Abstract
Background:
The United States is in the midst of an opioid overdose crisis. Little is known about the role of environmental factors in increasing risk of fatal opioid overdose.
Methods:
We conducted a case–crossover analysis of 3,275 opioid overdose deaths recorded in Connecticut and Rhode Island in 2014–2017. We compared the mean ambient temperature on the day of death, as well as average temperature up to 14 days prior to death, to referent periods matched on year, month, and day of week.
Results:
Low average temperature over the 3 to 7 days prior to death were associated with higher odds of fatal opioid overdose. Relative to 11°C, an average temperature of 0°C over the 7 days prior to death was associated with a 30% higher odds of death (OR: 1.3; 95% CI: 1.1–1.5).
Conclusions:
Low average temperature may be associated with higher risk of death due to opioid overdose.
Keywords: Drug Overdose, Temperature, Analgesics, Opioid, Fentanyl, New England
INTRODUCTION
The United States is experiencing an epidemic of opioid overdose with more than 300,000 opioid-related overdose deaths occurring since 2000.1,2 The rate of fatal opioid overdose continues to increase, driven largely by the involvement of highly potent synthetic opioids, such as fentanyl and its related analogs.3,4
Although the proximal causes of opioid overdose death are well studied,5 the risk of fatal drug overdose may be intensified by environmental exposures that influence the pharmacologic effects of substances.6–9 For example, previous research suggests that the risk of death from cocaine overdose is associated with higher outdoor temperatures,10–12 putatively because cocaine use increases core body temperature, decreases heat perception, and impairs sweating and skin blood flow, thus increasing the risk of hyperthermia on hot days.13 Opioids are also known to affect thermoregulation, reducing core temperature and the temperature thresholds for both shivering and vasoconstriction.14,15 Moreover, cold weather16 and opioids17 both promote respiratory depression, although whether opioids modify the respiratory response to cold weather has not been documented. Given the potential adverse interactions between cold weather and opioids, the risk of fatal opioid overdose may be increased at low temperatures. However, to our knowledge, this hypothesis has not been previously examined. Accordingly, we evaluated the association between daily changes in ambient temperature and acute risk of fatal opioid overdose in two states in New England (Connecticut and Rhode Island), hypothesizing that colder temperatures would be associated with higher risk of opioid overdose death.
METHODS
Data Sources
We conducted a retrospective case review of accidental drug overdose fatalities occurring in Connecticut and Rhode Island between January 1, 2014 and June 30, 2017.18,19 Deaths were considered to be confirmed accidental drug overdose fatalities if: (a) the death was pronounced in Connecticut or Rhode Island; (b) the final manner of death was deemed an accident by the medical examiner; and (c) a drug is listed on the death certificate as the primary cause of death or a significant contributing factor. For our analyses, cases were limited to those that listed an opioid on the death certificate. Data regarding the demographic characteristics of the decedent, toxicologic analyses, and circumstances of the overdose were abstracted from medical examiner files. As all patient data was de-identified, the study was deemed exempt from ethics review by the Rhode Island Department of Health.
We obtained daily estimates of population-weighted mean temperature and relative humidity for each of the 13 counties in the study area using a gridded meteorologic dataset as previously described.20 We linked a daily temperature time-series to each death by the recorded date of death and the reported county of overdose occurrence. Our primary hypothesis focused on the risk of opioid overdose death associated with average temperature on the day of death, but we also calculated the average temperature over the 1 to 14 days prior to death, given prior research demonstrating the cumulative associations between cold weather and mortality.21
Analytical Approach
We used a time-stratified case–crossover design22 to assess the association between ambient temperature and the odds of opioid overdose death. This method is suitable for evaluating the effects of time-varying exposures that transiently and acutely increase the risk of events with a clear onset time.23 In this design, each individual’s exposure immediately before the event is compared to that same individual’s exposure during referent periods in which the outcome did not occur (see eFigure). Because exposures during case and referent periods were matched within individuals, characteristics that were relatively stable over time (such as sex, race/ethnicity, socioeconomic status, living conditions, and medical history) did not confound the results.24
We matched each death to 3 or 4 referent days occurring in the same year, month, and day of week. This matching strategy enabled us to isolate the effect of short-term changes in temperature on risk of overdose death that were not confounded by seasonal patterns or other long-term time trends. We used conditional logistic regression to estimate odds ratios (OR) and 95% confidence intervals (CI) for the association, adjusting for relative humidity and federal holidays (as patterns of substance use may be different on federal holidays).25,26 To allow for potential non-linear exposure–response functions, we modeled temperature as a continuous variable using a natural cubic spline with three knots. We calculated all ORs relative to the median temperature observed during the study period (11°C). In a sensitivity analysis, we removed all deaths involving cocaine since the risk of fatal cocaine overdose may be elevated at high ambient temperatures.10–12 All analyses were conducted in R Studio (Version 1.1.456).
RESULTS
There were 3,275 documented opioid overdose deaths in Connecticut (n = 2,417) and Rhode Island (n = 858) during the study period, predominantly among males (73%, Table). One in three deaths were among individuals under 35 years old (35%). Opioid overdose deaths involved a median of two substances (IQR: 2–3), with a median of one opioid drug (IQR: 1–2) and one non-opioid drug (IQR: 0–2). The most common opioid drugs implicated were heroin (55%) and fentanyl and related analogs (46%), while the most common non-opioid drugs were alcohol (25%) and cocaine (26%).
Table.
Characteristics of unintentional drug overdose deaths involving opioids in Connecticut and Rhode Island, January 2014 to June 2017 (n = 3,275)
| Overall (n = 3,275) |
Connecticut (n = 2,417) |
Rhode Island (n = 858) |
|
|---|---|---|---|
| Year, % (n) | |||
| Jan. to Dec. 2014 | 21 (682) | 20 (474) | 24 (208) |
| Jan. to Dec. 2015 | 27 (884) | 26 (634) | 29 (250) |
| Jan. to Dec. 2016 | 34 (1118) | 35 (841) | 32 (277) |
| Jan. to June 2017 | 18 (591) | 19 (468) | 14 (123) |
| Age, % (n) | |||
| 18 to 24 years old | 8 (255) | 8 (182) | 9 (73) |
| 25 to 34 years old | 27 (870) | 26 (617) | 29 (253) |
| 35 to 44 years old | 23 (759) | 24 (579) | 21 (180) |
| 45 to 54 years old | 25 (820) | 25 (615) | 24 (205) |
| 55 years and older | 17 (571) | 18 (424) | 17 (147) |
| Sex, % (n) | |||
| Female | 27 (878) | 26 (629) | 2 (249) |
| Male | 73 (2397) | 74 (1788) | 71 (609) |
| Substances Involved (Opioids), % (n) | |||
| Heroin | 55 (1794) | 64 (1547) | 29 (247) |
| Fentanyl (includes fentanyl analogues) | 46 (1495) | 42 (1012) | 56 (483) |
| Oxycodone | 14 (471) | 15 (359) | 13 (112) |
| Methadone | 11 (359) | 11 (261) | 11 (98) |
| Substances Involved (Non-Opioids), % (n) | |||
| Alcohol | 25 (831) | 26 (631) | 23 (200) |
| Cocaine | 26 (844) | 25 (594) | 29 (250) |
| Alprazolam | 12 (405) | 13 (314) | 11 (91) |
| Clonazepam | 8 (254) | 9 (214) | 5 (40) |
| Diazepam | 6 (207) | 7 (167) | 5 (40) |
| Substances Involved (Median [IQR]) | |||
| Total Number of Drugs Involved | 2 (2–3) | 3 (2–3) | 2 (1–3) |
| Total Number of Opioid Drugs Involved | 1 (1–2) | 1 (1–2) | 1 (1–2) |
| Total Number of Non-Opioid Drugs Involved | 1 (0–2) | 1 (0–2) | 1 (0–2) |
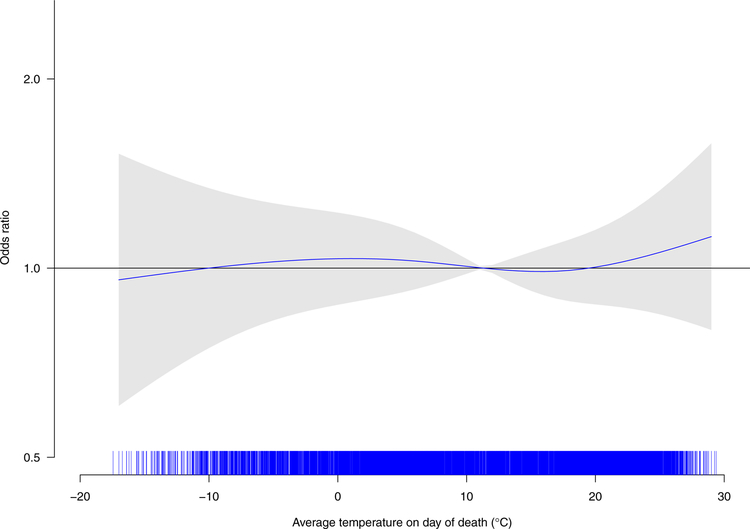
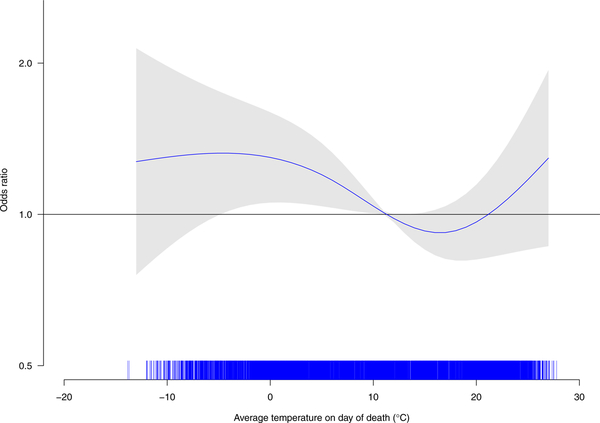
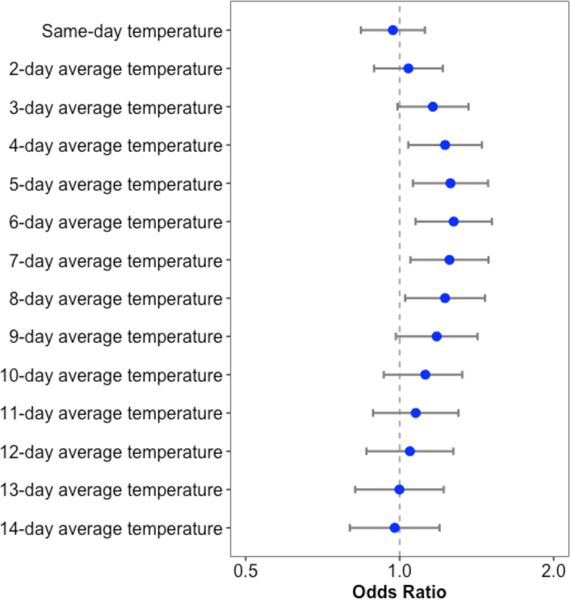
The association between temperature and risk of fatal opioid overdose appeared non-linear. Although there was no apparent association between low temperatures on the day of death and the risk of fatal opioid overdose (Figure 1A), low average temperatures averaged over 3 to 7 days prior to death (Figure 1 B) were associated with greater odds of death (Figure 2). For example, relative to 11°C, an average temperature of 0°C over the 7 days prior to death was associated with 30% higher odds of death (OR: 1.3; 95% CI: 1.1–1.5). Effect estimates were generally larger in sensitivity analyses excluding deaths also involving cocaine (eTable).
Figure 1.
Non-linear association of average temperature on the day of death (Panel A) and over the seven days (Panel B) prior to death with odds of opioid-involved overdose death in Connecticut and Rhode Island, January 2014 – June 2017 (n = 3,275)
Panel A
Panel B
Note: Case and referent periods were matched on year, month, and day of week and the association was adjusted for relative humidity and federal holidays.
Figure 2.
Odds of opioid-involved overdose death at an average temperature at 0°C relative to the odds of opioid-involved overdose death at an average temperature of 11°C among deaths occurring in Connecticut and Rhode Island, January 2014 – June 2017 (n = 3,275)
Note: Case and referent periods were matched on year, month, and day of week and all associations are adjusted for relative humidity and federal holidays.
DISCUSSION
Our findings provide preliminary evidence for an association between cold ambient temperatures and higher risk of opioid overdose death. Although this association has not been previously reported, there are several pathways by which cold weather may plausibly contribute to the risk of opioid overdose death. First, the combination of opioid use and cold temperatures may act in synergy to depress respiratory function, thereby increasing the risk of death by respiratory failure. Second, opioids may adversely impact users’ ability to thermoregulate during periods of cold weather, again raising the risk of death. Third, cold temperatures may alter patterns of drug use or impact networks of opioid supply and distribution. For example, opioid overdose deaths may be associated with cold weather if individuals are more likely to use opioids alone (i.e., in the absence of a bystander capable of administering the reversal agent naloxone if needed) during periods of cold weather. Similarly, cold weather may also alter patterns of drug trafficking and distribution, particularly during storms, potentially increasing the risk unintentional consumption of drugs adulterated with potent synthetic opioids. Further research should determine whether inclement weather or other noteworthy climatic events (e.g., blizzards) might explain some of the observed results.
Contrary to our primary hypothesis, cold temperature on the day of death was not associated with an increased likelihood of opioid overdose mortality. It is possible that this null association may be explained by some degree of misclassification regarding the timing of death, which is estimated during autopsy and may be inaccurate for some cases, particularly those that are not identified until several days after the overdose occurs. Nonetheless, our findings are consistent with the hypothesis that multiple days of cold weather exposure have a cumulative effect on fatal opioid overdose. The observed associations were also similar in sensitivity analyses restricted to deaths not involving cocaine. Nonetheless, future research is needed to quantify the extent to which observed associations may be altered in fatalities implicating multiple substances with varying impacts on thermoregulation.
These preliminary findings are not without limitation. First, the relatively small sample size limits statistical power, particularly at the extremes of temperature. Second, there are several sources of potential exposure classification, including a lack of knowledge about the geographic locations of individuals in the days leading up to death and whether individuals were indoors at the time of death. Third, the results may be subject to confounding by the presence of other meteorologic conditions. Fourth, we are unable to elucidate the mechanisms by which cold temperatures may alter the risk of opioid overdose death. Moreover, we are not able to distinguish whether cold temperatures are associated with the risk of experiencing an opioid overdose (regardless of whether or not it is fatal) rather than the risk of death conditional on experience of an opioid overdose. Fifth, the restriction of the sample to two states in New England may limit the generalizability of the results.
In summary, this study provides initial evidence that opioid overdose deaths are more common at lower temperatures. Further research is required to confirm or refute these findings, characterize associations in locations with varying weather patterns, and identify the potential pathways by which “cold snaps” may alter the risk of overdose death.
Supplementary Material
Acknowledgments:
We thank Jesse L. Yedinak, MPA and Jacqueline E. Goldman, BS for their research administrative assistance. We would also like to thank Lauren Brinkley-Rubenstein, PhD, Maximilian R.F. King, ScM; Alexandria Macmadu, ScM; Katherine M. Waye, MPH; Benjamin A. Bouvier, ScB; Jacqueline E. Goldman, BS; Elliott Liebling, AB; Esther Manu, BS; Jonathan Goyer; Connor Millard; and Kobe Pereira for their assistance with data abstraction and case file review at the Office of State Medical Examiners in Rhode Island.
Sources of Funding: This research was supported in part by a cooperative agreement between the National Center for Injury Prevention and Control and the Rhode Island Department of Health (U17CE002740; Principal Investigator: Jan Shedd, MEd). Dr. Weinberger is supported by a grant from the National Institute of Environmental Health Sciences (F32ES027742). Dr. Marshall is supported by a grant from the National Institute of General Medical Sciences (P20GM125507). Mr. Goedel is supported by the Brown University Clinical and Community-Based HIV/AIDS Research Training Fellowship funded by the National Institute of Mental Health (R25MH083620).
Footnotes
Conflicts of Interest: None declared.
Data Access: Given the sensitive nature of overdose deaths, the raw data used in this study on accidental drug-related deaths in Rhode Island cannot be made available. However, the raw data on accidental drug-related deaths in Connecticut is available online in the public domain from the Office of the Chief Medical Examiner. The raw data on ambient temperature is available online in the public domain from the PRISM Climate Group of Oregon State University. All R code used to generate the case–crossover dataset and fit the conditional logistic regression models are available in the Digital Repository of Brown University.
References
- 1.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(50–51):1445–1452. [DOI] [PubMed] [Google Scholar]
- 2.Seth P, Scholl L, Rudd RA, Bacon S. Overdose deaths involving opioids, cocaine, and psychostimulants - United States, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67(12):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Donnell JK, Gladden RM, Mattson CL, Kariisa M. Notes from the field: Overdose deaths with carfentanil and other fentanyl analogs detected - 10 states, July 2016-June 2017. MMWR Morb Mortal Wkly Rep. 2018;67(27):767–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700 – 10 states, July-December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brady JE, Giglio R, Keyes KM, DiMaggio C, Li G. Risk markers for fatal and non-fatal prescription drug overdose: A meta-analysis. Inj Epidemiol. 2017;4(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rowe C, Santos G-M, Vittinghoff E, Wheeler E, Davidson P, Coffin PO. Neighborhood-level and spatial characteristics associated with lay naloxone reverse events and opioid overdose deaths. J Urban Health. 2016;93(1):117–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cerdá M, Ransome Y, Keyes KM, et al. Revisiting the role of the urban environment in substance use: The case of analgesic overdose fatalities. Am J Public Health. 2013;103(12):2252–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nandi A, Galea S, Ahern J, Bucciarelli A, Vlahov D, Tardiff K. What explains the association between neighborhood-level income inequality and the risk of fatal overdose in New York City? Soc Sci Med. 2006;63(3):662–674. [DOI] [PubMed] [Google Scholar]
- 9.Bohnert ASB, Nandi A, Tracy M, et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marzuk PM, Tardiff K, Leon AC, et al. Ambient temperature and mortality from unintentional cocaine overdose. JAMA. 1998;279(22):1795–1800. [DOI] [PubMed] [Google Scholar]
- 11.Bohnert AS, Prescott M, Vlahov D, Tardiff KJ, Galea S. Ambient temperature and risk of death from accidental drug overdose in New York City, 1990–2006. Addiction. 2010;105(6):1049–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Auger N, Bilodeau-Bertrand M, Labesse ME, Kosatsky T. Association of elevated ambient temeprature with death from cocaine overdose. Drug Alcohol Depend. 2017;178:101–105. [DOI] [PubMed] [Google Scholar]
- 13.Crandall CG, Vongpatanasin W, Victor RG. Mechanism of cocaine-induced hyperthermia in humans. Ann Intern Med. 2002;136(11):785–791. [DOI] [PubMed] [Google Scholar]
- 14.Kurz A, Go JC, Sessler DI, Kaer K, Larson MD, Bjorksten AR. Alfentanil slightly increases the sweating threshold and markedly reduces the vasoconstriction and shivering thresholds. Anesthesiology. 1995;83(2):293–299. [DOI] [PubMed] [Google Scholar]
- 15.Sessler DI. Opioids and postoperative shivering. J Clin Anesth. 2016;31:42–43. [DOI] [PubMed] [Google Scholar]
- 16.Cheshire WP. Thermoregulatory disorders and illness related to heat and cold stress. Auton Neurosci. 2016;196:91–104. [DOI] [PubMed] [Google Scholar]
- 17.Gupta K, Prasad A, Nagappa M, Wong J, Abrahamyan L, Chung FF. Risk factors for opioid-induced respiratory depression and failure to rescue: A review. Curr Opin Anaesthesiol. 2018;31(1):110–119. [DOI] [PubMed] [Google Scholar]
- 18.Marshall BDL, Yedinak JL, Goyer J, Green TC, Koziol JA, Alexander-Scott N. Development of a statewide, publicly accessible drug overdose surveillance and information system. Am J Public Health. 2017;107(11):1760–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green TC, Grau LE, Carver HW, Kinzly M, Heimer R. Epidemioogic trends and geographic patterns of fatal opiod intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 2011;115(3):221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spangler KR, Weinberger KR, Wellenius GA. Suitability of gridded climate datasets for use in environmental epidemiology. J Expo Sci Environ Epidemiol. 2018; Available online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Analitis A, Katsouyanni K, Biggeri A, et al. Effects of cold weather on mortality: Results from 15 European cities within the PHEWE Project. Am J Epidemiol. 2008;168(12):1397–1408. [DOI] [PubMed] [Google Scholar]
- 22.Janes H, Sheppard L, Lumley T. Case–crossover analyses of air pollution exposure data: Referent selection strategies and their implications for bias. Epidemiology. 2005;16(6):717–726. [DOI] [PubMed] [Google Scholar]
- 23.Maclure M The case–crossover design: A method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144–153. [DOI] [PubMed] [Google Scholar]
- 24.Maclure M, Mittleman MA. Should we use a case–crossover design? Annu Rev Public Health. 2000;21:193–221. [DOI] [PubMed] [Google Scholar]
- 25.Lai FY, Bruno R, Hall W, et al. Profiles of illicit drug use during annual key holiday and control periods in Australia: Wastewater analysis in an urban, a semi-rural, and a vacation area. Addiction. 2013;108(3):556–565. [DOI] [PubMed] [Google Scholar]
- 26.Lloyd B, Matthews S, Livingston M, Jayasekara H, Smith K. Alcohol intoxication in the context of major public holidays, sporting and social events: A time-series analysis in Melbourne, Australia, 2000–2009. Addiction. 2013;108(4):701–709. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.