Abstract
Background
Parents of seriously ill children hold personal beliefs about what they should do to be good parents. How these beliefs change over time is unknown.
Objective
Describe the pattern of Good-Parent Beliefs over time, and determine whether parents’ hopeful patterns of thinking, affect, and perceived child’s health are associated with changes in beliefs at 12 and 24 months.
Methods
Our longitudinal sample included 124 parents of 100 children hospitalized with serious illness. We used latent transition models (LTM) to classify parents into groups with similar Good-Parent Beliefs during the baseline and follow-up periods, and modeled the change in good-parent beliefs over time as a function of covariates using generalized linear mixed models.
Results
Two parent belief profiles emerged from the LTM: Loved (“Making sure my child feels loved”, n=61 at baseline) and Informed (“Making informed decisions”, n=63 at baseline). At 12 months, 21 parents (20.4%) had moved into the Loved group and no parents transitioned to the Informed group. By 24 months, 8 parents transitioned to the Loved group and 4 to the Informed group (13.04%). Transition into the Loved group was associated with parents’ baseline degree of hopeful thinking and positive perceptions of child’s health at baseline.
Conclusion
Some parents change their parenting priorities over time. Hopeful patterns of thinking and perception of child health appear to predict change. Clinicians should regularly reevaluate Good-Parent Beliefs over time to promote priority-congruent dialogue.
Keywords: good-parent beliefs, children with serious illness, hopeful thinking, affect, perceived child health, change over time
Parents of seriously ill children hold strong personal beliefs about what they should do to be good parents.(1–4) These Good-Parent Beliefs can be seen as a lens or schema through which hopes for the child are viewed and evaluated(5, 6) or as a set of duties which a parent believes that a “good” parent must fulfill. Good-Parent Beliefs include prioritizing “making sure my child feels loved”, “focusing on my child’s health”, “making informed medical care decisions”, “advocating for my child with medical staff”, and “staying at my child’s side”.(2)
Over time Good-Parent Beliefs and parent hopes may interact and change in important ways as the child’s condition evolves and the parent potentially redefines their idea of what the duties of a good parent are in this situation.(7, 8) For instance, if a child’s condition worsens, parent hopes may become more concrete and short-term (e.g. focusing on getting through each day), or if a child’s condition improves, parental hopes may become more general and long-term (e.g. thinking about the child’s future life).(9) A previous study found that parents of children being treated for cancer reported learning to focus more on “being there” for the child (e.g. the importance of being present when the child was undergoing a painful procedure) and advocating for their child (e.g. asking for anesthesia during a spinal tap).(10) Another study found that Good-Parent Beliefs can play an important role at the end of life as parents find ways to fulfill their duty as a parent even as they accept that their child is dying.(11)
A clinician who understands what a given parent believes that “a good parent” should do may be able to support that parent more effectively. Little is known, however, about how specific Good-Parent Beliefs change over time, as prior studies have been retrospective or cross-sectional.(1–3) Additionally, these prior studies have not used advanced statistical approaches to examine how these Good-Parent Beliefs cluster together within parents (i.e. what Good-Parent Beliefs tend to go together for a given parent) and how that might change over time.
In the current, study, we characterized how Good-Parent Beliefs congregate into related sets of beliefs (specifically, grouping parents together who hold similar beliefs), and tested to see if parents’ beliefs change over time (that is, determining whether some parents’ beliefs changed such that they would be grouped with a different set of parents). We quantified the pattern of parents who transitioned to different sets of beliefs by 12 months or 24 months after the start of the study. We then examined whether factors known to influence decision making (i.e. level of hope, affect) might be associated with the transition from one set of Good-Parent Beliefs to another. Based on studies of changes in goals and hopes(8, 9, 12), we hypothesized that parents with higher levels of hopeful thinking, stronger affect (positive and negative), and more negative perceptions of child’s health status would be more likely to change Good-Parent Beliefs over time.
METHOD
The hospital’s Institutional Review Board approved the protocol for this study and all participants provided informed consent.
Participants
The sample included 124 parents from 100 families of hospitalized children from the Decision Making in Serious Pediatric Illness study, a mixed-methods prospective cohort study on parental decision making for children with serious illness conducted at The Children’s Hospital of Philadelphia (CHOP) from September 2010 to December 2014. “Parents” were defined as the adults who had primary decision-making responsibilities for the index patient, and included biological parents, adoptive or foster parents, and members of the extended family. Parents were eligible if they and their children met all of the following conditions: the child was a patient at CHOP; had been admitted to the Pediatric Intensive Care Unit (PICU), Neonatal Intensive Care Unit (NICU), Cardiac Intensive Care Unit (CICU), or had been referred to the Pediatric Advanced Care Team (PACT) for palliative care services; the patient’s attending physician thought that the patient had a serious illness and the parents would likely have to make a major medical decision in the next 12 to 24 months; the child was not able to make medical decisions due to age or impaired cognitive capacity; and the parents spoke English. Parents were not eligible if they were deemed by the physician to be emotionally overwhelmed by the clinical situation, did not speak English, or had lost custody rights; or if the child had died, had been discharged, had experienced a non-accidental injury, or if the physician thought the child might die within a month. Parents were asked to complete a 45–60 minute interview at baseline and twenty-minute interviews at 12 and 24 months. Additional details about recruitment have been reported previously.(2, 7)
Measures
The development of the 12-item Good-Parent Belief assessment has been described elsewhere.(2) The items are: (1) making sure my child feels loved, (2) focusing on my child’s health, (3) making informed medical care decisions, (4) advocating for my child with medical staff, (5) focusing on my child’s comfort, (6) focusing on my child’s quality of life, (7) putting my child’s needs above my own when making medical care decisions, (8) staying at my child’s side, (9) keeping a positive outlook, (10) focusing on my child having as long a life as possible, (11) focusing on my child’s spiritual well-being, and (12) keeping a realistic outlook.
Our methodology for measuring Good-Parent priorities differed across interview time periods. At baseline and 24 months, parents completed a discrete choice experiment in which they were shown subsets of the 12 items and asked to choose the best and worst items from each set of items.(2) After parents completed all of the 12 tasks within the discrete choice experiment, a rank ordering of the 12 Good-Parent items was estimated for each respondent. At the 12-month time period, parents were asked to list their top 5 priorities out of the 12 possible Good-Parent items.
Parents completed the Positive and Negative Affect Scale (PANAS) at baseline, 12 months, and 24 months to measure positive and negative affect.(13, 14) Parents completed The Adult Disposition Hope Scale at baseline, which includes subscales for agency thinking (an individual’s sense of being generally successful in achieving goals) and pathway thinking (an individual’s sense of being able to generate successful plans to achieve goals).(15)
Parents were asked at baseline to report the perceived child health status (rated on a scale from 1 to 10), parent age, race, ethnicity, educational level, marital status, employment status, financial difficulty, and type of health insurance.(2) Child characteristics included child age, child sex, whether the child had complex chronic conditions (based on the child’s diagnosis), whether the child was receiving consultative services from the palliative care team, and the child’s resuscitation status.
To make the analysis tractable given the sample size, we created binary versions of hopeful thinking, positive affect, and negative affect at each visit by using the median value as the cut-point. Similarly, we created a binary version of perceived child health status by classifying the values of 7 to 10 as better health and the remaining values as poorer health.
Analysis
Good Parent Belief Groups
Using baseline, 12 month, and 24 month Good-Parent Beliefs data, we first applied a latent transition model (LTM) to analyze how individuals in our cohort belonged to a “latent” Good-Parent Belief group based on their probability of shared beliefs over time, and whether individuals stayed in the same group or changed to another group over time.(16)
To use LTM methodology with a relatively small sample, we reduced the number of categories for parenting items. For each of the 12 items, we created a binary measure indicating if a parenting priority was chosen in the top 3 at that time period.
Models with two to four latent classes were run to determine the number of latent classes that not only provided optimal Akaike Information Criterion(17) and Bayesian Information Criterion(18) fit statistics but also provided the most conceptually clear and meaningful interpretation. We did not find a model that had uniformly lower values on all fit statistics, so we chose the 2-class model in order to avoid having small sample sizes in some latent classes and parenting priority categories. A chi-square test of measurement invariance of the item response probabilities across the three time points was found to be statistically non-significant, indicating that the parenting priorities in each group did not differ across the 3 time periods.
Using probability of group membership at each time generated by the latent transition model, we classified parents into latent class subgroups at baseline, 12, and 24 months based on the group to which they had the highest probability of membership. Our outcome measure was change in Good-Parent Beliefs, which was indicated by a transition from the baseline latent class group to the other class group by 12 months, or a transition in groups between 12 and 24 months.
Sample and Outcome Models
For the main DSPI study, we approached 295 parents; 200 enrolled; 124 parents had sufficient follow-up data for this analysis. Of the 76 parents excluded, 47 had a child who died after the baseline assessment; the remainder did not complete the visits. Of the 124 parents comprising the analytic sample, 21 did not complete the 12 month interview (17%) and 32 parents did not complete the 24 month interview (26%).
Because of concerns that study attrition was related to poorer outcomes or that parents with poorer outcomes would be more likely to drop out, we constructed two sets of models: 1) complete-data analysis using logistic generalized linear mixed models (GLMM) and 2) GLMMs for missing data in outcomes that are likely to be missing not at random (MNAR).(19) Prior to running the second set of models, we imputed missing baseline covariates using multiple imputation.(20)
Complete Case Analysis:
We used logistic GLMM for baseline predictors and to test if any of the individual psychological variables (hope, positive affect, negative affect, child health) were associated with a change in Good-Parent Beliefs by 12 or 24 months. Each logistic regression model used repeated measures data and included a random effect for each subject to account for subject-level variability in the outcome. All models included a fixed effect for the predictor of interest and time (0=12 months, 1=24 months). No statistically significant baseline predictor-time interactions were observed. The multivariable model included hopeful thinking, negative affect, and perceived child health status.
GLMMs for MNAR outcome data with multiple imputation for baseline covariates:
First, to address missing data of baseline covariates (at most 15% missing data) we conducted multiple imputation to generate ten imputed datasets using SAS Proc MI and later combined the regression results from the 10 datasets. Then to address the missing data of the outcome measures over time, which were likely to be MNAR, we used GLMMs which jointly model both the missing outcome indicators as well as the repeated measures outcomes. Logistic regression models were used to model all outcomes and missing indicators including a random effect for each subject. A separate model was used for each baseline covariate of interest as well as an additional model which includes all exposures of interest as predictors.
Statistical analysis was performed using SAS 9.4 (SAS Institute, Carey, NC). A two-sided p value of 0.05 was deemed statistically significant.
RESULTS
124 parents from 100 families had at least one year of follow-up data and multiple time points of data. (Table 1). The majority of the parents were mothers (73%), married or partnered (90%), White (86%), and non-Hispanic (91%). Five children of 6 parent participants (5%) died during the study.
Table 1.
Characteristics for parents and children by Good-Parent Belief group at baseline
| Parent Characteristics | Good-Parent Belief Groups | ||
|---|---|---|---|
| All (n= 124) |
Loved (n=61) |
Informed (n=63) |
|
| Parent Interviewed | |||
| Mother | 90 (72.58%) | 45 (73.77%) | 45(71.43%) |
| Father | 32(25.81%) | 14 (22.95%) | 18(28.57%) |
| Married/Partnered | 111 (89.52%) | 54 (88.52%) | 57 (90.48%) |
| Race | |||
| White | 107 (86.29%) | 54 (88.52%) | 53 (84.13%) |
| Black | 7 (5.65%) | 3 (4.92%) | 4 (6.35%) |
| Other | 10(8.06%) | 4 (6.56%) | 6 (9.52%) |
| Ethnicity: Hispanic | 11 (8.94%) | 6 (9.84%) | 5 (8.06%) |
| Full-time Employment | 68 (54.84%) | 33(54.10%) | 35 (55.56%) |
| Financial Hardship | 51 (41.46%) | 22 (36.67%) | 29 (46.03%) |
| College Education or more | 75 (60.48%) | 39 (63.93%) | 36(57.14%) |
| Positive Affect, mean (sd) | 34.39 (7.24) | 34.46 (6.67) | 34.32(7.81) |
| Negative Affect, mean (sd) | 27.51 (8.22) | 26.98 (8.59) | 28.02 (7.87) |
| Hope Total, mean (sd) | 53.06 (6.58) | 52.20(5.15) | 53.89 (7.67) |
| Hope Agency, mean (sd) | 26.81 (3.67) | 26.38 (3.33) | 27.22 (3.95) |
| Hope Pathway, mean (sd) | 26.25 (3.91) | 25.82 (2.94) | 26.67 (4.65) |
| Child Characteristics | |||
| Age | |||
| < 1 year | 58 (46.77%) | 27 (44.26%) | 31 (49.21%) |
| 1–9 years | 54 (43.55%) | 26 (42.62%) | 28 (44.44%) |
| 10–17 years | 12 (9.68%) | 8(13.11%) | 4 (6.35%) |
| Male | 74 (59.68%) | 38 (62.30%) | 36(57.14%) |
| Chronic Complex Condition* | |||
| Malignancy | 10(8.06%) | 5 (8.20%) | 5 (7.94%) |
| Metabolic | 13 (10.48%) | 8(13.11%) | 5 (7.94%) |
| Neurological | 48(38.71%) | 27 (44.26%) | 21 (33.33%) |
| Other | 35 (28.23%) | 21 (34.43%) | 14 (22.22%) |
| Renal | 12 (9.68%) | 6 (9.84%) | 6 (9.52%) |
| Respiratory | 68 (54.84%) | 34 (55.74%) | 34 (53.97%) |
| Health Status, Baseline, mean | 6.27 (2.50) | 6.24 (2.35) | 6.30 (2.65) |
| Palliative Care | 23 (18.85%) | 15 (25.42%) | 8 (12.70%) |
| DNAR | 3 (2.42%) | 2 (3.28%) | 1 (1.59%) |
| Child Died | 6 (4.84%) | 4 (6.56%) | 2(3.17%) |
Note that percentages add up to more than 100% because children may have more than one complex chronic condition.
Good-Parent Belief groups
Assignment to Good Parent Belief Groups
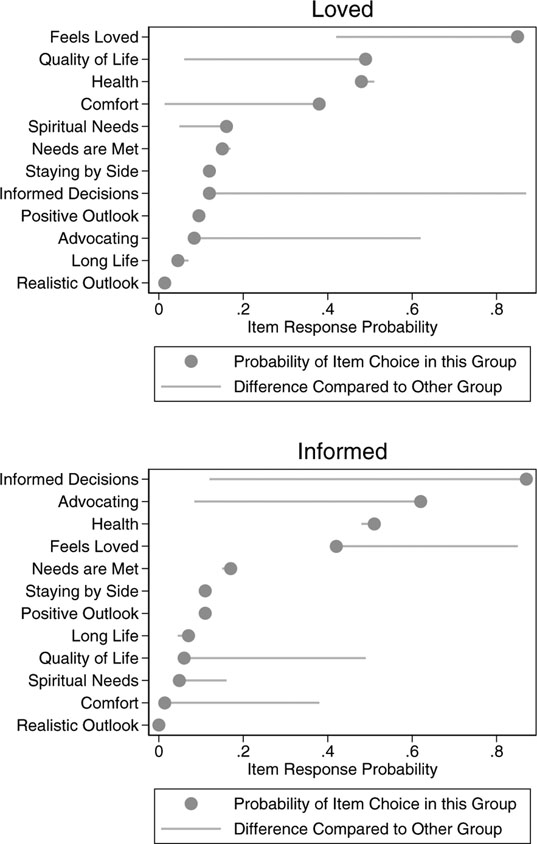
We identified two groups of parents based on their Good-Parent Beliefs (Figure 1) and calculated the item response probabilities for each group (the probability that a parent in a given group would endorse each item). Although top priorities for both groups of parents included “making sure my child feels loved” and “child’s health”, one group, Loved, placed highest priority on “making sure the child feels loved” (0.85), “child’s quality of life” (QOL) (0.49), “child’s health” (0.48), and “child’s comfort” (0.38). The other group, Informed, prioritized “making informed medical care decisions” (0.87), “advocating for the child” (0.62), “child’s health” (0.51), and “making sure child felt loved” (0.42).
Figure 1:
Good-Parent Belief item latent transition model based response probabilities for each group
Note: Item-response probabilities were constrained to be equal across baseline, 12, and 24 months.
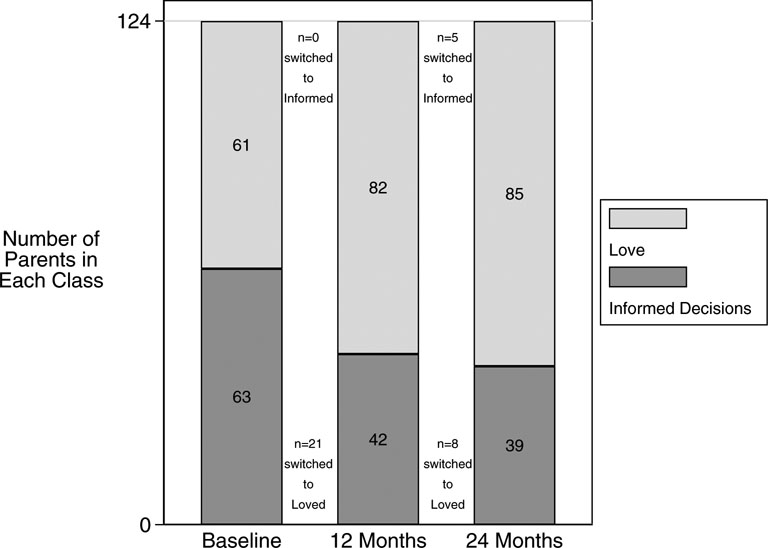
Transitions from one Good-Parent Belief group to another over time
At baseline there was an equal proportion of parents in each group (61 parents in Loved and 63 in Informed), but at the post-baseline follow-up times, more parents had shifted into the Loved group (Figure 2). At 12 months, 21 parents had transitioned from the Informed group to the Loved group, but there were no transitions in the other direction to Informed. From 12 to 24 months, one parent who had previously transitioned from the Informed group to the Loved group switched back to the Informed group, eight parents moved to the Loved group and 4 parents moved to the Informed group). Overall, 41 parents made at least one transition between baseline and 24 months.
Figure 2:
Number of parents transitioning to each Good-Parent belief group at each visit*
*Figure includes latent transition model-based estimates for 21 parents who did not have data at 12 months and 32 parents who did not have data at 24 months.
Outcome Analysis
The two sets of models (Complete Case Analysis and GLMMs for outcome data that are MNAR) did not show marked differences in results (Table 2). Therefore, in the following we focused on the results from GLMMs for outcome data that are MNAR.
Table 2:
Unadjusted univariable and adjusted multivariable association of baseline predictors and subsequent changes in Good-Parent Beliefs for complete case analyses and generalized linear mixed models for missing not at random (MNAR) outcome data.
| Complete Case Analysis | Generalized Linear Mixed Model for MNAR Outcome Data | |||
|---|---|---|---|---|
| OR 95% CI |
P-value | OR 95% CI |
P-value | |
| Univariable Models: | ||||
| Hope Total | 2.01 (0.92, 4.44) |
0.08 | 2.25 (0.93, 5.40) |
0.07 |
| Positive Affect | 1.22 (0.56, 2.65) |
0.61 | 1.32 (0.55,3.15) |
0.54 |
| Negative Affect | 1.70 (0.79, 3.69) |
0.17 | 1.60 (0.68, 3.77) |
0.29 |
| Child Health | 2.19 (0.98, 4.90) |
0.06 | 2.44 (1.00, 5.98) |
0.05 |
| Multivariable Model: | ||||
| Hope Total | 2.19 (0.97, 4.94) |
0.06 | 2.59 (1.03,6.48) |
0.03* |
| Negative Affect | 2.02 (0.90, 4.55) |
0.09 | 2.01 (0.81, 5.05) |
0.13 |
| Child Health | 2.35 (1.02,5.39) |
0.04* | 2.72 (1.09,6.84) |
0.04* |
p < 0.05
GLMMs for missing data in outcome that are MNAR with Imputed Baseline Data
Univariable Baseline Predictors of Change in Good-Parent Beliefs:
Parents with higher levels of hopeful thinking (hope total) and hopeful pathways thinking at baseline were moderately but not significantly more likely to change their Good-Parent Beliefs (OR=2.25, 95% CI: (0.93, 5.40), p=0.070, OR=2.21, 95% CI: (0.92, 5.30), p=0.075, respectively, Table 2), The agency hope subscale, positive affect, and negative affect were not associated with changes in Good-Parent Beliefs. Parents who perceived their children as healthier were more likely (but not significantly) to change their Good-Parent Beliefs (OR=2.44, 95% CI: (1.00, 5.98), p=0.051, Table 2).
Multivariable Adjusted Baseline Predictors of Change in Good-Parent Beliefs:
In the adjusted analysis, parents with higher levels of hopeful thinking (hope total) and who perceived their children as healthier at baseline were significantly more likely to change their Good-Parent Beliefs (OR=2.59, 95% CI: (1.03, 6.48), p=0.033, and OR=2.72, 95% CI: (1.09, 6.84), p=0.042 respectively, Table 2), after controlling for levels of negative affect. Parents with higher levels of negative affect at baseline were not more likely to change their Good-Parent Beliefs.
DISCUSSION
We found that almost 20% of parents of seriously ill children changed their Good-Parent Beliefs over time, from placing highest priority on “making informed medical decisions” and “advocating for my child” to “making sure my child feels loved” and “ focusing on my child’s comfort”. We found that the largest change over time happened at 12 months, which is consistent with our anecdotal clinical experience that parents go through the biggest adjustments in the first 4 – 12 months after a child’s hospitalization for serious illness. In addition, the changes at 12 months appeared to be stable, with only one parent switching back to their original Good-Parent Belief group at 24 months.
Our results are consistent with previous findings that parents of sick children find new ways to be a good parent over time, including being there for their child and advocating for their child.(10, 11) These findings are also consistent with studies finding that parents’ hopes change over time and that hopeful thinking and affect predict changes in parent decisions over time.(7, 9, 12) Our findings suggest that parents who are confident in their ability to generate strategies for achieving important goals (such as supporting their child through a serious illness) and who perceive that their child’s health is relatively good given their illness, will be more likely over time to think that the most important thing for a good parent to do is make sure their child feels loved. Alternatively, parents may have felt that their need to focus on making informed decisions lessened over time if their child’s health was improving.
Four aspects of our findings warrant discussion. First, the movement of parents from the Informed group to the Loved group does not necessarily mean that making informed decisions and advocating for their child’s medical needs became less important in an absolute sense. Because our Good-Parent Belief measures were relative, parents may have been increasing the priority of making the child feel loved while making informed decisions and advocacy remained important.
Second, our prediction that parents with higher levels of hopeful thinking and negative affect would be more likely to show changes in Good-Parent Beliefs over time was partially supported at 24 months. Follow-up analyses indicated that pathway hopeful thinking (the ability to think of approaches to a problem) was the strongest predictor of change in Good-Parent Beliefs over time. Pathways hopeful thinking may be more important than agency hopeful thinking (the belief that you personally can do something to change the situation) in this situation because parents have very little direct control over the child’s illness. Thinking of alternate ways to fulfill one’s duty as a good parent may be more important than confidence in one’s ability to be a good parent.
Third, while we did not find an overall significant effect for positive or negative affect, other research suggests affect may be involved in changing important beliefs. We have found in our previous work that hopes and concerns of parents of children with serious illness change over time.(7, 21) Negative affect is associated with more systematic, in-depth processing of available evidence(22), and may serve as an alarm signal that previously established beliefs, strategies, and goals need to be reevaluated.(23, 24) Positive affect may facilitate creative and flexible thinking and help individuals general new goals to work toward.(25, 26) Parents of children with serious illness who experience higher levels of negative and positive affect may be more likely to undergo this reevaluation process and form new beliefs about what goals are appropriate and how they should go about attaining them.(8)(27, 28)
Fourth and finally, an unexpected finding was that higher child health (versus lower) was associated with changing Good-Parent Beliefs. This finding should be interpreted in light of the fact that, in contrast to our earlier samples of parents of extremely sick children receiving palliative care (12), a greater proportion of children in this study of serious illness improved or stabilized over time and were discharged from the hospital. Accordingly, we likely have observed how Good-Parent Beliefs change as parents get past an immediate medical crisis in which the most important thing is making sure the child gets appropriate medical care and adjust to a longer-term situation of caring for a child with a chronic health condition.
One way for clinicians to provide effective decision support to parents of children with serious illness is explore the Good-Parent Beliefs of the parents and help parents find choices that align with their Good-Parent Beliefs.(29) Our study suggests that clinicians with long term relationships with parents should regularly reevaluate Good-Parent Beliefs over time, and, if warranted, tailor how they support parents in light of how these beliefs may be changing. A parent who initially only wanted to discuss treatment options and how to get better care for her child may over time be more interested in discussing ways to make her child more comfortable and increase her child’s quality of life.
This study has strengths and limitations that warrant mention. Strengths include a longitudinal assessment of psychological measures and Good-Parent Beliefs and use of a person-centered methodology to detect differences in subgroups of parents with different beliefs and different patterns of change over time. Our study findings were limited by the fact that all parents came from one institution, a relatively small sample size for the quantitative demands of a longitudinal analysis, and the length of time between visits, which leaves the possibility that parents made other transitions during the 12-month intervals that were not observed. The small sample size likely limited detection of other classes of Good-Parent Beliefs that emerged in our previously published baseline analyses. In order to minimize respondent burden, we also used a different technique to assess Good-Parent Beliefs at the 12-month visit, which may have influenced our results. Assigning parents to one Good-Parent Belief group at each time point may oversimplify parental priorities if parents have multiple priorities at the same time with some surfacing more or less at different moments. Lastly, our models did not adjust for post-baseline confounding variables occurring in the follow-up period, which might be related to changes in Good-Parent Beliefs and the other variables on the causal pathway. Future research could help build a more comprehensive conceptual model using a larger cohort with more complete parent and child data.
CONCLUSION
Some parents of children with serious illness change their parenting priorities over time. Hopeful patterns of thinking and perception of child health appear to predict or facilitate these changes. Clinicians should regularly reevaluate Good-Parent Beliefs over time in order to be able to engage in dialogue that is congruent with parents’ potentially changing priorities.
Acknowledgments
Funding for this project was provided by the National Institute of Nursing Research grant 1R01NR012026. We thank all parents who participated in this study and Pamela G. Nathanson for her comments on the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hinds PS, Oakes LL, Hicks J, et al. “Trying to be a good parent” as defined by interviews with parents who made phase I, terminal care, and resuscitation decisions for their children. J Clin Oncol 2009;27:5979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feudtner C, Walter JK, Faerber JA, et al. Good-parent beliefs of parents of seriously ill children. JAMA Pediatr 2015;169:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.October TW, Fisher KR, Feudtner C, Hinds PS. The Parent Perspective: “Being a Good Parent” When Making Critical Decisions in the PICU. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woodgate RL, Edwards M, Ripat JD, Borton B, Rempel G. Intense parenting: a qualitative study detailing the experiences of parenting children with complex care needs. BMC Pediatr 2015;15:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Markus H, Nurius P. Possible selves. American Psychologist 1986;41:954–969. [Google Scholar]
- 6.Eisenstadt D, Leippe MR, Rivers JA. Asymmetry and defense in self-comparison: Differential reactions to feedback about the rejected and ideal selves. Self and Identity 2002;1:289–311. [Google Scholar]
- 7.Hill DL, Nathanson PG, Fenderson RM, Carroll KW, Feudtner C. Parental Concordance Regarding Problems and Hopes for Seriously Ill Children: A Two-Year Cohort Study. J Pain Symptom Manage 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill DL, Miller V, Walter JK, et al. Regoaling: a conceptual model of how parents of children with serious illness change medical care goals. BMC palliative care 2014;13:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Granek L, Barrera M, Shaheed J, et al. Trajectory of parental hope when a child has difficult-to-treat cancer: a prospective qualitative study. Psycho-oncology 2013;22:2436–44. [DOI] [PubMed] [Google Scholar]
- 10.Kars MC, Duijnstee MS, Pool A, van Delden JJ, Grypdonck MH. Being there: parenting the child with acute lymphoblastic leukaemia. J Clin Nurs 2008;17:1553–62. [DOI] [PubMed] [Google Scholar]
- 11.Kars MC, Grypdonck MH, Beishuizen A, Meijer-van den Bergh EM, van Delden JJ. Factors influencing parental readiness to let their child with cancer die. Pediatr Blood Cancer 2010;54:1000–8. [DOI] [PubMed] [Google Scholar]
- 12.Feudtner C, Carroll KW, Hexem KR, et al. Parental hopeful patterns of thinking, emotions, and pediatric palliative care decision making: a prospective cohort study. Arch Pediatr Adolesc Med 2010;164:831–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology 1988;54:1063–1070. [DOI] [PubMed] [Google Scholar]
- 14.Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology 2004;43:245–265. [DOI] [PubMed] [Google Scholar]
- 15.Snyder CR, Harris C, Anderson JR, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 1991;60:570–85. [DOI] [PubMed] [Google Scholar]
- 16.Lanza ST, Collins LM. A new SAS procedure for latent transition analysis: transitions in dating and sexual risk behavior. Dev Psychol 2008;44:446–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akaike H A new look at the statistical model identification. IEEE Transactions on Automatic Control 1974;19:716–723. [Google Scholar]
- 18.Schwarz G Estimating the dimensions of a model. Annals of Statistics 1978;6:221–242. [Google Scholar]
- 19.Ibrahim JG, Chen MH, Lipsitz SR. Missing responses in generalised linear mixed models when the missing data mechanism is nonignorable. Biometrika 2001;88:551–564. [Google Scholar]
- 20.Rubin DB. Multiple Imputation for nonresponse in surveys, New York, NY: John Wiley & Sons, 1987. [Google Scholar]
- 21.Hill DL, Nathanson PG, Carroll KW, et al. Changes in Parental Hopes for Seriously Ill Children. Pediatrics 2018;141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwarz N, Clore GL. Feelings and phenomenal experiences In: Kruglanski AW, Higgins ET, eds. Social psychology: Handbook of basic principles, 2nd ed. New York: Guilford, 2007:385–407. [Google Scholar]
- 23.Carver CS, Scheier MF. Origins and functions of positive and negative affect: A control-process view. Psychological Review 1990;97:19–35. [Google Scholar]
- 24.Carver CS, Scheier MF. Scaling back goals and recalibration of the affect system are processes in normal adaptive self-regulation: understanding ‘response shift’ phenomena. Soc Sci Med 2000;50:1715–22. [DOI] [PubMed] [Google Scholar]
- 25.Carnevale PJ, Isen AM. The influence of positive affect and visual access on the discovery of integrative solutions in bilateral negotiation. Organizational Behavior and Human Decision Processes 1986;37:1–13. [Google Scholar]
- 26.Isen AM, Daubman KA, Nowicki GP. Positive affect facilitates creative problem solving. Journal of Personality and Social Psychology 1987;52:1122–1131. [DOI] [PubMed] [Google Scholar]
- 27.Larsen JT, Hemenover SH, Norris CJ, Cacioppo JT. Turning adversity to advantage: On the virtues of the coactivation of positive and negative emotions In: A psychology of human strengths: Fundamental questions and future directions for a positive psychology., Washington, DC, US: American Psychological Association, Washington, DC, 2003:211–225. [Google Scholar]
- 28.Elliot AJ, Thrash TM. Approach-avoidance motivation in personality: Approach and avoidance temperaments and goals. Journal of Personality and Social Psychology 2002;82:804–818. [DOI] [PubMed] [Google Scholar]
- 29.Hinds PS, Oakes LL, Hicks J, et al. Parent-clinician communication intervention during end-of-life decision making for children with incurable cancer. Journal of palliative medicine 2012;15:916–22. [DOI] [PMC free article] [PubMed] [Google Scholar]