Abstract
Background:
Globally, China is the largest country by population and contributes substantially to the burden of people who inject drugs (PWID). The aims of this study were to estimate the prevalence of HIV, hepatitis C virus (HCV) and hepatitis B virus (HBV) among PWID at the national and subnational level in China and examine characteristics of PWID.
Methods:
We undertook a systematic review of studies published from 2008–2017 on HIV, HCV, and HBV seroprevalence among PWID, and characteristics of PWID in Mainland China, Hong Kong, Macao and Taiwan. Meta-analyses were conducted to generate pooled prevalence estimates by province, region, and nationally.
Results:
Eighty-five papers were included. The pooled HIV, HCV antibody and HBV prevalence among PWID in China was 10.5% (95% confidence interval [95%CI]: 8.6%−12.5%), 71.6% (65.7%−77.6%) and 19.6% (13.7%−25.5%), respectively. In Mainland China, HIV prevalence was highest in the Southwest (14.4%, 10.5%−18.4%) and lowest in the North (1.3%, 0.4%−3.4%). Xinjiang Province had the highest HIV prevalence (42.6%, 35.5%−49.8%). HCV antibody prevalence was highest in the Southwest (77.7%, 69.9%−85.4%), followed by South (76.2%, 65.9%−86.4%). Sichuan had the highest HCV antibody prevalence (91.7%, 86.6%−95.3%), followed by Guangxi (86.1%, 81.8%−90.4%). HBsAg prevalence among PWID was highest in South (25.3%, 14.6%−36.0%), followed by Central (20.8%, 17.4%−24.1%). HBsAg prevalence ranged from 2.4% (0.6–5.9%) in Guizhou to 40.0% (33.7%−46.6%) in Shannxi Province. In China, women and young people accounted for 21.3% and 23.1% of PWID, respectively. It was estimated that 96.1% of PWID injected opioids mainly, and recent injecting risk and sexual risk was reported by 28.5% and 36.7%.
Conclusion:
There is a large burden of HIV, HCV and HBV prevalence among PWID in China, with considerable geographic variation. The disease burden of viral hepatitis is particularly high, implying that effective management should be integrated into harm reduction interventions among PWID in China.
Keywords: HIV, HCV, HBV, people who inject drugs, China, meta-analysis
Introduction
Injection drug use and related HIV infection and chronic viral hepatitis-mainly hepatitis B and C virus (HBV and HCV) - cause a substantial disease burden in China and globally (Degenhardt et al., 2016; Degenhardt et al., 2017). At the end of 2017, among the 2.55 million current registered drug users in China, 0.98 million reported the use of opiate drugs (Office of China National Narcotic Control Commission, 2018). It is estimated that35.9% of people who use opioids used them by injection (Office of National Narcotic Control Commission of China, 2015). Earlier studies and meta-analyses have identified large geographic variation in HIV and HCV among people who use drugs across regions and provinces in China (Bao and Liu, 2009; Wang et al., 2016; Zhang et al., 2013a). Yet, in recent decades China has experienced a huge change in disease burden and public health development (Zhou et al., 2016).The Chinese government has implemented harm reduction, including opioid substitution therapy (OST) and needle and syringe programs (NSP), throughout the country to control HIV infection in people who use drugs, especially in PWID (Wu et al., 2015). However, there are no recent detailed subregional estimates of HIV, nor estimates of HCV and HBV infection, among PWID at the national, region, or province-level. Updated estimates of HIV, HCV and HBV prevalence among PWID at these levels could provide detailed information for the allocation and assessment of harm reduction interventions and further understanding these geographical variations.
Some characteristics including age, gender, history of homelessness, arrest, incarceration, and sex work are associated with elevated risk of HIV, HCV, and HBV among PWID, as well as broader health harms in worldwide (Degenhardt et al., 2017). Estimating the prevalence and sociodemographic characteristics and risk factors for HIV, HBV and HCV infection among PWID in China will help to identify the extent to which there is variation in exposure to these risks within China. The aims of this study were to: i) estimate the current prevalence of HIV, HBV and HCV among PWID in China at provincial, regional, and national levels, and ii) describe sociodemographic characteristics and risk behaviours of Chinese PWID.
Methods
Search strategy and selection criteria
This study was a part of a global systematic review of peer-reviewed and grey literature to estimate the prevalence of HIV, HCV, and HBV among PWID (Degenhardt et al., 2017). In this review, PWID were defined as people who have recently (in the past 12 months) injected illicit drugs. The methods used were consistent with previous global reviews (Degenhardt et al., 2017) and in accordance with the PRISMA (Moher et al., 2009) and GATHER guideline (Stevens et al., 2016) (checklists presented in Appendix 1 and 2). The protocols were registered on PROSPERO (CRD42016052858 and CRD42016052853). The search strategy has been described in full in previous reviews (Degenhardt et al., 2017; Larney et al., 2017).
Briefly, three electronic peer-reviewed literature databases (MEDLINE, Embase, and PsycINFO) were searched using a comprehensive set of search terms developed in consultation with a specialist drug and alcohol librarian (Degenhardt et al., 2017) (see Appendix 3). To obtain recent data on infection prevalence, searches were limited to studies published since January 1, 2008, or since January 1, 2011 for hepatitis (determined based on the final year for identification of studies from previously published reviews(Degenhardt et al., 2010), to June, 2017. Previous systematic reviews were hand-searched for relevant papers or reports. Government reports and key documents by relevant international agencies, including the United Nations Office on Drugs and Crime (UNODC), World Health Organization, and Joint United Nations Programme on HIV and AIDS (UNAIDS) were searched to identify additional data. Additionally, requests for data were sent to international experts and agencies working in countries with limited published data. We did not limit the searches by language. Studies conducted in Mainland China, Hong Kong, Macao and Taiwan were selected for inclusion in this review.
Screening and extraction
An Endnote (version X.8) library was created to catalogue papers and reports and remove duplicates. Initial screening of title and abstract was done independently by one reviewer with a random 10% check by another, and discrepancies resolved through discussion and referral to a third author as necessary. Screened references were selected for full-text review if the title or abstract suggested that the document might contain relevant information. Full-text review was conducted by two independent authors.
Data from eligible studies were extracted by research assistants into a database in Microsoft Access 2016. Studies were screened based on pre-specified decisions rules and study quality assessment (see Appendix 4). The extracted data included study characteristics (country, province, study year, recruitment site); sample characteristics (sample source, sample size, age group, and percent male); estimated number or prevalence of HIV antibody, HCV antibody, HBV surface antigen (HBsAg); and characteristics and risk factors of PWID (gender, percent of young age [<=25 years], lifetime or recent homelessness or unstable housing, history of incarceration, injecting risk (defined mainly as receptive syringe sharing), sexual risk (defined mainly as unprotected sex with a casual sexual partner), recent sex work and reporting opioids as main drug injected). All data extraction was checked by one author independently. Discrepancies were resolved by discussion or through consultation with a third author.
Data analysis
Our approach was informed by methods used in earlier reviews (Degenhardt et al., 2010; Degenhardt et al., 2017). We extracted data for Mainland China, Hong Kong, Macao and Taiwan from the global dataset and coded the province and region of China according to the investigation location. In addition, two Chinese databases (CNKI and Wanfang) were searched. In accordance with methods used to develop the global estimates, estimates of a higher quality grade were selected over lower-grade estimates (Degenhardt et al., 2017) (Appendix 4). Where more than one estimate was available, random effects meta-analysis was used to pool the prevalence of HIV antibody, HCV antibody and HBsAg (and estimate the 95% confidence intervals) by using the metaprop command in Stata 14.Subgroup analysis was used to estimate prevalence at the provincial and regional levels. Pooled estimates were calculated for 1) Mainland China; 2) Hong Kong, Macao and Taiwan; and 3) Mainland China and Hong Kong, Macao and Taiwan combined. We also performed meta-analysis to estimate infection prevalence in the seven administrative regions in Mainland China (North, Northeast, Northwest, Central, East, South, and Southwest). Meta-analyses at the provincial level was performed where multiple estimates in a province were available.
All eligible estimates of characteristics and risk exposures of PWID were pooled by random effect meta-analysis, nationally and by region. The pooled estimates of the percentage of PWID who were young (age <25 years at the time of interview), had unstable housing or were homeless(current or past year), had a lifetime experience of police arrest, or had a lifetime history of incarceration, were reported. Risk behaviours relating to injecting drug use, recent sexual behaviour, engaging in sex work (current or past year among all PWID) and the main drug injected were pooled at the regional and national level.
Results
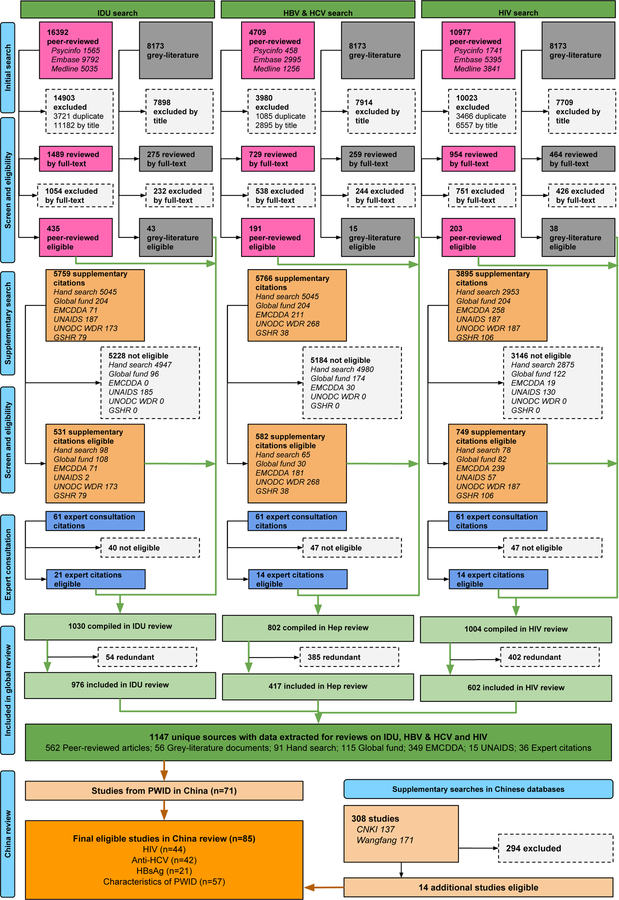
Figure 1 shows that 85 papers were eligible for this meta-analysis and Appendix 5 shows the study characteristics of these eligible papers. Among them, 44, 42 and 21 studies had HIV antibody, HCV antibody and HBsAg prevalence data among PWIDs in China, respectively. There was a limited number of studies for some characteristics (2 papers had data on homelessness or unstable housing among PWID, and 3 papers had data on history of incarceration among PWID).
Fig. 1.
Flowchart of study identification and inclusion.
Prevalence of HIV antibody, HCV antibody and HBsAg among PWID
The pooled HIV, HCV and HBsAg prevalence were 10.5% (95% confidence interval [95%CI]: 8.6%−12.5%), 71.6% (65.7–77.6%) and 19.6% (13.7%−25.5%) among PWID in China (Table 1). In Mainland China, the HIV, HCV and HBsAg prevalence were 10.4% (8.3%−12.4%), 70.8% (64.8%−76.8%) and 20.2% (14.2%−26.2%), respectively, and 12.4% (8.1%−16.8%), 86.8% (79.6%−93.9%) and 8.1% (3.3%−15.9%) among PWID for Hong Kong, Macao and Taiwan pooled.
Table 1.
Estimate of the prevalence of HIV, HCV antibody and HBsAg among PWID nationally and by region and province in China
| Province | HIV (95% UI) | HCV antibody (95% UI) | HBsAg (95% UI) | |||
|---|---|---|---|---|---|---|
| No. studies | Prevalence | No. studies | Prevalence | No. studies | Prevalence | |
| Mainland China | 40* | 10.4 (8.3–12.4) | 39* | 70.8 (64.8–76.8) | 20 | 20.2 (14.1–26.2) |
| North | 1 | 1.3 (0.4–3.4) | 1 | 58.7 (52.9–64.3) | 1 | 15.9 (12.8–19.4) |
| Beijing | 1 | 1.3 (0.4–3.4) | 1 | 58.7 (52.9–64.3) | 1 | 15.9 (12.8–19.4) |
| Hebei | 0 | - | 0 | - | 0 | - |
| Shannxi | 0 | - | 0 | - | 0 | - |
| Inner Mongolia | 0 | - | 0 | - | 0 | - |
| Northeast | 0 | - | 0 | - | 0 | - |
| Heilongjiang | 0 | - | 0 | - | 0 | - |
| Liaoning | 0 | - | 0 | - | 0 | - |
| Jilin | 0 | - | 0 | - | 0 | - |
| Northwest | 4 | 10.9 (2.8–19.0) | 4 | 67.1 (44.5–89.7) | 3 | 18.0 (2.6–38.7) |
| Gansu | 2 | 1.7 (0.3–3.1) | 2 | 69.5 (65.3–73.8) | 1 | 10.3 (5.1–18.1) |
| Qinghai | 1 | 2.0 (0.6–5.1) | 1 | 83.3 (77.3–88.2) | 0 | - |
| Shannxi | 0 | - | 0 | - | 1 | 40.0 (33.7–46.6) |
| Xinjiang | 1 | 42.6 (35.5–49.8) | 1 | 48.7 (41.5–56.0) | 1 | 4.1 (1.8–7.9) |
| Ningxia | 0 | - | 0 | - | 0 | - |
| Central | 3 | 10.0 (7.5–12.5) | 4 | 53.7 (19.2–88.2) | 3 | 20.8 (17.4–24.1) |
| Henan | 0 | - | 1 | 12.3 (11.0–13.7) | 0 | - |
| Hubei | 0 | - | 0 | - | 0 | - |
| Hunan | 2 | 10.0 (7.5–12.5) | 3 | 67.5 (42.6–92.4) | 3 | 20.8 (17.4–24.1) |
| East | 4 | 2.5 (0.5–4.6) | 6 | 64.4 (50.0–78.8) | 3 | 18.4 (0–37.0) |
| Anhui | 0 | - | 0 | - | 0 | - |
| Shandong | 0 | - | 0 | - | 0 | - |
| Shanghai | 0 | - | 1 | 63.4 (50.5–76.2) | 0 | - |
| Zhejiang | 1 | 1.3 (0.2–4.5) | 1 | 64.2 (56.2–71.6) | 1 | 34.6 (27.2–42.5) |
| Jiangsu | 1 | 1.2 (0.4–2.6) | 2 | 64.5 (39.2–89.8) | 0 | - |
| Jiangxi | 1 | 11.1 (3.7–24.1) | 1 | 64.4 (48.8–78.1) | 1 | 18.6 (13.0–25.3) |
| Fujian | 1 | 4.1 (2.8–5.8) | 1 | 67.8 (64.2–71.1) | 1 | 2.9 (1.8–4.3) |
| South | 8 | 6.6 (4.6–8.5) | 9 | 76.2 (65.9–86.4) | 5 | 25.3 (14.6–36.0) |
| Guangxi | 5 | 12.2 (6.7–17.6) | 3 | 86.1 (81.8–90.4) | 1 | 13.8 (7.6–22.5) |
| Guangdong | 8 | 4.2 (2.3–6.0) | 6 | 72.8 (60.7–84.9) | 4 | 25.3 (14.6–36.0) |
| Hainan | 0 | - | 0 | - | 0 | - |
| Southwest | 15 | 14.4 (10.5–18.4) | 13 | 77.7 (69.9–85.4) | 5 | 18.3 (5.1–31.5) |
| Yunnan | 5 | 21.1 (16.7–25.5) | 3 | 63.0 (42.6–83.3) | 2 | 21.3 (18.8–23.9) |
| Sichuan | 7 | 10.5 (5.4–15.5) | 6 | 91.7 (86.6–95.3) | 2 | 15.2 (11.7–18.7) |
| Guizhou | 3 | 8.9 (0.8–17.1) | 3 | 79.5 (66.6–92.3) | 1 | 2.4 (0.6–5.9) |
| Chongqing | 0 | - | 1 | 84.4 (81.6–87.0) | 0 | - |
| Tibet | 0 | - | 0 | - | 0 | - |
| Hong Kong, Macao, and Taiwan | 4 | 12.4 (8.1–16.8) | 3 | 86.8 (79.6–93.9) | 1 | 8.1 (3.3–15.9) |
| Hong Kong | 0 | - | 1 | 81.7 (78.4–84.6) | 0 | - |
| Macao | 0 | - | 0 | - | 0 | - |
| Taiwan | 4 | 12.4 (8.1–16.8) | 2 | 91.0 (89.5–92.4) | 1 | 8.1 (3.3–15.9) |
| Mainland China and HK, Macao, Taiwan | 44 | 10.5 (8.6–12.5) | 42 | 71.6 (65.7–77.6) | 21 | 19.6 (13.7–25.5) |
: Including one additional study with national-level data.
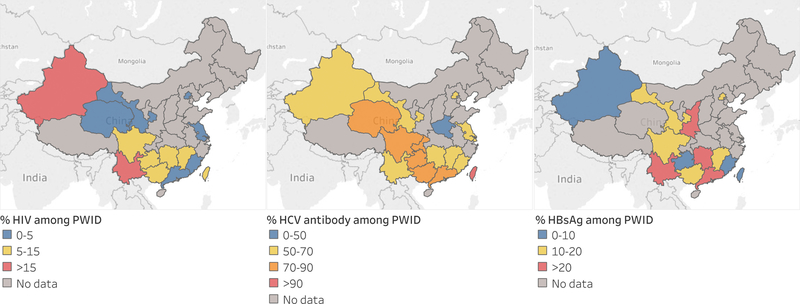
In Mainland China, HIV prevalence were highest in the Southwest (14.4%, 10.5%−18.4%), and lowest in the North (1.3%, 0.4%−3.4%). Figure 2 shows the provincial level prevalence of HIV, HCV and HBsAg among PWID in China. Among the fourteen provinces with data on HIV antibody prevalence, Xinjiang Province had the highest HIV prevalence (42.6%, 35.5%−49.8%), followed Yunnan (21.1%, 16.7%−25.5%), Guangxi (12.2%, 6.7%−17.6%). The prevalence of HCV was highest in the Southwest (77.7%,69.9%−85.4%), followed by South (76.2%,65.9%−86.4%). At the province level, Sichuan had highest HCV antibody positive prevalence (91.7%,86.6%−95.3%), followed by Guangxi (86.1%, 81.8%−90.4%). HBsAg prevalence among PWID was highest in South (25.3%, 14.6%−36.0%), followed by Central (20.8%, 17.4%−24.1%). There were fewer provincial estimates of HBsAg data among PWID in China with the estimates also showing considerable geographic variation from 40.0% (33.7%−46.6%) in Shannxi Province to 2.4% (0.6%−5.9%) in Guizhou.
Figure 2.
The pooled prevalence of HIV, anti-HCV and HBsAg among PWID in China ( 2008–2017)
Sociodemographic characteristics and risk factorsamong PWID
Table 2 shows the sociodemographic characteristics and risk exposures of PWID in China. Women and young people accounted for 21.3% (17.9%−24.7%) and 23.1% (17.5%−28.7%) of PWID across Mainland China, Hong Kong, Macao and Taiwan, respectively. The East region had the highest percentage of women who inject drugs (38.1%, 16.5%−59.8%), while the Central region (8.3%, 6.7%−10.1%), Northeast region (11.0%, 9.2%−12.8%), and Hong Kong, Macao, and Taiwan (14.2%, 13.2%−15.1%) had lower percentages of women. The East (10.2%, 8.7%−12.0%) and South (8.3%, 7.3%−9.3%) regions had lower percentage of young PWID than the Southwest region (24.1%, 16.8%−31.4%). The percentage of PWID reporting recent homelessness or unstable housing in Mainland China was 8.9% (6.3%−12.2%) based on data only from the Southwest region, which was higher than the 0.7% (0.3%−1.3%) observed in Taiwan. History of incarceration was higher in Taiwan at 89.5% (87.7%−91.2%) than the Southwest region at 78.4% (73.8%−82.5%).
Table 2:
Sociodemographic and risk characteristics for people who inject drugs in China
| Characteristics | Women | Young people* | Recent homelessness or unstable housing | History of incarceration | ||||
|---|---|---|---|---|---|---|---|---|
| No. studies | Percentage | No. studies | Percentage | No. studies | Percentage | No. studies | Percentage | |
| Mainland China | 34 | 22.9 (18.9–27.0) | 12 | 23.1 (17.5–28.7) | 1 | 8.9 (6.3–12.2) | 1 | 78.4 (73.8–82.5) |
| North | 1 | 24.0 (19.8–28.8) | 0 | - | 0 | - | 0 | - |
| Northeast | 0 | -- | 0 | - | 0 | - | 0 | - |
| Northwest | 2 | 11.0 (9.2–12.8) | 0 | - | 0 | - | 0 | - |
| Central | 1 | 8.3 (6.7–10.1) | 0 | - | 0 | - | 0 | - |
| East | 4 | 38.1 (16.5–59.8) | 1 | 10.2 (8.7–12.0) | 0 | - | 0 | - |
| South | 7 | 18.8 (13.3–24.2) | 2 | 8.3 (7.3–9.3) | 0 | - | 0 | - |
| Southwest | 15 | 20.7 (16.—25.0) | 9 | 24.1 (16.8–31.4) | 1 | 8.9 (6.4–12.2) | 1 | 78.4 (73.8–82.5) |
| Hong Kong, Macao, and Taiwan | 8 | 14.2 (13.2–15.1) | 0 | - | 1 | 0.7 (0.3–1.3) | 2 | 89.5 (87.7–91.2) |
| Hong Kong | 1 | 15.9 (13.0–19.2) | 0 | - | 0 | - | 0 | - |
| Macao | 0 | - | 0 | - | 0 | - | 0 | - |
| Taiwan | 7 | 13.8 (12.8–14.9) | 0 | - | 1 | 0.7 (0.3–1.3) | 2 | 89.5 (87.7–91.2) |
| Total | 42 | 21.3 (17.9–24.7) | 12 | 23.1 (17.5–28.7) | 2 | 0.9 (0.5–1.3) | 3 | 86.4 (79.2–93.6) |
| Characteristics | Recent injecting risk† | Recent sexual risk‡ | Recent sex work | Main drug injected opioid | ||||
| No. studies | Percentage | No. studies | Percentage | No. studies | Percentage | No. studies | Percentage | |
| Mainland China | 39# | 27.7 (221.7–33.6) | 19 | 36.6 (28.0–45.2) | 6 | 21.8 (8.3–35.3) | 4 | 94.0 (90.7–97.3) |
| North | 1 | 26.0 (21.1–31.4) | 1 | 77.0 (71.8–81.6) | 0 | - | 0 | - |
| Northeast | 0 | - | 0 | - | 0 | - | 0 | - |
| Northwest | 3 | 30.0 (12.7–46.6) | 2 | 33.0 (30.4–35.6) | 1 | 1.7 (0.9–3.0) | 0 | - |
| Central | 2 | 2.8 (1.2–4.3) | 0 | - | 0 | - | 0 | - |
| East | 6 | 40.2 (15.4–65.1) | 2 | 71.9 (69.1–74.7) | 2 | 24.6 (22.4–26.8) | 2 | 99.4 (98.9–99.9) |
| South | 7 | 35.3 (15.9–54.8) | 5 | 49.4 (34.1–64.6) | 0 | - | 0 | - |
| Southwest | 16 | 21.8 (17.8–30.9) | 9 | 25.7 (20.4–31.0) | 3 | 26.6 (12.7–40.6) | 2 | 99.0 (98.2–99.7) |
| Hong Kong, Macao, Taiwan | 5 | 28.8 (13.3–44.3) | 1 | 38.9 (34.9–43.0) | 0 | - | 1 | 99.5 (90.7–97.3) |
| Hong Kong | 1 | 61.2 (57.1–65.2) | 0 | - | 0 | - | 1 | 99.5 (90.7–97.3) |
| Macao | 0 | - | 0 | - | 0 | - | 0 | - |
| Taiwan | 4 | 28.8 (13.3–44.3) | 1 | 38.9 (34.9–43.0) | 0 | - | 0 | - |
| Total | 44 | 28.5 (22.9–34.1) | 20 | 36.7 (28.0–45.1) | 5 | 21.2 (6.3–36.0) | 5 | 96.1 (93.8–98.4) |
Young people who inject drugs were defined as younger than 25 years where possible.
Including 3 studies with national-level data.
Recent injecting risk was defined as receptive needle-syringe sharing within the past year (using a needle-syringe after someone else
Recent sexual risk was defined as unprotected sex with a non-regular (casual) sexual partner.
Results on risk characteristics (Table 2) showed that 28.5% (22.9%−34.1%), 36.7% (28.0%−45.1%) and 21.2% (6.3%−36.0%) of PWID had a history of recent injecting risk, sexual risk and sex work, respectively. The prevalence of recent injecting risk was lowest in the Central region (2.8%, 1.2%−4.3%) and highest in Hong Kong (61.2%, 57.1%−65.2%). The prevalence of recent sexual risk was very high in a study from the East region at 83.9% (80.5%−86.9%). The prevalence of recent sex work was reported as low in a study from the Northwest region at 1.7% (0.9%−3.0%). The majority of PWID primarily inject opioids (96.1%, 93.8%−98.4%); this was similar across different regions.
Discussion
China is the largest country by population in the world and contributes substantially to the global burden of injecting drug use and HIV, HCV and HBV among PWID. This updated estimation showed that approximately one in ten PWID in China are living with HIV, three in four PWID have been infected with HCV and one in five have current HBV infection, with substantial regional and provincial level variations in the prevalence of these blood borne viruses. The Southeast area of China had the highest prevalence of HIV infection, Taiwan had the highest prevalence of HCV infection and Mainland China has a consistently higher prevalence of HBV infection than other regions. These findings indicate that HIV and viral hepatitis are important harms among people who inject drugs in China, demonstrating the importance of expanding effective prevention and management strategies, particularly in regions with a higher burden. Another key finding of this paper is the major data gaps that exist in some of the provinces, making it difficult to estimate the burden of infections in these regions, especially for HBV infection. Given the considerable burden of these infections in China, it is critical to focus efforts to improve these data.
This analysis extends our knowledge of key blood-borne infections among people who inject drugs in China, providing estimates of HIV and HCV prevalence in the areas of Hong Kong, Macao and Taiwan, and the first pooled prevalence of HBsAg among PWID in China. This adds to a previous meta-analysis assessing HCV and HCV among populations of people who use drugs, including injecting drug use (Degenhardt et al., 2017). We observed that HIV prevalence was comparable between Mainland and Hong Kong, Macao and Taiwan. However, HCV antibody prevalence was higher in Taiwan (91.0%) than Mainland China (70.8%) and Hong Kong (81.7%). HBsAg was higher in mainland China (20.1%) compared to Taiwan (8.1%). The different patterns of the HCV and HBV infections in these regions indicate that there should be different prioritization for the targeting of interventions among PWID in Mainland China and Hong Kong, Macao and Taiwan. In Mainland China, HIV prevention and control among PWID has been the main emphasis of harm reduction programs (Ma Y, 1990; Zhang et al., 2013a). In the current study, the prevalence of HIV infection among PWID in Mainland China was lower than the estimate observed in a systematic review conducted in 2009 (12.6%; 12.3%−12.9%) (Bao and Liu, 2009). Further, our updated HCV prevalence estimate was 70.8% (65.1%−76.5%), which is higher than the estimate of 67.0% (66.6%−67.4%) from ten years ago (Bao and Liu, 2009). Further work is needed to enhance interventions for HIV and HCV prevention and to continue to improve the availability of data on the burden of HCV, HIV and HBV to inform how best to target these interventions in China.
In mainland China, the Southeast and Northwest regions had the highest HIV and HCV prevalence among PWID, consistent with previous meta-analysis and surveillance data in China (Zhang et al., 2013a). The Southwest and Northwest of China were the regions most affected by HIV, with substantially greater HIV prevalence in the provinces of Yunnan and Xinjiang, locations close to the Golden Triangle and the Golden Crescent areas (Zhang et al., 2013a). Among PWID in China, HIV and HCV infection are highest in the Southwest, especially in Sichuan and Yunnan Province. Since 2004, methadone maintenance treatment (MMT) programs, the most common available form of OST in China, have become the major form of harm reduction in China. However, a decrease in HIV infection in some high-risk areas has been attributed to the scale-up of OST and NSP (Wu et al., 2015). In Yunnan, HIV prevalence declined by about a half from 52.5% estimated in the previous review to 21.1% in this review. However, PWIDs in Xinjiang still had a high prevalence of HIV infection. Moreover, the HCV prevalence in Yunnan Province did not decrease considerably. These findings indicated that the burden of HIV and HCV infections is still high in some areas, and the scale-up of interventions to prevent and treat HIV and HCV among PWID remains a crucial priority to address the HIV and HCV epidemics.
Our findings showed that there is substantial HBsAg burden among PWID in Mainland China, higher than that in the 15–59 year-old general population (9%) in China (Liang et al., 2013). We demonstrated that large variation existed for HBsAg prevalence by province (range: 2.4% in Guizhou to 40.0% in Shannxi). However, the high HBsAg prevalence (40%) in Shannxi came from a small PWID sample (n=235) and only 11.7% of drug users had a clear history of hepatitis B vaccination (Wu et al., 2014). These findings indicated that the prevention and control of hepatitis B represent a serious challenge among PWID in Mainland China. Hepatitis B vaccination and other interventions are encouraged in this population. However, there were only twelve provinces with data on HBV, and about half of the provinces had no corresponding HBsAg data among PWID in this analysis. Future investigations with larger sample sizes and greater geographic coverage are needed to more robustly estimate the burden of HBV infection among PWID. Given that good understanding all three epidemics will be critical for global efforts to address these infections and the need of the development of drug policy and the corresponding infectious disease control in China, more investigation or monitoring are needed in the regions without data.
This is the first study to present pooled estimates of the sociodemographic characteristics and risk factors of PWID in China. The findings showed that 96.1% of PWID mainly injected opioids in China. Although we have seen synthetic drug use supersede opioids as the most common drug in China, our findings demonstrate that PWID in China still prefer injecting opioids; however, this is likely due to synthetic drugs more commonly being inhaled or smoked (Bao et al., 2012; Office of National Narcotic Control Commission of China, 2015). Future studies need to monitor and examine the risk of infection among PWID who switch to or engage in polydrug use of synthetic drugs, with the rising synthetic drug market in China.
There was a high prevalence of history of incarceration, recent injecting risk behaviours and recent sexual risk behaviours reported in PWID. The highest proportion of female PWID was found in East China and the highest percentage of young people among PWID was found in Southwest China. It is important to pay attention to and monitor trends of women and young people in relation to injecting drug use, as these groups can be particularly vulnerable to BBV and may experience barriers in accessing existing harm reduction services. the region with high proportion of the vulnerable characteristics for prevention and control of injection drug use. Recent exposure to sexual risk factors was associated with increased risk of HIV and HCV infection among PWIDs (Zhuang et al., 2012b). In our review, we found that percentage of PWID who reported recent sexual risk was high across regions of China (36.7%), especially in East North (77.0%). In addition, we found a high percentage of PWID involved in recent sex work in East and Southwest China. Clearly, implementing interventions to reduce sexual risk factors is important for PWID.
This review had strict inclusion and exclusion criteria as in previous large-scale reviews (Degenhardt et al., 2017), and we searched the Chinese database too according to the same criteria. This helped to ensure that only higher-quality data were included in the analysis, but also meant that limited data were available for some geographical areas, especially in relation to HBsAg prevalence. The limited geographic coverage and the limited sample size population for characteristics and risk factors were also challenges in this analysis. Moreover, this analysis did not capture all estimates of demographic characteristics and risk factors although we undertook a comprehensive search without language limitations. Finally, the tests used to determine HIV, HCV and HBsAg infections varied in the included studies, and the quality of tests used may influence the results of this review; however, we were unable to conduct additional subgroup analysis by quality of tests in this meta-analysis because of lack of data.
Conclusions
There is a large burden of HIV, HCV and HBV among PWID in China, with considerable geographic variation. A substantial proportion of PWID reported a history of incarceration and risk behaviours for infectious diseases, including injecting and sexual risks. The disease burden of viral hepatitis is particularly high among PWID and effective management for viral hepatitis should be integrated into harm reduction programmes among PWID in China.
Supplementary Material
Acknowledgments
The Australian National Drug and Alcohol Research Centre, UNSW Sydney and the State Scholarship Fund of China, provided some funding towards the costs of this systematic review. YB is supported by the State Scholarship Fund of China (no. 201706015001), LD is supported by an Australian National Health and Medical Research Council (NHMRC) Principal Research Fellowship. AP is supported by an NHMRC Early Career Fellowship. SL is supported by an NHMRC Career Development Fellowship (1140938). JL acknowledges funding from the Bill & Melinda Gates Foundation. The Kirby Institute is funded by the Australian Government Department of Health and Ageing. We thank the research assistants who assisted with searches for and extraction of data from the eligible papers in this review.
Funding Australian National Drug and Alcohol Research Centre, Australian National Health and Medical Research Council, Open Society Foundation, World Health Organization, the Global Fund, and UNAIDS, and the State Scholarship Fund of China.
References
- Bao Y, Du C, Lu H, Lian Z, Qiu Y, Mu Y, et al. (2012). The investigation of HIV and HCV infection and risk factors among opiate drug users in Beijing, China. American Journal of Drug & Alcohol Abuse 38, 140–145. [DOI] [PubMed] [Google Scholar]
- Bao YP, Liu ZM (2009). Systematic review of HIV and HCV infection among drug users in China. International journal of STD & AIDS 20, 399–405. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Charlson F, Stanaway J, Larney S, Alexander LT, Hickman M, et al. (2016). Estimating the burden of disease attributable to injecting drug use as a risk factor for HIV, hepatitis C, and hepatitis B: findings from the Global Burden of Disease Study 2013. The Lancet Infectious diseases 16, 1385–1398. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Mathers B, Vickerman P, Rhodes T, Latkin C, Hickman M (2010). Prevention of HIV infection for people who inject drugs: why individual, structural, and combination approaches are needed. Lancet (London, England) 376, 285–301. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. (2017). Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. The Lancet Global health 5, e1192–e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Peacock A, Leung J, Colledge S, Hickman M, Vickerman P, et al. (2017). Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. The Lancet Global health 5, e1208–e1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang X, Bi S, Yang W, Wang L, Cui G, Cui F, et al. (2013). Reprint of: Epidemiological serosurvey of Hepatitis B in China--declining HBV prevalence due to Hepatitis B vaccination. Vaccine 31 Suppl 9, J21–28. [DOI] [PubMed] [Google Scholar]
- Ma Y LZ, Zhang KX. (1990). Identification of HIV infection among drug users in China. Chin J Epidemiol 11, 184–185. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine 151, 264–269, w264. [DOI] [PubMed] [Google Scholar]
- Office of China National Narcotic Control Commission (2018) Annual Report on Drug Control in China 2017 Beijing: Office of China National Narcotic Control Commission. [Google Scholar]
- Office of National Narcotic Control Commission of China (2015) Annual report on drug control in China 2014 Beijing. [Google Scholar]
- Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. (2016). Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet (London, England) 388, e19–e23. [DOI] [PubMed] [Google Scholar]
- Wang C, Shi CX, Rou K, Zhao Y, Cao X, Luo W, et al. (2016). Baseline HCV Antibody Prevalence and Risk Factors among Drug Users in China’s National Methadone Maintenance Treatment Program. PloS one 11, e0147922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Guo W, Li D, Ding Z, McGoogan JM, Wang N, et al. (2015). HIV epidemic among drug users in China: 1995–2011. Addiction (Abingdon, England) 110 Suppl 1, 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q, Zu J, Wei X, You L, Kou L, Li H, et al. (2014). [Survey of Hepatitis B infection and vaccination status among drug users in Xi’an]. Zhonghua yu fang yi xue za zhi [Chinese journal of preventive medicine] 48, 862–866. [PubMed] [Google Scholar]
- Wu Z, Wang Y, Detels R, Bulterys M (2015). Towards ending HIV/AIDS among drug users in China. Addiction (Abingdon, England) 110 Suppl 1, 1–3. [DOI] [PubMed] [Google Scholar]
- Zhang L, Chow EP, Jing J, Zhuang X, Li X, He M, et al. (2013a). HIV prevalence in China: integration of surveillance data and a systematic review. The Lancet Infectious diseases 13, 955–963. [DOI] [PubMed] [Google Scholar]
- Zhang L, Zhang D, Chen W, Zou X, Ling L (2013b). High prevalence of HIV, HCV and tuberculosis and associated risk behaviours among new entrants of methadone maintenance treatment clinics in Guangdong Province, China. PLoS ONE [Electronic Resource] 8, e76931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. (2016). Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 387, 251–272. [DOI] [PubMed] [Google Scholar]
- Zhuang X, Liang Y, Chow EP, Wang Y, Wilson DP, Zhang L (2012a). HIV and HCV prevalence among entrants to methadone maintenance treatment clinics in China: a systematic review and meta-analysis. BMC infectious diseases 12, 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang X, Wang Y, Chow EP, Liang Y, Wilson DP, Zhang L (2012b). Risk factors associated with HIV/HCV infection among entrants in methadone maintenance treatment clinics in China: a systematic review and meta-analysis. Drug and alcohol dependence 126, 286–295. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.