Abstract
Aims/hypothesis
The prevalence of diabetes and heart failure is increasing, and diabetes has been associated with an increased risk of heart failure. However, whether diabetes confers the same excess risk of heart failure in women and men is unknown. The aim of this study was to conduct a comprehensive systematic review with meta-analysis of possible sex differences in the excess risk of heart failure consequent to diabetes. Our null hypothesis was that there is no such sex difference.
Methods
A systematic search was conducted in PubMed for population-based cohort studies published between January 1966 and November 2018. Studies were selected if they reported sex-specific estimates of RRs for heart failure associated with diabetes, and its associated variability, which were adjusted at least for age. Random-effects meta-analyses with inverse variance weighting were used to obtain pooled sex-specific RRs and women-to-men ratio of RRs (RRRs) for heart failure associated with diabetes.
Results
Data from 47 cohorts, involving 12,142,998 individuals and 253,260 heart failure events, were included. The pooled multiple-adjusted RR for heart failure associated with type 1 diabetes was 5.15 (95% CI 3.43, 7.74) in women and 3.47 (2.57, 4.69) in men, leading to an RRR of 1.47 (1.44, 1.90). Corresponding pooled RRs for heart failure associated with type 2 diabetes were 1.95 (1.70, 2.22) in women and 1.74 (1.55, 1.95) in men, with a pooled RRR of 1.09 (1.05, 1.13).
Conclusions/interpretation
The excess risk of heart failure associated with diabetes is significantly greater in women with diabetes than in men with diabetes.
PROSPERO registration: CRD42019135246
Electronic supplementary material
The online version of this article (10.1007/s00125-019-4926-x) contains peer-reviewed but unedited supplementary material, which is available to authorised users.
Keywords: Diabetes, Heart failure, Meta-analysis, Sex differences, Systematic review
Introduction
Diabetes and heart failure are now recognised as frequent comorbid conditions; the prevalence of type 2 diabetes in individuals with heart failure was reported to be 4.3–28%, whilst that of heart failure in those with type 2 diabetes was reported to be 12–57% [1]. Diabetes is associated with an increased risk of heart failure [2], and also increases the risk of premature death after diagnosis of heart failure [3, 4]. Furthermore, heart failure is the second most common initial presentation of cardiovascular disease in people with type 2 diabetes and more common than myocardial infarction or stroke [5]. Although heart failure appears to be a complication of diabetes [6], this is still not fully recognised [1]. The number of people with heart failure is expected to increase continuously in the future, and thus efficient earlier prevention and treatment of heart failure is crucial.
Accumulating evidence has found that there are considerable sex differences in the excess risk of cardiovascular diseases associated with diabetes [7]. Our previous meta-analyses have shown that, compared with men, women have a significantly greater excess risk of CHD [8], stroke [9], as well as the non-cardiovascular complications of dementia [10], and cancer [11], following diabetes. However, whether these associations are also observed for heart failure is unknown, as the previous meta-analysis on the diabetes–heart failure association [2] included single-sex studies, which may have led to unreliable results due to differences in methodology, confounding factors included and background risk between the studies of women alone and men alone. Herein, we report the most comprehensive systematic review of the literature with a meta-analysis of possible sex differences in the excess risk of heart failure consequent to diabetes using only studies that included both sexes.
Methods
Search strategy and selection criteria
We conducted a systematic search in PubMed on 16 November 2018 using a combination of text words and medical subject headings (electronic supplementary material [ESM] Table 1). The reference lists of identified studies were also reviewed to identify other relevant studies.
Observational cohort studies were included if they had provided sex-specific RRs, or equivalents, for the association between diabetes and heart failure in both women and men. Studies were excluded if they were cohorts based on individuals with any underlying diseases, reported data for a single sex only, did not adjust at least for age, or did not provide information about the variability around the point estimate. In cases of duplicate reports from the same study, the study providing the longest follow-up or the highest number of events was included. Two authors (T. Ohkuma and Y. Komorita) conducted the search and extracted the data independently, and uncertainties regarding the inclusion of studies and data extraction were discussed and resolved by mutual consent. The meta-analysis was conducted in accordance with Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines [12].
Data extraction and statistical analysis
The primary outcome was incident heart failure (either fatal or non-fatal). The primary metrics were the pooled multiple-adjusted sex-specific RRs and the women-to-men ratio of RRs (RRRs) for heart failure, comparing individuals with diabetes with those without diabetes. In pooling multiple-adjusted RRs, the set of adjustments made was allowed to vary by study, but had to include at least one other risk factor for heart failure, in addition to age. Multiple RRs of subgroups from one study were combined into a single RR using a fixed-effect model. The pooled estimates of sex-specific RRs across studies were computed using random-effects meta-analyses with inverse variance weighting applied on the log scale. The same method was used to pool the RRRs. Data on type 1 and type 2 were separately pooled, where studies which did not differentiate type of diabetes were classified as type 2, which accounts for about 90–95% of all individuals with diabetes [13]. The I2 statistic was used to estimate the percentage of variability across studies due to between-study heterogeneity. Cochran’s Q test was used to assess whether there was a significant between-study heterogeneity.
Age-adjusted RRs were also pooled separately in secondary analyses. A sensitivity analysis was conducted to compare multiple-adjusted and age-adjusted estimates, where the studies were restricted to those that reported both. The presence of publication bias was examined using funnel plots and Egger’s and Begg’s tests. Meta-regression analyses tested for differences between prespecified subgroups in multiple-adjusted analyses: study region (Asia or non-Asia), year of baseline study (pre-1985 or 1986 onwards), ascertainment of diabetes (self-reported only or others), study outcome (fatal only or fatal and non-fatal combined), study quality (the Newcastle-Ottawa Scale [14] [ESM text and ESM Table 2], ≥8 or <8 points) and by absolute risk differences (greater in men or greater in women). Since only two studies were identified for type 1 diabetes, the analyses described in this paragraph were only applied for type 2 diabetes.
A p value <0.05 was considered to be statistically significant. All analyses were performed using Stata software (release 13; StataCorp, College Station, TX, USA).
Results
Of the 5991 articles identified by the systematic search, 760 articles qualified for full-text evaluation, and 14 articles provided summary data for sex differences in the association between diabetes and the risk of heart failure [5, 15–27] (Fig. 1).
Fig. 1.
Flow chart of study selection
The characteristics of all 14 studies included are shown in Table 1 and ESM Table 2. Data on type 1 diabetes and heart failure were available from two studies, involving two cohorts, including 3,284,123 individuals, and 95,129 events. Data on type 2 diabetes and heart failure were available from 13 studies, involving 47 cohorts, including 11,925,128 individuals, and 249,560 events, among which two studies, involving two cohorts, including 368,072 individuals, and 4584 events, reported age-adjusted RRs only. Nine studies provided data on absolute risks (ESM Table 3).
Table 1.
Characteristics of the studies reporting on the association between diabetes and heart failure
| Cohort | Country | Baseline years | Follow-up (years) | Study population | N (% women) | Age range (years) | N of diabetes (% women) | Type of diabetes | Ascertainment of diabetes | N of outcome (% women) | Fatal or non-fatal | Maximum adjustment available |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| APCSC [16] a | Pool of 32 cohorts | 1966–1999 | 7 | Population-based, occupational settings | 543,694 (36) | ≥20 | NA | Both | Self-reported, measured | 496 (NA) | F | Age, SBP, BMI, cigarette smoking, regression dilution bias, study (stratified) |
| Policardo et al [23] b | Italy | 2008 | 5 | Population-based | 3,192,203 (NA) | ≥16 | 152,954 (NA) | Both | Prescription, exemption from paying for diabetes, hospitalisation with diagnosis of diabetes | 26,154 (55) | Both | Age, CCI, previous hospitalisations for other CVD |
| KPMCP [26] | US | 1978–1984 | 9.5 median | Health maintenance organisation | 64,877 (54) | ≥40 | NA | Both | Self-reported, measured | 1330 (46) | Both | Age, race, education, HT, MI, frequent chest pain, TC, BMI, creatinine, uric acid, urine protein, LVH, smoking, alcohol c |
| LRPP [25] | US, pool of 4 cohorts | 1948, 1971, 1987–1989, 1967–1973 | 27.1, 20.3 (for index aged 45 and 55) | Population-based | 19,249 (50), 23,915 (53) (for index aged 45 and 55) | 30–62, 5–70, 45–64, ≥18 | 659 (46), 1792 (52) (for index aged 45 and 55) | Both | Measured, treatment | 1677 (47), 2976 (52) (for index aged 45 and 55) | Both | Age, race, education, smoking status, HT, obesity |
| CHS [24] | US | 1989–1990, 1992–1993 | 12.5 median | Population-based | 4817 (61) | ≥65 | 681 (53) | Both | Measured, treatment | 1342 (57) | Both | Age, clinical site, education, smoking, alcohol consumption, BMI, physical activity |
| Swedish NDR (T1) [27] | Sweden | 1998–2011 | T1: 7.9, control: 8.3 | Population-based (T1 was identified through NDR) | T1: 33,402 (45), control: 166,228 (45) | ≥18 | 33,402 (45) | T1 | NDR | 2387 (39) | Both | Age, time-updated diabetes duration, birth in Sweden, educational level, baseline comorbidities |
| Swedish NDR (T2) [20] | Sweden | 1998–2012 | 5.6 median | Population-based (T2 was identified through NDR) | T2: 266,305 (45), control: 1,323,504 (45) | T2: 62, control: 62 mean | 266,305 (45) | T2 | NDR | T2: 18,715 (46), control: 50,157 (45) | Both | Age, duration of diabetes, income, education, marital status, immigration status, stroke, acute MI, CHD, AF, renal dialysis or transplantation |
| Kaiser Permanente Georgia [17] | US | 2000–2005 | 2.8 | Health maintenance organisation | 359,947 (53) | ≥18 | 12,344 (49) | Both | Medical record, pharmacy claim | 4001 (50) | Both | Age, HT, coronary artery disease, AF, valvular heart disease |
| NHANES I Epidemiologic Follow-up Study [15] | US | 1971–1975 | 19 | Population-based | 13,643 (59) | 25–74 | 521 (61) | Both | Self-reported | 1382 (46) | Both | Age, race, education, physical activity, smoking, alcohol consumption, overweight, HT, valvular heart disease, CHD, BMI, SBP, TC, hypercholesterolaemia |
| Taiwan’s NHI system [19] | Taiwan | 2000 | T2: 7.8, control: 8.0 | Population-based | T2: 34,291 (47), control: 34,291 (47) | 60 mean | 34,291 (47) | T2 | Ambulatory care claims | 8420 (51) | Both | Age, geographical area, urbanisation status, Hx of CHD, Hx of coronary revascularisation procedures, statins, β-blockers, diuretics |
| Saskatchewan Health databases [22] | Canada | 1991–1996 | 5.2 | Population-based | T2 11,881 (45), control: 552,765 (51) | ≥30 | 11,881 (45) | T2 | Prescription | 2263 (46) | Both | Age |
| CALIBER programme [5] | UK | 1998–2010 | 5.5 median | Primary care practices | 1,921,260 (51) | ≥30 | 34,198 (46) | T2 | Medical record | 13,938 (NA) | Both | Age, BMI, deprivation, HDL-C, TC, SBP, smoking, statin and antihypertensive drug prescriptions |
| Ballotari et al [21] | Italy | 2011 | 3 | Population-based | 356,191 (51) | 30–84 | 24,348 (44) | T2 | Diabetes register | 2321 (44) | Both | Age, foreign status d |
| NHS Information Services Scotland [18] | UK | 2004–2013 | 10 | Population-based | T1: 18,240 (45), T2 136,042 (46), no diabetes 3,066,253 (54) | ≥30 | T1: 18,240 (45), T2: 136,042 (46) | T1, T2 | Diabetes register | T1: 1313 (NA), T2: 22,959 (NA), no diabetes: 91,429 (NA) | Both | Age, socioeconomic status, calendar year e |
If endpoints were reported as incident, they were considered to include both fatal and non-fatal events, e.g. hospitalisation for heart failure
aN of total participants in APCSC was derived from overall participants. One out of 36 cohorts in APCSC (n = 12,203/543,694, 2.2%) consisted of male only
bN of total participants in Policardo et al was derived from overall participants (≥16 years old)
cRRs for controlled diabetes in participants aged <60 were extracted
dRRs were classified to be age-adjusted
eRRs for 2013 (aged ≥30 years) were extracted
AF, atrial fibrillation; APCSC, Asia Pacific Cohort Studies Collaboration; CALIBER, Cardiovascular disease research using LInked Bespoke studies and Electronic health Records; CCI, Charlson Comorbidity Index; CHS, Cardiovascular Health Study; COPD, chronic obstructive pulmonary disease; CVD, cardiovascular disease; F, fatal; HDL-C, HDL-cholesterol; HT, hypertension; Hx, history; KPMCP, Northern California Kaiser Permanente Medical Care Program; LRPP, Cardiovascular Disease Lifetime Risk Pooling Project (Framingham Heart, Framingham Offspring, Atherosclerosis Risk In Communities [ARIC], Chicago Heart Association Detection Project in Industry Study [CHA]); LVH, left ventricular hypertrophy; MI, myocardial infarction; NA, not available; NDR, National Diabetes Registry; NHANES I, First National Health and Nutrition Examination Survey; NHI, National Health Insurance; NHS, National Health Service; SBP, systolic BP; T1, type 1 diabetes; T2, type 2 diabetes; TC, total cholesterol
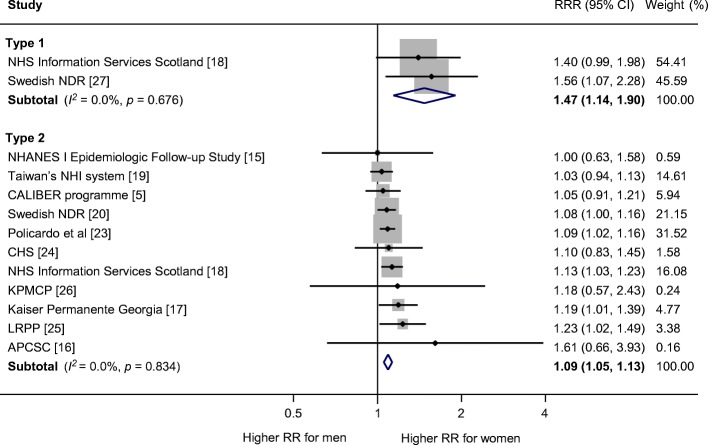
The multiple-adjusted pooled sex-specific RRs for heart failure associated with type 1 diabetes were 5.15 (95% CI 3.43, 7.74, p < 0.001) in women and 3.47 (2.57, 4.69, p < 0.001) in men (Fig. 2). The pooled multiple-adjusted RRR indicated a significantly greater excess risk for heart failure in women with type 1 diabetes compared with men. The women-to-men RRR was 1.47 (1.14, 1.90, p = 0.003 [Fig. 3]). The I2 statistics for heterogeneity between studies were 0.0%.
Fig. 2.
Multiple-adjusted RR for heart failure, comparing individuals with type 1 and type 2 diabetes with those without diabetes for (a) women and (b) men. APCSC, Asia Pacific Cohort Studies Collaboration; CALIBER, Cardiovascular disease research using LInked Bespoke studies and Electronic health Records; CHS, Cardiovascular Health Study; KPMCP, Northern California Kaiser Permanente Medical Care Program; LRPP, Cardiovascular Disease Lifetime Risk Pooling Project (Framingham Heart, Framingham Offspring, Atherosclerosis Risk In Communities [ARIC], Chicago Heart Association Detection Project in Industry Study [CHA]); NDR, National Diabetes Registry; NHANES I, First National Health and Nutrition Examination Survey; NHI, National Health Insurance; NHS, National Health Service
Fig. 3.
Multiple-adjusted women-to-men RRR for heart failure, comparing individuals with type 1 and type 2 diabetes with those without diabetes. APCSC, Asia Pacific Cohort Studies Collaboration; CALIBER, Cardiovascular disease research using LInked Bespoke studies and Electronic health Records; CHS, Cardiovascular Health Study; KPMCP, Northern California Kaiser Permanente Medical Care Program; LRPP, Cardiovascular Disease Lifetime Risk Pooling Project (Framingham Heart, Framingham Offspring, Atherosclerosis Risk In Communities [ARIC], Chicago Heart Association Detection Project in Industry Study [CHA]); NDR, National Diabetes Registry; NHANES I, First National Health and Nutrition Examination Survey; NHI, National Health Insurance; NHS, National Health Service
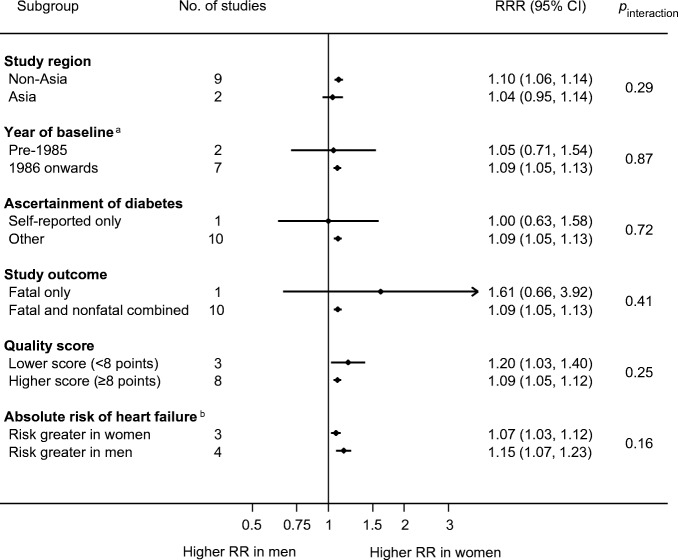
The sex-specific RRs for heart failure associated with type 2 diabetes was 1.95 (95% CI 1.70, 2.22, p < 0.001) in women and 1.74 (1.55, 1.95, p < 0.001) in men (Fig. 2), with the women-to-men RRR of 1.09 (1.05, 1.13), p < 0.001, I2 = 0.0% (Fig. 3). There was no evidence of publication bias for the association between type 2 diabetes and heart failure (Egger’s test p = 0.27, Begg’s test p = 0.31, ESM Fig. 1). In subgroup analyses, the pooled women-to-men multiple-adjusted RRR did not differ significantly by study region (p = 0.29), year of baseline study (p = 0.87), ascertainment of diabetes (p = 0.72), study outcome (p = 0.41), quality of study (p = 0.25), or absolute risk differences between men and women (p = 0.16) (Fig. 4).
Fig. 4.
Subgroup analyses of multiple-adjusted women-to-men RRR for heart failure, comparing individuals with type 2 diabetes with those without. aYear of baseline: two studies were excluded because baseline year bridged pre-1985 and 1986 onwards. bAbsolute risk of heart failure: absolute risk was derived using data from individuals with and without diabetes combined. Four studies were excluded because absolute risk was not available for both sexes
For type 2 diabetes, five studies provided age-adjusted estimates. The pooled age-adjusted sex-specific RRs for heart failure associated with diabetes were 2.56 (95% CI 2.31, 2.84, p < 0.001) in women and 2.49 (2.04, 3.04, p < 0.001) in men. The pooled age-adjusted women-to-men RRR for heart failure was 1.00 (0.78, 1.27, p = 0.98). The I2 statistics for heterogeneity between studies was 87.6%, suggesting substantial heterogeneity.
In sensitivity analysis, restricted to studies which provided the sex-specific RRs for both multiple-adjusted and age-adjusted models, the pooled women-to-men RRR was 1.17 (95% CI 1.02, 1.35, p = 0.02) for multiple-adjusted analysis, and 1.19 (1.06, 1.34, p = 0.005) for age-adjusted analysis (ESM Fig. 2).
Discussion
The present meta-analysis, of 47 cohorts including more than 12 million individuals, showed that both type 1 and type 2 diabetes were a stronger risk factor for heart failure in women than men. Type 1 diabetes was associated with a 47% greater excess risk of heart failure in women compared with men, and type 2 diabetes was associated with a 9% greater excess risk of heart failure in women than men. The sex difference in the association between type 2 diabetes and heart failure was consistent across a range of prespecified subgroups. These findings are in agreement with the previous evidence showing that diabetes has stronger associations with diabetic complications for women than men, and shed light on the importance of a routine sex-specific approach both in research and clinical practice in this field.
A previous meta-analysis reported that diabetes was associated with the risk of heart failure in both women and men [2]. However, this previous meta-analysis included studies consisting of women or men only, as well as studies among both women and men, and therefore could have introduced bias in quantifying sex differences. Further, sex-specific RRs were not reported for type 1 diabetes. The present meta-analysis includes additional two-sex studies that were not included previously, and provides evidence that both type 2 diabetes and type 1 diabetes are a risk factor for heart failure in both sexes, with significantly stronger associations in women than men. These findings suggest that healthcare providers and policy makers should be aware of this greater excess risk of heart failure, as well as other diabetic complications [8–11, 28, 29], in women than men.
In our analyses of type 2 diabetes, the women-to-men RRR was greater when multiple-adjusted RRs were pooled compared with when age-adjusted RRs were pooled (multiple-adjusted RRR 1.09 [95% CI 1.05, 1.13] vs age-adjusted RRR 1.00 [0.78, 1.27]). A significant degree of heterogeneity between studies was observed for age-adjusted analyses (I2 = 87.6%, p < 0.001), but not for multiple-adjusted analyses (I2 = 0.0%, p = 0.834). On the other hand, the sensitivity analysis including the studies that reported both multiple-adjusted and age-adjusted estimates provided almost similar results, indicating a greater excess risk of heart failure associated with diabetes in women than men. Therefore, we speculate that the difference observed between multiple-adjusted and age-adjusted analyses is likely due to chance differences between the studies included. Furthermore, we believe that multiple-adjusted estimates, which adjust for other major cardiovascular risk factors in addition to age, are more likely to represent true aetiology.
There are several potential explanations for the greater excess risk of heart failure associated with diabetes in women compared with men. First, the observed sex differences could be driven by there being a greater risk of CHD conferred by diabetes in women than men, because CHD is a major cause of heart failure in people with type 2 diabetes [1]. Our previous large-scale meta-analyses showed that diabetes conferred a 44% greater excess risk of incident CHD in women than men [8]. A significant sex difference was also observed in a meta-analysis which focused specifically on type 1 diabetes and CHD [28]. Sex differences in the management of diabetes could underpin these associations. Historically, women with diabetes had poorer glycaemic control than men with diabetes [30–34]. Second, in addition to CHD, undertreatment for women with diabetes could also contribute to the development of diabetic cardiomyopathy, a form of cardiac dysfunction that occurs independently of CHD and hypertension [35, 36], and could subsequently lead to a stronger association of diabetes with heart failure in women than men. Third, prolonged exposure to hyperglycaemia during the prediabetic state may also be involved. Women were reported to have 2 years longer duration of prediabetes than men [37]. Longer duration of prediabetes has been shown to be associated with left ventricular systolic and diastolic dysfunction [38]. Finally, it is also possible that sex differences in other cardiovascular risk factor profiles [30–33, 39–41] account for the greater excess risk of heart failure associated with diabetes in women compared with men. Deteriorations in major cardiovascular risk factor levels in individuals with diabetes compared with those without diabetes are reported to be greater in women than in men [9, 42, 43].
It might be also possible that the sex differences found in this study are a mathematical artefact caused by the relatively low absolute risk for heart failure in women compared with men. Suppose that the absolute risk difference following diabetes is the same in men as it is in women, then there would automatically be a larger RR among women compared with men. However, RRs, rather than absolute risk differences, are much more commonly reported in clinical studies, given their stability across different populations. No sex differences between women and men were found in our previous meta-analyses for risk factors and cardiovascular diseases [44, 45], which indicates that detection of a female disadvantage based on RRs is not inevitable.
Regarding type of diabetes, the excess risk of heart failure associated with diabetes was greater in type 1 diabetes than type 2 diabetes. The women-to-men RRR was 1.47 (95% CI 1.14, 1.90) for type 1 diabetes, and 1.09 (1.05, 1.13) for type 2 diabetes. The reason for this difference between type 1 and type 2 diabetes is unclear, but it may be partly explained by the above-mentioned sex differences in the association between diabetes and CHD. In our previous meta-analyses, type 1 diabetes showed a stronger sex difference in the association with incident CHD than type 2 diabetes, with women-to-men RRR of 2.54 (1.80, 3.60) for type 1 diabetes [28] and 1.44 (1.27, 1.63) for type 2 diabetes [8]. Future large-scale individual participant data meta-analysis and mechanistic studies might elucidate this difference.
The strengths of this meta-analysis are the large number of study participants and exclusion of studies which provided data for only one sex, which reduced the risk of both sampling and non-sampling error. This enabled us to provide robust evidence on the presence of sex differences in the risk of heart failure conferred by diabetes. Furthermore, the findings were consistent across a range of prespecified subgroups. Some limitations of this study should be mentioned. First, this meta-analysis was based on published data, with heterogeneity in study design, ascertainment of diabetes, definition of endpoint and extent of adjustment for confounding factors across studies. However, since we only included studies with results for both sexes, we minimised these issues by conducting within-study comparisons of the sexes. Second, there may be other unmeasured confounding factors in addition to those adjusted for in each study. Third, information on duration of diabetes, glycaemic control, glucose-lowering drugs or phenotype of heart failure was not available, and thus we cannot conduct detailed assessments regarding these factors. Analyses considering these factors would provide insight into potential explanation for the observed sex differences, and will be the subject of our future research. Fourth, the competing risk of premature death was not adjusted for in the present meta-analysis. Men with diabetes are at an increased risk of premature death compared with women with diabetes [46] (as indeed is the case in general populations), and therefore may be less likely to develop heart failure. This could partly explain the greater excess risk of heart failure following diagnosis of diabetes in women than men. Finally, we only found two studies of type 1 diabetes, which compromises the accuracy of our estimates in this regard. Additional studies are needed to address this issue.
In conclusion, the excess risk of heart failure following diagnosis of diabetes is significantly greater in women than men, highlighting the importance of intensive prevention and treatment of diabetes for women as well as men. Further research is required to understand the mechanisms underpinning the excess risk of heart failure conferred by diabetes (particularly type 1) in women and to reduce the burden associated with diabetes in both sexes.
Electronic supplementary material
(PDF 266 kb)
Abbreviation
- RRR
Ratio of RR
Contribution statement
TO conceived the research, conducted the systematic review and all the analyses, and wrote the paper. YK conducted the systematic review and made critical revision of the manuscript. MW supervised the work and, together with SAEP, interpreted the data and made critical revision of the manuscript. All authors gave final approval of the version to be published. TO is the guarantor of this work.
Funding
This study received no external funding. TO is supported by the John Chalmers Clinical Research Fellowship of the George Institute. SAEP is supported by a Medical Research Council (UK) fellowship and MW is supported by a National Health and Medical Research Council (Australia) fellowship and Program Grant.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Duality of interest
MW is a consultant to Amgen and Kirin. All other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Toshiaki Ohkuma, Email: tohkuma@georgeinstitute.org.au.
Sanne A. E. Peters, Email: speters@georgeinstitute.org.uk
References
- 1.Seferovic PM, Petrie MC, Filippatos GS, et al. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20(5):853–872. doi: 10.1002/ejhf.1170. [DOI] [PubMed] [Google Scholar]
- 2.Aune D, Schlesinger S, Neuenschwander M, et al. Diabetes mellitus, blood glucose and the risk of heart failure: a systematic review and meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis. 2018;28(11):1081–1091. doi: 10.1016/j.numecd.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Dauriz M, Targher G, Laroche C, et al. Association between diabetes and 1-year adverse clinical outcomes in a multinational cohort of ambulatory patients with chronic heart failure: results from the ESC-HFA heart failure long-term registry. Diabetes Care. 2017;40(5):671–678. doi: 10.2337/dc16-2016. [DOI] [PubMed] [Google Scholar]
- 4.Johansson I, Edner M, Dahlstrom U, Nasman P, Ryden L, Norhammar A. Is the prognosis in patients with diabetes and heart failure a matter of unsatisfactory management? An observational study from the Swedish Heart Failure Registry. Eur J Heart Fail. 2014;16(4):409–418. doi: 10.1002/ejhf.44. [DOI] [PubMed] [Google Scholar]
- 5.Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015;3(2):105–113. doi: 10.1016/S2213-8587(14)70219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sattar N, Preiss D. Research digest: heart failure in diabetes comes into focus. Lancet Diabetes Endocrinol. 2018;6(8):603. doi: 10.1016/S2213-8587(18)30212-2. [DOI] [PubMed] [Google Scholar]
- 7.Regensteiner JG, Golden S, Huebschmann AG, et al. Sex differences in the cardiovascular consequences of diabetes mellitus: a scientific statement from the American Heart Association. Circulation. 2015;132(25):2424–2447. doi: 10.1161/CIR.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 8.Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57(8):1542–1551. doi: 10.1007/s00125-014-3260-6. [DOI] [PubMed] [Google Scholar]
- 9.Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet. 2014;383(9933):1973–1980. doi: 10.1016/S0140-6736(14)60040-4. [DOI] [PubMed] [Google Scholar]
- 10.Chatterjee S, Peters SA, Woodward M, et al. Type 2 diabetes as a risk factor for dementia in women compared with men: a pooled analysis of 2.3 million people comprising more than 100,000 cases of dementia. Diabetes Care. 2016;39(2):300–307. doi: 10.2337/dc15-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohkuma T, Peters SAE, Woodward M. Sex differences in the association between diabetes and cancer: a systematic review and meta-analysis of 121 cohorts including 20 million individuals and one million events. Diabetologia. 2018;61(10):2140–2154. doi: 10.1007/s00125-018-4664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association Standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S1–S186. [Google Scholar]
- 14.Wells G, Shea B, O’Connell D et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 19 Dec 2018
- 15.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161(7):996–1002. doi: 10.1001/archinte.161.7.996. [DOI] [PubMed] [Google Scholar]
- 16.Huxley RR, Barzi F, Woo J, et al. A comparison of risk factors for mortality from heart failure in Asian and non-Asian populations: an overview of individual participant data from 32 prospective cohorts from the Asia-Pacific Region. BMC Cardiovasc Disord. 2014;14(1):61. doi: 10.1186/1471-2261-14-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal A, Norton CR, Thomas TN, et al. Predictors of incident heart failure in a large insured population: a one million person-year follow-up study. Circ Heart Fail. 2010;3(6):698–705. doi: 10.1161/CIRCHEARTFAILURE.110.938175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAllister DA, Read S, Kerssens J, et al. Incidence of hospitalisation for heart failure and case-fatality among 3.25 million people with and without diabetes. Circulation. 2018;138(24):2774–2786. doi: 10.1161/CIRCULATIONAHA.118.034986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen HF, Ho CA, Li CY. Risk of heart failure in a population with type 2 diabetes versus a population without diabetes with and without coronary heart disease. Diabetes Obes Metab. 2019;21(1):112–119. doi: 10.1111/dom.13493. [DOI] [PubMed] [Google Scholar]
- 20.Rosengren A, Edqvist J, Rawshani A, et al. Excess risk of hospitalisation for heart failure among people with type 2 diabetes. Diabetologia. 2018;61(11):2300–2309. doi: 10.1007/s00125-018-4700-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ballotari P, Venturelli F, Greci M, Giorgi Rossi P, Manicardi V. Sex differences in the effect of type 2 diabetes on major cardiovascular diseases: results from a population-based study in Italy. Int J Endocrinol. 2017;2017:6039356. doi: 10.1155/2017/6039356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leung AA, Eurich DT, Lamb DA, et al. Risk of heart failure in patients with recent-onset type 2 diabetes: population-based cohort study. J Card Fail. 2009;15(2):152–157. doi: 10.1016/j.cardfail.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Policardo L, Seghieri G, Francesconi P, Anichini R, Franconi F, Del Prato S. Gender difference in diabetes related excess risk of cardiovascular events: when does the ‘risk window’ open? J Diabetes Complicat. 2017;31(1):74–79. doi: 10.1016/j.jdiacomp.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Vimalananda VG, Biggs ML, Rosenzweig JL, et al. The influence of sex on cardiovascular outcomes associated with diabetes among older black and white adults. J Diabetes Complicat. 2014;28(3):316–322. doi: 10.1016/j.jdiacomp.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmad FS, Ning H, Rich JD, Yancy CW, Lloyd-Jones DM, Wilkins JT. Hypertension, obesity, diabetes, and heart failure-free survival: the cardiovascular disease Lifetime Risk Pooling Project. JACC Heart Fail. 2016;4(12):911–919. doi: 10.1016/j.jchf.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alexander M, Grumbach K, Selby J, Brown AF, Washington E. Hospitalization for congestive heart failure. Explaining racial differences. JAMA. 1995;274(13):1037–1042. [PubMed] [Google Scholar]
- 27.Rosengren A, Vestberg D, Svensson AM, et al. Long-term excess risk of heart failure in people with type 1 diabetes: a prospective case-control study. Lancet Diabetes Endocrinol. 2015;3(11):876–885. doi: 10.1016/S2213-8587(15)00292-2. [DOI] [PubMed] [Google Scholar]
- 28.Huxley RR, Peters SA, Mishra GD, Woodward M. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(3):198–206. doi: 10.1016/S2213-8587(14)70248-7. [DOI] [PubMed] [Google Scholar]
- 29.Shen Y, Cai R, Sun J, et al. Diabetes mellitus as a risk factor for incident chronic kidney disease and end-stage renal disease in women compared with men: a systematic review and meta-analysis. Endocrine. 2017;55(1):66–76. doi: 10.1007/s12020-016-1014-6. [DOI] [PubMed] [Google Scholar]
- 30.Penno G, Solini A, Bonora E, et al. Gender differences in cardiovascular disease risk factors, treatments and complications in patients with type 2 diabetes: the RIACE Italian multicentre study. J Intern Med. 2013;274(2):176–191. doi: 10.1111/joim.12073. [DOI] [PubMed] [Google Scholar]
- 31.Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex disparities in treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28(3):514–520. doi: 10.2337/diacare.28.3.514. [DOI] [PubMed] [Google Scholar]
- 32.Vaccaro O, Boemi M, Cavalot F, et al. The clinical reality of guidelines for primary prevention of cardiovascular disease in type 2 diabetes in Italy. Atherosclerosis. 2008;198(2):396–402. doi: 10.1016/j.atherosclerosis.2007.10.026. [DOI] [PubMed] [Google Scholar]
- 33.Nilsson PM, Theobald H, Journath G, Fritz T. Gender differences in risk factor control and treatment profile in diabetes: a study in 229 Swedish primary health care centres. Scand J Prim Health Care. 2004;22(1):27–31. doi: 10.1080/02813430310003264. [DOI] [PubMed] [Google Scholar]
- 34.Petitti DB, Klingensmith GJ, Bell RA, et al. Glycemic control in youth with diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr. 2009;155(5):668–672. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115(25):3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 36.Ryden L, Grant PJ, Anker SD, et al. ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the task force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD) Eur Heart J. 2013;34(39):3035–3087. doi: 10.1093/eurheartj/eht108. [DOI] [PubMed] [Google Scholar]
- 37.Bertram MY, Vos T. Quantifying the duration of pre-diabetes. Aust N Z J Public Health. 2010;34(3):311–314. doi: 10.1111/j.1753-6405.2010.00532.x. [DOI] [PubMed] [Google Scholar]
- 38.Reis JP, Allen NB, Bancks MP, et al. Duration of diabetes and prediabetes during adulthood and subclinical atherosclerosis and cardiac dysfunction in middle age: the CARDIA study. Diabetes Care. 2018;41(4):731–738. doi: 10.2337/dc17-2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gouni-Berthold I, Berthold HK, Mantzoros CS, Bohm M, Krone W. Sex disparities in the treatment and control of cardiovascular risk factors in type 2 diabetes. Diabetes Care. 2008;31(7):1389–1391. doi: 10.2337/dc08-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gobl CS, Brannath W, Bozkurt L, et al. Sex-specific differences in glycemic control and cardiovascular risk factors in older patients with insulin-treated type 2 diabetes mellitus. Gend Med. 2010;7(6):593–599. doi: 10.1016/j.genm.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Duggirala MK, Cuddihy RM, Cuddihy MT, Nyman MA, Naessens JM, Pankratz VS. Women with diabetes have poorer control of blood pressure than men. J Women's Health. 2005;14(5):418–423. doi: 10.1089/jwh.2005.14.418. [DOI] [PubMed] [Google Scholar]
- 42.Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non-diabetes than men? The British Regional Heart Study and British Women’s Heart Health Study. Diabetologia. 2012;55(1):80–87. doi: 10.1007/s00125-011-2284-4. [DOI] [PubMed] [Google Scholar]
- 43.Howard BV, Cowan LD, Go O, Welty TK, Robbins DC, Lee ET. Adverse effects of diabetes on multiple cardiovascular disease risk factors in women. The Strong Heart Study. Diabetes Care. 1998;21(8):1258–1265. doi: 10.2337/diacare.21.8.1258. [DOI] [PubMed] [Google Scholar]
- 44.Peters SA, Huxley RR, Woodward M. Comparison of the sex-specific associations between systolic blood pressure and the risk of cardiovascular disease: a systematic review and meta-analysis of 124 cohort studies, including 1.2 million individuals. Stroke. 2013;44(9):2394–2401. doi: 10.1161/STROKEAHA.113.001624. [DOI] [PubMed] [Google Scholar]
- 45.Mongraw-Chaffin ML, Peters SA, Huxley RR, Woodward M. The sex-specific association between BMI and coronary heart disease: a systematic review and meta-analysis of 95 cohorts with 1.2 million participants. Lancet Diabetes Endocrinol. 2015;3(6):437–449. doi: 10.1016/S2213-8587(15)00086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baena-Diez JM, Penafiel J, Subirana I, et al. Risk of cause-specific death in individuals with diabetes: a competing risks analysis. Diabetes Care. 2016;39(11):1987–1995. doi: 10.2337/dc16-0614. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 266 kb)
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.