Abstract
Liver cancer is among the leading global healthcare issues associated with high morbidity and mortality. Liver cancer consists of hepatocellular carcinoma (HCC), cholangiocarcinoma (CCA), hepatoblastoma (HB), and several other rare tumors. Progression has been witnessed in understanding the interactions between etiological as well as environmental factors and the host in the development of liver cancers. However, the pathogenesis remains poorly understood, hampering the design of rational strategies aiding in preventing liver cancers. Accumulating evidence demonstrates that aberrant activation of the Wnt/β-catenin signaling pathway plays an important role in the initiation and progression of HCC, CCA, and HB. Targeting Wnt/β-catenin signaling potentiates a novel avenue for liver cancer treatment, which may benefit from the development of numerous small-molecule inhibitors and biologic agents in this field. In this review, we discuss the interaction between various etiological factors and components of Wnt/β-catenin signaling early in the precancerous lesion and the acquired mechanisms to further enhance Wnt/β-catenin signaling to promote robust cancer formation at later stages. Additionally, we shed light on current relevant inhibitors tested in liver cancers and provide future perspectives for preclinical and clinical liver cancer studies.
Keywords: liver cancer, precancerous lesion, HCC, CCA, HB, Wnt/β-catenin signaling
1. Introduction
Liver cancer is among the leading global healthcare issues associated with high morbidity and mortality. Primary liver cancers consist of hepatocellular carcinoma (HCC), cholangiocarcinoma (CCA), and hepatoblastoma (HB). Other rare tumors are fibrolamellar carcinoma, hepatocellular adenoma, focal nodular hyperplasia, fibrosarcoma, angiosarcoma, leiomyosarcoma, and lymphoma.
HCC is the fifth most frequent cancer worldwide and is closely associated with cancer-related deaths [1]. HCC accounts for around 90% of liver cancer patients. The etiological factors for HCC include hepatitis B (HBV), hepatitis C (HCV) viruses, alcohol abuse, obesity-induced non-alcoholic steatohepatitis (NASH), as well as aflatoxin-B1 exposure. Most HCCs start with chronic hepatitis caused by the above etiological factors, which gives rise to fibrosis and progresses to cirrhosis around 10 years later [1].
CCA is the second most common liver cancer following HCC. CCA is a devastating malignancy with a dismal 5-year overall survival rate of less than 10%. Based on the anatomic location, CCAs are classified into intrahepatic (iCCA), perihilar (pCCA), and distal (dCCA) subtypes. iCCA associates better with cirrhosis resulting from HCV than HBV infection. pCCA is closely related to primary sclerosing cholangitis marked by chronic inflammation [2].
HB is the most common pediatric liver malignancy and stems from hepatic progenitor cells that undergo malignant transformation during embryogenesis [3]. Although surgery along with chemotherapy has largely improved prognosis, around one quarter of the patients die of the disease. Compared to the general population, the risk of HB is 750–7500 times higher in children predisposed to familial adenomatous polyposis (FAP) [4].
With the exception of HBs, most liver cancers take decades to facilitate the progression from the precancerous dysplasia of liver cells located in a chronic inflammatory microenvironment towards a malignant phenotype. During this process, the accumulation of aberrant genetic and epigenetic modifications leads to the dysregulation of signaling pathways, which in turn promote the initiation and progression of liver cancers.
Aberrantly activated Wnt/β-catenin signaling plays a critical role in precancerous dysplasia as well as the malignant transformation of liver cells and malignant expansion of cancer cells. Here, we summarize the latest advances in our understanding of Wnt/β-catenin signaling in the course of liver cancer development and highlight the clinical implications of Wnt/β-catenin signaling pathway as a rational therapeutic target.
2. Wnt/β-Catenin Signaling
The Wnt/β-catenin signaling pathway is evolutionarily conserved and required in both physiological and pathophysiological processes [5,6,7]. The association of Wnt ligands to corresponding receptors triggers the Wnt/β-catenin signaling pathway. These ligands are generated within the endoplasmic reticulum (ER), which undergoes palmitoylation by the Wnt acyl-transferase porcupine (PORCN). Next, Wntless (WLS) shuttles the palmitoylated ligands from the Golgi to the cell membrane, where they can signal in an autocrine or paracrine manner [8].
Wnt/β-catenin signaling is inactive in the normal tissues of adults, except for some stem cell niches [9]. This is achieved through a balanced regulation through Wnt ligands and the β-catenin destruction complex. Wnt antagonists, including secreted frizzled-related proteins (SFRPs), dickkopfs (DKKs), and the Wnt inhibitory factor (WIF) capturing Wnt ligands, as well as Kallistatin binding to the low-density lipoprotein receptor-related protein 6 (LRP6) inhibit the combination of Wnt ligands and receptors [10,11]. The central component β-catenin is tightly regulated by the destruction complex, which is composed of scaffold proteins AXIN1 and AXIN2, adenomatous polyposis coli (APC), and the kinases GSK3 and CK1α. β-catenin is subject to phosphorylation firstly at Ser45 by CK1α, potentiating the subsequent phosphorylation at Thr41, Ser37, and Ser33 by GSK3. Next, the phosphorylated β-catenin is recognized by the β-transducin repeat containing protein (βTRCP), which mediates its ubiquitylation and subsequent proteolysis [10,12].
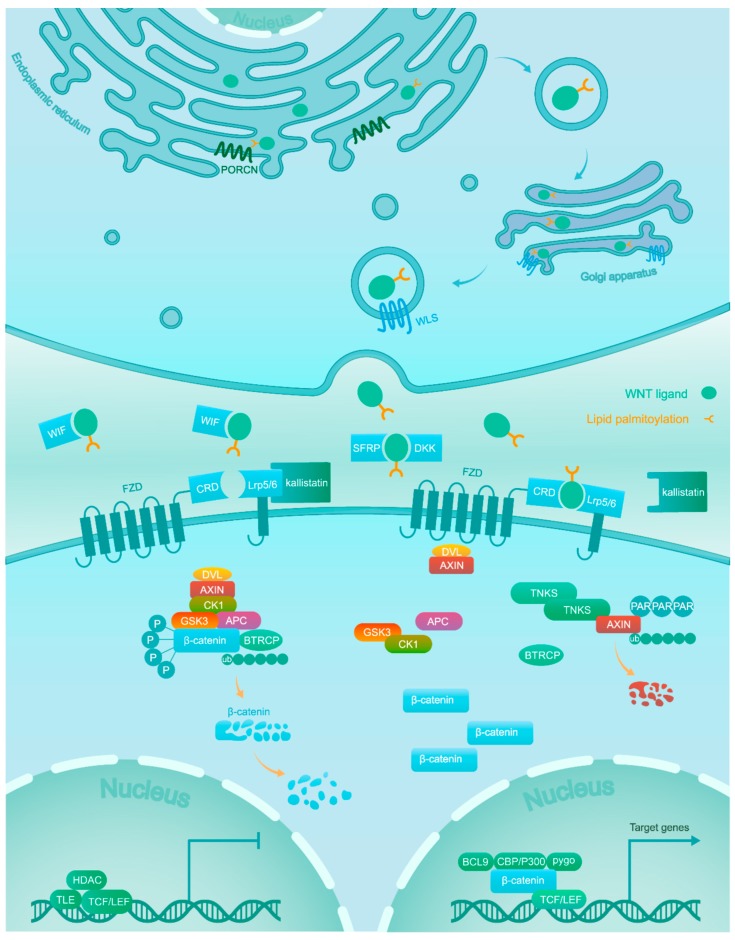
On the contrary, in the active condition Wnt ligands bind at the cysteine rich domain (CRD) of one of the frizzled (FZD) receptors and one of the LRP5/6 co-receptors. Next, the interaction between Wnt ligands and receptors recruits scaffolding proteins disheveled (DVL) and AXIN to the membrane. The AXIN proteins themselves are also under proteolytic control and are rapidly degraded following poly-ADP-ribosylation (PAR) by tankyrase (TNKS) enzymes [13,14]. The sequestration and degradation of AXIN result in the disassembly of the β-catenin destruction complex [15] and subsequent accumulation of unphosphorylated β-catenin in the cytoplasm, which acquires the ability to escape ubiquitylation and proteolysis. This allows active β-catenin to translocate to the nucleus [16], where it binds to transcription factors of the T-cell factor/lymphoid enhancer-binding factor (TCF/LEF) family with recruitment of co-activators (BCL9, CBP/300, Pygo, and others) to turn on the transcription of downstream target genes [17] (Figure 1).
Figure 1.
Wnts are lipid-modified by PORCN in the ER and escorted by WLS from the Golgi to the plasma membrane for secretion. In the absence of Wnt ligands due to Wnt antagonists (WIF, DKK, and SFRP) and Kallistatin, β-catenin is phosphorylated by a destruction complex consisting of GSK3, CK1, APC and AXIN. Phosphorylated β-catenin is targeted for proteasomal degradation after ubiquitination. In the nucleus, the TCF/LEF transcription factor activity is repressed by transducin-like enhancer of split (TLE) and histone deacetylase (HDAC). Association of Wnt ligands with their receptors leads to the dissociation of the destruction complex. As a result, β-catenin accumulates in the cytoplasm and translocates into the nucleus, where it promotes the expression of target genes via interaction with TCF/LEF and co-activators such as CBP/300, BCL9, and Pygo.
3. Precancerous Lesion
Aberrant activation of Wnt/β-catenin signaling exists at both hepatic precancerous lesions and cancerous foci. Uncovering how the signaling is deregulated in these precancerous lesions will be beneficial to better understand the mechanisms contributing to the progression of liver cancer. The most important event in precancerous lesions is the dysplasia and dysfunction of liver cells infected or affected by the given etiological factors. Thus, it is necessary to elucidate the interaction between these factors and components of Wnt/β-catenin signaling in these cells.
3.1. Hepatitis Viruses
3.1.1. HBV
HBV infection increases the risk of developing HCC about 100–200-fold [18]. HBV is a hepadnavirus with double-stranded DNA including four overlapping open reading frames encoding a viral DNA polymerase, two structural proteins (the surface and core antigens), and the regulatory hepatitis B viral X protein (HBx) [19]. Besides maintaining the transcription and replication of HBV, HBx plays an important role in activating Wnt/β-catenin signaling in the infected hepatocytes. HBx regulates multiple components of Wnt/β-catenin signaling at extracellular and intracellular levels. Extracellularly, HBx dramatically diminishes Wnt antagonist SFRP1 and SFRP5 expression due to genetic silencing by recruiting DNA methyltransferase 1 and 3A to gene promoters [20]. Intracellularly, HBx compromises the function of the destruction complex by competitively binding APC [21] or by inhibiting GSK3 activity through activation of Src kinase [22] as well as induction of cell-cycle-related kinase-mediated androgen receptor signaling [23].
The hepatitis B surface antigen (HBsAg) regulates the expression of LEF-1, a key transcription factor of β-catenin in the nucleus [24,25,26]. A marked increase of LEF-1 was observed in HBsAg-expressing HCC cell lines and confirmed by interference experiments with small interfering RNA [25]. Furthermore, the same group validated that HBsAg increased the level of LEF-1 along with c-Myc and cyclin D1 (β-catenin downstream genes), more pronounced in peritumor tissues compared to liver tumors in HBV-associated HCC patients [26].
The integration of viral DNA into the host genome is a special event during HBV infection that occurs mostly near particular sites, e.g., the long interspersed nuclear elements (LINEs). The HBV genome inserted into a LINE1 element produces an oncogenic HBV-LINE1 chimeric transcript, inducing nuclear localization of β-catenin and triggering target gene expression [18,27]. Nevertheless, the fusion transcripts were not detectable in other cohorts [28,29], and therefore the observation needs further investigation in more cohorts from different regions.
Despite a major risk factor for CCA, HBV function on Wnt/β-catenin signaling in infected cholangiocytes remains obscure. Part of the mechanisms revealed in infected hepatocytes could be shared.
3.1.2. HCV
Chronic HCV infection is a major risk factor for the development of HCC. HCV contains a single-stranded positive sense RNA with a single open reading frame encoding the structural proteins (core, E1, and E2), the viroporin p7, and the non-structural proteins (NS2, NS3, NS4A, NS4B, NS5A, and NS5B). Different from HBV, as an RNA virus HCV lacks a DNA intermediate phase during its life cycle. Hence, HCV infection relies on the interaction of its viral proteins with the infected hepatocytes but not the damage to the host genome [30]. Currently, the core protein NS5A and E2 have been reported to be closely related to the activation of Wnt/β-catenin signaling.
As the central component of HCV particles, the core protein is detectable in the cytoplasm, Golgi apparatus, lipid droplets, and nucleus [31,32]. Particularly, in the nucleus it potentiates the activation of Wnt/β-catenin signaling. This is achieved through increasing the expression levels of Wnt ligands, FZD, and LRP5/6 receptors [33,34], while simultaneously downregulating the transcription of Wnt antagonists SFRP2 and DKK1 [35,36]. In addition, the HCV core protein facilitates the hypermethylation at the CDH1 gene promoter [37], leading to a reduction of E-cadherin protein expression. As a result, the β-catenin/E-cadherin complexes at the cell membrane capture less β-catenin, leading to higher levels of free β-catenin in the cytosol, thus enhancing activation of Wnt/β-catenin signaling.
As a component of the HCV RNA replication complex, NS5A enhances the ability of HCV to counteract apoptosis [38]. On the other hand, NS5A promotes Wnt/β-catenin signaling directly by binding and stabilizing the β-catenin protein [39] and indirectly by stimulating the PI3K/Akt pathway, which further mediates the inactivation of GSK3β, stabilization of β-catenin, and subsequent stimulation of β-catenin-dependent transcription [40,41,42].
HCV structural E2 protein activates the Src homology region 2 domain-containing phosphatase-2 (SHP-2) [43], which promotes Wnt/β-catenin signaling by tyrosine dephosphorylation of parafibromin. The unphosphorylated parafibromin binds and stabilizes β-catenin in the nucleus, thereby inducing target gene expression [44].
HCV enhances Wnt/β-catenin signaling independent of its proteins as well. HCV infection upregulates the expression of microRNA-155 (miR-155), which directly restrains APC expression, one of the major negative regulators in the destruction complex to regulate cytoplasmic β-catenin levels [45]. Additionally, HCV infection increases epidermal growth factor receptor (EGFR) and fibroblast growth factor (FGF) signaling, both of which lead to the release of β-catenin from the β-catenin/E-cadherin complexes as a result of tyrosine phosphorylation of β-catenin at residue Y654 and the inactivation of GSK3β through stimulation of PI3K/Akt and Ras/Raf/MEK/ERK cascades [46,47].
Apparently, HCV proteins build a network consisting of a plethora of molecular events to stimulate Wnt/β-catenin signaling, which in turn further facilitates HCV infection. Firstly, the combination of Wnt1 and Wnt5a with FZD receptors leads to the release of soluble EGFR ligands [48], which bind to EGFR triggering the co-internalization of a HCV–CD81–EGFR complex to favor HCV entry [49,50]. Secondly, Wnt/β-catenin signaling activates FGF signaling by increasing FGF18 and FGF20 expression [51], which enhances HCV replication and the release of infectious particles [52].
However, whether and how HCV particles regulate Wnt/β-catenin signaling in the HCV-infected cholangiocytes is still unclear.
3.2. Alcohol Abuse
Chronic alcohol abuse leads to alcoholic liver disease, which progresses from fatty liver through alcoholic hepatitis, hepatic fibrosis to cirrhosis, and ultimately HCC. A widely used in vivo model of chronic alcohol abuse is to feed adult male Long Evans rats with 37% ethanol for 8 weeks. In this model, nuclear and cytoplasmic expression of β-catenin was decreased in the liver, indicating that Wnt/β-catenin signaling is disrupted [53,54]. In line with this are mouse models given low ethanol concentrations within a timeframe of a few days, in which hepatic loss of β-catenin increases susceptibility to alcoholic liver disease through disrupting alcohol metabolizing enzymes, fatty acid oxidation, and fasting ketogenesis [55,56,57]. In contrast, Wnt/β-catenin signaling is activated by chronic alcohol abuse to increase hepatocyte proliferation and diethylnitrosamine (DEN)-induced tumorigenesis in a different mouse model, which requires a 4-month feeding of a 4.9% ethanol-containing diet. Ethanol increased the total number of cancerous foci and liver tumors identified in situ fixed livers from the ethanol+DEN group compared to corresponding pair-fed (PF)+DEN and chow+DEN control groups. In the ethanol+DEN group, tumor multiplicity corresponded to a 3- to 4-fold increase in proliferation and immunohistochemical staining of β-catenin in non-tumorigenic hepatocytes when compared to the PF+DEN and chow+DEN groups [58]. A similar mouse model fed a Western alcohol diet for 4 months after DEN injection was used to validate Stearoyl-CoA desaturase 2 (Scd2) as responsible for liver tumor development. Importantly, Scd2 is a target gene of Wnt/β-catenin signaling and provides a positive feedback loop to amplify the pathway via stabilization of LRP5 and LRP6 mRNA levels [59].
The paradoxical conclusions in regards to the effect of chronic alcohol abuse on the Wnt/β-catenin signaling question the optimal model for alcoholic liver disease, especially the animal strains, ethanol concentration, as well as exposure time. For humans, it takes years to develop a fatty liver without abnormal physical findings, and decades to alcoholic hepatitis (often with concomitant cirrhosis). Short-term ethanol consumption may recapitulate the early stage of alcoholic liver disease, while the 4-month mouse models may coincide with late stage. Thus, Wnt/β-catenin signaling could play a different role from the early to late stages of alcoholic liver disease, which needs further investigation.
3.3. Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD), featuring fat accumulation in hepatocytes, ranges from simple steatosis to non-alcoholic steatohepatitis (NASH). The latter is associated with inflammation and fibrosis and is a major risk factor for the onset and progression of HCC [60]. From NAFLD to NASH and finally HCC, Wnt/β-catenin signaling is dynamically fine-tuned.
Aberrant adipogenesis is the central event for NAFLD, which needs the transcription factor peroxisome proliferator-activated receptor γ (PPARγ). However, Wnt/β-catenin signaling inhibits PPARγ mRNA expression [61,62]. Thus, its inactivation is required for NAFLD development, confirmed by hyperlipidemia as well as fatty liver disease resulting from non-conservative inactivating mutations in the Wnt coreceptor LRP6 in mice and by the rescue of NAFLD using Wnt ligand Wnt3A [63,64,65].
The increased burden of fat in hepatocytes, oxidative stress, and lipid peroxidation induces hepatic inflammation and fibrosis, exacerbating to NASH. During this process, Wnt/β-catenin signaling is restored by the overexpressed aortic carboxypeptidase-like protein (ACLP) that specifically binds FZD8 and LRP6 to form a ternary complex facilitating extracellular signaling transduction [66]. Levels of Wnt ligands are increased due to the complementary secretion from infiltrating macrophages [67]. Alternatively, epigenetic modifications of components involved contribute to the activation of Wnt/β-catenin signaling, including hypermethylation of Wnt antagonists, deacetylation of histones in the AXIN2 promoter, and downregulation of microRNAs negatively regulating Wnt/β-catenin signaling [15,68].
3.4. Aflatoxin-B1 Exposure
Aflatoxins are a class of carcinogenic mycotoxins produced by Aspergillus fungi, contaminating food supplies worldwide. Aflatoxin-B1 is the most toxic aflatoxin, and it has been well validated to dramatically increase the risk of HCC in humans and animals [69]. Aflatoxin-B1 frequently induces G:C to T:A transversions at the third base in codon 249 of TP53 and cooperates with HBV in causing p53 mutations in HCC [70]. Additionally, aflatoxin-B1 regulates Wnt/β-catenin signaling. In vitro studies using HCC cell lines treated with aflatoxin-B1 for 1 or 2 days showed that β-catenin protein levels were decreased by elevated miR-33a and miR-34a [71,72]. However, human HCCs with high exposure to aflatoxin B1 showed strong β-catenin membrane staining observed in tumor areas, compared to adjacent non-neoplastic liver tissue, possibly increasing Wnt/β-catenin signaling [73]. The discrepancy between the HCC cell lines and human HCC tissues indicates the dynamic alteration of Wnt/β-catenin signaling in the development of aflatoxin-B1-related HCC.
Accordingly, most major etiological factors of liver cancers contribute to the activation of Wnt/β-catenin signaling in precancerous lesions through multiple mechanisms, although non-virus factors suppress its activity temporarily in the early stage of pathological damage (Table 1). The elevated Wnt/β-catenin signaling enhances the proliferation of the affected liver cells, thereby overgrowing neighboring normal cells. This highlights the pivotal role of Wnt/β-catenin signaling in the transformation from precancerous lesions to liver cancers.
Table 1.
Summary of the function of etiological factors on the regulation of Wnt/β-catenin signaling.
| Etiological Factors | Roles to Regulate Wnt/β-Catenin Signaling | References |
|---|---|---|
| HBV | ||
| HBx |
|
[20] |
|
[21,22,23] | |
| HBsAg |
|
[24,25,26] |
| other |
|
[18,27] |
| HCV | ||
| core protein |
|
[33,34] |
|
[35,36] | |
|
[37] | |
| NS5A |
|
[39] |
|
[40,41,42] | |
| E2 |
|
[43,44] |
| others |
|
[45] |
|
[46,47] | |
| Alcohol abuse |
|
[53,54,55,56,57] |
|
[58,59] | |
| NAFLD |
|
[63,64,65] |
|
[15,66,67,68] | |
| Aflatoxin-B1 |
|
[71,72] |
|
[73] |
4. Liver Cancers
4.1. Hepatocellular Carcinoma
Around 40–70% of HCCs show β-catenin nuclear accumulation, augmenting Wnt/β-catenin signaling activity [74,75,76,77]. Mutations in key genes are involved in this process [78,79,80]. For instance, activating mutations in exon 3 of CTNNB1 encoding β-catenin are detected in 15–25% of HCCs, producing mutated β-catenin escaping phosphorylation and subsequent degradation [8,79,81,82]. Inactivating mutations occurring in AXIN1 are reported in 10.4% of HCCs, followed by AXIN2 and APC, which are mutated in 3.3% and 1.4%, respectively [8]. The mutations in these negative regulators diminish the biological function of the destruction complex, thus favoring β-catenin accumulation. Remarkably, CTNNB1 mutations show higher frequencies in HCV-related (26.7%) and non-viral HCCs (21.1%) than HBV-related HCCs (11.6%). Conversely, AXIN1 mutations are more frequent in HBV-related HCCs (18%) compared to HCV-related (14%) and non-viral HCCs (8%) [82]. The difference may derive from the fact that different etiological factors cause a different local microenvironment, serving as particular selection pressure for the optimal mutation types.
However, β-catenin nuclear accumulation is recently reported to be restricted to late-stage HCC. At earlier stages, β-catenin is primarily located at the plasma membrane in complexes with multiple cadherin family members, where it drives tumor cell survival by enhancing the signaling of growth factor receptors such as EGFR [83]. This study reveals the unexpected function of β-catenin in early stages of HCC and emphasizes the complex roles β-catenin is playing during HCC progression.
In addition, other genetic and epigenetic alterations in relevant genes enhance Wnt/β-catenin signaling in liver cancer cells. Wnt ligands are elevated by excessive secretion from liver cancer cells, infiltrating macrophages as well as other cell types within cancerous foci [67,84]. In contrast, Wnt antagonists including SFRP1/4/5 and Kallistatin are decreased in HCCs, thus facilitating the combination of Wnt ligands with receptors [85,86]. On the other hand, highly expressed miR-1246 decreases expression levels of AXIN2 and GSK3β [87]. Hypermethylation in the APC gene leads to the loss of APC protein [88]. Together, these epigenetic alterations synergistically compromise the function of the destruction complex to promote Wnt/β-catenin signaling in HCCs.
4.2. Cholangiocarcinoma
Aberrant activation of Wnt/β-catenin signaling is observed in the majority of CCA, which closely associates with tumor malignancy and patient outcome. Differently from HCC, mutations in related genes are less frequent in CCA, i.e., CTNNB1 (1.5%), AXIN1 (4%), and APC (2%) [82]. Apparently, the aberrant activation seems to be more transcriptionally and epigenetically mediated. Similar to HCC, the transcription of Wnt ligands, especially Wnt7A, is increased, which is largely attributable to the secretion from macrophages present in CCA tissues [89,90]. Wnt antagonists DKK2, SFRP1, and SFRP2 are reduced as a result of promoter hypermethylation [91]. Additionally, increased expression of the retinoic acid receptor gamma and long non-coding RNA PCAT1 have been suggested to promote Wnt/β-catenin signaling in CCA [92,93]. Similar suggestions have been made for reduced expression of SOX17 and the tumor suppressor LKB1 [94,95].
4.3. Hepatoblastoma
Activation of the Wnt/β-catenin signaling pathway is deemed an important hallmark during the development of hepatoblastomas [96]. Around 60–80% of hepatoblastomas possess activating mutations in CTNNB1, including point mutation or deletions in exon 3 [97]. Other mutations observed occur in APC (20.51%), AXIN1 (1.67%), AXIN2 (3.75%), and LGR6 (12.5%) [82]. Transcriptional and epigenetic modifications of related components remain unclear in the context of HB.
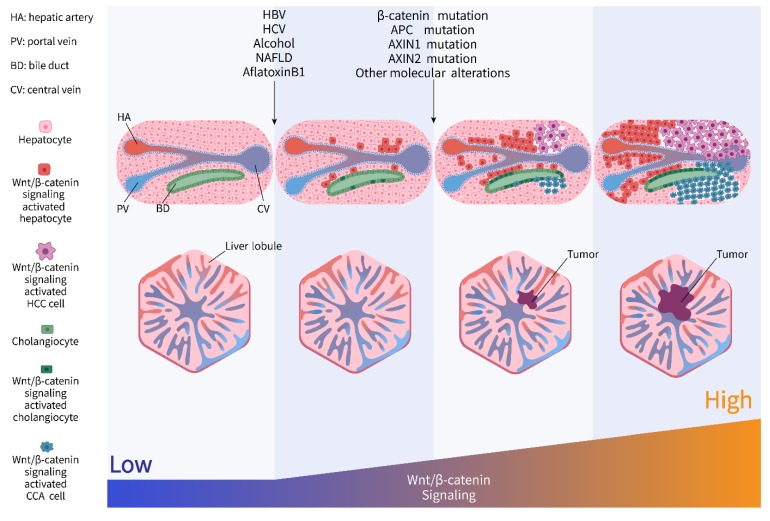
During the decades from risk factor exposure to final liver cancer, liver cells acquire activation of Wnt/β-catenin signaling due to the molecular interaction between etiological factors and the host. Then these cells evolve into tumor cells with robust stimulation strengthened by genomic, epigenetic, and transcriptional alterations of the components involved in Wnt/β-catenin signaling, conferring proliferative advantage and thereby contributing to the progression of tumor formation (Figure 2).
Figure 2.
Dynamic activation of Wnt/β-catenin signaling from risk factor exposure to final liver cancer.
5. Targeting Wnt/β-Catenin Signaling in Liver Cancers
As outlined above, accumulating evidence validates the pivotal role of aberrant activation of Wnt/β-catenin signaling in the pathological process of liver cancers. It highlights potential benefits to targeting components involved in Wnt/β-catenin signaling for liver cancer treatment. During the last decades, a tremendous progression of exploring potent Wnt/β-catenin signaling inhibitors has been witnessed for various tumor types. Table 2 summarizes the reported Wnt/β-catenin signaling inhibitors tested mainly in liver cancers. These inhibitors either target the upstream molecules of Wnt/β-catenin signaling involving the PORCN protein, Wnt ligands, Wnt antagonist DKK1, FZD receptors, and LRP5/6 co-receptors, or intracellularly interfere with tankyrase activity, phosphorylation, and translocation of β-catenin as well as its interaction with co-activators or transcriptional factors. Recently, Michael et al. show that CTNNB1 mutation in pericentral hepatocytes leads to glutamine-dependent mTORC1 activation and show a notable therapeutic benefit of mTORC1 inhibition in CTNNB1 mutant HCC in vivo. This provides a novel way to specifically target this subset of HCCs [98].
Table 2.
Wnt/β-catenin signaling inhibitors undergoing preclinical and clinical evaluation in liver cancers.
| Targets | Compounds | Diseases | Stage | References |
|---|---|---|---|---|
| FZD7 | sFZD7 | HCC | Preclinical | [99] |
| FZD8 | OMP-54F28 | HCC, ovarian cancer, pancreas cancer | Phase 1 | [100,101,102,103,104] |
| LRP5/6 | Salinomycin | breast, prostate, lung, gastric, osteosarcoma, HCC | Preclinical | [105,106,107,108,109,110] |
| Wnt1 | Anti-Wnt1 | HCC, CRC, lung cancer, sarcoma, breast cancer, head-neck squamous cell carcinoma | Preclinical | [111,112,113,114,115] |
| Wnt ligands | WIF-Fc/ SFRP-Fc | HCC | Preclinical | [116] |
| DKK1 | DKN-01 | HCC, CCA, biliary tract cancer, gallbladder cancer, and other cancers | Phase 1/2 | [117,118,119,120,121,122,123,124] |
| PORCN | CGX1321 | HCC, CCA, and other cancers | Phase 1 | [125,126,127] |
| IWP12 | HCC and CRC | Preclinical | [128] | |
| Tankyrase | XAV939/WXL-8 | HCC | Preclinical | [129] |
| β-catenin phosphorylation |
CGK062 | CRC, HCC, prostate cancer | Preclinical | [130] |
| β-catenin | β-catenin siRNA | HCC | Preclinical | [131] |
| BBI608 | Glioblastoma, CRC, HCC, gastric cancer, pancreas cancer, lung cancer | Phase 1/2 | [132] | |
| β-catenin/CBP | PRI-724 | Pancreatic adenocarcinoma, leukemia, CRC, HCV-induced cirrhosis, solid tumor | Phase 1/2 | [133,134,135,136,137,138] |
| β-catenin/TCF | PKF115-548 PKF222-815 CGP049090 FH535 |
HCC, CRC, lung cancer | Preclinical | [139,140,141,142] |
| β-catenin nuclear export | Peg-IFN | HCC | Preclinical | [143] |
The bold highlights the liver cancers, in which the compound have been tested.
6. Future Perspectives
Investigations exploring mechanisms underlying hepatocarcinogenesis accumulating over the last decades enrich our understanding of liver cancer development. Together with enormous progression in clinical technology and treatment guidelines, these achievements improve early detection and enable a more efficient treatment design for liver cancer patients. Nevertheless, liver cancer remains a major cause of tumor-related deaths worldwide.
Liver cancer patients show high phenotypic and molecular heterogeneity, contributing to the lack of a curative therapy. Correlation between phenotype and molecular characteristics is important for clinical practice in HCC patients, especially those diagnosed at an advanced stage depending on conservative treatment using small molecular inhibitors. In parallel to pathological classification, molecular profiles have been explored to categorize HCC. The group led by Jessica Zucman-Rossi proposed a distinct classification comprising six subtypes based on gene expression and have linked these subtypes to clinical and pathological classifications. Importantly, aberrant Wnt/β-catenin signaling activation is an outstanding biological feature in G5–G6, highlighting the predominant tumorigenic function of this pathway in these groups [144,145,146].
Due to its key role in HCC and other liver diseases, a large number of compounds inhibiting Wnt/β-catenin signaling have been explored. However, only a minority have been tested in liver cancer, as indicated in Table 2. These studies are mainly carried out in HCC and a few in CCA, with none in HB. In light of the critical role of Wnt/β-catenin signaling linking precancerous lesions to liver cancers, this implies the need for future investigation in non-tumor liver diseases, which is nevertheless challenging due to the dynamic regulation of Wnt/β-catenin signaling mediated by various etiological factors at different stages.
Moreover, current studies of molecules targeting components involved in Wnt/β-catenin signaling rarely consider genetic mutation or related molecular alterations. In this regard, we tested the PORCN inhibitor [128] and tankyrase inhibitor (manuscript in preparation) in HCC cell lines, some of which carry CTNNB1 or AXIN1 mutations. Apparently, Wnt/β-catenin signaling activity responds to these inhibitors differently depending on specific genetic defects. Despite a reduction in the signaling activity, it is not sufficient to significantly affect cell growth. These results highlight the importance of identifying the molecular features and genomic traits of liver cancer patients as well as the demand for a combined therapy to improve clinical treatment.
7. Conclusions
Wnt/β-catenin signaling is aberrantly stimulated during the course of liver cancer progression. The underlying mechanisms range from complicated regulation by etiological factors in precancerous lesions at early stages to acquired genomic, epigenetic and transcriptional alterations of the components involved in Wnt/β-catenin signaling in tumor foci at later stages. Therefore, targeting Wnt/β-catenin signaling potentiates a novel avenue to treat liver cancers as well as non-tumor liver diseases. However, application of molecular inhibitors targeting Wnt/β-catenin signaling for liver cancer treatment remains dim. A deeper study to explore the sensitive subgroups to these inhibitors carrying particular molecular features would aid in designing more efficient treatment strategies. Additionally, investigations targeting Wnt/β-catenin signaling in non-tumor liver diseases are still lacking, which demonstrate the need for further studies in this field.
Abbreviations
| HCC | Hepatocellular carcinoma |
| CCA | Cholangiocarcinoma |
| HB | Hepatoblastoma |
| HBV | Hepatitis B virus |
| HCV | Hepatitis C virus |
| FAP | Familial adenomatous polyposis |
| NAFLD | Non-alcoholic fatty liver disease |
| NASH | Obesity-induced non-alcoholic steatohepatitis |
| ER | Endoplasmic reticulum |
| PORCN | Wnt acyl-transferase porcupine |
| SFRP | Secreted frizzled-related protein |
| WIF | Wnt inhibitory factor |
| LRP | Low-density lipoprotein receptor-related protein |
| APC | Adenomatous polyposis coli |
| β-TRCP | β-transducin repeat containing protein |
| CRD | Cysteine rich domain |
| FZD | Frizzled |
| DVL | Disheveled |
| PAR | Poly-ADP-ribosylation |
| TNKS | Tankyrase |
| TCF/LEF | T-cell factor/lymphoid enhancer-binding factor |
| TLE | Transducin-like enhancer of split |
| HDAC | Histone deacetylase |
| HBx | Hepatitis B viral X protein |
| HBsAg | Hepatitis B surface antigen |
| LINE | Long interspersed nuclear element |
| SHP-2 | Src homology region 2 domain-containing phosphatase-2 |
| EGFR | Epidermal growth factor receptor |
| FGF | Fibroblast growth factor |
| DEN | Diethylnitrosamine |
| PPARγ | Peroxisome proliferator-activated receptor γ |
| ACLP | Aortic carboxypeptidase-like protein |
| CRC | Colorectal cancer |
Funding
This research was supported by the National Natural Science Foundation of China (81670425), Jiangsu Specially-Appointed Professors Program, the Jiangsu Innovative and Entrepreneurial Program, the ‘‘Double First Class’’ University Project of China Pharmaceutical University (CPU2018GF04), and the Open Project of the State Key Laboratory of Natural Medicines of China Pharmaceutical University (3144060173) through funding awarded to Chaoyong He, as well as the Fundamental Research Funds for the Central Universities (3011900173) through funding awarded to Wenhui Wang.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Farazi P.A., DePinho R.A. Hepatocellular carcinoma pathogenesis: From genes to environment. Nat. Rev. Cancer. 2006;6:674–687. doi: 10.1038/nrc1934. [DOI] [PubMed] [Google Scholar]
- 2.Razumilava N., Gores G.J. Cholangiocarcinoma. Lancet. 2014;383:2168–2179. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Darbari A., Sabin K.M., Shapiro C.N., Schwarz K.B. Epidemiology of primary hepatic malignancies in U.S. children. Hepatology. 2003;38:560–566. doi: 10.1053/jhep.2003.50375. [DOI] [PubMed] [Google Scholar]
- 4.Aretz S., Koch A., Uhlhaas S., Friedl W., Propping P., von Schweinitz D., Pietsch T. Should children at risk for familial adenomatous polyposis be screened for hepatoblastoma and children with apparently sporadic hepatoblastoma be screened for APC germline mutations? Pediatr. Blood Cancer. 2006;47:811–818. doi: 10.1002/pbc.20698. [DOI] [PubMed] [Google Scholar]
- 5.Qu B., Liu B.R., Du Y.J., Chen J., Cheng Y.Q., Xu W., Wang X.H. Wnt/β-catenin signaling pathway may regulate the expression of angiogenic growth factors in hepatocellular carcinoma. Oncol. Lett. 2014;7:1175–1178. doi: 10.3892/ol.2014.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anastas J.N., Moon R.T. WNT signalling pathways as therapeutic targets in cancer. Nat. Rev. Cancer. 2012;13:11–26. doi: 10.1038/nrc3419. [DOI] [PubMed] [Google Scholar]
- 7.Klaus A., Birchmeier W. Wnt signalling and its impact on development and cancer. Nat. Rev. Cancer. 2008;8:387–398. doi: 10.1038/nrc2389. [DOI] [PubMed] [Google Scholar]
- 8.Wang W., Pan Q., Fuhler G.M., Smits R., Peppelenbosch M.P. Action and function of Wnt/beta-catenin signaling in the progression from chronic hepatitis C to hepatocellular carcinoma. J. Gastroenterol. 2017;52:419–431. doi: 10.1007/s00535-016-1299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peifer M., Polakis P. Wnt signaling in oncogenesis and embryogenesis—A look outside the nucleus. Science. 2000;287:1606–1609. doi: 10.1126/science.287.5458.1606. [DOI] [PubMed] [Google Scholar]
- 10.Dahmani R., Just P.A., Perret C. The Wnt/beta-catenin pathway as a therapeutic target in human hepatocellular carcinoma. Clin. Res. Hepatol. Gastroenterol. 2011;35:709–713. doi: 10.1016/j.clinre.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Liu X., Zhang B., McBride J.D., Zhou K., Lee K., Zhou Y., Liu Z., Ma J.X. Antiangiogenic and antineuroinflammatory effects of kallistatin through interactions with the canonical Wnt pathway. Diabetes. 2013;62:4228–4238. doi: 10.2337/db12-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hart M., Concordet J.P., Lassot I., Albert I., del los Santos R., Durand H., Perret C., Rubinfeld B., Margottin F., Benarous R., et al. The F-box protein beta-TrCP associates with phosphorylated beta-catenin and regulates its activity in the cell. Curr. Biol. 1999;9:207–210. doi: 10.1016/S0960-9822(99)80091-8. [DOI] [PubMed] [Google Scholar]
- 13.Zhong Y., Katavolos P., Nguyen T., Lau T., Boggs J., Sambrone A., Kan D., Merchant M., Harstad E., Diaz D., et al. Tankyrase Inhibition Causes Reversible Intestinal Toxicity in Mice with a Therapeutic Index <1. Toxicol. Pathol. 2016;44:267–278. doi: 10.1177/0192623315621192. [DOI] [PubMed] [Google Scholar]
- 14.Mariotti L., Pollock K., Guettler S. Regulation of Wnt/beta-catenin signalling by tankyrase-dependent poly(ADP-ribosyl)ation and scaffolding. Br. J. Pharm. 2017;174:4611–4636. doi: 10.1111/bph.14038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian Y., Mok M.T., Yang P., Cheng A.S. Epigenetic Activation of Wnt/beta-Catenin Signaling in NAFLD-Associated Hepatocarcinogenesis. Cancers (Basel) 2016;8:76. doi: 10.3390/cancers8080076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma M., Jamieson C., Johnson M., Molloy M.P., Henderson B.R. Specific armadillo repeat sequences facilitate beta-catenin nuclear transport in live cells via direct binding to nucleoporins Nup62, Nup153, and RanBP2/Nup358. J. Biol. Chem. 2012;287:819–831. doi: 10.1074/jbc.M111.299099. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Ma L., Wei W., Chua M.-S., So S. WNT/β-catenin pathway activation in hepatocellular carcinoma: A clinical perspective. Gastrointest. Cancer Targets Ther. 2014;4:49–63. doi: 10.2147/GICTT.S44256. [DOI] [Google Scholar]
- 18.Lau C.C., Sun T., Ching A.K., He M., Li J.W., Wong A.M., Co N.N., Chan A.W., Li P.S., Lung R.W., et al. Viral-human chimeric transcript predisposes risk to liver cancer development and progression. Cancer Cell. 2014;25:335–349. doi: 10.1016/j.ccr.2014.01.030. [DOI] [PubMed] [Google Scholar]
- 19.Tiollais P., Pourcel C., Dejean A. The hepatitis B virus. Nature. 1985;317:489–495. doi: 10.1038/317489a0. [DOI] [PubMed] [Google Scholar]
- 20.Xie Q., Chen L., Shan X., Shan X., Tang J., Zhou F., Chen Q., Quan H., Nie D., Zhang W., et al. Epigenetic silencing of SFRP1 and SFRP5 by hepatitis B virus X protein enhances hepatoma cell tumorigenicity through Wnt signaling pathway. Int. J. Cancer. 2014;135:635–646. doi: 10.1002/ijc.28697. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh A., Kim H.S., Lim S.O., Yu D.Y., Jung G. Hepatitis B viral X protein interacts with tumor suppressor adenomatous polyposis coli to activate Wnt/beta-catenin signaling. Cancer Lett. 2011;300:162–172. doi: 10.1016/j.canlet.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Cha M.Y., Kim C.M., Park Y.M., Ryu W.S. Hepatitis B virus X protein is essential for the activation of Wnt/beta-catenin signaling in hepatoma cells. Hepatology. 2004;39:1683–1693. doi: 10.1002/hep.20245. [DOI] [PubMed] [Google Scholar]
- 23.Yu Z., Gao Y.Q., Feng H., Lee Y.Y., Li M.S., Tian Y., Go M.Y., Yu D.Y., Cheung Y.S., Lai P.B., et al. Cell cycle-related kinase mediates viral-host signalling to promote hepatitis B virus-associated hepatocarcinogenesis. Gut. 2014;63:1793–1804. doi: 10.1136/gutjnl-2013-305584. [DOI] [PubMed] [Google Scholar]
- 24.Daud M., Rana M.A., Husnain T., Ijaz B. Modulation of Wnt signaling pathway by hepatitis B virus. Arch. Virol. 2017;162:2937–2947. doi: 10.1007/s00705-017-3462-6. [DOI] [PubMed] [Google Scholar]
- 25.Tian X., Zhao C., Ren J., Ma Z.M., Xie Y.H., Wen Y.M. Gene-expression profiles of a hepatitis B small surface antigen-secreting cell line reveal upregulation of lymphoid enhancer-binding factor 1. J. Gen. Virol. 2007;88:2966–2976. doi: 10.1099/vir.0.83108-0. [DOI] [PubMed] [Google Scholar]
- 26.Tian X., Li J., Ma Z.M., Zhao C., Wan D.F., Wen Y.M. Role of hepatitis B surface antigen in the development of hepatocellular carcinoma: Regulation of lymphoid enhancer-binding factor 1. J. Exp. Clin. Cancer Res. 2009;28:58. doi: 10.1186/1756-9966-28-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niknafs Y.S., Chinnaiyan A.M. RNA identity crisis: Hepatitis B walks the LINE. Cancer Cell. 2014;25:259–260. doi: 10.1016/j.ccr.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 28.Budzinska M.A., Shackel N.A., Urban S., Tu T. Cellular Genomic Sites of Hepatitis B Virus DNA Integration. Genes (Basel) 2018;9:365. doi: 10.3390/genes9070365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao Q., Imbeaud S., Datta S., Zucman-Rossi J. Authors’ response: Virus-host interactions in HBV-related hepatocellular carcinoma: More to be revealed? Gut. 2015;64:853–854. doi: 10.1136/gutjnl-2014-308482. [DOI] [PubMed] [Google Scholar]
- 30.Lin M.V., King L.Y., Chung R.T. Hepatitis C virus-associated cancer. Annu. Rev. Pathol. 2015;10:345–370. doi: 10.1146/annurev-pathol-012414-040323. [DOI] [PubMed] [Google Scholar]
- 31.McLauchlan J. Properties of the hepatitis C virus core protein: A structural protein that modulates cellular processes. J. Viral. Hepat. 2000;7:2–14. doi: 10.1046/j.1365-2893.2000.00201.x. [DOI] [PubMed] [Google Scholar]
- 32.Ray R.B., Ray R. Hepatitis C virus core protein: Intriguing properties and functional relevance. FEMS Microbiol. Lett. 2001;202:149–156. doi: 10.1111/j.1574-6968.2001.tb10796.x. [DOI] [PubMed] [Google Scholar]
- 33.Fukutomi T., Zhou Y., Kawai S., Eguchi H., Wands J.R., Li J. Hepatitis C virus core protein stimulates hepatocyte growth: Correlation with upregulation of wnt-1 expression. Hepatology. 2005;41:1096–1105. doi: 10.1002/hep.20668. [DOI] [PubMed] [Google Scholar]
- 34.Liu J., Ding X., Tang J., Cao Y., Hu P., Zhou F., Shan X., Cai X., Chen Q., Ling N. Enhancement of canonical Wnt/β-catenin signaling activity by HCV core protein promotes cell growth of hepatocellular carcinoma cells. PLoS ONE. 2011;6:e27496. doi: 10.1371/journal.pone.0027496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Umer M., Qureshi S.A., Hashmi Z.Y., Raza A., Ahmad J., Rahman M., Iqbal M. Promoter hypermethylation of Wnt pathway inhibitors in hepatitis C virus-induced multistep hepatocarcinogenesis. Virol. J. 2014;11:117. doi: 10.1186/1743-422X-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quan H., Zhou F., Nie D., Chen Q., Cai X., Shan X., Zhou Z., Chen K., Huang A., Li S. Hepatitis C virus core protein epigenetically silences SFRP1 and enhances HCC aggressiveness by inducing epithelial—mesenchymal transition. Oncogene. 2014;33:2826–2835. doi: 10.1038/onc.2013.225. [DOI] [PubMed] [Google Scholar]
- 37.Ripoli M., Barbano R., Balsamo T., Piccoli C., Brunetti V., Coco M., Mazzoccoli G., Vinciguerra M., Pazienza V. Hypermethylated levels of E-cadherin promoter in Huh-7 cells expressing the HCV core protein. Virus Res. 2011;160:74–81. doi: 10.1016/j.virusres.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 38.Sawey E.T., Chanrion M., Cai C., Wu G., Zhang J., Zender L., Zhao A., Busuttil R.W., Yee H., Stein L. Identification of a therapeutic strategy targeting amplified FGF19 in liver cancer by Oncogenomic screening. Cancer Cell. 2011;19:347–358. doi: 10.1016/j.ccr.2011.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park C.Y., Choi S.H., Kang S.M., Kang J.I., Ahn B.Y., Kim H., Jung G., Choi K.Y., Hwang S.B. Nonstructural 5A protein activates beta-catenin signaling cascades: Implication of hepatitis C virus-induced liver pathogenesis. J. Hepatol. 2009;51:853–864. doi: 10.1016/j.jhep.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 40.Street A., Macdonald A., Crowder K., Harris M. The Hepatitis C virus NS5A protein activates a phosphoinositide 3-kinase-dependent survival signaling cascade. J. Biol. Chem. 2004;279:12232–12241. doi: 10.1074/jbc.M312245200. [DOI] [PubMed] [Google Scholar]
- 41.Macdonald A., Harris M. Hepatitis C virus NS5A: Tales of a promiscuous protein. J. Gen. Virol. 2004;85:2485–2502. doi: 10.1099/vir.0.80204-0. [DOI] [PubMed] [Google Scholar]
- 42.Street A., Macdonald A., McCormick C., Harris M. Hepatitis C virus NS5A-mediated activation of phosphoinositide 3-kinase results in stabilization of cellular β-catenin and stimulation of β-catenin-responsive transcription. J. Virol. 2005;79:5006–5016. doi: 10.1128/JVI.79.8.5006-5016.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Balasubramanian A., Ganju R.K., Groopman J.E. Hepatitis C virus and HIV envelope proteins collaboratively mediate interleukin-8 secretion through activation of p38 MAP kinase and SHP2 in hepatocytes. J. Biol. Chem. 2003;278:35755–35766. doi: 10.1074/jbc.M302889200. [DOI] [PubMed] [Google Scholar]
- 44.Takahashi A., Tsutsumi R., Kikuchi I., Obuse C., Saito Y., Seidi A., Karisch R., Fernandez M., Cho T., Ohnishi N. SHP2 tyrosine phosphatase converts parafibromin/Cdc73 from a tumor suppressor to an oncogenic driver. Mol. Cell. 2011;43:45–56. doi: 10.1016/j.molcel.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y., Wei W., Cheng N., Wang K., Li B., Jiang X., Sun S. Hepatitis C virus-induced up-regulation of microRNA-155 promotes hepatocarcinogenesis by activating Wnt signaling. Hepatology. 2012;56:1631–1640. doi: 10.1002/hep.25849. [DOI] [PubMed] [Google Scholar]
- 46.Israsena N., Hu M., Fu W., Kan L., Kessler J.A. The presence of FGF2 signaling determines whether β-catenin exerts effects on proliferation or neuronal differentiation of neural stem cells. Dev. Biol. 2004;268:220–231. doi: 10.1016/j.ydbio.2003.12.024. [DOI] [PubMed] [Google Scholar]
- 47.Igloi Z., Kazlauskas A., Saksela K., Macdonald A., Mankouri J., Harris M. The hepatitis C virus NS5A protein blocks EGFR degradation via a proline motif dependent interaction. J. Gen. Virol. 2015;96:2133–2144. doi: 10.1099/vir.0.000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Civenni G., Holbro T., Hynes N.E. Wnt1 and Wnt5a induce cyclin D1 expression through ErbB1 transactivation in HC11 mammary epithelial cells. EMBO Rep. 2003;4:166–171. doi: 10.1038/sj.embor.embor735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Meyer K., Kwon Y.-C., Liu S., Hagedorn C.H., Ray R.B., Ray R. Interferon-α inducible protein 6 impairs EGFR activation by CD81 and inhibits hepatitis C virus infection. Sci. Rep. 2015;5:9012. doi: 10.1038/srep09012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Diao J., Pantua H., Ngu H., Komuves L., Diehl L., Schaefer G., Kapadia S.B. Hepatitis C virus induces epidermal growth factor receptor activation via CD81 binding for viral internalization and entry. J. Virol. 2012;86:10935–10949. doi: 10.1128/JVI.00750-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Katoh M., Katoh M. Review Cross-talk of WNT and FGF Signaling Pathways at GSK3β to Regulate β-Catenin and SNAIL Signaling Cascades. Cancer Biol. Ther. 2006;5:1059–1064. doi: 10.4161/cbt.5.9.3151. [DOI] [PubMed] [Google Scholar]
- 52.Van N.D., Falk C.S., Vondran F.W., Helfritz F., Wedemeyer H., Manns M.P., Ciesek S., von Hahn T. Modulation of HCV reinfection after orthotopic liver transplantation by fibroblast growth factor-2 and other non-interferon mediators. Gut. 2015;65:1015–1023. doi: 10.1136/gutjnl-2014-308003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang C.K., Yu T., de la Monte S.M., Wands J.R., Derdak Z., Kim M. Restoration of Wnt/beta-catenin signaling attenuates alcoholic liver disease progression in a rat model. J. Hepatol. 2015;63:191–198. doi: 10.1016/j.jhep.2015.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu C.Q., de la Monte S.M., Tong M., Huang C.K., Kim M. Chronic Ethanol-Induced Impairment of Wnt/beta-Catenin Signaling is Attenuated by PPAR-delta Agonist. Alcohol. Clin. Exp. Res. 2015;39:969–979. doi: 10.1111/acer.12727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Behari J., Sylvester K.G. Role of the Wnt/beta-Catenin Pathway in the Pathogenesis of Alcoholic Liver Disease. Curr. Mol. Pharm. 2017;10:186–194. doi: 10.2174/1874467208666150817111256. [DOI] [PubMed] [Google Scholar]
- 56.Liu S., Yeh T.H., Singh V.P., Shiva S., Krauland L., Li H., Zhang P., Kharbanda K., Ritov V., Monga S.P., et al. Beta-catenin is essential for ethanol metabolism and protection against alcohol-mediated liver steatosis in mice. Hepatology. 2012;55:931–940. doi: 10.1002/hep.24766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lehwald N., Tao G.Z., Jang K.Y., Papandreou I., Liu B., Liu B., Pysz M.A., Willmann J.K., Knoefel W.T., Denko N.C., et al. Beta-Catenin regulates hepatic mitochondrial function and energy balance in mice. Gastroenterology. 2012;143:754–764. doi: 10.1053/j.gastro.2012.05.048. [DOI] [PubMed] [Google Scholar]
- 58.Mercer K.E., Hennings L., Ronis M.J. Alcohol consumption, Wnt/beta-catenin signaling, and hepatocarcinogenesis. Adv. Exp. Med. Biol. 2015;815:185–195. doi: 10.1007/978-3-319-09614-8_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lai K.K.Y., Kweon S.M., Chi F., Hwang E., Kabe Y., Higashiyama R., Qin L., Yan R., Wu R.P., Lai K., et al. Stearoyl-CoA Desaturase Promotes Liver Fibrosis and Tumor Development in Mice via a Wnt Positive-Signaling Loop by Stabilization of Low-Density Lipoprotein-Receptor-Related Proteins 5 and 6. Gastroenterology. 2017;152:1477–1491. doi: 10.1053/j.gastro.2017.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bhala N., Angulo P., van der Poorten D., Lee E., Hui J.M., Saracco G., Adams L.A., Charatcharoenwitthaya P., Topping J.H., Bugianesi E., et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: An international collaborative study. Hepatology. 2011;54:1208–1216. doi: 10.1002/hep.24491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takada I., Kouzmenko A.P., Kato S. Wnt and PPARgamma signaling in osteoblastogenesis and adipogenesis. Nat. Rev. Rheumatol. 2009;5:442–447. doi: 10.1038/nrrheum.2009.137. [DOI] [PubMed] [Google Scholar]
- 62.Ross S.E., Hemati N., Longo K.A., Bennett C.N., Lucas P.C., Erickson R.L., MacDougald O.A. Inhibition of adipogenesis by Wnt signaling. Science. 2000;289:950–953. doi: 10.1126/science.289.5481.950. [DOI] [PubMed] [Google Scholar]
- 63.Go G.W., Srivastava R., Hernandez-Ono A., Gang G., Smith S.B., Booth C.J., Ginsberg H.N., Mani A. The combined hyperlipidemia caused by impaired Wnt-LRP6 signaling is reversed by Wnt3a rescue. Cell Metab. 2014;19:209–220. doi: 10.1016/j.cmet.2013.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Go G.W. Low-Density Lipoprotein Receptor-Related Protein 6 (LRP6) Is a Novel Nutritional Therapeutic Target for Hyperlipidemia, Non-Alcoholic Fatty Liver Disease, and Atherosclerosis. Nutrients. 2015;7:4453–4464. doi: 10.3390/nu7064453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang S., Song K., Srivastava R., Dong C., Go G.W., Li N., Iwakiri Y., Mani A. Nonalcoholic fatty liver disease induced by noncanonical Wnt and its rescue by Wnt3a. FASEB J. 2015;29:3436–3445. doi: 10.1096/fj.15-271171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Teratani T., Tomita K., Suzuki T., Furuhashi H., Irie R., Nishikawa M., Yamamoto J., Hibi T., Miura S., Minamino T., et al. Aortic carboxypeptidase-like protein, a WNT ligand, exacerbates nonalcoholic steatohepatitis. J. Clin. Invest. 2018;128:1581–1596. doi: 10.1172/JCI92863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Debebe A., Medina V., Chen C.Y., Mahajan I.M., Jia C., Fu D., He L., Zeng N., Stiles B.W., Chen C.L., et al. Wnt/beta-catenin activation and macrophage induction during liver cancer development following steatosis. Oncogene. 2017;36:6020–6029. doi: 10.1038/onc.2017.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tian Y., Wong V.W., Wong G.L., Yang W., Sun H., Shen J., Tong J.H., Go M.Y., Cheung Y.S., Lai P.B., et al. Histone Deacetylase HDAC8 Promotes Insulin Resistance and beta-Catenin Activation in NAFLD-Associated Hepatocellular Carcinoma. Cancer Res. 2015;75:4803–4816. doi: 10.1158/0008-5472.CAN-14-3786. [DOI] [PubMed] [Google Scholar]
- 69.Rushing B.R., Selim M.I. Aflatoxin B1: A review on metabolism, toxicity, occurrence in food, occupational exposure, and detoxification methods. Food Chem. Toxicol. 2019;124:81–100. doi: 10.1016/j.fct.2018.11.047. [DOI] [PubMed] [Google Scholar]
- 70.Hussain S.P., Schwank J., Staib F., Wang X.W., Harris C.C. TP53 mutations and hepatocellular carcinoma: Insights into the etiology and pathogenesis of liver cancer. Oncogene. 2007;26:2166–2176. doi: 10.1038/sj.onc.1210279. [DOI] [PubMed] [Google Scholar]
- 71.Fang Y., Feng Y., Wu T., Srinivas S., Yang W., Fan J., Yang C., Wang S. Aflatoxin B1 negatively regulates Wnt/beta-catenin signaling pathway through activating miR-33a. PLoS ONE. 2013;8:e73004. doi: 10.1371/journal.pone.0073004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhu L., Gao J., Huang K., Luo Y., Zhang B., Xu W. miR-34a screened by miRNA profiling negatively regulates Wnt/beta-catenin signaling pathway in Aflatoxin B1 induced hepatotoxicity. Sci. Rep. 2015;5:16732. doi: 10.1038/srep16732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Devereux T.R., Stern M.C., Flake G.P., Yu M.C., Zhang Z.Q., London S.J., Taylor J.A. CTNNB1 mutations and beta-catenin protein accumulation in human hepatocellular carcinomas associated with high exposure to aflatoxin B1. Mol. Carcinog. 2001;31:68–73. doi: 10.1002/mc.1041. [DOI] [PubMed] [Google Scholar]
- 74.Nhieu J.T., Renard C.A., Wei Y., Cherqui D., Zafrani E.S., Buendia M.A. Nuclear accumulation of mutated beta-catenin in hepatocellular carcinoma is associated with increased cell proliferation. Am. J. Pathol. 1999;155:703–710. doi: 10.1016/S0002-9440(10)65168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lachenmayer A., Alsinet C., Savic R., Cabellos L., Toffanin S., Hoshida Y., Villanueva A., Minguez B., Newell P., Tsai H.W., et al. Wnt-pathway activation in two molecular classes of hepatocellular carcinoma and experimental modulation by sorafenib. Clin. Cancer Res. 2012;18:4997–5007. doi: 10.1158/1078-0432.CCR-11-2322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wong C.M., Fan S.T., Ng I.O. beta-Catenin mutation and overexpression in hepatocellular carcinoma: Clinicopathologic and prognostic significance. Cancer. 2001;92:136–145. doi: 10.1002/1097-0142(20010701)92:1<136::AID-CNCR1301>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 77.Lin Y.T., Chao C.C. Identification of the beta-catenin/JNK/prothymosin-alpha axis as a novel target of sorafenib in hepatocellular carcinoma cells. Oncotarget. 2015;6:38999–39017. doi: 10.18632/oncotarget.5738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Laurent-Puig P., Zucman-Rossi J. Genetics of hepatocellular tumors. Oncogene. 2006;25:3778–3786. doi: 10.1038/sj.onc.1209547. [DOI] [PubMed] [Google Scholar]
- 79.Fujimoto A., Totoki Y., Abe T., Boroevich K.A., Hosoda F., Nguyen H.H., Aoki M., Hosono N., Kubo M., Miya F., et al. Whole-genome sequencing of liver cancers identifies etiological influences on mutation patterns and recurrent mutations in chromatin regulators. Nat. Genet. 2012;44:760–764. doi: 10.1038/ng.2291. [DOI] [PubMed] [Google Scholar]
- 80.Monga S.P. beta-Catenin Signaling and Roles in Liver Homeostasis, Injury, and Tumorigenesis. Gastroenterology. 2015;148:1294–1310. doi: 10.1053/j.gastro.2015.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bruix J., Han K.H., Gores G., Llovet J.M., Mazzaferro V. Liver cancer: Approaching a personalized care. J. Hepatol. 2015;62:S144–S156. doi: 10.1016/j.jhep.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perugorria M.J., Olaizola P., Labiano I., Esparza-Baquer A., Marzioni M., Marin J.J.G., Bujanda L., Banales J.M. Wnt-beta-catenin signalling in liver development, health and disease. Nat. Rev. Gastroenterol. Hepatol. 2019;16:121–136. doi: 10.1038/s41575-018-0075-9. [DOI] [PubMed] [Google Scholar]
- 83.Kim E., Lisby A., Ma C., Lo N., Ehmer U., Hayer K.E., Furth E.E., Viatour P. Promotion of growth factor signaling as a critical function of beta-catenin during HCC progression. Nat. Commun. 2019;10:1909. doi: 10.1038/s41467-019-09780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fodde R., Smits R., Clevers H. APC, signal transduction and genetic instability in colorectal cancer. Nat. Rev. Cancer. 2001;1:55–67. doi: 10.1038/35094067. [DOI] [PubMed] [Google Scholar]
- 85.Pez F., Lopez A., Kim M., Wands J.R., Caron de Fromentel C., Merle P. Wnt signaling and hepatocarcinogenesis: Molecular targets for the development of innovative anticancer drugs. J. Hepatol. 2013;59:1107–1117. doi: 10.1016/j.jhep.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 86.Zhi X., Lin L., Yang S., Bhuvaneshwar K., Wang H., Gusev Y., Lee M.H., Kallakury B., Shivapurkar N., Cahn K., et al. betaII-Spectrin (SPTBN1) suppresses progression of hepatocellular carcinoma and Wnt signaling by regulation of Wnt inhibitor kallistatin. Hepatology. 2015;61:598–612. doi: 10.1002/hep.27558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chai S., Ng K.Y., Tong M., Lau E.Y., Lee T.K., Chan K.W., Yuan Y.F., Cheung T.T., Cheung S.T., Wang X.Q., et al. Octamer 4/microRNA-1246 signaling axis drives Wnt/beta-catenin activation in liver cancer stem cells. Hepatology. 2016;64:2062–2076. doi: 10.1002/hep.28821. [DOI] [PubMed] [Google Scholar]
- 88.Jain S., Chang T.T., Hamilton J.P., Lin S.Y., Lin Y.J., Evans A.A., Selaru F.M., Lin P.W., Chen S.H., Block T.M., et al. Methylation of the CpG sites only on the sense strand of the APC gene is specific for hepatocellular carcinoma. PLoS ONE. 2011;6:e26799. doi: 10.1371/journal.pone.0026799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Loilome W., Bungkanjana P., Techasen A., Namwat N., Yongvanit P., Puapairoj A., Khuntikeo N., Riggins G.J. Activated macrophages promote Wnt/beta-catenin signaling in cholangiocarcinoma cells. Tumour Biol. 2014;35:5357–5367. doi: 10.1007/s13277-014-1698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Boulter L., Guest R.V., Kendall T.J., Wilson D.H., Wojtacha D., Robson A.J., Ridgway R.A., Samuel K., Van Rooijen N., Barry S.T., et al. WNT signaling drives cholangiocarcinoma growth and can be pharmacologically inhibited. J. Clin. Invest. 2015;125:1269–1285. doi: 10.1172/JCI76452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Goeppert B., Konermann C., Schmidt C.R., Bogatyrova O., Geiselhart L., Ernst C., Gu L., Becker N., Zucknick M., Mehrabi A., et al. Global alterations of DNA methylation in cholangiocarcinoma target the Wnt signaling pathway. Hepatology. 2014;59:544–554. doi: 10.1002/hep.26721. [DOI] [PubMed] [Google Scholar]
- 92.Zhang F., Wan M., Xu Y., Li Z., Leng K., Kang P., Cui Y., Jiang X. Long noncoding RNA PCAT1 regulates extrahepatic cholangiocarcinoma progression via the Wnt/beta-catenin-signaling pathway. Biomed Pharm. 2017;94:55–62. doi: 10.1016/j.biopha.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 93.Huang G.L., Luo Q., Rui G., Zhang W., Zhang Q.Y., Chen Q.X., Shen D.Y. Oncogenic activity of retinoic acid receptor gamma is exhibited through activation of the Akt/NF-kappaB and Wnt/beta-catenin pathways in cholangiocarcinoma. Mol. Cell. Biol. 2013;33:3416–3425. doi: 10.1128/MCB.00384-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Merino-Azpitarte M., Lozano E., Perugorria M.J., Esparza-Baquer A., Erice O., Santos-Laso A., O’Rourke C.J., Andersen J.B., Jimenez-Aguero R., Lacasta A., et al. SOX17 regulates cholangiocyte differentiation and acts as a tumor suppressor in cholangiocarcinoma. J. Hepatol. 2017;67:72–83. doi: 10.1016/j.jhep.2017.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang J., Zhang K., Wang J., Wu X., Liu X., Li B., Zhu Y., Yu Y., Cheng Q., Hu Z., et al. Underexpression of LKB1 tumor suppressor is associated with enhanced Wnt signaling and malignant characteristics of human intrahepatic cholangiocarcinoma. Oncotarget. 2015;6:18905–18920. doi: 10.18632/oncotarget.4305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Russell J.O., Monga S.P. Wnt/beta-Catenin Signaling in Liver Development, Homeostasis, and Pathobiology. Annu. Rev. Pathol. 2018;13:351–378. doi: 10.1146/annurev-pathol-020117-044010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dubbink H.J., Hollink I., Avenca Valente C., Wang W., Liu P., Doukas M., van Noesel M.M., Dinjens W.N.M., Wagner A., Smits R. A novel tissue-based ss-catenin gene and immunohistochemical analysis to exclude familial adenomatous polyposis among children with hepatoblastoma tumors. Pediatr. Blood Cancer. 2018;65:e26991. doi: 10.1002/pbc.26991. [DOI] [PubMed] [Google Scholar]
- 98.Adebayo Michael A.O., Ko S., Tao J., Moghe A., Yang H., Xu M., Russell J.O., Pradhan-Sundd T., Liu S., Singh S., et al. Inhibiting Glutamine-Dependent mTORC1 Activation Ameliorates Liver Cancers Driven by beta-Catenin Mutations. Cell Metab. 2019;29:1135–1150. doi: 10.1016/j.cmet.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wei W., Chua M.S., Grepper S., So S.K. Soluble Frizzled-7 receptor inhibits Wnt signaling and sensitizes hepatocellular carcinoma cells towards doxorubicin. Mol. Cancer. 2011;10:16. doi: 10.1186/1476-4598-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jimeno A., Gordon M., Chugh R., Messersmith W., Mendelson D., Dupont J., Stagg R., Kapoun A.M., Xu L., Uttamsingh S., et al. A First-in-Human Phase I Study of the Anticancer Stem Cell Agent Ipafricept (OMP-54F28), a Decoy Receptor for Wnt Ligands, in Patients with Advanced Solid Tumors. Clin. Cancer Res. 2017;23:7490–7497. doi: 10.1158/1078-0432.CCR-17-2157. [DOI] [PubMed] [Google Scholar]
- 101.Dose Escalation Study of OMP-54F28 in Combination with Sorafenib in Patients With Hepatocellular Cancer. [(accessed on 24 February 2014)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02069145.
- 102.A Dose Escalation Study of OMP-54F28 in Subjects with Solid Tumors. [(accessed on 31 May 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01608867.
- 103.Dose Escalation Study of OMP-54F28 in Combination With Paclitaxel and Carboplatin in Patients With Recurrent Platinum-Sensitive Ovarian Cancer. [(accessed on 20 March 2014)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02092363.
- 104.Dose Escalation Study of OMP-54F28 in Combination With Nab-Paclitaxel and Gemcitabine in Patients with Previously Untreated Stage IV Pancreatic Cancer. [(accessed on 30 January 2014)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02050178.
- 105.Arafat K., Iratni R., Takahashi T., Parekh K., Al Dhaheri Y., Adrian T.E., Attoub S. Inhibitory Effects of Salinomycin on Cell Survival, Colony Growth, Migration, and Invasion of Human Non-Small Cell Lung Cancer A549 and LNM35: Involvement of NAG-1. PLoS ONE. 2013;8:e66931. doi: 10.1371/journal.pone.0066931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lu W., Li Y. Salinomycin suppresses LRP6 expression and inhibits both Wnt/beta-catenin and mTORC1 signaling in breast and prostate cancer cells. J. Cell. Biochem. 2014;115:1799–1807. doi: 10.1002/jcb.24850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mao J., Fan S., Ma W., Fan P., Wang B., Zhang J., Wang H., Tang B., Zhang Q., Yu X., et al. Roles of Wnt/beta-catenin signaling in the gastric cancer stem cells proliferation and salinomycin treatment. Cell Death Dis. 2014;5:e1039. doi: 10.1038/cddis.2013.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tang Q.L., Zhao Z.Q., Li J.C., Liang Y., Yin J.Q., Zou C.Y., Xie X.B., Zeng Y.X., Shen J.N., Kang T., et al. Salinomycin inhibits osteosarcoma by targeting its tumor stem cells. Cancer Lett. 2011;311:113–121. doi: 10.1016/j.canlet.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 109.Wang F., Dai W., Wang Y., Shen M., Chen K., Cheng P., Zhang Y., Wang C., Li J., Zheng Y., et al. The synergistic in vitro and in vivo antitumor effect of combination therapy with salinomycin and 5-fluorouracil against hepatocellular carcinoma. PLoS ONE. 2014;9:e97414. doi: 10.1371/journal.pone.0097414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang F., He L., Dai W.Q., Xu Y.P., Wu D., Lin C.L., Wu S.M., Cheng P., Zhang Y., Shen M., et al. Salinomycin inhibits proliferation and induces apoptosis of human hepatocellular carcinoma cells in vitro and in vivo. PLoS ONE. 2012;7:e50638. doi: 10.1371/journal.pone.0050638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wei W., Chua M.S., Grepper S., So S.K. Blockade of Wnt-1 signaling leads to anti-tumor effects in hepatocellular carcinoma cells. Mol. Cancer. 2009;8:76. doi: 10.1186/1476-4598-8-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.He B., Reguart N., You L., Mazieres J., Xu Z., Lee A.Y., Mikami I., McCormick F., Jablons D.M. Blockade of Wnt-1 signaling induces apoptosis in human colorectal cancer cells containing downstream mutations. Oncogene. 2005;24:3054–3058. doi: 10.1038/sj.onc.1208511. [DOI] [PubMed] [Google Scholar]
- 113.He B., You L., Uematsu K., Xu Z., Lee A.Y., Matsangou M., McCormick F., Jablons D.M. A monoclonal antibody against Wnt-1 induces apoptosis in human cancer cells. Neoplasia. 2004;6:7–14. doi: 10.1016/S1476-5586(04)80048-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mikami I., You L., He B., Xu Z., Batra S., Lee A.Y., Mazieres J., Reguart N., Uematsu K., Koizumi K., et al. Efficacy of Wnt-1 monoclonal antibody in sarcoma cells. BMC Cancer. 2005;5:53. doi: 10.1186/1471-2407-5-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rhee C.S., Sen M., Lu D., Wu C., Leoni L., Rubin J., Corr M., Carson D.A. Wnt and frizzled receptors as potential targets for immunotherapy in head and neck squamous cell carcinomas. Oncogene. 2002;21:6598–6605. doi: 10.1038/sj.onc.1205920. [DOI] [PubMed] [Google Scholar]
- 116.Hu J., Dong A., Fernandez-Ruiz V., Shan J., Kawa M., Martinez-Anso E., Prieto J., Qian C. Blockade of Wnt signaling inhibits angiogenesis and tumor growth in hepatocellular carcinoma. Cancer Res. 2009;69:6951–6959. doi: 10.1158/0008-5472.CAN-09-0541. [DOI] [PubMed] [Google Scholar]
- 117.A Study of DKN-01 in Multiple Myeloma or Advanced Solid Tumors. [(accessed on 24 October 2011)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01457417.
- 118.A Study of DKN-01 and Lenalidomide/Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. [(accessed on 22 October 2012)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01711671.
- 119.A Study of DKN-01 in Combination With Paclitaxel or Pembrolizumab (P102) [(accessed on 17 December 2013)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02013154.
- 120.Study of DKN-01 and Gemcitabine/Cisplatin in Patients with Carcinoma to Primary to the Intra- or Extra-Hepatic Biliary System or Gallbladder. [(accessed on 3 March 2015)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02375880.
- 121.A Study of DKN-01 as a Monotherapy or in Combination With Paclitaxel in Patients with Recurrent Epithelial Endometrial or Epithelial Ovarian Cancer (P204) [(accessed on 10 January 2018)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03395080.
- 122.Bendell J.C., Murphy J.E., Mahalingam D., Halmos B., Sirard C.A., Landau S.B., Ryan D.P. A Phase 1 study of DKN-01, an anti-DKK1 antibody, in combination with paclitaxel (pac) in patients with DKK1 relapsed or refractory esophageal cancer (EC) or gastro-esophageal junction tumors (GEJ) J. Clin. Oncol. 2016;34:111. doi: 10.1200/jco.2016.34.4_suppl.111. [DOI] [Google Scholar]
- 123.DKN-01 Inhibition in Advanced Liver Cancer. [(accessed on 24 August 2018)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03645980.
- 124.Combination of Targeted and Immunotherapy for Advanced Biliary Tract and Esophagogastric Gastric Cancer (DYNAMIC) [(accessed on 28 January 2019)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03818997.
- 125.CGX1321 in Subjects With Advanced Solid Tumors and CGX1321 with Pembrolizumab in Subjects With Advanced GI Tumors (Keynote 596) [(accessed on 5 February 2016)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02675946.
- 126.Phase 1 Dose Escalation Study of CGX1321 in Subjects with Advanced Gastrointestinal Tumors. [(accessed on 25 April 2018)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03507998.
- 127.Li C., Cao J., Zhang N., Tu M., Xu F., Wei S., Chen X., Xu Y. Identification of RSPO2 Fusion Mutations and Target Therapy Using a Porcupine Inhibitor. Sci. Rep. 2018;8:14244. doi: 10.1038/s41598-018-32652-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang W., Xu L., Liu P., Jairam K., Yin Y., Chen K., Sprengers D., Peppelenbosch M.P., Pan Q., Smits R. Blocking Wnt Secretion Reduces Growth of Hepatocellular Carcinoma Cell Lines Mostly Independent of beta-Catenin Signaling. Neoplasia. 2016;18:711–723. doi: 10.1016/j.neo.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ma L., Wang X., Jia T., Wei W., Chua M.S., So S. Tankyrase inhibitors attenuate WNT/beta-catenin signaling and inhibit growth of hepatocellular carcinoma cells. Oncotarget. 2015;6:25390–25401. doi: 10.18632/oncotarget.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gwak J., Lee J.H., Chung Y.H., Song G.Y., Oh S. Small molecule-based promotion of PKCalpha-mediated beta-catenin degradation suppresses the proliferation of CRT-positive cancer cells. PLoS ONE. 2012;7:e46697. doi: 10.1371/journal.pone.0046697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zeng G., Apte U., Cieply B., Singh S., Monga S.P. siRNA-mediated beta-catenin knockdown in human hepatoma cells results in decreased growth and survival. Neoplasia. 2007;9:951–959. doi: 10.1593/neo.07469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Li Y., Rogoff H.A., Keates S., Gao Y., Murikipudi S., Mikule K., Leggett D., Li W., Pardee A.B., Li C.J. Suppression of cancer relapse and metastasis by inhibiting cancer stemness. Proc. Natl. Acad. Sci. USA. 2015;112:1839–1844. doi: 10.1073/pnas.1424171112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Safety and Efficacy Study of PRI-724 in Subjects with Advanced Solid Tumors. [(accessed on 24 February 2011)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01302405.
- 134.Safety and Efficacy Study of PRI-724 in Subjects with Advanced Myeloid Malignancies. [(accessed on 25 May 2012)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01606579.
- 135.Safety and Efficacy Study of PRI-724 Plus Gemcitabine in Subjects with Advanced or Metastatic Pancreatic Adenocarcinoma. [(accessed on 9 January 2013)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01764477.
- 136.An Open Label, Single Arm, Dose Escalation Phase 1 Trial of PRI-724 in Patients with HCV-induced Cirrhosis. [(accessed on 21 July 2014)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02195440.
- 137.Kimura K., Ikoma A., Shibakawa M., Shimoda S., Harada K., Saio M., Imamura J., Osawa Y., Kimura M., Nishikawa K., et al. Safety, Tolerability, and Preliminary Efficacy of the Anti-Fibrotic Small Molecule PRI-724, a CBP/beta-Catenin Inhibitor, in Patients with Hepatitis C Virus-related Cirrhosis: A Single-Center, Open-Label, Dose Escalation Phase 1 Trial. EBioMed. 2017;23:79–87. doi: 10.1016/j.ebiom.2017.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Emami K.H., Nguyen C., Ma H., Kim D.H., Jeong K.W., Eguchi M., Moon R.T., Teo J.L., Kim H.Y., Moon S.H., et al. A small molecule inhibitor of beta-catenin/CREB-binding protein transcription [corrected] Proc. Natl. Acad. Sci. USA. 2004;101:12682–12687. doi: 10.1073/pnas.0404875101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Handeli S., Simon J.A. A small-molecule inhibitor of Tcf/beta-catenin signaling down-regulates PPARgamma and PPARdelta activities. Mol. Cancer. 2008;7:521–529. doi: 10.1158/1535-7163.MCT-07-2063. [DOI] [PubMed] [Google Scholar]
- 140.Wei W., Chua M.S., Grepper S., So S. Small molecule antagonists of Tcf4/beta-catenin complex inhibit the growth of HCC cells in vitro and in vivo. Int. J. Cancer. 2010;126:2426–2436. doi: 10.1002/ijc.24810. [DOI] [PubMed] [Google Scholar]
- 141.Lepourcelet M., Chen Y.N., France D.S., Wang H., Crews P., Petersen F., Bruseo C., Wood A.W., Shivdasani R.A. Small-molecule antagonists of the oncogenic Tcf/beta-catenin protein complex. Cancer Cell. 2004;5:91–102. doi: 10.1016/S1535-6108(03)00334-9. [DOI] [PubMed] [Google Scholar]
- 142.Mologni L., Brussolo S., Ceccon M., Gambacorti-Passerini C. Synergistic effects of combined Wnt/KRAS inhibition in colorectal cancer cells. PLoS ONE. 2012;7:e51449. doi: 10.1371/journal.pone.0051449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Thompson M.D., Dar M.J., Monga S.P. Pegylated interferon alpha targets Wnt signaling by inducing nuclear export of beta-catenin. J. Hepatol. 2011;54:506–512. doi: 10.1016/j.jhep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dhanasekaran R., Nault J.C., Roberts L.R., Zucman-Rossi J. Genomic Medicine and Implications for Hepatocellular Carcinoma Prevention and Therapy. Gastroenterology. 2019;156:492–509. doi: 10.1053/j.gastro.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Calderaro J., Couchy G., Imbeaud S., Amaddeo G., Letouze E., Blanc J.F., Laurent C., Hajji Y., Azoulay D., Bioulac-Sage P., et al. Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J. Hepatol. 2017;67:727–738. doi: 10.1016/j.jhep.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 146.Boyault S., Rickman D.S., de Reynies A., Balabaud C., Rebouissou S., Jeannot E., Herault A., Saric J., Belghiti J., Franco D., et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology. 2007;45:42–52. doi: 10.1002/hep.21467. [DOI] [PubMed] [Google Scholar]