Abstract
Background:
Acute Kidney Injury (AKI) survivors are at risk for chronic kidney disease, recurrent AKI, and cardiovascular disease. The transition from hospital to ambulatory care is an opportunity to reduce these sequelae by launching self-care plans through effective patient education. How well AKI survivors are informationally prepared to apply kidney-specific self-care is unknown. The purpose of this study was to identify awareness and disease-specific knowledge among AKI survivors.
Methods:
We performed a cross-sectional survey of AKI-related awareness and knowledge in 137 patients with KDIGO Stage II or III AKI near the time of hospital discharge. Patients were asked: 1) “Did you experience acute kidney injury (AKI) while in the hospital?” and 2) “Do you have a problem with your kidney health?” Objective knowledge of AKI was evaluated with a 15-item adapted version of the validated Kidney Knowledge Survey (KiKS) that included topics such as common causes, risk factors, and how AKI is diagnosed.
Results:
Median age was 54 (IQR: 43–63) and 81% were white. Eighty percent (80%) of patients were unaware they had experienced AKI and 53% were both unaware they had experienced AKI or had a ‘problem with their kidneys’. Multivariable logistic regression identified being male and lack of nephrology consult as predictors of unawareness with Odds Ratios (OR) of 3.92 (95%CI: 1.48–10.33) and 5.10 (95%CI:1.98–13.13), respectively. Less than 50% recognized non-steroidal anti-inflammatory drugs, contrast, or phosphate-based cathartics as risk factors for AKI. Two-thirds of patients did not agree that they knew a lot about AKI and more than 80% desired more information.
Conclusions:
Most patients with moderate to severe AKI are unaware of their condition, lack understanding of risk factors for recurrent AKI, and desire more information. Patient-centered communication to optimize awareness, understanding, and care will require coordinated educational strategies throughout the continuum of AKI care.
Keywords: Acute Kidney Injury, Knowledge, Awareness
Introduction
Effective communication about health status and self-care is essential for recently hospitalized patients to promote a successful transition to home. Although education is a fundamental part of discharge planning, less than two-thirds of patients hospitalized can accurately describe their primary diagnosis in post-discharge interviews.[1] Greater knowledge about diagnoses is associated with improved health outcomes;[2, 3] however, care provided during this time can be complex and fragmented, threatening the execution of treatment plans. The American Society of Nephrology and Kidney Disease Improving Global Outcomes (KDIGO) AKI Guidelines have highlighted the transition of care for survivors of acute kidney injury (AKI) as an opportunity to reduce poor outcomes.[4, 5]
Patients with AKI represent a growing subpopulation among the hospitalized, with in-hospital and population-based annual incidence rates increasing by 10–11% per year.[6] Survivors of AKI are a particularly vulnerable population at high risk for rehospitalization,[7] recurrent AKI,[8] loss of kidney function,[9] and death.[10] Equipping patients and caregivers to take a more active role in their care at the time of transitions between settings can improve outcomes including reducing rehospitalization.[11, 12] However, studies of discharge practices from inpatient hospitalization and emergency rooms show that patients often lack understanding of key elements of transitional care including their primary reason for admission, discharge medications, or follow-up appointments.[1, 13–15]
Patient ‘activation’ has been identified as essential to an effective transition of care and depends, in part, upon an understanding of one’s health status.[11, 12, 16] Awareness, defined as a ‘bare minimum’ level of knowledge of one’s disease, is considered a basic element needed to begin to apply health-related instructions.[17] In patients with chronic kidney disease (CKD), directed education in an ambulatory setting has been shown to improve self-care, decision-making, and outcomes.[18–20]
To promote future rigorous evaluation of AKI-directed patient education programs, it is important to first identify information deficits by characterizing patients’ AKI-specific knowledge. The purpose of this study was to examine diagnosis awareness and disease-specific knowledge among survivors of AKI to guide the development of future educational interventions that might improve clinical outcomes in this population. We hypothesized that AKI-specific awareness and knowledge would be low. To test this hypothesis, we surveyed hospitalized adult patients who survived an episode of moderate to severe AKI. We employed adapted kidney disease validated knowledge surveys to examine patients’ level of awareness of their own AKI diagnosis, knowledge of AKI risk factors and treatment strategies, and additionally queried perceptions about kidney-related communication from their health providers.
Materials and Methods
Study Setting
This cross-sectional study was performed at Vanderbilt University Hospital, a tertiary referral center, between 2013 and 2014. Data were collected from self-report surveys and abstracted from the electronic medical record (EMR). EMR data included laboratory values (baseline, peak, and discharge serum creatinine; hemoglobin; serum albumin), hospital unit, duration of AKI, nephrology consultation and comorbid diagnoses. The study was performed in accordance with the principles of the Declaration of Helsinki. The institutional review board from Vanderbilt University Medical Center approved the study, and written consent was obtained from all patients. No compensation was provided to participants.
Study Population and Definitions
Adult patients aged 18–80 years were screened for eligibility corresponding to KDIGO Stages 2 and 3 AKI, defined as a minimum doubling of baseline creatinine during hospitalization with or without acute dialysis.[21] Urine output criteria were not applied as our patient population included patients outside of an ICU setting where urine output is not reliably recorded. We restricted our study population to patients with KDIGO Stage 2 and 3 AKI as this population of survivors is at highest risk for long-term loss of kidney function.[22] Patients were required to have a minimum of 1 inpatient serum creatinine. Additionally, to determine that AKI occurred during the hospitalization, patients were ascertained for at least 1 preadmission outpatient serum creatinine between 7–365 days before hospitalization, but if a prehospital baseline was not available, we required the admission serum creatinine to reflect an estimated glomerular filtration rate (eGFR) of >90 ml/min/1.73 m2 as calculated using the CKD-EPI equation.[23] Patients who were receiving chronic dialysis or kidney transplant prior to hospital admission, had a baseline serum creatinine below 0.5 mg/dL (to minimize misclassification of AKI due to erroneous lab values or very low muscle mass), were discharged to hospice care (as details of diagnosis and risk reduction strategies for AKI may not be prioritized as part of routine transitions of care communications), could not communicate fluently in English, or provide informed consent, or were previously diagnosed with a cognitive disability were excluded. Patients discharged to skilled nursing facilities or long-term rehabilitation facilities were included. In addition, all patients were administered the Mini-COG screening test for dementia and were required to have a score of 2 or greater to participate.[24] Potential participants were approached as close to discharge as possible (targeted within 48 hours of anticipated discharge). All surveys were administered by trained study personnel.
Measures
Study participants self-reported demographic information. All surveys were administered by trained study personnel. Health literacy was evaluated with the Brief Health Literacy Screen (range: 0–12) and low health literacy was defined by a score of 6 or less.[25, 26] An 11-item survey of objective kidney knowledge was performed adapted from the Kidney Knowledge Survey (KiKS) scored a percent correct.[27]. Awareness of AKI and general kidney health were evaluated with the following two “Yes/No” questions: 1) “Did you experience acute kidney injury (AKI) while in the hospital?” and 2) “Do you have a problem with your kidney health?” [17] To assess whether the term ‘acute kidney injury’ affected patients’ response to the survey questions because of potential unfamiliarity with the terminology, additional questions were asked replacing AKI with phrases such as “acute renal/kidney failure”, “damage to your kidneys” or “cause kidneys to stop working well,” in a subset of 50 participants.
Objective knowledge of AKI was evaluated with a 15-item adapted version of the validated Kidney Knowledge Survey (KiKS).[27] The question topics included common causes, risk factors, and methods of diagnosis for AKI. Correct responses were given a score of 1 and incorrect responses a score of 0, with the overall score calculated as the percentage of correct responses. The Kuder-Richardson coefficient for the 15-items in this sample is 0.54, which may be seen in knowledge scales where knowing 1 item does not necessarily mean that you also know the answer to the other items. In addition, perceived knowledge of AKI—what a patient believes they know about AKI—was assessed using a 5-item adapted version of the Perceived Kidney Knowledge Survey.[28] These items, such as “I know a lot about Acute Kidney Injury (AKI)”, were scored on a 5-point Likert scale, with responses ranging from “Strongly Agree”‘ to “Strongly Disagree”. Using this same response scale, two questions were asked about informational needs, 1) “I want to learn more about AKI in general”, and 2) “I want to learn more about how AKI might affect my body”. Finally, participants were asked if their doctor or nurse told them all they want to know about AKI. Example questions and response options are shown in Appendix 1.
Statistical Analyses
Patient characteristics were described as medians with interquartile range [IQR] for continuous variables and compared using the Wilcoxon rank sum test. Categorical variables were expressed as proportions and compared using the Pearson χ2 test. Correlations between ordinal and continuous variables were calculated using Spearman’s rank-order correlation. Multivariable logistic regression was used to examine the effects of age, sex, and nephrology consultation on AKI awareness. Statistical analyses were performed using SPSS Version 22 (IBM SPSS Statistics, Version 22.0. Armonk, NY: IBM Corp).
Results
Subject Characteristics
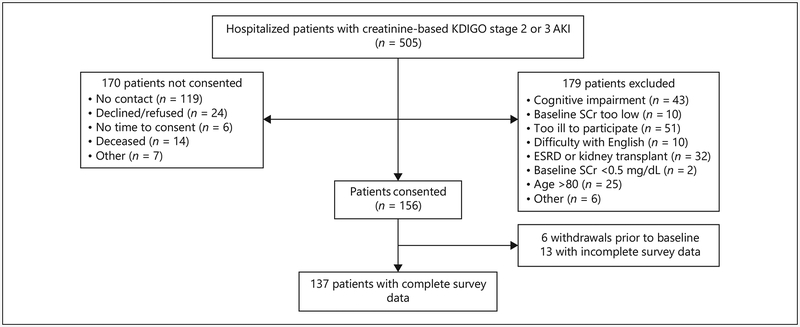
Of 505 hospitalized patients with KDIGO Stage 2 or 3 AKI, 179 patients were ineligible based on exclusion criteria. Due to the limited scope of the study, we were unable to consent an additional 170 additional patients due largely to non-contact (e.g. discharge from hospital before being able to be approached). (Figure 1). Six patients withdrew from the study before data collection. Of the 150 remaining patients, thirteen did not have complete data (i.e. answered the primary AKI awareness question) and were not included.
Figure 1. Patient selection flow diagram. Patient selection flowchart demonstrating the number of patients excluded and derivation of the final study cohort. KDIGO, kidney disease improving global outcomes; AKI, acute kidney injury.
Patient selection flowchart demonstrating the number of patients excluded and derivation of the final study cohort.
Median patient age was 54 (IQR: 43, 63), most were male (53%) and 81% were white (Table 1). Ninety percent (90%) had a high school education or higher, but 30% had low health literacy. There was a high prevalence of underlying comorbid conditions, including diabetes (33%), hypertension (56%), cardiovascular disease (45%), 23% with evidence of pre-existing CKD and 15% (N=20; 55% of those with baseline CKD) had been previously seen in the medical center’s nephrology outpatient practice. Most patients were cared for by medical services and approximately one-half were admitted to the intensive care unit during their hospitalization. There was an even distribution between Stage 2 and 3 AKI with 79% of patients meeting criteria for AKI for at least 2 days duration. Thirty-nine percent (39%) of patients were cared for by a nephrologist and 11 % received dialysis during the hospitalization. The median time from study enrollment to discharge was 1.0 (IQR: 0–4) days and was not statistically different between patients who were aware and unaware (p=0.17).
Table 1.
Demographic and clinical characteristics of study participants.
| Characteristics | Total (N=137) | Aware of AKI N=28 (20%) | Unaware of AKI N=109 (80%) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 54 (43–63) | 48 (35–59) | 55 (44–64) | 0.05 |
| Sex (% Male) | 72 (53%) | 8 (29%) | 64 (59%) | 0.01 |
| Race (% White) | 109 (81%) | 21 (75%) | 88 (82%) | 0.39 |
| Income < $20,000/year (n=122) | 41 (34%) | 9 (36%) | 32 (33%) | 0.78 |
| Education ≥12 years (n=135) | 121 (90%) | 24 (86%) | 97 (90%) | 0.45 |
| Low Health Literacy Score [0–6]; (n=132) | 39 (30%) | 5 (19%) | 34 (32%) | 0.16 |
| General Kidney knowledge score (n=123) | 73% (55–73) | 68% (64–73) | 73% (55–73) | 0.47 |
| Clinical Characteristics | ||||
| Baseline eGFR ml/min/1.73m2 | 82 (61–103) | 68 (55–110) | 85 (63–103) | 0.51 |
| % CKD (baseline eGFR < 60 ml/min/1.73m2) | 32 (23%) | 9 (32%) | 23 (21%) | 0.22 |
| Cardiovascular disease | 62 (45%) | 11 (39%) | 51 (47%) | 0.48 |
| Diabetes | 45 (33%) | 11 (39%) | 34 (31%) | 0.42 |
| Hypertension | 76 (56%) | 14 (50%) | 62 (57%) | 0.51 |
| Primary service | 0.14 | |||
| Medicine | 92 (67%) | 23 (82%) | 69 (63%) | |
| Surgery | 45 (33%) | 5 (18%) | 40 (37%) | |
| Length of stay (days) | 12 (7–18) | 15 (9–26) | 11 (7–18) | 0.03 |
| Intensive Care Unit during hospitalization | 71 (52%) | 14 (50%) | 57 (52%) | 0.83 |
| Peak serum creatinine (mg/dl) | 2.93 (2.14–4.48) | 4.54 (3.13–5.66) | 2.65 (2.06–4.07) | <0.001 |
| Peak Stage of AKI experienced Stage 2 Stage 3 |
68 (50%) 69 (50%) |
5 (18%) 23 (82%) |
63 (58%) 46 (42%) |
<0.001 |
| Required dialysis | 15 (11%) | 8 (29%) | 7 (6%) | 0.01 |
| Baseline serum creatinine (mg/dl) | 0. 90 (0.76–1.26) | 0.97 (0.72–1.41) | 0.90 (0.76–1.24) | 0.80 |
| Enrollment serum creatinine (mg/dl) | 1.67 (1.11–2.75) | 2.72 (1.28–3.68) | 1.61 (1.07–2.37) | 0.03 |
| Change in serum creatinine from baseline to enrollment (mg/dl) | 0.71 (0.13–1.53) | 0.96 (0.36–2.62) | 0.69 (0.10–1.19) | 0.08 |
| Duration of AKI ≥ 2 days | 108 (79%) | 24 (86%) | 84 (77%) | 0.32 |
| Days meeting AKI criteria | 3 (2–9) | 6 (3–13) | 3 (2–7) | 0.04 |
| Nephrology consult | 53 (39%) | 19 (68%) | 34 (31%) | <0.001 |
| Acknowledged discussing kidney problem during hospitalization (n=134) | 77 (58%) | 18 (54%) | 59 (56%) | 0.41 |
| Acknowledge discussing AKI during hospitalization (n=133) | 34 (26%) | 12 (43%) | 22 (21%) | 0.41 |
| Discharge serum creatinine (mg/dl) | 1.50 (0.98–2.43) | 2.21 (1.10–3.95) | 1.49 (0.94–2.07) | 0.05 |
| Proportion recovering to within 20% of baseline serum creatinine | 48 (35%) | 10 (36%) | 38 (35%) | 0.93 |
| Proportion recovering to within 50% of baseline serum creatinine | 69 (50%) | 14 (50%) | 55 (50%) | 0.97 |
Abbreviations: eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease; AKI, acute kidney injury. Continuous variables are reported as median (interquartile range). Nominal and categorical variables are listed as N (%). P<0.05 denotes statistical significance (bold).
Awareness of AKI
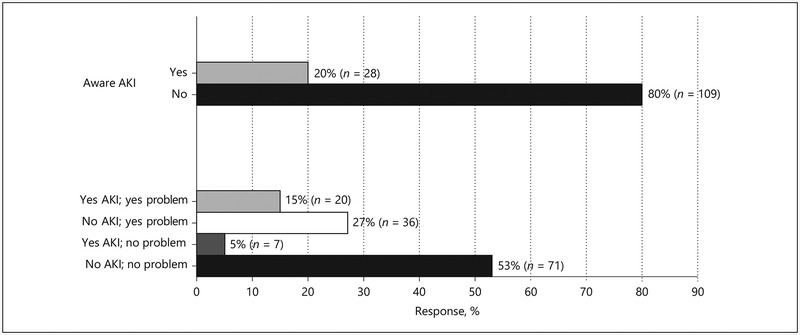
Eighty percent (80%) of patients were unaware that they had experienced AKI while in the hospital, including 7 patients who received dialysis treatments. When also asked if they had a problem with their kidney health, 53% reported both no to this question and no to experiencing AKI (Figure 2). Only 15% acknowledged experiencing both AKI and a problem with their kidney health overall, and this increased to 25% if limited to the patients who had been seen by nephrology prior to hospitalization. Patient with baseline CKD were more likely to report a problem with their kidney health (53%) compared to those without CKD (38%), although this was not statistically significant (p=0.14). Patients who were unaware they had experienced AKI were more likely to be male, have less severe AKI (Stage 2), shorter duration of AKI, shorter overall length of stay, less likely to have had a nephrology consult, and had a lower discharge serum creatinine. No differences in baseline general kidney knowledge were observed between those aware and those unaware of AKI. Multivariable logistic regression identified male sex, and lack of nephrology consult as predictors of lack of AKI awareness with Odds Ratios (OR) of 3.92 (95% CI: 1.48–10.33) and 5.10 (95% CI: 1.98–13.13), respectively. Notably, only 58% of patients reported having a discussion with their clinicians while hospitalized of a kidney problem and only 26% specifically recalled discussing AKI. Overall, 23% of patients acknowledged both having a discussion and specifically discussing AKI, with this increasing among those who also received a nephrology consultation (34% versus 16%; p<0.0001).
Figure 2. Proportion of patients who reported being aware of having experienced AKI. The top panel shows the proportion of patients responding yes/no to the question of “Did you experience AKI while in the hospital?.” The bottom panel stratifies this question further based on the response to the additional question “Do you have a problem with your kidney health?.” AKI, acute kidney injury.
The top panel shows the proportion of patients responding yes/no to the question of “Did you experience AKI while in the hospital?”. The bottom panel stratifies this question further based on the response to the additional question “Do you have a problem with your kidney health?”.
Objective and Perceived AKI Knowledge
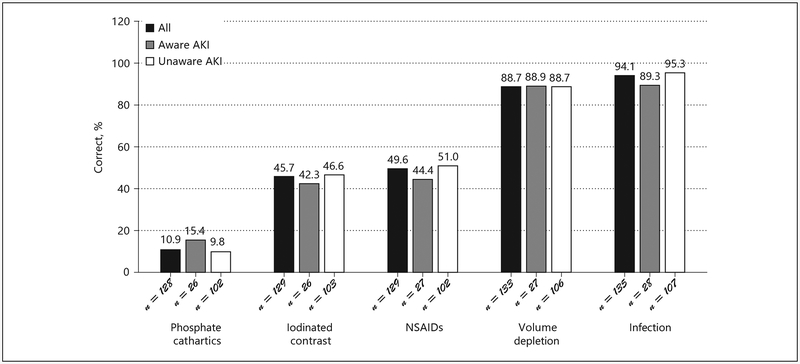
Overall, the median AKI objective knowledge score was 60% (IQR: 50%, 70%). Men had lower AKI knowledge scores compared with women (60% IQR: 47%. 67% versus 67% IQR: 53%, 73%; p=0.004). In total, 72% of patients correctly defined AKI as when ‘your kidneys suddenly stop working well’, 60% identified that AKI was more common if someone has underlying CKD, and 73% knew that AKI was diagnosed by measuring creatinine in the blood. Patients were also surveyed regarding potential AKI precipitants. Most patients recognized ‘infection’ and ‘dehydration’ as risk factors for AKI; however, less than 50% recognized non-steroidal anti-inflammatory drugs (NSAIDS), iodinated contrast, and phosphate cathartics as risk factors (Figure 3).
Figure 3. Identification of specific AKI risk factors. This figure shows the proportion of study participants who recognized specific risk factors for AKI. AKI, acute kidney injury.
This figure shows the proportion of study participants who recognized specific risk factors for AKI.
Most patients did not express confidence in their knowledge of AKI and responded that they ‘disagree’ or ‘strongly disagree’ when questioned whether they know a lot about AKI (65%), how AKI is diagnosed (66%), how to prevent AKI (60%), and how AKI might hurt the body (52%).
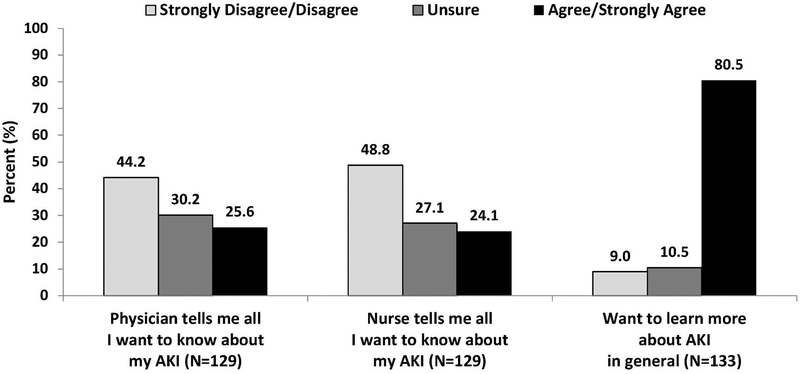
Informational Needs
Approximately one-half of patients disagreed or strongly disagreed that physicians’ or nurses’ communication fulfilled their informational needs regarding AKI, and approximately one-quarter were unsure. Greater than 80% of patients agreed or strongly agreed with a desire to learn more about AKI in general (Figure 4).
Figure 4. AKI Informational Needs.
This figure shows the distribution of responses of study participants to questions regarding whether physicians or nurses met their informational needs and whether they desired to learn more about AKI in general. Responses were grouped by strongly disagree/disagree, not sure, and agree/strongly agree.
Sensitivity Analyses
In a subset of 50 participants, we also administered all knowledge survey items substituting the term ‘acute kidney injury’ with ‘kidneys to suddenly stop working well’ or ‘kidney damage’. Results were similar to the primary analysis with 73% of patients correctly defining acute renal/kidney failure, 81% identifying CKD as a risk factor for the kidneys to stop working well and 79% knowing AKI is diagnosed by measuring serum creatinine. Recognition of NSAIDs (59%), iodinated contrast (47%), and phosphate cathartics (14%) as potential causes of kidney damage or agents that can make the kidneys ‘stop working well’ were similarly low. There was no statistically significant difference in responses to any of the alternate plain language AKI objective knowledge items when compared to the questionnaire using the term ‘AKI’.
Discussion
This initial study suggests that hospitalized patients experiencing moderate to severe AKI are frequently unaware of their condition at discharge and have limited knowledge to inform prevention of future loss of kidney function. Specifically, fewer than half of AKI survivors were aware of the potential hazards of common nephrotoxins including NSAIDs that can negatively impact recovery or the risk for recurrent AKI. Men, patients with less severe AKI, and those who did not see a nephrologist were less likely to be aware of their condition. Most patients desired education to improve their AKI knowledge and preferred additional counseling directly from clinicians.
We suspect several reasons for the low patient awareness of AKI observed. First, general knowledge about kidney disease is poor and below expectations among patients with CKD, including those hospitalized or receiving care from nephrologists.[27, 29, 30] Prior experiences with kidney disease education and care are likely important considerations when diagnosing and educating patients about their AKI. In our study, we observed a trend toward higher awareness and knowledge in the subgroup of patients with evidence of underlying CKD; however, the number of patients with CKD was small and this difference did not reach statistical significance. Nevertheless, overall awareness even among patients with CKD was low (i.e. only 32% aware), suggesting a need to improve awareness and knowledge even among patients with established CKD. Second, despite adoption of standardized definitions for AKI,[31] this condition is often under-recognized and knowledge of risk factors for AKI is highly variable among physicians.[32, 33] These findings suggest that improving awareness and knowledge among healthcare professionals may also be an opportunity to improve education for patients. Thirdly, it is possible that AKI was not deemed clinically significant by hospital clinicians. Treatment nihilism has been previously recognized in CKD,[34] and one recent study also found a large discrepancy between the expectations that nephrologists would have for follow-up of certain AKI survivors and the actual follow-up that occurred.[35] In this context, providers may not believe that the course or sequelae of AKI are significantly modified by patient self-care, resulting in a low priority placed on allocating time and resources to delivering AKI education. Although this might be expected to occur more often in cases of mild AKI, this study included patients with at least a doubling of baseline serum creatinine or who received dialysis for AKI, where clinical guidelines recognize the expectation that at a minimum patients are informed of their diagnosis.[36] Physician engagement strategies to secure provider buy-in on the value of providing patient education will be a necessary component of comprehensive AKI care programs.
Another potential reason for low awareness may be that clinicians are not communicating effectively about kidney health in ways that patients can understand, interpret, and apply.[37] Although widely adopted in communication between providers, the term ‘acute kidney injury’ or ‘AKI’ may not be being used in common parlance with patients to a similar degree. However, it was telling that over half of this cohort with moderate to severe AKI answered both no to being aware of AKI AND having a problem with their kidneys. It is also possible that providers are delivering AKI education during their hospital consultations, but this information may not be effectively interpreted or incorporated. There are a variety of barriers to effective patient-physician communication that include deficiencies of the physician to deliver counseling in a clear communication style,[38] intentional nondisclosure or avoidance of specific discussions, and discouragement by the provider for patients to engage in a collaborative or shared-decision making conversation.[39] We did not evaluate clinician behavior and direct observation of discussions in this initial study, though future studies might include these measures to enhance understanding of the elements most helpful to tailoring provider communication curriculums specific to AKI.
Several patient factors may have also contributed to a limited understanding of AKI, such as education level or socioeconomic status. Most patients in our study completed at least a high school level education and few reported low income, suggesting that that our modest levels of awareness may be optimistic compared to broader or more vulnerable populations.[27, 40] The ability of some patients to accept, understand, and retain information about AKI during the hospitalization context may also be limited. For example, we found that 30% of our study participants had low health literacy, which may have contributed to low awareness and knowledge, even when more ‘lay’ terms were used. In addition, as most AKI usually occurs from illness or procedures, many patients would likely have to process complex health-related information for at least two different conditions and interact with providers from different specialties. One-half of study participants were also critically ill at some point during hospitalization, when delirium is common.[41] Although we enrolled participants later in their hospitalization when deemed by their clinical team to be ready for discharge, subtle deficits may have been present either at the time of discussions with their clinicians or during our assessments due to sleep deprivation, sedatives, recent delirium, and pain.[42] The latter raise questions surrounding the optimal timing of education during hospitalization for AKI survivors. Lastly, we found that men were more likely to be unaware of their AKI diagnosis compared to women. Sex differences in knowledge have been previously demonstrated in other chronic and acute conditions such as hypertension and stroke, which we also observed in our analysis.[43, 44] One potential explanation is that men, in general, have been observed to have lower health literacy than women,[45] with a possible contributor including less frequent interactions with the healthcare system.[46]
Self-care relating to AKI may be challenging. Patients who experience AKI are responsible for understanding and participating in care for both their primary illness and the sequelae of AKI. The latter may include, for example, a higher risk for incident heart failure and recurrent AKI.[7, 47] Particular attention to understanding volume status and medical reconciliation, including appropriate diuretic use may be valuable adjunctive goals of educational interventions in specific AKI subpopulations. Furthermore, as most AKI survivors will not see a nephrologist as part of routine follow-up,[48] patient education activities focusing on common-sense interventions such as improving medication safety, understanding dietary intake parameters, recognizing signs of volume depletion and overload, and avoiding nephrotoxins are reasonable targets that can be applied by primary caregivers. For example, we recently demonstrated that nearly 20% of patients with a hospitalization that involved a discharge diagnosis of acute renal failure regularly take non-steroidal anti-inflammatory agents (NSAIDs) following hospital discharge.[49] One recent study examined whether self-reported knowledge of AKI might be modified in patients referred to a specialized post-AKI clinic.[50] Similar to our study, patients tended to fall on the more severe spectrum of AKI severity; however, in contrast to our study, the authors observed a higher level of baseline AKI awareness, possibly due to the high prevalence of patients already seen by nephrologists during hospitalization (85%). The authors demonstrated that education directed at improving understanding of AKI and its consequences, modifiable risk factors, and patient-specific risk factors improved patients’ self-perceived knowledge about AKI. Whether the latter can lead to objective gains in knowledge that translate to improved outcomes remains to be studied.
While a notable strength of this study includes being among the first to examine kidney-related awareness and knowledge in patients with moderate to severe AKI, several limitations are important to consider. Assessments of awareness of AKI were based on widely accepted question formats used to in kidney health;[17] however, the measures of objective and perceived knowledge of AKI are novel. Although they are derived from other validated measures of CKD knowledge,[27, 28] they will require on-going assessment in larger studies to extend evidence beyond this initial research of their validity in AKI. The study was performed at a single tertiary referral center and extension of these findings to other centers and examining these tools in the post-discharge period may help both examine knowledge retention and improve validation and generalizability. Information on primary hospital diagnosis was not captured and the causes of AKI were not clinically adjudicated, though were likely due predominantly to hemodynamic or nephrotoxic injury in a generalized hospital population. Future studies to also examine how the cause of AKI relates to overall awareness and knowledge would help target educational-based interventions. We also did not have detailed information on prior episodes of AKI and their potential impact on AKI awareness of knowledge. However, even among patients with CKD, awareness was low. Although we enrolled patients close to the time of discharge, it is possible that counseling regarding AKI diagnosis and risk factors was delivered only at the time of discharge. We also do not have information on the timing of dialysis in relation to survey administration. Research assistants were trained in survey administration best practices but were not blinded to the design as this was an observational study collecting different variables among eligible patients. Lastly, we did not systematically assess knowledge and awareness of AKI among caretakers in this study. However, given the challenges of communicating, processing, and retaining this information outlined above, further studies to assess caretaker knowledge and their potential role in educational initiatives should be studied.
In conclusion, we found that most patients with moderate to severe AKI are unaware of having experienced AKI, did not reliably identify common nephrotoxic drug exposures, felt that patient-clinician communication regarding their disease status could be improved, and expressed a desire to learn more about AKI and its implications for their overall health. Studies examining how AKI-related knowledge associates with future outcomes and whether education-specific interventions can improve outcomes are warranted.
Acknowledgements and Funding Sources
KLC is supported by R01DK103935. SKP was supported by National Institutes of Health Training Grant 5T32-DK007569–25 and the Department of Veterans Affairs, Office of Academic Affiliations, Advanced Fellowship Program in Medical Informatics. EDS was supported by the Vanderbilt Center for Kidney Disease (VCKD). KGM was supported by an NIH-NIDDK Summer Student Program Grant P30 DK 079341. EMU was supported by K23 DK114566. Support for was also provided by the Vanderbilt National Center for Advancing Translational Sciences Clinical and Translational Science Awards (CTSA) UL1TR000445.
Statement of Ethics
The institutional review board from Vanderbilt University Medical Center approved the study, and written consent was obtained from all patients.
Funding: National Institutes of Health, Department of Veterans Affairs, and the Vanderbilt Center for Kidney Disease (VCKD).
Appendix
Select Questions from AKI Knowledge Survey
AKI Awareness:
- Did you experience acute kidney injury (AKI) while in the hospital?
- ☐-0 No, I did not have AKI
- ☐-Yes, mild AKI
- ☐-Yes, moderate AKI
- ☐-Yes, severe AKI
- Do you have a problem with your kidney health?
- ☐-1 Yes
- ☐-0 No
AKI Objective Knowledge:
- Acute kidney injury (AKI) is when_ .
- your blood counts drop too low
- your kidneys suddenly stop working well
- your back hurts suddenly
- your stomach hurts
- The most common cause of AKI is.
- taking tylenol
- eating too much salt
- dehydration
- kidney stones
- AKI is more common if you.
- have chronic kidney disease
- are younger
- do not have diabetes
- all of the above
- AKI is diagnosed by checking.
- creatinine levels in your blood
- your blood count
- an x-ray
- your blood pressure
- Severe AKI may be dangerous because it may.
- increase poisonous substances in your body
- cause you to retain fluid
- require dialysis treatments
- all of the above
- Which of the following can cause AKI?
Yes No Not sure a. Dehydration b. Infection c. Dye used in CAT or CT scans d. Fleets Enemas e. Giving blood f. Cell phones g. Motrin/Advil or Ibuprofen h. Eating too much red meat - What may be an early symptom of AKI?
- Not making as much urine
- Skin turning yellow
- Back pain
- Headache
- Select the ONE MEDICATION from the list below that a person with CHRONIC kidney disease should AVOID:
- Lisinopril
- Tylenol
- Motrin/Ibuprofen
- Vitamin E
- Iron Pills
AKI Provider Discussion:
- Has anyone talked to you about acute kidney injury during your stay?
- ☐-Yes
- ☐-No, I didn’t talk about acute kidney injury
AKI Perceived Knowledge:
| Strongly Disagree | Disagree | Not sure | Agree | Strongly Agree | |
|---|---|---|---|---|---|
| 1. I know a lot about acute kidney injury (AKI) | |||||
| 2. I know about who is at risk for getting AKI | |||||
| 3. I know how to diagnose AKI | |||||
| 4. I know how to prevent AKI | |||||
| 5. I know a lot about how AKI might hurt my body |
AKI Informational Needs:
| Strongly Disagree | Disagree | Not sure | Agree | Strongly Agree | |
|---|---|---|---|---|---|
| 6. I want to learn more about AKI in general | |||||
| 7. I want to learn more about how AKI might affect my body | |||||
| 8. My doctor tells me all I want to know about my AKI | |||||
| 9. My nurse tells me all I want to know about my AKI |
Footnotes
Disclosures
The views expressed herein do not necessarily represent those of the Veterans Administration, National Institutes of Health or Vanderbilt University Medical Center.
Conflict of Interest Statement
The authors do not report any relevant conflicts of interest. The results presented in this paper have not been published previously in whole or part, except in abstract format at the American Society of Nephrology 2015 Annual Scientific Meeting.
References
- 1.Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med 2013;173(18):1715–1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA 2004;291(11):1358–1367 [DOI] [PubMed] [Google Scholar]
- 3.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med 2009;150(3):178–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldstein SL, Jaber BL, Faubel S, et al. AKI transition of care: a potential opportunity to detect and prevent CKD. Clin J Am Soc Nephrol 2013;8(3):476–483 [DOI] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012;2:1–138 [Google Scholar]
- 6.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY Temporal Changes in Incidence of dialysis-requiring Acute Kidney Injury. Journal of the American Society of Nephrology 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siew ED, Parr SK, Abdel-Kader K, et al. Predictors of Recurrent AKI. J Am Soc Nephrol 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thakar CV, Christianson A, Himmelfarb J, et al. Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clinical journal of the American Society of Nephrology : CJASN 2011;6(11):2567–2572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney international 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.James MT, Hemmelgarn BR, Wiebe N, et al. Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: a cohort study. Lancet 2010;376(9758):2096–2103 [DOI] [PubMed] [Google Scholar]
- 11.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166(17):1822–1828 [DOI] [PubMed] [Google Scholar]
- 12.Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc 2004;52(11):1817–1825 [DOI] [PubMed] [Google Scholar]
- 13.Crane JA. Patient comprehension of doctor-patient communication on discharge from the emergency department. J Emerg Med 1997;15(1):1–7 [DOI] [PubMed] [Google Scholar]
- 14.Engel KG, Heisler M, Smith DM, et al. Patient comprehension of emergency department care and instructions: are patients aware of when they do not understand? Ann Emerg Med 2009;53(4):454–461 e415 [DOI] [PubMed] [Google Scholar]
- 15.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc 2005;80(8):991–994 [DOI] [PubMed] [Google Scholar]
- 16.Parry C, Kramer HM, Coleman EA. A qualitative exploration of a patient-centered coaching intervention to improve care transitions in chronically ill older adults. Home Health Care Serv Q 2006;25(3–4):39–53 [DOI] [PubMed] [Google Scholar]
- 17.Cavanaugh KL, Ikizler TA. Acknowledging kidney disease: is ignorance salubrious? Am J Kidney Dis 2013;61(4):536–539 [DOI] [PubMed] [Google Scholar]
- 18.Kurella Tamura M, Li S, Chen SC, et al. Educational programs improve the preparation for dialysis and survival of patients with chronic kidney disease. Kidney Int 2014;85(3):686–692 [DOI] [PubMed] [Google Scholar]
- 19.Wright Nunes J, Greene JH, Wallston K, et al. Pilot Study of a Physician-Delivered Education Tool to Increase Patient Knowledge About CKD. Am J Kidney Dis 2013;62(1):23–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Green JA, Boulware LE. Patient Education and Support During CKD Transitions: When the Possible Becomes Probable. Adv Chronic Kidney Dis 2016;23(4):231–239 [DOI] [PubMed] [Google Scholar]
- 21.Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines for Acute Kidney Injury. Kidney International 2012;2(1):1–138 [Google Scholar]
- 22.Chawla LS, Amdur RL, Amodeo S, et al. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney international 2011;79(12):1361–1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150(9):604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borson S, Scanlan JM, Chen P, et al. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc 2003;51(10):1451–1454 [DOI] [PubMed] [Google Scholar]
- 25.Cavanaugh KL, Osborn CY, Tentori F, et al. Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clin Kidney J 2015;8(4):462–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wallston KA, Cawthon C, McNaughton CD, et al. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med 2014;29(1):119–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright JA, Wallston KA, Elasy TA et al. Development and Results of a Kidney Disease Knowledge Survey Given to Patients With CKD. American journal of kidney diseases : the official journal of the National Kidney Foundation 2011;57(3):387–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright Nunes JA, Wallston KA, Eden SK, et al. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int 2011;80(12):1344–1351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finkelstein FO, Story K, Firanek C, et al. Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int 2008;74(9):1178–1184 [DOI] [PubMed] [Google Scholar]
- 30.Saunders MR, Kim SD, Patel N, et al. Hospitalized patients frequently unaware of their chronic kidney disease. J Hosp Med 2015;10(9):619–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kellum JA, Lameire N, for the KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care 2013;17(1):204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aitken E, Carruthers C, Gall L, et al. Acute kidney injury: outcomes and quality of care. QJM 2013;106(4):323–332 [DOI] [PubMed] [Google Scholar]
- 33.Greer RC, Liu Y, Crews DC, et al. Hospital discharge communications during care transitions for patients with acute kidney injury: a cross-sectional study. BMC Health Serv Res 2016;16:449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCullough PA, Maynard RC. Treatment disparities in acute coronary syndromes, heart failure, and kidney disease. Contrib Nephrol 2011;171:68–73 [DOI] [PubMed] [Google Scholar]
- 35.Karsanji DJ, Pannu N, Manns BJ, et al. Disparity between Nephrologists’ Opinions and Contemporary Practices for Community Follow-Up after AKI Hospitalization. Clin J Am Soc Nephrol 2017;12(11):1753–1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mehta R, Bihorac A, Selby NM, et al. Establishing a continuum of acute kidney injury - tracing AKI using data source linkage and long-term follow-up: Workgroup Statements from the 15th ADQI Consensus Conference. Can J Kidney Health Dis 2016;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dageforde LA, Cavanaugh KL. Health literacy: emerging evidence and applications in kidney disease care. Adv Chronic Kidney Dis 2013;20(4):311–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cavanaugh KL. Patient Experience Assessment is a Requisite for Quality Evaluation: A Discussion of the In-Center Hemodialysis Consumer Assessment of Health Care Providers and Systems (ICH CAHPS) Survey. Semin Dial 2016;29(2):135–143 [DOI] [PubMed] [Google Scholar]
- 39.Ha JF, Longnecker N. Doctor-patient communication: a review. Ochsner J 2010;10(1):38–43 [PMC free article] [PubMed] [Google Scholar]
- 40.Morton RL, Schlackow I, Staplin N, et al. Impact of Educational Attainment on Health Outcomes in Moderate to Severe CKD. Am J Kidney Dis 2016;67(1):31–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pisani MA, Kong SY, Kasl SV, et al. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med 2009;180(11):1092–1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joray S, Wietlisbach V, Bula CJ. Cognitive impairment in elderly medical inpatients: detection and associated six-month outcomes. Am J Geriatr Psychiatry 2004;12(6):639–647 [DOI] [PubMed] [Google Scholar]
- 43.Rahman M, Williams G, Al Mamun A. Gender differences in hypertension awareness, antihypertensive use and blood pressure control in Bangladeshi adults: findings from a national cross-sectional survey. J Health Popul Nutr 2017;36(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Madsen TE, Baird KA, Silver B, et al. Analysis of Gender Differences in Knowledge of Stroke Warning Signs. J Stroke Cerebrovasc Dis 2015;24(7):1540–1547 [DOI] [PubMed] [Google Scholar]
- 45.von Wagner C, Knight K, Steptoe A, et al. Functional health literacy and health-promoting behaviour in a national sample of British adults. J Epidemiol Community Health 2007;61(12):1086–1090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Davey J, Holden CA, Smith BJ. The correlates of chronic disease-related health literacy and its components among men: a systematic review. BMC Public Health 2015;15:589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silver SA, Harel Z, McArthur E, et al. 30-Day Readmissions After an Acute Kidney Injury Hospitalization. Am J Med 2017;130(2):163–172 e164 [DOI] [PubMed] [Google Scholar]
- 48.Siew ED, Peterson JF, Eden SK, et al. Outpatient nephrology referral rates after acute kidney injury. Journal of the American Society of Nephrology : JASN 2012;23(2):305–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lipworth L, Abdel-Kader K, Morse J, et al. High prevalence of non-steroidal anti-inflammatory drug use among acute kidney injury survivors in the southern community cohort study. BMC Nephrol 2016;17(1):189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ortiz-Soriano V, Alcorn JL 3rd, Li X, et al. A Survey Study of Self-Rated Patients’ Knowledge About AKI in a Post-Discharge AKI Clinic. Can J Kidney Health Dis 2019;6:2054358119830700. [DOI] [PMC free article] [PubMed] [Google Scholar]