Abstract
Background:
Operating room personnel are at high risk of needlestick injuries (NSIs) and exposure to blood and body fluids.
Objective:
To investigate the predictors of NSIs preventive behaviors during surgery among operating room personnel based on a health belief model (HBM).
Methods:
This cross-sectional study was conducted on 128 operating room personnel in Hamadan, western Iran. Participants were selected, by census sampling, from teaching hospitals, completed a self-reported questionnaire including demographic characteristics, knowledge and HBM constructs.
Results:
The levels of knowledge and perceived self-efficacy for the NSIs preventive behaviors among operating room personnel were not satisfactory. However, the levels of perceived benefits, susceptibility and severity were reported to be relatively good. The results showed that the perceived susceptibility (β ‑0.627) and cues to action (β 0.695) were the most important predictors of the NSIs preventive behaviors.
Conclusion:
The framework of the HBM is useful to predict the NSIs preventive behaviors among operating room personnel.
Keywords: Attitude, Health belief model, Needlestick injuries, Operating room nursing, Occupational exposure
TAKE-HOME MESSAGE
Risk of needlestick injuries (NSIs) and exposure to blood and body fluids (BBFs) in health care worker are high. The prevalence of NSIs is in operating room personnel is higher than other HCWs.
Hepatitis B and C viruses and HIV are the most common and dangerous pathogens that can be transmitted to the HCWs after exposure to BBFs or NSIs.
Considering preventive health behaviors is crucial to HCWs.
The rate of adherence to universal precautions is moderate among the operating room personnel.
Framework of the HBM is useful for the prediction of NSIs preventive behaviors.
Introduction
Health care-associated infections represent a main health issue and cause many in-hospital deaths. These infections can transfer from patients to patients, from patients to health care workers (HCWs), and from HCWs to patients.1,2 Hepatitis B and C viruses and HIV are the most common and dangerous pathogens that can be transmitted to the HCWs after exposure to blood and body fluids (BBFs) or needle stick injuries (NSIs).3-5
High prevalence of the NSIs among the HCWs was reported from Cuba (62.2%) and India (37.5%).6,7 This prevalence was 62 cases per 1000 beds in Japan,8 and 69 per 1000 beds in Germany.9
The prevalence of NSIs is higher in operating room personnel than other HCWs.5,7,8,10-12 In Iran, like other countries, the prevalence of NSIs is relatively high. In Hamadan, western Iran, the prevalence was reported to be 24.1% among HCWs and 44.6% among nurses.13 The prevalence was 47.3% among HCWs, higher among nurses and operating room personnel, in Jahrom, southern Iran.14 The prevalence of NSIs was 44.2%, 55%, and 43.8% among nurses in Saqqez, Ardabil, and Hamadan, respectively.15-17
Development of blood-borne infections is associated with several problems including disease-induced complications, decreased quality of life, and economical burdens due to workplace absence and direct and indirect costs spent on the treatment and follow-up of the associated complications.18-20
Operating room personnel due to the nature of their work are at higher risk of developing NSIs.4,21,22 Not considering psychosocial models in designing analytical studies, particularly lack of paying attention to specific intellectual frameworks in educational planning, would be the reasons why such plannings are failed.23
First developed in the 1950s by social psychologists Hochbaum, Rosenstock and Kegels working in the US Public Health Services, Health Belief Model (HBM) is one of the most frequently used psychological model that attempts to explain and predict health behaviors through focusing on the attitudes and beliefs of individuals (Fig 1). According to the HBM, decision-makers mentally calculate whether the benefits of a change in their behavior outweigh the consequent practical and psychological costs or obstacles. That is, individuals conduct an internal assessment of the net benefits of changing their behavior, and decide whether or not to act. The model identifies four aspects of this assessment: perceived susceptibility to ill-health (risk perception), perceived severity of ill-health, perceived benefits of behavior change, and perceived barriers to taking action.23 This model has been studied for preventive health behaviors;24,25 the efficacy of the HBM has also been confirmed in preventing NSIs.26,27 Given the significance of this issue, we conducted this study to determine the predictors of NSIs preventive behaviors during surgeries among operating room personnel based on HBM.
Figure 1.
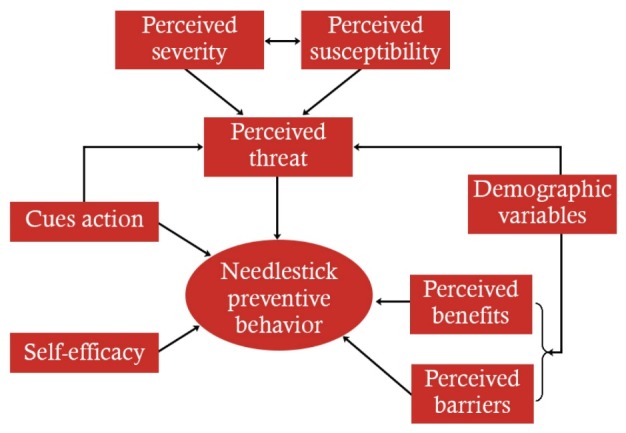
Health Belief Model framework
Materials and Methods
This cross-sectional study was conducted from autumn 2015 to winter 2016 on the operating room personnel of five teaching hospitals in Hamadan, western Iran. The study participants were selected according to census sampling. One-hundred and forty questionnaires were distributed. All operating room personnel who agreed to participate in the study, were included in the study. The study protocol was approved by the Ethics Committee of the Hamadan University of Medical Sciences. The study protocol and purposes were explained to the participants. The participants were ensured that their information would be kept confidential. Informed written consents were taken from all participants,
Data were collected using a self-reported questionnaire. The questionnaire consisted of three sections—demographic characteristics, knowledge, and the HBM constructs.
The demographic and background factors included age, sex, marital status, level of education, and work experience.
The knowledge was assessed by 20 three-choice (“yes,” “no,” and “I don't know”) items on the NSIs preventive behaviors during surgery. An answer of “yes” was scored ‘1,’ otherwise, the response was scored ‘0.’ Therefore, a higher score reflected a higher level of knowledge.
The HBM constructs were assessed by 31 questions rated by a 3-point Likert scale (“I agree,” “I partly agree,” and “I disagree” scored ‘2,’ ‘1,’ and ‘0,’ respectively). The construct perceived susceptibility was assessed by five items, ie, “I may also become infected with blood-borne diseases in the future.” The perceived severity was assessed by eight items, ie, “blood-borne diseases cause disability and inability.” The perceived benefits was assessed by four items, ie, “considering preventive practices for sharp injuries in the operating room causes my health to be promoted.” The perceived barriers was assessed by five items, ie, “considering preventive practices for sharp injuries in operating room is not time-consuming.” The cues to action was evaluated by seven items, ie, “doctors in the operating room help me to take preventive practices of sharps injuries.” And finally, the self-efficacy was assessed by two items, ie, “I'm sure that I can appropriately prevent risks due to sharp instruments in the operating room.”
Adherence to the NSIs preventive behaviors during surgery was measured by 21 items rated by 3-point Likert scale (“always,” “sometimes,” and “never,” scored ‘2,’ ‘1,’ and ‘0,’ respectively).
The items of the questionnaire were developed according to relevant references. Prior to conducting the main project, a pilot study was carried out. Validity of the questionnaire was confirmed using the viewpoints of 10 health education experts. The content validity ratio and content validity index were calculated and confirmed. Furthermore, the questionnaires were initially administered to 40 nurses who were similar to participants in the main study to obtain feedback about the clarity, length comprehensiveness, time of completion, and internal reliability of the measures. The reliability of the questionnaire was investigated by calculating internal consistency; the Cronbach's α was found to be 0.92 for “knowledge,” 0.74 for “perceived susceptibility,” 0.88 for “perceived severity,” 0.83 for “perceived benefits,” 0.87 for “perceived barriers,” 0.73 for “cues to action,” and 0.81 for “self-efficacy.”
Statistical Analysis
Data analysis was done by SPSS® for Windows® ver 20. Descriptive statistics, Pearson correlation coefficient, and linear regression analysis were used. A p <0.05 was considered statistically significant.
Results
Of 140 distributed questionnaires, 12 were excluded because they were not filled out completely. The remaining 128 questionnaires were analyzed, reflecting a response rate of 91.4%.
The mean age of the participants was 29.6 (SD 3.3) years. Most of the participants (66.4%) aged between 21 and 30 years, were female (68.8%) and married (57%); most of the participants had work experience <10 years (75.8%), held a BSc degree (68%), and had been trained in NSIs and blood-borne diseases (60.9%). Forty-seven (36.7%) participants obtained their information on NSIs through attending training courses (Table 1).
| Table 1: Characteristics of the study participants (n=128) | |
| Variables | n (%) |
| Age (yrs) | |
| 20–30 | 85 (66.4) |
| 31–40 | 31 (24.2) |
| 41–50 | 12 (9.4) |
| Sex | |
| Male | 40 (31.2) |
| Female | 88 (68.8) |
| Marital status | |
| Single | 55 (43.0) |
| Marriage | 73 (57.0) |
| Degree | |
| Diploma | 7 (5.5) |
| Technician | 31 (24.3) |
| Bachelor | 87 (68.0) |
| MSc | 3 (2.2) |
| Work experience (yrs) | |
| 0–10 | 97 (75.8) |
| 11–20 | 21 (16.4) |
| 21–30 | 10 (7.8) |
| Sources of information toward needlestick | |
| Educational pamphlets | 35 (27.3) |
| Training courses | 47 (36.7) |
| Friends | 28 (22.7) |
| Other | 17 (13.3) |
| History of hepatitis B vaccination | |
| Yes | 122 (95.3) |
| No | 6 (4.7) |
| Mean (SD) age, yrs | 29.6 (6.6) |
| Mean (SD) work experience, yrs | 7.3 (6.4) |
Overall, 71.7% of the participants attained a moderate-to-high score for the NSIs preventive behaviors. Certain behaviors such as determining the location of the sharp instruments on the operating table, based on the surgeon's comment (safety area) (5.5%), wearing two gloves for all surgeries (14.1%), informing surgical team members in an appropriate manner when they are going to leave sharp instruments on or grab them off the table (33.6%), and using forceps to place the needle on the handle (39.1%), were the least frequent preventive behaviors of the NSIs.
Out of the HBM constructs, the perceived barriers (93% of the maximum possible score) was the most frequently reported construct followed by the perceived susceptibility (85.5% of the maximum possible score), and the perceived self-efficacy (58.7% of the maximum possible score). In addition, the participants' knowledge about the outcomes and preventive practices of the NSIs was assessed to be moderate with a score of 68.5% of the maximum possible value (Table 2). The results demonstrated that the behavior and perceived susceptibility were inversely and significantly correlated (r -0.261). The behavior was directly and significantly correlated with the perceived self-efficacy (r 0.272) and cues to action (r 0.339) (Table 3).
| Table 2: Mean, SD, and range of scores and percentage of mean from maximum obtainable score for HBM constructs (n=128) | ||||
| Variables | Mean | SD | Range | Percentage |
| Perceived susceptibility | 8.55 | 1.7 | 0-10 | 85.5 |
| Perceived severity | 12.71 | 3.2 | 0-16 | 79.4 |
| Perceived benefits | 7.44 | 1.2 | 0-8 | 93.0 |
| Perceived barriers | 8.23 | 1.5 | 0-10 | 82.3 |
| Perceived self-efficacy | 2.35 | 1.1 | 0-4 | 58.7 |
| Cues to action | 10.52 | 2.7 | 0-14 | 75.1 |
| Knowledge | 13.61 | 2.1 | 0-20 | 68.5 |
| Behavior | 30.15 | 4.8 | 0-42 | 71.7 |
| Table 3: Pearson correlation coefficients among the constructs of health belief model (n=128) | ||||||
| Variables | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Perceived susceptibility | 1 | |||||
| 2. Perceived severity | 0.162 | 1 | ||||
| 3. Perceived benefits | 0.031 | 0.378** | 1 | |||
| 4. Perceived barriers | -0.019 | 0.199* | 0.079 | 1 | ||
| 5. Perceived self-efficacy | -0.199** | 0.090 | 0.272** | -0.005 | 1 | |
| 6. Cues to action | -0.043 | 0.346** | 0.480** | 0.101 | 0.394** | 1 |
| 7. Behavior | -0.261** | 0.073 | 0.126 | 0.057 | 0.272** | 0.399** |
| *p<0.05, **p<0.01 | ||||||
Out of the HBM constructs, the perceived susceptibility and cues to action were the best predictors of the NSIs preventive behaviors. Overall, the HBM constructs explained 23% of the variance observed in these behaviors (Table 4).
| Table 4: Linear regression analysis to predict the preventive behaviors of needlestick injuries based on the constructs of the health belief model | ||||
| Independent Variables | Coefficient | SE | β | p value |
| Perceived susceptibility | -0.627 | 0.236 | -0.221 | 0.009 |
| Perceived severity | -0.013 | 0.136 | -0.009 | 0.921 |
| Perceived benefits | 0.320 | 0.381 | -0.080 | 0.403 |
| Perceived barriers | 0.069 | 0.260 | 0.022 | 0.791 |
| Perceived self-efficacy | 0.412 | 0.378 | 0.097 | 0.278 |
| Cues to action | 0.695 | 0.175 | 0.390 | <0.001 |
| Constant | 29.214 | 3.682 | — | <0.001 |
| β: Standardized regression coefficient, SE: Standard error. Adj R2 = 0.23 | ||||
Discussion
The status of the NSIs preventive behaviors was found to be moderate among the participants in the current study. The findings of our study were consistent with many studies on adherence to universal precautions by HCWs.18,23,28-30 The rate of adherence to universal precautions was reported to be acceptable among the emergency department staff in the USA.19 Inconsistency in the findings can be explained by many factors such as the level of knowledge, the availability of the necessary equipment, and workload.28
According to our findings, certain behaviors such as determining safety or neutral zone, wearing two gloves for all surgeries, and using forceps to place suture needle on needle holder were the least frequently practiced behaviors. It has been shown that adhering to all precautions during surgery contributes to reducing the NSIs.31 Determining the safety zone on operating table is referred to as “hands-free technique.” The surgeon or scrub nurse determines a certain area, if necessary, where sharp instruments should not be given or taken; such instruments should be left on or grabbed off the table in a way that no two surgical team members touch the same sharp item simultaneously.32,33 In addition, according to the Association of Preoperative Registered Nurses and the Association of Surgical Technologists, wearing two gloves is necessary for all types of surgeries.31,34,35 It seems that lack of adherence to these practices among our participants was because these practices are time-consuming, the personnel are not used to conduct such practices, and declined precision and dexterity to work with hands.
However, if the staff continuously or intermittently wear two gloves on top of each other, they would ultimately accustom to it and satisfied.33 In the current study, using forceps to place the suture needle on the needle holder was not found to be a common practice. Over half of the NSIs, according to the available evidence, occur due to suture needles.5,10,11 These findings are consistent with findings of Stringer, et al,21 and Harris, et al,20 but inconsistent with Geong and Park study.22 Low level of knowledge, having negative attitude, lack of accustoming, interference with other duties, being time-consuming, and lack of understanding the significance of adherence to safety principles to prevent the NSIs, are the major reasons for inconsistency in the reported findings.22,28 It is therefore essential to take certain measures such as continuously monitoring adherence to the safety principles, and appropriately and sufficiently training the operating room personnel to promote their knowledge and attitudes.
The current study demonstrated that the NSIs preventive behaviors were directly correlated with the cues to action and perceived self-efficacy, and indirectly correlated with the perceived susceptibility. In other words, the rate of practicing preventive behaviors increased with increase in the cues to action and self-efficacy level, and decrease in the perceived susceptibility level among the participants. Regarding the observed direct correlation between the NSIs preventive behaviors and the self-efficacy, our findings were consistent with some studies,28,36 while about the indirect correlation between these behaviors and the perceived susceptibility, our observations were not consistent with other reports.24,36 This inconsistency in the findings could be attributed to high levels of both perceived susceptibility to the disease and self-efficacy among the participants in previous studies.28,36
The participants in the current study did not have high levels of self-efficacy. The educations about preventive behaviors of the NSIs in the studied people were likely to focus on the NSIs outcomes, and perhaps the efficacy of the preventive practices and people had not been incorporated into such educations. Theoretically, people first assess the threat of a risk for its seriousness and their own predisposition to experiencing it. Therefore, as the seriousness of the perceived threat increases, they are more stimulated to start the second assessment, ie, the assessment of the recommended solution. Under such conditions, individuals assess and evaluate the levels of their self-efficacy in addition to assessing the recommended solution. When the levels of both perceived susceptibility and perceived self-efficacy are high, the people are sufficiently stimulated to control the risk and consent to adopt the recommended solution.37
When individuals perceive that the threat is serious but assess the levels of recommended solution's efficacy and their self-efficacy to be low, they develop unreasonable fear, show a passive reaction, and do not take preventive measures satisfactorily. Indeed, if the level of threat is high and that of the self-efficacy is low, lack of adhering to desired practices is likely.38 It is therefore necessary to incorporate efficacy-promoting solutions into educational plans.
The regression analysis demonstrated that the perceived susceptibility and cues to action were the best predictors of the NSIs preventive behaviors, which is consistent with findings of Tabak, et al,36 and Mortada and Zalat.24 However, Brevidelli, et al, reported that the perceived benefits and the perceived barriers are the predictors of the NSIs.39 The study of Yousafzai, et al, showed that the perceived barriers are the predictors of the NSIs preventive behaviors.29 The inconsistency in the observed findings could be attributed to difference in the studied behaviors.
The results of current study showed that the HBM constructs explained 23% of the variance in the NSIs preventive behaviors, which was consistent with similar studies.24,36 Evidence suggests that on average, HBM determinants predict approximately 20% of the variance in healthy behavior,40 underlying the need to investigate other determinants not considered by HBM. Therefore, further studies are needed to assess the validity of other theories. When applying these theories, it is important to take into account the influence of socio-psychological factors too.
Altogether, it is recommended to develop and implement in-service educational plans with emphasis on the preventability of infections transmitted from patients, and take into account promotion of the operating room personnel's self-efficacy levels to promote the NSIs preventive behaviors.
Assessing behaviors using questionnaire was a limitation of this study. Some of the staff did not volunteer to participate in the study. This was also another limitation of this study.
In conclusion, adherence to the NSIs preventive practices was found to be moderate among the operating room personnel. In addition, the framework of the HBM was found useful for the prediction of NSIs preventive behaviors. Development of training interventions based on the results of the present study may therefore be beneficial.
Acknowledgments
The study was funded by Vice Chancellor for Research and Technology, Hamadan University of Medical Sciences (Grant no. 9209193284).
Conflicts of Interest:
None declared.
Cite this article as: Fathi Y, Barati M, Zandiyeh M, Bashirian S. Prediction of preventive behaviors of the needlestick injuries during surgery among operating room personnel: Application of the health belief model. Int J Occup Environ Med 2017;8:232-240. doi: 10.15171/ijoem.2017.1051
References
- 1.Saxena A, Singh MP, Brahmchari S, Banerjee M. Surgical site infection among postoperative patients of tertiary care centre in Central India--a prospective study. Asian Journal of Biomedical and Pharmaceutical Sciences. 2013;3:41–44. [Google Scholar]
- 2.Saleem T, Khalid U, Ishaque S, Zafar A. Knowledge, attitudes and practices of medical students regarding needle stick injuries. J Pak Med Assoc. 2010;60:151–6. [PubMed] [Google Scholar]
- 3.Efstathiou G, Papastavrou E, Raftopoulos V, Merkouris A. Prevalence of occupational exposure to pathogens and reporting behaviour among Cypriot nurses. International Journal of Caring Sciences. 2013;6:420–30. [Google Scholar]
- 4.Shah SF, Bener A, Al-Kaabi S. et al. The epidemiology of needle stick injuries among health care workers in a newly developed country. Saf Sci. 2006;44:387–94. [Google Scholar]
- 5. Rothrock JC. Alexander's Care of the Patient in Surgery, Elsevier Health Sciences, 2014.
- 6. Junco Díaz R. Occupational exposure to blood and body fluids among Cuban healthcare workers from three levels of medical care: Ascertaining the value of a reporting system. 30th International congress on occupational health, March 18-23, 2012, Cancun, Mexico. Available from www.ilo.org/safework/events/meetings/WCMS_170404/lang--en/index.htm (Accessed January 12, 2017).
- 7.Prakash KP. Epidemiology of needle-stick injuries in Mangalore. Journal of Evolution of Medical and Dental Sciences. 2012;1:128–136. [Google Scholar]
- 8.Yoshikawa T, Wada K, Lee JJ. et al. Incidence rate of needlestick and sharps injuries in 67 Japanese hospitals: a national surveillance study. PLoS One. 2013;8:e77524. doi: 10.1371/journal.pone.0077524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffmann C, Buchholz L, Schnitzler P. Reduction of needlestick injuries in healthcare personnel at a university hospital using safety devices. J Occup Med Toxicol. 2013;8:20. doi: 10.1186/1745-6673-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakaeen F, Awad S, Albo D. et al. Epidemiology of exposure to blood borne pathogens on a surgical service. Am J Surg. 2006;192:e18–21. doi: 10.1016/j.amjsurg.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Beker J, Bamlie T. Needle stick and sharp injuries and associated factors among nurses working in jimma university specialized hospital, south west Ethiopia. Journal of Nursing & Care. 2015;4:1–8. [Google Scholar]
- 12.Memish ZA, Assiri AM, Eldalatony MM, Hathout HM. Benchmarking of percutaneous injuries at the Ministry of Health hospitals of Saudi Arabia in comparison with the United States hospitals participating in exposure prevention information network (EPINet TM) Int J Occup Environ Med. 2015;6:26–33. doi: 10.15171/ijoem.2015.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hashemi S, Torabian S, Mamani M, Moazen DS. [The prevalence of needlestick and sharps injuries among health care workers in Hamadan, Iran] Sci J Hamadan Univ Med Sci. 2012;18:41–6. [in Persian]. [Google Scholar]
- 14.Abdi MH, Najafipour S, Hamidizadeh S. et al. [Survey of accidental injuries caused by sharp instruments among the jahrom university of medical sciences hospitals health care workers 2008] J Jahrom Univ Med Sci. 2009;7:30–8. [in Persian]. [Google Scholar]
- 15.Ghanei Gheshlagh R, Zahednezhad H, Shabani F. et al. [Needle sticks injuries and its related factors among nurses] Iran Journal of Nursing. 2014;27:21–9. [in Persian]. [Google Scholar]
- 16.Ghasemi A, Eatemad E, Pourmohammadjan N. et al. Needle Stick Injuries among Health Care Workers of Ardebil University of Medical Science. Iranian Journal of Infectious Diseases and Tropical Medicine. 2009;14:27–32. [in Persian]. [Google Scholar]
- 17.Moradi A, Mostafavi E, Moradi A. [The prevalence and causes of needle stick injuries among the primary health care workers of Bahar city, Hamadan Province] Iran Occupational Health. 2010;7:39–42. [in Persian]. [Google Scholar]
- 18.Oliveira AC, Pinto SA, Garbaccio JL. Needle-stick stuffs with safety device for prevention of percutaneous injuries: a literature review. Journal of Nursing UFPE on line. 2012;6:2830–8. [Google Scholar]
- 19.Sabbah I, Sabbah H, Sabbah S. et al. [Occupational exposures to blood and body fluids (BBF): Assessment of knowledge, attitude and practice among health care workers in general hospitals in Lebanon] Health. 2013;5:70. [in Persian]. [Google Scholar]
- 20.Harris SA, Nicolai LA. Occupational exposures in emergency medical service providers and knowledge of and compliance with universal precautions. Am J Infect Control. 2010;38:86–94. doi: 10.1016/j.ajic.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Stringer B, Infante-Rivard C, Hanley J. Effectiveness of the hands-free technique in reducing operating theatre injuries. Occup Environ Med. 2002;59:703–7. doi: 10.1136/oem.59.10.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeong IS, Park S. Use of hands-free technique among operating room nurses in the Republic of Korea. Am J Infect Control. 2009;37:131–5. doi: 10.1016/j.ajic.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 23. Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. John Wiley & Sons, 2008.
- 24.Mortada EM, Zalat MM. Assessment of compliance to standard precautions among surgeons in Zagazig University Hospitals, Egypt, using the Health Belief Model. Journal of The Arab Society for Medical Research. 2014;9:6. [Google Scholar]
- 25.MazlomiMahmodabad SH, Alaeei M, MirzaeeiAlavigeh M. et al. [Preventive behavior status of diabetes mellitus II in persons at risk: Application of Health Belief Model] Iranian Journal of Diabetes and Metabolism. 2012;11:544–50. [in Persian]. [Google Scholar]
- 26.Javaheri Tehrani F, Nikpour S. Effect of an Educational Program Based on the Health Belief Model on Preventive Behaviors of Urinary Tract Infection among Women. Preventive Care In Nursing & Midwifery Journal. 2013;3:1–11. [Google Scholar]
- 27.Mahdizadeh M, Mahdizadeh M, Peyman N. [Evaluation of education in promoting healthy lifestyle behaviors among adolescent girls, according to the Health Belief Model] J Sabzevar Univ Med Sci. 2014;21:164–74. [in Persian]. [Google Scholar]
- 28.Simbar M, Shayan-Menesh M, Nahidi F, Akbar Zadeh AR. Health beliefs of midwives about HIV/AIDS protection and the barriers to reducing risk of infection: An Iranian study. Leadersh Health Serv. 2011;24:106–17. [Google Scholar]
- 29.Yousafzai MT, Siddiqui AR, Janjua NZ. Health belief model to predict sharps injuries among health care workers at first level care facilities in rural Pakistan. Am J Ind Med. 2013;56:479–87. doi: 10.1002/ajim.22117. [DOI] [PubMed] [Google Scholar]
- 30.Al-Khatib IA, El Ansari W, Areqat TA. et al. Occupational Safety Precautions among Nurses at Four Hospitals, Nablus District, Palestine. Int J Occup Environ Med. 2015;6:243–6. doi: 10.15171/ijoem.2015.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. AST, Association of Surgical Technologists. AST Guidelines for Best Practices for Sharps Safety and Use of the Neutral Zone, 2014.
- 32. AST, Association of Surgical Technologists. Guideline Statement for the Implementation of the Neutral Zone in the Perioperative Environment, 2013.
- 33.Berguer R, Heller PJ. Preventing sharps injuries in the operating room. J Am Coll Surg. 2004;199:462–7. doi: 10.1016/j.jamcollsurg.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Childs T. Use of double gloving to reduce surgical personnel's risk of exposure to bloodborne pathogens: An integrative review. AORN J. 2013;98:585–96 e6. doi: 10.1016/j.aorn.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 35.Ford DA. Implementing AORN recommended practices for sharps safety. AORN J. 2014;99:106–20. doi: 10.1016/j.aorn.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 36.Tabak N, Shiaabana AM, ShaSha S. The health beliefs of hospital staff and the reporting of needlestick injury. J Clin Nurs. 2006;15:1228–39. doi: 10.1111/j.1365-2702.2006.01423.x. [DOI] [PubMed] [Google Scholar]
- 37.Witte K, Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Educ Behav. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- 38.Barati M, Amirzargar MA, Bashirian S. et al. Psychological Predictors of Prostate Cancer Screening Behaviors Among Men Over 50 Years of Age in Hamadan: Perceived Threat and Efficacy. Iran J Cancer Prev. 2016;9:e4144. doi: 10.17795/ijcp-4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brevidelli MM, Cianciarullo TI. [Application of the health belief model to the prevention of occupational needlestick injuries] Rev Saude Publica. 2001;35:193–201. doi: 10.1590/s0034-89102001000200014. [in Portuguese]. [DOI] [PubMed] [Google Scholar]
- 40.Orji R, Vassileva J, Mandryk R. Towards an Effective Health Interventions Design: An Extension of the Health Belief Model. Online J Public Health Inform. 2012:4. doi: 10.5210/ojphi.v4i3.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]


