Abstract
Background:
Research suggests that diabetes mellitus (DM) has a negative impact on employment and workplace injury, but there is little data within the Canadian context.
Objective:
To determine if DM has an impact on various occupational health outcomes using the Canadian Community Health Survey (CCHS).
Methods:
CCHS data between 2001 and 2014 were used to assess the relationships between DM and various occupational health outcomes. The final sample size for the 14-year study period was 505 606, which represented 159 432 239 employed Canadians aged 15–75 years during this period.
Results:
We found significant associations between people with diabetes and their type of occupation (business, finance, administration: 2009, p=0.002; 2010, p=0.002; trades, transportation, equipment: 2008, p=0.025; 2011, p=0.002; primary industry, processing, manufacturing, utility: 2013, p=0.018), reasons for missing work (looking for work: 2001, p=0.024; school or education: 2003, p=0.04; family responsibilities: 2014, p=0.015; other reasons: 2001, p<0.001; 2003, p<0.001; 2010, p=0.015), the number of work days missed (2010, 3 days, p=0.033; 4 days, p=0.038; 11 days, p<0.001; 24 days, p<0.001), and workrelated injuries (traveling to and from work: 2014, p=0.003; working at a job or business: 2009, p=0.021; 2014, p=0.001).
Conclusion:
DM is associated with various occupational health outcomes, including workrelated injury, work loss productivity, and occupation type. This allows stakeholders to assess the impact of DM on health outcomes in workplace.
Keywords: Diabetes mellitus, Occupational health, Surveys and questionnaires, Workplace, Canada
TAKE-HOME MESSAGE
Diabetes mellitus has a negative impact on employment and workplace.
Various factors might be associated with diabetes within the Canadian context.
Diabetes may be more common in “blue collar” occupations where manual labor comprises much of the work they do.
Diabetes is associated with various occupational health outcomes including work-related injury, loss of work productivity due to absenteeism, and the types of occupations.
Introduction
Currently, there are three million Canadians living with diabetes mellitus (DM). The number has been more than doubled the 2000 value and directly costs the health care system C$ 3 billion (US$ 2.2 billion) annually.1 Despite the current, high economic burden of DM in Canada, it is expected to increase by 40% in the next 10 years. However, while the cost of DM on the health care system has been well studied, less is known about the effect the disease has at the workplace.
Studies from the USA and several European countries found that patients with DM had a higher number of sick days owing to their illness than patients without DM.2-5 Previous research has found that people who left the labor force early due to diabetes had an income five times less than those who did not have a chronic illness.6 Men and women with DM were 7.1% and 4.4%, respectively, less likely to be working compared to their counterparts without the disease.7 The same study also found that people with diabetes had more work-loss days per year than those without the disease. Furthermore, patients with DM were more likely to have work limitations that affect the kind or amount of work they could do.7
In a Canadian study, researchers found that diabetes has a negative impact on employment of women, but no association was observed in men. The author suggests that diabetes affects women more than men and that the severity of their diabetes inhibits them from finding job.8 Two studies also looked at the risk of workplace injury and diabetes but found opposite results. There was a 17% increased risk of injury in a study of diabetic, blue collar workers in the US, while a British study found no evidence linking diabetes as a contributor to increased workplace injury.9,10 A recent Swedish study suggested that diabetes and work disability were jointly associated with a high risk of premature death, highlighting the importance of prevention and early detection.11
While these studies are useful in gaining a general understanding of the impact that diabetes has on the workplace, the results may vary depending on the country where the study was performed. To the best of our knowledge, there is a dearth of evidence on the impact DM has at the workplace within the Canadian context.
This study used the retrospective Canadian Community Health Survey (CCHS) data from 2001 to 2014 to investigate whether DM had any effects on occupational health outcomes over time, such as the type of occupation, employment status, work productivity, absence due to chronic disease, and injury occurring at the workplace.
Materials and Methods
Survey Data Collection
The CCHS is a cross-sectional survey conducted by Statistics Canada to collect information about health status, health care utilization, and determinants of health from a representative sample of the Canadian general population. The survey population includes Canadians over the age of 12 years living in all 10 provinces and three territories, which make up 136 Health Regions. Excluded from the survey are full-time members of the Canadian Forces, and institutionalized population and people living in the Quebec health regions of Région du Nunavik and Région des Terres-Cries-de-la-Baie-James, all of which account for less than 3% of the Canadian population aged 12 years and older. From 2001 to 2005, the survey was administered every two years with approximately 130000 respondents during the 2001, 2003, and 2005 reference periods. In 2007, the study was administered every year with a sample size of 65000 respondents. All analyses were performed using data from the CCHS Public Use Micro-Data File obtained from Statistics Canada.
Variables
The primary outcome for this study was whether having diabetes is associated with various occupational health outcomes. Respondents aged 15–74 years, who reported to be working at the time of the survey, were included in our analyses for each CCHS cohort. The variables that were included in our analyses were occupation type, full- or part-time employment status, reasons for missing work, the number of work days lost due to a chronic condition in the previous three months, and the activity where the most serious injury occurred. Several covariates were included in this study to account for potential confounding variables including age, gender, and physical activity index. The physical activity index is based on the average daily physical activity of the respondent over the past three months. Individuals were categorized as “inactive” (physical activity index of <1.5 kcal/kg/day), “moderately active” (physical activity index of 1.5–2.9 kcal/kg/day), and physically “active” (physical activity index of >3.0 kcal/kg/day). Also, some variables were not available for certain years of the CCHS. A summary of the variables included in the analysis for each year can be found in Table 1.
| Table 1: Summary of variables analyzed in each CCHS cohort. A long dash represents where data were not available. | |||||||||||
| 2001 | 2003 | 2005 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Type of occupation | √ | √ | — | √ | √ | √ | √ | √ | √ | √ | √ |
| Full/Part-time status | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Reasons for missing work during the last week | √ | √ | — | — | √ | — | √ | √ | √ | √ | √ |
| Number of work days lost due to chronic condition | — | — | — | — | — | — | √ | √ | √ | √ | √ |
| Activity where the most serious injury occurred | √ | √ | √ | √ | — | √ | √ | √ | √ | √ | √ |
Statistical Analysis
Bivariate analysis was used to filter variables—those with p<0.1 were retained for model building. The significance level of p<0.1 was used to ensure potential useful variables were not excluded from the analysis. Manual backward stepwise logistic regression analysis was then used to develop two models of occupational health factors associated with diabetes in Canada: (1) type of occupation and full/part-time status, and (2) number of work days missed, reasons for missed work, and activity where the most serious injury occurred. A significance level of p<0.05 was used in each of the final models; variables were corrected using post hoc analysis. The analysis was completed in StataMP 14, with “svyset” commands to apply sampling weights and to adjust for clustering of observations within the health region stratification. A representative set of Stata command codes for the statistical analysis of the 2001 CCHS dataset is included in the Appendix. Post hoc pairwise comparisons on significant variables were performed using the Bonferroni multiple comparison test.
Results
Study Sample and Population
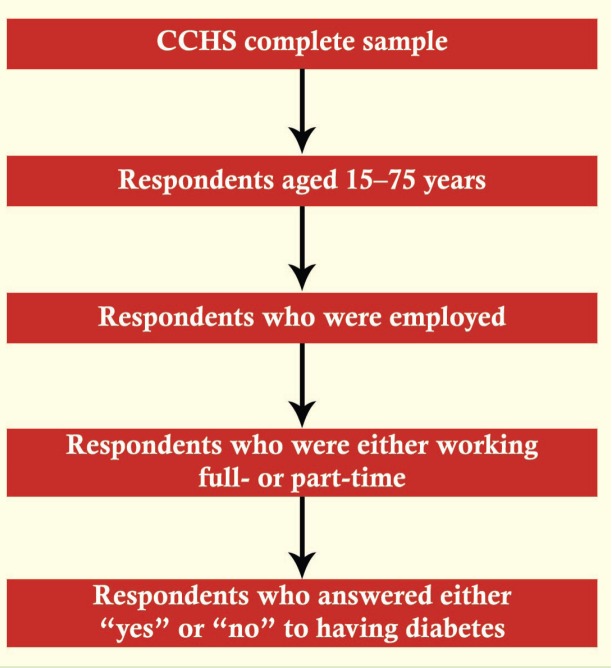
Figure 1 presents the flow chart on how the final analysis sample was obtained. In total, there were 1123845 respondents for the CCHS between 2001 and 2014. Respondents were excluded from the study based on the age criteria and employment status. A summary of the study sample characteristics in each CCHS is provided in Table 2. The final sample size was 505606 for the 2001 to 2014 CCHS, and this represented a total of 159432239 employed Canadians aged 15 to 75 years during this period (Table 3).
Figure 1.
Flow chart of sample selection
| Table 2: Study sample characteristics, CCHS 2001 to 2014 survey of employed respondents aged 15–75 years. Figures are percentages. A long dash represents where data were not available. | |||||||||||
| Variables | 2001 | 2003 | 2005 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
| Age | |||||||||||
| 15–19 | 10.03 | 10.58 | 7.36 | 6.43 | — | 6.88 | 6.68 | 6.43 | 6.36 | 6.11 | 5.98 |
| 20–29 | 17.6 | 16.82 | 18.26 | 16.33 | — | 17.36 | 18.09 | 17.24 | 16.93 | 16.22 | 16.03 |
| 30–39 | 24.30 | 23.09 | 23.28 | 22.33 | — | 20.69 | 20.14 | 19.59 | 19.31 | 19.13 | 18.69 |
| 40–49 | 25.78 | 22.70 | 23.20 | 22.78 | 18.65 | 20.31 | 20.06 | 19.53 | 19.32 | 17.96 | 17.50 |
| 50–59 | 16.66 | 20.63 | 20.14 | 22.64 | 49.95 | 23.22 | 23.18 | 23.75 | 23.77 | 24.79 | 25.21 |
| 60–69 | 5.04 | 5.72 | 6.95 | 8.56 | 28.44 | 10.44 | 10.66 | 12.11 | 12.85 | 14.03 | 14.64 |
| 70–74 | 0.59 | 0.46 | 0.83 | 0.93 | 2.95 | 1.10 | 1.20 | 1.36 | 1.46 | 1.77 | 1.95 |
| Male sex | 51.25 | 50.15 | 50.71 | 49.87 | 51.03 | 49.18 | 49.03 | 48.58 | 48.46 | 48.38 | 48.40 |
| With diabetes | 2.53 | 2.96 | 3.24 | 3.95 | 8.87 | 4.27 | 4.37 | 4.53 | 4.54 | 4.99 | 5.14 |
| Physical activity index | |||||||||||
| Active | 24.15 | 23.86 | 26.2 | 25.36 | — | 27.4 | 28.15 | 29.2 | 29.24 | 29.4 | 29.08 |
| Moderate active | 24.8 | 25.7 | 25.92 | 25.73 | — | 26.1 | 25.94 | 26.22 | 26.06 | 26.2 | 26.28 |
| Inactive | 51.05 | 50.44 | 47.88 | 48.91 | — | 46.3 | 45.91 | 44.58 | 44.7 | 44.4 | 44.63 |
| Type of occupation | |||||||||||
| Management, sciences, health, education, arts, culture | 32.07 | —* | — | 34.5 | 33.6 | 24.52 | 34.53 | 34.95 | 35.43 | 35.28 | 35.33 |
| Business, finance, administration | 11.34 | —* | — | 17.9 | 21.55 | 18.34 | 18.27 | 17.83 | 17.13 | 16.92 | 17.07 |
| Sales and service | 24.11 | —* | — | 23.5 | 22.26 | 24.04 | 24.45 | 24.11 | 23.96 | 24.31 | 24.26 |
| Trades, transportation, equipment | 14.97 | —* | — | 15.3 | 14.19 | 14.6 | 14.45 | 14.8 | 15.02 | 14.56 | 14.49 |
|
Primary industry, processing, manufacturing, utilities |
10.56 | —* | — | 8.83 | 8.39 | 8.51 | 8.30 | 8.31 | 8.45 | 8.94 | 8.84 |
| Employment status | |||||||||||
| Full-time | 81.64 | 82.15 | 82.88 | 82.71 | 81.12 | 80.9 | 80.58 | 80.44 | 80.48 | 80.14 | 80.14 |
| Part-time | 18.36 | 17.85 | 17.12 | 17.29 | 18.88 | 19.1 | 19.42 | 19.56 | 19.52 | 19.86 | 19.86 |
| Reasons for missing work during the last week | |||||||||||
| Illness/disability/permanently unable | 12.26 | 11.2 | — | — | 31.64 | — | 23.36 | 32.72 | 33.07 | 25.97 | 35.66 |
| Family responsibility | 7.75 | 7.92 | — | — | — | — | 33.04 | 37.58 | 40.24 | 18.18 | 37.53 |
| School or education | 17.28 | 13.5 | — | — | — | — | 6.97 | 3.84 | 0.8 | — | 1.25 |
| Labor dispute | 6.23 | 6.98 | — | — | — | — | — | — | — | — | 10.1 |
| Retired | 6.25 | 7.14 | — | — | — | — | 4.36 | 2.22 | 1.99 | 1.3 | 2.24 |
| Looking for work | 22.71 | 23.9 | — | — | — | — | — | — | — | — | — |
| Other | 27.52 | 29.44 | — | — | 68.36 | — | 32.26 | 23.63 | 23.9 | 54.55 | 13.22 |
| Number of work days lost due to chronic condition | |||||||||||
| 1–10 | — | — | — | — | — | — | 81.66 | 73.33 | 72.32 | 74.50 | 78.96 |
| 11–20 | — | — | — | — | — | — | 8.18 | 8.16 | 9.13 | 8.82 | 8.53 |
| 21–30 | — | — | — | — | — | — | 4.41 | 6.67 | 8.15 | 9.80 | 4.74 |
| 31+ | — | — | — | — | — | — | 5.76 | 11.85 | 10.42 | 6.86 | 7.77 |
| Activity where the most serious injury occurred | |||||||||||
| Sports or physical activity | 40.20 | 25.08 | 27.24 | 30.2 | — | 30.04 | 30.05 | 29.81 | 28.83 | 28.56 | 28.11 |
| Leisure activity or hobby | 12.69 | 10.61 | 13.57 | — | 6.59 | 6.55 | 7.26 | 6.83 | 6.75 | 6.62 | |
| Working at a job or business | 32.82 | 31.73 | 26.51 | 25.44 | — | 20.61 | 20.86 | 23.34 | 23.33 | 20.07 | 20.05 |
| Travelling to and from work | — | 6.48 | 4.96 | 5.48 | — | 5.44 | 5.59 | 6.91 | 5.33 | 5.57 | 5.85 |
| Household chores | 17.53 | 15.65 | 13.16 | 14.48 | — | 15.12 | 16.08 | 13.72 | 16 | 15.92 | 16.26 |
| Other | 9.46 | 8.37 | 17.52 | 10.83 | — | 22.2 | 20.87 | 18.97 | 19.66 | 23.14 | 23.13 |
| *Occupation type collected in 2003 was classified differently than other years. | |||||||||||
| Table 3: Survey sample size and representative population size for each CCHS dataset | ||||
| Year |
Total survey
sample size |
Total representative
population size |
Study sample size | Representative study population size |
| 2001 | 130880 | 25787334.1 | 76789 | 16066998 |
| 2003 | 134072 | 26555429.5 | 5085 | 988707 |
| 2005 | 132221 | 27104036.7 | 70505 | 16144453 |
| 2007 | 131061 | 28017371.9 | 67701 | 16476623 |
| 2008 | 30865 | 13635505.7 | 10430 | 7106159 |
| 2009 | 124188 | 28725105.5 | 62245 | 16711537 |
| 2010 | 62908 | 28878418.4 | 31317 | 16718723 |
| 2011 | 124929 | 29335211 | 61158 | 16991617 |
| 2012 | 61707 | 29491030 | 30196 | 17202001 |
| 2013 | 127462 | 30002817 | 60364 | 17465257 |
| 2014 | 63552 | 30154391.7 | 29816 | 17560164 |
| Total | 1123845 | 297686651.5 | 505606 | 159432239 |
Bivariate Analysis
In bivariate analysis, diabetes was associated with the following: type of occupation in 2001, 2007–2012, 2013, and 2014; full- or part-time employment in 2005, 2013, and 2014; reasons for missing work in 2001, 2003, 2008, 2010, 2012, 2014; number of work days lost due to chronic condition in 2010; activity where the most serious injury occurred in 2001, 2003, 2005, 2007, 2009, 2010, 2013, and 2014; age in 2001, 2003, 2005, 2007–2014; sex in 2001, 2003, 2005, 2007–2014; and physical activity index in 2001, 2003, 2005, 2007, 2009–2014. Only these variables were subsequently used in the manual backwards stepwise logistic regression models. Several factors were associated with diabetes in each year of the CCHS as determined by the regression models. The variables that remained significant after Bonferroni correction are summarized in Table 4.
| Table 4: Summary of the significant associations between occupational health factors and diabetes based on backwards, stepwise logistic regression model. Figures are OR (95% CI). A long dash represents where data were not available. Non-significant ORs are not presented. | |||||||||||
| 2001 | 2003 | 2005 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
| Type of occupation | |||||||||||
| Management, sciences, health, education, arts, culture | 1.0 | — | — | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Business, finance, administration | — | — |
1.39 (1.12 to 1.71) |
1.64 (1.20 to 2.23) |
|||||||
| Sales and service | — | — | |||||||||
| Trades, transportation, equipment | — | — |
1.60 (1.06 to 2.43) |
1.43 (1.14 to 1.79) |
|||||||
| Primary industry, processing, manufacturing, utilities | — | — |
1.24 (1.04 to 1.47) |
||||||||
| Full/Part-time status | |||||||||||
| Reasons for missing work | |||||||||||
| Illness/disability/permanently unable | 1.0 | 1.0 | — | — | 1.0 | — | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Family responsibility | — | — | — | — |
0.09 (0.01 to 0.61) |
||||||
| School or education |
0.19 (0.04 to 0.92) |
— | — | — | — | — | |||||
| Labor dispute | — | — | — | — | — | — | — | — | |||
| Retired | — | — | — | — | |||||||
| Looking for work |
0.67 (0.47 to 0.95) |
— | — | — | — | — | — | — | — | — | |
| Other |
0.50 (0.50 to 0.72) |
0.37 (0.22 to 0.64) |
— | — | — |
4.31 (1.33 to 13.95) |
|||||
| Number of work days lost due to chronic condition | |||||||||||
| 1 | — | — | — | — | — | — | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 3 | — | — | — | — | — | — |
3.11 (1.10 to 8.79) |
||||
| 4 | — | — | — | — | — | — |
3.92 (1.08 to 14.23) |
||||
| 11 | — | — | — | — | — | — |
77.01 (9.52 to 622.91) |
||||
| 24 | — | — | — | — | — | — |
35.06 (4.36 to 281.63) |
||||
| Activity where the most serious injury occurred | |||||||||||
| Sports or physical activity | 1.0 | 1.0 | 1.0 | 1.0 | — | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Leisure activity or hobby |
1.94 (1.05 to 3.59) |
— | |||||||||
| Working at a job or business | — |
1.97 (1.11 to 3.50) |
4.41 (1.91 to 10.17) |
||||||||
| Travelling to and from work | — | — |
5.25 (1.75 to 15.77) |
||||||||
| Household chores | — | ||||||||||
| Going up and down stairs or walking | — | — | — | — | — |
3.69 (2.14 to 6.34) |
2.98 (1.03 to 8.63) |
4.81 (2.12 to 10.91) |
|||
| Other | — |
2.77 (1.16 to 6.60) |
4.31 (1.33 to 13.95) |
2.67 (1.17 to 6.10) |
|||||||
Type of Occupation
In the final multivariate regression model, five of the 10 CCHS (2008–2011, 2013) where the type of occupation data was collected, a significant positive association with diabetes was observed (p<0.05). Respondents with occupations in the business, finance, and administration; trades, transportation, and equipment; and primary industry, processing, manufacturing, and utilities sectors, were more likely to have diabetes compared to people with occupations in management, sciences, health, education, arts, and culture. A positive association between sales and service occupations and diabetes was observed in five CCHS cohorts (2009–2013); however, none were significant after post hoc analysis (Table 4).
Full/Part-time Employment
No significant association was found between full- or part-time employment and diabetes in any of the CCHS cohorts between 2001 and 2014.
Reasons for Missing Work
In the final multivariate regression model, a negative association between the reasons for missing work and diabetes was observed in four out of the eight CCHS that collected this data (2001, 2003, 2010, and 2014). People with diabetes were less likely to miss work due to reasons such as looking for work, school or education, family responsibilities, or other reasons compared to missing work due to an illness/disability or being permanently unable to work (Table 4).
Number of Work Days Lost due to a Chronic Condition
Of the five CCHS where data on the number of work days missed due to a chronic disease were collected, a positive association to diabetes was observed in the 2010 cohort. Compared to one work day missed, those with diabetes were more likely to miss 3, 4, 11, and 24 days of work (Table 4).
Activity where the Most Serious Injury Occurred
In four of the 10 CCHS (2005, 2009, 2010, and 2014) that collected data on the activity where an individual sustained the most serious injury, a positive association was found between the variable and diabetes. Compared to sports and physical activity, people with diabetes were more likely to sustain a serious injury performing a leisure activity or hobby, travelling to and from work, working at a job or business, going up and down the stairs or walking, or performing other activities including sleeping, eating, and personal care (Table 4).
Discussion
In this secondary analysis of the 2001 to 2014 CCHS data, we found various factors that might be associated with diabetes within the Canadian context. Previous research has suggested that diabetes may be more common in “blue collar” occupations where manual labor comprises much of the work that they do. A 34-year longitudinal US study found that people with blue-collar occupations have a 42% and 55% higher risk of having diabetes than white-collar occupations for men and women, respectively.12 Another study found that men in a low occupational class, characterized by unskilled or semi-skilled manual occupations, have a significantly higher risk of having diabetes than men in higher occupational classes.13 However, the results of this study suggest that this may not always be the case. We found that “white-collar” occupations in business, finance, and administration were significantly associated with diabetes, and had similar risks as “blue-collar” occupations in the primary industry, processing, manufacturing, and utility sector.
A Japanese study of the incidence of diabetes amongst male white-collar workers found that sales workers aged 40–49 and 50–59 had 1.55 and 2.01 times the risk for DM compared to other white-collar workers, respectively.14 The authors of the same study suggested that sales workers may have some occupational risk factors for DM, independent from traditional risk factors. An alternative reason would be that working in a sales or service occupation may exacerbate any pre-existing traditional risk factors for DM.14 Interestingly, an association between DM and sales and service occupations was observed in five of the 10 CCHS cohorts (2009–2013) after running the logistic regression model. While these associations were not significant after post hoc analysis, more research should be done to better understand this relationship. This is especially important in Canada as workers in the sales and service sector make up a large percentage of the labor force. In 2011, 27.1% and 18.7% of women and men aged 15 years and over, respectively, were most likely to be employed in sales and service occupations.15 A possible cause for these results may be the level of strain experienced by people in sales and service occupations. A recent study found that passive occupations, characterized by low demand and control, are associated with a significantly increased risk of diabetes.16 Studies on the effect of job strain on various outcomes utilize a questionnaire to determine where an individual lies on the four quadrants of the job strain model.16–18 As a result, there may be variations in the level of strain experienced by different individuals within the same occupation. An area of potential future research is to discern whether an association between sales and service occupations and diabetes truly exists and if so, whether it is due to the level of strain experienced.
An association between diabetes and experiencing a serious injury working at a job or business, and traveling to and from work, was observed in this study in four CCHS cohorts. There is limited literature on work-related injury due to diabetes, and the results of each study are variable. Canadian studies on the risk of a crash in truck-permit and commercial drivers were higher in individuals with diabetes than healthy drivers.19,20 Other medical conditions, including coronary disease, hypertension, and visual impairment, did not have a significant effect on the risk of accidents.20 A British population-based, case-controlled study found no evidence that diabetes contributes to workplace injury.10 However, due to the CCHS design, the nature of the injury experienced by the respondents was not included, making it difficult to make any further meaningful conclusions from these results.
In four CCHS cohorts, people with diabetes were more likely to miss work due to an illness/disability or being permanently unable to work compared to other reasons such as looking for work, school or education, labor dispute, family responsibilities, and other reasons. These results suggested that an individual's diabetes might have a higher negative impact on the labor force, as demonstrated by the higher likelihood for workplace absenteeism, than any other reason. For this study, only individuals who reported that they were currently employed at the time of the survey were included in the analysis, and those not in the labor force due to their disability were excluded. As a result, the loss of productivity was even higher if individuals not currently in the work force would have been included in the analysis. This finding was consistent with other studies that have also documented higher workplace absenteeism in people with diabetes than those without.4,21-24 Cawley and colleagues found that obese and morbidly obese men missed 2.64 and 5.69 extra days of work per year compared to healthy weight non-diabetic people.21 The economic impact that absenteeism due to diabetes has on the labor force has been analyzed in the same study. Obese and morbidly obese diabetics cost an extra US$ 429 and US$ 924, respectively, in absenteeism costs compared to the control group.21 While presenteeism was not investigated in this study, several studies have also found higher rates amongst people with diabetes than those without.4,22,23
The data from this study will be useful in highlighting the importance of interventions and methods to reduce risk factors for diabetes in the workplace. A recent study on educational seminars tailored for transport workers demonstrated a positive impact on their health behaviors and may lower risk factors associated with obesity-related disorders such as diabetes.25 The loss of work productivity in patients with diabetes has been well studied in other countries, but our results provided data on the Canadian context.
There are a few limitations to this study. One is the self-reported nature of the questionnaires and the reliance on recall for some questions. Self-reported data may affect the accuracy of the responses to some of the questions, including the number of days missed from work due to a chronic condition in the past three months. However, a study found that self-reported recall of missed work days in the past three months is better than the recall for the past year.26 Another limitation was that the CCHS questionnaires do not distinguish between type 1 and type 2 DM. Previous studies have found an association between low socioeconomic status and occupational class, and increased risk of type 2 DM. However, less is known about the relationship between type 1 DM and occupational outcomes.12,13 As a result, not being able to account for type 1 and type 2 DM may lead to an over- or under-estimation of the associations between occupational health outcomes and DM. Future research is needed to compare occupational health outcomes with type 1 and type 2 DM, separately.
Collectively, our results suggest that diabetes is associated with various occupational health outcomes, including work-related injury, loss of work productivity due to absenteeism, and the types of occupations. These results will allow Canadian policy makers, employers, and other stakeholders to assess and examine the impact diabetes have at the workplace.
Conflicts of Interest:
None declared.
Financial Support:
None.
Appendix
Stata command codes for the statistical analysis of the 2001 CCHS dataset. This is a representative set of codes for all CCHS datasets. Italicized words were not part of the command code, but indicate the action that was taken following the command.
svyset GEOADPMF [pweight=WTSAM], vce(linearized) singleunit(missing)
keep LBFA_31A LBFADPFT LBFAGRNW INJAG09 CCC_101 DHHGAGE DHH_SEX PACADPAI WTSAM GEOADPMF LBFAG31
drop if DHHGAGE < 2
drop if DHHGAGE > 13
drop if LBFAG31 >2
drop if LBFADPFT >2
drop if LBFA_31A >9
drop if CCC_101 >5
rename CCC_101 Diabetic
recode Diabetic (2=0)(1=1)
svy: tab Diabetic LBFA_31A (variable kept)
svy: tab Diabetic LBFADPFT (variable dropped)
svy: tab Diabetic LBFAGRNW (variable kept)
svy: tab Diabetic INJAG09 (variable kept)
svy: tab Diabetic DHHGAGE (variable kept)
svy: tab Diabetic DHH_SEX (variable kept)
svy: tab Diabetic PACADPAI (variable kept)
keep LBFA_31A LBFAGRNW INJAG09 Diabetic DHHGAGE DHH_SEX PACADPAI WTSAM GEOADPMF
A. xi: svy: logistic Diabetic i.DHHGAGE i.DHH_SEX i.PACADPAI i.LBFA_31A
B. test _ILBFA_31A_2 _ILBFA_31A_3 _ILBFA_31A_4 _ILBFA_31A_5 _ILBFA_31A_6 _ILBFA_31A_7 _ILBFA_31A_8 _ILBFA_31A_9 (variable kept)
C. test _IPACADPAI_2 _IPACADPAI_3 (variable kept)
D. test _IDHH_SEX_2 (variable kept)
E. test _IDHHGAGE_3 _IDHHGAGE_4 _IDHHGAGE_5 _IDHHGAGE_6 _IDHHGAGE_7 _IDHHGAGE_8 _IDHHGAGE_9 _IDHHGAGE_10 _IDHHGAGE_11 _IDHHGAGE_12 _IDHHGAGE_13 (variable kept)
F. xi: svy: logistic Diabetic i.DHHGAGE i.DHH_SEX i.PACADPAI i.LBFA_31A
A. xi: svy: logistic Diabetic i.DHHGAGE i.DHH_SEX i.PACADPAI i.LBFAGRNW i.INJAG09
B. test _IINJAG09_2 _IINJAG09_3 _IINJAG09_4 (variable dropped)
C. xi: svy: logistic Diabetic i.DHHGAGE i.DHH_SEX i.PACADPAI i.LBFAGRNW
D. test _ILBFAGRNW_2 _ILBFAGRNW_3 _ILBFAGRNW_4 _ILBFAGRNW_5 _ILBFAGRNW_6 _ILBFAGRNW_7 (variable kept)
E. xi: svy: logistic Diabetic i.DHHGAGE i.DHH_SEX i.PACADPAI i.LBFAGRNW
Cite this article as: Li AKC, Nowrouzi-Kia B. Impact of diabetes mellitus on occupational health outcomes in Canada. Int J Occup Environ Med 2017;8:96-108. doi: 10.15171/ijoem.2017.992
References
- 1. Canadian Diabetes Association. 2015 Report on Diabetes - Driving Change. 2015;1-84.
- 2.Dray-Spira R, Herquelot E, Bonenfant S. et al. Impact of diabetes mellitus onset on sickness absence from work--a 15-year follow-up of the GAZEL Occupational Cohort Study. Diabet Med. 2013;30:549–56. doi: 10.1111/dme.12076. [DOI] [PubMed] [Google Scholar]
- 3.De Backer G, Leynen F, De Bacquer D. et al. Diabetes mellitus in middle-aged people is associated with increased sick leave: the BELSTRESS study. Int J Occup Environ Health. 2006;12:28–34. doi: 10.1179/oeh.2006.12.1.28. [DOI] [PubMed] [Google Scholar]
- 4.Fu AZ, Qiu Y, Radican L, Wells BJ. Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions. Diabetes Care. 2009;32:2187–92. doi: 10.2337/dc09-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kivimäki M, Vahtera J, Pentti J. et al. Increased sickness absence in diabetic employees: what is the role of co-morbid conditions? Diabet Med. 2007;24:1043–8. doi: 10.1111/j.1464-5491.2007.02216.x. [DOI] [PubMed] [Google Scholar]
- 6.Schofield D, Cunich MM, Shrestha RN. et al. The economic impact of diabetes through lost labour force participation on individuals and government: evidence from a microsimulation model. BMC Public Health. 2014;14:220. doi: 10.1186/1471-2458-14-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tunceli K, Bradley CJ, Nerenz D. et al. The impact of diabetes on employment and work productivity. Diabetes Care. 2005;28:2662–7. doi: 10.2337/diacare.28.11.2662. [DOI] [PubMed] [Google Scholar]
- 8.Latif E. The impact of diabetes on employment in Canada. Health Econ. 2009;18:577–89. doi: 10.1002/hec.1390. [DOI] [PubMed] [Google Scholar]
- 9.Kubo J, Goldstein BA, Cantley LF. et al. Contribution of health status and prevalent chronic disease to individual risk for workplace injury in the manufacturing environment. Occup Environ Med. 2014;71:159–66. doi: 10.1136/oemed-2013-101653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palmer KT, D'Angelo S, Harris EC. et al. Epilepsy, diabetes mellitus and accidental injury at work. Occup Med (Lond) 2014;64:448–53. doi: 10.1093/occmed/kqu079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lallukka T, Ervasti J, Mittendorfer-Rutz E. et al. The joint contribution of diabetes and work disability to premature death during working age: a population-based study in Sweden. Scand J Public Health. 2016;44:580–6. doi: 10.1177/1403494816655059. [DOI] [PubMed] [Google Scholar]
- 12.Maty SC, Everson-Rose SA, Haan MN. et al. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 2005;34:1274–81. doi: 10.1093/ije/dyi167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hedén Stahl C, Novak M, Hansson P-O. et al. Incidence of Type 2 diabetes among occupational classes in Sweden: a 35-year follow-up cohort study in middle-aged men. Diabet Med. 2014;31:674–80. doi: 10.1111/dme.12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nagaya T, Yoshida H, Takahashi H, Kawai M. Incidence of type-2 diabetes mellitus in a large population of Japanese male white-collar workers. Diabetes Res Clin Pract. 2006;74:169–74. doi: 10.1016/j.diabres.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 15.Statistics Canada. Analytical document Portrait of Canada's Labour Force. National Household Survey 2011. 2013:1–19. [Google Scholar]
- 16.Mutambudzi M, Javed Z. Job Strain as a Risk Factor for Incident Diabetes Mellitus in Middle and Older Age US Workers. J Gerontol B Psychol Sci Soc Sci. 2016;71:1089–96. doi: 10.1093/geronb/gbw091. [DOI] [PubMed] [Google Scholar]
- 17.Söderberg M, Rosengren A, Hillström J. et al. A cross-sectional study of the relationship between job demand-control, effort-reward imbalance and cardiovascular heart disease risk factors. BMC Public Health. 2012;12:1102. doi: 10.1186/1471-2458-12-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gimeno D, Elovainio M, Jokela M. et al. Association between passive jobs and low levels of leisure-time physical activity: the Whitehall II cohort study. Occup Environ Med. 2009;66:772–6. doi: 10.1136/oem.2008.045104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laberge-Nadeau C, Dionne G, Ekoé JM. et al. Impact of diabetes on crash risks of truck-permit holders and commercial drivers. Diabetes Care. 2000;23:612–7. doi: 10.2337/diacare.23.5.612. [DOI] [PubMed] [Google Scholar]
- 20.Dionne G, Desjardins D, Laberge-Nadeau C, Maag U. Medical conditions, risk exposure, and truck drivers' accidents: an analysis with count data regression models. Accid Anal Prev. 1995;27:295–305. doi: 10.1016/0001-4575(94)00071-s. [DOI] [PubMed] [Google Scholar]
- 21.Cawley J, Rizzo JA, Haas K. The association of diabetes with job absenteeism costs among obese and morbidly obese workers. J Occup Environ Med. 2008;50:527–34. doi: 10.1097/JOM.0b013e31816ed029. [DOI] [PubMed] [Google Scholar]
- 22.DiBonaventura M, Link C, Pollack MF. et al. The relationship between patient-reported tolerability issues with oral antidiabetic agents and work productivity among patients having type 2 diabetes. J Occup Environ Med. 2011;53:204–10. doi: 10.1097/JOM.0b013e318209e0ce. [DOI] [PubMed] [Google Scholar]
- 23.Rodbard HW, Fox KM, Grandy S. Impact of Obesity on Work Productivity and Role Disability in Individuals With and at Risk for Diabetes Mellitus. Am J Heal Promot. 2009;23:353–60. doi: 10.4278/ajhp.081010-QUAN-243. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Economic costs of diabetes in the US in 2012. Diabetes Care. 2013;36:1033–46. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naug HL, Colson NJ, Kundur A. et al. Occupational health and metabolic risk factors: A pilot intervention for transport workers. Int J Occup Med Environ Health. 2016;29:573–84. doi: 10.13075/ijomeh.1896.00570. [DOI] [PubMed] [Google Scholar]
- 26.Zhang W, Bansback N, Anis AH. Measuring and valuing productivity loss due to poor health: A critical review. Soc Sci Med. 2011;72:185–92. doi: 10.1016/j.socscimed.2010.10.026. [DOI] [PubMed] [Google Scholar]