Abstract
Background
African-Americans lose less weight during a behavioral intervention compared with Whites, which may be from differences in dietary intake or physical activity.
Methods
Subjects (30% African-American, 70% White; n=346; 42.4±9.0 yrs.; BMI=33.0±3.7 kg/m2) in an 18-month weight loss intervention were randomized to a standard behavioral (SBWI) or a stepped-care (STEP) intervention. Weight, dietary intake, self-report and objective physical activity, and fitness were assessed at 0, 6, 12, and 18 months.
Results
Weight loss at 18 months was greater in Whites (−8.74 kg with 95% CI [−10.10, −7.35]) compared with African-Americans (−5.62 kg with 95% CI[ −7.86, −3.37]) (p=0.03) in the SBWI group and the STEP group(White:−7.48 kg with 95% CI[−8.80, −6.17] vs. African-American:−4.41kg with 95% CI[−6.41,−2.42]) (p=0.01). Patterns of change in dietary intake were not different between groups. Objective physical activity changed over time (p<.0001) and was higher in Whites when compared to African-Americans (p=0.01).
Conclusions
Whites lost more weight (3.10 kg) than African-American adults. Although there were no differences in dietary intake, Whites had higher levels of objective PA and fitness. Thus, the discrepancy in weight loss may be due to differences in PA rather than dietary intake. However, the precise role of these factors warrants further investigation.
Keywords: race/ethnicity, obesity, weight loss, physical activity, diet
INTRODUCTION
The epidemic of overweight and obesity continues to be a serious public health concern with considerable consequences.1–4 The current prevalence of overweight (body mass index (BMI) > 25 kg/m2) and obesity (BMI > 30 kg/m2) in American adults is estimated to be 68.5% and 34.9%, respectively.5 Although these estimates represent an overall slowing in the rise of obesity since 2003–2008, data suggests that this is not necessarily the case in all racial/ethnic groups. African-American adults in particular have been shown to have disproportionately higher rates of overweight (76.2% vs. 67.2%) and obesity (47.8% vs. 32.6%) when compared to their white counterparts that do not appear to be decreasing.5 Consequently, African-Americans also have higher rates of obesity-related co-morbidities, such as hypertension, type II diabetes, and some forms of cancer.1,2,6,7
Behavioral weight loss interventions have been shown to effectively treat overweight and obesity, producing a clinically meaningful average weight loss of about 10.7 kg, or 10–11% of initial body weight in approximately 32 weeks.8 However, these interventions may be less effective for weight loss in African-Americans compared to Whites, as African-American adults typically lose 2.1 – 5.1 kg less than White adults.9–13 The Diabetes Prevention Program revealed that about half as many African-Americans achieved the 7% weight loss goal at 6 months when compared to the Whites. 10,11
We have recently reported the promising weight loss benefits of a stepped-care intervention approach (STEP), defined as a low-intensity intervention that only increases in intensity and contact when pre-determined weight loss goals are not met, compared to a standard behavioral intervention (SBWI).14 However, the response to these interventions by race has not been examined and so this investigation provides an opportunity to evaluate differences in response between African-Americans and Whites.
This study also examined components of energy balance, physical activity and energy intake. Resting metabolic rate, cardiorespiratory fitness, and energy expenditure from physical activity may be lower in African-Americans compared to Whites,15–22 which may impact body weight changes. While much of the data to support these ideas have stemmed from self-reported physical activity, conclusions from limited available objective data have varied. Accelerometry data from NHANES have suggested that physical activity levels in African-Americans were equivalent to or higher than their White counterparts,17 while armband data from the Energy Balance Study showed African-American women spent significantly more time in sedentary and light activity, and less time in moderate-to-vigorous activity compared to White women.16 This study also showed that African American women had a lower resting metabolic rate (approximately 100kcal/day) than White women, with low cardiorespiratory fitness explaining 25% this difference.16 It has been theorized that cardiorespiratory fitness may influence metabolic rate through differences in physical activity, sympathetic nervous system activation, in muscle structure and fiber type, or in substrate cycling.15,16 However there is limited research directly comparing and examining objectively measured physical activity and cardiorespiratory fitness over time in African-Americans and Whites during a weight loss intervention.
Alternatively, racial differences in weight loss may be attributed to differences in energy intake or diet composition.18,19,23,24 However, few studies have compared energy intake and diet composition in response to a weight loss intervention between African-Americans and Whites.
Thus, the current investigation aims to examine the potential differences in weight loss, self-reported and objectively measured physical activity, and dietary intake between African-American and White adults in response to SBWI and STEP interventions. In addition, measures of body composition, fitness, resting heart rate, and resting blood pressure will also be compared.
METHODS and PROCEDURES
This was a randomized clinical trial conducted at two clinical sites (University of Pittsburgh and University of North Carolina at Chapel Hill) from May 2008 through September 2011. Subjects were recruited using strategies that included television and newspaper advertisements. Primary eligibility criteria included a body mass index (BMI) between 25.0 to <40.0 kg/m2 and age between 18–55 years. Exclusionary criteria included history of cardiovascular disease, the presence of a medical condition that would affect body weight, contraindicate reducing energy intake or increasing physical activity. Additional exclusionary criteria were taking medication that would affect body weight or heart rate response to exercise, sustaining a weight loss of >4.5 kg within the past 6 months, or regular participation in physical activity (>20 min/d on >3 days/wk) over the prior 6 months. Women pregnant within the past 6 months, currently pregnant, or planning on becoming pregnant within the subsequent 18 months were excluded. Subjects completed a medical history and a physical activity readiness questionnaire,20 provided written clearance from their physician, and provided written informed consent prior to participation. Study procedures were approved by the Institutional Review Boards at the University of Pittsburgh and University of North Carolina at Chapel Hill.
Eligible participants were randomized to one of two intervention groups, a standard behavioral weight loss intervention (SBWI) or a stepped-care intervention (STEP). Randomization was stratified within each clinical site based on gender and ethnicity (white or non-white). Full details describing the study protocol and methods have been described elsewhere 14 and will be reviewed briefly here.
Outcome Assessments
Weight and self-reported physical activity were assessed at baseline, 3, 6, 9, 12, 15, and 18 months. Resting heart rate and blood pressure, waist girth, body composition, fitness, objective physical activity, and dietary intake were measured at baseline, 6, 12, and 18 months. Weight was assessed to the nearest 0.1 kg using a digital scale with the subject clothed in a cloth hospital gown or light-weight clothing with shoes removed. Height was measured at baseline using a calibrated stadiometer to the nearest 0.1 cm. BMI was computed as kg/m2.
Lean body mass (LBM) was assessed using bioelectrical impedance and computed using a prediction equation21 and then used to compute percent body fat. Waist circumference was measured horizontally at the level of the umbilicus, with data represented as the average of two measures that differed by ≤1.0 cm.
Self-reported physical activity was measured using a questionnaire.25,26 Objective physical activity was measured using an armband (SenseWear Pro Armband, BodyMedia, Inc.) device worn for a period of one week during all waking hours. Moderate-to-vigorous physical activity (MVPA) was defined as the sum of minutes from bouts of activity that were >10 minutes in duration performed at >3 metabolic equivalents (METS) per minute.
The Block Food Frequency questionnaire was used to provide an estimate of self-reported energy intake (kcal/d) and percent of macronutrient composition (fat, carbohydrates, protein) of the diet.27,28
Following a 5 minute seated rest period, resting heart rate was measured by palpation. Resting blood pressure was then manually measured in duplicate and was represented as the average of two measures in which systolic pressure (SBP) differed by ≤10 mmHg and diastolic pressure (DBP) differed by ≤6 mmHg.
Fitness was assessed using a submaximal graded exercise treadmill test terminated at ≥85% of age-predicted maximal heart rate (220 minus the age of the subject). Termination heart rate was measured by electrocardiography (ECG) and any subject determined to have abnormalities on the ECG or possessed other contraindications to exercise were referred to their primary care physician for evaluation prior to proceeding with this study. Fitness was defined as the time (minutes) to achieve 85% of age-predicted maximal heart rate.
Interventions
As previously described,14 participants were randomized to one of two intervention groups (SBWI or STEP) that both included group behavioral sessions, and identical diet and physical activity recommendations. Both groups decreased energy intake to 1200–1800 kcal/d (20%−30% fat) depending on starting body weight. Physical activity was prescribed to be of moderate-to-vigorous intensity (11–15 on the 15-point rating of perceived exertion (RPE) scale20) starting at 100 min/wk and progressing to 300 min/wk by week 24. All subjects were instructed to self-monitor food intake and physical activity in a weekly diary, and interventionists reviewed these upon completion with feedback provided to the subject in an attempt to maximize adherence to the recommendations of the study.
Participants randomized to the SBWI group attended weekly group sessions for the first 6 months, biweekly sessions in months 7–12, and monthly sessions in months 13–18. The participants in the STEP group attended monthly group sessions throughout the 18 months, combined with additional contact and strategies only if pre-determined weight loss goals were not achieved at 3 month intervals. The weight loss goals were 5% at 3 months, 7% at 6 months, 10% at 9 months, and remained at 10% at 12, 15, and 18 months for all subjects. Intervention details have been published previously.14
Statistical Analysis
Statistical analyses were performed using SAS (version 9.2), with the type I error rate fixed at 0.05 (two-tailed). Analysis dataset included 346 randomized participants who were either non-Hispanic White or African American based on self-reported race/ethnicity. Normality of outcome variables was checked using the Kolmogorov-Smirnov test. Differences between White and African American participants in baseline characteristics were examined using the Chi-square test for categorical variables and the Student’s T-test or Wilcoxon rank sum test for continuous variables.
Weight, weight change, BMI, waist circumference, % body fat, resting heart rate, resting SBP and DBP, fitness, self-reported physical activity, physical activity measured using the armband, dietary intake, % fat intake, % carbohydrate intake, and % protein intake were analyzed using separate mixed effects models using the first-order autoregressive dependence structure or AR(1). Each mixed effects model included covariate adjustment for clinical site and gender because both were randomization stratification factors. Inferences were focused on the effects of race, time, and race by time interaction. The three-way interaction between race, time, and treatment and all two-way interactions of those three variables were also included in the models. For the primary outcome, weight change from baseline was calculated and modeled using a mixed effects model with 6 time points adjusting for baseline weight in the model as a covariate.
Missing data were handled through multiple imputation implemented using SAS procedures PROC MI and PROC MIANALYZE. For each outcome, ten datasets were imputed and results were then combined. Least square means along with the 95% confidence intervals are presented in the tables.
RESULTS
Participants in the current investigation were sedentary, overweight and obese adults, with a mean age of 42.4±9.0 years and a mean BMI of 33.0±3.7 kg/m2. Baseline demographic characteristics of the participants, separated by racial groups, were similar and shown in Table 1. There were no significant baseline differences between racial groups for gender, weight, body mass index, or education level. There was a significant difference (p<0.01) in age between races, with African-Americans being slightly younger (40.4±8.7 vs. 43.2±9.0 years) in the intent-to-treat sample (Table 1). Baseline characteristics separated by treatment group have previously been published.14
Table 1.
Summary of Demographic Characteristics of Subjects for All Randomized Participants (N=346).
| Total | Whites | African-Americans | P-value# for Race | |
|---|---|---|---|---|
| Number of Subjects | ||||
| Intention-to-Treat Analysis | N=346 | N=243 | N=103 | |
| Completers | N=250 | N=181 | N=69 | |
| Lost to Follow-Up | N=96 | N=62 | N=34 | |
| Gender(Females) | ||||
| Intention-to-Treat Analysis | N=285 | N=194 | N=91 | 0.0574 |
| Completers | N=197 | N=138 | N=59 | 0.1092 |
| Lost to Follow-Up | N=88 | N=56 | N=32 | 0.5199 |
| Age(years) | ||||
| Intention-to-Treat Analysis | 42.38+/−8.98 | 43.21+/−9.00 | 40.40+/−8.66 | 0.0075 |
| Completers | 43.01+/−8.90 | 43.68+/−9.04 | 41.25+/−8.32 | 0.0532 |
| Lost to Follow-Up | 40.73+/−9.02 | 41.85+/−8.80 | 38.68+/−9.18 | 0.0989 |
| Body Mass Index(kg/m2) | ||||
| Intention-to-Treat Analysis | 32.96+/−3.65 | 32.83+/−3.68 | 33.25+/−3.58 | 0.3277 |
| Completers | 32.72+/−3.56 | 32.51+/−3.61 | 33.26+/−3.41 | 0.1338 |
| Lost to Follow-Up | 33.59+/−3.82 | 33.78+/−3.76 | 33.23+/−3.97 | 0.5044 |
| Education Level+ | ||||
| Grade School(6 years or less) | - | - | - | 0.8198 |
| High School(10–12 years) | N=24(N=15) | N=19(N=12) | N=5(N=3) | |
| Vocational Training(beyond High School) | N=17(N=11) | N=13(N=10) | N=4(N=1) | |
| Some College(less than 4 years) | N=97(N=70) | N=64(N=47) | N=33(N=23) | |
| College/University Degree | N=119(N=89) | N=83(N=64) | N=36(N=25) | |
| Graduate or Professional Education | N=87(N=64) | N=64(N=48) | N=23(N=16) |
Indicates that numbers not in parenthesis are based on the intent-to-treat analysis and numbers in parenthesis are based on subjects completing 18 months.
Categorical variables are tested with chi-square, continuous variables are tested with Students T-test
Retention and Adherence
A total of 363 participants were randomized to one of two groups, 165 to SBWI and 198 to STEP. Results are presented based on analyses of the 346 participants randomized that were self-classified as either White (n=243) or African-American (n=103). Two sensitivity analyses, which only included a select subgroup of participants, were performed to investigate the robustness of the results found in the full sample of all randomized participants. The first sensitivity analysis used only the subset of randomized subjects who provided assessment data at 18 months (n=250). The second sensitivity analysis was performed excluding participants deemed ineligible by investigators due to pregnancy, relocation, or a non-study-related medical condition. The pattern of findings from both of these analyses was similar to what is reported for the analyses based on the 346 randomized subjects, thus, we only report the results of those analyses.
Process measures of attendance at intervention sessions and return of intervention diaries were also analyzed to compare Whites and African-Americans across the 18 month study period. Because of differences in intervention, data for the Standard intervention and Stepped-Care intervention were analyzed separately. Data were not normally distributed and therefore were analyzed using Wilcoxon Ranked Sum test, with results presented as median and interquartile range (IQR). Whites completed significantly more intervention contacts than African-Americans in both the Standard Intervention (51.4% [IQR: 41.7%, 60.0%] vs. 37.7% [IQR: 14.8%, 53.4%]; p=0.0004) and Stepped-Care Intervention (36.2 [IQR: 23.3, 51.6] vs. 26.8 [IQR: 18.2, 33.4]; p=0.0026). Whites also returned more intervention diaries than African-Americans in both the Standard Intervention (32.0 [IQR: 16.0, 58.0] vs. 14.0 [IQR: 6.0, 35.0]; p=0.0003) and Stepped-Care intervention (27.0 [IQR: 10.0, 48.0] vs. 18.5 [6.0, 35.0]; p=0.0096).
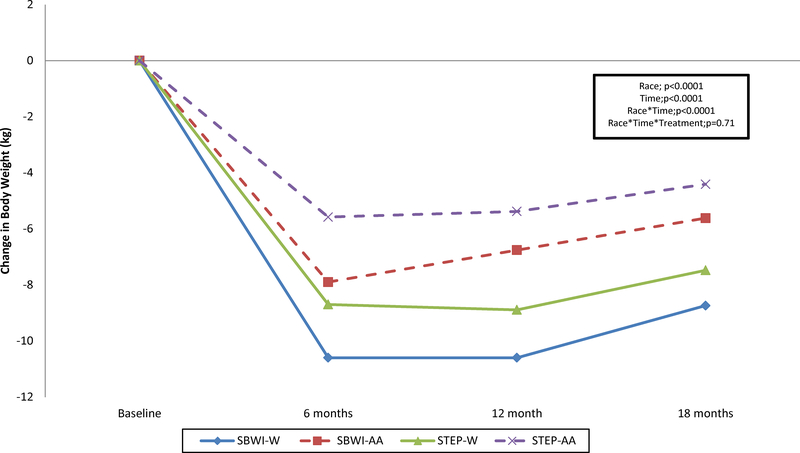
Weight and Body Composition
Both Whites and African-Americans had significant weight loss across the 18-month intervention, with a significant race*time interaction observed (p=0.0001) (Figure 1). Weight loss at 18 months was significantly greater in Whites when compared with African Americans in SBWI (−8.74 kg; 95% CI[−10.10, −7.35] vs. −5.62 kg; 95% CI[−7.86,−3.37]) (p=0.03) and in STEP (−7.48 kg; 95% CI[−8.80,−6.17] vs. −4.41 kg; 95% CI[−6.41,−2.42]) (p=0.01). The non-significant race*treatment*time interaction effect (p=0.71) indicates that the pattern of weight loss between Whites and African-Americans over time was not influenced by the intervention condition (SBWI vs. STEP). See Figure 1. Similar results were revealed when examining percent weight change, BMI, percent body fat, and waist circumference. Data are provided in Supplementary Table 1 online.
Figure I.
Change in body weight (kg) over time for White (W) and African-American (AA) adults who were randomly assigned to one of two intervention conditions: a standard behavioral weight loss intervention (SBWI) or a stepped-care intervention (STEP).
Physical Activity
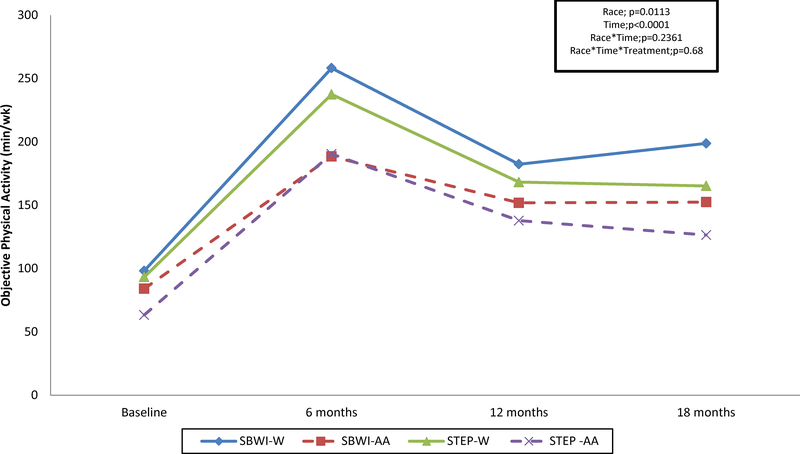
There were significant differences in the pattern of self-reported physical activity by race over time (Race*time interaction, p=0.03), and self-reported physical activity did increase relative to baseline in both races (p<0.0001). See Table 2. In contrast, the pattern of change in objectively measured physical activity did not differ between Whites and African-Americans (Race*time interaction, p=0.24) (Figure 2). MVPA increased relative to baseline levels (p<0.0001) and there was a significant main effect for race (p=0.01), with higher amounts of MVPA observed in Whites compared to African-Americans. There was no significant influence of intervention (SBWI vs. STEP) on the pattern of these findings. See Table 2 and Figure 2.
Table 2.
Change in Self-Reported Physical Activity and Dietary Intake (mean(95%CI)) by Race and Intervention Condition (N=346)
| Variable Treatment Group Race | Assessment Period | P-values | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | 6 Months | 9 Months | 12 Months | 15 Months | 18 Months | Race | Time | Trt | Race*Time | Race*Trt | Trt*Time | Race*Trt*Time | |
| Self-reported Physical Activity (kcal/wk) | 0.4344 | <.0001 | 0.6489 | 0.0322 | 0.5208 | 0.7204 | 0.4540 | |||||||
| SBWI | ||||||||||||||
| White | 690.7 (450.6, 930.9) | 2023 (1752, 2294) | 1573 (1323, 1824) | 1505 (1257, 1754) | ||||||||||
| African-American | 770.0 (401.1, 1139) | 1988 (1567, 2409) | 1607 (1123, 2090) | 1298 (868.1, 1728) | ||||||||||
| Difference | 79.25 (−362, 520.7) (p= 0.7249) | −35.4 (−539, 468.1) (p= 0.8905) | 33.44 (−490, 556.4) (p= 0.9005) | −207 (−710, 295.8) (p= 0.4205) | ||||||||||
| STEP | ||||||||||||||
| White | 649.8 (432.1, 867.6) | 2064 (1839, 2290) | 1536 (1284, 1787) | 1665 (1429, 1901) | ||||||||||
| African-American | 713.6 (376.6, 1051) | 1781 (1419, 2143) | 1783 (1383, 2184) | 1282 (896.3, 1667) | ||||||||||
| Difference | 63.82 (−339, 466.4) (p= 0.7560) | −284 (−709, 141.6) (p= 0.1915) | 247.7 (−242, 737.5) (p= 0.3244) | −383 (−837, 70.61) (p= 0.0995) | ||||||||||
| Dietary Intake(kcal/d) | 0.6002 | <.0001 | 0.1830 | 0.3954 | 0.7009 | 0.0178 | 0.3376 | |||||||
| SBWI | ||||||||||||||
| White | 2156 (2022, 2291) | 1504 (1367, 1641) | 1491 (1351, 1630) | 1559 (1418, 1701) | ||||||||||
| African-American | 2157 (1945, 2369) | 1469 (1253, 1685) | 1644 (1405, 1882) | 1588 (1346, 1830) | ||||||||||
| Difference | 0.72 (−252, 253.0) (p= 0.9955) | −35.5 (−294, 222.5) (p= 0.7873) | 152.9 (−130, 436.2) (p= 0.2916) | 28.67 (−264, 321.8) (p= 0.8483) | ||||||||||
| STEP | ||||||||||||||
| White | 1957 (1835, 2080) | 1472 (1345, 1599) | 1485 (1359, 1611) | 1440 (1306, 1574) | ||||||||||
| African-American | 1948 (1758, 2138) | 1505 (1303, 1708) | 1533 (1309, 1756) | 1504 (1301, 1707) | ||||||||||
| Difference | −8.81 (−236, 218.2) (p= 0.9394) | 33.71 (−200, 267.3) (p= 0.7773) | 47.17 (−204, 298.2) (p= 0.7130) | 64.34 (−178, 306.7) (p= 0.6031) | ||||||||||
Figure II.
Objective Physical Activity (min/wk) over time for White (W) and African-American (AA) adults who were randomly assigned to one of two intervention conditions: a standard behavioral weight loss intervention (SBWI) or a stepped-care intervention (STEP).
Dietary Intake
There were no significant differences in the patterns of dietary intake, reported as overall energy intake in kcal/day, measured over time between the races (Race*time interaction, p=0.3954). Dietary intake decreased significantly over time by approximately 400–600 kcal/d (p<.0001 for time main effect). See Table 2. There was no significant difference between African-Americans and Whites for the pattern of change in percent fat intake (Race*time interaction, p=0.12), percent carbohydrate intake (Race*time interaction, p=0.60), or percent protein intake (Race*time interaction, p=0.65). There was no significant influence of intervention (SBWI vs. STEP) on the pattern of these findings. See Supplementary Table 2 online.
Fitness, Resting Heart Rate, Resting Blood Pressure
Fitness increased significantly relative to baseline in response to the interventions (p<0.0001). The significant Race*Time interaction (p=0.02) indicates that change in fitness was greater in Whites (SBWI=13.4 min, 95% CI[12.7,14.1]; STEP=13.2 min, 95% CI[12.5, 13.9]) compared with African Americans (SBWI=11.6 min, 95% CI[10.4,12.9]; STEP= 11.9 min, 95% CI[10.9,13.0]). See Supplementary Table 3 online.
There was a significant reduction in resting heart rate, systolic blood pressure, and diastolic blood pressure over the intervention period compared to baseline (p<0.0001). However, the pattern of change in these outcomes did not differ by racial group (African-Americans vs. Whites) or by intervention condition (SBWI vs. STEP). See Supplementary Table 3 online.
DISCUSSION
Behavioral weight loss interventions typically produce a mean weight loss of about 10.7 kg between 6 to 12 months.8 Unfortunately not all subjects achieve this magnitude of weight loss, and African-Americans regularly achieve weight losses 2.1–5.1 kg less than their white counterparts.9–13 Results from this study reveal a remarkably consistent finding, with African-Americans losing approximately 3.1 kg less than Whites at 18 months (5.0 kg vs. 8.1 kg; 5.5% vs. 8.6%) (See Figure 1 and supplementary Table 1 online). However, it should be noted that although African Americans lost less weight, the intervention resulted in significant and clinically meaningful weight loss for both racial groups that is comparable to previous studies. In a secondary analysis of racial and gender differences in the Diabetes Prevention Program (DPP), weight losses at 18 months in the lifestyle arm were approximately 5.7 kg (5.5%) in the African-Americans and 7.0 kg (7.3%) in the Whites,11 which is nearly identical to the weight losses at 18 months observed in the present study.
Attempts have been made to improve weight loss in African-Americans by developing culturally relevant intervention materials12,29, tailoring interventions to individual needs,11,30 and conducting interventions within religious/social communities.31–33 The ORBIT Study was a randomized controlled weight loss and weight maintenance trial designed specifically for African-American women,34 and resulted in an unadjusted mean weight loss of 2.3 kg at 18 months.12 A recent review of studies that were culturally tailored for African-Americans reported the average mean difference in weight loss was −2.66 kg between intervention and control groups.35,36 In contrast, the interventions examined in the current study were not culturally tailored, and while less effective for weight loss in African-Americans compared to Whites, resulted in weight loss of approximately 5.0 kg (5.5% of initial weight) at 18 months, which has been shown to result in clinically meaningful improvements in many health-related outcomes.
One consideration is that the less weight loss observed in African-Americans may not negatively impact the health benefits of weight loss in this population. For example, despite achieving less weight loss in this study, the reduction in blood pressure and resting heart rate was similar between African-Americans and Whites. Moreover, it should be noted that a number of studies have shown inconsistent associations between BMI and total mortality in African-Americans, in that they may reap similar health benefits as their White counterparts while at a higher BMI, especially in the women.37–39 Other studies, however, have shown positive associations between BMI and mortality similar to that of whites.40,41 Research should continue to examine this relationship in order to determine the magnitude of weight loss necessary to optimize health benefits in African-Americans and if weight recommendations should be different between races.
Exploration of racial differences should take into account variations in the intervention approach as well as adherence to the intervention. We have reported that a STEP intervention approach can result in clinically meaningful weight loss at a lower cost when compared to SBWI.14 However, whether the effectiveness of STEP versus SBWI varies by racial group (African-Americans vs. Whites), has not been examined. The results from this study showed that while African-Americans lost less weight than Whites overall, differences within racial groups were not seen when comparing the effectiveness of SBWI to STEP (See Figure 1 and supplementary Table 1 online). These results suggest that a STEP intervention can be an effective alternative for African-Americans as well as White participants. In addition, adherence to either intervention, as evidenced by more intervention contacts and returned diaries, was found to be greater in Whites when compared African-Americans. Systematic reviews have shown consistent significant associations between increased dietary self-monitoring and weight loss across all racial groups,42 while a study by Hollis et al. revealed that the number of food records completed had a stronger association with weight loss in African Americans when compared to Whites, regardless of sex.43 Additional research has also highlighted the importance of intervention attendance and weight loss,43–45 indicating these are important components of success. Although other key measures of adherence such as frequency of self-weighing and use of e-monitoring tools were not measured, it should be noted that greater adherence by Whites to two important aspects of the intervention may have contributed to the racial differences in weight loss seen in this study, especially as it relates to participation in prescribed eating and exercise behaviors.
The discrepancy in weight loss between African-Americans and Whites may be a result of differences in the effectiveness of interventions to improve key components of energy balance, primarily physical activity and energy intake. With regard to objectively measured physical activity, there were no differences in the pattern of change over time between the races, but there was a main effect of race, with Whites having higher levels of MVPA compared to the African-Americans across the intervention period (See Figure 2). Other studies have also shown that in response to a weight loss intervention Whites have a higher level of physical activity energy expenditure when compared to African-Americans.46,47 This suggests that researchers need to develop intervention strategies that are equally effective at increasing and maintaining physical activity behaviors in both races, as it is known that physical activity is a key behavior for improving long-term weight loss.48
A unique aspect of this study is that it also included measures of self-reported physical activity. Data revealed that although the patterns of change in self-reported physical activity were different over time between the races, there were no differences between the groups at 18 months (See Table 2). This is in contrast to the objectively measured physical activity, which showed more minutes of MVPA for Whites compared to African-Americans. This discrepancy in findings between self-report and objectively measured physical activity may be partially explained by the results reported by Walsh et al.,47 which showed that in response to a weight loss intervention, African-Americans are less accurate at estimating their energy expenditure from physical activity when compared to Whites. This may suggest the need to include objective measures of physical activity and incorporate strategies that allow African-Americans to more accurately estimate the amount of physical activity completed, when examining racial differences in overweight and obese adults. The change in cardiorespiratory fitness was greater in Whites when compared to African-Americans (See supplementary Table 3 online), which also substantiates the objectively measured physical activity findings. These results confirm the findings of other studies that have reported both physical activity and cardiorespiratory fitness are greater in Whites compared to African-Americans in response to a weight loss intervention.46,47 One such study that used doubly labeled water to objectively measure physical activity found higher physical activity energy expenditure (~122kcal/day) in Whites when compared with African-Americans.23 Another study revealed a significant race effect on cardiorespiratory fitness (expressed as maximal oxygen consumption (VO2max)) indicating lower fitness in African-Americans compared to Whites even after adjusting for changes in weight or fat-free mass.49
This study also examined if differences in energy intake between African-Americans and Whites would partially explain the differences in weight loss. The results, however, showed no significant differences in energy intake per day between the two racial groups (see Table 2). Moreover, there were no differences by racial group for macronutrient composition expressed as percentage of total calories from dietary fat, carbohydrate, or protein. Similar results were seen in a previous weight loss intervention study that reported no differences between blacks and whites for calories consumed or percentage of calories from fat.50 An obvious consideration is that self-reported dietary data are often inaccurate and underreported, especially in the obese. 51 However given the data available in this study and others, differences in dietary intake do not appear to be entirely responsible for the racial differences in weight loss observed between African-Americans and Whites.
Several strengths and limitations of this study need to be considered. This study was part of a larger randomized clinical trial that examined weight loss in response to two types of interventions (SBWI vs. STEP) over a period of 18 months. While approximately 30% of the sample who were recruited self-identified as African-American, this study was not designed or powered to specifically examine differences in the effectiveness of these interventions by race. Thus, future studies need to be designed to specifically examine differences in effectiveness of weight loss interventions by racial group to understand how to make these interventions better for all races/ethnicities, including how to improve adherence. Additional strengths of this study were the inclusion of objectively measured physical activity and cardiorespiratory fitness. As noted in the results, self-reported physical activity was inaccurate when compared to the objective measures. Therefore studies that have only used self-reported physical activity may not be getting a clear picture of the differences in activity between races. In addition, energy intake and diet composition were assessed using a food frequency questionnaire, which may be prone to inaccuracy and underreporting. Thus, future studies should consider using more objective measures of energy intake, such as doubly-labeled water, to elucidate racial differences in components of energy balance that may contribute to these weight loss disparities.
In summary, the present study confirms previous findings that African-Americans lose less weight compared to Whites in response to a behavioral weight loss intervention, regardless of whether a SBWI or STEP intervention was implemented. Similar to other studies, no differences were found in dietary intake between races. However, Whites had higher levels of objectively measured physical activity, which may have contributed to the observed higher levels of cardiorespiratory fitness when compared to African-Americans. Based on these findings, the source of the discrepancy in weight loss between African-Americans and Whites may be due to differences in physical activity levels rather than differences in energy intake or diet composition. However, the precise role of these factors in weight loss differences among African-American and White adults warrants further investigation with larger samples and alternative intervention methods.
Supplementary Material
Acknowledgements
We would also like to acknowledge all of the faculty, staff, and graduate students who contributed to this project through assistance with recruitment, assessments, intervention delivery, and data management at the University of Pittsburgh Physical Activity and Weight Management Research Center, the University of North Carolina at Chapel Hill, and Wake Forest University. This study was supported by grant HL084400 from the National Institutes of Health and the National Heart, Lung, and Blood Institute.
Footnotes
This study is registered at Clinical Trials Registration, clinicaltrials.gov (NCT00714168).
LIST OF REFERENCES
- 1.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. May 2007;132(6):2087–2102. [DOI] [PubMed] [Google Scholar]
- 2.Pi-Sunyer FX. The obesity epidemic: pathophysiology and consequences of obesity. Obes Res December 2002;10 Suppl 2:97S–104S. [DOI] [PubMed] [Google Scholar]
- 3.Pi-Sunyer FX. The medical risks of obesity. Obes Surg. April 2002;12 Suppl 1:6S–11S. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer X The medical risks of obesity. Postgraduate medicine. November 2009;121(6):21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA : the journal of the American Medical Association. February 26 2014;311(8):806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pi-Sunyer FX. A review of long-term studies evaluating the efficacy of weight loss in ameliorating disorders associated with obesity. Clin Ther. Nov-Dec 1996;18(6):1006–1035; discussion 1005. [DOI] [PubMed] [Google Scholar]
- 7.Zhang H, Rodriguez-Monguio R. Racial disparities in the risk of developing obesity-related diseases: a cross-sectional study. Ethn Dis. Summer 2012;22(3):308–316. [PubMed] [Google Scholar]
- 8.Wadden TA, Butryn ML, Wilson C. Lifestyle modification for the management of obesity. Gastroenterology. May 2007;132(6):2226–2238. [DOI] [PubMed] [Google Scholar]
- 9.Kumanyika SK, Wadden TA, Shults J, et al. Trial of family and friend support for weight loss in African American adults. Arch Intern Med. October 26 2009;169(19):1795–1804. [DOI] [PubMed] [Google Scholar]
- 10.Wing RR, Hamman RF, Bray GA, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. September 2004;12(9):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program. Obesity (Silver Spring). June 2008;16(6):1413–1420. [DOI] [PubMed] [Google Scholar]
- 12.Fitzgibbon ML, Stolley MR, Schiffer L, Sharp LK, Singh V, Dyer A. Obesity reduction black intervention trial (ORBIT): 18-month results. Obesity (Silver Spring). December 2010;18(12):2317–2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev. March 2012;13(3):193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakicic JM, Tate DF, Lang W, et al. Effect of a stepped-care intervention approach on weight loss in adults: a randomized clinical trial. JAMA. June 27 2012;307(24):2617–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swift DL, Johannsen NM, Lavie CJ, et al. Racial differences in the response of cardiorespiratory fitness to aerobic exercise training in Caucasian and African American postmenopausal women. J Appl Physiol (1985). May 15 2013;114(10):1375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shook RP, Hand GA, Wang X, et al. Low fitness partially explains resting metabolic rate differences between African American and white women. Am J Med. May 2014;127(5):436–442. [DOI] [PubMed] [Google Scholar]
- 17.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. January 2008;40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 18.Kant AK, Graubard BI, Kumanyika SK. Trends in black-white differentials in dietary intakes of U.S. adults, 1971–2002. Am J Prev Med. April 2007;32(4):264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCrory MA, Suen VM, Roberts SB. Biobehavioral influences on energy intake and adult weight gain. J Nutr December 2002;132(12):3830S–3834S. [DOI] [PubMed] [Google Scholar]
- 20.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 8th Edition. Philadelphia: Wolters Kluwer / Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 21.Segal KR, Gutin B, Presta E, Wang J, Van Itallie TB. Estimation of human body composition by electrical impedance methods: a comparative study. J Appl Physiol. 1985;58(5):1565–1571. [DOI] [PubMed] [Google Scholar]
- 22.Swift DL, Staiano AE, Johannsen NM, et al. Low cardiorespiratory fitness in African Americans: a health disparity risk factor? Sports Med. December 2013;43(12):1301–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carpenter WH, Fonong T, Toth MJ, et al. Total daily energy expenditure in free-living older African-Americans and Caucasians. The American journal of physiology. January 1998;274(1 Pt 1):E96–101. [DOI] [PubMed] [Google Scholar]
- 24.Johnston DW, Lee WS. Explaining the female black-white obesity gap: a decomposition analysis of proximal causes. Demography. November 2011;48(4):1429–1450. [DOI] [PubMed] [Google Scholar]
- 25.Paffenbarger RS Jr., Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Medicine and science in sports and exercise. January 1993;25(1):60–70. [DOI] [PubMed] [Google Scholar]
- 26.Paffenbarger RS Jr., Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. The New England journal of medicine. March 6 1986;314(10):605–613. [DOI] [PubMed] [Google Scholar]
- 27.Block G, Hartman AM, Dresser CM, M.D. C, J. G, L. G A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;108:161–175. [DOI] [PubMed] [Google Scholar]
- 28.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. [DOI] [PubMed] [Google Scholar]
- 29.Kanders BS, Ullmann-Joy P, Foreyt JP, et al. The black American lifestyle intervention (BALI): the design of a weight loss program for working-class African-American women. J Am Diet Assoc. March 1994;94(3):310–312. [DOI] [PubMed] [Google Scholar]
- 30.Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. American journal of health promotion : AJHP. Jul-Aug 2009;23(6):S33–56. [DOI] [PubMed] [Google Scholar]
- 31.McNabb WL, Quinn MT, Rosing L. Weight loss program for inner-city black women with non-insulin-dependent diabetes mellitus: PATHWAYS. J Am Diet Assoc. January 1993;93(1):75–77. [DOI] [PubMed] [Google Scholar]
- 32.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. October 2005;97(10):1393–1402. [PMC free article] [PubMed] [Google Scholar]
- 33.Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: a pilot randomized trial. J Behav Med. October 2008;31(5):367–377. [DOI] [PubMed] [Google Scholar]
- 34.Fitzgibbon ML, Stolley M, Schiffer L, et al. Obesity Reduction Black Intervention Trial (ORBIT): design and baseline characteristics. J Womens Health (Larchmt). September 2008;17(7):1099–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Osei-Assibey G, Boachie C. Dietary interventions for weight loss and cardiovascular risk reduction in people of African ancestry (blacks): a systematic review. Public health nutrition. June 1 2011:1–6. [DOI] [PubMed] [Google Scholar]
- 36.Osei-Assibey G, Kyrou I, Adi Y, Kumar S, Matyka K. Dietary and lifestyle interventions for weight management in adults from minority ethnic/non-White groups: a systematic review. Obes Rev. November 2010;11(11):769–776. [DOI] [PubMed] [Google Scholar]
- 37.Jackson CL, Wang NY, Yeh HC, Szklo M, Dray-Spira R, Brancati FL. Body-mass index and mortality risk in U.S. blacks compared to whites. Obesity (Silver Spring). March 2014;22(3):842–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park Y, Hartge P, Moore SC, Kitahara CM, Hollenbeck AR, Berrington de Gonzalez A. Body mass index and mortality in non-Hispanic black adults in the NIH-AARP Diet and Health Study. PLoS One. 2012;7(11):e50091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW, Jr. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. October 7 1999;341(15):1097–1105. [DOI] [PubMed] [Google Scholar]
- 40.Cohen SS, Park Y, Signorello LB, et al. A Pooled Analysis of Body Mass Index and Mortality among African Americans. PLoS One. 2014;9(11):e111980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boggs DA, Rosenberg L, Cozier YC, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. September 8 2011;365(10):901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. January 2011;111(1):92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hollis JF, Gullion CM, Stevens VJ, et al. Weight Loss During the Intensive Intervention Phase of the Weight-Loss Maintenance Trial. American Journal of Preventive Medicine. 2008;35(2):118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Acharya SD, Elci OU, Sereika SM, et al. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient preference and adherence. 2009;3:151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. December 2004;12 Suppl:151S–162S. [DOI] [PubMed] [Google Scholar]
- 46.Weinsier RL, Hunter GR, Schutz Y, Zuckerman PA, Darnell BE. Physical activity in free-living, overweight white and black women: divergent responses by race to diet-induced weight loss. Am J Clin Nutr. October 2002;76(4):736–742. [DOI] [PubMed] [Google Scholar]
- 47.Walsh MC, Hunter GR, Sirikul B, Gower BA. Comparison of self-reported with objectively assessed energy expenditure in black and white women before and after weight loss. Am J Clin Nutr. June 2004;79(6):1013–1019. [DOI] [PubMed] [Google Scholar]
- 48.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. February 2009;41(2):459–471. [DOI] [PubMed] [Google Scholar]
- 49.Weinsier RL, Hunter GR, Zuckerman PA, et al. Energy expenditure and free-living physical activity in black and white women: comparison before and after weight loss. Am J Clin Nutr. May 2000;71(5):1138–1146. [DOI] [PubMed] [Google Scholar]
- 50.Wing RR, Anglin K. Effectiveness of a behavioral weight control program for blacks and whites with NIDDM. Diabetes Care. May 1996;19(5):409–413. [DOI] [PubMed] [Google Scholar]
- 51.Johansson G, Wikman A, Ahren AM, Hallmans G, Johansson I. Underreporting of energy intake in repeated 24-hour recalls related to gender, age, weight status, day of interview, educational level, reported food intake, smoking habits and area of living. Public health nutrition. August 2001;4(4):919–927. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.