus in eastern China, 2007: further evidence of person-to-person transmission. Clin Infect Dis 2011; 53:1208–14. [DOI] [PubMed] [Google Scholar]
- 15. Chen H, Hu K, Zou J, Xiao J. A cluster of cases of human-to-human transmission caused by severe fever with thrombocytopenia syndrome bunyavirus. Int J Infect Dis 2013; 17:e206–8. [DOI] [PubMed] [Google Scholar]
- 16. Jiang XL, Zhang S, Jiang M, et al. A cluster of person-to-person transmission cases caused by SFTS virus in Penglai, China. Clin Microbiol Infect 2015; 21:274–9. [DOI] [PubMed] [Google Scholar]
- 17. Park S-J, Kim Y-I, Park A, et al. Ferret animal model of severe fever with thrombocytopenia syndrome phlebovirus for human lethal infection and pathogenesis. Nat Microbiol. 2019; 4:438–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiagen. R Neasy Mini Handbook, 2012. Available at: https://www.qiagen.com/es/resources/resourcedetail?id=14e7cf6e-521a-4cf7-8cbc-bf9f6fa33e24&lang=en. Accessed June 2012. [Google Scholar]
- 19. Shimada S, Posadas-Herrera G, Aoki K, et al. Therapeutic effect of post-exposure treatment with antiserum on severe fever with thrombocytopenia syndrome (SFTS) in a mouse model of SFTS virus infection. Virology 2015; 482:19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jeong EJ, Song JY, Lim CS, et al. Viral shedding from diverse body fluids in a patient with severe fever with thrombocytopenia syndrome. J Clin Virol 2016; 80:33–5. [DOI] [PubMed] [Google Scholar]
- 21. Kim WY, Choi W, Park SW, et al. Nosocomial transmission of severe fever with thrombocytopenia syndrome in Korea. Clin Infect Dis 2015; 60:1681–3. [DOI] [PubMed] [Google Scholar]