Abstract
This paper explores the concept that reducing general psychopathology early in the life course provides unprecedented opportunities to prevent the development of all forms of psychopathology later in life. We review empirical evidence for the existence of the general factor of psychopathology and theories regarding the psychological nature of the factor. We then highlight specific examples of environmental risk factors for general psychopathology and discuss translational implications for the transdiagnostic prevention of psychopathology beginning in early childhood. Ultimately, we propose a developmentally informed and transdiagnostic stepped care approach to intervention in which reduction of general psychopathology in early childhood represents the foundational step for prevention and intervention of subsequent psychopathology. This model heralds three key benefits over the current treatment Zeitgeist: (1) Reducing the burden and confusion in healthcare and education systems by providing a coherent and systematic structure for early intervention across a child's development, (2) maximising the breadth of the impact of intervention by focusing on common shared risks across psychopathology, and (3) increasing the efficiency of intervention by corresponding with the development of psychopathology and leveraging the emergence of general psychopathology in early childhood.
Keywords: General psychopathology, p factor, Transdiagnostic psychopathology, Prevention, Intervention, Developmental psychopathology
When considering risk factors for psychopathology in early childhood and beyond, a hierarchical model of psychopathology offers a flexible and integrative framework. Research in the context of this framework has increasingly converged on evidence for a general factor of psychopathology that provides a helpful construct for understanding systematic patterns of co-occurrence among symptom domains of psychopathology at the broadest and most general level of abstraction. Effects of non-specific etiologic factors that increase risk for all symptom domains can also be understood from this perspective.
This paper explores the opportunities for prevention of all forms of psychopathology by reducing general psychopathology, which represents a novel and compelling target for interventions starting at a very early age. In structuring this conceptual paper, we first review empirical evidence for the existence of the general factor of psychopathology and current theories regarding the psychological nature of this factor. We then highlight specific examples of risk for general psychopathology—with an emphasis on early childhood risk factors—and discuss translational implications for the broad prevention of psychopathology beginning in early childhood. Ultimately, we propose a developmentally informed transdiagnostic stepped care approach to intervention, which heralds several benefits over the current status quo.
1. Evidence for a meaningful general factor of psychopathology
Mental disorders are traditionally conceptualized in terms of hundreds of discrete and putatively separate categories. This is the type of approach taken in authoritative nosologies; most notably, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (i.e., DSM-III, DSM-IV, and DSM-5; APA, 2013). However, these mental disorder categories tend to co-occur at levels much higher than chance. From a categorical standpoint, this phenomenon has been termed “co-morbidity,” reflecting the idea that two putatively distinct “categorical forms of morbidity” (mental disorders) have co-occurred. In fact, “multi-morbidity” is a more accurate term for what is observed, because essentially all DSM-defined mental disorders covary at rates higher than chance (e.g., Kessler, Chiu, et al., 2005).
The observation that diverse forms of psychopathology co-occur at high rates gave rise to efforts to model the multivariate patterns empirically. This is now a topic of substantial interest in the psychopathology literature. Earlier literature in this area focused specifically on mental disorders known to be relatively common in the general population, as observed in large, community-based epidemiologic samples. Statistical models of the patterns of co-occurrence among common mental disorders generally converged on the idea that mood and anxiety disorders can be understood as elements within a broad internalizing spectrum, and substance use and antisocial disorders can be understood as elements within a broad externalizing spectrum (see e.g., Krueger & Markon, 2006 for a review). Although recent literature has focused on DSM categories, this structural approach to psychopathology began in many ways with Achenbach and Edelbrock’s (1978, 1984) seminal work on the patterns of co-occurrence among common psychopathological syndromes in childhood. The structural approach has recently expanded to integrate maladaptive personality and a wide variety of common and less common mental disorders (see Kotov et al., 2017; Krueger et al., 2018 for recent reviews). We focue here on the developmentally coherent elements that tend to emerge in statistical models of the structure of common mental disorders shown in Fig. 1 (see Forbes, Tackett, Markon, & Krueger, 2016 for a review).
Fig. 1.
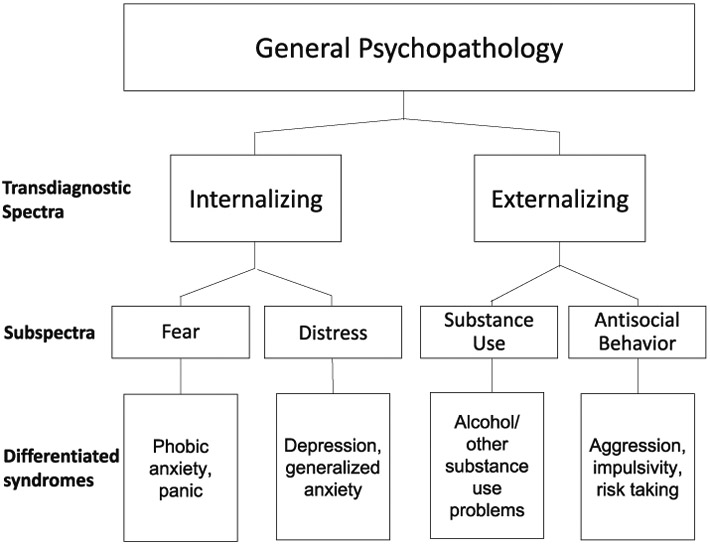
An adaptation of the Hierarchical Taxonomy of Psychopathology (HiTOP) model (Kotov et al., 2017), summarizing selected elements that tend to emerge in statistical models of the structure of common mental disorders across development. Kotov, Krueger, Watson et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454-477. 2017. American Psychological Association. Adapted with permission.
Kotov et al. (2017) recently proposed the Hierarchical Taxonomy of Psychopathology (HiTOP) model to summarize the extant literature on the structural approach to psychopathology, emphasising the importance of a dimensional and hierarchical model to classify mental disorders empirically. The evidence for these two features—recently reviewed in Krueger et al. (2018)—underpins the idea of a “general factor of psychopathology”. First, that each dimension of psychopathology (e.g., general psychopathology, internalizing, or fear in Fig. 1) is indeed dimensional, rather than categorical, representing a continuous spectrum of risk and severity. Individuals at the low end of a given spectrum have low risk for symptoms of psychopathology in that domain, whereas individuals at the high end have high risk for multiple persistent and/or severe symptoms (see Forbes et al., 2016 for a more detailed discussion). Second, while essentially all DSM-defined mental disorders are correlated, they show different degrees of positive association. For example, mood, anxiety, substance use, and antisocial disorders are all positively correlated, but mood and anxiety disorders are more correlated with each other than they are with substance use and antisocial disorders (and vice versa). These patterns of association give rise to the internalizing and externalizing spectra described above, but also mean that the emergent internalizing and externalizing spectra are notably correlated. Various authors (e.g., Caspi et al., 2014; Lahey et al., 2012; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011) suggested that this internalizing-externalizing correlation—together with the consistent positive correlations among mental disorders—might be well-understood by the existence of a very broad dimension connecting essentially all forms of psychopathology; that is, a general factor of psychopathology. Caspi et al. (2014) referred to this concept as the p-factor to highlight the similarity to the g-factor (i.e., general intelligence) in the study of individual differences in cognitive ability (Spearman, 1904). Several recent papers have explored how the HiTOP framework can be integrated with mental health research (Conway et al., 2019), psychotherapy (Hopwood et al., 2019), and clinical assessment and practice more broadly (Ruggero et al., in review).
There are various potential ways to statistically model a hierarchy of individual differences, with a general factor at the apex of this hierarchy. For example, influential papers from Lahey et al. (2012) and Caspi et al. (2014) have proposed a bifactor modelling approach that involves a general factor that saturates all indicators (e.g., a general factor manifest in all types of psychopathology observed in a sample), and more specific factors that are independent of general psychopathology and manifest only in specific types of psychopathologies. In this modelling framework, an internalizing factor would be set up to be entirely uncorrelated with indicators of an overarching general factor as well as a complementary externalizing factor. The bifactor model is often found to statistically fit slightly better than other models, but commonly used fit indices have been found to be biased in favour of the bifactor model (Greene et al., 2019) indicating that these findings of superior fit are likely not trustworthy. Further, these minor differences in model fit are not as important as construct validity for specific purposes (e.g., Watts, Poore, & Waldman, 2019). Ultimately, the hierarchical approach we depict here is technically a different type of statistical model, but because the general factor in both types of models is indicated by all the psychopathologies observed in the sample, they are very similar variables.
Conceptually, the patterns of association described above are best accommodated by the hierarchical model in which a general factor is at the top of a more variegated hierarchical model of psychopathology—subdivided into increasingly finer-grained dimensions, as in Fig. 1. Clinically, a core idea of this model is that three people suffering different specific forms of psychopathology (e.g., depression, generalized anxiety, and phobic anxiety) have shared underlying features (e.g., negative affect) that cut across the boundaries of these syndromes and can be captured in a transdiagnostic dimension (e.g., internalizing). In the same way, features that are shared across all forms of psychopathology can be mapped onto the general factor of psychopathology. This general factor may thus provide a novel and compelling target for the primary prevention of psychopathology, particularly given it can be observed reliably in children as young as three years old (Olino et al., 2018), and from childhood to adolescence, with predictive validity and stability throughout adulthood (e.g., Greene & Eaton, 2017; Murray, Eisner, & Ribeaud, 2016; Snyder, Young, & Hankin, 2017a).
2. Can we target the general factor of psychopathology to prevent psychopathology?
The idea of the general factor of psychopathology has been of substantial interest in recent literature (see Lahey, Krueger, Rathouz, Waldman, & Zald, 2017 for a recent review), including consideration of its possible indications for clinical level treatment (Caspi & Moffitt, 2018). Clinical treatment directed at general psychopathology across a range of life stages could provide a parsimonious and focused target for very broad transdiagnostic intervention. One exciting avenue that has not been explicated to date is whether this general factor might also prove useful in working to prevent psychopathology in a more coherent manner. If all forms of common psychopathology are connected with a general underlying factor that can be observed from the very earliest years of development, then understanding the psychological nature of that general factor as well as factors that increase its levels may provide new directions in contemplating how to reduce levels of the general factor and subsequently prevent a wide range of mental disorders from emerging later in development. A psychological level of enquiry is particularly fitting, given that evidence for the existence of the general factor has been identified primarily from the patterns of co-occurrence among psychopathological signs and symptoms, as reviewed above (see also Jones et al., 2018 and Selzam, Coleman, Caspi, Moffitt, & Plomin, 2018 for examples of molecular and behavioural genetic evidence for the general factor; and Romer et al., 2018 and Snyder, Hankin, Sandman, Head & Davis, 2017 for examples of neural evidence for the general factor). Specifically, when considering how we might reduce levels of the general factor, we are first interested in the question: What are the psychological and environmental factors that increase an individuals’ risk for general psychopathology early in life?
2.1. The psychological nature of general psychopathology
There are two recent prominent theories that elucidate the psychological factors underlying general psychopathology. For example, DeYoung and Krueger (2018) suggested a cybernetic theory of psychopathology—that is, that psychopathology is characterized by both difficulty in pursuing important psychological goals effectively, and failure to adapt to changes in the environment. This theory draws on the interrelationships among normal and maladaptive personality traits, and highlights how an overarching model of personality interfaces with psychopathology (cf. Oltmanns, Smith, Oltmanns, & Widiger, 2018). Specifically, DeYoung and Krueger emphasize high levels of neuroticism, low levels of agreeableness, and low levels of conscientiousness as the consistent personality correlates of general psychopathology (see also Caspi et al., 2014). Another theory, proposed by Carver, Johnson, and Timpano (2017), is that impulsive reactivity to emotion is the core underlying process of general psychopathology. These theories converge on a consistent set of psychological processes underlying propensity towards general psychopathology, highlighting that this vulnerability lies not only in prominent negative emotionality, but also in predispositions towards impulsive failures to take others’ perspectives into account, and to take broad life considerations into account (i.e., high neuroticism, low agreeableness, and low conscientiousness, respectively).
Temperamental precursors to these personality dispositions emerge in infancy, and have moderate stability through early childhood and adulthood (e.g., Caspi, 2000; Caspi, Roberts, & Shiner, 2005; McCrae et al., 2000; Rothbart, Ahadi, & Evans, 2000; Smart & Sanson, 2005). Specific examples include the correspondence between both reactivity and negative affectivity in early childhood with subsequent neuroticism, and between both disinhibition and low effortful control in early childhood with subsequent conscientiousness (Clark, 2005; De Pauw & Mervielde, 2010). Correspondingly, high negative affectivity and low effortful control have both been found to be associated with the general factor of psychopathology in children (Hankin, Davis, Snyder, Young, Glynn, & Sandmann, 2017). Together, these findings provide insight into opportunities for psychological interventions at the level of general psychopathology beginning early in life, as discussed in detail below.
2.2. Environmental risks for general psychopathology
In addition to psychological factors that increase risk for high levels of a general psychopathology factor, there is also a growing literature on environmental risks. A salient example is research on varied experiences of childhood adversity—including abuse, maltreatment, victimisation, harsh parenting, domestic violence, parental dysfunction, and chronic life stress—that have all been found to confer risk across multiple transdiagnostic dimensions of psychopathology (Albott, Forbes, & Anker, 2018; Conway, Raposa, Hammen, & Brennan, 2018; Forbes, Magson, & Rapee, 2019; Jaffee, Moffitt, Caspi, Taylor, & Arsenault, 2002; Keyes et al., 2012; Meyers et al., 2015; Schaefer et al., 2018; Snyder, Young, & Hankin, 2017b; Vachon, Krueger, Rogosch, & Cicchetti, 2015; Wiggins, Mitchell, Hyde, & Monk, 2015). Executive dysfunction in childhood and adolescence has also recently been found to map onto general psychopathology, rather than individual symptom domains (Bloemen et al., 2018; Snyder, Friedman, & Hankin, 2019). Increasingly.
Studies have explicitly taken a transdiagnostic and hierarchical approach to these questions to understand how individual risk factors correspond with this framework (see Conway et al., 2019 for a recent review). One substantial advantage to this approach is the opportunity to resolve literatures with multitudes of proposed connections between stressors and specific domains of psychopathology (e.g., between physical abuse and subsequent aggression, or between loss and depression). These findings have often emerged from literatures with patterns of association described in the developmental literature as multifinality—that is, the observation that a single risk factor can result in a wide variety of later psychopathology (Cicchetti & Rogosch, 1996; Ollendick & Hirshfeld-Becker, 2002). Testing the nature of these associations in the context of a hierarchical model of psychopathology allows us to identify the level of specificity of these associations (i.e., whether there is a unique association between a risk factor and a specific domain of psychopathology). More often than not, studies that have taken this approach have found risks to be non-specific and conferred at a transdiagnostic level. The childhood adversity literature mentioned above contains many such findings, and a variety of other environmental stressors throughout the lifespan have also been implicated as broadband transdiagnostic risk factors in a hierarchical framework (e.g., racial discrimination, minority stress, marital distress, lower socioeconomic status, and traumatic experiences; Caspi et al., 2014; Lehavot & Simoni, 2011; Meyers et al., 2015; Rodriguez-Seijas, Stohl, Hasin, & Eaton, 2015; South, Krueger, & Iacono, 2011; Sunderland et al., 2016).
Other factors with similar patterns of widespread risk across both internalizing and externalizing psychopathology in childhood include social isolation, sleep problems, maladaptive thinking styles and beliefs, and self-regulation (e.g., Fairholme et al., 2013; Harvey, Murray, Chandler, & Soehner, 2011; Moffitt et al., 2011; Rubin & Mills, 1988; Schniering & Rapee, 2004). However, to our knowledge these factors have not yet been empirically tested in a hierarchical framework to tease apart the level of specificity of these effects (e.g., to specific syndromes or spectra). As such, it is not yet clear to what extent these factors might have unique relationships with specific domains of psychopathology, but there is evidence they represent transdiagnostic risk factors at high levels of the hierarchy, and likely at the level of general psychopathology. These will be interesting questions for future research. As this literature on transdiagnostic risks for psychopathology develops, the patterns of association will become clearer, and ultimately a hierarchical model of risks for psychopathology will also emerge and indicate specific targets for treatment at each level of the hierarchical structure of psychopathology.
In describing these psychological and environmental risk factors for general psychopathology, it is useful to distinguish modifiable from limited-modifiable risks to contemplate how to purposefully induce change in individuals’ levels on this factor. For example, risk factors such as harsh parenting, social isolation, sleep problems, maladaptive thinking styles, and self-regulation are modifiable, in that they can be directly targeted through personal intervention and skills training. On the other hand, factors such as abuse, maltreatment, victimisation, socio-economic adversity, and personality characteristics are difficult to modify directly, and hence are limited-modifiable. This does not prevent these risks from being targets of intervention, but intervention is more likely to be successful if the aim is to alter personal reactions to the risk (e.g., helping abuse victims to reduce personal attributions and helplessness) or modifying downstream expressions of the risk (e.g., teaching skills to modify impulsive responsivity to emotion), rather than trying to change the limited-modifiable risk directly. Identifying avenues to modify these risk factors for general psychopathology provides a simplified and more focused direction for prevention, with substantial implications for interventions. We turn now to discuss the opportunities for the prevention of psychopathology beginning in early childhood, after briefly reviewing the status quo.
3. Implications for interventions
As described earlier, mental disorders have traditionally been conceptualized as comprising distinct categories. This medical model of psychopathology focuses on the identification of specific and putatively independent diagnoses that predict the efficacy of focused and unique psychiatric treatments. Psychological conceptualisation of treatment correspondingly shifted from its early roots in individual case formulation to embrace the medical model, leading to a proliferation of treatment programs and packages covering many forms of psychopathology. However, rather than having specific effects on only the intended disorder, treatment effects are consistent with predictions from a hierarchical model of psychopathology (Fig. 1). Empirical evidence shows that putatively targeted treatments have generalized impacts on multiple mental disorders and that more closely related disorders show larger effects, while more distal disorders show smaller effects. For example, mirroring the patterns of covariation among disorders that underlie a hierarchical structural model, treatments aimed specifically at childhood anxiety will typically show moderate impact on closely related disorders such as depression and smaller, inconsistent impact on externalizing problems (e.g., Rapee et al., 2013).
Following these observations, a small but gradually increasing literature has begun to argue for the value of transdiagnostic intervention (Ehrenreich, Goldstein, Wright, & Barlow, 2009; Mansell, Harvey, Watkins, & Shafran, 2009), finding these interventions to have equivalent symptom reduction to standard treatments (e.g., Barlow et al., 2017). In practice, transdiagnostic treatment packages developed to date have often been amalgams of several disorder-specific treatments that consequently have broader treatment effects than a single disorder-specific treatment used in isolation. However, increasingly transdiagnostic treatments are being implemented based on therapeutic elements shared across multiple programs with the aim of targeting transdiagnostic processes that are presumed to maintain a variety of individual disorders (e.g., targeting negative emotionality, maladaptive thinking styles, and executive dysfunction using the common elements from several disorder-specific CBT programs; Caspi & Moffitt, 2018; Kaplan et al., 2018).
Another increasingly accepted concept in the development of psychological treatments has been that mental disorders can be prevented, which has substantial implications for extending transdiagnostic treatments to the early childhood stage. A number of highly promising prevention and early-intervention programs have been developed, especially for externalizing psychopathology (Bayer et al., 2009). However, by and large, these programs still largely target a specific symptom domain or disorder. From a public health perspective, it would be far more useful to have a single (or single set of) intervention (s) that can be applied early in life to prevent the full spectrum of lifetime mental disorders.
Together with the dimensional and hierarchical structure of psychopathology discussed above, the intersection of these emerging fields in the treatment literature highlight exciting opportunities for the transdiagnostic prevention of psychopathology. For example, from the dimensional perspective of psychopathology that underpins the evidence for the general factor described above, interventions aim not to cure the occurrence of a categorical disease, but to reduce individuals’ standing on the dimension, thus lowering the likelihood and severity of manifest psychopathology. This dimensional perspective lends itself to preventative interventions. Further, the hierarchical conceptualization of psychopathology takes the concept of transdiagnostic treatment to a whole new level because intervening on the factors that maintain or increase risk for general psychopathology should have far-reaching impact for the full spectrum of mental disorders (cf. Caspi & Moffitt, 2018). The hierarchical structure also highlights the possibility that a consistent and systematic approach to prevention of psychopathology could be implemented with a single program (or set of programs) that dovetails with this hierarchical structure and provide a beneficial parsimony for treatment providers. Together, these ideas indicate that a transdiagnostic stepped care approach to prevention—intervening on general psychopathology as the first step—is the next frontier for psychopathology interventions.
Pairing this idea with development provides particularly exciting opportunities: The emergence of a general psychopathology factor in early childhood highlights the potential for early preventive interventions that will have flow-on effects across development. The “intervention fan” described by the Committee on Prevention of Mental Disorders (Mrazek & Haggerty, 1994) highlights that there is no need to dichotomise between prevention and treatment. Rather, interventions vary along a spectrum according to the progression of disorder and the focus of the application of intervention. At one end of the spectrum are universal interventions, applied across a population when disorders have not yet emerged; at the other end is long-term care, applied in the case of chronic disorder in a single individual. Early in childhood, it is extremely unlikely that individuals will be suffering end stages of a mental disorder and it is much more likely that disorder will not yet have fully emerged, given that only 10% of mental disorders start by age 5 (Cía et al., 2018; Kessler, Berglund, et al., 2005). Therefore, at this developmental stage, intervention will be much more beneficial if it is aimed at prevention or early intervention. We recognise that despite our best efforts, no early intervention program will be 100% effective, and some psychopathology will develop in later years. Our suggestion therefore is to use early intervention for general psychopathology as a foundational scaffold on which to introduce gradually more focused interventions later in development.
Fig. 2 shows an example of how such a developmentally-paired and transdiagnostic stepped care approach to intervention might look beginning with intervention for general psychopathology in early childhood. Starting in preschool, preventive interventions would focus on risk factors that represent early-detectable risks for general psychopathology. From middle childhood, more complex CBT elements could be added to this initial prevention approach, as developmentally appropriate. At this stage the focus would be on teaching coping skills for negative life events and victimisation, challenging maladaptive thinking styles and beliefs, and fostering social support and connection. Targeted modules could also be added for children with prominent internalizing or externalizing behaviors. Some young people will nonetheless go on to develop manifest psychopathology. For individuals who enter early adolescence with persistent or emergent symptoms in specific domains, additional selective transdiagnostic interventions could be added that target the shared processes that underpin specific spectra (e.g., teaching problem-solving and behavioral activation to reduce distress-based problems; targeting substance-related expectations to reduce the risk of substance misuse). At the end of the school years, individuals requiring ongoing support for chronic or severe manifest symptoms could transition into tailored treatment programs for those symptom domains (Ruggero et al., in review). The Achenbach System of Empirically Based Assessment (Achenbach, 2009) represents one set of inventories that would be particularly well-suited to measuring these symptoms and transdiagnostic constructs from preschool through to adulthood (see also https://psychology.unt.edu/hitop for a list of measures consistent with the HiTOP framework and Ruggero et al., in review for a detailed description of the assessment and treatment of HiTOP dimensions).
Fig. 2.

Example of a developmentally informed and transdiagnostic stepped care approach to intervention, paired with examples of elements drawn from the Hierarchical Taxonomy of Psychopathology (HiTOP) model.
3.1. Targeting general psychopathology in early childhood
Our conceptual model suggests that researchers should move their focus for early intervention during the pre-school years away from a wide variety of individual forms of psychopathology and toward intervention to reduce general psychopathology. We do not yet have the knowledge required to prescribe a specific intervention, or set of interventions, for this purpose. Rather than providing the answers, this paper proposes that developing and testing interventions following the framework in Fig. 2 may be a fruitful new direction for the field, and substantial research will be required to translate this theoretical framework into practice. Nonetheless, we speculate here about some possible approaches that may prove useful.
Early intervention for general psychopathology could be delivered universally or as selective intervention (targeting those high on risk factors). It is likely that the most effective programs will involve a systematic and complementary integration of the two. Universal interventions (delivered to all young children) would likely be best used to increase protective factors that are generally associated with positive mental health. For example, this might include education for all parents to increase authoritative parenting, increase healthy bedtime routines, and maximise positive parent/child interactions. Preschools would similarly focus on protective factors such as teaching pro-social peer relationship skills and positive emotion regulation. Naturally, societal efforts to reduce abuse or poverty, and increase education will also have positive impact on general psychopathology.
Selective interventions should complement the universal ones and focus in greater detail on children who show high levels of known risks for general psychopathology. For example, excessive tantrum behaviour has been conceptualised as an indicator of poor emotion regulation (Giesbrecht, Miller, & Müller, 2010), which is widely associated with a range of mental disorders (Zeman, Shipman, & Suveg, 2002). Hence targeting intervention toward children who show high tantrum frequency and introducing them (and their parents) to strategies to increase tolerance and cope with frustration is likely to be widely beneficial. Similar principles might be aimed toward children who demonstrate poor executive control abilities, such as poor attentional focus or difficulty inhibiting impulses; targeting these specific domains would likely be more effective than interventions aimed at improving executive function broadly (e.g., Melby-Lervåg, Redick, & Hulme, 2016). At a different level, identifying parents who are especially harsh or neglectful and assisting them to develop more positive parenting strategies is likely to have very broad benefits for the prevention of a range of future mental disorders.
While many of these suggestions are not especially novel in and of themselves and such programs and efforts already exist, they tend to be piecemeal programs developed to address a specific issue. We propose that these various strategies should be viewed as part of a greater whole that together re-focus intervention efforts in early childhood to systematically reduce general psychopathology.
3.2. Advantages to this approach
There are three particular benefits that this approach could offer over current disorder-specific approaches. First, reducing the burden and confusion in healthcare and education systems as well as for parents. The majority of existing prevention programs focus on reductions in the manifestation of existing symptoms of psychopathology. For example, we have distinct school-based or community programs to specifically reduce depression, anxiety, aggressive behaviors, eating pathology, substance use problems, and so on (e.g., Hahn et al., 2007; Le, Barendregt, Hay, & Mihalopoulos, 2017; Melendez-Torres, Tancred, Fletcher, Thomas, Campbell, & Bonell, 2018; Merry et al., 2011; Werner-Seidler, Perry, Calear, Newby, & Christensen, 2017). As such, schools, parents, and bureaucrats are faced with a bewildering array of possible programs to select, and there are few (if any) coherent pathways that families can navigate. Our proposed approach outlined in Fig. 2 instead provides a coherent and systematic structure for early intervention across a child's development. This approach would also allow consistent funding from community or government systems, a coherent and planned delivery within education or community bodies, and a clearer focus for families with young children.
Second, from a public health perspective, this approach would have the greatest impact for the most people by focusing on common shared risks across psychopathology. By starting with general psychopathology, we would expect population-level effects towards prevention and decreases in psychopathology, as well as increases in resilience via adaptive coping and emotion regulation strategies. Further, modifying risk for general psychopathology early in life would be expected to trigger broad-ranging positive impact later in development via developmental cascades (Masten & Cicchetti, 2010). Specifically, benefits from targeting early risk for general psychopathology would be expected from both a direct impact across the spectrum of psychopathology as well as an indirect effect via a cascading positive influence on later, mediating, risk factors. For example, early childhood intervention promoting emotion regulation and reducing impulsivity should lead to stronger social skills and positive peer relationships in middle childhood, which increase school engagement and academic performance in high school, and ultimately reduce risk for psychopathology in adulthood.
Third, taking a developmentally informed approach maximises the efficiency of the intervention, particularly by corresponding with the development of psychopathology. For example, as discussed above, predispositions towards general psychopathology emerge in early childhood, specific propensities towards internalizing versus externalizing emerge in childhood, and more differentiated diagnoses tend to emerge in later childhood, adolescence, and early adulthood (e.g., Hankin et al., 2016; Kessler, Berglund, et al., 2005). This general correspondence of the hierarchical structure unfolding over development can guide the focus of a stepped care approach by targeting specific symptom domains at the developmentally appropriate period.
4. Conclusion
In sum, the latest research on the structure and nature of psychopathology, corresponding risk factors, and directions for intervention come together to suggest potential opportunities for widespread prevention of psychopathology beginning early in life. We propose moving away from the medical model of mental disorders for treatment and towards a developmentally informed, transdiagnostic stepped care approach to prevention and early intervention for psychopathology. In particular, we argue that a critical focus for intervention at the early stages of life should be the reduction of general psychopathology and its associated risk factors. Later intervention would benefit from this foundation to allow a systematic and developmentally-informed approach to reduce all forms of mental disorder. Incorporating this type of coherent approach within existing health, education, and community systems should lead to a significant decrease in future burden from psychopathology, which could hold tremendous economic and social benefits (Mihalopoulos, Vos, Pirkis, & Carter, 2011).
Acknowledgments
Funding
This work was supported by a Macquarie University Research Fellowship, the Australian Research Council (FL150100096), the National Institutes of Health (R01AG053217, U19AG051426, and R21AA025689), and the Templeton Foundation.
Footnotes
Declarations of interest
The authors declare no conflict of interest.
References
- Achenbach TM (2009). The Achenbach system of empirically based assessment (ASEBA): Development, findings, theory, and applications. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families. [Google Scholar]
- Achenbach TM, & Edelbrock CS (1978). The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin, 85, 1275–1301. [PubMed] [Google Scholar]
- Achenbach TM, & Edelbrock CS (1984). Psychopathology of childhood. Annual Review of Psychology, 35, 227–256. [DOI] [PubMed] [Google Scholar]
- Albott CS, Forbes MK, & Anker JJ (2018). Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Network Open, 1, e185354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disordersInternational Version(5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, et al. (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74(9), 875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayer JK, Hiscock H, Scalzo K, Mathers M, McDonald M, Morris A, et al. (2009). Systematic review of preventive interventions for children's mental health: What would work in Australian contexts? Australian and New Zealand Journal of Psychiatry, 43, 695–710. [DOI] [PubMed] [Google Scholar]
- Bloemen AJP, Oldehinkel AJ, Laceulle OM, Ormel J, Rommelse NNJ, & Hartman CA (2018). The association between executive functioning and psychopathology: General or specific? Psychological Medicine, 48, 1787–1794. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, & Timpano KR (2017). Toward a functional view of the p factor in psychopathology. Clinical Psychological Science, 5, 880–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A (2000). The child is father of the man: Personality continuities from childhood to adulthood. Journal of Personality and Social Psychology, 78, 158. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175, 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, & Shiner RL (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484. [DOI] [PubMed] [Google Scholar]
- Cía AH, Stagnaro JC, Gaxiola SA, Vommaro H, Loera G, MedinaMora ME, et al. (2018). Lifetime prevalence and age-of-onset of mental disorders in adults from the argentinean study of mental health epidemiology. Social Psychiatry and Psychiatric Epidemiology, 53, 341–350. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (1996). Equifinality and multifinality in developmental psychopathology. Development and Psychopathology, 8(4), 597–600. [Google Scholar]
- Clark LA (2005). Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology, 114, 505–521. [DOI] [PubMed] [Google Scholar]
- Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, ... Eaton NR (2019). A hierarchical taxonomy of psychopathology can transform mental health research. Perspectives on Psychological Science, 14, 419–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway CC, Raposa EB, Hammen C, & Brennan PA (2018). Transdiagnostic pathways from early social stress to psychopathology: A 20-year prospective study. Journal of Child Psychology and Psychiatry, 59, 855–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Pauw SS, & Mervielde I (2010). Temperament, personality and developmental psychopathology: A review based on the conceptual dimensions underlying childhood traits. Child Psychiatry & Human Development, 41, 313–329. [DOI] [PubMed] [Google Scholar]
- DeYoung CG, & Krueger RF (2018). A cybernetic theory of psychopathology. Psychological Inquiry, 29, 117–138. [Google Scholar]
- Ehrenreich JT, Goldstein CR, Wright LR, & Barlow DH (2009). Development of a unified protocol for the treatment of emotional disorders in youth. Child & Family Behavior Therapy, 31, 20–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairholme CP, Nosen EL, Nillni YI, Schumacher JA, Tull MT, & Coffey SF (2013). Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behaviour Research and Therapy, 51, 540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Magson NR, & Rapee RM (2019). Evidence that different types of peer victimization experiences have equivalent and broadband associations with transdiagnostic general psychopathology in adolescence. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Forbes MK, Tackett JL, Markon KE, & Krueger RF (2016). Beyond comorbidity: Toward a dimensional and hierarchical approach to understanding psychopathology across the lifespan. Development and Psychopathology, 28, 971–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giesbrecht GF, Miller MR, & Müller U (2010). The anger–distress model of temper tantrums: Associations with emotional reactivity and emotional competence. Infant and Child Development, 19(5), 478–497. [Google Scholar]
- Greene AL, & Eaton NR (2017). The temporal stability of the bifactor model of comorbidity: An examination of moderated continuity pathways. Comprehensive Psychiatry, 72, 74–82. [DOI] [PubMed] [Google Scholar]
- Greene AL, Eaton NR, Li K, Forbes MK, Krueger RF, Markon KE, Waldman I, Cicero DC, Conway CC, Docherty AR, Fried EI, Ivanova MY, Jonas KJ, Latzman RD, Patrick CJ, Tackett JL, Reininghaus U, Wright AGC, & Kotov R (2019). Are fit indices used to test psychopathology structure biased? A simulation study. (Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Hahn R, Fuqua-Whitley D, Wethington H, Lowy J, Crosby A, Fullilove M, et al. (2007). Effectiveness of universal school-based programs to prevent violent and aggressive behavior: A systematic review. American Journal of Preventive Medicine, 33(2, Supplement), S114–S129. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Davis EP, Snyder H, Young JF, Glynn LM, & Sandman CA (2017). Temperament factors and dimensional, latent bifactor models of child psychopathology: Transdiagnostic and specific associations in two youth samples. Psychiatry Research, 252, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, Gulley LD, Schweizer TH, Bijttebier P, Nelis S, et al. (2016). Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology, 28(4pt1), 987–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandler RA, & Soehner A (2011). Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review, 31, 225–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Bagby M, Gralnick TM, Ro E, Ruggero C, Mullins-Sweatt S, ... Zimmermann J (2019). Integrating psychotherapy with the hierarchical taxonomy of psychopathology (HiTOP). Journal of Psychotherapy Integration (in press). [Google Scholar]
- Jaffee SR, Moffitt TE, Caspi A, Taylor A, & Arseneault L (2002). Influence of adult domestic violence on children's internalizing and externalizing problems: An environmentally informative twin study. Journal of the American Academy of Child & Adolescent Psychiatry, 41, 1095–1103. [DOI] [PubMed] [Google Scholar]
- Jones HJ, Heron J, Hammerton G, Stochl J, Jones PB, Cannon M, et al. (2018). Investigating the genetic architecture of general and specific psychopathology in adolescence. Translational Psychiatry, 8, 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan DM, Palitsky R, Carey AL, Crane TE, Havens CM, Medrano MR, et al. (2018). Maladaptive repetitive thought as a transdiagnostic phenomenon and treatment target: An integrative review. Journal of Clinical Psychology, 74, 1126–1136. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, et al. (2012). Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry, 200, 107–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby M, et al. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ, et al. (2018). Progress in achieving quantitative classification of psychopathology. World Psychiatry, 17, 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger R, & Markon K (2006). Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, & Rathouz PJ (2012). Is there a general factor of prevalent psychopathology during adulthood? Journal of Abnormal Psychology, 121, 971–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, & Rathouz PJ (2011). Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry, 68, 181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le LK-D, Barendregt JJ, Hay P, & Mihalopoulos C (2017). Prevention of eating disorders: A systematic review and meta-analysis. Clinical Psychology Review, 53, 46–58. [DOI] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansell W, Harvey A, Watkins E, & Shafran R (2009). Conceptual foundations of the transdiagnostic approach to CBT. Journal of Cognitive Psychotherapy, 23, 6–19. [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development & Psychopathology, 22, 491–495. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT Jr., Ostendorf F, Angleitner A, Hřebíčková M, Avia MD, et al. (2000). Nature over nurture: Temperament, personality, and life span development. Journal of Personality and Social Psychology, 78, 173. [DOI] [PubMed] [Google Scholar]
- Melby-Lervåg M, Redick TS, & Hulme C (2016). Working memory training does not improve performance on measures of intelligence or other measures of “far transfer” evidence from a meta-analytic review. Perspectives on Psychological Science, 11, 512–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melendez-Torres GJ, Tancred T, Fletcher A, Thomas J, Campbell R, & Bonell C (2018). Does integrated academic and health education prevent substance use? Systematic review and meta-analyses. Child: Care, Health and Development, 44, 516–530. [DOI] [PubMed] [Google Scholar]
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, & McDowell H (2011). Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database of Systematic Reviews(12). [DOI] [PubMed] [Google Scholar]
- Meyers JL, Lowe SR, Eaton NR, Krueger R, Grant BF, & Hasin D (2015). Childhood maltreatment, 9/11 exposure, and latent dimensions of psychopathology: A test of stress sensitization. Journal of Psychiatric Research, 68, 337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihalopoulos C, Vos T, Pirkis J, & Carter R (2011). The economic analysis of prevention in mental health programs. Annual Review of Clinical Psychology, 7, 169–201. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, et al. (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences of the United States of America, 108, 2693–2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrazek PJ, & Haggerty RJ (1994). In Mrazek PJ, & Haggerty RJ (Eds.). Reducing risks for mental disorders. Washington, D.C.: National Academy Press. [PubMed] [Google Scholar]
- Murray AL, Eisner M, & Ribeaud D (2016). The development of the general factor of psychopathology ‘p factor’ through childhood and adolescence. Journal of Abnormal Child Psychology, 44, 1573–1586. [DOI] [PubMed] [Google Scholar]
- Olino TM, Bufferd SJ, Dougherty LR, Dyson MW, Carlson GA, & Klein DN (2018). The development of latent dimensions of psychopathology across early childhood: Stability of dimensions and moderators of change. Journal of Abnormal Child Psychology, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, & Hirshfeld-Becker DR (2002). The developmental psychopathology of social anxiety disorder. Biological Psychiatry, 51, 44–58. [DOI] [PubMed] [Google Scholar]
- Oltmanns JR, Smith GT, Oltmanns TF, & Widiger TA (2018). General factors of psychopathology, personality, and personality disorder: Across domain comparisons. Clinical Psychological Science, 6(4), 581–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Lyneham HJ, Hudson JL, Kangas M, Wuthrich VM, & Schniering CA (2013). The effect of comorbidity on treatment of anxious children and adolescents: Results from a large, combined sample. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 47–56. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Seijas C, Stohl M, Hasin DS, & Eaton NR (2015). Transdiagnostic factors and mediation of the relationship between perceived racial discrimination and mental disorders. JAMA Psychiatry, 72, 706–713. [DOI] [PubMed] [Google Scholar]
- Romer AL, Knodt AR, Houts R, Brigidi BD, Moffitt TE, Caspi A, et al. (2018). Structural alterations within cerebellar circuitry are associated with general liability for common mental disorders. Molecular Psychiatry, 23(4), 1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, & Evans DE (2000). Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology, 78, 122. [DOI] [PubMed] [Google Scholar]
- Rubin KH, & Mills RS (1988). The many faces of social isolation in childhood. Journal of Consulting and Clinical Psychology, 56, 916–924. [DOI] [PubMed] [Google Scholar]
- Ruggero CJ, Kotov R, Hopwood C, First M, Clark LA, Skodol A, et al. Integrating the hierarchical taxonomy of psychopathology into clinical practice (in review) Manuscript submitted for publication 10.31234/osf.io/r2jt6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer JD, Moffitt TE, Arseneault L, Danese A, Fisher HL, Houts R, et al. (2018). Adolescent victimization and early-adult psychopathology: Approaching causal inference using a longitudinal twin study to rule out noncausal explanations. Clinical Psychological Science, 6, 352–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schniering CA, & Rapee RM (2004). The structure of negative self-statements in children and adolescents: A confirmatory factor-analytic approach. Journal of Abnormal Child Psychology, 32, 95–109. [DOI] [PubMed] [Google Scholar]
- Selzam S, Coleman JR, Caspi A, Moffitt TE, & Plomin R (2018). A polygenic p factor for major psychiatric disorders. Translational Psychiatry, 8, 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart D, & Sanson A (2005). A comparison of children's temperament and adjustment across 20 years. Family Matters, 72, 50–57. [Google Scholar]
- Snyder H, Friedman N, & Hankin BL (2019). Transdiagnostic mechanisms of psychopathology in youth: Executive functions, dependent stress, and rumination. Cognitive Therapy and Research (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Hankin BL, Sandman CA, Head K, & Davis EP (2017). Distinct patterns of reduced prefrontal and limbic gray matter volume in childhood general and internalizing psychopathology. Clinical Psychological Science, 5(6), 1001–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017a). Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science, 5, 98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017b). Chronic stress exposure and generation are related to the p-factor and externalizing specific psychopathology in youth. Journal of Clinical Child & Adolescent Psychology, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South SC, Krueger RF, & Iacono WG (2011). Understanding general and specific connections between psychopathology and marital distress: A model based approach. Journal of Abnormal Psychology, 120, 935–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spearman C (1904). General Intelligence," objectively determined and measured. The American Journal of Psychology, 15, 201–292. [Google Scholar]
- Sunderland M, Carragher N, Chapman C, Mills K, Teesson M, Lockwood E, et al. (2016). The shared and specific relationships between exposure to potentially traumatic events and transdiagnostic dimensions of psychopathology. Journal of Anxiety Disorders, 38, 102–109. [DOI] [PubMed] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry, 72, 1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts AL, Poore H, & Waldman I (2019). Riskier tests of the validity of the bifactor model of psychopathology. Preprint on PsyArXiv. 10.31234/osf.io/3f28h. [DOI] [Google Scholar]
- Werner-Seidler A, Perry Y, Calear AL, Newby JM, & Christensen H (2017). School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clinical Psychology Review, 51, 30–47. [DOI] [PubMed] [Google Scholar]
- Wiggins JL, Mitchell C, Hyde LW, & Monk CS (2015). Identifying early pathways of risk and resilience: The co-development of internalizing and externalizing symptoms and the role of harsh parenting. Development and Psychopathology, 27, 1295–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeman J, Shipman K, & Suveg C (2002). Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology, 31(3), 393–398. [DOI] [PubMed] [Google Scholar]


