Abstract
Objectives:
Despite the high prevalence of non-suicidal self-injury (NSSI), no research has systematically studied the occurrence and effects of stigmatization by others towards NSSI scarring.
Method:
The current study measured implicit and explicit attitudes among undergraduates towards NSSI scarring using the Implicit Association Test and questionnaires to compare implicit and explicit biases towards NSSI with biases towards tattoos, a culturally-sanctioned form of self-determined marking, as well as non-intentional disfigurement.
Results:
Our study demonstrated strong negative implicit and explicit biases towards NSSI when comparing NSSI to tattoos and non-intentional disfigurement.
Conclusions:
Results extend previous research describing stigma towards mental illness and suggest a large negative bias towards NSSI. The importance of studying how stigma affects those who bear scarring from NSSI is discussed.
Keywords: Stigma, non-suicidal self-injury, implicit attitudes, explicit attitudes
Non-suicidal self-injury (NSSI) is defined as the intentional damage of one’s own tissue without associated suicidal intent (Nock, 2010). Research indicates that this behavior is relatively prevalent with pooled estimates suggesting that, among nonclinical samples, 17.2% of adolescents, 13.4% of young adults, and 5.5% of adults endorse a history of NSSI (Swannell, Martin, Page, Hasking, & St. John, 2014). Of those who have engaged in NSSI, as many as half report that they have permanent visible scarring as a result of the behavior (Burke, Hamilton, Cohen, Stange, & Alloy, 2016). Although scarring is a well-known direct consequence of NSSI, relatively few empirical studies have systematically examined its psychosocial consequences and correlates. Extant research suggests that individuals with NSSI scarring often report negative cognitions about their scars and associated feelings of shame and embarrassment (Bachtelle & Pepper, 2015; Burke, Olino, & Alloy, 2017; Lewis & Mehrabkhani, 2016). Burke and colleagues (2017) found that those who reported greater negative socially-related cognitions (e.g., shame, embarrassment) about their scars exhibited higher levels of social anxiety, depression, and suicidal ideation. Other literature has found that NSSI scars are associated with significantly elevated levels of negative body image, including lower appearance evaluation and body area satisfaction (Dyer, Hennrich, Borgmann, White, & Alpers, 2013; Dyer, Mayer-Eckhard, White, & Alpers, 2015). Taken together, this literature suggests that permanent scarring from NSSI may have a detrimental impact on individuals’ psychological health.
Despite the high prevalence of NSSI and scarring from the behavior, no research has systematically studied the occurrence and effects of stigmatization by others towards visible NSSI scarring. This lack of research on stigmatization of visible scarring from NSSI is surprising, as these marks may be interpreted as physical documentation of a behavioral symptom of mental illness by the general public (despite literature suggesting that not all with a NSSI history meet criteria for a mental disorder; Nock, 2009). Research indicates that the stigmatization of mental disorders has increased in the United States over the past 50 years, and those with psychiatric disorders are one of the most stigmatized classes of individuals (Stier & Hinshaw, 2007). In general, the public perceives individuals with mental illnesses to be threatening, violent, and/or inept, which, in turn, leads to social rejection (Corrigan, Edwards, Green, Diwan, & Penn, 2001; Corrigan, Kerr, & Knudsen, 2005). These negative perceptions align with experimental research, which has demonstrated significant discrimination against those with mental illness, both with respect to interpersonal interactions as well as workplace hiring, when compared to physical illness (Hipes, Lucas, Phelan, & White, 2016; Lucas & Phelan, 2012). Importantly, individuals who engage in NSSI may be at risk for additional stigmatization beyond that directed towards those perceived as generally mentally ill, as clinical opinion suggests that the act of NSSI is often interpreted pejoratively by the public as not only associated with mental illness but also as a manipulative or attention-seeking behavior (Favazza, 1998; Gratz, 2006).
Research suggests that stigmatized individuals suffer a variety of adverse social, emotional, and economic effects, such as social withdrawal, low self-esteem, self-deprecation, negative affect, shame, and decreased economic productivity (Heatherton, Kleck, Hebl, & Hull, 2000; Link, Struening, Rahav, Phelan, & Nuttbrock, 1997; Stier & Hinshaw, 2007). For those with psychiatric disorders, stigmatization has been associated with higher symptom levels, even after accounting for pre-existing symptoms (Markowitz, 1998; Stier & Hinshaw, 2007). Recent research suggests that engaging in NSSI may not only follow psychopathology, but also may put individuals at risk for greater levels of psychopathology (e.g., lower self-esteem, higher depression) (Garisch & Wilson, 2015; Lundh, Wångby-Lundh, & Bjärehed, 2011), which, coupled with the effects of stigmatization, may give rise to a vicious cycle of psychopathology and self-destructive behaviors (You, Leung, & Fu, 2012). Indeed, the stigmatization associated with scarring from NSSI may have a lasting negative impact on an individual’s psychological health and interpersonal interactions, putting vulnerable individuals at greater risk for these outcomes. Despite the high prevalence of NSSI and the awareness of the long-term consequences of stigma towards mental health, to our knowledge, there has been no research that has examined the occurrence and nature of stigma towards NSSI.
To address this gap in the literature, we measured stigma towards NSSI among individuals without a history of NSSI using both implicit and explicit measures. There is a broad literature describing the relationship between scores on measures of explicit attitudes and stigmatizing behavior (Angermeyer & Matschinger, 2004; Hinshaw & Stier, 2008; Link et al., 1987; Link, Phelan, Bresnahan, Stueve, & Pescosolido, 1999; Rüsch, Todd, Bodenhausen, & Corrigan, 2010). For example, studies have demonstrated that those who hold more negative beliefs about individuals with mental disorders are more likely to report a desire for social distance (i.e., decreased prosocial behaviors) (Jorm & Oh, 2009) and greater acceptance of discriminatory practices (Angermeyer & Matschinger, 2004). Notably, findings from this body of literature suggest that not all stigma towards psychiatric disorders is of the same nature or severity (Link et al., 1999), highlighting the utility of examining stigma towards NSSI specifically.
Although explicit measures can provide meaningful information about stigmatization, they are inherently limited by social desirability biases (Teachman, Wilson, & Komarovskaya, 2006). Further, research suggests that individuals respond differently when assessed with explicit measures than with implicit measures, which assess unconscious, automatic, and immediate reactions (Gawronski & Bodenhausen, 2006). Studies that have used implicit measures of stigma have shown that greater negative implicit bias can predict discriminatory behavior (e.g., greater social distancing) even when explicit measures do not indicate the presence of bias (Bessenoff & Sherman, 2000; Neumann, Hülsenbeck, & Seibt, 2004; Ziegert & Hanges, 2005). Explicit and implicit measures provide complementary, but distinct, information regarding attitudes towards NSSI. Thus, we assessed both implicit and explicit attitudes towards NSSI in this study.
The Implicit Association Test (IAT) examines response time to stimuli in order to measure one’s implicit association of a concept (e.g., NSSI scarring, tattoos) with a particular attribute (e.g., good-bad) (Greenwald, Mcghee, & Schwartz, 1998). Faster response times indicate a stronger implicit association between the concept and the attribute and slower response times indicate a weaker implicit association between concept and attribute (Greenwald et al., 1998). The IAT has been used to examine stigmatization across a range of concepts and recently has been used to measure stigma towards mental health. Results suggest that individuals from the general population implicitly view individuals with mental illness in a pejorative manner (Lincoln, Arens, Berger, & Rief, 2008). For example, using the IAT, researchers found that healthy samples possess negative implicit attitudes towards mental illness, such that they are more likely to view individuals with mental illness as both helpless and blameworthy (Teachman et al., 2006). Another group of researchers compared implicit attitudes towards depression versus physical illness and found that participants displayed more negative attitudes towards depression than physical illness on the IAT (Pettit & Monteith, 2011). However, individuals did not explicitly rate depression more negatively than physical illness.
Importantly, although the IAT is useful in that it can compare the relative strength of associations with attributes between complementary concepts (e.g., NSSI/non-intentional disfigurement; NSSI/tattoo), it is unable to measure the absolute strength of a single association between a concept and an attribute. Thus, the Single Category-IAT (SC-IAT) was developed to fill this gap in the assessment of implicit attitudes (Karpinski & Steinman, 2006) and has been used in social psychology research. For example, Wang and colleagues utilized the SC-IAT to demonstrate that Chinese undergraduates’ automatic associations between mental illness and negative descriptors were stronger than their associations between mental illness and positive descriptors (Wang, Huang, Jackson, & Chen, 2012).
Current Study
We investigated the presence of implicit and explicit stigmatization towards scarring from NSSI. Implicit and explicit attitudes towards NSSI scarring were compared to explicit and implicit attitudes towards two comparison forms of disfigurement, including non-intentional disfigurement (e.g., accidental injury, surgical injury, birthmarks) and tattoos. Scarring from non-intentional incidents was intended to represent an involuntary form of body disfigurement. In contrast, markings from tattoos were intended to represent an intentional, voluntary, and culturally-sanctioned form of body modification, as opposed to NSSI, which is intentional, voluntary, but not culturally-sanctioned. Implicit attitudes towards NSSI were measured by comparing attitudes towards NSSI to the two comparison conditions using the traditional IAT. Absolute implicit attitudes towards NSSI were examined using the SC-IAT. Finally, we assessed explicit attitudes towards NSSI via two self-report measures. One measure assessed explicit ratings of the attributes used in the IAT tasks. The second measure assessed behavioral intentions and discriminatory practices towards those with a history of NSSI.
Based on literature suggesting negative implicit and explicit views towards mental illness (Pettit & Monteith, 2011; Teachman et al., 2006; Wang et al., 2012), we hypothesized that there would be greater negative implicit and explicit attitudes towards NSSI when measured absolutely and when compared to implicit and explicit attitudes towards tattoos and non-intentional disfigurement. Specifically, we hypothesized that when measured absolutely, participants would demonstrate implicit and explicit attitudes that those with NSSI scarring are bad, rejection-worthy, and dangerous. Moreover, we hypothesized that participants would demonstrate significantly more negative implicit and explicit attitudes towards NSSI as compared to their attitudes towards intentional, but culturally sanctioned, forms of disfigurement (i.e., tattoos), as well as involuntary forms of disfigurement (i.e., accidental scars). Furthermore, we hypothesized that results from explicit measures would follow the direction of results from implicit measures, but that these results would be of lesser magnitude, due to social desirability biases.
Methods
Participants
Participants in the current study were 368 undergraduate students enrolled in a university in a large city in the northeastern United States. Participants were recruited from psychology classes and compensated for participation with course credit. Participants first completed an online screener to determine study eligibility. Participants who were eligible for the study were instructed to sign up for an in-person session. Exclusion criteria in the current study included: having any lifetime history of NSSI (n = 115), being unable to read or speak English (n = 0), not understanding the definition of NSSI (n = 1), having abnormal vision (n = 0), being under the age of 18 (n = 0), not completing the in-person session (n = 16). The final study sample included 236 undergraduates. The majority of the sample was female (n = 193; 82.5%) and the mean age was 20 years (SD = 3.93). Participants were 58.1% White, 12.8% Black, 10.3% East Asian, 6.8% South Asian, 7.3% Biracial, and 4.7% other. A total of 15 participants (6.4%) identified as Hispanic or Latino.
Measures
Explicit self-report measures
Deliberate Self-Harm Inventory (DSHI).
The DSHI (Gratz, 2001) assesses the frequency, duration, and forms of non-suicidal self-injurious behaviors (e.g., cutting, carving, burning, biting, head-banging). The DSHI asks how often the participant has engaged in each of 17 types of NSSI behaviors with the prompt, “Have you ever intentionally (i.e., on purpose) _______?” For each of the 17 types of NSSI behaviors, respondents are asked about age at onset, frequency, recency, years of engagement, and if the behavior ever resulted in a hospitalization or required medical treatment. Research has supported the DSHI’s internal consistency, test-retest reliability, and construct, discriminant, and convergent validity in a university-student sample (Fliege et al., 2006; Gratz, 2001). In the current study, the internal consistency was α = .67. This measure was used to assess history of engagement in NSSI, and participants who reported a positive history were excluded from the current analyses.
Behavioral Intention Questionnaires (BIQs).
The BIQs were designed for the purposes of this study to measure explicit behavioral intentions. The BIQs used a format developed by Triandis (1977) and included items similar to those used in social distancing scales (Corrigan, Markowitz, Watson, Rowan, & Kubiak, 2003; Link et al., 1987; Triandis, 1977). Similar behavioral intention questionnaires have been used in IAT research (Bonar et al., 2012; White, Hogg, & Terry, 2002). Separate BIQs were created to assess behavioral intentions towards individuals with scarring from NSSI, those with visible tattoos, and individuals with scarring from non-intentional incidents. Each BIQ contained 17 items that assessed the extent to which individuals would either include or discriminate against those from the three groups. A sample item is “Would you want to become friends with X?” where X represents a same-age peer who has engaged in NSSI in the past, has visible tattooing, or has visible scars from a car accident. Individuals responded using a Likert scale ranging from 1 (very unlikely) to 7 (very likely). Scores ranged from 17 to 119 for each questionnaire with higher scores indicating a greater likelihood that the participant would engage in social interaction with the same-age peer.
We expected that responses might differ based on whether the item assessed a sexual/romantic relationship versus a non-sexual/non-romantic relationship. Thus, we created corresponding BIQ subscales and conducted analyses for each subscale to assess non-sexual/non-romantic interactions separately from sexual/romantic interactions for NSSI (sexual/romantic α = .97, non-sexual/non-romantic α = .95), tattoos (sexual/romantic α = .97, non-sexual/non-romantic α = .95), and non-intentional disfigurement (sexual/romantic α = .98, non-sexual/non-romantic α = .95).
Semantic Differential Scale (SDS).
The SDS is another explicit measure that is often used in conjunction with IATs to evaluate explicit (i.e., self-reported) ratings of attributes used in the implicit tasks. SDS measures were developed using semantic differential methodology described in previous literature (Maguire, 1973; Osgood, Suci, & Tannenbaum, 1957; Schibeci, 1982) and used a bipolar scale to rank a group on a pair of attributes. SDS measures for NSSI (α = .75), tattoos (α = .77), and non-intentional disfigurement (α = .69) were designed to assess the extent to which individuals endorse qualities taken from the attribute trials of the IAT, including good/bad, safe/dangerous, and accepted/rejected. Each item used a 7-point bipolar scale anchored at either end by one word of the dichotomous pair, such as −3 (positive attribute), 0 (neutral), and +3 (negative attribute). Participants were first provided with a description of a person with each characteristic (i.e., NSSI, tattoos, or non-intentional disfigurement) and then asked to rate each group on the three pairs of attributes. Ratings were recoded from −3 to +3 into scores ranging from 1 to 7, with higher scores representing more negative attributes. A mean score of 3.5 was used to represent neutral ratings towards the group.
Implicit Association Tests (IAT).
Participants completed four IATs administered via computer using E-Prime software (Psychological Software Tools Incorporated, 2016): an accept/reject NSSI/non-intentional disfigurement IAT (split-half α = .54), an accept/reject NSSI/tattoo IAT (split-half α = .43), a good/bad NSSI/non-intentional disfigurement IAT (split-half α = .61), and a good/bad NSSI/tattoo IAT (split-half α = .52). The IAT procedure was modeled after the IAT used in a previous study on implicit attitudes about anxiety (Wong, Morrison, Heimberg, Goldin, & Gross, 2014).
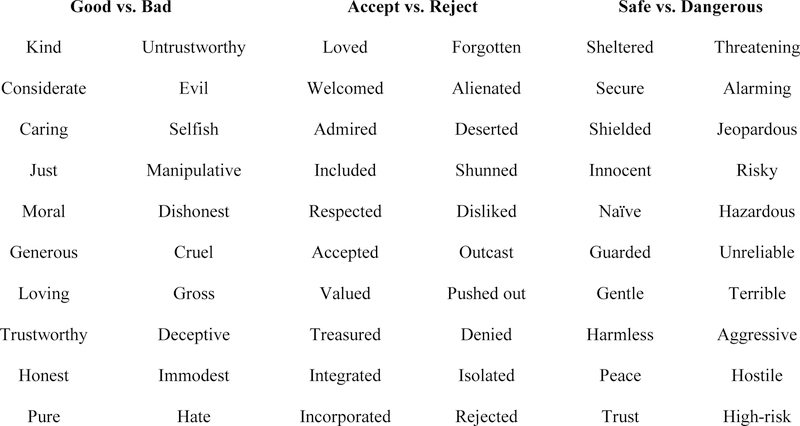
In each IAT, participants were asked to quickly categorize concept and attribute descriptors (see Figure 1 for complete list of attributes). In the accept/reject NSSI/non-intentional disfigurement IAT, participants categorized concepts describing NSSI scars (i.e., cutting, self-harm, self-injury, self-mutilation) and accident scars (i.e., injury, wounds, hurt, disfigurement) and accept and reject attributes. In the accept/reject NSSI/tattoo IAT, participants categorized concepts describing NSSI scars and tattoos (i.e., tat, branded, body modification, inked) and accept and reject attributes. In the good/bad NSSI/non-intentional disfigurement IAT, participants categorized concepts describing NSSI scars and accident scars and good and bad attributes. In the good/bad NSSI/tattoo IAT, participants categorized concepts describing NSSI scars and tattoos and good and bad attributes.
Figure 1.
Complete list of words for the IAT and SC-IAT attribute categories.
This dual categorization task consisted of five blocks of trials with three practice blocks of 24 trials each and two critical blocks of 48 trials each. The practice blocks were single categorizations (i.e., categorization of only attributes or only concepts), and the critical blocks were dual categorization tasks (i.e., categorization of both attributes and concepts). The first block included 24 practice trials for attribute discrimination (i.e., good and bad or acceptance and rejection). Participants categorized good/acceptance attributes with the A key and bad/rejection words with the L key. The second block included 24 practice trials of concept discrimination (i.e., NSSI scars and tattoos or NSSI scars and accident scars). Participants categorized NSSI concepts with the A key and accident scars/tattoos concepts with the L key. The third block was a dual categorization task consisting of 48 critical trials in which participants categorized concepts and attributes on the same key. NSSI scars concepts and good/acceptance attributes were categorized with the A key, and accident scars/tattoos concepts and bad/rejection attributes were categorized with the L key. The fourth block included another practice block of 24 trials for concept discrimination similar to the second block, however, the key assignments switched. Participants now categorized NSSI scars concepts with the L key and accident scars/tattoos concepts with the A key. The fifth block was another dual categorization task consisting of 48 critical trials similar to block three, but here the concept categorization keys switched. Accident scars/tattoos concepts and good/acceptance attributes were categorized with the A key, and NSSI scars concepts and bad/rejection attributes were categorized with the L key. All IATs followed the same procedure. Participants had as much time as needed to respond to each trial.
Single Category Implicit Association Test (SC-IAT).
In the second half of the study, participants completed a series of three SC-IATs, designed to examine absolute strength of implicit attitudes towards NSSI, without comparing NSSI attitudes to another concept category (e.g., tattoos or scarring from non-intentional incidents) as in the IAT. Participants completed three SC-IATs: a good/bad SC-IAT (split-half α = .36), an accept/reject SC-IAT (split-half α = .42), and a safe/dangerous SC-IAT (split-half α = .64). All SC-IATs were modeled after original research using the SC-IAT (Karpinski & Steinman, 2006).
In each SC-IAT, participants categorized concept and attribute words. Across all SC-IATs, NSSI scar concepts (e.g., cutting, self-harm, self-injury, non-suicidal self-injury, self-mutilation, self-burning) remained the same; however, the attributes varied. Participants categorized good and bad attributes in the good/bad SC-IAT, dangerous and safe attributes in the dangerous/safe SC-IAT, and accept and reject attributes in the accept/reject SC-IAT. The SC-IAT NSSI concepts and good/bad and accept/reject attributes were the same as in the IAT. The safe (i.e., safe, innocent, naive, guarded) and dangerous (i.e., threatening, alarming, risky, hazardous) attributes were unique to the SC-IAT. (For a complete list of attribute words, see Figure 1.)
Each SC-IAT consisted of three blocks of trials with one practice block of 30 trials and two critical blocks of 96 trials each. The first block included 30 practice trials in which participants categorized attributes. Participants categorized safe/good/accept attributes with the A key and dangerous/bad/reject attributes with the L key. The second block included 96 critical trials in which participants categorized NSSI concepts and attributes. Participants categorized NSSI concepts and safe/good/accept attributes with the A key and dangerous/bad/reject attributes with the L key. The third block included 96 critical trials in which the key for NSSI concepts categorization switched. Participants categorized safe/good/accept attributes with the A key and NSSI concepts and dangerous/bad/reject attributes with the L key. Participants had a total of 1500ms to respond to each trial. Participants received response feedback for 500ms after each trial. A green OOO appeared following correct categorizations, a red XXX appeared following incorrect categorizations, and the phrase, “Please respond more quickly!” appeared if participants responded too slowly.
Procedure
Participants were recruited using an online screener survey. Participants who completed the screener survey and met inclusion/exclusion criteria received an email instructing them to sign up for the current study. Participants arrived at the lab and completed the IAT and SC-IAT tasks. They then completed self-report measures assessing psychiatric symptoms and personality traits that were not included in this current study. Finally, participants completed self-report measures of explicit attitudes towards NSSI, tattoos, and non-intentional disfigurement, as well as the BIQs. Participants received compensation in the form of course credit.
Data Analytic Plan
A priori power analyses were conducted to determine the number of participants necessary to detect small to moderate (i.e., 0.20 – 0.50) effects in the implicit association tasks. Results suggested that 210 participants were necessary. We recruited beyond this number to account for data with response times and error scores that were outside our cutoffs. Our sample size of 236 participants suggested that the study was well-powered to detect effects. Standardized D scores were calculated for both the IAT and SC-IAT according to the methods described in previous literature and are reported here as the mean D score (MD) (Greenwald, Nosek, & Banaji, 2001; Karpinski & Steinman, 2006). Exclusion criteria were implemented using the recommendations for the IAT (Greenwald et al., 2001) and the SC-IAT (Karpinski & Steinman, 2006). That is, participants who exhibited error values of greater than 40% were excluded from the IAT study analyses, and participants who exhibited error values of greater than 20% were excluded from the SC-IAT study analyses. We conducted a repeated measures ANOVA to compare participants’ scores on the explicit measures (i.e., SDS and BIQs) across conditions. We examined pairwise comparisons between NSSI and tattoo or non-intentional disfigurement conditions using a Bonferroni correction to adjust for multiple comparisons.
Before conducting study analyses, we evaluated whether scores on implicit and explicit measures differed significantly based on gender. Scores on implicit measures (i.e., IAT and SC-IAT) did not differ based on gender. Likewise, scores on the NSSI SDS explicit measure did not differ based on gender. However, total scores on the NSSI BIQ and non-intentional disfigurement BIQ differed across gender. We evaluated gender differences further in a series of post-hoc analyses.
Results
Implicit Measures
Participants with error values outside of the stated cutoffs were excluded from each set of analyses. There were no significant differences between those who were included and those who were excluded from IAT or SC-IAT analyses on demographic variables and explicit measures.
Accept/Reject NSSI/non-intentional disfigurement IAT.
Participants (n = 35) were excluded from the accept/reject NSSI/non-intentional disfigurement IAT analyses for having error scores greater than 40%. One-sample t-test analyses of the accept-reject NSSI/non-intentional disfigurement IAT scores revealed that participants showed an overall acceptance of non-intentional disfigurement and rejection of NSSI scarring (MD = 0.92, SD = 0.45, 95% CI [0.85, 0.98]), t(204) = 28.83, p < .001, |d| = 2.01 .
Accept/Reject NSSI/tattoo IAT.
Participants (n =15) were excluded from the accept/reject NSSI/tattoo IAT analyses for having error scores greater than 40%. One-sample t-test analyses of the accept-reject NSSI/tattoo IAT scores revealed that participants showed an overall acceptance of tattoos and rejection of NSSI scarring (MD = 1.09, SD = 0.46, 95% CI [1.03, 1.15]), t(215) = 35.11, p < .001, |d| = 2.39.
Good/Bad NSSI/non-intentional disfigurement IAT.
Participants (n = 3) were excluded from the good/bad NSSI/non-intentional disfigurement IAT analyses for having error scores greater than 40%. One-sample t-test analyses of the good/bad NSSI/non-intentional disfigurement IAT scores revealed that participants demonstrated greater associations between non-intentional disfigurement and good and between NSSI scarring and bad (MD = 0.38, SD = 0.37, 95% CI [0.33, 0.43]), t(222) = 15.21, p < .001, |d| = 1.02.
Good/Bad NSSI/tattoo IAT.
No participants were excluded from the good/bad NSSI/tattoo IAT analyses, as all participants had error scores less than 40%. One-sample t-test analyses of the good/bad NSSI/tattoo IAT scores revealed that participants demonstrated greater associations between tattoos and good and between NSSI scarring and bad (MD = 0.60, SD = 0.34, 95% CI [0.56, 0.65]), t(226) = 26.41, p < .001, |d| = 1.75.
Good/Bad SC-IAT.
Participants (n = 14) were excluded from the good/bad SC-IAT analyses for having error scores greater than 20%. One-sample t-test analyses of the good-bad SC-IAT scores revealed that participants were more likely to associate NSSI scarring with bad than good (MD = −0.49, SD = 0.32, 95% CI [−0.54, −0.45]), t(204) = −22.23, p < .001, |d| = 1.55.
Accept/Reject SC-IAT.
Participants (n = 15) were excluded from the accept/reject SC-IAT analyses for having error scores greater than 20%. One-sample t-test analyses of the accept-reject SC-IAT scores revealed that participants were more likely to associate NSSI scarring with rejection than acceptance (MD = −0.39, SD = 0.33, 95% CI [−0.43, −0.34]), t(203) = −16.95, p < .001, |d| = 1.19.
Safe/Dangerous SC-IAT.
Participants (n = 35) were excluded from the safe/dangerous SC-IAT analyses for having error scores greater than 20%. One-sample t-test analyses of the safe/dangerous SC-IAT scores revealed that participants were more likely to associate NSSI scarring with danger than safety (MD = −0.43, SD = 0.37, 95% CI [−0.48, −0.38]), t(185) = −15.89, p < .001, |d| = 1.17.
Explicit Measures
Separate repeated measures ANOVAs were conducted to compare participants’ scores on explicit measures across conditions. Pairwise comparisons between NSSI, tattoos, and non-intentional disfigurement conditions were examined using a Bonferroni correction to adjust for multiple comparisons.
SDS.
A repeated measures ANOVA with a Greenhouse-Geisser correction demonstrated that total SDS score differed across the three comparison conditions [F(1.89, 433.83) = 250.79, p < .001, η2 = 0.52]. Post hoc tests using a Bonferroni correction revealed that participants responded significantly differently on the NSSI SDS compared to the tattoo SDS (MD = −4.40, SD = 0.30, 95% CI [−5.14, −3.67]), p < .001, |d| = 0.96. Similarly, results suggested a significant difference between NSSI SDS scores and non-intentional disfigurement SDS scores (MD = −6.07, SD = 0.29, 95% CI [−6.76, −5.38]), p < .001, |d| = 1.39. These results indicate that participants assigned more negative ratings to NSSI.
BIQ.
A repeated measures ANOVA with a Greenhouse-Geisser correction demonstrated that BIQ scores for non-sexual/non-romantic interactions differed across comparison conditions [F(1.73, 405.30) = 106.09, p < .001, η2 = 0.31]. Post hoc tests using a Bonferroni correction revealed that there was a significant difference between non-sexual/non-romantic NSSI BIQ scores and non-sexual/non-romantic tattoo BIQ scores (MD = −7.71, SD = 0.92, 95% CI [−9.92, −5.50]), p < .001, |d| = 0.55, as well as a significant difference between non-sexual/non-romantic NSSI BIQ scores and non-sexual/non-romantic non-intentional disfigurement BIQ scores (MD = −12.96, SD = 1.03, 95% CI [−15.44, −10.48]), p < .001, |d| = 0.84. These results indicate that participants were less willing to engage in a non-sexual/non-romantic interaction with an individual who had a history of NSSI.
A second repeated measures ANOVA demonstrated that BIQ score for sexual/romantic interactions also differed across comparison conditions [F(2, 470) = 55.73, p < .001, η2 = 0.19]. Post hoc tests using a Bonferroni correction revealed that there was a significant difference between sexual/romantic NSSI BIQ scores and sexual/romantic tattoo BIQ scores (MD = −1.97, SD = 0.24, 95% CI [−2.56, −1.38]), p < .001, |d| = 0.53, as well as a significant difference between sexual/romantic NSSI BIQ scores and sexual/romantic non-intentional disfigurement BIQ scores (MD = −2.23, SD = 0.23, 95% CI [−2.79, −1.68]), p < .001, |d| = 0.63. These results indicate that participants also were less willing to engage in a sexual/romantic interaction with an individual who had a history of NSSI.
Correlations between Implicit and Explicit Measures
Zero-order correlational analyses were conducted between implicit measures, between explicit measures, and between implicit and explicit measures (Table 1). Correlations between the traditional IATs were positive and small, r(222) = |.22|, to moderate, r(196) = |.40|, and correlations between the SC-IATs were positive and small, rs < |.30|. Both sets of correlations were statistically significant. Correlations between implicit and explicit measures were small, rs < |.25|, and often were not statistically significant. Finally, correlations between explicit measures ranged from small, r(233) = |.02|, to large, r(236) = |.75|, and many associations achieved statistical significance.
Table 1.
Correlational analyses between implicit and explicit measures.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | 19. | 20. | 21. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Accept/Reject Non-intentional disfigurement IAT | 1 | ||||||||||||||||||||
| 2. Good/Bad Non-intentional disfigurement IAT | .26** | 1 | |||||||||||||||||||
| 3. Accept/Reject Tattoo IAT | .40** | .12 | 1 | ||||||||||||||||||
| 4. Good/Bad Tattoo IAT | ** | .22** | .30** | 1 | |||||||||||||||||
| 5. Accept/Reject SC-IAT | −10 | −.09 | −.07 | −.07 | 1 | ||||||||||||||||
| 6. Good/Bad SC-IAT | .09 | −.11 | .04 | −.13 | .26** | 1 | |||||||||||||||
| 7. Safe/Dangerous SC-IAT | −.05 | −.19** | −.03 | −.14 | .19** | .25** | 1 | ||||||||||||||
| 8. NSSI familiarity | −.04 | −.01 | −.09 | .03 | .10 | .10 | .03 | 1 | |||||||||||||
| 9. Participant BDI score | −.13 | −.05 | −.11 | −.02 | .08 | .07 | .17* | .15* | 1 | ||||||||||||
| 10. Accept/Reject NSSI SDS | .07 | −.02 | .08 | .05 | −.03 | −.10 | −.12 | −.23** | .13* | 1 | |||||||||||
| 11. Good/Bad NSSI SDS | .03 | .06 | .13 | .04 | .004 | −.02 | −.21** | −.11 | .10 | .39** | 1 | ||||||||||
| 12. Accept/Reject Non-intentional disfigurement SDS | −.09 | −.18** | .01 | .01 | .03 | .09 | −.02 | .06 | .11 | .18** | .06 | 1 | |||||||||
| 13. Good/Bad Non-intentional disfigurement SDS | −.04 | −.03 | −.03 | .03 | −.03 | .02 | −.07 | −.09 | .04 | .31** | 33** | .38** | 1 | ||||||||
| 14. Accept/Reject Tattoo SDS | −.02 | −.20** | .03 | −.04 | .21** | .02 | .07 | −.05 | .17* | .26** | .03 | .40** | .25** | 1 | |||||||
| 15. Good/Bad Tattoo SDS | −.04 | −.16* | −.04 | .04 | .07 | −.06 | −.004 | −.19** | .04 | .25** | .28** | .25** | .37** | .46** | 1 | ||||||
| 16. Non-sexual/non-romantic NSSI BIQ | −.004 | −.002 | −.01 | −.001 | .12 | .11 | .14 | .21** | .04 | −.32** | −.32** | −.06 | −.15* | −.02 | −.30** | 1 | |||||
| 17. Sexual/Romantic NSSI BIQ | −.04 | −.04 | .01 | −.001 | .08 | .15* | .18* | .26** | .07 | −.28** | −.31** | .14* | .02 | .04 | −.16* | .63** | 1 | ||||
| 18. Non-sexual/non-romantic Non-intentional disfigurement BIQ | .05 | .10 | .04 | .01 | −.01 | −.03 | −.04 | .11 | −.07 | −.10 | −.11 | −.31** | −.32** | −.07 | −.28** | .54** | .24** | 1 | |||
| 19. Sexual/Romantic Non-intentional disfigurement BIQ | −.05 | .01 | .10 | .06 | −.11 | .02 | .09 | .12 | .03 | −.17* | −.12 | −.14* | −.11 | −.02 | −.18** | .33** | .48** | .55** | 1 | ||
| 20. Non-sexual/non-romantic Tattoo BIQ | .10 | .11 | .07 | .01 | −.06 | .05 | .02 | .17* | −.07 | −.12 | −.11 | −.26** | −.19** | −.22** | −.46** | .67** | .36** | .75** | .43** | 1 | |
| 21. Sexual/Romantic Tattoo BIQ | .01 | .08 | .10 | .09 | −.05 | .04 | .05 | .21** | .07 | −.04 | −.08 | −.02 | −.07 | −.15* | −.36** | .36** | .47** | .33** | .56** | .52** | 1 |
Note. Correlational analyses were conducted by selecting out participants with IAT error scores > .40, resulting in different samples sizes for each IAT. All correlations between IAT variables were conducted on sample sizes ranging from n =196–222. All correlations between IAT and SC-IAT variables were conducted on sample sizes ranging from n =171–204. All correlations between SC-IAT variables were conducted on sample sizes ranging from n =186–200. Correlational analyses conducted between the Accept/Reject NSSI/Non-intentional disfigurement IAT and explicit variables used sample sizes that ranged from n =194–205. Correlational analyses conducted between the Good/Bad NSSI/Non-intentional disfigurement IAT and explicit variables used sample sizes that ranged from n =212–223. Correlational analyses conducted between the Accept/Reject Tattoo/NSSI IAT and explicit variables used sample sizes that ranged from n =205–216. Correlational analyses conducted between the Good/Bad Tattoo/NSSI IAT and explicit variables used sample sizes that ranged from n =215–227. Correlational analyses conducted between explicit variables used sample sizes that ranged from n =230–236.
Correlational analyses conducted between the Accept/Reject SC-IAT and explicit variables used sample sizes that ranged from n =195–204. Correlational analyses conducted between the Good/Bad SC-IAT and explicit variables used sample sizes that ranged from n =196–205. Correlational analyses conducted between the Safe/Dangerous SC-IAT and explicit variables used sample sizes that ranged from n =178–186. IAT = Implicit Association Task; SC-IAT = Single Category Implicit Association Task; NSSI = Non-suicidal self-injury; BDI = Beck Depression Inventory – II; SDS = Semantic Differential Scale; BIQ = Behavioral Intention Questionnaire.
indicates p < .05
indicates p < 0.001
Post hoc tests
Relationship between familiarity and implicit and explicit measures.
Participants reported on the number of people they knew who had engaged in NSSI. The total number of people a participant knew was not associated with any of the implicit measures. However, the total number of people a participant knew was significantly positively correlated with total scores on the NSSI BIQ, (r(233) = .23, p < .001), tattoo BIQ, (r(233) = .20, p = .002), and non-intentional disfigurement BIQ, (r(233) = .14, p = .030). This number also was significantly negatively correlated with NSSI SDS total, (r(233) = −.20, p = .002). This suggests that the more people participants knew who had engaged in NSSI, the more positive their intended behaviors were towards people with NSSI, tattoos, and non-intentional disfigurement. Additionally, the more people participants knew who had engaged in NSSI also was related to more positive explicit ratings of NSSI.
Relationship between gender and behavioral intentions.
Independent samples t-tests were conducted to determine whether there were gender differences across behavioral intention measures. The total score on the NSSI BIQ significantly differed between men and women (MD = −7.08, SD = 3.52, 95% CI [−14.03, −0.14]), t(230) = −2.01, p = .045, |d| = 0.35. Additionally, the total score on the non-intentional disfigurement BIQ significantly differed between men and women (MD = −10.38, SD = 2.72, 95% CI [−15.75, −5.01]), t(230) = −3.81, p < .001, |d| = 0.63. We then examined whether there were significant gender differences across each of the BIQ subscales. Overall women were more accepting of a sexual/romantic interaction with individuals who had a history of NSSI compared to men. Women also were more accepting towards individuals with non-intentional disfigurement compared to men.1
Discussion
This study examined implicit and explicit stigma towards NSSI. Young adults without a history of NSSI exhibited negative implicit biases against NSSI, as demonstrated by examining NSSI alone and by comparing it to scarring from non-intentional (i.e., accidents) or self-determined (i.e., tattoos) scarring. Results from the analyses of explicit measures largely echoed the results for implicit measures. Participants demonstrated a significant negative bias towards NSSI when asked to explicitly rate individuals with NSSI on the same attribute characteristics that were included in the implicit tasks (i.e., good/bad, accept/reject, and safe/dangerous). Results from the behavioral intention measures were consistent with other analyses. Participants demonstrated a significant negative bias towards individuals with a history of NSSI, compared to individuals with tattoos or non-intentional disfigurement, when asked to consider non-sexual/non-romantic interaction (e.g., hiring someone with NSSI, tattoos, or scarring from non-intentional disfigurement for a job). Similarly, participants also demonstrated a significant negative bias towards individuals with a history of NSSI, as compared to the other groups, when asked to consider engaging in a sexual/romantic interaction (e.g., initiating a dating or sexual relationship). Overall, these results suggest that individuals demonstrate a strong and significant implicit and explicit negative bias towards individuals with a history of NSSI.
Results from the implicit tasks were consistent with study hypotheses and with previous literature. Researchers have demonstrated that participants exhibit negative implicit biases towards mental illness (Wang et al., 2012) and that these negative biases towards those with mental illness are stronger than the biases towards individuals from comparison conditions, such as those with physical illness (Pettit & Monteith, 2011; Teachman et al., 2006). Prior research suggests that participants are more likely to implicitly categorize individuals with mental illness as bad, helpless, and blameworthy as compared to individuals with physical illness (Pettit & Monteith, 2011). Furthermore, researchers also have demonstrated the presence of a negative implicit bias (e.g., rating NSSI as bad) among both individuals with and without a history of self-injury (Nock & Banaji, 2007). These findings are consistent with results from the present study, which demonstrated a strong and significant negative bias towards NSSI, classifying it as bad and rejection-worthy as compared to tattoos and non-intentional disfigurement using the traditional IAT, and as bad, rejection-worthy, and dangerous when classifying NSSI alone using the single-category IAT.
Furthermore, analyses using explicit measures suggest that individuals were more likely to explicitly rate those with NSSI scarring as bad, rejection-worthy, and dangerous, rather than good, acceptance-worthy, and safe, compared to those with tattoos or non-intentional disfigurement (|d|’s = 0.96, 1.39). These findings are in keeping with study hypotheses, although the magnitude of the effects were not smaller than the magnitude of effects for implicit analyses across all explicit measures. Overall, these results are consistent with social distancing theories and findings from previous literature. For example, a previous study used vignettes of individuals with various psychiatric disorders to demonstrate that healthy individuals were more likely to avoid individuals who experienced addiction or depression, as opposed to individuals who were experiencing general stress (Link et al., 1999). Similarly, a German nationwide survey revealed that individuals from the general population described individuals with schizophrenia as unpredictable and incompetent. These views were associated with a greater desire to engage in social distancing (i.e., greater desire to reject an individual with schizophrenia from a series of social relationships) (Angermeyer & Matschinger, 2004).
Accordingly, participants were less likely to report that they would accept individuals with a history of NSSI as a friend, roommate, or classmate, as compared to those with tattoos or non-intentional disfigurement (|d|’s = 0.55, 0.84; medium-large effect size). Likewise, participants also were significantly less likely to desire a sexual/romantic relationship with an individual who had a history of NSSI, compared to an individual with tattoos or non-intentional disfigurement (|d|’s = 0.53, 0.63; medium effect size). Overall, these results suggest that participants were less accepting of social relationships with an individual who had a history of NSSI compared to an individual with either tattoos or non-intentional disfigurement. Interestingly, the effect sizes for the comparisons between the NSSI and non-intentional disfigurement conditions were larger than the effect sizes for the comparisons between the NSSI and the tattoo conditions, potentially suggesting that tattoos, while culturally sanctioned, are viewed more negatively than non-intentional disfigurement.
Additionally, exploratory post hoc analyses indicated that individuals who reported that they were more familiar with NSSI (e.g., having a family member or friend with a history of NSSI) were more likely to hold accepting and inclusionary attitudes towards NSSI when considering both sexual/romantic and non-sexual/non-romantic relationships. This finding is consistent with previous literature that suggest that mental health stigma is typically decreased among family and friends of those with mental health symptoms (Jorm & Oh, 2009). These results may suggest that increased familiarity and contact with individuals who have engaged in NSSI may promote greater acceptance of NSSI among their peers. Although there were some noted gender differences, the direction of these effects was largely consistent with findings from the entire sample.
Most research to date has focused primarily on the immediate affective consequences of NSSI (Klonsky, 2009) and long-term psychological consequences, including suicidal behavior (Hamza, Stewart, & Willoughby, 2012). However, prior literature has neglected to elucidate the presence and extent of stigmatization from others based on this self-injurious behavior. This stigmatization arguably has a lasting interpersonal and psychological impact on those who engage in NSSI. This is the first study to examine implicit and explicit beliefs about NSSI. Strengths of this study include the use of two comparison conditions, especially the tattoo comparison condition, which represents a unique extension of the current literature. Previous studies have primarily compared mental illness (e.g., schizophrenia or depression) to physical illness (Pettit & Monteith, 2011; Teachman et al., 2006). As tattoos are a voluntary form of body modification that is largely culturally sanctioned, this comparison condition may help to provide context for evaluating the difference between NSSI, which is self-inflicted and non-sanctioned, and scarring from non-intentional disfigurement, which may be viewed as uncontrollable and involuntary. Additionally, the use of the single-category IAT in addition to the traditional IAT allowed for the examination of NSSI stigma in an absolute sense, without assessing it in relation to comparison conditions, compared to previous studies that have exclusively used the traditional IAT or other implicit tasks that use comparison conditions (e.g., brief IAT, Sriram & Greenwald, 2009; Go/No-Go Association Tasks, Nosek, 2001).
Notably, there were few significant associations between implicit and explicit measures. Such findings are largely consistent with other studies that use both implicit and explicit measures (Pettit & Monteith, 2011; Teachman et al., 2006; Wang et al., 2012). However, results from a meta-analysis suggested that the relationship between implicit and explicit measures may be moderated by participant factors, such as the degree of controlled responding that participants exhibit when responding to self-report (Hofmann, Gawronski, Gschwendner, Le, & Schmitt, 2005). For example, implicit and explicit ratings are more closely associated when participants respond to explicit ratings in a more spontaneous manner (i.e., relying on their initial, automatic reaction versus carefully considering the question). Accordingly, it may be that participants in this study responded to explicit measures more carefully and less spontaneously, contributing to the few significant associations between the implicit and explicit ratings.
Limitations
The current results should be considered in light of the limitations of this study. First, this study employed a sample of undergraduates, and thus, the generalizability of these findings may be limited. Future research may consider replicating this study among community samples of varying demographics. Second, we did not control for the presence of tattoos or non-intentional disfigurement, which may have influenced the strength and direction of the bias scores. Future studies focused on bias towards tattoo or non-intentional disfigurement may want to include the presence of tattoos or non-intentional disfigurement in study analyses to account for the effect of self-stigma. Third, the current study did not directly examine whether implicit attitudes towards NSSI predict stigmatizing behavior. Previous research has demonstrated that implicit attitudes can predict behavior (e.g., Dasgupta, 2010; Greenwald, Poehlman, Uhlmann, & Banaji, 2009; Kurdi et al., 2018); future studies utilizing experimental designs should examine whether implicit attitudes towards NSSI predict discriminatory behavior. Finally, this study focused on better understanding the bias towards NSSI among those without a history of the behavior. We believe that this subset of individuals is important to study in order to understand the stigmatization faced by those with a history of NSSI. However, it is also important to understand attitudes towards those with a history of NSSI among self-injurers. Indeed, self-stigmatization may occur when public stigmatization ideas are accepted, and can in turn, lead to decreases in self-esteem (Corrigan & Watson, 2002). Although beyond the scope of the current study, our team aims to examine self-stigmatization among those with a history of NSSI in future work.
Conclusions
Results indicated that negative bias towards individuals with a history of NSSI is strongly present in both implicit and explicit measures. Measuring stigma-related attitudes can be useful for identifying, preventing, and addressing stigma against mental health. For example, research has demonstrated that educational programs, especially those that facilitate contact with an individual who has struggled with mental illness, reduced scores on explicit or behavioral stigma measures, such as social distancing (Pinfold et al., 2003; Schulze, Richter-Werling, Matschinger, & Angermeyer, 2003). However, Stier and Hinshaw (2007) argue that anti-stigma interventions may increase the risk of social desirability bias, which may reduce the validity of explicit measures, underscoring the need for assessment of implicit attitudes in prevention and intervention efforts. For example, Teachman, Gapinski, Brownell, Rawlins, and Jeyaram (2003) demonstrated that negative implicit bias could be modified by manipulating information about the etiology of obesity. This suggests that there is a role for researchers to measure both explicit and implicit attitudes when designing research studies that could help improve existing prevention and intervention efforts.
Interventions that integrate education regarding risk factors and reasons for engaging in NSSI coupled with disclosure from individuals who have engaged in NSSI and are in recovery may be helpful in mitigating stigma towards NSSI (Corrigan & Fong, 2014). These interventions may be best implemented in school settings via a multipronged approach that combines both education and contact with individuals who have a history of NSSI. Researchers have demonstrated that contact with individuals who have a history of mental illness may be an important factor in developing efficacious anti-stigma interventions (Rüsch, Angermeyer, & Corrigan, 2005). For example, interventions in high schools designed to challenge stigma towards mental illness demonstrated that educational programs, especially those that facilitated contact with an individual who struggled with mental illness, reduced explicitly measured stigma, such as social distancing (Pinfold et al., 2003; Schulze et al., 2003).
Results from this research also may assist in guiding clinical interventions and navigating the therapeutic relationship between mental health professionals and individuals who engage in or have a history of NSSI. Although evidence (including the results from some of the post-hoc analyses in this study) suggests that increased contact with people with mental disorders is associated with decreased social distancing (as described in Jorm & Oh, 2009), this protective relationship may not extend to mental health professionals. Research suggests that mental health providers engage in similar amounts of social distancing as members of the general community, despite increased contact (Nordt, Rossler, & Lauber, 2005; Stuart & Arboleda-Flórez, 2001; Van Dorn, Swanson, Elbogen, & Swartz, 2005), although there is some evidence to counter this finding (Chung, Chen, & Liu, 2001; Rivera, Rossetto, Pesqueira, & Otero, 2007). Thus, based on some direction from previous literature, we urge clinicians who work with individuals who self-injure to carefully examine any personal biases that they may hold towards individuals who self-injure during their work with these individuals.
Similarly, results from this research also may be helpful for clinicians to better understand and validate discriminatory experiences that clients may face, especially in social interactions. For example, results from the stigma literature suggest that accepting and owning one’s stigmatized identity (e.g., through disclosure) may decrease the negative effects of stigma (as discussed by Corrigan & Matthews, 2003). Thus, clinicians may encourage clients to consider disclosing or displaying their scarring as an important part of the recovery process. Indeed, from a public health perspective, such displays would increase contact and awareness of individuals who engage in NSSI and may contribute to anti-stigma efforts. Notably, however, there is some research that suggests self-injury disclosure among youth may lead to contagion (Hasking, Rees, Martin, & Quigley, 2015), an important caveat when contemplating the public health perspective. Moreover, based on the results from this study that demonstrated negative implicit and explicit bias and research suggesting that disclosure to peers may lead to reductions in perceived social support (Hasking et al., 2015), the authors caution that disclosure and display may be best conducted in a supportive environment. Helping clients who are navigating these relationships find safe ways to disclose a history of NSSI and provide education about NSSI (e.g., through information provided in outlets such as Self-Injury Outreach and Support, University of Guelph & McGill University, n.d.) may ultimately help individuals counter potential discriminatory or invalidating experiences.
Overall, this study provides evidence of implicit and explicit biases towards NSSI and highlights the need for further research to examine the downstream effects of these negative biases, such as self-stigma among those who self-injure. Results also underscore the need for future educational and contact-based interventions for the general public to mitigate the effects of stigma towards mental health and NSSI.
Acknowledgements
Taylor A. Burke was supported by a National Science Foundation Graduate Research Fellowship; Marilyn L. Piccirillo was supported by National Research Service Award F31 MH 115641-01 from the National Institute of Mental Health; Lauren Alloy was supported by NIMH grant MH101168. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Women’s desire for non-romantic interactions with someone with a history of NSSI did not significantly differ from men’s desire for such interactions (MD = −4.46, SD = 3.08, 95% CI [−10.52, 1.60]), t(232) = −1.45, p = .148, |d| = 0.24. In contrast, women’s desire for romantic or sexual interactions with someone with a history of NSSI significantly differed from men’s desire for such interactions (MD = −1.28, SD = 0.58, 95% CI [−2.42, −0.14]), t(232) = −2.20, p = .028, |d| = 0.37, such that men were significantly less likely to desire such interactions. Additionally, women’s desire for non-romantic interactions with someone with non-intentional disfigurement was significantly greater than men’s desire for such interactions (MD = −8.26, SD = 2.34, 95% CI [−12.87, −3.64]), t(232) = −3.53, p = .001, |d| = 0.57. Similarly, women’s desire for romantic or sexual interactions with someone with non-intentional disfigurement also was significantly greater than men’s desire for such interactions (MD = −2.37, SD = 0.56, 95% CI [−3.48, −1.26]), t(232) = −4.20, p < .001, |d| = 0.68.
References
- Angermeyer MC, & Matschinger H (2004). The stereotype of schizophrenia and its impact on discrimination against people with schizophrenia: Results from a representative survey in Germany. Schizophrenia Bulletin, 30, 1049–1061. 10.1093/oxfordjounrals.schbul.a007120 [DOI] [PubMed] [Google Scholar]
- Bachtelle SE, & Pepper CM (2015). The physical results of monsuicidal self-injury: The meaning behind the scars. Journal of Nervous and Mental Disease, 203, 927–933. 10.1097/NMD.0000000000000398 [DOI] [PubMed] [Google Scholar]
- Bessenoff GR, & Sherman JW (2000). Automatic and controlled components of prejudice toward fat people: Evaluation versus stereotype activation. Social Cognition, 18, 329–353. 10.1521/soco.2000.18.4.329 [DOI] [Google Scholar]
- Bonar EE, Hoffmann E, Rosenberg H, Kryszak E, Young KM, Ashrafioun L, … Bannon EE (2012). Development of a questionnaire to assess university students’ intentions to use behavioral alcohol-reduction strategies. Journal of American College Health, 60, 365–402. 10.1080/07448481.2012.663842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke TA, Hamilton JL, Cohen JN, Stange JP, & Alloy LB (2016). Identifying a physical indicator of suicide risk: Non-suicidal self-injury scars predict suicidal ideation and suicide attempts. Comprehensive Psychiatry, 65, 79–87. 10.1016/j.comppsych.2015.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke TA, Olino TM, & Alloy LB (2017). Initial psychometric validation of the non-suicidal self-injury scar cognition scale. Journal of Psychopathology and Behavioral Assessment, 39, 546–562. 10.1007/s10862-017-9595-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung KF, Chen EYH, & Liu CSM (2001). University students’ attitudes towards mental patients and psychiatric treatment. International Journal of Social Psychiatry, 47, 63–72. 10.1177/002076400104700206 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Edwards AB, Green A, Diwan SL, & Penn DL (2001). Prejudice, social distance, and familiarity with mental illness. Schizophrenia Bulletin, 27, 219–225. 10.1093/oxfordjournals.schbul.a006868 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, & Fong MWM (2014). Competing perspectives on erasing the stigma of illness: What says the dodo bird? Social Science & Medicine, 103, 110–117. 10.1016/j.socscimed.2013.05.027 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kerr A, & Knudsen L (2005). The stigma of mental illness: Explanatory models and methods for change. Applied and Preventive Psychology, 11, 179–190. 10.1016/j.appsy.2005.07.001 [DOI] [Google Scholar]
- Corrigan PW, & Matthews AK (2003). Stigma and disclosure: Implications for coming out of the closet. Journal of Mental Health, 12, 235–248. 10.1080/0963823031000118221 [DOI] [Google Scholar]
- Corrigan PW, Markowitz FE, Watson A, Rowan D, & Kubiak MA (2003). An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior, 44, 162–179. 10.2307/1519806 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, & Watson AC (2002). Understanding the impact of stigma on people with mental illness. World Psychiatry, 1, 16–20. [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N (2010). Implicit measures of social cognition: Common themes and unresolved questions. Journal of Psychology, 218, 54–57. 10.1027/0044-3409/a000009 [DOI] [Google Scholar]
- Dyer A, Hennrich L, Borgmann E, White AJ, & Alpers GW (2013). Body image and noticeable self-inflicted scars. Journal of Nervous and Mental Disease, 201, 1080–1084. 10.1097/NMD.000000000000057 [DOI] [PubMed] [Google Scholar]
- Dyer A, Mayer-Eckhard L, White AJ, & Alpers GW (2015). The role of scar origin in shaping men’s body image. American Journal of Men’s Health, 9, 115–123. 10.1177/1557988314531446 [DOI] [PubMed] [Google Scholar]
- Favazza A (1998). The coming of age of self-mutilation. Journal of Nervous & Mental Disease, 186, 259–268. 10.1097/00005053-199805000-00001 [DOI] [PubMed] [Google Scholar]
- Fliege H, Kocalevent R-D, Walter OB, Beck S, Gratz KL, Gutierrez PM, & Klapp BF (2006). Three assessment tools for deliberate self-harm and suicide behavior: Evaluation and psychopathological correlates. Journal of Psychosomatic Research, 61, 113–121. 10.1016/j.jpsychores.2005.10.006 [DOI] [PubMed] [Google Scholar]
- Garisch JA, & Wilson MS (2015). Prevalence, correlates, and prospective predictors of non-suicidal self-injury among New Zealand adolescents: Cross-sectional and longitudinal survey data. Child and Adolescent Psychiatry and Mental Health, 9, 1–11. http:/doi.org/10/1186/s13034-015-0055-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawronski B, & Bodenhausen GV (2006). Associative and propositional processes in evaluation: An integrative review of implicit and explicit attitude change. Psychological Bulletin, 132, 692–731. 10.1037/0033-2909.132.5.692 [DOI] [PubMed] [Google Scholar]
- Gratz KL (2001). Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment, 23, 253–263. 10.1023/A:1012779403943 [DOI] [Google Scholar]
- Gratz KL (2006). Risk factors for and functions of deliberate self-harm: An empirical and conceptual review. Clinical Psychology: Science and Practice, 10, 192–205. 10.1093/clipsy.bpg022 [DOI] [Google Scholar]
- Greenwald AG, Mcghee DE, & Schwartz JLK (1998). Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology, 74, 1464–1480. 10.1037/0022-3514.74.6.1464 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, & Banaji MR (2001). Understanding and using the Implicit Association Test: An Improved Scoring Algorithm. Attitudes and Social Cognition, 85, 197–216. 10.1037/0022-3514.85.2.197 [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman AT, Uhlmann EL, Banaji MR, Akalis S, Bargh J, … Walton G (2009). Understanding and using the implicit association test: III, Meta-analysis of predictive validity. Journal of Personality and Social Psychology, 97, 17–41. 10.1037/a0015575 [DOI] [PubMed] [Google Scholar]
- Hamza CA, Stewart SL, & Willoughby T (2012). Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clinical Psychology Review, 32, 482–495. 10.1016/j.cpr.2012.05.003 [DOI] [PubMed] [Google Scholar]
- Hasking P, Rees CS, Martin G, & Quigley J (2015). What happens when you tell someone you self-injure? The effects of disclosing NSSI to adults and peers. BMC Public Health, 15, 1039 10.1186/s12889-015-2383-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kleck RE, Hebl M, & Hull J (2000). Stigma: Social psychological perspectives New York, NY: Guilford Press. [Google Scholar]
- Hinshaw SP, & Stier A (2008). Stigma as related to mental disorders. Annual Review of Clinical Psychology, 4, 367–393. 10.1146/annurev.clinpsy.4.022007.141245 [DOI] [PubMed] [Google Scholar]
- Hipes C, Lucas J, Phelan JC, & White RC (2016). The stigma of mental illness in the labor market. Social Science Research, 56, 16–25. 10.1016/j.ssresearch.2015.12.001 [DOI] [PubMed] [Google Scholar]
- Hofmann W, Gawronski B, Gschwendner T, Le H, & Schmitt M (2005). A meta-analysis on the correlation between the Implicit Association Test and explicit self-report measures. Personality and Social Psychology Bulletin, 31, 1369–1385. 10.1177/0146167205275613 [DOI] [PubMed] [Google Scholar]
- Jorm AF, & Oh E (2009). Desire for social distance from people with mental disorders: A review. Australian and New Zealand Journal of Psychiatry, 43, 183–200. 10.1080/00048670802653349 [DOI] [PubMed] [Google Scholar]
- Karpinski A, & Steinman RB (2006). The single category implicit association test as a measure of implicit social cognition. Journal of Personality and Social Psychology, 91, 16–32. 10.1037/0022-3514.91.1.16 [DOI] [PubMed] [Google Scholar]
- Klonsky DE (2009). The functions of self-injury in young adults who cut themselves: Clarifying the evidence for affect-regulation. Psychiatry Research, 166, 260–268. 10.1016/j.psychres.2008.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurdi B, Seitchik AE, Axt J, Carroll T, Karapetyan A, Kaushik N, … Banaji MR (2018). Relationship between the implicit association test and intergroup behavior: A meta-analysis. American Psychologist 10.31234/osf.io/582gh [DOI] [PubMed]
- Lewis SP, & Mehrabkhani S (2016). Every scar tells a story: Insight into people’s self-injury scar experiences. Counseling Psychology Quarterly, 29, 296–310. 10.1080/09515070.2015.1088431 [DOI] [Google Scholar]
- Lincoln TM, Arens E, Berger C, & Rief W (2008). Can antistigma campaigns be improved? A test of the impact of biogenetic vs. psychosocial causal explanations on implicit and explicit attitudes to schizophrenia. Schizophrenia Bulletin, 34, 984–994. 10.1093/schbul/sbm131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Frank J, Wozniak JF, Kentucky JF, & College W (1987). The social rejection of former mental patients: Understanding why labels matter. American Journal of Sociology, 92, 1461–1500. 10.1086/228672 [DOI] [Google Scholar]
- Link BG, Phelan JC, Bresnahan M, Stueve A, & Pescosolido BA (1999). Public conceptions of mental illness: Labels, causes, dangerousness, and social distance. American Journal of Public Health, 89, 1328–1333. 10.2105/AJPH.89.9.1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Struening EL, Rahav M, Phelan JC, & Nuttbrock L (1997). On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior, 38, 177–190. 10.2307/2955424 [DOI] [PubMed] [Google Scholar]
- Lucas JW, & Phelan JC (2012). Stigma and status: The interrelation of two theoretical perspectives. Social Psychology Quarterly, 75, 310–333. 10.1177/0190272512459968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundh L-G, Wångby-Lundh M, & Bjärehed J (2011). Deliberate self-harm and psychological problems in young adolescents: Evidence of a bidirectional relationship in girls. Scandanavian Journal of Psychology, 52, 476–483. 10.1111/j.1467-9450.2011.00894.x [DOI] [PubMed] [Google Scholar]
- Maguire TO (1973). Semantic differential methodology for the structuring of attitudes. American Educational Research Journal American Education Research Journal, 10, 295–306. http://doi.org/0.2307/1161660 [Google Scholar]
- Markowitz FE (1998). The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. Journal of Health and Social Behavior, 39, 335–347. 10.2307/2676342 [DOI] [PubMed] [Google Scholar]
- Neumann R, Hülsenbeck K, & Seibt B (2004). Attitudes towards people with AIDS and avoidance behavior: Automatic and reflective bases of behavior. Journal of Experimental Social Psychology, 40, 543–550. 10.1016/j.jesp.2003.10.006 [DOI] [Google Scholar]
- Nock MK (2009). Why do people hurt themselves? New insights into the nature and functions of self-injury. Current Directions in Psychological Science, 18, 78–83. 10.1111/j.1467-8721.2009.01613.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK (2010). Self-Injury. Annual Review of Clinical Psychology, 6, 339–363. 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- Nock MK, & Banaji MR (2007). Assessment of self-injurious thoughts using a behavioral test. American Journal of Psychiatry, 1645, 820–823. 10.1176/appi.ajp.164.5.820 [DOI] [PubMed] [Google Scholar]
- Nordt C, Rossler W, & Lauber C (2005). Attitudes of mental health professionals toward people with schizophrenia and major depression. Schizophrenia Bulletin, 32, 709–714. 10.1093/schbul/sbj065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosek BA (2001). The Go/No-Go Association Task. Social Cognition, 19, 625–666. 10.1521/soco.19.6.625.20886 [DOI] [Google Scholar]
- Osgood CE, Suci GJ, & Tannenbaum PH (1957). The Measurement of Meaning Oxford, England: University of Illinois Press. [Google Scholar]
- Pettit JW, & Monteith LL (2011). Implicit and explicit stigmatizing attitudes and stereotypes about depression. Journal of Social and Clinical Psychology, 30, 484–505. 10.1521/jscp.2011.30.5.484 [DOI] [Google Scholar]
- Pinfold V, Toulmin H, Thornicroft G, Huxley P, Famer P, & Graham T (2003). Reducing psychiatric stigma and discrimination: Evaluation of educational interventions in UK secondary schools. British Journal of Psychiatry, 182, 342–346. 10.1192/bjp.182.4.342 [DOI] [PubMed] [Google Scholar]
- Psychological Software Tools Incorporated (2016). E-Prime, 3.0 Pittsburgh, PA: Retrieved from https://www.pstnet.com [Google Scholar]
- Rivera CS, Rossetto ADA, Pesqueira GS, & Otero MJE (2007). Attitudes of university students towards people with paranoid schizophrenia. Psychological Reports, 100, 325–332. 10.2466/pr0.100.1.325-332 [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, & Corrigan PW (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20, 529–539. 10.1016/j.eurpsy.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Rüsch N, Todd AR, Bodenhausen GV, & Corrigan PW (2010). Do people with mental illness deserve what they get? Links between meritocratic worldviews and implicit versus explicit stigma. European Archives of Psychiatry and Clinical Neuroscience, 260, 617–625. 10.1007/s00406-010-0111-4 [DOI] [PubMed] [Google Scholar]
- Schibeci RA (1982). Measuring student attitudes: Semantic differential or Likert instruments? Science Education, 66, 565–570. 10.1002/sce.3730660407 [DOI] [Google Scholar]
- Schulze B, Richter-Werling M, Matschinger H, & Angermeyer MC (2003). Crazy? So what! Effects of a school project on students’ attitudes towards people with schizophrenia. Acta Psychiatrica Scandinavica, 107, 142–150. 10.1034/j.1600-0447.2003.02444.x [DOI] [PubMed] [Google Scholar]
- Sriram N, & Greenwald AG (2009). The brief implicit association test. Experimental Psychology, 56, 283–294. 10.1027/1618-3169.56.4.283 [DOI] [PubMed] [Google Scholar]
- Stier A, & Hinshaw SP (2007). Explicit and implicit stigma against individuals with mental illness. Australian Psychologist, 42, 106–117. 10.1080/00050060701280599 [DOI] [Google Scholar]
- Stuart H, & Arboleda-Flórez J (2001). Community attitudes toward people with schizophrenia. The Canadian Journal of Psychiatry, 46, 245–252. 10.1177/070674370104600304 [DOI] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St. John NJ. (2014). Prevalence of nonsuicidal self-injury in nonclinical samples: Systematic review, meta-analysis and meta-regression. Suicide and Life-Threatening Behavior, 44, 273–303. 10.1111/sltb.12070 [DOI] [PubMed] [Google Scholar]
- Teachman BA, Wilson JG, & Komarovskaya I (2006). Implicit and explicit stigma of mental illness in diagnosed and healthy samples. Journal of Social and Clinical Psychology, 25, 75–95. http://doi.org/10.1521.jcsp.2006.25.1.75 [Google Scholar]
- Triandis HC (1977). Interpersonal Behavior Monterey, CA: Brooks/Cole. [Google Scholar]
- University of Guelph, & McGill University. Self-Injury Outreach and Support. (n.d.) Retrieved from http://sioutreach.org/
- Van Dorn RA, Swanson JW, Elbogen EB, & Swartz MS (2005). A comparison of stigmatizing attitudes toward persons with schizophrenia in four stakeholder groups: Perceived likelihood of violence and desire for social distance. Psychiatry, 68, 152–63. 10.1521/psyc.2005/68.2.152 [DOI] [PubMed] [Google Scholar]
- Wang X, Huang X, Jackson T, & Chen R (2012). Components of implicit stigma against mental illness among Chinese students. PloS ONE, 7, 1–6. 10.1371/journal.pone.0046016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White KM, Hogg MA, & Terry DJ (2002). Improving attitude–behavior correspondence through exposure to normative support from a salient ingroup. Basic and Applied Social Psychology, 24, 91–103. 10.1207/153248302753674604 [DOI] [Google Scholar]
- Wong J, Morrison AS, Heimberg RG, Goldin PR, & Gross JJ (2014). Implicit associations in social anxiety disorder: The effects of comorbid depression. Journal of Anxiety Disorders, 28, 537–546. 10.1016/j.janxdis.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- You J, Leung F, & Fu K (2012). Exploring the reciprocal relations between nonsuicidal self-injury, negative emotions and relationship problems in Chinese adolescents: A longitudinal cross-lag study. Journal of Abnormal Child Psychology, 40, 829–836. 10.1007/s10802-011-9597-0 [DOI] [PubMed] [Google Scholar]
- Ziegert JC, & Hanges PJ (2005). Employment discrimination: The role of implicit attitudes, motivation, and a climate for racial bias. Journal of Applied Psychology, 90, 553–562. 10.1037/0021-9010.90.3.553 [DOI] [PubMed] [Google Scholar]