Abstract
5-methyl cytosine (5mC) is a key epigenetic mark entwined with gene expression and the specification of cellular phenotypes. Its distribution around gene promoters sets a barrier for transcriptional enhancers or inhibitor proteins binding to their target sequences. As a result, an additional level of regulation is added to the signals that organize the access to the chromatin and its structural components. The tumor suppressor gene RASSF1A is a microtubule-associated and multitasking scaffold protein communicating with the RAS pathway, estrogen receptor signaling, and Hippo pathway. RASSF1A action stimulates mitotic arrest, DNA repair and apoptosis, and controls the cell cycle and cell migration. De novo methylation of the RASSF1A promoter has received much attention due to its increased frequency in most cancer types. RASSF1A methylation is preceded by histones modifications and could represent an early molecular event in cell transformation. Accordingly, RASSF1A methylation is proposed as an epigenetic candidate marker in many cancer types, even though an inverse correlation of methylation and expression remains to be fully ascertained. Some findings indicate that the epigenetic abrogation of RASSF1A can promote the alternative expression of the putative oncogenic isoform RASSF1C. Understanding the complexity and significance of RASSF1A methylation is instrumental for a more accurate determination of its biological and clinical role. The review covers the molecular events implicated in RASSF1A methylation and gene silencing and provides a deeper view into the significance of the RASSF1A methylation patterns in a number of gastrointestinal cancer types.
Keywords: RASSF1, RASSF1A, DNA methylation, grastrointestinal cancers, biomarker
1. The Tumor Suppressor RASSF1A
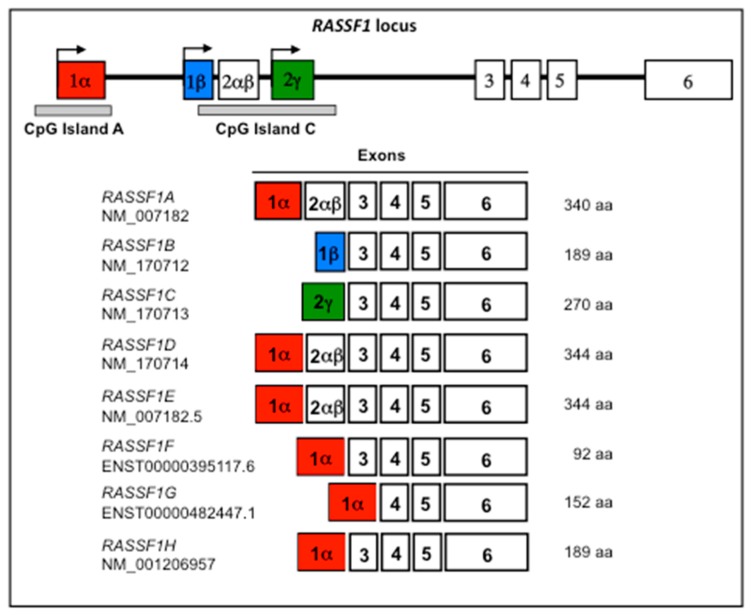
The RASSF1 locus, in the cytogenetic band chr3:p21.31, expresses eight main transcript variants under the control of two promoters overlapped to the CpG islands A and C [1]. The major, ubiquitous transcripts expressed by the RASSF1 locus are RASSF1A and RASSF1C [1,2]. RASSF1B and RASSF1C differ in the first exon. Additional RASSF1 isoforms, RASSF1D, RASSF1E, RASSF1F, RASSF1G, and RASSF1H derive from alternative splicing of RASSF1A. A schematic representation of the RASSF1 locus is reported in Figure 1.
Figure 1.
Schematic representation of the RASSF1 locus and its transcription map. White boxes represent the exons and the bold line represents the introns. RASSF1A (red), RASSF1B (blue), and RASSF1C (green) variants are generated by differential promoter and first exon usage (arrows). RASSF1D, RASSF1E, RASSF1F, RASSF1G, and RASSF1H are variants derived from alternative splicing of RASSF1A. Two CpG islands (grey bands below exons 1 and 2) are associated to RASSF1 promoter region: CpG island A (736 bp, 85 CpGs, chr3:50,340,373-50,341,109, GRCh38/hg38) extending in the promoter region of RASSF1A; CpG island C (1364 bp, 139 CpGs, chr3:50,336,834-50,338,198, GRCh38/hg38) in the regulatory region of RASSF1B and RASSF1C. A CpG island is defined as a sequence with a length greater than 200 bp, a GC content greater than 50% and a ratio greater than 0.6 of the observed number of CG dinucleotides with respect to the expected number on the basis of the number of Gs and Cs nucleotides in the segment.
The first exon of RASSF1A contains a cysteine-rich domain, reminiscent of the diacylglycerol-binding–CRD domain [1]. This domain is lacking in RASSF1B and RASSF1C. Most studies published on RASSF1 concern RASSF1A and RASSF1C. The function of RASSF1B, RASSF1D, RASSF1E, RASSF1F, RASSF1G, and RASSF1H has received little research attention.
The RASSF1A isoform is transcribed in the RASSF1 locus about 180 base pairs aside to the gene ZMYND10 (protein name BLU). Three binding sites for the insulator CCCTC-binding factor (CTCF) are overlapped to the 3′ end of ZMYND10, in a region between −453 and −2050 bp from the RASSF1A transcription start site. The insulator CTCF binds insulator sequences that separate functionally the transcription start sites of the two close genes forming two distinct epigenetic domains [3]. For this reason, despite their proximity, RASSF1A has often been found down-regulated in cancer as opposed to ZMYND10 [4].
The 3p.21.31 region may harbor candidate tumor suppressor genes due to the frequent copy number loss in various cancer types [5,6,7], including HYAL2, TUSC2, RASSF1, ZMYND10, NPRL2, CYB561D2, TMEM115. and CACNA2D2 [8]. The gene RASSF1A (RASSF1-association domain family 1, isoform A) was initially identified as a potential RAS binding molecule due to the presence of a RAS-association domain in its primary sequence. RASSF1A binds RAS in the GTP-bound form to promote apoptosis [9]. RASSF1A has been proposed to act as a tumor suppressor, since the loss of its function induces cell proliferation and tumorigenesis [10], and may be implicated in microtubule stabilization, apoptosis, cell cycle, and DNA repair [11,12,13,14,15]. The most relevant cell protection functions operated by RASSF1A are mediated by the interaction with the Hippo and the Wnt pathways and the modulator of apoptosis 1 (MOAP1) [16,17,18,19,20,21]. Aged RASSF1A(−/−) mice are prone to spontaneous tumorigenesis [20], particularly in the liver [22], suggesting that RASSF1A function is essential for a correct homeostasis and healthy state of cells. Moreover, DNA methylation and silencing of RASSF1A, along with another tumor suppressor gene, HIC1, transforms mesenchymal stem cells into cancer stem cells [23], implying that RASSF1A methylation (RASSF1Am) is part of a delicate hierarchical network of oncogenic gene silencing patterns involved in neoplastic transformation. In accordance with the above mentioned observations, RASSF1A is expressed in all normal tissues and at a lower level than RASSF1C [24]. Reverting RASSF1A down-regulation in cancer cell lines restores controlled growth and colony formation, as well as decreased cell migration and apoptosis [10,25,26,27,28,29,30].
2. Biological Role of RASSF1C
The function of the isoform RASSF1C is less well defined with respect to that of RASSF1A, although various studies converge upon the idea that the molecule could promote cell survival and proliferation, to thereby exert an opposite role to that attributed to RASSF1A. RASSF1C has been demonstrated to be nuclear or perinuclear with translocation to the cytosol upon DNA damage [31], or localized to microtubules similarly to RASSF1A [32,33]. The Daxx-RASSF1C complex has been shown to be involved in the DNA damage response and the SAPK/JNK signaling pathway [34]. Initially, RASSF1C has been shown to induce cell cycle arrest in cancer cell lines suggesting that, like RASSF1A, the RASSF1C gene could act as a tumor suppressor function [35]. Other findings support a potential role of RASSF1C as oncogene, promoting beta-catenin (CTNNB1) accumulation in HeLa cells [36] and proliferation of lung cancer cells [37], supporting cell migration and attenuated apoptosis in breast cancer [38].
3. DNA Methylation Changes
Methylation of cytosine to 5-methylcytosine (5mC) is a central epigenetic modification that feeds back on cellular processes including genome regulation organism development and disease. DNA methyltransferases DNMT1, DNMT3a, and DNMT3b establish specific 5mC patterns during embryonic development and cell differentiation and maintain them over many cell division cycles in adults [39]. DNMT1 is the enzyme responsible for the addition of methyl groups, immediately following DNA replication, preferentially to hemimethylated DNA. DNMT1 is post-transcriptionally regulated by a mutually exclusive Ser/Thr phosphorylation and Lys methylation under the control of PI3K-AKT-mTOR pathway [40,41,42]. DNMT3a and DNMT3b are preferentially implicated in de novo DNA methylation, that is the addition of one methyl group to cytosine in unmethylated CpG dinucleotides after DNA duplication [43]. DNA methylation can be reversed by Ten-eleven translocation (TET) enzymes (TET1, TET2, TET3), which are responsible for the fine-tuning methylation of patterns [44]. TET enzymes oxidize the methyl group of 5mC to yield 5-hydroxymethylcytosine, which facilitates both passive and active demethylation. The implications of methylation-demethylation epigenetic disequilibrium and of TET enzymes in gastrointestinal cancers have been observed in various studies [45,46,47,48,49,50,51]. Understanding DNA methylation-demethylation dynamics, and their epigenetic interplays in modulating transcription will open new perspectives for research on cellular differentiation and oncogenic transformation (see Ambrosi et al. [52] for a review).
DNMT1, DNMT3A, and DNMT3B enzymes are responsible for RASSF1Am in different contexts [53,54,55,56,57,58]. RASSF1Am seems to follow a precise cascade of events with recruitment of the complex HDAC1/SETDB1, that in turn attracts DNMT3A in cancer cells [58]. In lung cancer, ΔDNMT3B4 (DNMT3 that lacks exon 6) appears essential for RASSF1A silencing [55], while its high methylation profile is driven by other epigenetic signals to support gene silencing architecture that favors cancer growth [59].
5mCs are recognized by methyl-binding proteins that in turn recruit histone modifying and chromatin remodeling enzymes [60]. Capped 5mCs promote a closed chromatin structure by obstructing the binding of transcription factors (inhibitors and enhancers of gene transcription) [61,62]. Somatic reprogramming is a dramatic demonstration of the impact of DNA methylation on cell fate [63]. 5mCs are less frequent in the target sequences of transcription factors, or are selectively over-represented in some CpG islands, but are yet influencing transcriptional programs [64], suggesting that fine-tuned DNA methylation tends to be dynamically and functionally interconnected with cellular signaling pathways [65] (see Du et al. [66] for a review).
4. Methylation of RASSF1A in Normal Tissues of the Gastroenteric System
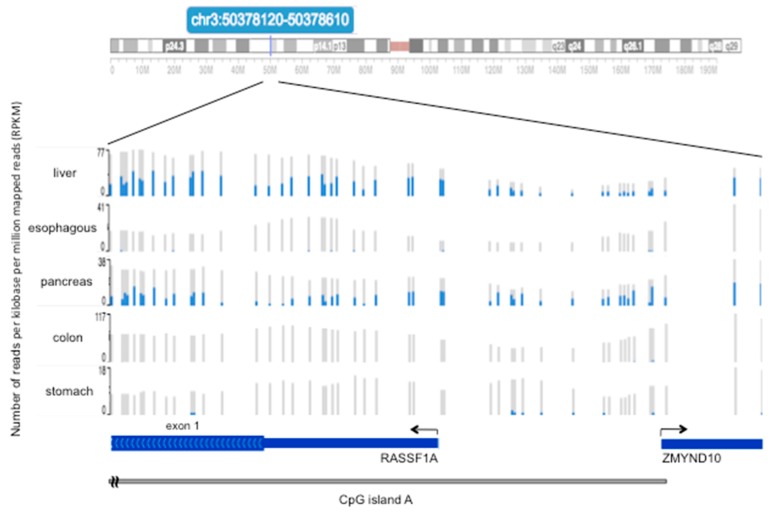
RASSF1Am usually refers to the methylation of the CpG island A, which covers the promoter and first exon of RASSF1A. There are few descriptions of the methylation status of RASSF1A at single CpG resolution in normal gastrointestinal tissues. Heterogeneous distribution and level of 5mCs in adjacent CpGs in the RASSF1A promoter and first exon was observed in the normal pancreas adjacent to pancreatic endocrine tumors [67]. In these individuals, CpG methylation ranged from absent to diffuse. Figure 2 shows the variable CpG methylation patterns found in five normal tissues of a 34-year-old healthy individual. In this example, CpG methylation was higher in the liver and pancreas and was almost absent in the esophagus, colon and, stomach. According to data reported in Figure 2, unmethylated RASSF1A status was found in 15 stomach normal tissues [68]. The Cancer Genome Atlas (TCGA) data confirmed a variable and higher RASSF1Am level in the normal liver and pancreas compared to colon and stomach (see Section 7).
Figure 2.
Methylation level of 48 CpGs in the promoter and first exon of RASSF1A in five normal tissue types. Results of bisulfite DNA sequencing on liver, esophagus, pancreas, colon, and stomach tissues samples taken from a 34-year-old healthy subject. The grey/blue vertical bars represent 48 CpGs overlapped to the promoter of RASSF1A and partially to first exon and CpG island A. For each CpG, the blue line is the number of reads for the 5mC and grey is the total number of reads (number of reads per kilobase per million mapped reads, RPKM) obtained by bisulfite DNA sequencing. The ratio between the two numbers represents the methylation level of a CpG. The grey bar at the bottom of the figure identifies the 3′ end of the CpG island A. The data were retrieved by the WashUp EpiGenome Browser at www.epigenomegateway.wustl.edu, provided by the Roadmap EpiGenome Project [69].
5. Mechanisms of RASSF1A Methylation in Cancer and Aging
All cancers are characterized by some degree of global epigenetic alteration entailing general DNA hypomethylation and abnormal hypermethylation in specific CpG islands. Alteration of DNA methylation patterns may depend on altered methyl group transfer during DNA duplication, or on defects of 5mC hydroxylation and demethylation operated by TET enzymes. In cancer and during aging, a substantial fraction of genes undergo a cell type-specific DNA hypermethylation of silenced genomic loci protein that is preceded by H3-K27 and H3-K9 trimethylations [70,71,72,73,74,75,76]. Analogously, an aberrant transcriptional silencing of RASSF1A triggered by the inactivating chromatin modification histone deacetylation and H3-K9 methylation preceded CpG island A hypermethylation [59] (see Klutstein et al. [77] for a review).
In differentiated cells, CpG islands particularly rich in CpGs and overlapped to gene promoters, as those present in RASSF1A, remain mostly unmethylated, even when the gene is inactive [59,78,79,80]. Thus, the occurrence of 5mCs in the CpG island A (Figure 2) could be considered as a somatically acquired abnormal event that spreads through the core region to initiate gene silencing, possibly reflecting distinct interactions among epigenetic machinery and components of the chromatin responsible for transcriptional regulation. [75,81,82].
RASSF1A is hypermethylated in most cancer types, and in some cases also in the adjacent normal tissues [1,83]. Aberrant RASSF1A promoter DNA methylation has been detected also in childhood neoplasia, including neuroblastoma, thyroid carcinoma, hepatocellular carcinoma, pancreatoblastoma, adrenocortical carcinoma, Wilms’ tumor, Burkitt’s lymphoma, and T-cell lymphoma [78]. The methylation of CpGs in the promoter and first exon of RASSF1A shows extreme variability in terms of distribution and relative levels of each CpG in single cell types, as well as in cancer and normal tissues [10,27,67,68,84,85,86,87,88,89,90]. This may possibly reflect a cell type- and/or clonal-based epigenetic heterogeneity.
It is reported that internal or environmental stimuli can promote epigenetic modifications that spread as silent events [85]. For example, RASSF1Am increases during physiological or patho-physiological processes such as aging, hypoxic conditions, senescence, inflammation, and viral infection [30,75,77,91,92,93,94,95]. De novo RASSF1Am associates with different factors and conditions; folate metabolism, DNA polymorphisms, as well as choline-deficient L-amino acid-defined diet in rats [96,97]. Early stages of estrogen-induced breast carcinogenesis in female rats is characterized by altered global DNA methylation, aberrant expression of proteins responsible for maintenance of DNA methylation pattern, and also by de novo RASSF1Am [98]. Transfection of hepatitis C virus core protein into hilar cholangiocarcinoma cell lines induces RASSF1A promoter DNA methylation and silencing [95]. In these contexts, RASSF1Am would function as an epigenetic sensor, associated to physiologic and disease conditions. The cell progeny could inherit a gene dosage pernicious for the RASSF1A-dependent cell functions that remains altered for the entire life of the organism. According to this model, de novo DNA methylation or demethylation at regulatory sites can anticipate the pathological transformation in different cell phenotypes before transformation ensues (epigenetic field defect) [85,99,100].
An age-dependent increase of RASSF1Am at differing speeds in different organs of healthy individuals is largely recapitulated in corresponding cancer types [74,75,76,77]. Thus, site-specific DNA hypermethylations that overlap in aging and tumorigenesis candidate these sites as cancer susceptibility hotspots. The epigenetic changes and the parallel increased risk of tumor onset occurring during aging keep open the possibility of a causative role of epigenetic reprogramming in RASSF1A silencing in support of progressive tumorigenesis.
6. Relationship between RASSF1A Methylation and Expression
The mechanisms that regulate DNA methylation and its consequences on gene transcription are only partially understood. The relative levels and patterns of methylation at specific CpG sites along the entire genome associate variably with gene expression [101]. More precisely, for each gene the correlation can be both positive or negative in different cell types suggesting tissue-specificity [102]. However, data relative to RASSF1 derived from omics techniques should be considered with caution since the applied experimental procedures might have not been sufficiently sensitive and able to provide high resolution data in the RASSF1 genomic region. RASSF1A expression is lost in different cancer types, as in lung, breast, and kidney cancer [103,104]. Consistently, epigenetic loss of RASSF1A has been proposed to serve as a diagnostic marker of clinical outcome in some cancer types [90,100,105,106,107].
There is currently poor understanding of the functional relevance of methylation of single CpG. From a mechanistic point of view, the methylation of cytosines in the normally unmethylated CpG island A can determine inhibitory cumulative effects on RASSF1A transcription due to the action of methyl-binding proteins. In experiments based on reporter constructs containing an artificial RASSF1A promoter with four groups of four CpGs at increasing distance from the transcription start site, two separated clusters of four consecutive methylated CpGs (not other combinations) determined a 63% decrease in promoter activity. Oct1 and Sp1 transcription factors bound preferentially to regulatory sequences overlapped to the regulatory CpGs when unmethylated [108]. Volodko et al. screened CpGs methylation and searched for correlation with RASSF1A transcription in various cancer types [109]. In colorectal cancer, seven CpGs hotspot in the RASSF1A promoter have been described to contribute to most of the DNA methylation. In breast and thyroid cancers, the methylation level of single CpGs mirrors the average value for the whole promoter. In normal breast tissue, RASSF1A exon 1 is found methylated without affecting gene expression [87], whereas matched breast cancers tissues show RASSF1A hypermethylation in both exon 1 and spreading towards the promoter region in association with the gene silencing.
In pancreatic endocrine tumors (PET), it has been demonstrated that a down-modulation of RASSF1A correlates with increased methylation of 51 CpG in the CpG island A and RASSF1C expression [67]. An expression switch between RASSF1A and RASSF1C concomitant to CpG island A hypermethylation has also been observed in breast cancer, neuroblastoma, some lung cancers [24,31], esophageal squamous cell carcinoma [110], renal cell carcinoma [111], breast, thyroid, and colorectal cancers [109], but not in pancreatic ductal adenocarcinoma [84]. RASSF1A is a Hippo pathway scaffold protein that subtracts YAP1 from oncogenic TEAD (TEA domain) transcriptional complexes and promotes tumor-suppressive YAP1/p73 activity [112]. RASSF1Am and alternated RASSF1A and RASSF1C expression correlates with loss of inhibitor signals mediated by YAP1, E-cadherin internalization and epithelial integrity is associated with an acquired invasive phenotype [113].
The alternated expression of distinct RASSF1 isoforms with opposing functions would explain the association between loss of RASSF1A expression and an adverse outcome and disease progression for certain cancer types, calling upon the need of more functional studies to better understand the functional consequence of this switch. Furthermore, these data suggest that cell type-specific factors to be discovered modulate the transcriptional silencing of RASSF1A supported by the cytosine methylation.
7. RASSF1A Methylation and Expression in Gastrointestinal Cancers
By considering the published RASSF1Am data in gastrointestinal cancer types, the overall frequency of RASSF1Am is 78% in hepatocellular carcinoma, 34.6% in hepatoblastoma, 50% in esophageal squamous cell carcinoma, 54% in pancreatic ductal adenocarcinoma, 75% in PET, 35.6% in CRC and 31% in gastric cancer (Table 1).
Table 1.
Frequency of RASSF1A methylation in gastrointestinal cancers *.
| Cancer Type | Methylation of RASSF1A |
|---|---|
| Hepatocellular carcinoma (HCC) | 522 of 669 (78%) HCC |
| Hepatoblastoma (HB) | 46 of 133 (34.6%) HB |
| Esophageal squamous cell carcinoma (ESCC) | 442 of 884 (50%) ESCC |
| Pancreatic ductal adenocarcinoma (PDAC) | 32 of 59 (54%) PDAC |
| Pancreatic endocrine tumor (PET) | 114 of 175 (75%) PET |
| Colorectal carcinoma (CRC) | 558 of 1567 (35.6%) CRC |
| Gastric cancer (GC) | 179 of 378 (31%) GC |
* see Tables S1 to S5 for experimental details and references.
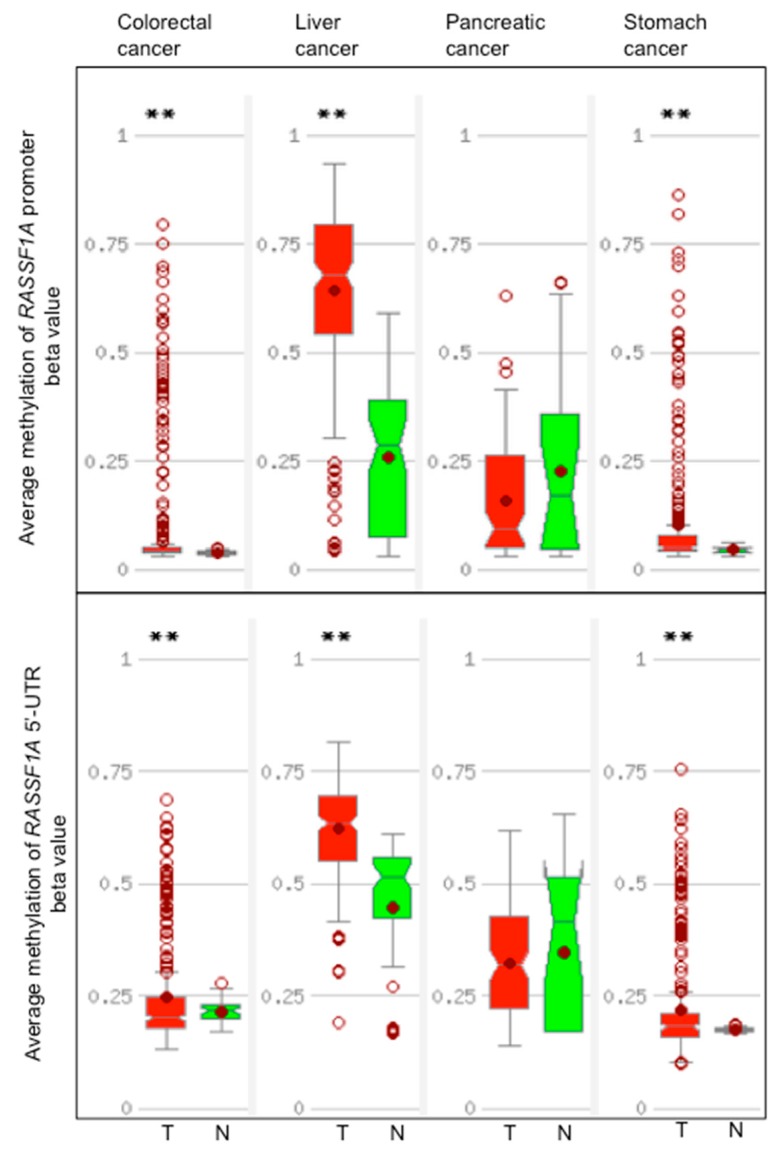
Data from TCGA show that RASSF1Am is detected at higher frequency as compared to normal tissues in liver, colorectal, and stomach cancers but not in pancreatic cancers (Figure 3).
Figure 3.
DNA methylation of the promoter and 5′-UTR of RASSF1A in colorectal, liver, pancreatic, and stomach cancers and in the corresponding normal tissues. Distribution of average methylation in the promoter and 5′-UTR of RASSF1A (NM_007182) in colorectal, liver, pancreatic, and stomach cancers cases. T, tumor tissues (red), N, normal tissue (green). 5′-UTR is the 5′ untranslated region of the first exon of RASSF1A. The promoter region is defined as from 1.5 kb upstream to 0.5 kb downstream of the RASSF1A transcription start site. The graphs show the distribution of beta values calculated as methylated probe intensity divided the unmethylated probe intensity plus methylated probe intensity, plus 100. In the boxes, a horizontal line represents the median and the filled circle the average; the box represents the 25th percentile interval and the whiskers the 95th percentile interval of the distribution. Empty points represent outliers. The double asterisk indicates a significant difference between T and N samples (p < 0.005) calculated by the t-test. The graphs, retrieved from the MethHC site [114], are based on The Cancer Genome Atlas (TCGA) data.
The RASSF1Am data extracted from the literature and TCGA are consistent for liver, but not for pancreatic, colorectal, and gastric cancers. For pancreatic cancer, 20% to 35% RASSF1Am shown by TCGA data is close to the 35% reported by Amato et al. [84]. In general, differences of RASSF1Am may depend from the assay types applied and assay location, as discussed earlier in this review. A detailed description of the results and methods applied for the detection RASSF1Am in five gastrointestinal cancer types and the corresponding normal tissues is reported in Tables S1 to S5. All TCGA data were obtained by Illumina platforms. However, most of RASSF1Am data described in published studies were obtained by methylation-specific PCR (MSP), a qualitative technique informative of one or few CpGs. MSP tends to overestimate the frequency of DNA methylation as even few methylated CpGs belonging to a small fractions of the genomes present in the sample will produce a positive signal [115]. Given these premises, a certain variability in the association between DNA methylation and expression of RASSF1A or between RASSF1Am and the patients’ clinico-pathological parameters is expected to be found.
RASSF1A hypermethylation is a common finding in all gastrointestinal cancer types often along with other tumor suppressor genes in a pattern that is typical of CpG island methylator phenotype (CIMP). CIMP is an epigenetic disorder, characterized by widespread and simultaneous hypermethylation of CpG islands, that differentiates distinct subsets of cancer patients [116]. Genome-scale analysis found CIMP state generally concordant between primary colorectal cancers (CRCs) and corresponding metastases [117]. RASSF1A is candidate gene of CIMP in colorectal cancers [118] (see Weisenberger et al. [119] for e review).
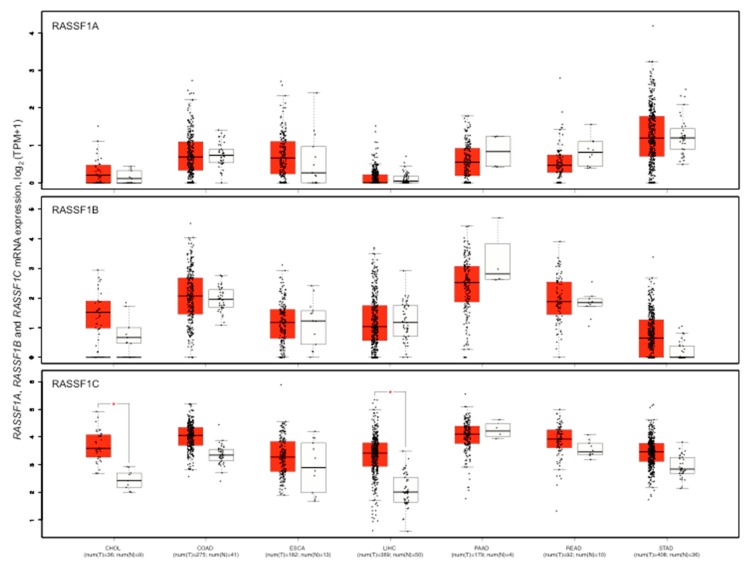
RASSF1 isoforms expression is variable in different gastrointestinal cancer types (Figure 4).
Figure 4.
mRNA level of RASSF1A, RASSF1B, RASSF1C in seven gastrointestinal cancer types and the corresponding normal tissues. Red box, cancer types; white box normal tissues. The box plots show the expression distribution of the RASSF1 isoforms RASSF1A, RASSF1B, and RASSF1C in the cancer types indicated in figure and the respective normal tissues. The expression levels of the samples are represented by black points. The expression data are log2 of Transcripts Per Million plus 1 (TPM+1) transformed for differential analysis and the log2 fold change defined as median of cancers minus median of normal tissues. Expression data of cancer and normal samples derived from the TCGA. Box plot represents the 25th percentile interval and whiskers represent the 95th percentile interval of the distribution. A horizontal line indicates the median value of the expressions. The number of samples for each series in cancers (T) and normal (N) is indicated below the acronym of cancer. CHOL, cholangiocarcinoma; COAD, colon adenocarcinoma; ESCA, esophageal carcinoma; LIHC, liver hepatocellular carcinoma; PAAD, pancreatic adenocarcinoma; READ, rectum adenocarcinoma; STAD, stomach adenocarcinoma. The asterisk indicates a significant difference of expression between a cancer type and the corresponding normal tissues (p < 0.01). Graphs were obtained from GEPIA2 at http://gepia2.cancer-pku.cn.
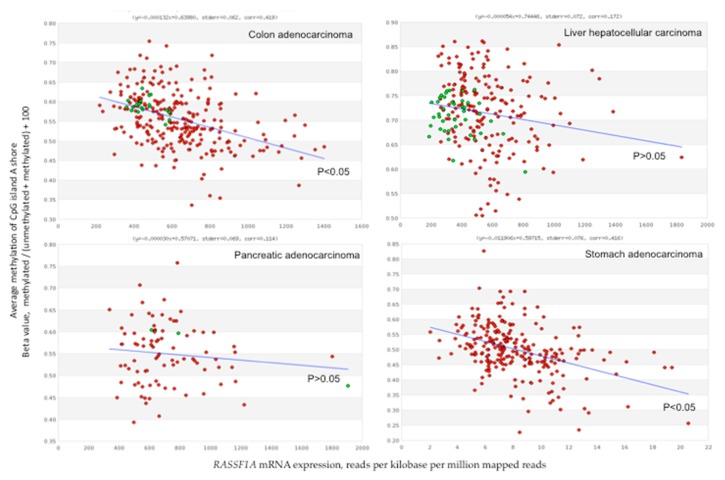
RASSF1A expression level is higher in stomach cancers and lower in liver cancers. RASSF1C level is, in general, higher than RASSF1A and RASSF1B level. RASSF1C expression is significantly higher in cancers than in normal tissues in cholangiocarcinoma and hepatocellular carcinoma (Figure 4). Certain studies have reported a robust correlation between 5mCs distribution and RASSF1A mRNA levels on one side, and methylation hotspots and transcription on the other. Concomitant RASSF1Am increase and gene expression loss has been reported in many studies regarding gastrointestinal cancers (Tables S1 to S5). However, TCGA data show no significant inverse correlation between promoter or 5′-UTR average DNA methylation and number of reads in colorectal, liver, pancreatic, and stomach cancers. High stringency is observed for methylation in the shore elements of the CpG island A in colorectal and stomach cancers (Figure 5).
Figure 5.
Average methylation of 15 CpGs in the CpG island A shore in function of the mRNA level of RASSF1A in colorectal, liver, pancreatic, and stomach cancers. Average methylation of cytosines in the CpG island A shore in function of the mRNA level (NM_007182) in colorectal, liver, pancreatic, and stomach cancers. RASSF1A mRNA expression represent the number of reads per kilobase per million mapped reads. CpG island A shore methylation correspond to the average methylation of 15 CpGs (chr3 from 50,378,611 to chr3:50,377,755, GRCh37/hg19). Red points, tumor tissues; green points, normal tissues. Blue line represents the trend line through the points. Parameters of the trend line, equation of the straight line, standard error, and correlation coefficient, are shown above graphs. A significant inverse correlation between CpG island A methylation and RASSF1A expression is found in colorectal and stomach cancers. The p-value of the trend line is indicated. The graphs, retrieved from the MethHC site [114], are based on The Cancer Genome Atlas (TCGA) data.
Flanking regions of CpG islands, referred to as CpG island shores, showed tissue-specific DNA hypermethylation and association with gene silencing in cancer [61,120]. Based on TCGA data, CpG island A shore methylation correlated inversely with RASSF1A mRNA levels in colon and stomach cancers, but not in liver and pancreatic cancers (Figure 5). An average methylation of the whole RASSF1A promoter region higher than 20% results in a reduced RASSF1A mRNA expression in various cancer cell lines, suggesting that it represents a critical threshold for efficient gene silencing [109]. At this degree of methylation, it is probable that in each genome some of the regulatory CpGs of a gene are methylated, thereby establishing an efficient contrast to the transcription initiation complex.
8. Conclusions and Perspectives
Multiple lines of evidence demonstrate that loss of RASSF1A promotes cell transformation and that epigenetic regulation by DNA methylation may be one of the responsible mechanisms in a wide variety of malignancies. RASSF1Am is a widespread event in gastrointestinal cancers and promises to serve as a valuable diagnostic/prognostic marker, making it possible to translate epigenomics into clinical relevant information [121].
A large body of experimental data underline the importance of a controlled and adequate supply of RASSF1A for correct functionality of cells, whereas it is questionable if the current knowledge about the DNA methylation pattern is sufficient to allow the exploitation of DNA methylation data as a biomarker. Single CpGs may carry out specialized functions, in particular if they rule over the binding of transcription factors acting as master tissue homeostasis regulators [62]. Our ability to resolve unique patterns of methylation in complex arrays of different tissues is still limited and the use of different, non-comparable, techniques for the detection of methylation and relative expression of RASSF1A has counteracted its power as a reliable tumor marker and this limitation therefore encourages to adopt more standardized methods.
Although DNA methylation data have long been considered a promising source of biomarkers for cancer diagnosis, prognosis, and prediction, there are a few successful examples that confirmed the previous findings and were applied to clinics [122]. Concerning RASSF1A, its methylation was used a marker in a panel for the early detection of the hepatocellular carcinoma [90]. RASSF1Am was applied to clinics as tissue biomarker only for prostate cancer [123].
It is believed that a biomarker based on DNA methylation does not necessarily have to be correlated with gene expression. However, a correlation DNA methylation-gene expression provides a biological rationale to support the clinical application as biomarker of the DNA methylation. Koch et al. have used TCGA data on prostate cancer to assess the correlation between DNA methylation and mRNA expression of RASSF1A [122]. They showed that different assays aimed at determining RASSF1Am result in contradictory outcomes and insufficiently effective discriminating power (positive or negative or no correlation between RASSF1A methylation and mRNA expression). Analogous conclusions have been obtained for the methylation of other genes, suggesting that finding a reliable assay location is needed [122]. The conclusions drawn by Koch et al. challenge the results of previous studies on RASSF1Am and solicit a revision of available methods and strategies so far applied [122]. Well-designed/informative high resolution and quantitative DNA methylation and mRNA/protein analyses are required.
The exact location of biologically and clinically relevant hypermethylation of RASSF1A, with reference to specific contexts and pathologies, is still unknown. In addition to the promoter region, attention should be paid at distal enhancers. An association between deregulated gene expression and CpGs methylation in cancer may result significantly stronger for distal enhancers than the promoters of many genes [124]. To our knowledge, the role of the methylation of distal enhancer sequences in the RASSF1A expression regulation has never been established.
In conclusion, we do not know precisely why methylation of cytosines rises at a spot, if it originates from a random process, and/or if it is acquired through selection. In addition, the inhibitory efficiency of 5mCs at a certain CpG site on gene transcription is not easily predictable. The relevance of 5mCs at specific CpG positions might regard the loss of binding of transcription factors and of communication between signaling pathways and the functions powered by RASSF1A. Future DNA methylation analyses should extend assay locations, provide the patterns of methylation in single or few genomes complemented by the effect on the binding of transcription factors, and the consequent transcriptional output [125]. The exploitation of this knowledge is of strategic importance for the correct interpretation of the consequences that methylation plays on cellular function and to achieve robust associations with clinical data.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/11/7/959/s1, Table S1: RASSF1A methylation in liver neoplasms, Table S2: RASSF1A methylation in esophageal squamous cell carcinoma, Table S3: RASSF1A methylation in pancreatic neoplasms, Table S4: RASSF1A methylation in colorectal cancer, Table S5: RASSF1A methylation in gastric cancers.
Author Contributions
G.M., G.I., R.P., and C.B. drew conceptual frameworks, searched the literature, and wrote the manuscript. I.D., M.B., A.H.N.K., revised the manuscript.
Funding
This work was funded by Associazione Italiana per la Ricerca sul Cancro (AIRC) IG17132.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Donninger H., Vos M.D., Clark G.J. The RASSF1A tumor suppressor. J. Cell Sci. 2007;120:3163–3172. doi: 10.1242/jcs.010389. [DOI] [PubMed] [Google Scholar]
- 2.Van der Weyden L., Adams D.J. The Ras-association domain family(RASSF) members and their role in human tumourigenesis. Biochim. Biophys. Acta. 2007;1776:58–85. doi: 10.1016/j.bbcan.2007.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang J.W., Hsu H.S., Ni H.J., Chuang C.T., Hsiung C.H., Huang T.H., Wang Y.C. Distinct epigenetic domains separated by a CTCF bound insulator between the tandem genes, BLU and RASSF1A. PLoS ONE. 2010;5:e12847. doi: 10.1371/journal.pone.0012847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hesson L., Bieche I., Krex D., Criniere E., Hoang-Xuan K., Maher E.R., Latif F. Frequent epigenetic inactivation of RASSF1A and BLU genes located within the critical 3p21.3 region in gliomas. Oncogene. 2004;23:2408–2419. doi: 10.1038/sj.onc.1207407. [DOI] [PubMed] [Google Scholar]
- 5.Senchenko V.N., Liu J., Loginov W., Bazov I., Angeloni D., Seryogin Y., Ermilova V., Kazubskaya T., Garkavtseva R., Zabarovska V.I., et al. Discovery of frequent homozygous deletions in chromosome 3p21.3 LUCA and AP20 regions in renal, lung and breast carcinomas. Oncogene. 2004;23:5719–5728. doi: 10.1038/sj.onc.1207760. [DOI] [PubMed] [Google Scholar]
- 6.Ito M., Ito G., Kondo M., Uchiyama M., Fukui T., Mori S., Yoshioka H., Ueda Y., Shimokata K., Sekido Y. Frequent inactivation of RASSF1A, BLU, and SEMA3B on 3p21.3 by promoter hypermethylation and allele loss in non-small cell lung cancer. Cancer Lett. 2005;225:131–139. doi: 10.1016/j.canlet.2004.10.041. [DOI] [PubMed] [Google Scholar]
- 7.Amato E., Barbi S., Malpeli G., Bersani S., Pelosi G., Capelli P., Scarpa A. Chromosome 3p alterations in pancreatic endocrine neoplasia. Virchows Arch. 2011;458:39–45. doi: 10.1007/s00428-010-1001-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hesson L.B., Cooper W.N., Latif F. The role of RASSF1A methylation in cancer. Dis. Mark. 2007;23:73–87. doi: 10.1155/2007/291538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vos M.D., Ellis C.A., Bell A., Birrer M.J., Clark G.J. Ras uses the novel tumor suppressor RASSF1 as an effector to mediate apoptosis. J. Biol. Chem. 2000;275:35669–35672. doi: 10.1074/jbc.C000463200. [DOI] [PubMed] [Google Scholar]
- 10.Dammann R., Li C., Yoon J.H., Chin P.L., Bates S., Pfeifer G.P. Epigenetic inactivation of a RAS association domain family protein from the lung tumour suppressor locus 3p21.3. Nat. Genet. 2000;25:315–319. doi: 10.1038/77083. [DOI] [PubMed] [Google Scholar]
- 11.Baksh S., Tommasi S., Fenton S., Yu V.C., Martins L.M., Pfeifer G.P., Latif F., Downward J., Neel B.G. The tumor suppressor RASSF1A and MAP-1 link death receptor signaling to Bax conformational change and cell death. Mol. Cell. 2005;18:637–650. doi: 10.1016/j.molcel.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Pefani D.E., O’Neill E. Safeguarding genome stability: RASSF1A tumor suppressor regulates BRCA2 at stalled forks. Cell Cycle. 2015;14:1624–1630. doi: 10.1080/15384101.2015.1035845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song M.S., Song S.J., Ayad N.G., Chang J.S., Lee J.H., Hong H.K., Lee H., Choi N., Kim J., Kim H., et al. The tumour suppressor RASSF1A regulates mitosis by inhibiting the APC-Cdc20 complex. Nat. Cell Biol. 2004;6:129–137. doi: 10.1038/ncb1091. [DOI] [PubMed] [Google Scholar]
- 14.Dittfeld C., Richter A.M., Steinmann K., Klagge-Ulonska A., Dammann R.H. The SARAH Domain of RASSF1A and Its Tumor Suppressor Function. Mol. Biol. Int. 2012;2012:196715. doi: 10.1155/2012/196715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu L., Tommasi S., Lee D.H., Dammann R., Pfeifer G.P. Control of microtubule stability by the RASSF1A tumor suppressor. Oncogene. 2003;22:8125–8136. doi: 10.1038/sj.onc.1206984. [DOI] [PubMed] [Google Scholar]
- 16.Fausti F., Di Agostino S., Sacconi A., Strano S., Blandino G. Hippo and rassf1a Pathways: A Growing Affair. Mol. Biol. Int. 2012;2012:307628. doi: 10.1155/2012/307628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foley C.J., Freedman H., Choo S.L., Onyskiw C., Fu N.Y., Yu V.C., Tuszynski J., Pratt J.C., Baksh S. Dynamics of RASSF1A/MOAP-1 association with death receptors. Mol. Cell. Biol. 2008;28:4520–4535. doi: 10.1128/MCB.02011-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Law J., Salla M., Zare A., Wong Y., Luong L., Volodko N., Svystun O., Flood K., Lim J., Sung M., et al. Modulator of apoptosis 1(MOAP-1) is a tumor suppressor protein linked to the RASSF1A protein. J. Biol. Chem. 2015;290:24100–24118. doi: 10.1074/jbc.M115.648345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papaspyropoulos A., Bradley L., Thapa A., Leung C.Y., Toskas K., Koennig D., Pefani D.E., Raso C., Grou C., Hamilton G., et al. RASSF1A uncouples Wnt from Hippo signalling and promotes YAP mediated differentiation via p73. Nat. Commun. 2018;9:424. doi: 10.1038/s41467-017-02786-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tommasi S., Dammann R., Zhang Z., Wang Y., Liu L., Tsark W.M., Wilczynski S.P., Li J., You M., Pfeifer G.P. Tumor susceptibility of Rassf1a knockout mice. Cancer Res. 2005;65:92–98. [PubMed] [Google Scholar]
- 21.Wang W.G., Chen S.J., He J.S., Li J.S., Zang X.F. The tumor suppressive role of RASSF1A in osteosarcoma through the Wnt signaling pathway. Tumour Biol. 2016;37:8869–8877. doi: 10.1007/s13277-015-4660-z. [DOI] [PubMed] [Google Scholar]
- 22.Zhang X., Guo C., Wu X., Li A.X., Liu L., Tsark W., Dammann R., Shen H., Vonderfecht S.L., Pfeifer G.P. Analysis of liver tumor-prone mouse models of the hippo kinase scaffold proteins RASSF1A and SAV1. Cancer Res. 2016;76:2824–2835. doi: 10.1158/0008-5472.CAN-15-3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Teng I.W., Hou P.C., Lee K.D., Chu P.Y., Yeh K.T., Jin V.X., Tseng M.J., Tsai S.J., Chang Y.S., Wu C.S., et al. Targeted methylation of two tumor suppressor genes is sufficient to transform mesenchymal stem cells into cancer stem/initiating cells. Cancer Res. 2011;71:4653–4663. doi: 10.1158/0008-5472.CAN-10-3418. [DOI] [PubMed] [Google Scholar]
- 24.Reeves M.E., Firek M., Chen S.T., Amaar Y. The RASSF1 Gene and the Opposing Effects of the RASSF1A and RASSF1C Isoforms on Cell Proliferation and Apoptosis. Mol. Biol. Int. 2013;2013:145096. doi: 10.1155/2013/145096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agathanggelou A., Bieche I., Ahmed-Choudhury J., Nicke B., Dammann R., Baksh S., Gao B., Minna J.D., Downward J., Maher E.R., et al. Identification of novel gene expression targets for the Ras association domain family 1(RASSF1A) tumor suppressor gene in non-small cell lung cancer and neuroblastoma. Cancer Res. 2003;63:5344–5351. [PMC free article] [PubMed] [Google Scholar]
- 26.Dallol A., Agathanggelou A., Tommasi S., Pfeifer G.P., Maher E.R., Latif F. Involvement of the RASSF1A tumor suppressor gene in controlling cell migration. Cancer Res. 2005;65:7653–7659. doi: 10.1158/0008-5472.CAN-05-0247. [DOI] [PubMed] [Google Scholar]
- 27.Dreijerink K., Braga E., Kuzmin I., Geil L., Duh F.M., Angeloni D., Zbar B., Lerman M.I., Stanbridge E.J., Minna J.D., et al. The candidate tumor suppressor gene, RASSF1A, from human chromosome 3p21.3 is involved in kidney tumorigenesis. Proc. Natl. Acad. Sci. USA. 2001;98:7504–7509. doi: 10.1073/pnas.131216298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reu F.J., Leaman D.W., Maitra R.R., Bae S.I., Cherkassky L., Fox M.W., Rempinski D.R., Beaulieu N., MacLeod A.R., Borden E.C. Expression of RASSF1A, an epigenetically silenced tumor suppressor, overcomes resistance to apoptosis induction by interferons. Cancer Res. 2006;66:2785–2793. doi: 10.1158/0008-5472.CAN-05-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xue W.J., Li C., Zhou X.J., Guan H.G., Qin L., Li P., Wang Z.W., Qian H.X. RASSF1A expression inhibits the growth of hepatocellular carcinoma from Qidong County. J. Gastroenterol. Hepatol. 2008;23:1448–1458. doi: 10.1111/j.1440-1746.2007.05067.x. [DOI] [PubMed] [Google Scholar]
- 30.Zhou P.H., Zheng J.B., Wei G.B., Wang X.L., Wang W., Chen N.Z., Yu J.H., Yao J.F., Wang H., Lu S.Y., et al. Lentivirus-mediated RASSF1A expression suppresses aggressive phenotypes of gastric cancer cells in vitro and in vivo. Gene Ther. 2015;22:793–801. doi: 10.1038/gt.2015.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pelosi G., Fumagalli C., Trubia M., Sonzogni A., Rekhtman N., Maisonneuve P., Galetta D., Spaggiari L., Veronesi G., Scarpa A., et al. Dual role of RASSF1 as a tumor suppressor and an oncogene in neuroendocrine tumors of the lung. Anticancer Res. 2010;30:4269–4281. [PubMed] [Google Scholar]
- 32.Rong R., Jin W., Zhang J., Sheikh M.S., Huang Y. Tumor suppressor RASSF1A is a microtubule-binding protein that stabilizes microtubules and induces G2/M arrest. Oncogene. 2004;23:8216–8230. doi: 10.1038/sj.onc.1207901. [DOI] [PubMed] [Google Scholar]
- 33.Vos M.D., Martinez A., Elam C., Dallol A., Taylor B.J., Latif F., Clark G.J. A role for the RASSF1A tumor suppressor in the regulation of tubulin polymerization and genomic stability. Cancer Res. 2004;64:4244–4250. doi: 10.1158/0008-5472.CAN-04-0339. [DOI] [PubMed] [Google Scholar]
- 34.Kitagawa D., Kajiho H., Negishi T., Ura S., Watanabe T., Wada T., Ichijo H., Katada T., Nishina H. Release of RASSF1C from the nucleus by Daxx degradation links DNA damage and SAPK/JNK activation. EMBO J. 2006;25:3286–3297. doi: 10.1038/sj.emboj.7601212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li J., Wang F., Protopopov A., Malyukova A., Kashuba V., Minna J.D., Lerman M.I., Klein G., Zabarovsky E. Inactivation of RASSF1C during in vivo tumor growth identifies it as a tumor suppressor gene. Oncogene. 2004;23:5941–5949. doi: 10.1038/sj.onc.1207789. [DOI] [PubMed] [Google Scholar]
- 36.Estrabaud E., Lassot I., Blot G., Le Rouzic E., Tanchou V., Quemeneur E., Daviet L., Margottin-Goguet F., Benarous R. RASSF1C, an isoform of the tumor suppressor RASSF1A, promotes the accumulation of beta-catenin by interacting with betaTrCP. Cancer Res. 2007;67:1054–1061. doi: 10.1158/0008-5472.CAN-06-2530. [DOI] [PubMed] [Google Scholar]
- 37.Amaar Y.G., Minera M.G., Hatran L.K., Strong D.D., Mohan S., Reeves M.E. Ras association domain family 1C protein stimulates human lung cancer cell proliferation. Am. J. Physiol. Lung Cell. Mol. Physiol. 2006;291:L1185–L1190. doi: 10.1152/ajplung.00072.2006. [DOI] [PubMed] [Google Scholar]
- 38.Reeves M.E., Firek M., Chen S.T., Amaar Y.G. Evidence that RASSF1C stimulation of lung cancer cell proliferation depends on IGFBP-5 and PIWIL1 expression levels. PLoS ONE. 2014;9:e101679. doi: 10.1371/journal.pone.0101679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bestor T.H. The DNA methyltransferases of mammals. Hum. Mol. Genet. 2000;9:2395–2402. doi: 10.1093/hmg/9.16.2395. [DOI] [PubMed] [Google Scholar]
- 40.Esteve P.O., Chang Y., Samaranayake M., Upadhyay A.K., Horton J.R., Feehery G.R., Cheng X., Pradhan S. A methylation and phosphorylation switch between an adjacent lysine and serine determines human DNMT1 stability. Nat. Struct. Mol. Biol. 2011;18:42–48. doi: 10.1038/nsmb.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sun L., Zhao H., Xu Z., Liu Q., Liang Y., Wang L., Cai X., Zhang L., Hu L., Wang G., et al. Phosphatidylinositol 3-kinase/protein kinase B pathway stabilizes DNA methyltransferase I protein and maintains DNA methylation. Cell. Signal. 2007;19:2255–2263. doi: 10.1016/j.cellsig.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 42.Lyko F. The DNA methyltransferase family: A versatile toolkit for epigenetic regulation. Nat. Rev. Genet. 2018;19:81–92. doi: 10.1038/nrg.2017.80. [DOI] [PubMed] [Google Scholar]
- 43.Okano M., Bell D.W., Haber D.A., Li E. DNA methyltransferases Dnmt3a and Dnmt3b are essential for de novo methylation and mammalian development. Cell. 1999;99:247–257. doi: 10.1016/S0092-8674(00)81656-6. [DOI] [PubMed] [Google Scholar]
- 44.Koivunen P., Laukka T. The TET enzymes. Cell. Mol. Life Sci. 2018;75:1339–1348. doi: 10.1007/s00018-017-2721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhattacharyya S., Pradhan K., Campbell N., Mazdo J., Vasantkumar A., Maqbool S., Bhagat T.D., Gupta S., Suzuki M., Yu Y., et al. Altered hydroxymethylation is seen at regulatory regions in pancreatic cancer and regulates oncogenic pathways. Genome Res. 2017;27:1830–1842. doi: 10.1101/gr.222794.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Du C., Kurabe N., Matsushima Y., Suzuki M., Kahyo T., Ohnishi I., Tanioka F., Tajima S., Goto M., Yamada H., et al. Robust quantitative assessments of cytosine modifications and changes in the expressions of related enzymes in gastric cancer. Gastric Cancer. 2015;18:516–525. doi: 10.1007/s10120-014-0409-4. [DOI] [PubMed] [Google Scholar]
- 47.Ma L., Qi T., Wang S., Hao M., Sakhawat A., Liang T., Zhang L., Cong X., Huang Y. Tet methylcytosine dioxygenase 1 promotes hypoxic gene induction and cell migration in colon cancer. J. Cell. Physiol. 2019;234:6286–6297. doi: 10.1002/jcp.27359. [DOI] [PubMed] [Google Scholar]
- 48.Murata A., Baba Y., Ishimoto T., Miyake K., Kosumi K., Harada K., Kurashige J., Iwagami S., Sakamoto Y., Miyamoto Y., et al. TET family proteins and 5-hydroxymethylcytosine in esophageal squamous cell carcinoma. Oncotarget. 2015;6:23372–23382. doi: 10.18632/oncotarget.4281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sajadian S.O., Ehnert S., Vakilian H., Koutsouraki E., Damm G., Seehofer D., Thasler W., Dooley S., Baharvand H., Sipos B., et al. Induction of active demethylation and 5hmC formation by 5-azacytidine is TET2 dependent and suggests new treatment strategies against hepatocellular carcinoma. Clin. Epigenetics. 2015;7:98. doi: 10.1186/s13148-015-0133-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tian Y., Pan F., Sun X., Gan M., Lin A., Zhang D., Zhu Y., Lai M. Association of TET1 expression with colorectal cancer progression. Scand. J. Gastroenterol. 2017;52:312–320. doi: 10.1080/00365521.2016.1253767. [DOI] [PubMed] [Google Scholar]
- 51.Wang K.C., Kang C.H., Tsai C.Y., Chou N.H., Tu Y.T., Li G.C., Lam H.C., Liu S.I., Chang P.M., Lin Y.H., et al. Ten-eleven translocation 1 dysfunction reduces 5-hydroxymethylcytosine expression levels in gastric cancer cells. Oncol. Lett. 2018;15:278–284. doi: 10.3892/ol.2017.7264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ambrosi C., Manzo M., Baubec T. Dynamics and Context-Dependent Roles of DNA Methylation. J. Mol. Biol. 2017;429:1459–1475. doi: 10.1016/j.jmb.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 53.Bai J., Zhang X., Hu K., Liu B., Wang H., Li A., Lin F., Zhang L., Sun X., Du Z., et al. Silencing DNA methyltransferase 1(DNMT1) inhibits proliferation, metastasis and invasion in ESCC by suppressing methylation of RASSF1A and DAPK. Oncotarget. 2016;7:44129–44141. doi: 10.18632/oncotarget.9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gjoneska E., Pfenning A.R., Mathys H., Quon G., Kundaje A., Tsai L.H., Kellis M. Conserved epigenomic signals in mice and humans reveal immune basis of Alzheimer’s disease. Nature. 2015;518:365–369. doi: 10.1038/nature14252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang J., Bhutani M., Pathak A.K., Lang W., Ren H., Jelinek J., He R., Shen L., Issa J.P., Mao L. Delta DNMT3B variants regulate DNA methylation in a promoter-specific manner. Cancer Res. 2007;67:10647–10652. doi: 10.1158/0008-5472.CAN-07-1337. [DOI] [PubMed] [Google Scholar]
- 56.Wang X.Z., Cheng Y., Wang K.L., Liu R., Yang X.L., Wen H.M., Chai C., Liang J.Y., Wu H. Peperomin E reactivates silenced tumor suppressor genes in lung cancer cells by inhibition of DNA methyltransferase. Cancer Sci. 2016;107:1506–1519. doi: 10.1111/cas.13029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Palakurthy R.K., Wajapeyee N., Santra M.K., Gazin C., Lin L., Gobeil S., Green M.R. Epigenetic silencing of the RASSF1A tumor suppressor gene through HOXB3-mediated induction of DNMT3B expression. Mol. Cell. 2009;36:219–230. doi: 10.1016/j.molcel.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li H., Rauch T., Chen Z.X., Szabo P.E., Riggs A.D., Pfeifer G.P. The histone methyltransferase SETDB1 and the DNA methyltransferase DNMT3A interact directly and localize to promoters silenced in cancer cells. J. Biol. Chem. 2006;281:19489–19500. doi: 10.1074/jbc.M513249200. [DOI] [PubMed] [Google Scholar]
- 59.Strunnikova M., Schagdarsurengin U., Kehlen A., Garbe J.C., Stampfer M.R., Dammann R. Chromatin inactivation precedes de novo DNA methylation during the progressive epigenetic silencing of the RASSF1A promoter. Mol. Cell. Biol. 2005;25:3923–3933. doi: 10.1128/MCB.25.10.3923-3933.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boyes J., Bird A. DNA methylation inhibits transcription indirectly via a methyl-CpG binding protein. Cell. 1991;64:1123–1134. doi: 10.1016/0092-8674(91)90267-3. [DOI] [PubMed] [Google Scholar]
- 61.Stirzaker C., Song J.Z., Ng W., Du Q., Armstrong N.J., Locke W.J., Statham A.L., French H., Pidsley R., Valdes-Mora F., et al. Methyl-CpG-binding protein MBD2 plays a key role in maintenance and spread of DNA methylation at CpG islands and shores in cancer. Oncogene. 2017;36:1328–1338. doi: 10.1038/onc.2016.297. [DOI] [PubMed] [Google Scholar]
- 62.Medvedeva Y.A., Khamis A.M., Kulakovskiy I.V., Ba-Alawi W., Bhuyan M.S., Kawaji H., Lassmann T., Harbers M., Forrest A.R., Bajic V.B., et al. Effects of cytosine methylation on transcription factor binding sites. BMC Genom. 2014;15:119. doi: 10.1186/1471-2164-15-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee D.S., Shin J.Y., Tonge P.D., Puri M.C., Lee S., Park H., Lee W.C., Hussein S.M., Bleazard T., Yun J.Y., et al. An epigenomic roadmap to induced pluripotency reveals DNA methylation as a reprogramming modulator. Nat. Commun. 2014;5:5619. doi: 10.1038/ncomms6619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lister R., Pelizzola M., Dowen R.H., Hawkins R.D., Hon G., Tonti-Filippini J., Nery J.R., Lee L., Ye Z., Ngo Q.M., et al. Human DNA methylomes at base resolution show widespread epigenomic differences. Nature. 2009;462:315–322. doi: 10.1038/nature08514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khavari D.A., Sen G.L., Rinn J.L. DNA methylation and epigenetic control of cellular differentiation. Cell Cycle. 2010;9:3880–3883. doi: 10.4161/cc.9.19.13385. [DOI] [PubMed] [Google Scholar]
- 66.Du Q., Luu P.L., Stirzaker C., Clark S.J. Methyl-CpG-binding domain proteins: Readers of the epigenome. Epigenomics. 2015;7:1051–1073. doi: 10.2217/epi.15.39. [DOI] [PubMed] [Google Scholar]
- 67.Malpeli G., Amato E., Dandrea M., Fumagalli C., Debattisti V., Boninsegna L., Pelosi G., Falconi M., Scarpa A. Methylation-associated down-regulation of RASSF1A and up-regulation of RASSF1C in pancreatic endocrine tumors. BMC Cancer. 2011;11:351. doi: 10.1186/1471-2407-11-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Byun D.S., Lee M.G., Chae K.S., Ryu B.G., Chi S.G. Frequent epigenetic inactivation of RASSF1A by aberrant promoter hypermethylation in human gastric adenocarcinoma. Cancer Res. 2001;61:7034–7038. [PubMed] [Google Scholar]
- 69.Roadmap Epigenomics C., Kundaje A., Meuleman W., Ernst J., Bilenky M., Yen A., Heravi-Moussavi A., Kheradpour P., Zhang Z., Wang J., et al. Integrative analysis of 111 reference human epigenomes. Nature. 2015;518:317–330. doi: 10.1038/nature14248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rauch T., Wang Z., Zhang X., Zhong X., Wu X., Lau S.K., Kernstine K.H., Riggs A.D., Pfeifer G.P. Homeobox gene methylation in lung cancer studied by genome-wide analysis with a microarray-based methylated CpG island recovery assay. Proc. Natl. Acad. Sci. USA. 2007;104:5527–5532. doi: 10.1073/pnas.0701059104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schlesinger Y., Straussman R., Keshet I., Farkash S., Hecht M., Zimmerman J., Eden E., Yakhini Z., Ben-Shushan E., Reubinoff B.E., et al. Polycomb-mediated methylation on Lys27 of histone H3 pre-marks genes for de novo methylation in cancer. Nat. Genet. 2007;39:232–236. doi: 10.1038/ng1950. [DOI] [PubMed] [Google Scholar]
- 72.Fraga M.F., Esteller M. Epigenetics and aging: The targets and the marks. Trends Genet. 2007;23:413–418. doi: 10.1016/j.tig.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 73.Nejman D., Straussman R., Steinfeld I., Ruvolo M., Roberts D., Yakhini Z., Cedar H. Molecular rules governing de novo methylation in cancer. Cancer Res. 2014;74:1475–1483. doi: 10.1158/0008-5472.CAN-13-3042. [DOI] [PubMed] [Google Scholar]
- 74.Kuzmina N.S., Lapteva N., Rubanovich A.V. Hypermethylation of gene promoters in peripheral blood leukocytes in humans long term after radiation exposure. Environ. Res. 2016;146:10–17. doi: 10.1016/j.envres.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 75.Waki T., Tamura G., Sato M., Motoyama T. Age-related methylation of tumor suppressor and tumor-related genes: An analysis of autopsy samples. Oncogene. 2003;22:4128–4133. doi: 10.1038/sj.onc.1206651. [DOI] [PubMed] [Google Scholar]
- 76.Baylin S.B., Jones P.A. A decade of exploring the cancer epigenome—Biological and translational implications. Nat. Rev. Cancer. 2011;11:726–734. doi: 10.1038/nrc3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Klutstein M., Nejman D., Greenfield R., Cedar H. DNA Methylation in Cancer and Aging. Cancer Res. 2016;76:3446–3450. doi: 10.1158/0008-5472.CAN-15-3278. [DOI] [PubMed] [Google Scholar]
- 78.Wong I.H., Chan J., Wong J., Tam P.K. Ubiquitous aberrant RASSF1A promoter methylation in childhood neoplasia. Clin. Cancer Res. 2004;10:994–1002. doi: 10.1158/1078-0432.CCR-0378-3. [DOI] [PubMed] [Google Scholar]
- 79.Bird A. DNA methylation patterns and epigenetic memory. Genes Dev. 2002;16:6–21. doi: 10.1101/gad.947102. [DOI] [PubMed] [Google Scholar]
- 80.Weber M., Hellmann I., Stadler M.B., Ramos L., Paabo S., Rebhan M., Schubeler D. Distribution, silencing potential and evolutionary impact of promoter DNA methylation in the human genome. Nat. Genet. 2007;39:457–466. doi: 10.1038/ng1990. [DOI] [PubMed] [Google Scholar]
- 81.Christensen B.C., Houseman E.A., Marsit C.J., Zheng S., Wrensch M.R., Wiemels J.L., Nelson H.H., Karagas M.R., Padbury J.F., Bueno R., et al. Aging and environmental exposures alter tissue-specific DNA methylation dependent upon CpG island context. PLoS Genet. 2009;5:e1000602. doi: 10.1371/journal.pgen.1000602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Issa J.P., Ahuja N., Toyota M., Bronner M.P., Brentnall T.A. Accelerated age-related CpG island methylation in ulcerative colitis. Cancer Res. 2001;61:3573–3577. [PubMed] [Google Scholar]
- 83.Agathanggelou A., Cooper W.N., Latif F. Role of the Ras-association domain family 1 tumor suppressor gene in human cancers. Cancer Res. 2005;65:3497–3508. doi: 10.1158/0008-5472.CAN-04-4088. [DOI] [PubMed] [Google Scholar]
- 84.Amato E., Barbi S., Fassan M., Luchini C., Vicentini C., Brunelli M., Malleo G., Scarpa A., Malpeli G. RASSF1 tumor suppressor gene in pancreatic ductal adenocarcinoma: Correlation of expression, chromosomal status and epigenetic changes. BMC Cancer. 2016;16:11. doi: 10.1186/s12885-016-2048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Malpeli G. Potential etiologic of the epigenetic field defect in the diseases and in cancer. Edorium J. Pathol. 2015;2:10–13. [Google Scholar]
- 86.Peters I., Rehmet K., Wilke N., Kuczyk M.A., Hennenlotter J., Eilers T., Machtens S., Jonas U., Serth J. RASSF1A promoter methylation and expression analysis in normal and neoplastic kidney indicates a role in early tumorigenesis. Mol. Cancer. 2007;6:49. doi: 10.1186/1476-4598-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yan P.S., Shi H., Rahmatpanah F., Hsiau T.H., Hsiau A.H., Leu Y.W., Liu J.C., Huang T.H. Differential distribution of DNA methylation within the RASSF1A CpG island in breast cancer. Cancer Res. 2003;63:6178–6186. [PubMed] [Google Scholar]
- 88.Lo K.W., Kwong J., Hui A.B., Chan S.Y., To K.F., Chan A.S., Chow L.S., Teo P.M., Johnson P.J., Huang D.P. High frequency of promoter hypermethylation of RASSF1A in nasopharyngeal carcinoma. Cancer Res. 2001;61:3877–3881. [PubMed] [Google Scholar]
- 89.Lee M.G., Kim H.Y., Byun D.S., Lee S.J., Lee C.H., Kim J.I., Chang S.G., Chi S.G. Frequent epigenetic inactivation of RASSF1A in human bladder carcinoma. Cancer Res. 2001;61:6688–6692. [PubMed] [Google Scholar]
- 90.Jain S., Xie L., Boldbaatar B., Lin S.Y., Hamilton J.P., Meltzer S.J., Chen S.H., Hu C.T., Block T.M., Song W., et al. Differential methylation of the promoter and first exon of the RASSF1A gene in hepatocarcinogenesis. Hepatol. Res. 2015;45:1110–1123. doi: 10.1111/hepr.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gordon M., El-Kalla M., Zhao Y., Fiteih Y., Law J., Volodko N., Anwar-Mohamed A., El-Kadi A.O., Liu L., Odenbach J., et al. The tumor suppressor gene, RASSF1A, is essential for protection against inflammation -induced injury. PLoS ONE. 2013;8:e75483. doi: 10.1371/journal.pone.0075483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Guarasci F., D’Aquila P., Mandala M., Garasto S., Lattanzio F., Corsonello A., Passarino G., Bellizzi D. Aging and nutrition induce tissue-specific changes on global DNA methylation status in rats. Mech. Ageing Dev. 2018;174:47–54. doi: 10.1016/j.mad.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 93.Zekri A.R., Bahnasy A.A., Shoeab F.E., Mohamed W.S., El-Dahshan D.H., Ali F.T., Sabry G.M., Dasgupta N., Daoud S.S. Methylation of multiple genes in hepatitis C virus associated hepatocellular carcinoma. J. Adv. Res. 2014;5:27–40. doi: 10.1016/j.jare.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Saunderson E.A., Stepper P., Gomm J.J., Hoa L., Morgan A., Allen M.D., Jones J.L., Gribben J.G., Jurkowski T.P., Ficz G. Hit-and-run epigenetic editing prevents senescence entry in primary breast cells from healthy donors. Nat. Commun. 2017;8:1450. doi: 10.1038/s41467-017-01078-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Guo N., Chen R., Li Z., Liu Y., Cheng D., Zhou Q., Zhou J., Lin Q. Hepatitis C virus core upregulates the methylation status of the RASSF1A promoter through regulation of SMYD3 in hilar cholangiocarcinoma cells. Acta Biochim. Biophys. Sin. 2011;43:354–361. doi: 10.1093/abbs/gmr021. [DOI] [PubMed] [Google Scholar]
- 96.Kader F., Ghai M. DNA methylation-based variation between human populations. Mol. Genet. Genom. 2017;292:5–35. doi: 10.1007/s00438-016-1264-2. [DOI] [PubMed] [Google Scholar]
- 97.Shimizu K., Onishi M., Sugata E., Sokuza Y., Mori C., Nishikawa T., Honoki K., Tsujiuchi T. Disturbance of DNA methylation patterns in the early phase of hepatocarcinogenesis induced by a choline-deficient L-amino acid-defined diet in rats. Cancer Sci. 2007;98:1318–1322. doi: 10.1111/j.1349-7006.2007.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Starlard-Davenport A., Tryndyak V.P., James S.R., Karpf A.R., Latendresse J.R., Beland F.A., Pogribny I.P. Mechanisms of epigenetic silencing of the Rassf1a gene during estrogen-induced breast carcinogenesis in ACI rats. Carcinogenesis. 2010;31:376–381. doi: 10.1093/carcin/bgp304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rauscher G.H., Kresovich J.K., Poulin M., Yan L., Macias V., Mahmoud A.M., Al-Alem U., Kajdacsy-Balla A., Wiley E.L., Tonetti D., et al. Exploring DNA methylation changes in promoter, intragenic, and intergenic regions as early and late events in breast cancer formation. BMC Cancer. 2015;15:816. doi: 10.1186/s12885-015-1777-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Spitzwieser M., Holzweber E., Pfeiler G., Hacker S., Cichna-Markl M. Applicability of HIN-1, MGMT and RASSF1A promoter methylation as biomarkers for detecting field cancerization in breast cancer. Breast Cancer Res. 2015;17:125. doi: 10.1186/s13058-015-0637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhou V.W., Goren A., Bernstein B.E. Charting histone modifications and the functional organization of mammalian genomes. Nat. Rev. Genet. 2011;12:7–18. doi: 10.1038/nrg2905. [DOI] [PubMed] [Google Scholar]
- 102.Anastasiadi D., Esteve-Codina A., Piferrer F. Consistent inverse correlation between DNA methylation of the first intron and gene expression across tissues and species. Epigenetics Chromatin. 2018;11:37. doi: 10.1186/s13072-018-0205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dammann R., Takahashi T., Pfeifer G.P. The CpG island of the novel tumor suppressor gene RASSF1A is intensely methylated in primary small cell lung carcinomas. Oncogene. 2001;20:3563–3567. doi: 10.1038/sj.onc.1204469. [DOI] [PubMed] [Google Scholar]
- 104.Dammann R., Yang G., Pfeifer G.P. Hypermethylation of the cpG island of Ras association domain family 1A(RASSF1A), a putative tumor suppressor gene from the 3p21.3 locus, occurs in a large percentage of human breast cancers. Cancer Res. 2001;61:3105–3109. [PubMed] [Google Scholar]
- 105.Freitas M., Ferreira F., Carvalho S., Silva F., Lopes P., Antunes L., Salta S., Diniz F., Santos L.L., Videira J.F., et al. A novel DNA methylation panel accurately detects colorectal cancer independently of molecular pathway. J. Transl. Med. 2018;16:45. doi: 10.1186/s12967-018-1415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ge Y.Z., Xu L.W., Jia R.P., Xu Z., Feng Y.M., Wu R., Yu P., Zhao Y., Gui Z.L., Tan S.J., et al. The association between RASSF1A promoter methylation and prostate cancer: Evidence from 19 published studies. Tumour Biol. 2014;35:3881–3890. doi: 10.1007/s13277-013-1515-3. [DOI] [PubMed] [Google Scholar]
- 107.Zhan L., Zhang B., Tan Y., Yang C., Huang C., Wu Q., Zhang Y., Chen X., Zhou M., Shu A. Quantitative assessment of the relationship between RASSF1A gene promoter methylation and bladder cancer(PRISMA) Medicine. 2017;96:e6097. doi: 10.1097/MD.0000000000006097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Han W., Shi M., Spivack S.D. Site-specific methylated reporter constructs for functional analysis of DNA methylation. Epigenetics. 2013;8:1176–1187. doi: 10.4161/epi.26195. [DOI] [PubMed] [Google Scholar]
- 109.Volodko N., Salla M., Zare A., Abulghasem el A., Vincent K., Benesch M.G., McMullen T.P., Bathe O.F., Postovit L., Baksh S. RASSF1A Site-Specific Methylation Hotspots in Cancer and Correlation with RASSF1C and MOAP-1. Cancers. 2016;8:55. doi: 10.3390/cancers8060055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Guo W., Cui L., Wang C., Guo Y., Shen S., Kuang G., Dong Z. Decreased expression of RASSF1A and up-regulation of RASSF1C is associated with esophageal squamous cell carcinoma. Clin. Exp. Metastasis. 2014;31:521–533. doi: 10.1007/s10585-014-9646-5. [DOI] [PubMed] [Google Scholar]
- 111.Klacz J., Wierzbicki P.M., Wronska A., Rybarczyk A., Stanislawowski M., Slebioda T., Olejniczak A., Matuszewski M., Kmiec Z. Decreased expression of RASSF1A tumor suppressor gene is associated with worse prognosis in clear cell renal cell carcinoma. Int. J. Oncol. 2016;48:55–66. doi: 10.3892/ijo.2015.3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Van der Weyden L., Papaspyropoulos A., Poulogiannis G., Rust A.G., Rashid M., Adams D.J., Arends M.J., O’Neill E. Loss of RASSF1A synergizes with deregulated RUNX2 signaling in tumorigenesis. Cancer Res. 2012;72:3817–3827. doi: 10.1158/0008-5472.CAN-11-3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vlahov N., Scrace S., Soto M.S., Grawenda A.M., Bradley L., Pankova D., Papaspyropoulos A., Yee K.S., Buffa F., Goding C.R., et al. Alternate RASSF1 Transcripts Control SRC Activity, E-Cadherin Contacts, and YAP-Mediated Invasion. Curr. Biol. 2015;25:3019–3034. doi: 10.1016/j.cub.2015.09.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Huang W.Y., Hsu S.D., Huang H.Y., Sun Y.M., Chou C.H., Weng S.L., Huang H.D. MethHC: A database of DNA methylation and gene expression in human cancer. Nucleic Acids Res. 2015;43:D856–D861. doi: 10.1093/nar/gku1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Herman J.G., Graff J.R., Myohanen S., Nelkin B.D., Baylin S.B. Methylation-specific PCR: A novel PCR assay for methylation status of CpG islands. Proc. Natl. Acad. Sci. USA. 1996;93:9821–9826. doi: 10.1073/pnas.93.18.9821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Toyota M., Ahuja N., Ohe-Toyota M., Herman J.G., Baylin S.B., Issa J.P. CpG island methylator phenotype in colorectal cancer. Proc. Natl. Acad. Sci. USA. 1999;96:8681–8686. doi: 10.1073/pnas.96.15.8681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cohen S.A., Yu M., Baker K., Redman M., Wu C., Heinzerling T.J., Wirtz R.M., Charalambous E., Pentheroudakis G., Kotoula V., et al. The CpG island methylator phenotype is concordant between primary colorectal carcinoma and matched distant metastases. Clin. Epigenetics. 2017;9:46. doi: 10.1186/s13148-017-0347-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ashktorab H., Rahi H., Wansley D., Varma S., Shokrani B., Lee E., Daremipouran M., Laiyemo A., Goel A., Carethers J.M., et al. Toward a comprehensive and systematic methylome signature in colorectal cancers. Epigenetics. 2013;8:807–815. doi: 10.4161/epi.25497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Weisenberger D.J., Liang G., Lenz H.J. DNA methylation aberrancies delineate clinically distinct subsets of colorectal cancer and provide novel targets for epigenetic therapies. Oncogene. 2018;37:566–577. doi: 10.1038/onc.2017.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Irizarry R.A., Ladd-Acosta C., Wen B., Wu Z., Montano C., Onyango P., Cui H., Gabo K., Rongione M., Webster M., et al. The human colon cancer methylome shows similar hypo- and hypermethylation at conserved tissue-specific CpG island shores. Nat. Genet. 2009;41:178–186. doi: 10.1038/ng.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Grawenda A.M., O’Neill E. Clinical utility of RASSF1A methylation in human malignancies. Br. J. Cancer. 2015;113:372–381. doi: 10.1038/bjc.2015.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Koch A., Joosten S.C., Feng Z., de Ruijter T.C., Draht M.X., Melotte V., Smits K.M., Veeck J., Herman J.G., Neste L.V., et al. Analysis of DNA methylation in cancer: Location revisited. Nat. Rev. Clin. Oncol. 2018;15:459. doi: 10.1038/s41571-018-0004-4. [DOI] [PubMed] [Google Scholar]
- 123.Van Neste L., Bigley J., Toll A., Otto G., Clark J., Delree P., Van Criekinge W., Epstein J.I. A tissue biopsy-based epigenetic multiplex PCR assay for prostate cancer detection. BMC Urol. 2012;12:16. doi: 10.1186/1471-2490-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aran D., Sabato S., Hellman A. DNA methylation of distal regulatory sites characterizes dysregulation of cancer genes. Genome Biol. 2013;14:R21. doi: 10.1186/gb-2013-14-3-r21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Widschwendter M., Jones A., Evans I., Reisel D., Dillner J., Sundstrom K., Steyerberg E.W., Vergouwe Y., Wegwarth O., Rebitschek F.G., et al. Epigenome-based cancer risk prediction: Rationale, opportunities and challenges. Nat. Rev. Clin. Oncol. 2018;15:292. doi: 10.1038/nrclinonc.2018.30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.