Abstract
Objectives
Cross-country (CC) skiing consists of two main techniques: classic and skating. Hip motion during the skating technique is similar to that in ice skating and is considered a risk factor for femoroacetabular impingement (FAI) in ice hockey players. We aimed to compare the presence of CAM-type FAI in a cohort of elite junior CC (EJCC) skiers with a control group of non-athlete (NA) high school students.
Methods
Observational cohort study: EJCC skiers and NAs were recruited from a sports school and a regular high school, respectively. Baseline demographics and training history were obtained via a questionnaire. Bilateral hip MRI was performed and the alpha angle was measured in three planes. CAM deformity was defined as an alpha angle>55° on at least two MRI planes per hip.
Results
A total of 20 EJCC skiers and 10 NAs participated. All participants were male, aged 16–19 years. Average training volume was 528.10±68.34 hours per year for the EJCC skiers compared with 153.50±57.09 for the NAs (p<0.001). The prevalence of CAM deformity in at least one hip on MRI was 50% in both groups (10 CC skiers and 5 NAs). The average alpha angles were 52.4±6.1° in the EJCC group and 52.5±4.9° in the NA group (p=0.94).
Conclusion
Radiographic evidence of CAM-type FAI was not more common in the CC skiers compared with NAs. The type, rather than volume or intensity of training, maybe a more important risk factor for the development of CAM-type FAI in young athletes.
Keywords: FAI, femoroacetabular impingement, CAM, cross-country, athlete
What are the new findings?
Using MRI, there was no evidence of greater prevalence of CAM-type femoroacetabular impingement (FAI) among elite junior cross-country (EJCC) skiers than non-athlete (NA) high school students.
The prevalence of positive clinical tests for FAI was not more common among the EJCC skiers than NA controls.
The type, rather than volume or intensity of training, maybe a more important risk factor for CAM-type FAI in young athletes.
Introduction
Femoroacetabular impingement (FAI) syndrome is a diagnosis based on a triad of appropriate symptoms, positive clinical signs and correlating imaging findings.1 Abnormal morphology of the proximal femur and/or acetabulum is the underlying cause, resulting in premature contact between these two structures during hip motion. FAI can be classified based on the abnormal morphology with CAM-type impingement involving the proximal femur and pincer-type isolated to the acetabulum. A mixed-type involves abnormalities of both the femur and acetabulum.2
FAI has received considerable attention in the scientific community over the past several years as our understanding of the causes, natural history and treatments has evolved. While this has identified some possible aetiologies for the development of the syndrome, there remain many questions about risk factors and preventative strategies. One proposed aetiology for the creation of CAM deformity is the effect of high-volume training on the developing proximal femoral physis. This has been implicated in the creation of CAM deformity in several sports, including ice hockey,3 4 soccer,5 basketball6 and athletics.7 It is unclear if this relationship is true for all athletic activities or specific to certain sports. Specifically, there is a paucity of information related to the risk of developing CAM-type FAI in cross-country (CC) skiing.
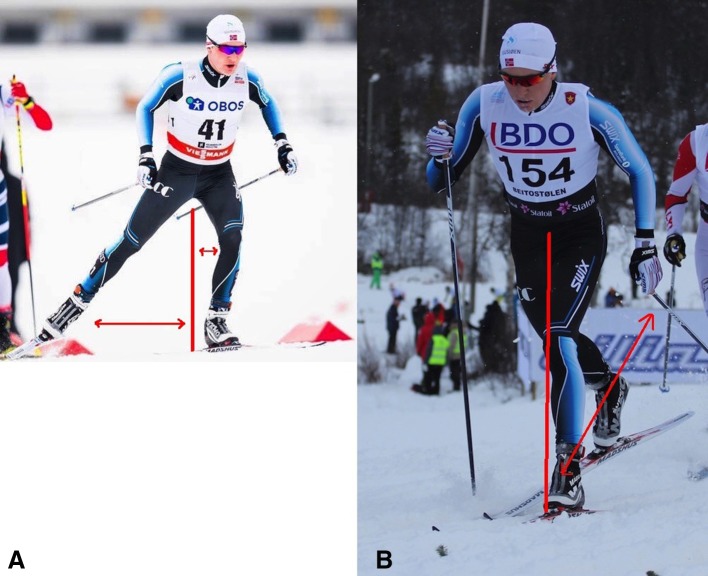
CC skiing is one of the most popular Nordic sports and competitive athletes must devote a substantial amount of time to training. CC skiing consists of two main techniques: classic and skating (figure 1). Hip motion during the classic technique primarily consists of repeated flexion and extension, while the skating technique involves a more complex movement pattern adding abduction, adduction and rotational actions. This motion is similar to ice skating, which is a proposed risk factor for CAM-type FAI.4 The purpose of this study was to compare the presence of CAM-type FAI in a cohort of elite junior CC (EJCC) skiers with a control group of non-athletes (NA).
Figure 1.
(a) Skating technique involving abduction/adduction and internal/external rotation movements of the hip. (b) Classic technique with a primarily flexion/extension hip movement pattern.
Methods
Study design
This observational cohort study was implemented to study the relationship between excessive training and the development of CAM-type FAI. EJCC skiers and NA were recruited from a sports school and a regular high school, respectively. Baseline demographic information and training history were obtained via a questionnaire (online supplementary file 1). Subjective assessment of hip function was evaluated with the International Hip Outcome Tool-33 (iHOT-33)8 for each hip (online supplementary file 2). Inclusion criteria for the EJCC skiers consisted of a minimum weekly training volume of 10 hours, while the maximum weekly training volume was 3.5 hours for the NA. Exclusion criteria included previous hip surgery or other diagnosed hip pathology.
bmjsem-2019-000530supp001.pdf (87.7KB, pdf)
bmjsem-2019-000530supp002.pdf (73.5KB, pdf)
Clinical examination
Hip range of motion was recorded through clinical examination which was performed by two authors (SAS and LE). The presence or absence of impingement signs was assessed with the Flexion-Adduction-Internal Rotation (FADIR) and Flexion-Abduction-External Rotation (FABER) tests, with a positive result defined as a provocation of symptoms during testing.
Radiological examination
All subjects were scanned in a GE Achieva 1.5 T MRI scanner with a torso coil. No contrast material was administered. Only one sequence, a three-dimensional isotropic T1-weighted turbo spin-echo sequence (3D PelvicView), 350×350 matrix, 1 mm voxel, repetition time (TR)=400, echo time (TE)=shortest, flip angle=90°, was acquired. The scan covered pelvis and both hips. All measurements were done by one blinded radiologist (EA).
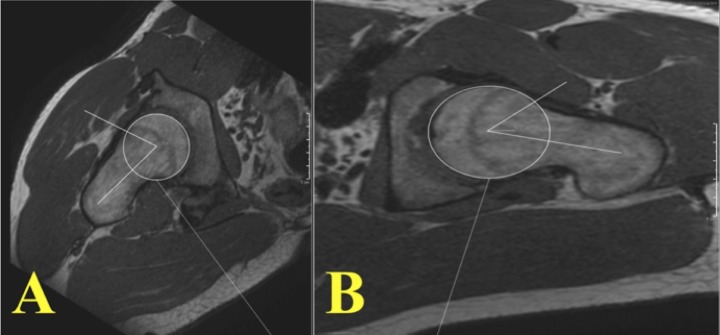
The MRI examination was sent to Picture Archiving and Communication System (PACS) (Carestream Vue PACS) where the study was loaded into a multiplanar reconstruction tool. Three reconstructions were made on both sides: one oblique axial along the femoral neck axis, one coronal oblique along the femoral neck and one oblique coronal/axial (figure 2).
Figure 2.
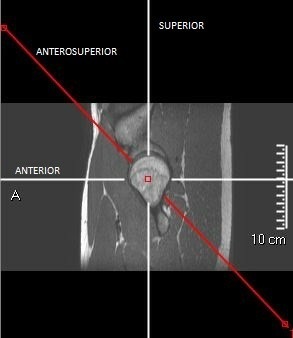
The three axes of alpha angle measurement.
This provided three sets of images per hip depicting the anterior, anterosuperior and superior femoral head–neck junction with respect to the femoral neck axis.
The alpha angle was measured in these three planes. Using PACS tools, a best-fit circle was drawn around the femoral head and a centre was defined. Alpha angle was measured between one line parallel to the neck axis through the head centre, and one line through the head centre and an intersection point of the best-fit circle and the head–neck border anteriorly (figure 3). Presence of CAM deformity was defined as an alpha angle>55° on at least two out of three of these MRI planes.9 10
Figure 3.
Example of alpha angle measurement. A best-fit circle was first drawn around the femoral head and the centre was defined. A line was then drawn parallel to the femoral neck axis from the head centre. A second line was drawn from the head centre to the point at which the femoral head/neck fell outside of the best-fit circle. The alpha angle was measured between these two lines. (A) Shows an alpha angle>55° (70.6°) and (B) shows an alpha angle<55° (52.2°).
The proximal femoral physis was assessed and graded as open or closed. An open physis was defined as a visible hypointense line through the femoral head.
Statistical analysis
Thirty persons (60 hips) were recruited and all participated in the study. Comparisons were conducted using t statistic tests and descriptive statistics. Statistical calculations were performed using GraphPad software. The alpha level for accepting statistical significance was set at 0.05.
Results
Baseline data
A total of 20 EJCC skiers and 10 NA participated, and all participants were male. No participants were excluded from the study due to a history of previous hip surgery or other diagnosed hip pathology. Baseline demographic information is presented in table 1.
Table 1.
Demographics
| EJCC skiers (n=20) | NA (n=10) | P value | |
| Age in years±SD | 17.82±0.89 | 18.07±0.64 | 0.437 |
| Open physis | 12 | 4 | 0.142 |
| Closed physis | 8 | 6 | 0.142 |
Three-year training history revealed a significantly greater average annual training volume of 528.10±68.34 hours for the EJCC skiers compared with 153.50±57.09 hours for the NA (p<0.001). Average training volume per week was 12.53±1.81 vs 3.10±1.11 hours, respectively.
EJCC, elite junior cross-country; NA, non-athletes.
No difference was detected in the evaluation of the iHOT-33. A score of 0 represents a significant amount of pain, while a score of 100 means that there is no hip pain. EJCC skiers scored on average 94.97±5.36 vs 92.49±5.60 in the NA (p=0.249).
Clinical examination
EJCC skiers had less hip abduction (p=0.014) and external rotation (p=0.032) versus the controls. Flexion, extension, adduction, and internal rotation were not statistically different (table 2).
Table 2.
Clinical examination included range of motion and impingement tests
| EJCC skiers | NA | P value | |
| Flexion | 120±3.87 | 122±5.10 | 0.240 |
| Extension | 10±0 | 10±0 | 1 |
| Abduction | 54.13±8.80 | 62.5±6.98 | 0.014 |
| Adduction | 30±0 | 30±0 | 1 |
| Internal rotation | 31.63±9.45 | 27±11.66 | 0.252 |
| External rotation | 45.63±7.92 | 53.75±11.71 | 0.032 |
| Positive impingement sign | n=6 | n=1 | 0.224 |
EJCC, elite junior cross-country; NA, non-athletes.
Radiological examination
Radiographic findings are summarised in tables 3–5.
Table 3.
Radiological findings I
| EJCC skiers (n=20) | NA (n=10) |
P value | |
| α-angle (anterior) | 49.50±7.58 | 50.25±7.01 | 0.713 |
| α-angle (anterosuperior) | 58.68±10.11 | 60.05±8.89 | 0.609 |
| α-angle (superior) | 48.85±5.64 | 47.05±5.57 | 0.247 |
| Average α-angle | 52.35±6.10 | 52.45±4.89 | 0.938 |
| CAM deformity in at least one hip | n=10 | n=5 | 1 |
EJCC, elite junior cross-country; NA, non-athletes.
Table 4.
Radiological findings II
| Open physis (n=16) | Closed physis (n=14) | P value | |
| α-angle (anteriorly) | 49.21±7.24 | 50.35±7.54 | 0.5529 |
| α-angle (anterosuperiorly) | 57.81±9.75 | 60.64±9.51 | 0.2612 |
| α-angle (superiorly) | 47.91±5.59 | 48.64±5.76 | 0.6207 |
Table 5.
Radiological findings III
| EJCC skiers (n=40 hips) | NA (n=20 hips) | P value | |
| Number of hips with CAM-type FAI in MRI | 13 | 9 | 0.3520 |
EJCC, elite junior cross-country; FAI, femoroacetabular impingement; NA, non-athletes.
The rate of CAM deformity in at least one hip on MRI was 50% in both groups (10 EJCC skiers and 5 NA). Three EJCC skiers and four NA had evidence of bilateral CAM deformity (p=0.3520) (table 5). The average alpha angle in the EJCC skier group was 52.35±6.10° compared with 52.45±4.89° in the NA group (p=0.938). There was no statistical difference in alpha angles between the participants with open and closed physes (table 4). Average alpha angles were higher in participants with positive clinical impingement signs than in those without clinical impingement (table 6).
Table 6.
Alpha angle in participants with positive impingement test
| Hips with positive clinical impingement | Hips with no clinical impingement | P value | |
| Number of hips | 10 | 50 | |
| Average alpha angle | 54.23±4.10 | 52.006±5.93 | <0.0001 |
Discussion
Main findings
The most significant finding of this study was that CAM-type FAI was not more common among a group of young elite CC skiers who devote a substantial amount of time to training versus the same age group in the general population. There was no statistical difference in the prevalence of CAM-type FAI on MRI or clinical impingement signs, and the 2° difference in average alpha angle between groups may be within measurement error. The EJCC skiers attend a sports school that accommodates their athletic training and competition schedules and allows at least one workout during school hours along with normal academic activities. The students at the sports school all participate in one specific sport, and they have to be at an elite level in their sport to be admitted. These student athletes engage in high-volume, high-intensity and sport-specific training throughout the year.
Relation to previous studies
Similar high levels of athletic activity have been implicated in other studies as a risk factor for developing FAI, specifically of the CAM-type.5–7 In particular, higher rates of CAM deformity have previously been associated with increasing age and level of competition in ice hockey players with a reported incidence of approximately 70%.4 Despite the similarities in hip motion between hockey and CC skiing, there was no increased rate of FAI observed in the EJCC cohort. It is possible that the proximal femoral physis may be partially protected by skiers alternating between classic and skating techniques in both training and competition. Another factor may be the surface difference between CC skiing and ice hockey. Skating style training activities of EJCC skiers are divided between skiing on snow and practising this technique on pavement with rollerskis (table 7).
Table 7.
Training specifics for EJCC skiers and NA
| EJCC skiers (% of total training) | NA (% of total training) | P value | |
| Running | 25 | 45 | 0.0137 |
| Rollerski classic | 15 | 0 | <0.0001 |
| Rollerski skating | 15 | 0 | <0.0001 |
| Ski classic | 15 | 2 | <0.0001 |
| Ski skating | 15 | 0 | <0.0001 |
| Bike riding | 7 | 1 | 0.0019 |
| Strength training | 8 | 52 | <0.0001 |
| Total | 100 | 100 |
EJCC, elite junior cross-country; NA, non-athletes.
In contrast, hockey players skate exclusively on ice or pavement which are much harder surfaces. Basketball players, in whom the prevalence of CAM deformity has been reported as 89%,6 also train and compete on wooden floors and other hard surfaces. It is possible that the softer snow confers some protection to the physis.
Previous studies have shown a prevalence of asymptomatic CAM deformities in 37%–55% of athletes, and 23% in the general population.11 This corresponds with the finding that the EJCC skier group had a 50% rate of CAM-type deformity. However, the rate of CAM-type deformity in the NA group was higher than expected, with 50% having an alpha angle above 55°. The amount of activity that puts one at risk for developing CAM deformity has not been previously identified and it is possible that the control group in this study were above this threshold with an average of 3 hours per week reported.
Clinical assessment of the two groups did not reveal any major differences. It is important to remember that the diagnosis of FAI relies on the presence of positive clinical findings and not radiography alone. The FADIR and FABER impingement tests have a low specificity, but the sensitivity is high for ruling out FAI.12 This finding is also consistent with the notion that high-intensity training of EJCC skiers may not increase the risk of developing FAI.
Limitations
There are limitations to this study. First, the survey used has not been previously validated. Further, the retrospective nature of the survey and subject recall introduces the potential for biassed estimates in training volume. The small number of participants limits the power to detect differences between groups and there may be risk factors other than training volume that contributed to the high rate of CAM deformity in both groups. This includes possible influences of genetic, environmental or other factors that were not accounted for. This study, also, only included male participants; we cannot draw conclusions about female elite CC skiers. Finally, the status of the proximal femoral physis may have influenced the outcome of this study. Twelve CC skiers still had open physes on MRI. On the basis of the proposed mechanism, it follows that they are still at risk of developing CAM deformity and thus, the effect of their training on the proximal femur morphology may be underestimated. To assess this, a group of senior elite CC skiers with closed physes would need to be evaluated with MRI and clinical signs.
Future directions
This study challenges the theory that high-intensity training increases the risk of developing CAM-type FAI. Future research should seek to quantify not only the training volume threshold but also the type of training activities that place young athletes at risk.
Conclusion
Radiographic evidence of CAM-type FAI was not more common in EJCC skiers compared with non-athlete controls. The type, rather than volume or intensity of training, may be a more important risk factor for the development of CAM-type FAI in young athletes. Future investigations should include the ‘type’ of training variable.
Footnotes
Contributors: SAS and LE contributed to project planning. SAS, EA and LE contributed to data collection. SAS, KM and LE contributed to the manuscript preparations and data analysis. LE is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The authors have no personal financial or institutional interest in any of the drugs, materials or devices described in this manuscript.
Competing interests: None declared.
Patient and public involvement statement: Patients were not involved in the design, recruitment, or execution of this study.
Patient consent for publication: Not required.
Ethics approval: The regional health research ethics board granted approval (date: 20 December 2016, No. 2016/1937).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request.
References
- 1. Griffin DR, Dickenson EJ, O'Donnell J, et al. . The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50:1169–76. 10.1136/bjsports-2016-096743 [DOI] [PubMed] [Google Scholar]
- 2. Ganz R, Parvizi J, Beck M, et al. . Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;(417):112–20. 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 3. Lerebours F, Robertson W, Neri B, et al. . Prevalence of Cam-Type morphology in elite ice hockey players. Am J Sports Med 2016;44:1024–30. 10.1177/0363546515624671 [DOI] [PubMed] [Google Scholar]
- 4. Philippon MJ, Ho CP, Briggs KK, et al. . Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am J Sports Med 2013;41:1357–62. 10.1177/0363546513483448 [DOI] [PubMed] [Google Scholar]
- 5. Lahner M, Walter PA, von Schulze Pellengahr C, et al. . Comparative study of the femoroacetabular impingement (FAI) prevalence in male semiprofessional and amateur soccer players. Arch Orthop Trauma Surg 2014;134:1135–41. 10.1007/s00402-014-2008-6 [DOI] [PubMed] [Google Scholar]
- 6. Siebenrock KA, Ferner F, Noble PC, et al. . The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res 2011;469:3229–40. 10.1007/s11999-011-1945-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lahner M, Bader S, Walter PA, et al. . Prevalence of femoro-acetabular impingement in international competitive track and field athletes. Int Orthop 2014;38:2571–6. 10.1007/s00264-014-2486-8 [DOI] [PubMed] [Google Scholar]
- 8. Mohtadi NGH, Griffin DR, Pedersen ME, et al. . The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International hip outcome tool (iHOT-33). Arthroscopy 2012;28:595–610. 10.1016/j.arthro.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 9. Johnston TL, Schenker ML, Briggs KK, et al. . Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy 2008;24:669–75. 10.1016/j.arthro.2008.01.010 [DOI] [PubMed] [Google Scholar]
- 10. Nötzli HP, Wyss TF, Stoecklin CH, et al. . The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002;84:556–60. 10.1302/0301-620X.84B4.12014 [DOI] [PubMed] [Google Scholar]
- 11. Frank JM, Harris JD, Erickson BJ, et al. . Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy 2015;31:1199–204. 10.1016/j.arthro.2014.11.042 [DOI] [PubMed] [Google Scholar]
- 12. Reiman MP, Goode AP, Cook CE, et al. . Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: a systematic review with meta-analysis. Br J Sports Med 2015;49:811 10.1136/bjsports-2014-094302 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjsem-2019-000530supp001.pdf (87.7KB, pdf)
bmjsem-2019-000530supp002.pdf (73.5KB, pdf)