Abstract
BACKGROUND:
Planning for mass critical care in resource-poor and constrained settings has been largely ignored, despite large, densely crowded populations who are prone to suffer dis-proportionately from natural disasters. As a result, disaster response has been suboptimal and in many instances hampered by lack of planning, education and training, information, and communication.
METHODS:
The Resource-Poor Settings panel developed five key question domains; defining the term resource poor and using the traditional phases of the disaster cycle (mitigation/preparedness/response/recovery). Literature searches were conducted to identify evidence to answer the key questions in these areas. Given a lack of data on which to develop evidence-based recommendations, expert-opinion suggestions were developed, and consensus was achieved using a modified Delphi process.
RESULTS:
The five key questions were as follows: definition, capacity building and mitigation, what resources can we bring to bear to assist/surge, response, and reconstitution and recovery of host nation critical care capabilities. Addressing these led the panel to offer 33 suggestions. Because of the large number of suggestions, the results have been separated into two sections: part I, Infrastructure/Capacity in the accompanying article, and part II, Response/Recovery/Research in this article.
CONCLUSIONS:
A lack of rudimentary ICU resources and capacity to enhance services plagues resource-poor or constrained settings. Capacity building therefore entails preventative strategies and strengthening of primary health services. Assistance from other countries and organizations is often needed to mount a surge response. Moreover, the disengagement of these responding groups and host country recovery require active planning. Future improvements in all phases require active research activities.
Summary of Suggestions
Response
-
1
We suggest developing countries or health-care systems employ an appropriate incident command system to organize the pre-hospital, transportation and in-hospital response effort.
-
2
We suggest early in the response effort that attempts be made to estimate the needs beyond acute care and to inform and guide providers of rehabilitation and prolonged care needs.
-
3
We suggest host nation rehabilitation and pro-longed care capabilities that are likely to exist following the disaster be considered when deter- mining the appropriateness of initiating critical intensive care.
-
4
We suggest only critical care providers with previous training or expertise in disaster response, or those who are aligned with experienced groups (eg, foreign medical teams), and invited by the host nation deploy to support a disaster.
-
5
We suggest if not available at the time of a disaster, critical care be instituted using an intensive care model with providers skilled in critical care medicine.
-
6
We suggest government and non-governmental organizations (NGOs) collaborate with military health-care systems (with their experience in operating in austere conditions) for process and procedure sharing as well as to establish linkages to facilitate the sharing of patient care.
-
7
We suggest all deploying response teams employ simple, pre-established, and standardized data collection tools in order to meet the needs of local authorities, increase accountability of care, and facilitate review of care provided during the event.
Reconstitution/Recovery of Host Nation Critical Care Capabilities and Disengagement
-
8During strategic disengagement of surge resources and reconstitution of emergency and critical care services in resource-poor settings post-disaster, we suggest:
- 8a. Forming partnerships and close coordination between surge teams and pre-existing stakeholders (local government officials, medical and surgical care providers, rehabilitation-related NGOs, local and national public health) to ensure a successful transition,
- 8b. Assessing the access to and capacity of local emergency and critical care services once the surge resources leave,
- 8c. Addressing the disaster’s impact on health-care providers’ and surviving patients’ short and long-term mental health needs,
- 8d. Developing and using standardized data collection instruments to facilitate assessment and validation of best practices for effective disengagement and reconstitution, and to monitor on-going long-term health needs,
- 8e. Implementing a tailored approach to disengagement and reconstitution based on the identified local community’s needs,
- 8f. Addressing local logistical challenges to deliver emergency and critical care routinely and during disasters,
- 8g. Ensuring that public health programs are restored and improved and that reconstitution efforts do not displace essential public health activities, which may have greater impact upon the overall community’s health, especially for children,
- 8h. Integrating emergency and critical care services with the delivery of all other medical care and public health programs in the community,
- 8i. Including long-term follow-up care to the maximum extent possible in planning for the medical needs of survivors; and
- 8j. Incorporating the training and staffing needs for provision of all needed post disaster services, including medical, nursing, social workers, mental health providers, community and public health.
Research Considerations
-
9
We suggest research focus on health monitoring/ syndromic surveillance, needs assessment, prognostication, and cost effectiveness to help establish care priorities.
-
10
We suggest cost-effectiveness studies on critical care in developing countries to justify the need and ability to advocate for resources to provide basic critical care.
Quality Improvement Factors:
-
11
We suggest developing countries and health-care organizations institute quality improvement programs, in part to justify to donors, population, and government that increases in investment in health systems provide cost effective benefits.
Innovative Treatments and Technologies:
-
12
We suggest professional critical care societies advise and support research that brings new technologies and diagnostic tools to resource-poor settings and stress adapting diagnostic and treatment modalities to this environment in a cost effective and efficient manner.
-
13
We suggest professional critical care societies advise and guide the development of disaster related protocols to study pressing issues relating to diagnosis, treatment, and systems improvement and have these vetted through ethics committees and other groups a priori in order to rapidly deploy them during or following an event.
Introduction
Planning for mass critical care (MCC) in resource-limited settings has been largely ignored, despite large densely crowded populations who are prone to suffer disproportionately from natural disasters. In these settings, crisis standards of care are a regular if not a daily reality. Addressing MCC in these settings has the potential to benefit large populations and to also inform planning in better-resourced areas. In addition, an approach that works well in one country may work less well in another, and not all approaches are equally acceptable to all governments or their multiple constituencies. There is no one blueprint for an ideal health-care system, nor is there a panacea that will automatically elicit improved performance.1 This is hardly surprising: Health-care systems are complex social systems, and the success of any one approach will depend on the system into which it is intended to fit as well as on its consistency with local values and ideologies. In fact, the need to modify World Health Organization (WHO) protocols and the need to work cooperatively within an integrated model with local authorities, especially when local infrastructure is even partially intact, is highlighted by the recent experience with Typhoon Yolanda in the Philippines.2 Thus, how these suggestions are implemented is best left to the local authorities. Given this background, the Resource-Poor Settings group of the Task Force for Mass Critical Care examined support to natural crises or pandemics. In “Resource-Poor Settings: Infrastructure and Capacity Building” by Geiling et al3 in this consensus statement, we addressed definitions and preparation for disasters. In this article, we address response and recovery phases as well as research. Although these issues primarily relate to clinicians, administrators and policy makers, engagement is important for success, and hence this manuscript is directed at all involved. Moreover, the involvement of ethicists in all stages is an absolute necessity to ensure care priorities are ethical and fair.
Materials and Methods
The Resource-Poor Settings panel developed five key question domains, and literature searches were conducted to identify an evidence base on which to answer the key questions (see e-Appendix 1 for search terms and literature results if sufficient evidence found). Searches were limited to 2007 to 2013; English-language and non-English-language papers were included. Given the lack of data upon which to develop evidence-based recommendations, expert-opinion suggestions were developed, with consensus achieved using a modified Delphi process. This process was in adherence with the American College of Chest Physicians (CHEST) Guidelines Oversight Committee’s methodology; full details of the methodology used may be found in the ”Methodology” article by Ornelas et al4 this consensus statement.
Results
The term “developing country” is used throughout this manuscript to indicate a developing or underdeveloped country. Progress in health-care response, rehabilitation, and recovery in developing countries has been slow or even regressed because of many barriers external to health care, such as the presence of war, conflict, economic strife, environmental changes, or other socioeconomic catastrophes.5 Response is further limited by poor infrastructure and lack of trained staffing, capacity, and coordination. Critical care under these circumstances differs significantly from that in developed countries and involves the provision of care for life-threatening illness without regard to the location, including the prehospital, emergency outpatient care, and hospital wards, and likely without ICUs and capabilities.
Response
1. We suggest developing countries or health-care systems employ an appropriate incident command system to organize the pre-hospital, transportation and in-hospital response effort.
Greater resiliency in the health-care system prior to a large-scale natural disaster or pandemic facilitates a mass casualty response. Hence, improving primary and basic emergency care and building public health capacity can improve disaster response.6 Capacity building and improved basic care are especially important in resource-poor areas where intensive care is limited. The international community has a role to play in predisaster preparedness, as demonstrated in the 2010 Haiti earthquake, where this involvement was sorely needed. Indeed, predisaster planning can maximize the results of international assistance and decrease the seemingly inevitable human and material tolls from disasters.7
Response efforts also require resources to be available in a timely manner. As previously noted in the “Resource-Poor Settings: Infrastructure and Capacity Building” article by Geiling et al3 in this consensus statement, prepositioned, stored emergency materials and teams may effectively streamline disaster response efforts. Especially in events in which critical care needs are surgical, prepositioned resources and infrastructure to support integration of foreign medical teams (FMTs) with existing surgical teams improves overall surgical services and overall public health.8
The international response to the earthquake in Bam, Iran, in 2003 was substantial but inefficient, partly because of lack of an international incident command system to orchestrate the response effort.9,10 In comparison, at the 1998 US Embassy bombings in Kenya and Tanzania, effective response efforts were partially attributed to an organized hospital response, which included an appropriate incident command system.11
2. We suggest early in the response effort that attempts be made to estimate the needs beyond acute care and to inform and guide providers of rehabilitation and prolonged care needs.
3. We suggest host nation rehabilitation and pro-longed care capabilities that are likely to exist following the disaster be considered when deter-mining the appropriateness of initiating critical intensive care.
Often the intensive care capabilities of responding groups exceed those of the resource-poor host nation. As a result, patients may survive the acute event but require prolonged rehabilitation and special requirements (such as chronic ventilation or dialysis) that the host nation is unable to support. In this situation, critical care responders face the dilemma of continuing care indefinitely or choosing to withdraw care. Thus, rehabilitation needs and availability must be considered before initiating advanced intensive care support.12–15 Although “dialyzer reuse protocols” have been useful during disasters such as the Haiti earthquake, this approach does not address the long-term needs of patients (see the “Special Populations” article by Dries et al16 in this consensus statement).
4. We suggest only critical care providers with previous training or expertise in disaster response, or those who are aligned with experienced groups, and invited by the host nation deploy to support a disaster.
Disaster response to critical care needs in a developing country occurs at the behest of the affected nation or region and comes from a variety of governmental, nongovernmental, foreign national, faith-based, and other organizations. The response usually is driven by disaster-specific injury patterns and is requested by assessment groups at the scene, as occurred in Haiti.17,18 However, FMTs rarely arrive in time to provide immediate trauma care. Additionally, disaster relief and health donations typically do not follow WHO guidelines, and often local medical volunteers are available but are not linked to medical supplies and logistic support.19 Thus, an appropriate response requires a systematic approach to coordinating the care.20 The WHO Regional Organization establishes a Health Cluster in which FMTs register and report on a regular basis. Other recognized Clusters, such as water, sanitation, and shelter, fall under the auspices of the United Nations Secretariat’s Office for the Coordination of Humanitarian Affairs.
Many disaster responders come from academic medical centers or groups without prior experience and arrive ill prepared to function in a resource-poor setting. For instance, although skilled in the provision of trauma care, many do not know how to adjust or adapt those skills to an austere environment or appreciate the complexities of care in patients with tropical diseases; understand the political, historical, or cultural back-ground contributing to the disaster; or understand humanitarian core competencies, such as international humanitarian law. Professionalism in disaster response calls for flexibility; training and coordination rather than good intentions are highlighted in response to the recent experience during Typhoon Haiyan in the Phillipines.2,21 Prior to deploying, responders must undergo specific training in unique injury patterns as well as the cultural setting and the nuances of disaster relief to ensure personal and group safety.22
5. We suggest if not available at the time of a disaster, critical care be instituted using an intensive care model with providers skilled in critical care medicine.
In the 2010 earthquake in Haiti, the highest proportion of deaths occurred in children, and admission to an ICU, either with or without trauma, was significantly associated with a high risk of death.23 In such a setting, critical care needs may be substantial and may divert scarce resources from other areas. The use of intensivist-directed teams of critical care providers has been shown to improve mortality in resource-poor settings.24 However, critical care providers should be skilled to practice in a resource-poor environment where equipment and supplies may be unfamiliar or in short supply. A quick primer guide, in addition to other organization training as noted in suggestion 20 of in the “Resource-Poor Settings: Infrastructure and Capacity Building” article by Geiling et al3 in this consensus statement, is useful.25
6. We suggest government and NGOs collaborate with military health-care systems (with their experience in operating in austere conditions) for process and procedure sharing as well as to establish linkages to facilitate the sharing of patient care.
Military critical care in wartime provides critical care in austere settings using trained personnel, standardized practices, and equipment, supported where possible with aeromedical evacuation.26 Military forces also provide subject matter experts (including communications, engineering, logistics, transportation, security, and medical) in the immediate chaos that often follows a disaster.27,28 The military also may be the only resource available to assist in medical evacuation of critically ill patients.29
7. We suggest all deploying response teams employ simple, pre-established, and standardized data collection tools in order to meet the needs of local authorities, increase accountability of care, and facilitate review of care provided during the event.
Complete, efficient, and standard documentation of patient care data, especially surgical data collected by FMTs, exists in the larger NGOs, such as the International Committee of the Red Cross and Médecins Sans Frontières (Doctors Without Borders).25 Standardized data collection would ensure all teams contribute relevant information to meet the needs of local authorities and the WHO Health Cluster and would increase accountability of care, thereby facilitating review of care provided.30
Reconstitution/Recovery of Host Nation Critical Care Capabilities and Disengagement
8. During strategic disengagement of surge resources and reconstitution of emergency and critical care services in resource-poor settings post-disaster, we suggest:
8a. Forming partnerships and close coordination between surge teams and pre-existing stakeholders (local government officials, medical and surgical care providers, rehabilitation-related NGOs, local and national public health) to ensure a successful transition,
8b. Assessing the access to and capacity of local emergency and critical care services once the surge resources leave,
8c. Addressing the disaster’s impact on health-care providers’ and surviving patients’ short and long-term mental health needs,
8d. Developing and using standardized data collection instruments to facilitate assessment and validation of best practices for effective disengagement and reconstitution, and to monitor on-going long-term health needs,
8e. Implementing a tailored approach to disengage-ment and reconstitution based on the identified local community’s needs,
8f. Addressing local logistical challenges to deliver emergency and critical care routinely and during disasters,
8g. Ensuring that public health programs are restored and improved and that reconstitution efforts do not displace essential public health activities, which may have greater impact upon the overall community’s health, especially for children,
8h. Integrating emergency and critical care services with the delivery of all other medical care and public health programs in the community,
8i. Including long-term follow-up care to the max-imum extent possible in planning for the medical needs of survivors; and
8j. Incorporating the training and staffing needs for provision of all needed post disaster services, including medical, nursing, social workers, mental health providers, community and public health.
Reconstitution of emergency and critical care services after a disaster is extremely challenging in developing countries. Indeed, recovery may take several years following major disasters, even in high-resource settings.31 The lack of adequate baseline emergency and critical care services in resource-poor environments further impedes critical care service recovery after a disaster.5,32 In fact, access and capacity of preexisting emergency and critical care medical practice may be further limited with disengagement and withdrawal of supply chains.33–35 Before a disaster, such services may have been supported by NGOs or other international groups rather than by local providers.36,37 These parties may not be available in the aftermath of a disaster, highlighting the need to identify partners to help with reconstitution and disengagement.38,39
Mental health care or mental and physical rehabilitation services may also be nonexistent or restricted even at baseline in resource-poor settings.40–43 Thus, postdisaster treatment of emotional and psychologic trauma and physical rehabilitation are less likely to be offered, with long-lasting deleterious consequences.
Evidence to guide emergency and critical care services’ disengagement and reconstitution in resource-poor settings is scant and derived mostly from high-resource settings.44 Accordingly, it is prudent to initiate efforts to establish an evidence base. Yet emergency and critical care services are just one of competing needs in the health-care system that must be prioritized. The success of preventative and primary care programs also relies on confidence in acute care services.32,45 The recovery and reconstitution phase, therefore, is an opportunity to expand and improve basic emergency and critical care services.
Research Considerations
9. We suggest research focus on health monitoring/syndromic surveillance, needs assessment, prognostication, and cost effectiveness to help establish care priorities.
10. We suggest cost-effectiveness studies on critical care in developing countries to justify the need and ability to advocate for resources to provide basic critical care.
To improve country-specific education and training in developing countries, research should focus on needs assessment, prognostication, and cost-effective treatments and methods of caring for critically ill patients.46 Unfortunately, research in small hospitals may be difficult.47 With this lack of information, critical care services are often considered too costly or complicated for resource-poor settings. Yet some of the most effective critical care interventions, including oxygen, fluid resuscitation, early antibiotics, and patient monitoring, are relatively inexpensive.32 In the developing world, where many critically ill patients are younger and have fewer comorbidities, critical care presents a remarkable opportunity to provide significant incremental benefit, more so than in the developed world.32 Integrating emergency care into existing health-care systems will ideally rely on modest investments to augment current models of primary health-care delivery.48
These research suggestions focus on general critical care rather than MCC in resource-poor settings. However, research in the noncrisis period has a dual effect of enhancing both nondisaster, everyday critical care as well as improving all aspects of MCC during a crisis.49
Quality Improvement Factors:
11. We suggest developing countries and health-care organizations institute quality improvement programs, in part to justify to donors, population, and government that increases in investment in health systems provide cost effective benefits.
Health-care leaders have suggested that quality improvement (QI) activities have the potential to optimize the use of limited resources targeted at achieving shared aims. For example, simple QI tools, including plan-do-study-act cycles and process maps, were useful in rural Africa in improving performance and resource aid decisions.50 The WHO has developed a field-tested toolkit that contains adaptable instruments, including a framework for QI, evidence-based clinical guidelines in the form of the Pocket Book of Hospital Care for Children.51 QI activities may also encourage greater investment in the health systems of developing countries by increasing donor, population, and governmental confidence that resources are being used appropriately.52
Innovative Treatments and Technologies:
12. We suggest professional critical care societies advise and support research that brings new technologies and diagnostic tools to resource-poor settings and stress adapting diagnostic and treatment modalities to this environment in a cost effective and efficient manner.
13. We suggest professional critical care societies advise and guide the development of disaster related protocols to study pressing issues relating to diagnosis, treatment, and systems improvement and have these vetted through ethics committees and other groups a priori in order to rapidly deploy them during or following an event.
Research into the most cost-effective treatments and methods of caring for critically ill patients is urgently needed. Professional critical care associations in the developed world should support operational research that brings new technologies and diagnostic tools and adapts crucial diagnostic and treatment modalities to this environment. This should be done by developing simplified tools and guidelines, ensuring engagement with regulatory bodies, and mobilizing community health workers. In the developing world, prevention should be a high priority. Development assistance from wealthier nations must therefore shift away from its present donor-driven agendas to country-driven, sector-wide approaches to development with sufficient accountability and sustainability.53 Arguably, a strong political will is necessary at all levels of government.54,55
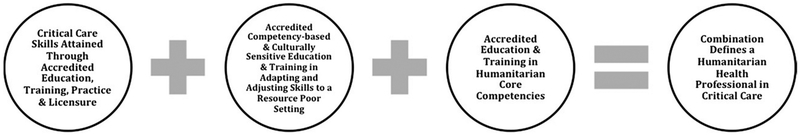
Areas for Future Research/Interventions/Limitations
MCC responders should receive special training. The professionalization of humanitarian health workers is a regionally supported, worldwide movement that relies on competency-based curricula provided by academic-affiliated training centers and trainers.56–58 Completion of the accredited training results in a certificate of completion that is placed in a professional registry available to NGOs and international organizations that employ and deploy health workers. The system also allows the health-care provider to add new training and field experiences to their personal registry “passport.”49–52 Competencies and crisis standards of care for health specialists being developed in anesthesia, mental health, physical medicine and rehabilitation, critical care (see the “Engagement and Education” article by Devereaux et al59 in this consensus statement), surgery, and other such activities must include ways to adjust and adapt their specialty skills to the resource-poor setting and learn the humanitarian core competencies that are crucial when working in an environment with multiple NGOs, international organizations, national agencies, and FMTs, among others60,61 (Fig 1).62
Figure 1 –
Humanitarian health workers without prior field experience responding to crises in developing countries should have attained accredited education and training in adapting and adjusting their skills to a resource-poor country as well as a knowledge base in humanitarian core competencies. Such training is available from many accredited academic centers and professional specialty associations and societies. (Adapted with permission from Johnson et al.62)
Conclusions
Resource-poor settings offer a unique challenge to the provision of MCC to vulnerable victims. However, by better defining those at risk, we can begin to build greater capacity and resilience. In these settings, recovery and reconstitution capabilities may be severely limited. Knowing these limitations early in a disaster response will guide patient-care activities that can be supported once response groups disengage. Future MCC efforts in resource-poor settings require more evidence-based actions and quality improvement initiatives. Only through the application of such research and process improvement tools can the victims of large-scale disasters or pandemics garner the benefits of the response and recovery efforts.
Supplementary Material
Acknowledgments
FUNDING/SUPPORT: This publication was supported by the Cooperative Agreement Number 1U90TP00591–01 from the Centers of Disease Control and Prevention, and through a research sub award agreement through the Department of Health and Human Services grant Number 1 - HFPEP070013-01-00 from the Office of Preparedness of Emergency Operations. In addition, this publication was supported by a grant from the University of California–Davis.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts: Dr West receives research funding from the National Institutes of Health, the Wellcome Trust, the Doris Duke Charitable Foundation, the Defense Threat Reducation Agency, the Firland Foundation, and the Henry M. Jackson Foundation. The remaining authors report that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The American College of Chest Physicians was solely responsible for the development of these guidelines. The remaining supporters played no role in the development process. External supporting organizations cannot recommend panelists or topics, nor are they allowed prepublication access to the manuscripts and recommendations. Further details on the Conflict of Interest Policy are available online at http://chestnet.org.
ABBREVIATIONS:
- FMT
foreign medical team
- MCC
mass critical care
- NGO
nongovernmental organization
- QI
quality improvement
- WHO
World Health Organization
Footnotes
COI grids reflecting the conflicts of interest that were current as of the date of the conference and voting are posted in the online supplementary materials.
DISCLAIMER: American College of Chest Physicians guidelines and consensus statements are intended for general information only, are not medical advice, and do not replace professional care and physician advice, which always should be sought for any medical condition. The complete disclaimer for this consensus statement can be accessed at http://dx.doi.org/10.1378/chest.1464S1.
Endorsements: This consensus statement is endorsed by the American Association of Critical-Care Nurses, American Association for Respiratory Care, American College of Surgeons Committee on Trauma, International Society of Nephrology, Society for Academic Emergency Medicine, Society of Critical Care Medicine, Society of Hospital Medicine, World Federation of Pediatric Intensive and Critical Care Societies, World Federation of Societies of Intensive and Critical Care Medicine.
Additional information: The e-Appendix can be found in the Supplemental Materials section of the online article.
References
- 1.Mills A Health care systems in low- and middle-income countries. N Engl J Med. 2014;370(6):552–557. [DOI] [PubMed] [Google Scholar]
- 2.Merin O, Kreiss Y, Lin G, Pras E, Dagan D. Collaboration in response to disaster—Typhoon Yolanda and an integrative model. N Engl J Med. 2014;370(13):1183–1184. [DOI] [PubMed] [Google Scholar]
- 3.Geiling J, Burkle FM Jr, Amundson D, et al. ; on behalf of the Task Force for Mass Critical Care. Resource-poor settings: infrastructure and capacity building: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4_suppl):e156S–e167S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ornelas J, Dichter JR, Devereaux AV, Kissoon N, Livinski A, Christian MD; on behalf of the Task Force for Mass Critical Care. Methodology: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4_suppl):35S–41S. [DOI] [PubMed] [Google Scholar]
- 5.Leaning J, Guha-Sapir D. Natural disasters, armed conflict, and public health. N Engl J Med. 2013;369(19):1836–1842. [DOI] [PubMed] [Google Scholar]
- 6.Dünser MW, Baelani I, Ganbold L. A review and analysis of intensive care medicine in the least developed countries. Crit Care Med. 2006;34(4):1234–1242. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin E, Bassily-Marcus AM, Babu E, Silver L, Martin ML. Principles and practice of disaster relief: lessons from Haiti. Mt Sinai J Med. 2011;78(3):306–318. [DOI] [PubMed] [Google Scholar]
- 8.McIntyre T, Hughes CD, Pauyo T, et al. Emergency surgical care delivery in post-earthquake Haiti: Partners in Health and Zanmi Lasante experience. World J Surg. 2011;35(4):745–750. [DOI] [PubMed] [Google Scholar]
- 9.Abolghasemi H, Radfar MH, Khatami M, Nia MS, Amid A, Briggs SM. International medical response to a natural disaster: lessons learned from the Bam earthquake experience. Prehosp Disaster Med. 2006;21(3):141–147. [DOI] [PubMed] [Google Scholar]
- 10.United States Department of Labor. Incident command system. Occupational Safety & Health Administration website. https://www.osha.gov/SLTC/etools/ics/. Published 2013. Accessed September 16, 2013, 2013.
- 11.Abdallah S, Heinzen R, Burnham G. Immediate and long-term assistance following the bombing of the US Embassies in Kenya and Tanzania. Disasters. 2007;31(4):417–434. [DOI] [PubMed] [Google Scholar]
- 12.Xie J, Du L, Xia T, Wang M, Diao X, Li Y. Analysis of 1856 inpatients and 33 deaths in the West China Hospital of Sichuan University from the Wenchuan earthquake. J Evid Based Med. 2008;1(1):20–26. [DOI] [PubMed] [Google Scholar]
- 13.Huffman JL. Surgical palliative care in Haiti. Surg Clin North Am. 2011;91(2):445–457. [DOI] [PubMed] [Google Scholar]
- 14.Lei BL, Zhou Y, Zhu Y, et al. Emergency response and medical rescue in the worst hit Mianyang areas after the Wenchuan earthquake. J Evid Based Med. 2008;1(1):27–36. [DOI] [PubMed] [Google Scholar]
- 15.Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y. The Israeli field hospital in Haiti—ethical dilemmas in early disaster response. N Engl J Med. 2010;362(11):e38. [DOI] [PubMed] [Google Scholar]
- 16.Dries DJ, Reed MJ, Kissoon N, et al. ; on behalf of the Task Force for Mass Critical Care. Special populations: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4_suppl):e75S–e86S. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC). Post-earthquake injuries treated at a field hospital — Haiti, 2010. MMWR Morb Mortal Wkly Rep. 2011;59(51):1673–1677. [PubMed] [Google Scholar]
- 18.Murakami H, Paramitasari D, Ohno R. Human casualty and damage distribution in relation to seismic intensity in the 2006 central Java earthquake in Indonesia. Paper presented at: Proceedings of 14th World Conference on Earthquake Engineering; October 12–17, 2008; Beijing, China. [Google Scholar]
- 19.de Ville de Goyet C. Health lessons learned from the recent earthquakes and Tsunami in Asia. Prehosp Disaster Med. 2007;22(1):15–21. [DOI] [PubMed] [Google Scholar]
- 20.Macias DJ, Williams J. Austere, remote, and disaster medicine missions: an operational mnemonic can help organize a deployment. South Med J. 2013;106(1):89–93. [DOI] [PubMed] [Google Scholar]
- 21.Cranmer HH, Biddinger PD. Typhoon Haiyan and the profession-alization of disaster response. N Engl J Med. 2014;370(13):1185–1187. [DOI] [PubMed] [Google Scholar]
- 22.Archer N, Moschovis PP, Le PV, Farmer P. Perspective: postearthquake Haiti renews the call for global health training in medical education. Acad Med. 2011;86(7):889–891. [DOI] [PubMed] [Google Scholar]
- 23.Dulski TM, Basavaraju SV, Hotz GA, et al. Factors associated with inpatient mortality in a field hospital following the Haiti earthquake, January-May 2010. Am J Disaster Med. 2011;6(5):275–284. [DOI] [PubMed] [Google Scholar]
- 24.Grathwohl KW, Venticinque SG. Organizational characteristics of the austere intensive care unit: the evolution of military trauma and critical care medicine; applications for civilian medical care systems. Crit Care Med. 2008;36(suppl 7):S275–S283. [DOI] [PubMed] [Google Scholar]
- 25.Jawa RS, Heir JS, Cancelada D, Young DH, Mercer DW. A quick primer for setting up and maintaining surgical intensive care in an austere environment: practical tips from volunteers in a mass disaster. Am J Disaster Med. 2012;7(3):223–229. [DOI] [PubMed] [Google Scholar]
- 26.Venticinque SG, Grathwohl KW. Critical care in the austere environment: providing exceptional care in unusual places. Crit Care Med. 2008;36(suppl 7): S284–S292. [DOI] [PubMed] [Google Scholar]
- 27.Burkle FM Jr, Argent AC, Kissoon N; Task Force for Pediatric Emergency Mass Critical Care. The reality of pediatric emergency mass critical care in the developing world. Pediatr Crit Care Med. 2011;12(suppl 6):S169–S179. [DOI] [PubMed] [Google Scholar]
- 28.Dressler DP, Hozid JL. Austere military medical care: a graded response. Mil Med. 1994;159(3):196–201. [PubMed] [Google Scholar]
- 29.Grissom TE, Farmer JC. The provision of sophisticated critical care beyond the hospital: lessons from physiology and military experiences that apply to civil disaster medical response. Crit Care Med. 2005;33(suppl 1):S13–S21. [DOI] [PubMed] [Google Scholar]
- 30.Burkle FM Jr, Nickerson JW, von Schreeb J, et al. Emergency surgery data and documentation reporting forms for sudden-onset humanitarian crises, natural disasters and the existing burden of surgical disease. Prehosp Disaster Med. 2012;27(6):577–582. [DOI] [PubMed] [Google Scholar]
- 31.Kates RW, Colten CE, Laska S, Leatherman SP. Reconstruction of New Orleans after Hurricane Katrina: a research perspective. Proc Natl Acad Sci U S A. 2006;103(40):14653–14660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riviello ED, Letchford S, Achieng L, Newton MW. Critical care in resource-poor settings: lessons learned and future directions. Crit Care Med. 2011;39(4):860–867. [DOI] [PubMed] [Google Scholar]
- 33.Molyneux EM. Paediatric emergency care in resource-constrained health services is usually neglected: time for change. Ann Trop Paediatr. 2010;30(3):165–176. [DOI] [PubMed] [Google Scholar]
- 34.Baelani I, Jochberger S, Laimer T, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. 2011;15(1):R10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Belle J, Cohen H, Shindo N, et al. Influenza preparedness in low-resource settings: a look at oxygen delivery in 12 African countries. J Infect Dev Ctries. 2010;4(7):419–424. [DOI] [PubMed] [Google Scholar]
- 36.Pfeiffer J International NGOs and primary health care in Mozambique: the need for a new model of collaboration. Soc Sci Med. 2003;56(4):725–738. [DOI] [PubMed] [Google Scholar]
- 37.Gill Z, Ahmed JU. Experience from Bangladesh: implementing emergency obstetric care as part of the reproductive health agenda. Int J Gynaecol Obstet. 2004;85(2):213–220. [DOI] [PubMed] [Google Scholar]
- 38.Degennaro V Jr, Degennaro V Sr, Ginzburg E. Haiti’s dilemma: how to incorporate foreign health professionals to assist in short-term recovery while capacity building for the future. J Public Health (Oxf). 2011;33(3):459–461. [DOI] [PubMed] [Google Scholar]
- 39.Hotz GA, Moyenda ZB, Bitar J, et al. Developing a trauma critical care and rehab hospital in Haiti: a year after the earthquake. Am J Disaster Med. 2012;7(4):273–279. [DOI] [PubMed] [Google Scholar]
- 40.Saraceno B, van Ommeren M, Batniji R, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370(9593):1164–1174. [DOI] [PubMed] [Google Scholar]
- 41.Kay E, Kilonzo C, Harris MJ. Improving rehabilitation services in developing nations: the proposed role of physiotherapists. Physiotherapy. 1994;80(2):77–82. [Google Scholar]
- 42.Landry MD, O’Connell C, Tardif G, Burns A. Post-earthquake Haiti: the critical role for rehabilitation services following a humanitarian crisis. Disabil Rehabil. 2010;32(19): 1616–1618. [DOI] [PubMed] [Google Scholar]
- 43.Rauch A, Baumberger M, Moise FG, von Elm E, Reinhardt JD. Rehabilitation needs assessment in persons with spinal cord injury following the 2010 earthquake in Haiti: a pilot study using an ICF-based tool. J Rehabil Med. 2011;43(11):969–975. [DOI] [PubMed] [Google Scholar]
- 44.Jacob ST, Lim M, Banura P, et al. Integrating sepsis management recommendations into clinical care guidelines for district hospitals in resource-limited settings: the necessity to augment new guidelines with future research. BMC Med. 2013;11:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. [PMC free article] [PubMed] [Google Scholar]
- 46.Hyder AA, Dawson L. Defining standard of care in the developing world: the intersection of international research ethics and health systems analysis. Dev World Bioeth. 2005;5(2):142–152. [DOI] [PubMed] [Google Scholar]
- 47.English M, Irimu G, Wamae A, et al. Health systems research in a low-income country: easier said than done. Arch Dis Child. 2008;93(6):540–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Anthony DR. Promoting emergency medical care systems in the developing world: weighing the costs. Glob Public Health. 2011;6(8):906–913. [DOI] [PubMed] [Google Scholar]
- 49.Ortiz JR, Rudd KE, Clark DV, Jacob ST, West TE. Clinical research during a public health emergency: a systematic review of severe pandemic influenza management. Crit Care Med. 2013;41(5):1345–1352. [DOI] [PubMed] [Google Scholar]
- 50.Kotagal M, Lee P, Habiyakare C, et al. Improving quality in resource poor settings: observational study from rural Rwanda. BMJ. 2009;339:b3488. [DOI] [PubMed] [Google Scholar]
- 51.Burkle FM Jr. Do pandemic preparedness planning systems ignore critical community- and local-level operational challenges? Disaster Med Public Health Prep. 2010;4(1):24–29. [DOI] [PubMed] [Google Scholar]
- 52.Bremer R Policy development in disaster preparedness and management: lessons learned from the January 2001 earthquake in Gujarat, India. Prehosp Disaster Med. 2003;18(4):372–384. [DOI] [PubMed] [Google Scholar]
- 53.Onen CL. Medicine in resource-poor settings: time for a paradigm shift? Clin Med. 2004;4(4):355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ehiawaguan IP. Mass casualty incidents and disasters in Nigeria: the need for better management strategies. Niger Postgrad Med J. 2007;14(4):341–346. [PubMed] [Google Scholar]
- 55.Kapiriri L, Martin DK. Bedside rationing by health practitioners: a case study in a Ugandan hospital. Med Decis Making. 2007;27(1):44–52. [DOI] [PubMed] [Google Scholar]
- 56.Walker P, Hein K, Russ C, Bertleff G, Caspersz D. A blueprint for professionalizing humanitarian assistance. Health Aff (Millwood). 2010;29(12):2223–2230. [DOI] [PubMed] [Google Scholar]
- 57.Walker P, Russ C. Fit for purpose: the role of modern profession-alism in evolving the humanitarian endeavour. International Review of the Red Cross. 2011;93(884):1193–1210. [Google Scholar]
- 58.Burkle FM, Walls AE, Heck JP, et al. Academic affiliated training centers in humanitarian health, part I: program characteristics and professionalization preferences of centers in North America. Prehosp Disaster Med. 2013;28(2):155–162. [DOI] [PubMed] [Google Scholar]
- 59.Devereaux AV, Tosh PK, Hick JL, et al. ; on behalf of the Task Force for Mass Critical Care. Engagement and education: care of the critically ill and injured during pandemics and disasters: CHEST consensus statement. Chest. 2014;146(4_suppl):e118S–e133S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Burkle FM Jr. The development of multidisciplinary core competencies: the first step in the professionalization of disaster medicine and public health preparedness on a global scale. Disaster Med Public Health Prep. 2012;6(1):10–12. [DOI] [PubMed] [Google Scholar]
- 61.Chackungal S, Nickerson JW, Knowlton LM, et al. Best practice guidelines on surgical response in disasters and humanitarian emergencies: report of the 2011 Humanitarian Action Summit Working Group on Surgical Issues within the Humanitarian Space. Prehosp Disaster Med. 2011;26(6):429–437. [DOI] [PubMed] [Google Scholar]
- 62.Johnson K, Idzerda L, Baras R, et al. Competency-based standardized training for humanitarian providers: making humanitarian assistance a professional discipline. Disaster Med Public Health Prep. 2013;7(4):369–372. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.