Abstract
Although online health communities (OHCs) are increasingly popular in public health promotion, few studies have explored the factors influencing patient e-health literacy in OHCs. This paper aims to address the above gap. Based on social cognitive theory, we identified one behavioral factor (i.e., health knowledge seeking) and one social environmental factor (i.e., social interaction ties) and proposed that both health knowledge seeking and social interaction ties directly influence patient e-health literacy; in addition, social interaction ties positively moderate the effect of health knowledge seeking on patient e-health literacy. We collected 333 valid data points and verified our three hypotheses. The empirical results provide two crucial findings. First, both health knowledge seeking and social interaction ties positively influence patient e-health literacy in OHCs. Second, social interaction ties positively moderate the effect of health knowledge seeking on patient e-health literacy. These findings firstly contribute to public health literature by exploring the mechanism of how different factors influence patient e-health literacy in OHCs and further contribute to e-health literacy literature by verifying the impact of social environmental factors.
Keywords: e-health literacy, online health communities, social cognitive theory
1. Introduction
1.1. Online Health Communities
Online health communities (OHCs), as a specific application of information and communication technologies (ICTs), have recently become a crucial platform for individuals to conduct health-related activities [1,2,3]. The OHC is a specific type of virtual community (VC). It enables and facilitates “social networking, participation, apomediation, collaboration, and openness within and between different health-related stakeholders” (i.e., health care consumers, caregivers, patients, health professionals, and biomedical researchers) [4,5]. In OHCs, health care consumers and patients can exchange health knowledge and social support [6,7,8] and/or make online appointments with health professionals [9,10,11]. Health caregivers and professionals can use OHCs to deliver health information [12,13] and/or conduct health-related education [14,15]. These advantages make OHCs important places to manage public health activities.
As OHCs have become popular, more and more health-related stakeholders have begun to use OHCs to promote personal e-health literacy. E-health literacy sources from health literacy and refers to “the ability to seek, find, understand and appraise health information from electronic sources and apply knowledge gained to addressing or solving a health problem” [16]. E-health literacy is a behavioral health outcome that can be improved by different interventions (e.g., OHCs) [17,18,19]. Because of the user-generated contents, OHCs are like a health knowledge reservoir that is full of health-related resources shared by different health-related stakeholders [5,20,21]. Consumers can seek and find useful health knowledge in OHCs and use them to tackle their health issues or check up on their health status [22,23]. These activities are helpful for patients to conduct health self-management activities and empower themselves [24,25].
1.2. E-Health Literacy
Scholars place emphases on e-health literacy because e-health literacy directly reflects individuals’ ability to use online health-related resources and in turn achieve better health outcomes [16,24]. Exploring the ways of promoting e-health literacy can help consumers better utilize the health information on the Internet. During the past decades, scholars have also explored the potential factors influencing individual e-health literacy (summarized in Table 1).
Table 1.
A summary of prior studies on e-health literacy.
| Sources | Context/Objective | Independent Variables | Dependent Variables | Findings |
|---|---|---|---|---|
| [26] | Internet, 2371 parents | e-health literacy | parent’s gender; parent’s race/ethnicity; parental language spoken at home; parent’s educational attainment; parent’s marital status; household type; child’s health; age | Exception of parent’s gender, parent’s marital status, and household type, all other factors have positive effects |
| [27] | Internet, 182 middle schoolers | e-health literacy | outcome expectations; training involvement; health motivation; perceived injunctive norm; perceived descriptive norm; subjective norm; personal norm | Exception of health motivation, all other factors have positive effects |
| [28] | 59 college students | levels of e-health literacy | race, age, class standing, college major, final course grades, use of the Internet, time spent on the Internet | Only the effect of use of the Internet is significant and positive |
| [29] | 525 valid college students | e-health literacy (as a mediator) | health status; degree of health concern | All effects are significant and positive |
| [30] | 83 lung cancer survivors | e-health literacy | age; gender; living situation; overall health; overall quality of life; histology; education; access to e-resources | Only the effects of education and access to e-resources are significant and positive |
| [31] | 1917 parents and 1417 students | e-health literacy | parent: age; education; marital status; household poverty; area; parent Internet skill confidence; parent Internet skills adolescent: sex; grade; academic performance; adolescent health information literacy |
Parent: Exception of age, marital status, and area, all other factors have positive effects Adolescent: Exception of sex, all other factors have positive effects |
| [32] | 192 participants | e-health literacy | gender; department; education level; health status; monthly income; website preference categories | All effects are positive and significant |
| [33] | 65 traditional college students and 143 older adult students | overall e-health literacy; functional e-health literacy | age | Age difference does exist between different groups |
| [2] | 1162 patients who use the Internet | e-health literacy | age; self-rated health; Internet use frequency; online health information seeking frequency; types of health information sought | Age difference exists. All other effects are positive and significant |
Based on the prior studies shown in Table 1, we can draw two major conclusions. First, prior studies mainly focused on the effect of Internet use; however, few studies investigated the effect of OHCs that act as a specific intervention on e-health literacy. Future studies should provide more positive evidence to support the roles of OHCs in promoting individual e-health literacy [18]. Second, prior studies mainly focused on the effect of demographic factors (e.g., age, gender, and education) [2,26,31,32,33]; however, a recent review study has also stressed the importance of accessible media environments and contextual spheres [34].
Although there are many studies that have addressed e-health literacy in OHCs, few studies have investigated the factors influencing patient e-health literacy in OHCs. OHCs and other social media are crucial interventions to eliminate the digital divide and promote public health [3,4,14,17,18,24,35]. OHCs provide vulnerable populations with an effective toolkit to access health information and services and give them great promise to influence behavioral health outcomes via their interactivity features and user-generated content mechanism [36,37,38]. E-health literacy, as a personal health outcome state, is a result of both personal determinants (i.e., personal behaviors and cognitive factors) and socio-structural determinants (i.e., social environmental factors) of health [39,40,41]. However, there is a paucity of studies that have investigated the specific mechanism of how personal determinants and social environmental factors influence patient e-health literacy in OHCs [34]. This paper aims to address the above gap. We focus on the following question:
How do patient OHC participatory behavior and OHC social environmental factors influence a patient’s e-health literacy?
1.3. Social Cognitive Theory
We adopt social cognitive theory (SCT) as the theoretical foundation to address the above question. SCT is a widely accepted theory in explaining individual behaviors. SCT is triadic reciprocal determinism in which individual behaviors are a result of three factors: environment, person, and behavior [42]. The person refers to personal individual cognitive factors; the environment includes both physical environment and social environment; and the behavior refers to a focal individual’s actions [42]. According to SCT, every two out of the three factors can interact with each other and then influence the third one; for example, human beliefs and cognitive competencies can be developed and modified by personal behaviors and structures within the environment [42].
During the past several decades, SCT has been widely used in explaining different individual behaviors (e.g., health knowledge sharing behaviors in VCs [43] and adoption intention of telehealth systems [44]) and in explaining personal cognition change (e.g., personal-computer-related technostress [45] and health outcomes [46]). Considering that health outcome change is not only a result of personal behaviors but is also under the influence of social systems [39,40,41], it is suitable to use SCT to explore the factors influencing patient e-health literacy in OHCs.
1.4. Hypotheses and Research Model
Based on SCT and prior studies on e-health literacy, we chose patient health knowledge seeking as a personal behavior and social interaction ties as a social environmental factor in OHCs. Health knowledge seeking behaviors refer to a patient’s consumption of the health knowledge that is available in an OHC or their soliciting of answers or help from other members of the same OHC [47]. Social interaction ties refer to the strength of the relationships between different interaction parties, the amount of time spent, and the communication frequency among different OHC members, and they act as channels for information and resource flows [48]. Directed by SCT, we treated patient e-health literacy as a consequence of both individual behaviors (i.e., health knowledge seeking) and the social environment (i.e., social interaction ties) [39,40,41].
The user-generated content mechanism makes OHCs a health knowledge reservoir. With the facilitation of technologies, users dispersed in different places can freely access OHCs and collaboratively conduct health-related activities. For typical OHC users, seeking health knowledge is one of their basic targets [8,21,49]. They even can seek and exchange health knowledge, treatment experience, or personal information on embarrassing conditions or stigmatized illnesses [7,21,50]. These knowledge seeking behaviors are helpful for patients to manage self-education activities [17,18] and improve their e-health literacy [2,28]. We thus hypothesize the following:
Hypothesis 1.
Patient health knowledge seeking behaviors in OHCs positively influence their e-health literacy.
Besides personal health-related behaviors, the social environment around patients also influences their health-related outcomes [40,41]. Typical users also turn to OHCs for social support or companionship [4,6,7]. They look for patients like them, and they interact and communicate with them to conduct health-related activities. Such an interaction activity acts as an important part of the community sphere and in turn influences patient health outcomes (e.g., e-health literacy) [34]. We thus hypothesize the following:
Hypothesis 2.
Social interaction ties as an OHC social environmental factor positively influence patient e-health literacy.
Social interaction ties are crucial channels for information and resource flows [48]. In OHCs, these information and resource flows are completed via texts, pictures, and/or videos. However, compared with face-to-face communication, online communication channels such as texts, pictures, and/or videos belong to typical lean media and can only deliver limited information [51]. Social interaction ties can change the above situation. Stronger social interaction ties are powerful indicators of an active community sphere and harmonious relationships [48]. They provide users with more opportunities to conduct health-related activities, which are helpful for them to understand and use the knowledge that other members have shared and then obtain better health outcomes. We thus hypothesize the following:
Hypothesis 3.
Social interaction ties positively moderate the effect of health knowledge seeking behavior on patient e-health literacy; i.e., when social interaction ties are strong, the effect of health knowledge seeking behavior on patient e-health literacy will be high; when social interaction ties are weak, the effect of health knowledge seeking behavior on patient e-health literacy will be low.
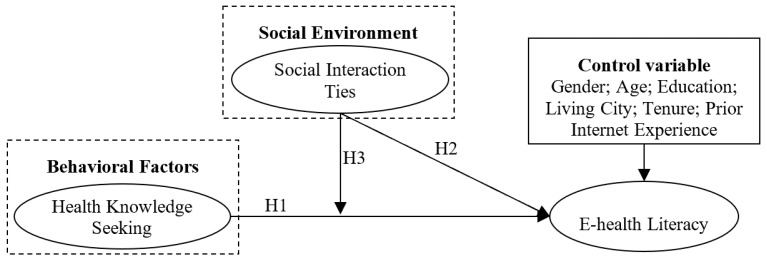
Besides the above factors, patient gender, age, education level, living city, tenure in an OHC, and prior Internet experience might also influence patient e-health literacy. We treated these as control variables. Based on the above factors, we built a research model as shown in Figure 1.
Figure 1.
Hypotheses and research model. Note: H1, H2, and H3 respectively short for Hypothesis 1, Hypothesis 2, and Hypothesis 3.
As discussed above, this paper aims to explore how patient health knowledge seeking behaviors and their social interaction ties in OHCs influence their e-health literacy. We will examine their direct effects and interaction effect to address how OHC use influences patient e-health literacy.
2. Materials and Methods
2.1. Research Design
We adopted a survey approach. This study was approved by STU academic and ethical committees. We developed scales to estimate the three key constructs (i.e., health information seeking, social interaction ties, and e-health literacy). All scales for the three key constructs were adopted from prior studies and adapted to the OHC context. Health knowledge seeking had three items [49]; social interaction ties had four items [48]; and e-health literacy had eight items [16]. All items were scaled with a 5-point Likert scale with 1 representing “totally disagree” and 5 representing “totally agree”.
2.2. Data Collection
We developed a questionnaire composed of the above scales and demographic variables to collect data. The questionnaire was made via an online survey system. We asked the help of community administrators to allow us to post the questionnaire link in their community and finally were approved by four communities. The questionnaire was totally voluntary and anonymous. In order to improve the respondent rate, we provided 50 textbooks to randomly selected participants after the survey was over. The 50 textbooks are current popular books on how to preserve health and their prices were about 30 Chinese Yuan (about 4.3 dollars).
We took several countermeasures to ensure high data quality. First, we added the question “have you ever used an OHC” to identify those actual OHC users. Because the questionnaire link is open and could be answered by anyone on the online survey system, we added the above question to identify the actual OHC users. If they answered “no”, the survey would end; otherwise, they would be required to write out the OHC name. Second, each IP address was allowed to answer only once to avoid repeated participants. Third, we added a reverse question to exclude careless respondents. If a respondent failed to notice the reverse question, the sample will be treated as an invalid one. The survey period lasted two months. There are 409 participants who have ever used an OHC, and 76 out of 409 respondents who had failed in answering the reverse question. We threw out the 76 respondents and finally obtained 333 valid data points. The descriptive statistics results are shown in Table 2.
Table 2.
Descriptive statistics (n = 333).
| Variables | n | % |
|---|---|---|
| Gender | ||
| Male | 112 | 33.6 |
| Female | 221 | 66.4 |
| Age (years) | ||
| < 16 | 1 | 0.3 |
| 16–25 | 86 | 25.8 |
| 26–35 | 82 | 24.6 |
| 36–45 | 69 | 20.7 |
| 46–55 | 66 | 19.8 |
| > 55 | 29 | 8.7 |
| Education | ||
| High school and below | 80 | 24 |
| College | 73 | 21.9 |
| Bachelor | 110 | 33 |
| Master and above | 70 | 21 |
| City | ||
| First tier | 112 | 33.6 |
| Second tier | 113 | 33.9 |
| Others | 108 | 32.4 |
| Prior Internet Experience (years) | ||
| < 1 | 14 | 4.2 |
| 1–2 | 17 | 5.1 |
| 2–3 | 32 | 9.6 |
| 3–4 | 132 | 39.6 |
| 4–5 | 5 | 1.5 |
| > 5 | 133 | 39.9 |
| Tenure (years) | ||
| < 1 | 139 | 41.7 |
| 1–2 | 106 | 31.8 |
| 2–3 | 44 | 13.2 |
| 3–4 | 24 | 7.2 |
| 4–5 | 3 | 0.9 |
| > 5 | 17 | 5.1 |
2.3. Data Analysis
We conducted exploratory factor analysis (EFA, see Table 3) and confirmatory factor analysis (CFA, see Table 4) to estimate the measurement model.
Table 3.
Items and Factor Loadings.
| Constructs | Items | HKS | SIT | EHL |
|---|---|---|---|---|
| Health knowledge seeking | I often use this online health community (OHC) to seek knowledge | 0.817 | 0.140 | 0.145 |
| I frequently use this OHC to seek knowledge | 0.873 | 0.252 | 0.152 | |
| I spend a lot of time using this OHC to seek knowledge | 0.773 | 0.319 | 0.071 | |
| Social interaction ties | I maintain close social relationships with some members in this OHC | 0.277 | 0.844 | 0.055 |
| I spend a lot of time interacting with some members in this OHC | 0.295 | 0.840 | 0.091 | |
| I know some members in this OHC on a personal level | 0.179 | 0.879 | 0.118 | |
| I have frequent communication with some members in this OHC | 0.130 | 0.926 | 0.109 | |
| E-health literacy | I know how to find helpful health resources on the Internet | 0.179 | 0.010 | 0.795 |
| I know how to use the Internet to answer my health questions | 0.181 | 0.023 | 0.841 | |
| I know what health resources are available on the Internet | 0.183 | 0.036 | 0.852 | |
| I know where to find helpful health resources on the Internet | 0.177 | 0.102 | 0.831 | |
| I know how to use the health information I find on the Internet to help me | 0.158 | 0.139 | 0.825 | |
| I have the skills I need to evaluate the health resources I find on the Internet | 0.067 | 0.169 | 0.780 | |
| I can tell high-quality from low-quality health resources on the Internet | 0.044 | 0.157 | 0.781 | |
| I feel confident in using information from the Internet to make health decisions | 0.101 | 0.201 | 0.768 | |
| Cronbach’s α | 0.835 | 0.928 | 0.933 | |
| C.R. | 0.825 | 0.929 | 0.931 | |
| AVE | 0.662 | 0.767 | 0.630 |
Note: HKS, SIT, and EHL respectively short for health knowledge seeking, social interaction ties, and e-health literacy; C.R. is short for composite reliability; AVE is short for average variance extraction.
Table 4.
Covariance Matrix.
| Variables | Mean | SD | Gender | Age | Edu. | City | Tenure | PIE | HKS | SIT | EHL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1.660 | 0.473 | - | ||||||||
| Age | 3.600 | 1.303 | -0.018 | - | |||||||
| Edu. | 2.510 | 1.074 | −0.242 ** | −0.282 ** | - | ||||||
| City | 2.010 | 0.814 | −0.060 | −0.027 | 0.368 ** | - | |||||
| Tenure | 4.490 | 1.435 | −0.149 ** | 0.098 | 0.023 | −0.038 | - | ||||
| PIE | 2.090 | 1.316 | −0.289 ** | −0.333 ** | 0.553 ** | 0.235 ** | 0.280 ** | - | |||
| HKS | 3.382 | 0.945 | 0.084 | 0.250 ** | −0.250 ** | −0.337 ** | −0.084 | -0.154 ** | 0.813 | ||
| SIT | 2.728 | 1.020 | 0.038 | 0.204 ** | −0.335 ** | −0.305 ** | 0.001 | −0.236 ** | 0.502 ** | 0.876 | |
| EHL | 3.705 | 0.761 | 0.011 | 0.081 | −0.030 | −0.055 | −0.033 | 0.007 | 0.328 ** | 0.261 ** | 0.793 |
Note: ** p < 0.01; Edu. and PIE are short for education and prior Internet experience, respectively.
We used two methods to estimate convergent validity [47]. As shown in Table 3, all factor loadings in their respective constructs are greater than 0.7; in addition, all Cronbach’s α and composite reliability values are greater than 0.8. These indices suggest a good convergent validity.
We used two methods to estimate discriminant validity [47]. As shown in Table 3, all factor loadings in their respective constructs are significantly greater than the values in their irrespective constructs. In addition, the values in diagonal lines (i.e., average variance extraction (AVE) square root) in Table 4 are greater than the respective values in non-diagonal lines (i.e., correlation value). These indices suggest a good discriminant validity.
We further estimated the model fit. As shown in Table 5, the values of χ2/df, GFI (Goodness-of-Fit Index), AGFI (Adjusted GFI), NFI (Normed Fit Index), CFI (Comparative Fit Index), and RMSEA (Root-Mean-Square Error of Approximation) are all above the suggested good or acceptable levels [47], indicating a good model fit.
Table 5.
Fit Indices.
| Indices | χ2 | df | χ2/df | GFI | AGFI | NFI | CFI | RMSEA |
|---|---|---|---|---|---|---|---|---|
| Results | 229.840 | 84 | 2.736 | 0.915 | 0.878 | 0.943 | 0.963 | 0.072 |
| Criteria | - | - | < 3 | > 0.9 | > 0.8 | > 0.9 | > 0.9 | < 0.08 |
3. Results
We used hierarchical regression analysis to test all hypotheses. We respectively incorporated control variables, main variables, and interaction variables, and built three models. The F value and R-square value indicated that Model 3 is the best one (see Table 6).
Table 6.
Results of hierarchical regression.
| Model 1 | Model 2 | Model 3 | VIF | ||||
|---|---|---|---|---|---|---|---|
| β | T Value | β | T Value | β | T Value | ||
| Control variables | |||||||
| Gender | 0.002 ns | 0.034 | 0.012 ns | 0.212 | 0.002 ns | 0.041 | 1.143 |
| Age | 0.078 ns | 1.273 | 0.018 ns | 0.302 | 0.034 ns | 0.590 | 1.269 |
| Edu. | 0.001 ns | 0.017 | 0.046 ns | 0.675 | 0.041 ns | 0.609 | 1.706 |
| City | 0.013 ns | 0.213 | 0.056 ns | 0.993 | 0.061 ns | 1.087 | 1.204 |
| Tenure | −0.034 ns | −0.564 | −0.028 ns | −0.496 | −0.017 ns | −0.308 | 1.183 |
| PIE | −0.023 ns | −0.305 | 0.069 ns | 0.969 | 0.058 ns | 0.820 | 1.884 |
| Main variables | |||||||
| HKS | 0.280 *** | 4.525 | 0.288 *** | 4.697 | 1.438 | ||
| SIT | 0.166 ** | 2.649 | 0.148 * | 2.380 | 1.475 | ||
| Interaction variables | |||||||
| SIT × HKS | 0.146 ** | 2.787 | 1.041 | ||||
| R2 | 0.009 | 0.133 | 0.153 | ||||
| Adjusted R2 | −0.009 | 0.111 | 0.130 | ||||
| △R2 | 0.009 | 0.124 | 0.020 | ||||
| F (df) | 0.479 (6) ns | 6.206 (8) *** | 6.495 (9) *** | ||||
| △F | 0.479 ns | 23.192 *** | 7.769 ** | ||||
Note: * p < 0.05, ** p < 0.01, *** p < 0.001, ns, nonsignificant.
As shown in Table 6, all three hypotheses are supported. Namely, patient health knowledge seeking behaviors and their social interaction ties in OHCs positively influence a patient’s e-health literacy. Social interaction ties as an environmental factor positively enhance the effect of health knowledge seeking on patient e-health literacy.
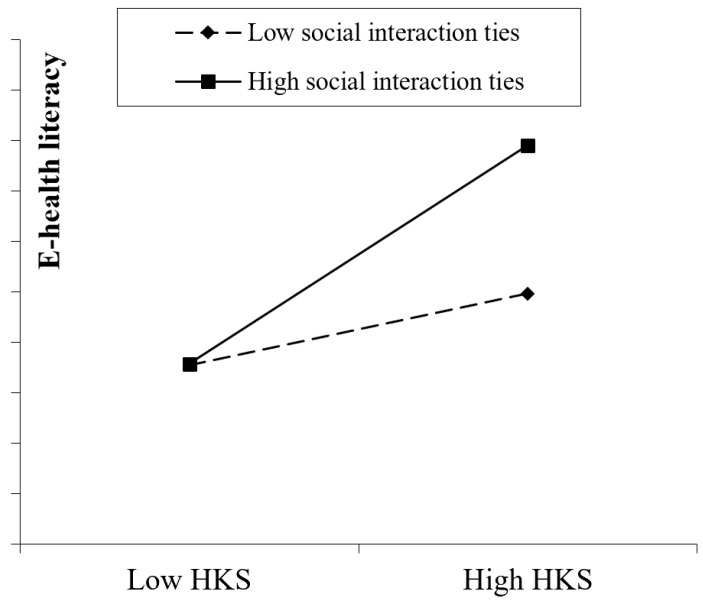
Following the recommended procedures [52], we drew a plot of the moderating effect at one standard deviation below and above the respective means of social interaction ties, health knowledge seeking, and e-health literacy (see Figure 2). As shown in Figure 2, social interaction ties can enhance the effect of health knowledge seeking. When social interaction ties are strong, the effect of patient health knowledge seeking behavior will be high; when social interaction ties are weak, the effect of patient health knowledge seeking behavior will be low.
Figure 2.
SIT positively moderating the effect of HKS on e-health literacy.
4. Discussion
4.1. Theoretical Contributions
This paper makes two significant theoretical contributions. First, we contribute to the literature on the impacts of OHCs on personal health outcomes by exploring the mechanism of how OHC use influences patient e-health literacy. Although OHCs are increasingly popular in public health education and e-health literacy promotion, prior studies are mainly on the impact of the Internet, and few studies have investigated the impact of OHCs [26,27,28,31,32]. In order to address the above gap, this paper explored how behavioral factors (i.e., health knowledge seeking) and social environmental factors (i.e., social interaction ties) influence patient e-health literacy in OHCs. The empirical results show that both health knowledge seeking and social interaction ties positively influence patient e-health literacy; in addition, social interaction ties positively moderate the effect of health knowledge seeking. These findings can enhance our understanding of the mechanism of how OHC use influences patient e-health literacy.
Second, we contribute to the e-health literacy literature by verifying the impact of social environmental factors. Although many studies have explored the antecedents of e-health literacy, they mainly focus on the impacts of demographic factors (e.g., age, gender, and education) [2,26,28,30,31]. Scholars appeal for an emphasis on the importance of accessible media environments and contextual spheres [34]. This study has addressed the above appeal and verified the direct and moderating effects of a social environmental factor (i.e., social interaction ties) on e-health literacy promotion in OHCs. This finding enriches the literature on the roles of social environmental factors in e-health literacy promotion.
4.2. Practical Implications
This paper verified the roles of OHCs in promoting e-health literacy and has two significant practical implications in terms of public health promotion. First, considering that this paper has provided positive evidence supporting the role of OHCs in e-health literacy promotion, health caregivers and educators can use OHCs to conduct e-health literacy education. They can organize health promotion courses via OHCs and deliver more health knowledge to vulnerable groups.
Second, OHC managers should form policies to encourage health knowledge contribution and social networking activities. Considering the positive roles of health knowledge seeking behaviors and social interaction ties, OHC managers can encourage different health-related stakeholders to contribute more health knowledge and member interactions. These endeavors are helpful to keeping OHCs vibrant.
5. Conclusions
This paper focused on the factors influencing patient e-health literacy in OHCs. We identified one behavioral factor and one social environmental factor and developed a model for patient e-health literacy based on the SCT and prior studies on e-health literacy. Our empirical results based on 333 valid data points provided two crucial findings: First, both health knowledge seeking and social interaction ties positively influence patient e-health literacy in OHCs. Second, social interaction ties positively moderate the effect of health knowledge seeking on patient e-health literacy.
This paper has three potential limitations that might undermine our findings. First, we treated patient health knowledge seeking as one integral construct and did not explore the effect of behavior frequencies. Future studies could link patient actual health knowledge seeking behaviors and their e-health literacy together. Second, we did not differentiate the types of health knowledge. Different health knowledge might have different effects on e-health literacy [2]. Future studies could take this into consideration. Third, the time-ordering effect between OHC participation behavior and e-health literacy might be a problem. We had tried to control the above effect by setting OHC participation behavior as time perfect tense while setting e-health literacy as simple present tense. Future studies can also focus on the factors influencing patients’ OHC participation behaviors.
Acknowledgments
The authors thank Zhang Zhen for his excellent job on data collection.
Author Contributions
Conceptualization, J.J.Z.; methodology, J.J.Z.; software, T.T.F.; validation, J.J.Z. and T.T.F.; formal analysis, T.T.F.; investigation, T.T.F.; resources, J.J.Z.; data curation, T.T.F.; writing—original draft preparation, J.J.Z.; writing—review and editing, J.J.Z.; visualization, J.J.Z. and T.T.F.; supervision, J.J.Z.; project administration, J.J.Z.; funding acquisition, J.J.Z.
Funding
This research was funded by NATIONAL NATURAL SCIENCE FOUNDATION OF CHINA, grant number 71501062 and STU SCIENTIFIC RESEARCH INITIATION GRANT, grant number STF18011.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Gu D., Guo J., Liang C., Lu W., Zhao S., Liu B., Long T. Social Media-Based health management systems and sustained health engagement: TPB perspective. Int. J. Environ. Res. Public Health. 2019;16:1495. doi: 10.3390/ijerph16091495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong D.K., Cheung M. Online health information seeking and eHealth literacy among patients attending a primary care clinic in hong kong: A Cross-Sectional survey. J. Med. Internet Res. 2019;21:e10831. doi: 10.2196/10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang A., Schulz P. The measurements and an elaborated understanding of chinese eHealth literacy (C-eHEALS) in chronic patients in china. Int. J. Environ. Res. Public Health. 2018;15:1553. doi: 10.3390/ijerph15071553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eysenbach G. Medicine 2.0: Social networking, collaboration, participation, apomediation, and openness. J. Med. Internet Res. 2008;10:e22. doi: 10.2196/jmir.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hara N., Foon Hew K. Knowledge-sharing in an online community of health-care professionals. Inf. Technol. People. 2007;20:235–261. doi: 10.1108/09593840710822859. [DOI] [Google Scholar]
- 6.Huang K., Chengalur-Smith I., Ran W. Not just for support: Companionship activities in healthcare virtual support communities. Commun. Assoc. Inf. Syst. 2014;29:561–594. doi: 10.17705/1CAIS.03429. [DOI] [Google Scholar]
- 7.Yan L., Tan Y. Feeling blue? Go online: An empirical study of social support among patients. Inf. Syst. Res. 2014;25:667–891. doi: 10.1287/isre.2014.0538. [DOI] [Google Scholar]
- 8.Yao T., Zheng Q., Fan X. The impact of online social support on patients’ quality of life and the moderating role of social exclusion. J. Serv. Res. 2015;18:369–383. doi: 10.1177/1094670515583271. [DOI] [Google Scholar]
- 9.Guo S., Guo X., Fang Y., Vogel D. How doctors gain social and economic returns in online Health-Care communities: A professional capital perspective. J. Manag. Inf. Syst. 2017;34:487–519. doi: 10.1080/07421222.2017.1334480. [DOI] [Google Scholar]
- 10.Liu X., Guo X., Wu H., Wu T. The impact of individual and organizational reputation on physicians’ appointments online. Int. J. Electron. Commer. 2016;20:551–577. doi: 10.1080/10864415.2016.1171977. [DOI] [Google Scholar]
- 11.Zhou J., Amo L., Ye C., Kai S. Using reputation to predict online psychological counselor appointment: Evidence from a chinese website; Proceedings of the 2018 ACM SIGMIS Conference on Computers and People Research; Buffalo, NY, USA. 18–20 June 2018. [Google Scholar]
- 12.Gentles S.J., Lokker C., McKibbon K.A. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: A scoping review. J. Med. Internet Res. 2010;12:e22. doi: 10.2196/jmir.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van der Eijk M., Faber M.J., Aarts J.W., Kremer J.A., Munneke M., Bloem B.R. Using online health communities to deliver patient-centered care to people with chronic conditions. J. Med. Internet Res. 2013;15:e115. doi: 10.2196/jmir.2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boulos M.N.K., Maramba I., Wheeler S. Wikis, blogs and podcasts: A new generation of Web-based tools for virtual collaborative clinical practice and education. BMC Med. Educ. 2006;6:41. doi: 10.1186/1472-6920-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciesielka D. Using a wiki to meet graduate nursing education competencies in collaboration and community health. J. Nurs. Educ. 2008;47:473–476. doi: 10.3928/01484834-20081001-02. [DOI] [PubMed] [Google Scholar]
- 16.Norman C.D., Skinner H.A. EHealth literacy: Essential skills for consumer health in a networked world. J. Med. Internet Res. 2006;8:e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chou W.S., Prestin A., Lyons C., Wen K. Web 2.0 for health promotion: Reviewing the current evidence. Am. J. Public Health. 2013;103:e9–e18. doi: 10.2105/AJPH.2012.301071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korda H., Itani Z. Harnessing social media for health promotion and behavior change. Health Promot. Pract. 2013;14:15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- 19.Balatsoukas P., Kennedy C.M., Buchan I., Powell J., Ainsworth J. The role of social network technologies in online health promotion: A narrative review of theoretical and empirical factors influencing intervention effectiveness. J. Med. Internet Res. 2015;17:e141. doi: 10.2196/jmir.3662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yan Z., Wang T., Chen Y., Zhang H. Knowledge sharing in online health communities: A social exchange theory perspective. Inf. Manag. 2016;53:643–653. doi: 10.1016/j.im.2016.02.001. [DOI] [Google Scholar]
- 21.Zhou J. Factors influencing people’s personal information disclosure behaviors in online health communities: A pilot study. Asia Pac. J. Public Health. 2018;30:286–295. doi: 10.1177/1010539518754390. [DOI] [PubMed] [Google Scholar]
- 22.Nambisan P. Information seeking and social support in online health communities: Impact on patients’ perceived empathy. J. Am. Med. Inf. Assoc. 2011;18:298–304. doi: 10.1136/amiajnl-2010-000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell R.A., Hu X., Orrange S.E., Kravitz R.L. Lingering questions and doubts: Online information-seeking of support forum members following their medical visits. Patient Educ. Couns. 2011;85:525–528. doi: 10.1016/j.pec.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Bodie G.D., Dutta M.J. Understanding health literacy for strategic health marketing: EHealth literacy, health disparities, and the digital divide. Health Mark. Q. 2008;25:175–203. doi: 10.1080/07359680802126301. [DOI] [PubMed] [Google Scholar]
- 25.Gutierrez N., Kindratt T.B., Pagels P., Foster B., Gimpel N.E. Health literacy, health information seeking behaviors and internet use among patients attending a private and public clinic in the same geographic area. J. Community Health. 2014;39:83–89. doi: 10.1007/s10900-013-9742-5. [DOI] [PubMed] [Google Scholar]
- 26.Knapp C., Madden V., Wang H., Sloyer P., Shenkman E. Internet use and eHealth literacy of low-income parents whose children have special health care needs. J. Med. Internet Res. 2011;13:e75. doi: 10.2196/jmir.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paek H., Hove T. Social cognitive factors and perceived social influences that improve adolescent eHealth literacy. Health Commun. 2012;27:727–737. doi: 10.1080/10410236.2011.616627. [DOI] [PubMed] [Google Scholar]
- 28.Robb M., Shellenbarger T. Influential factors and perceptions of eHealth literacy among undergraduate college students. Online J. Nurs. Inform. 2014:18. doi: 10.5210/ojphi.v10i3.9487. [DOI] [Google Scholar]
- 29.Hsu W., Chiang C., Yang S. The effect of individual factors on health behaviors among college students: The mediating effects of eHealth literacy. J. Med. Internet Res. 2014;16:e287. doi: 10.2196/jmir.3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Milne R.A., Puts M.T., Papadakos J., Le L.W., Milne V.C., Hope A.J., Catton P., Giuliani M.E. Predictors of high eHealth literacy in primary lung cancer survivors. J. Cancer Educ. 2015;30:685–692. doi: 10.1007/s13187-014-0744-5. [DOI] [PubMed] [Google Scholar]
- 31.Chang F., Chiu C., Chen P., Miao N., Lee C., Chiang J., Pan Y. Relationship between parental and adolescent eHealth literacy and online health information seeking in Taiwan. Cyberpsychol. Behav. Soc. Netw. 2015;18:618–624. doi: 10.1089/cyber.2015.0110. [DOI] [PubMed] [Google Scholar]
- 32.Dashti S., Peyman N., Tajfard M., Esmaeeli H. E-Health literacy of medical and health sciences university students in Mashhad, Iran in 2016: A pilot study. Electron. Physician. 2017;9:3966. doi: 10.19082/3966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsu W. The effect of age on electronic health literacy: Mixed-Method study. JMIR Hum. Factors. 2019;6:e11480. doi: 10.2196/11480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levin-Zamir D., Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int. J. Environ. Res. Public Health. 2018;15:1643. doi: 10.3390/ijerph15081643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cao X., Wang D. The role of online communities in reducing urban-rural health disparities in china. J. Am. Soc. Inf. Sci. Technol. 2018;69:890–899. doi: 10.1002/asi.24013. [DOI] [Google Scholar]
- 36.Kreps G.L., Neuhauser L. New directions in eHealth communication: Opportunities and challenges. Patient Educ. Couns. 2010;78:329–336. doi: 10.1016/j.pec.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 37.Neuhauser L., Kreps G.L. EHealth communication and behavior change: Promise and performance. Soc. Semiot. 2010;20:9–27. doi: 10.1080/10350330903438386. [DOI] [Google Scholar]
- 38.Graffigna G., Barello S., Triberti S., Wiederhold B.K., Bosio A.C., Riva G. Enabling eHealth as a pathway for patient engagement: A toolkit for medical practice. In: Wiederhold B.K., Riva G., editors. Annual Review of Cybertherapy and Telemedicine. IOS Press; Amsterdam, The Netherlands: 2014. pp. 13–21. [PubMed] [Google Scholar]
- 39.Abraham C., Conner M., Norman P. Understanding and Changing Health Behaviour. Psychology Press; London, UK: 2013. Health Promotion from the Perspective of Social Cognitive Theory; pp. 315–356. [Google Scholar]
- 40.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol. Health. 1998;13:623–649. doi: 10.1080/08870449808407422. [DOI] [Google Scholar]
- 41.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 42.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ, USA: 1986. [Google Scholar]
- 43.Zhang X., Liu S., Deng Z., Chen X. Knowledge sharing motivations in online health communities: A comparative study of health professionals and normal users. Comput. Hum. Behav. 2017;75:797–810. doi: 10.1016/j.chb.2017.06.028. [DOI] [Google Scholar]
- 44.Tsai C. Integrating social capital theory, social cognitive theory, and the technology acceptance model to explore a behavioral model of telehealth systems. Int. J. Environ. Res. Public Health. 2014;11:4905–4925. doi: 10.3390/ijerph110504905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shu Q., Tu Q., Wang K. The impact of computer self-efficacy and technology dependence on computer-related technostress: A social cognitive theory perspective. Int. J. Hum. Comput. Interact. 2011;27:923–939. doi: 10.1080/10447318.2011.555313. [DOI] [Google Scholar]
- 46.Baranowski T., Perry C.L., Parcel G.S. How individuals, environments, and health behavior interact. In: Glanz K., Rimer B.K., Lewis F.M., editors. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed. Jossey-Bass; San Francisco, CA, USA: 2002. pp. 165–184. [Google Scholar]
- 47.Zhou J., Zuo M., Yu Y., Chai W. How fundamental and supplemental interactions affect users’ knowledge sharing in virtual communities? A social cognitive perspective. Internet Res. 2014;24:566–586. doi: 10.1108/IntR-07-2013-0143. [DOI] [Google Scholar]
- 48.Chiu C.M., Hsu M.H., Wang E.T.G. Understanding knowledge sharing in virtual communities: An integration of social capital and social cognitive theories. Decis. Support Syst. 2006;42:1872–1888. doi: 10.1016/j.dss.2006.04.001. [DOI] [Google Scholar]
- 49.Yan Y., Davison R.M. Exploring behavioral transfer from knowledge seeking to knowledge contributing: The mediating role of intrinsic motivation. J. Am. Soc. Inf. Sci. Technol. 2013;64:1144–1157. doi: 10.1002/asi.22820. [DOI] [Google Scholar]
- 50.Alleman J.R. Online counseling: The internet and mental health treatment. Psychother. Theory Res. Pract. Train. 2002;39:199–209. doi: 10.1037/0033-3204.39.2.199. [DOI] [Google Scholar]
- 51.Dennis A.R., Fuller R.M., Valacich J.S. Media, tasks, and communication processes: A theory of media synchronicity. MIS Q. 2008;32:575–600. doi: 10.2307/25148857. [DOI] [Google Scholar]
- 52.Aiken L.S., West S.G., Reno R.R. Multiple Regression: Testing and Interpreting Interactions. SAGE Publications; London, UK: 1991. [Google Scholar]