Abstract
Background:
Environmental phenols, compounds used widely in personal care and consumer products, are known endocrine disruptors. Few epidemiologic studies have examined the association of phenol biomarkers with breast cancer incidence and, to our knowledge, none have considered associations with mortality following breast cancer. We examined seven urinary phenol biomarkers in association with breast cancer incidence and subsequent mortality, and examined effect measure modification by body mass index (BMI).
Methods:
Participants included 711 women with breast cancer and 598 women without breast cancer who were interviewed for the population-based Long Island Breast Cancer Study Project. Among women with breast cancer, phenol biomarkers were quantified in spot urine samples collected on average within three months of a first diagnosis of primary in situ or invasive breast cancer in 1996-1997. Women with breast cancer were monitored for vital status using the National Death Index. After a median follow-up of 17.6 years, we identified 271 deaths, including 98 deaths from breast cancer. We examined creatinine-corrected phenol concentrations and the sum of parabens (Σparabens) in association with breast cancer incidence using logistic regression to estimate odds ratios (ORs) and 95% confidence intervals (CIs), and with mortality using Cox regression to estimate hazard ratios (HRs) and 95% CIs. We evaluated multiplicative effect measure modification using cross-product terms in nested models.
Results:
The highest (vs lowest) quintiles of urinary methylparaben, propylparaben, and Σparabens were associated with risk of breast cancer with ORs ranging from 1.31-1.50. Methylparaben, propylparaben, and Σparabens were also associated with all-cause mortality HRs ranging from 0.68-0.77. Associations for breast cancer incidence were more pronounced among women with BMI<25.0 kg/m2 than among women with BMI≥25.0 kg/m2; however, associations for mortality were more pronounced among women with BMI≥25 kg/m2 than among women with BMI<25 kg/m2.
Conclusions:
Select parabens may have differential associations with risk of developing breast cancer and mortality following breast cancer.
Keywords: Breast cancer, environmental phenols, incidence, mortality, personal care products, parabens, BPA, triclosan
Introduction
Environmental and behavioral factors may play a role in the development of breast cancer,1 the most frequently diagnosed cancer and the second-leading cause of cancer-related death among women in the United States (US).2 Epidemiologic studies of environmental chemical exposures and breast cancer risk or mortality following breast cancer have focused primarily on associations with legacy persistent organic pollutants (POPs) and polycyclic aromatic hydrocarbons.3-9 The role of other chemicals, including environmental phenols, on breast cancer risk and prognosis has received little scientific attention.10 Although less environmentally and biologically persistent than the POPs,11,12 as estrogen mimics, some environmental phenols may initiate or promote breast carcinogenesis.13,14
Many phenols are naturally occurring byproducts of plants and microorganisms; however, others are industrially synthesized for use in personal care and consumer products and pharmaceuticals.15,16 The chemical 2,5-dichlorophenol, for example, is a metabolite of p-dichlorobenzene, a putative carcinogen and potent allergen used in mothballs and bathroom deodorizers.17,18 Other synthetic chemicals in this class include bisphenol A (BPA), which is used in the production of plastics and food and beverage storage containers,19 benzophenone-3, an ultraviolet (UV) filter and the active ingredient in many sunscreen lotions and cosmetics,20 triclosan, a broad spectrum antibacterial agent added to soaps, toothpastes, and underarm deodorants,21 and parabens, a group of alkyl esters of p-hydroxybenzoic acid, which are used as preservatives in cosmetics and topical pharmaceutical preparations.13,22
Because environmental phenols or their precursors are commonly found in a wide range of conventional personal care and consumer products and may be found in “alternative” products that do not list specific chemical ingredients on the label,23 human exposure may occur via oral, dermal, and inhalation routes,14 with dermal exposures of greatest concern due to prolonged exposure and potential for migration into the bloodstream.22 In the body, environmental phenols are quickly conjugated and excreted in urine; however, habitual use of personal care products results in continuous exposure. Quantification of environmental phenols in urine rather than in blood in which phenol concentrations may be ~50 times lower,24 is therefore the preferred and most common and reliable method for assessing exposure in biomonitoring and epidemiologic studies,25,26 which readily detect these chemical biomarkers.27-32 Furthermore, some phenols are detected in human breast milk,25,30,33-36 albeit at lower concentrations, suggesting their passage through breast epithelial cells.37
Few epidemiologic studies have examined environmental phenol sources of exposure or phenol biomarkers and breast cancer incidence38-42 and, to our knowledge, no studies have examined whether urinary phenol biomarkers are associated with mortality following breast cancer. Herein, we examined the associations between seven select urinary environmental phenols and breast cancer incidence and subsequent mortality among participants in a population-based study of breast cancer conducted in the USA.
Methods
We used the case-control43 and follow-up44 resources from the Long Island Breast Cancer Study Project (LIBCSP), a population-based study of breast cancer which included 1,508 women with a first diagnosis of in situ or invasive breast cancer between August 1, 1996 and July 31, 1997 and 1,556 women without breast cancer (see Table 1 for descriptive characteristics of the LIBCSP participants). Institutional Review Board approval was obtained from all participating institutions and written informed consent was obtained prior to study participation. The analysis of blinded specimens by the Centers for Disease Control and Prevention (CDC) laboratory was determined not to constitute any engagement in human subjects’ research.
Table 1.
Distribution of select characteristics among the LIBCSP women by breast cancer status, comparing the ancillary study sample with available values of urinary concentrations of creatinine-corrected phenols and the parent-study sample.
| Women with Breast Cancer |
Women without Breast Cancer |
|||
|---|---|---|---|---|
| Phenols Sample (n=711) |
Parent Study Sample (n=1,508) |
Phenols Sample (n=598) |
Parent Study Sample (n=1,556) |
|
| Age at reference (years) | ||||
| <50 | 196 (27.6%) | 407 (27.0%) | 197 (32.9%) | 499 (32.1%) |
| 50–64 | 259 (36.4%) | 582 (38.6%) | 250 (41.8%) | 617 (39.7%) |
| ≥65 | 256 (36.0%) | 519 (34.4%) | 151 (25.2%) | 440 (28.3%) |
| Income | ||||
| <$24,999 | 154 (21.7%) | 286 (19.0%) | 104 (17.4%) | 295 (19.0%) |
| $25,000–$49,999 | 227 (32.0%) | 488 (32.4%) | 172 (28.8%) | 475 (30.6%) |
| ≥$50,000 | 328 (46.3%) | 730 (48.5%) | 321 (53.8%) | 784 (50.5%) |
| Missing | 2 | 4 | 1 | 2 |
| Education | ||||
| <HS/HS graduate | 340 (47.9%) | 721 (48.0%) | 240 (40.2%) | 676 (43.6%) |
| College | 261 (36.8%) | 551 (36.7%) | 263 (44.0%) | 651 (41.9%) |
| Post-college | 109 (15.3%) | 230 (15.3%) | 94 (15.8%) | 225 (14.5%) |
| Missing | 1 | 6 | 1 | 4 |
| Menopausal status | ||||
| Premenopausal | 226 (32.6%) | 472 (31.9%) | 211 (37.1%) | 503 (33.7%) |
| Postmenopausal | 468 (67.4%) | 1,006 (68.1%) | 357 (62.9%) | 990 (66.3%) |
| Missing | 17 | 30 | 30 | 63 |
| HRT use | ||||
| Never | 506 (71.3%) | 1,096 (72.9%) | 439 (73.4%) | 1,159 (74.5%) |
| Ever | 204 (28.7%) | 408 (27.1%) | 159 (26.6%) | 396 (25.5%) |
| Missing | 1 | 4 | 0 | 1 |
| Age at menarche (years) | ||||
| ≤12 | 311 (44.1%) | 658 (44.0%) | 274 (46.0%) | 677 (43.8%) |
| >12 | 394 (55.9%) | 837 (56.0%) | 321 (54.0%) | 870 (56.2%) |
| Missing | 6 | 13 | 3 | 9 |
| Oral Contraceptive use | ||||
| Never | 406 (57.2%) | 848 (56.3%) | 304 (50.8%) | 840 (54.0%) |
| Ever | 304 (42.8%) | 657 (43.7%) | 294 (49.2%) | 715 (46.0%) |
| Missing | 1 | 3 | 0 | 1 |
| Parity/lactation history | ||||
| Nulliparous | 92 (12.9%) | 198 (13.1%) | 70 (11.7%) | 171 (11.0%) |
| Parous/never lactated | 375 (52.7%) | 830 (55.0%) | 302 (50.5%) | 832 (53.5%) |
| Parous/ever lactated | 244 (34.3%) | 480 (31.8%) | 226 (37.8%) | 553 (35.5%) |
| Family history of breast cancer | ||||
| None | 564 (82.1%) | 1,166 (79.8%) | 498 (84.7%) | 1,321 (87.0%) |
| First degree | 123 (17.9%) | 295 (20.2%) | 90 (15.3%) | 197 (13.0%) |
| Missing | 24 | 47 | 10 | 38 |
| BMI at reference (kg/m2) | ||||
| <25.0 | 316 (44.6%) | 683 (45.8%) | 309 (52.2%) | 750 (49.1%) |
| 25.0-29.9 | 220 (31.0%) | 476 (31.9%) | 160 (27.0%) | 455 (29.8%) |
| ≥30.0 | 173 (24.4%) | 332 (22.3%) | 123 (20.8%) | 323 (21.1%) |
| Missing | 2 | 17 | 6 | 28 |
| BMI at age 20 (kg/m2) | ||||
| <25.0 | 653 (93.0%) | 1,377 (93.0%) | 534 (90.2%) | 1,397 (91.2%) |
| ≥25.0 | 49 (7.0%) | 103 (7.0%) | 58 (9.8%) | 135 (8.8%) |
| Missing | 9 | 28 | 6 | 24 |
| Lifetime alcohol intake (g/day) | ||||
| Non-drinkers | 263 (37.0%) | 598 (39.7%) | 225 (37.7%) | 605 (39.0%) |
| <15 | 339 (47.7%) | 691 (45.8%) | 289 (48.4%) | 735 (47.3%) |
| 15-29 | 71 (10.0% | 147 (9.7%) | 48 (8.0%) | 119 (7.7%) |
| ≥30 | 38 (5.3%) | 72 (4.8%) | 35 (5.3%) | 94 (6.1%) |
| Stage | ||||
| In situ | 112 (15.8%) | 235 (15.6%) | – | – |
| Invasive | 599 (84.2%) | 1,273 (84.4%) | – | – |
| Tumor size | ||||
| ≤2cm | 279 (73.6%) | 622 (75.5%) | – | – |
| >2cm | 100 (26.4%) | 202 (24.5%) | – | – |
| Missing | 332 | 684 | – | – |
| ER status | ||||
| Negative | 115 (23.8%) | 264 (26.7%) | – | – |
| Positive | 368 (76.2%) | 726 (73.3%) | – | – |
| Missing | 228 | 518 | – | – |
| Radiation therapy | ||||
| No | 192 (38.4%) | 401 (39.1%) | – | – |
| Yes | 308 (61.6%) | 625 (60.9%) | – | – |
| Missing | 211 | 482 | – | – |
| Chemotherapy | ||||
| No | 297 (59.6%) | 599 (58.6%) | – | – |
| Yes | 201 (40.4%) | 423 (41.4%) | – | – |
| Missing | 213 | 486 | – | – |
| Hormone therapy | ||||
| No | 188 (38.1%) | 393 (39.0%) | – | – |
| Yes | 306 (61.9%) | 616 (61.0%) | – | – |
| Missing | 217 | 499 | – | – |
Long Island Breast Cancer Study Project (LIBCSP) population-based women without breast cancer were frequency matched by age to women diagnosed with breast cancer between August 1, 1996 and July 31, 1997.
Case-Control Design
The case-control design of this LIBCSP ancillary study included 711 of the 1,508 women with breast cancer and 598 of the 1,556 women without breast cancer who had available data on urinary phenol metabolites and creatinine. The women with breast cancer were adult residents of Nassau and Suffolk Counties on Long Island, NY, with newly diagnosed breast cancer and were identified using rapid-case ascertainment, which involved active daily or weekly contact with local hospitals with confirmation by physicians and medical records, as previously reported.43 Women without breast cancer were residents of the same two Long Island counties who were identified by Health Care Finance Administration rosters for those 65 years of age and older, and by random digit dialing for those under age 65, and were frequency-matched to the expected distribution of women with breast cancer in 5-year age groups in 1996-1997. After providing written informed consent, the women with breast cancer, on average within three months of their breast cancer diagnoses, and the women without breast cancer were interviewed at home by trained interviewers using a structured questionnaire. At the time of the interview, 93% of women with breast cancer and 83% of women without breast cancer donated 25 mL spot urine for laboratory analyses. For the women with breast cancer, 79.1% of urine samples were collected prior to the initiation of chemotherapy.
Follow-up Design
The follow-up design of this LIBCSP ancillary study included 711 the 1,508 women with breast cancer with available data on urinary phenols and creatinine. These women with breast cancer were monitored for vital status using the National Death Index (NDI), a centralized database of death record information compiled from state vital statistics offices.45 Women with breast cancer were followed-up from the time of diagnosis in 1996/1997 through December 31, 2014 to determine the date and cause of death, including death from breast cancer, identified using International Classification of Death codes 174.9 and C-50.9 listed on the death certificate.44 Over a median follow-up of 17.6 years (range=0.4-18.4), we identified 271 deaths, including 98 from breast cancer, among the 711 women with breast cancer included here.
Quantification of urinary phenol concentrations
Details of the urine sample collection, processing, storage, and biomarker assays have been previously published.44 In brief, stored samples were shipped overnight on dry ice from Columbia University to the National Center for Environmental Health at the CDC in two batches in 2007 and 2010. The first was batch analyzed in 2007, and included a random sample of 400 women with invasive breast cancer and 400 women without breast cancer from among those with available urine. The second batch was analyzed in 2010 and included 493 women with in situ disease or invasive breast cancer who had an available tumor specimen and had not been previously selected and 250 women without breast cancer randomly selected whose urine had not been previously analyzed.
At the CDC, using online solid phase extraction followed by high performance liquid chromatography-isotope dilution tandem mass spectrometry, samples were analyzed for the following seven environmental phenols: 2,5-dichlorophenol, benzophenone-3, BPA, methylparaben, propylparaben, butylparaben, and triclosan. Detection frequencies were >90% for 2,5 dichlorophenol, benzophenone-3, methylparaben, and propylparaben. BPA was detected in 82% of women. Butylparaben and triclosan were detected in 50% and 51% of women, respectively (Table 2). The coefficients of variation (SD/mean concentration) for the individual biomarkers based on masked quality control specimens (3% and 2% in batches 1 and 2, respectively; total n=34) from a single urine pool in all analysis batches ranged between 0.0% and 9.3% (median=2.9%) in both batches. The limits of detection (LODs) ranged from 0.2-2.3 μg/L (Table 2). Values below the LOD were imputed as the LOD divided by the square root of two.46 To correct for urine dilution, concentrations (μg/L) were divided by creatinine for final units of micrograms per gram (μg/g) creatinine. After excluding 234 women with missing creatinine (n=224) or with dilute urine as assessed by creatinine <10 mg/dL (n=10), the final analytic sample for this ancillary study comprised 711 women with breast cancer, including 112 women with in situ disease and 599 women with invasive breast cancer, and 598 women without breast cancer.
Table 2.
Distribution of urinary biomarker concentrations among the ancillary study sample of LIBCSP women.
| Biomarker | LOD | n (%) <LOD | Median uncorrected urinary concentrations (μg/L)a |
Median creatinine-corrected urinary concentrations (μg/g creatinine)a |
||||
|---|---|---|---|---|---|---|---|---|
| With Breast Cancer (n=893) |
No Breast Cancer (n=650) |
Pb | With Breast Cancer (n=711) |
No Breast Cancer (n=598) |
Pb | |||
| 2,5-dichlorophenol | 0.2 | 3 (0.2) | 7.50 | 8.30 | 0.55 | 9.95 | 10.4 | 0.26 |
| Benzophenone-3 | 0.4 | 115 (7.5) | 8.60 | 10.1 | 0.39 | 11.5 | 11.9 | 0.40 |
| Bisphenol A | 0.4 | 282 (18.3) | 1.20 | 1.30 | 0.41 | 1.53 | 1.69 | 0.13 |
| Triclosan | 2.3 | 759 (49.2) | 2.40 | 2.40 | 0.52 | 5.18 | 5.77 | 0.64 |
| Methylparaben | 1.0 | 7 (0.5) | 104 | 100 | 0.24 | 160 | 150 | 0.37 |
| Propylparaben | 0.2 | 35 (2.3) | 25.6 | 22.4 | 0.13 | 39.9 | 34.8 | 0.36 |
| Butylparaben | 0.2 | 779 (50.5) | <LOD | 0.200 | 0.31 | 0.440 | 0.551 | 0.06 |
| Creatinine | 76.4 | 71.2 | 0.57 | |||||
Long Island Breast Cancer Study Project (LIBCSP) population-based women without breast cancer were frequency matched by age to women diagnosed with breast cancer between August 1, 1996 and July 31, 1997.
LOD, limit of detection (in μg/L)
Values <LOD were imputed as LOD/√2.
P-value for Wilcoxon rank-sum test.
Other Covariates
Potential confounders of the associations between environmental phenols and breast cancer incidence and mortality were identified based on previous epidemiologic studies of breast cancer.47,48 Characteristics assessed during the in-person interview included: demographics [age (continuous), income (<$24,999, $25,000-$49,999, ≥$50,000), education (<high school/high school graduate, college, post-college)]; reproductive factors [menopausal status (pre-, postmenopausal), age at menarche (≤12, >12 years), and parity and lactation history (nulliparous, parous/never lactated, parous/ever lactated)]; medical-related factors [family history of breast cancer (none or at least one first degree relative), pre-chemotherapy biospecimen collection (yes, no); exogenous hormone use [contraceptive use (ever, never), hormone replacement therapy use (ever, never)]; and lifestyle/behavioral factors [body mass index (BMI) in the year prior to diagnosis and at age 20 (<25.0, 25.0-29.9, ≥30.0 kg/m2), and percent weight change since age 20 (weight loss and 0-19%, 20-39%, and ≥40% weight gain) and lifetime alcohol intake (non-drinkers, <15, 15-29, ≥30 grams per day)]. Estrogen receptor (ER) status of the first primary breast cancer was assessed by review of the medical record.
Statistical Analysis
In addition to examining the phenols individually, we combined the three parabens into a molar sum (Σparabens), computed as the creatinine-corrected molar sum of methylparaben, propylparaben, and butylparaben, and expressed as methylparaben, molecular weight 152. We categorized creatinine-corrected phenol concentrations of 2,5-dichlorophenol, benzophenone-3, BPA, methylparaben, propylparaben, and Σparabens into quintiles for use in primary analyses and tertiles for use in secondary analyses of effect measure modification. We categorized phenol concentrations based on the distributions in the women without breast cancer. Because butylparaben and triclosan were only detected in approximately half of the women, we categorized women with non-detectable concentrations into the lowest exposure group and women with detectable concentrations into quantiles based on the distributions in the women without breast cancer.
Prior to the case-control and follow-up analyses, we examined associations between urinary phenol biomarkers and the other covariates among women without breast cancer. We first examined Spearman correlations (ρs) between creatinine-corrected phenol concentrations and continuous covariates, and chi-square tests between quintiles of creatinine-corrected phenol concentrations and categorical covariates. Second, among the women with breast cancer, using generalized linear models, we regressed each of the phenol biomarkers on age and receipt of chemotherapy or hormone therapy treatments prior to urine sample collection separately to determine the impact of treatment on urinary phenol concentrations. Third, we compared age-adjusted means of ln-transformed creatinine-corrected urinary phenol concentrations by tumor and treatment characteristics among the women with breast cancer to examine associations between phenols and breast tumor and treatment characteristics.
Case-Control Analyses
We compared continuous uncorrected and creatinine-corrected phenol concentrations between women with and without breast cancer using Wilcoxon rank-sum tests. Next, we examined multivariable associations between quintiles or quantiles (for butylparaben and triclosan) of creatinine-corrected phenol concentrations as well as ln-transformed concentrations and breast cancer incidence using logistic regression to estimate odds ratios (ORs) and 95% confidence intervals (CIs). Logistic regression models were adjusted for the frequency matching factor, age (i.e., age-adjusted models), as well as other covariates that were statistically significantly correlated (P<0.05) with any of the phenols (i.e., multivariable-adjusted models).
In secondary analyses, using tertiles or quantiles (for butylparaben and triclosan) of creatinine-corrected phenol concentrations, we examined effect measure modification by BMI (<25.0 kg/m2 vs ≥25.0 kg/m2) by conducting BMI-stratified covariate-adjusted logistic regression analyses. We evaluated effect measure modification on the multiplicative scale by comparing the log-likelihood statistics from nested models with and without continuous cross-product terms for BMI and ln-transformed creatinine-corrected phenol concentrations.
Case-control analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Follow-up Analyses
We used Kaplan-Meier survival curves to examine the unadjusted associations between urinary phenol concentrations and all-cause and breast cancer-specific mortality up to 18 years following diagnosis. We examined the proportional hazards assumption by Schoenfeld residuals;49 no violations of the proportional hazards assumption were evident. Next, using Cox regression to estimate hazard ratios (HRs) and 95% CIs, we examined age-adjusted and multivariable-adjusted associations between quintiles or quantiles (for butylparaben and triclosan) of ln-transformed urinary phenol concentrations and mortality.
In secondary analyses, using tertiles or quantiles (for butylparaben and triclosan) of creatinine-corrected phenol concentrations, we examined effect measure modification by BMI (<25.0 kg/m2 vs ≥25.0 kg/m2) by conducting BMI-stratified covariate-adjusted Cox regression analyses. Effect measure modification on the multiplicative scale was evaluated by comparing the log-likelihood statistics from nested models with and without continuous cross-product terms for BMI and ln-transformed creatinine-corrected phenol concentrations.
Follow-up analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Most women in the ancillary study reported here were postmenopausal (65.4%), self-identified as Caucasian (93.0%), and ranged in age from 22-96 years at reference, consistent with the characteristics of the full sample of participants from the LIBCSP (Table 1). The mean age at diagnosis among the women with breast cancer was 59.0 years (SD=12.8). Among women with breast cancer, the median (interquartile range, IQR) creatinine was 76.4 (43.1-122.2) mg/dL and among women without breast cancer, the median (IQR) creatinine was 71.2 (42.1-120.7) mg/dL
Among women without breast cancer, Spearman correlations between urinary creatinine-corrected phenol concentrations and continuous covariates were generally weak, with the strongest correlations between 2,5-dichlorophenol and age at reference (ρs=0.23, P<0.01), butylparaben and age at menopause (ρs=0.18, P<0.01), and methylparabern and propylparaben and BMI at reference (both ρs=−0.16, P<0.01) (eTable S1). All phenols were associated with one or more covariate (all chi-square P<0.05), except oral contraceptive use and parity/lactation history (eTable S2). Among women with breast cancer, there were no differences in phenols concentrations by receipt of chemotherapy treatment or receipt of hormone therapy treatment prior to urine sample collection (all P>0.05) (eTable S3). Furthermore, among women with breast cancer, ln-transformed creatinine-corrected urinary phenol concentrations (μg/g creatinine) did not vary by tumor or treatment characteristics (eTable S4).
Case-Control Results
Among women without breast cancer, creatinine-corrected urinary phenol concentrations were highest for methylparaben (median=150 μg/g creatinine) and propylparaben (median=34.8 μg/g creatinine) while the lowest concentrations were for BPA (median=1.69 μg/g creatinine) and butylparaben (median=0.551 μg/g creatinine) (Table 2). Compared to women without breast cancer, women with breast cancer had higher median concentrations of methylparaben (160 vs. 150 μg/g creatinine) and propylparaben (median=39.9 vs. 34.8 μg/g creatinine); however, there were no statistically significant differences in the sample rankings based on Wilcoxon rank sum tests.
The associations between urinary phenol concentrations and breast cancer incidence are presented in Table 3. Among all women, the highest (vs lowest) quintiles of methylparaben, propylparaben, and Σparabens were associated with breast cancer ORs of 1.50 (95%CI=1.03-2.18), 1.31 (95%CI=0.90-1.90), and 1.35 (95%CI=0.93-1.97), respectively. Additionally, one ln-unit increases in methylparaben, propylparaben, and the Σparabens were associated with breast cancer ORs of 1.09 (95%CI=1.00-1.18), 1.06 (95%CI=1.00-1.13), and 1.09 (95%CI=1.00-1.18), respectively. There was little or no association between the remaining phenol biomarkers and breast cancer incidence.
Table 3.
Odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between urinary phenol concentrations (μg/g creatinine) and breast cancer incidence among the ancillary study sample of LIBCSP women (n=1,309).
| Biomarker (μg/g creatinine) | Median in Women without Breast Cancer |
Breast Cancer/ No Breast Cancer |
Age- Adjusted |
Multivariable- Adjusteda |
|
|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | PTrend | |||
| 2,5-dichlorophenol | |||||
| 0.648-4.28 | 3.03 | 147/119 | 1.00 | 1.00 | |
| 4.30-7.62 | 5.93 | 163120 | 1.07 (0.76-1.50) | 1.20 (0.84-1.72) | |
| 7.63-14.9 | 10.4 | 122/120 | 0.81 (0.57-1.16) | 0.86 (0.59-1.25) | |
| 15.1-45.0 | 24.1 | 143120 | 0.92 (0.65-1.30) | 0.95 (0.66-1.37) | |
| 46.0-9,159 | 171 | 136/119 | 0.81 (0.57-1.15) | 0.92 (0.63-1.33) | |
| Ln(2,5-dichlorophenol) | 0.93 (0.86-0.99) | 0.94 (0.87-1.00) | 0.06 | ||
| Benzophenone-3 | |||||
| <LOD-2.13 | 1.11 | 147/119 | 1.00 | 1.00 | |
| 2.14-6.98 | 3.76 | 151/120 | 1.07 (0.76-1.51) | 1.10 (0.77-1.58) | |
| 7.20-23.7 | 11.9 | 137/120 | 1.02 (0.72-1.44) | 1.01 (0.70-1.46) | |
| 23.9-184 | 65.0 | 142/120 | 1.05 (0.74-1.49) | 1.17(0.81-1.70) | |
| 185-26,184 | 774 | 133/119 | 0.99 (0.70-1.40) | 1.10(0.76-1.61) | |
| Ln(Benzophenone-3) | 0.99 (0.95-1.04) | 1.01 (0.96-1.06) | 0.73 | ||
| Bisphenol A | |||||
| <LOD-0.950 | 0.627 | 174/119 | 1.00 | 1.00 | |
| 0.958-1.38 | 1.16 | 132/120 | 0.76 (0.54-1.07) | 0.76 (0.53-1.09) | |
| 1.38-2.04 | 1.69 | 135/120 | 0.78 (0.56-1.10) | 0.76 (0.53-1.09) | |
| 2.05-3.63 | 2.66 | 142/120 | 0.82 (0.59-1.16) | 0.80 (0.56-1.15) | |
| 3.63-388 | 5.72 | 128/119 | 0.74 (0.52-1.04) | 0.75 (0.52-1.08) | |
| Ln(Bisphenol A) | 0.90 (0.81-1.02) | 0.91 (0.80-1.02) | 0.11 | ||
| Triclosan | |||||
| <LOD | – | 334/294 | 1.00 | 1.00 | |
| LOD-10.4 | 5.58 | 142/101 | 1.35 (1.00-1.83) | 1.31 (0.96-1.80) | |
| 10.5-33.8 | 16.0 | 107/102 | 1.02 (0.74-1.40) | 1.02 (0.72-1.44) | |
| 34.0-1,715 | 79.1 | 128/101 | 1.19 (0.87-1.62) | 1.18 (0.86-1.63) | NDb |
| Methylparaben | |||||
| 1.04-31.2 | 15.0 | 126/119 | 1.00 | 1.00 | |
| 32.2-100 | 62.3 | 147/120 | 1.16 (0.82-1.65) | 1.34 (0.93-1.95) | |
| 102-209 | 150 | 132/120 | 1.03 (0.72-1.47) | 1.24 (0.85-1.81) | |
| 215-412 | 303 | 153/120 | 1.20 (0.85-1.70) | 1.48 (1.02-2.15) | |
| 414-3,174 | 658 | 153/119 | 1.21 (0.86-1.72) | 1.50 (1.03-2.18) | |
| Ln(Methylparaben) | 1.04 (0.96-1.12) | 1.09(1.00-1.18) | 0.04 | ||
| Propylparaben | |||||
| <LOD-5.21 | 1.63 | 142/119 | 1.00 | 1.00 | |
| 5.27-20.3 | 9.90 | 120/120 | 0.85 (0.60-1.21) | 0.97 (0.67-1.41) | |
| 20.6-54.2 | 34.8 | 153/120 | 1.08 (0.77-1.52) | 1.27 (0.89-1.83) | |
| 54.4-125 | 80.6 | 147/120 | 1.04 (0.73-1.46) | 1.16 (0.81-1.67) | |
| 128-3,116 | 216 | 149/119 | 1.07 (0.76-1.51) | 1.31 (0.90-1.90) | |
| Ln(Propylparaben) | 1.03 (0.97-1.09) | 1.06 (1.00-1.13) | 0.06 | ||
| Butylparaben | |||||
| <LOD | – | 370/288 | 1.00 | 1.00 | |
| LOD-1.06 | 0.553 | 107/103 | 0.85 (0.62-1.17) | 0.96 (0.69-1.33) | |
| 1.10-6.52 | 2.50 | 111/104 | 0.86 (0.63-1.17) | 0.85 (0.61-1.19) | |
| 6.55-173 | 18.9 | 123/103 | 0.96 (0.71-1.31) | 1.03 (0.74-1.42) | NDb |
| Σparabensc | |||||
| 2.57-42.7 | 19.4 | 132/119 | 1.00 | 1.00 | |
| 42.7-133 | 80.7 | 142/120 | 1.05 (0.74-1.49) | 1.21 (0.84-1.75) | |
| 133-279 | 191 | 132/120 | 1.00 (0.69-1.41) | 1.21 (0.83-1.76) | |
| 280-550 | 395 | 159/120 | 1.18 (0.84-1.67) | 1.39 (0.97-2.01) | |
| 551-3,766 | 897 | 146/119 | 1.09 (0.77-1.55) | 1.35 (0.93-1.97) | |
| Ln(ΣParabens) | 1.04 (0.96-1.12) | 1.09 (1.00-1.18) | 0.05 | ||
Long Island Breast Cancer Study Project (LIBCSP) population-based women without breast cancer were frequency matched by age to women diagnosed with breast cancer between August 1, 1996 and July 31, 1997.
CI, confidence interval; ND, not determined; OR, odds ratio
Adjusted for age (continuous in years), education (<HS/HS graduate, College, and Post-college), menopausal status (pre- vs post-menopausal), hormone replacement therapy use (never vs ever), age at menarche (≤12 vs >12 years of age), parity/lactation history (Nulliparous, Parous/never lactated, Parous/ever lactated), family history of breast cancer (None vs First degree), body mass index (<25.0, 25.0-29.9, and ≥30.0 kg/m2), and lifetime alcohol intake (non-drinkers, <15, 15-29, ≥30 grams per day).
Not determined due to high proportions <LOD.
ΣParabens: Creatinine-corrected molar sum of paraben metabolites: methylparaben, propylparaben, and butylparaben (expressed as methylparaben, molecular weight 152).
Results of effect measure modification by BMI are presented in Table 4. Among women with BMI<25.0 kg/m2, the highest (vs. lowest) tertiles of methylparaben, propylparaben, and the Σparabens were associated with breast cancer ORs of 1.47 (95%CI=0.95-2.25), 1.52 (95%CI=0.98-2.34), and 1.55 (95%CI=1.01-2.37), respectively, but not among women with BMI≥25.0 kg/m2. Furthermore, among women with BMI<25.0 kg/m2, one ln-unit increases in methylparaben, propylparaben, and Σparabens were associated with ORs of 1.13 (1.00-1.28), 1.12 (95%CI=1.02-1.24), and 1.13 (95%CI=0.99-1.27), respectively, but not among women with BMI≥25.0 kg/m2.
Table 4.
BMI-stratified odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between urinary phenol concentrations (μg/g creatinine) and breast cancer incidence among the ancillary study sample of LIBCSP women (n=1,301).
| Biomarker (μg/g creatinine) |
Body Mass Index (BMI) |
pInteraction | |||
|---|---|---|---|---|---|
| BMI <25.0 kg/m2 (n=625) |
BMI ≥25.0 kg/m2 (n=676) |
||||
| With Breast Cancer/ No Breast Cancer |
OR (95% CI)a | With Breast Cancer/ No Breast Cancer |
OR (95% CI)a | ||
| 2,5-dichlorophenol | 0.14 | ||||
| 0.648-6.41 | 130/111 | 1.00 | 136/86 | 1.00 | |
| 4.42-20.9 | 99/102 | 0.87 (0.59-1.29) | 117/96 | 0.79 (0.52-1.20) | |
| 21.0-9,149 | 87/96 | 0.77 (0.51-1.16) | 140/101 | 0.77 (0.51-1.16) | |
| Ln(2,5-dichlorophenol) | 0.92 (0.83-1.03) | 0.95 (0.86-1.04) | |||
| Benzophenone-3 | 0.50 | ||||
| <LOD-4.55 | 86/97 | 1.00 | 153/100 | 1.00 | |
| 4.71-44.1 | 104/96 | 1.17 (0.75-1.81) | 147/102 | 1.05 (0.71-1.55) | |
| 44.5-26,184 | 125/116 | 1.17 (0.77-1.77) | 93/81 | 0.91 (0.60-1.39) | |
| Ln(Benzophenone-3) | 1.01 (0.95-1.08) | 0.99 (0.92-1.06) | |||
| Bisphenol A | 0.15 | ||||
| <LOD-1.23 | 119/99 | 1.00 | 139/97 | 1.00 | |
| 1.24-2.44 | 105/101 | 0.80 (0.53-1.19) | 124/97 | 0.93 (0.63-1.39) | |
| 2.45-388 | 92/109 | 0.65 (0.44-0.98) | 130/89 | 1.07 (0.71-1.60) | |
| Ln(Bisphenol A) | 0.78 (0.66-0.93) | 1.04 (0.87-1.24) | |||
| Triclosan | NDb | ||||
| <LOD | 137/164 | 1.00 | 196/125 | 1.00 | |
| LOD-15.9 | 94/76 | 1.63 (1.08-2.45) | 94/75 | 0.94 (0.63-1.42) | |
| 16.0-1,715 | 85/69 | 1.46 (0.97-2.22) | 103/83 | 0.86 (0.58-1.27) | |
| Methylparaben | 0.50 | ||||
| 1.04-73.3 | 71/84 | 1.00 | 151/113 | 1.00 | |
| 73.7-267 | 106/107 | 1.27 (0.82-1.98) | 135/92 | 1.13 (0.76-1.67) | |
| 270-3,174 | 139/118 | 1.47 (0.95-2.25) | 107/78 | 1.02 (0.68-1.53) | |
| Ln(Methylparaben) | 1.13 (1.00-1.28) | 1.04 (0.93-1.16) | |||
| Propylparaben | 0.20 | ||||
| <LOD-12.4 | 64/83 | 1.00 | 140/115 | 1.00 | |
| 12.9-67.7 | 109/100 | 1.57 (1.00-2.47) | 144/97 | 1.43 (0.97-2.10) | |
| 68.2-3,116 | 143/126 | 1.52 (0.98-2.34) | 109/71 | 1.29 (0.85-1.96) | |
| Ln(Propylparaben) | 1.12 (1.02-1.24) | 1.00 (0.92-1.09) | |||
| Butylparaben | NDb | ||||
| <LOD | 135/133 | 1.00 | 233/152 | 1.00 | |
| LOD-2.49 | 80/83 | 0.98 (0.65-1.48) | 81/70 | 0.88 (0.58-1.32) | |
| 2.51-173 | 101/93 | 1.00 (0.68-1.48) | 79/61 | 0.88 (0.58-1.34) | |
| Σparabensc | 0.43 | ||||
| 2.57-97.1 | 68/85 | 1.00 | 161/112 | 1.00 | |
| 100-353 | 103/103 | 1.30 (0.83-2.03) | 128/96 | 0.94 (0.64-1.39) | |
| 354-3,766 | 145/121 | 1.55 (1.01-2.37) | 104/75 | 0.97 (0.64-1.46) | |
| Ln(Σparabens) | 1.13 (0.99-1.27) | 1.03 (0.93-1.15) | |||
CI, confidence interval; ND, not determined; OR, odds ratio
Long Island Breast Cancer Study Project (LIBCSP) population-based women without breast cancer were frequency matched by age to women diagnosed with breast cancer between August 1, 1996 and July 31, 1997.
CI, confidence interval; ND, not determined; OR, odds ratio
Adjusted for age (continuous in years), education (<HS/HS graduate, College, and Post-college), menopausal status (pre- vs post-menopausal), hormone replacement therapy use (never vs ever), age at menarche (≤12 vs >12 years of age), parity/lactation history (Nulliparous, Parous/never lactated, Parous/ever lactated), family history of breast cancer (None vs First degree), and lifetime alcohol intake (non-drinkers, <15, 15-29, ≥30 grams per day).
Not determined due to high proportions <LOD.
ΣParabens: Creatinine-corrected molar sum of paraben metabolites: methylparaben, propylparaben, and butylparaben (expressed as methylparaben, molecular weight 152).
Follow-up Results
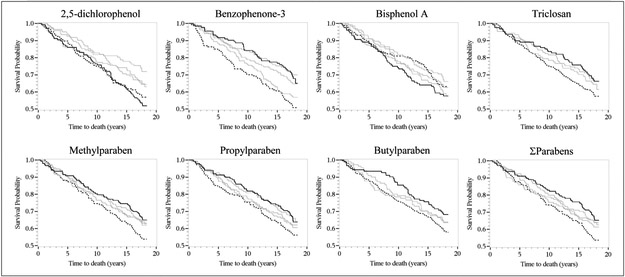
From the Kaplan-Meier survival curves Figure 1, the highest (vs. lowest) quintiles of benzophenone-3, triclosan, methylparaben, propylparaben, butylparaben, and Σparabens were associated with lower all-cause mortality. Furthermore, the highest (vs. lowest) quintiles of 2,5-dichlorophenol, benzophenone-3, methylparaben, propylparaben, butylparaben, and Σparabens were associated with lower breast cancer-specific mortality (eFigure S1).
Figure 1.
Kaplan–Meier survival curves for all-cause mortality and creatinine-adjusted quintiles (Quintile 5, solid line vs. Quintile 1, dashed line) of urinary environmental phenols among LIBCSP women diagnosed with breast cancer in 1996–1997 (n=711). The x-axis shows times to death in years; the y-axis shows proportion of participants alive.
In multivariable-adjusted Cox models, the highest (vs. lowest) quintiles of methylparaben, propylparaben, butylparaben, and Σparabens were associated with all-cause mortality HRs of 0.71 (95%CI=0.48-1.05), 0.77 (95%CI=0.52-1.13), and 0.73 (95%CI=0.51-1.05), and 0.68 (95%CI=0.46-1.00) (Table 5). Additionally, one ln-unit increases of methylparaben, propylparaben, and Σparabens were associated with all-cause mortality HRs of 0.92 (95%CI=0.85-1.00), 0.93 (95%CI=0.87-0.99), and 0.92 (95%CI=0.85-1.00), respectively. The highest (vs. lowest) quintiles of benzophenone-3 and Σparabens were associated with breast cancer-specific mortality HRs of 0.52 (95%CI=0.25-1.08) and 0.74 (95%CI=0.39-1.42), respectively.
Table 5.
Cox regression hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between urinary phenol concentrations (μg/g creatinine) and all-cause and breast cancer-specific mortality among the ancillary study sample of LIBCSP women with breast cancer (n=711).
| All-Cause Mortality |
Breast Cancer-Specific Mortality |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Biomarker (μ/g creatinine) |
Deaths (n=271) |
Censored (n=440) |
Age- adjusted HR (95% CI) |
Multivariable- adjusted HR (95% CI)a |
PTrend | Deaths (n=98) |
Censored (n=605) |
Age- adjusted HR (95% CI) |
Multivariable- adjusted HR (95% CI)a |
PTrend |
| 2,5-dichlorophenol | ||||||||||
| 0.648-4.28 | 63 | 84 | 1 (Reference) | 1 (Reference) | 23 | 123 | 1 (Reference) | 1 (Reference) | ||
| 4.30-7.62 | 58 | 105 | 0.82 (0.57-1.17) | 0.86 (0.59-1.25) | 24 | 136 | 0.93 (0.52-1.65) | 0.90 (0.49-1.62) | ||
| 7.63-14.9 | 34 | 88 | 0.64 (0.42-0.97) | 0.67 (0.44-1.03) | 13 | 106 | 0.64 (0.33-1.27) | 0.64 (0.32-1.28) | ||
| 15.1-45.0 | 51 | 92 | 0.75 (0.52-1.09) | 0.76 (0.52-1.10) | 18 | 124 | 0.76 (0.41-1.40) | 0.68 (0.36-1.28) | ||
| 46.0-9,159 | 65 | 71 | 0.87 (0.62-1.24) | 0.92 (0.65-1.32) | 20 | 116 | 0.91 (0.49-1.66) | 0.84 (0.45-1.56) | ||
| Ln(2,5-dichlorophenol) | 0.95 (0.89-1.02) | 0.96 (0.89-1.03) | 0.25 | 0.95 (0.84-1.08) | 0.94 (0.83-1.07) | 0.35 | ||||
| Benzophenone-3 | ||||||||||
| <LOD-2.13 | 72 | 75 | 1 (Reference) | 1 (Reference) | 27 | 117 | 1 (Reference) | 1 (Reference) | ||
| 2.14-6.98 | 65 | 86 | 0.97 (0.69-1.35) | 0.96 (0.68-1.36) | 22 | 129 | 0.75 (0.43-1.33) | 0.74 (0.41-1.32) | ||
| 7.20-23.7 | 41 | 96 | 0.69 (0.47-1.01) | 0.77 (0.52-1.13) | 15 | 120 | 0.55 (0.29-1.04) | 0.63 (0.33-1.21) | ||
| 23.9-184 | 50 | 92 | 0.89 (0.62-1.29) | 0.92 (0.63-1.34) | 23 | 117 | 0.83 (0.47-1.46) | 0.90 (0.50-1.62) | ||
| 185-26,184 | 43 | 90 | 0.75 (0.51-1.10) | 0.84 (0.57-1.25) | 11 | 121 | 0.41 (0.20-0.83) | 0.52 (0.25-1.08) | ||
| Ln(Benzophenone-3) | 0.97 (0.93-1.02) | 0.99 (0.94-1.04) | 0.67 | 0.91 (0.84-1.00) | 0.95 (0.86-1.04) | 0.25 | ||||
| Bisphenol A | ||||||||||
| <LOD-0.950 | 64 | 110 | 1 (Reference) | 1 (Reference) | 26 | 145 | 1 (Reference) | 1 (Reference) | ||
| 0.958-1.38 | 44 | 88 | 0.97 (0.66-1.43) | 0.96 (0.65-1.41) | 16 | 116 | 0.80 (0.43-1.48) | 0.78 (0.41-1.47) | ||
| 1.38-2.04 | 50 | 85 | 1.13 (0.78-1.64) | 1.10 (0.75-1.60) | 16 | 119 | 0.79 (0.42-1.47) | 0.77 (0.41-1.44) | ||
| 2.05-3.63 | 59 | 83 | 1.22 (0.85-1.73) | 1.16 (0.81-1.67) | 22 | 119 | 1.06 (0.60-1.88) | 1.03 (0.57-1.85) | ||
| 3.63-388 | 54 | 74 | 1.27 (0.88-1.83) | 1.27 (0.87-1.83) | 18 | 106 | 1.00 (0.55-1.82) | 0.93 (0.50-1.73) | ||
| Ln(Bisphenol A) | 1.12 (0.98-1.27) | 1.12 (0.98-1.28) | 0.09 | 1.03 (0.83-1.29) | 1.02 (0.82-1.28) | 0.85 | ||||
| Triclosan | ||||||||||
| <LOD | 141 | 193 | 1 (Reference) | 1 (Reference) | 50 | 282 | 1 (Reference) | 1 (Reference) | ||
| LOD-10.4 | 48 | 94 | 0.95 (0.68-1.32) | 0.95 (0.68-1.33) | 18 | 122 | 0.84 (0.49-1.44) | 0.90 (0.52-1.55) | ||
| 10.5-33.8 | 39 | 68 | 0.96 (0.67-1.36) | 0.94 (0.65-1.36) | 15 | 92 | 0.93 (0.52-1.66) | 0.96 (0.53-1.73) | ||
| 34.0-1,715 | 43 | 85 | 0.88 (0.62-1.24) | 0.91 (0.64-1.29) | NDb | 15 | 109 | 0.77 (0.43-1.38) | 0.82 (0.45-1.47) | NDb |
| Methylparaben | ||||||||||
| 1.04-31.2 | 58 | 68 | 1 (Reference) | 1 (Reference) | 23 | 103 | 1 (Reference) | 1 (Reference) | ||
| 32.2-100 | 54 | 93 | 0.79 (0.55-1.15) | 0.82 (0.56-1.19) | 18 | 126 | 0.66 (0.34-1.22) | 0.74 (0.39-1.38) | ||
| 102-209 | 50 | 82 | 0.80 (0.55-1.16) | 0.83 (0.56-1.22) | 17 | 113 | 0.69 (0.37-1.30) | 0.75 (0.39-1.42) | ||
| 215-412 | 56 | 97 | 0.74 (0.51-1.06) | 0.76 (0.52-1.12) | 21 | 129 | 0.72 (0.40-1.31) | 0.80 (0.43-1.50) | ||
| 414-3,174 | 53 | 100 | 0.68 (0.47-0.98) | 0.71 (0.48-1.05) | 19 | 134 | 0.65 (0.35-1.18) | 0.83 (0.44-1.56) | ||
| Ln(Methylparaben) | 0.91 (0.84-0.99) | 0.92 (0.85-1.00) | 0.05 | 0.92 (0.81-1.05) | 0.96 (0.84-1.11) | 0.59 | ||||
| Propylparaben | ||||||||||
| <LOD-5.21 | 62 | 80 | 1 (Reference) | 1 (Reference) | 25 | 117 | 1 (Reference) | 1 (Reference) | ||
| 5.27-20.3 | 47 | 73 | 0.88 (0.60-1.29) | 0.84 (0.57-1.24) | 22 | 96 | 1.01 (0.57-1.79) | 1.02 (0.57-1.82) | ||
| 20.6-54.2 | 58 | 95 | 0.86 (0.60-1.23) | 0.84 (0.59-1.22) | 16 | 134 | 0.58 (0.31-1.09) | 0.58 (0.31-1.09) | ||
| 54.4-125 | 51 | 96 | 0.69 (0.48-1.00) | 0.65 (0.44-0.96) | 17 | 127 | 0.62 (0.34-1.15) | 0.61 (0.31-1.17) | ||
| 128-3,116 | 53 | 96 | 0.75 (0.52-1.08) | 0.77 (0.52-1.13) | 18 | 131 | 0.64 (0.35-1.17) | 0.87 (0.45-1.65) | ||
| Ln(Propylparaben) | 0.93 (0.88-0.99) | 0.93 (0.87-0.99) | 0.03 | 0.91 (0.83-1.01) | 0.94 (0.84-1.05) | 0.28 | ||||
| Butylparaben | ||||||||||
| <LOD | 153 | 217 | 1 (Reference) | 1 (Reference) | 56 | 309 | 1 (Reference) | 1 (Reference) | ||
| <LOD-1.06 | 39 | 68 | 1.00 (0.70-1.43) | 1.01 (0.71-1.44) | 15 | 91 | 0.93 (0.53-1.65) | 1.06 (0.59-1.89) | ||
| 1.10-6.52 | 40 | 71 | 0.87 (0.61-1.23) | 0.84 (0.59-1.21) | 14 | 96 | 0.81 (0.45-1.45) | 0.86 (0.47-1.58) | ||
| 6.55-173 | 39 | 84 | 0.73 (0.51-1.03) | 0.73 (0.51-1.05) | NDb | 13 | 109 | 0.66 (0.36-1.21) | 0.78 (0.42-1.44) | NDb |
| Σparabensc | ||||||||||
| 2.57-42.7 | 61 | 71 | 1 (Reference) | 1 (Reference) | 25 | 107 | 1 (Reference) | 1 (Reference) | ||
| 42.7-133 | 51 | 91 | 0.74 (0.51-1.07) | 0.77 (0.53-1.14) | 18 | 121 | 0.66 (0.36-1.21) | 0.76 (0.41-1.41) | ||
| 133-279 | 51 | 81 | 0.86 (0.59-1.25) | 0.89 (0.61-1.32) | 19 | 111 | 0.76 (0.42-1.37) | 0.81 (0.44-1.49) | ||
| 280-550 | 58 | 101 | 0.74 (0.52-1.06) | 0.77 (0.53-1.12) | 19 | 137 | 0.61 (0.33-1.10) | 0.67 (0.35-1.26) | ||
| 551-3,766 | 50 | 96 | 0.64 (0.44-0.93) | 0.68 (0.46-1.00) | 17 | 129 | 0.57 (0.31-1.06) | 0.74 (0.39-1.42) | ||
| Ln(ΣParabens) | 0.91 (0.84-0.99) | 0.92 (0.85-1.00) | 0.06 | 0.90 (0.79-1.03) | 0.95 (0.82-1.09) | 0.45 | ||||
CI, confidence interval; ND, not determined; HR, hazard ratio
Long Island Breast Cancer Study Project (LIBCSP) women with breast cancer were diagnosed between August 1, 1996 and July 31, 1997 and monitored for vital status from diagnosis through December 31, 2014.
Adjusted for age at diagnosis (continuous in years), education (<HS/HS graduate, College, and Post-college), menopausal status (pre- vs post-menopausal), hormone replacement therapy use (never vs ever), parity/lactation history (nulliparous, parous/never lactated, and parous/ever lactated), and body mass index (<25.0, 25.0-29.9, and ≥30.0 kg/m2).
Not determined due to high proportions <LOD.
ΣParabens: Creatinine-corrected molar sum of paraben metabolites: methylparaben, propylparaben, and butylparaben (expressed as methylparaben, molecular weight 152).
Results of effect measure modification by BMI for all-cause and breast cancer-specific mortality are presented in Table 6 and Table 7, respectively. Among women with BMI≥25.0 kg/m2, the highest (vs. lowest) tertiles of triclosan, methylparaben, propylparaben, butylparaben, and Σparabens were associated with all-cause mortality HRs of 0.75 (95%CI=0.51-1.11), 0.74 (95%CI=0.50-1.09), 0.62 (95%CI=0.42-0.92), 0.64 (95%CI=0.42-0.99), and 0.70 (95%CI=0.47-1.03), respectively, but not among women with BMI<25.0 kg/m2.
Table 6.
BMI-stratified Cox regression hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between urinary phenol concentrations (μg/g creatinine) and all-cause mortality among the ancillary study sample of LIBCSP women with breast cancer (n=709).
| BMI <25.0 kg/m2(n=316) |
BMI ≥25.0 kg/m2 (n=393) |
PInteraction | |||||
|---|---|---|---|---|---|---|---|
| Biomarker (μ/g creatinine) |
Deaths (n=101) |
Censored (n=215) |
Multivariable- adjusted HR (95% CI)a |
Deaths (n=169) |
Censored (n=224) |
Multivariable- adjusted HR (95% CI)a |
|
| 2,5-dichlorophenol | 0.38 | ||||||
| 0.648-6.41 | 48 | 82 | 1 (Reference) | 57 | 79 | 1 (Reference) | |
| 4.42-20.9 | 22 | 77 | 0.53 (0.32-0.89) | 50 | 67 | 1.20 (0.81-1.78) | |
| 21.0-9,149 | 31 | 56 | 0.80 (0.50-1.27) | 62 | 78 | 0.96 (0.66-1.38) | |
| Ln(2,5-dichlorophenol) | 0.93 (0.82-1.06) | 0.98 (0.90-1.07) | |||||
| Benzophenone-3 | 0.95 | ||||||
| <LOD-4.55 | 35 | 51 | 1 (Reference) | 79 | 74 | 1 (Reference) | |
| 4.71-44.1 | 30 | 74 | 0.82 (0.50-1.37) | 52 | 95 | 0.89 (0.62-1.27) | |
| 44.5-26,184 | 36 | 89 | 0.87 (0.53-1.41) | 38 | 55 | 1.02 (0.68-1.53) | |
| Ln(Benzophenone-3) | 0.98 (0.91-1.06) | 0.99 (0.92-1.06) | |||||
| Bisphenol A | 0.41 | ||||||
| <LOD-1.23 | 36 | 83 | 1 (Reference) | 58 | 81 | 1 (Reference) | |
| 1.24-2.44 | 35 | 70 | 1.16 (0.72-1.87) | 47 | 77 | 0.85 (0.57-1.26) | |
| 2.45-388 | 30 | 62 | 1.29 (0.78-2.12) | 64 | 66 | 1.28 (0.89-1.84) | |
| Ln(Bisphenol A) | 1.05 (0.84-1.32) | 1.17 (0.99-1.37) | |||||
| Triclosan | NDb | ||||||
| <LOD | 48 | 89 | 1 (Reference) | 93 | 103 | 1 (Reference) | |
| LOD-15.9 | 31 | 63 | 1.30 (0.80-2.09) | 40 | 54 | 1.02 (0.70-1.49) | |
| 16.0-1,715 | 22 | 63 | 0.88 (0.52-1.49) | 36 | 67 | 0.75 (0.51-1.11) | |
| Methylparaben | 0.96 | ||||||
| 1.04-73.3 | 26 | 45 | 1 (Reference) | 72 | 79 | 1 (Reference) | |
| 73.7-267 | 29 | 77 | 0.65 (0.37-1.12) | 54 | 81 | 0.78 (0.54-1.12) | |
| 270-3,174 | 46 | 93 | 0.77 (0.47-1.28) | 43 | 64 | 0.74 (0.50-1.09) | |
| Ln(Methylparaben) | 0.93 (0.80-1.08) | 0.90 (0.81-1.00) | |||||
| Propylparaben | 0.55 | ||||||
| <LOD-12.4 | 22 | 42 | 1 (Reference) | 67 | 73 | 1 (Reference) | |
| 12.9-67.7 | 34 | 75 | 1.04 (0.59-1.80) | 60 | 84 | 0.81 (0.57-1.15) | |
| 68.2-3,116 | 45 | 98 | 0.87 (0.51-1.46) | 42 | 67 | 0.62 (0.42-0.92) | |
| Ln(Propylparaben) | 0.96 (0.85-1.07) | 0.92 (0.85-0.99) | |||||
| Butylparaben | NDb | ||||||
| <LOD | 48 | 87 | 1 (Reference) | 104 | 129 | 1 (Reference) | |
| LOD-2.49 | 22 | 58 | 0.89 (0.53-1.49) | 37 | 44 | 1.00 (0.68-1.46) | |
| 2.51-173 | 31 | 70 | 0.83 (0.51-1.32) | 28 | 51 | 0.64 (0.42-0.99) | |
| Σparabensc | 0.82 | ||||||
| 2.57-97.1 | 25 | 43 | 1 (Reference) | 74 | 87 | 1 (Reference) | |
| 100-353 | 29 | 74 | 0.69 (0.40-1.21) | 56 | 72 | 0.90 (0.63-1.28) | |
| 354-3,766 | 47 | 98 | 0.80 (0.49-1.32) | 39 | 65 | 0.70 (0.47-1.03) | |
| Ln(Σparabens) | 0.94 (0.81-1.09) | 0.90 (0.81-0.99) | |||||
CI, confidence interval; ND, not determined; HR, hazard ratio
Long Island Breast Cancer Study Project (LIBCSP) women with breast cancer were diagnosed between August 1, 1996 and July 31, 1997 and monitored for vital status from diagnosis through December 31, 2014.
Adjusted for age at diagnosis (continuous in years), education (<HS/HS graduate, College, and Post-college), menopausal status (pre- vs post-menopausal), hormone replacement therapy use (never vs ever), and parity/lactation history (nulliparous, parous/never lactated, and parous/ever lactated).
Not determined due to high proportions <LOD.
ΣParabens: Creatinine-corrected molar sum of paraben metabolites: methylparaben, propylparaben, and butylparaben (expressed as methylparaben, molecular weight 152).
Table 7.
BMI-stratified Cox regression hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between urinary phenol concentrations (μg/g creatinine) and breast cancer-specific mortality among the ancillary study sample of LIBCSP women with breast cancer (n=701).
| Biomarker (μ/g creatinine) |
BMI <25.0 kg/m2 (n=313) |
BMI ≥25.0 kg/m2 (n=388) |
PInteraction | ||||
|---|---|---|---|---|---|---|---|
| Deaths (n=33) |
Censored (n=280) |
Multivariable- adjusted HR (95% CI)a |
Deaths (n=65) |
Censored (n=323) |
Multivariable- adjusted HR (95% CI)a |
||
| 2,5-dichlorophenol | 0.62 | ||||||
| 0.648-6.41 | 17 | 111 | 1 (Reference) | 25 | 109 | 1 (Reference) | |
| 4.42-20.9 | 7 | 91 | 0.49 (0.20-1.20) | 20 | 95 | 1.04 (0.57-1.91) | |
| 21.0-9,149 | 9 | 78 | 0.78 (0.34-1.78) | 20 | 119 | 0.78 (0.42-1.44) | |
| Ln(2,5-dichlorophenol) | 0.90 (0.71-1.16) | 0.97 (0.83-1.12) | |||||
| Benzophenone-3 | 0.16 | ||||||
| <LOD-4.55 | 9 | 77 | 1 (Reference) | 29 | 121 | 1 (Reference) | |
| 4.71-44.1 | 12 | 90 | 1.02 (0.42-2.50) | 21 | 124 | 0.80 (0.44-1.46) | |
| 44.5-26,184 | 12 | 112 | 0.83 (0.33-2.06) | 15 | 78 | 0.94 (0.49-1.81) | |
| Ln(Benzophenone-3) | 0.96 (0.83-1.11) | 0.92 (0.82-1.04) | |||||
| Bisphenol A | 0.33 | ||||||
| <LOD-1.23 | 11 | 108 | 1 (Reference) | 25 | 111 | 1 (Reference) | |
| 1.24-2.44 | 14 | 90 | 1.33 (0.59-2.99) | 13 | 111 | 0.54 (0.27-1.07) | |
| 2.45-388 | 8 | 82 | 1.05 (0.42-2.64) | 27 | 101 | 1.20 (0.68-2.10) | |
| Ln(Bisphenol A) | 0.85 (0.55-1.30) | 1.11 (0.85-1.44) | |||||
| Triclosan | NDb | ||||||
| <LOD | 12 | 123 | 1 (Reference) | 38 | 158 | 1 (Reference) | |
| LOD-15.9 | 11 | 83 | 1.56 (0.66-3.69) | 18 | 74 | 1.02 (0.57-1.82) | |
| 16.0-1,715 | 10 | 74 | 1.46 (0.61-3.49) | 9 | 91 | 0.43 (0.20-0.89) | |
| Methylparaben | 0.22 | ||||||
| 1.04-73.3 | 8 | 62 | 1 (Reference) | 28 | 122 | 1 (Reference) | |
| 73.7-267 | 7 | 98 | 0.40 (0.14-1.18) | 21 | 112 | 0.83 (0.47-1.48) | |
| 270-3,174 | 18 | 120 | 1.07 (0.46-2.52) | 16 | 89 | 0.82 (0.43-1.54) | |
| Ln(Methylparaben) | 1.05 (0.79-1.38) | 0.91 (0.77-1.08) | |||||
| Propylparaben | 0.52 | ||||||
| <LOD-12.4 | 8 | 56 | 1 (Reference) | 27 | 112 | 1 (Reference) | |
| 12.9-67.7 | 8 | 98 | 0.52 (0.19-1.41) | 24 | 116 | 0.84 (0.48-1.46) | |
| 68.2-3,116 | 17 | 126 | 0.89 (0.38-2.10) | 14 | 95 | 0.60 (0.30-1.17) | |
| Ln(Propylparaben) | 0.94 (0.76-1.16) | 0.93 (0.82-1.05) | |||||
| Butylparaben | NDb | ||||||
| <LOD | 14 | 120 | 1 (Reference) | 42 | 187 | 1 (Reference) | |
| LOD-2.49 | 9 | 70 | 1.01 (0.43-2.39) | 14 | 67 | 1.00 (0.54-1.85) | |
| 2.51-173 | 10 | 90 | 0.80 (0.34-1.88) | 9 | 69 | 0.63 (0.30-1.30) | |
| Σparabensc | 0.28 | ||||||
| 2.57-97.1 | 8 | 59 | 1 (Reference) | 30 | 129 | 1 (Reference) | |
| 100-353 | 8 | 94 | 0.49 (0.17-1.36) | 21 | 105 | 0.86 (0.49-1.53) | |
| 354-3,766 | 17 | 127 | 0.95 (0.40-2.24) | 14 | 89 | 0.70 (0.36-1.35) | |
| Ln(Σparabens) | 1.01 (0.76-1.32) | 0.90 (0.76-1.07) | |||||
CI, confidence interval; ND, not determined; HR, hazard ratio
Long Island Breast Cancer Study Project (LIBCSP) women with breast cancer were diagnosed between August 1, 1996 and July 31, 1997 and monitored for vital status from diagnosis through December 31, 2014.
Adjusted for age at diagnosis (continuous in years), education (<HS/HS graduate, College, and Post-college), menopausal status (pre- vs post-menopausal), hormone replacement therapy use (never vs ever), and parity/lactation history (nulliparous, parous/never lactated, and parous/ever lactated).
Not determined due to high proportions <LOD.
ΣParabens: Creatinine-corrected molar sum of paraben metabolites: methylparaben, propylparaben, and butylparaben (expressed as methylparaben, molecular weight 152).
Discussion
In this study of urinary phenol biomarkers and breast cancer incidence and mortality, we observed 30-50% higher odds of developing breast cancer among women with the highest (vs. lowest) quintiles of parabens and these associations were more pronounced among women with BMI<25.0 kg/m2 than among women with BMI≥25.0 kg/m2. For mortality following breast cancer, we observed inverse associations between parabens and all-cause mortality, and contrary to our case-control results, associations were more pronounced among women with BMI≥25.0 kg/m2 than among women with BMI<25.0 kg/m2. While the confidence intervals were imprecise and included the null, the highest (vs. lowest) quintiles of benzophenone-3 and the parabens were inversely associated with breast cancer-specific mortality.
Few studies have examined associations between the use of personal care products and breast cancer development and, to our knowledge, no studies have considered mortality following breast cancer. Of the personal care products that have been examined in association with breast cancer incidence, particular attention has been placed on the association between deodorant use, a source of exposure to parabens and other chemicals,13 due to observations of an increasing incidence of tumors in the upper, outer quadrant of the breast directly adjacent to the area of the breast where deodorants are applied.50 Even so, studies examining deodorant use and breast cancer development are limited. A recent review38 identified two studies, one of which reported an inverse association,51 and the other a small increase in risk of breast cancer development,52 in association with deodorant use. Additionally, a recently published hospital-based case-control study reported an increase in breast cancer risk in association with use of underarm cosmetic products several times per day when women were under the age of 30.42 However, the authors hypothesized that the association was due to the aluminum-based compounds found in the underarm cosmetic products.42 Last, a study examining patterns of personal care product use reported an increased risk of breast cancer among frequent users of beauty and skincare products relative to infrequent users.39
At least two studies outside of the USA have examined biomarkers of BPA exposure in association with breast cancer development. The first, a small case-control study of Korean women (82 cases and 70 controls) reported higher serum BPA concentrations among cases compared to controls (median=0.61 vs. median=0.03 μg/L).41 Measurement of BPA in serum, however, is likely unreliable for reasons of pharmacokinetics and external contamination,26 and so results may not be directly comparable to the findings reported here. The second, a case-control study of Polish women (575 cases and 575 controls), reported an increase in postmenopausal breast cancer odds among women in the second quartile of urinary BPA (OR=1.70, 95% CI=0.91-1.17), but not for the third (OR=1.02, 95% CI=0.67-1.55) and fourth (OR=1.09, 95% CI=0.73-1.63) quartiles, compared to the first quartile.40 These results are contrary to our findings reported here of a suggestive inverse association between BPA and breast cancer incidence. Differences in the distributions of BPA urinary concentrations, which were much lower in our study than in the study by Trabert et al., may be one reason for the discrepant findings. To our knowledge, no studies have examined 2,5-dichlorophenol, benzophenone-3, parabens, and triclosan in association with breast cancer development. Although previous studies reported an association between 2,5-dichlorophenol and earlier menarche in girls, which is known to increase a woman’s risk of breast cancer,53 in our study, we did not observe a positive association between urinary 2,5-dichlorophenol and breast cancer incidence.
Many environmental phenols are known endocrine disruptors,14,54 and are thus biologically plausible breast carcinogens. Parabens are weakly estrogenic and increase ER-α and ER-β mRNA and protein expression and expression of the aromatase gene, inducing proliferation of MCF-7 human breast cancer cells and MCF-10A non-transformed breast epithelial cells in vitro.37,55-57 Butylparaben has been shown to increase c-Myc RNA expression and ER-α-mediated breast cancer cell proliferation in human epidermal growth factor receptor (HER)-2 overexpressing BT-474 cells, synergistically in the presence of the HER ligand heregulin.58 In vivo, parabens cause uterotrophic activity and up-regulate estrogen-responsive genes in the uteri of immature Sprague-Dawley rats at human exposure levels.59 Although, estrogen-mediated mechanisms may be most relevant to breast carcinogenesis, parabens may also play a role in breast carcinogenesis through non-estrogen mediated mechanisms.13 Propylparaben, for example, has been associated with the inhibition of apoptosis in MCF-7 breast cancer cells through the activation of PI3K/Akt pathway, measured as Akt phosphorylation,60
In this study, we report inverse associations between urinary parabens and all-cause mortality among a sample of women with breast cancer. The biological mechanisms by which parabens may be inversely associated mortality are unclear and require further investigation. However, two potential causal explanations are plausible. First, parabens have been shown to be peroxisome proliferator-activated receptor (PPAR) agonists,61-63 which may result in anti-inflammatory effects through the inhibition of pro-inflammatory cytokines.64 Second, parabens have also been shown to shown to exert anti-androgenic activity. In a cell-based study, at the highest concentrations tested, methyl-, butyl-, and propylparaben inhibited the transcriptional activity of testosterone.65 High bioavailable testosterone levels have been associated with metabolic syndrome or its components in cross-sectional studies66 and with greater risk of incident type 2 diabetes67 and coronary heart disease events in prospective studies.68,69 Thus, inhibition of testosterone by parabens may result in favorable mortality outcomes. Future studies should work to replicate our findings among a population-based sample of women without breast cancer in order to elucidate these associations.
Our BMI-stratified results suggest that exposure to phenols or their precursors and BMI may interact to increase the risk of breast cancer development. In postmenopausal women, with cessation of estrogen synthesis in the ovaries, the major pathway of estrogen production becomes the conversion of androstenedione into estrone in adipose tissue.70,71 Additionally, postmenopausal obese women may have a higher proportion of bioavailable estrogen and testosterone due to lower levels of SHBG 72,73 Estrogens are well known breast carcinogens74 and so it is conceivable that phenols may promote estrogen-initiated breast cancer, or that phenols may alter body weight,75 thus impacting breast cancer risk. Additional research into the potential interactions between endocrine disrupting chemicals, obesity, and breast cancer is needed.
The strengths of our study include the large sample size and the use of biological samples from a population-based case-control study of breast cancer; however, this study had several limitations. First, among women with breast cancer, urine samples were collected after breast cancer diagnosis, but before initiation of chemotherapy for most participants. At-diagnosis phenol urinary concentrations may not reflect the etiologically relevant time period for breast cancer, which is hypothesized to be decades years prior to disease diagnosis for environmental pollutants;1 however, because environmental phenols are estrogen mimics, concentrations measured shortly after diagnosis may be relevant to breast cancer progression as well as mortality following breast cancer. Furthermore, breast cancer or its treatments may impact phenol concentrations or women may alter their patterns of personal care product use after diagnosis. However, we observed higher concentrations of parabens among women with breast cancer compared to women without breast cancer and did not observe associations between chemotherapy treatment and phenol concentrations. It is unlikely women with breast cancer would increase their use of personal care products if they believed it was associated with their breast cancer diagnosis. Additionally, women with breast cancer were diagnosed in the mid- 1990s, before the onset of widespread public concern about endocrine disrupting chemicals in personal care products. Therefore, it is highly unlikely that women specifically changed their behavior with the intention of altering their chemical exposures. However, the hospital or medical settings could potentially be a source of exposure to environmental phenols including those chemicals used in cleaning products such as antimicrobials,23 which could result in higher biomarker levels among women with breast cancer as compared to women without breast cancer, potentially biasing our results. Additionally, we compared environmental phenol concentrations by receipt of chemotherapy treatment, but we did not consider specific chemotherapy regimens, and thus potential differences by chemotherapy type may have been masked. However, chemotherapy treatment at the time of the LIBCSP in the-mid-1990s was generally uniform consisting primarily of cyclophosphamide, methotrexate, and fluorouracil or cyclophosphamide and doxorubicin.76 Second, some phenols show fair to good reproducibility over weeks or months, with intraclass correlations (ICCs) of 0.50-0.61 for 2,5-dichlorophenol, 0.62 for benzophenone-3, 0.42-0.61 for methylparaben, 0.32-0.55 for propylparaben, and 0.47-.058 for triclosan, but BPA shows poor reproducibility (ICC=0.24-0.27).77-80 The fair reproducibility of most of these biomarkers suggests that concentrations from a single spot urine sample may allow for the moderately reliable ranking of women’s exposure, but additional studies are needed that examine the ICCs over longer time periods. This may be especially relevant to our follow-up analyses that considered a single urinary measurement of phenol biomarkers in association with mortality up to 18 years following breast cancer diagnosis. Third, we included a subsample of the population-based LIBCSP sample. Although we observed little difference between the women included in this ancillary study and the parent LIBCSP, there remains a small potential for selection bias. Furthermore, as NHANES did not begin urinary biomonitoring of most of the environmental phenols we considered here until 2005-2006, we do not know whether the levels reported here are reflective of the general population at the time of participant enrollment into the LIBCSP in 1996-1997. Thus, the generalizability of our findings may be limited. Last, we cannot fully rule out residual and unmeasured confounding as a source of bias in this observational study. However, we examined a comprehensive list of covariates as potential confounders.
Conclusion
The results of our study support a hypothesized positive association between exposure to parabens and breast carcinogenesis. However, select parabens may have differential associations with the risk of developing breast cancer and mortality following breast cancer. Our results are consistent with laboratory evidence and thus biologically plausible; however, our findings should be interpreted with caution given that biospecimens were spot urine samples and collection among the women with breast cancer occurred after their diagnosis. Confirmation of our case-control results with a prospective study design is warranted, but if confirmed, our findings have implications about the widespread use of these chemicals in personal care and consumer products.
Supplementary Material
Highlights.
Select parabens were associated with 30-50% higher odds of breast cancer
BC incidence associations were more pronounced among women with low versus high BMI
Select parabens were inversely associated with all-cause mortality
Mortality associations were more pronounced among women with high versus low BMI
Acknowledgements:
This study was supported in part by funds from the National Cancer Institute and the National Institute of Environmental Health Sciences (U01 CA/ES66572, U01 CA66572, 1K07 CA102640-01, U01 ES019459, P30 ES009089, K01 ES012645, and T32 ES007018). We acknowledge the technical assistance of the late X. Ye, and J. Reidy (CDC, Atlanta, GA) in measuring the urinary concentrations of phenol biomarkers.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC). Use of trade names is for identification only and does not imply endorsement by the CDC, the Public Health Service, or the US Department of Health and Human Services.
Footnotes
Conflicts of interest: Dr. Neugut has consulted for Otsuka, United Biosource Corporation, Hospira, Teva, and Eisai, and serves on the Scientific Advisory Board of EHE Intl. The authors declare no other conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brody JG, Rudel RA. Environmental pollutants and breast cancer. Environ Health Perspect. 2003;111(8):1007–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 3.Ingber SZ, Buser MC, Pohl HR, Abadin HG, Edward Murray H, Scinicariello F. DDT/DDE and breast cancer: a meta-analysis. Regul Toxicol Pharmacol. 2013;67(3):421–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.López-Cervantes M, Torres-Sánchez L, Tobías A, López-Carrillo L. Dichlorodiphenyldichloroethane burden and breast cancer risk: a meta-analysis of the epidemiologic evidence. Environ Health Perspect. 2004;112(2):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J, Huang Y, Wang X, Lin K, Wu K. Environmental polychlorinated biphenyl exposure and breast cancer risk: a meta-analysis of observational studies Lehmler H-J, ed. PLoS One. 2015;10(11):e0142513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korsh J, Shen A, Aliano K, Davenport T. Polycyclic aromatic hydrocarbons and breast cancer: a review of the literature. Breast Care. 2015;10(5):316–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parada H, Wolff MS, Engel LS, et al. Organochlorine insecticides DDT and chlordane in relation to survival following breast cancer. Int J Cancer. 2016;138(3):565–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parada H, Wolff MS, Engel LS, et al. Polychlorinated biphenyls and their association with survival following breast cancer. Eur J Cancer. 2016;56:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sagiv SK, Gaudet MM, Eng SM, et al. Polycyclic aromatic hydrocarbon-DNA adducts and survival among women with breast cancer. Environ Res. 2009;109:287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siddique S, Kubwabo C, Harris SA. A review of the role of emerging environmental contaminants in the development of breast cancer in women. Emerg Contam. 2016;2(4):204–219. [Google Scholar]
- 11.Vione D, Caringella R, De Laurentiis E, Pazzi M, Minero C. Phototransformation of the sunlight filter benzophenone-3 (2-hydroxy-4-methoxybenzophenone) under conditions relevant to surface waters. Sci Total Environ. 2013;463-464:243–251. [DOI] [PubMed] [Google Scholar]
- 12.Bester K Fate of triclosan and triclosan-methyl in sewage treatment plants and surface waters. Arch Environ Contam Toxicol. 2005;49(1):9–17. [DOI] [PubMed] [Google Scholar]
- 13.Darbre PD, Harvey PW. Paraben esters: review of recent studies of endocrine toxicity, absorption, esterase and human exposure, and discussion of potential human health risks. J Appl Toxicol. 2008;28(5):561–578. [DOI] [PubMed] [Google Scholar]
- 14.Witorsch RJ, Thomas JA. Personal care products and endocrine disruption: a critical review of the literature. Crit Rev Toxicol. 2010;40(sup3):1–30. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention, Department of Health and Human Services. Fourth National Report on Human Exposure to Environmental Chemicals.; 2013. http://www.cdc.gov/exposurereport/pdf/fourthreport.pdf.
- 16.Centers for Disease Control and Prevention. Fourth National Report on Human Exposure to Environmental Chemicals, Updated Tables, January, 2019, Volume One. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA; 2019. https://www.cdc.gov/exposurereport/. [Google Scholar]
- 17.Yoshida T, Andoh K, Fukuhara M. Urinary 2,5-dichlorophenol as biological index for p-dichlorobenzene exposure in the general population. Arch Environ Contam Toxicol. 2002;43(4):481–485. [DOI] [PubMed] [Google Scholar]
- 18.Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological profile for dichlorobenzenes. https://www.atsdr.cdc.gov/toxprofiles/tp10.pdf. Published 2006. Accessed March 17, 2018. [PubMed]
- 19.Staples CA, Dorn PB, Klecka GM, O’Block ST, Harris LR. A review of the environmental fate, effects, and exposures of bisphenol A. Chemosphere. 1998;36(10):2149–2173. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez H, Farbrot A, Larko O, Wennberg A-M. Percutaneous absorption of the sunscreen benzophenone-3 after repeated whole-body applications, with and without ultraviolet irradiation. Br J Dermatol. 2006;154(2):337–340. [DOI] [PubMed] [Google Scholar]
- 21.Bhargava HN, Leonard PA. Triclosan: applications and safety. Am J Infect Control. 1996;24(3):209–218. [DOI] [PubMed] [Google Scholar]
- 22.Lokhnauth JK, Snow NH. Determination of parabens in pharmaceutical formulations by solid-phase microextraction-ion mobility spectrometry. Anal Chem. 2005;77(18):5938–5946. [DOI] [PubMed] [Google Scholar]
- 23.Dodson RE, Nishioka M, Standley LJ, Perovich LJ, Brody JG, Rudel RA. Endocrine disruptors and asthma-associated chemicals in consumer products. Environ Health Perspect. 2012;120(7):935–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engel S, Wolff M. Causal inference considerations for endocrine disruptor research in children’s health. Annu Rev Public Health. 2013;34:139–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hines EP, Mendola P, von Ehrenstein OS, Ye X, Calafat AM, Fenton SE. Concentrations of environmental phenols and parabens in milk, urine and serum of lactating North Carolina women. Reprod Toxicol. 2015;54:120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calafat AM, Longnecker MP, Koch HM, Swan SH, Hauser R. Optimal exposure biomarkers for nonpersistent chemicals in environmental epidemiology. Environ Health Perspect. 2015;123(7):A166–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calafat AM, Valentin-Blasini L, Ye X. Trends in exposure to chemicals in personal care and consumer products. Curr Environ Heal Reports. 2015;2(4):348–355. [DOI] [PubMed] [Google Scholar]
- 28.Calafat AM, Ye X, Wong L-Y, Bishop AM, Needham LL. Urinary concentrations of four parabens in the U.S. population: NHANES 2005-2006. Environ Health Perspect. 2010;118(5):679–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frederiksen H, Jørgensen N, Andersson A-M. Parabens in urine, serum and seminal plasma from healthy Danish men determined by liquid chromatography-tandem mass spectrometry (LC-MS/MS). J Expo Sci Environ Epidemiol. 2011;21(3):262–271. [DOI] [PubMed] [Google Scholar]
- 30.Allmyr M, Adolfsson-Erici M, McLachlan MS, Sandborgh-Englund G. Triclosan in plasma and milk from Swedish nursing mothers and their exposure via personal care products. Sci Total Environ. 2006;372(1):87–93. [DOI] [PubMed] [Google Scholar]
- 31.Koeppe ES, Ferguson KK, Colacino JA, Meeker JD. Relationship between urinary triclosan and paraben concentrations and serum thyroid measures in NHANES 2007–2008. Sci Total Environ. 2013;445-446:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Calafat AM, Wong L-Y, Ye X, Reidy JA, Needham LL. Concentrations of the sunscreen agent benzophenone-3 in residents of the United States: National Health and Nutrition Examination Survey 2003--2004. Environ Health Perspect. 2008; 116(7):893–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adolfsson-Erici M, Pettersson M, Parkkonen J, Sturve J. Triclosan, a commonly used bactericide found in human milk and in the aquatic environment in Sweden. Chemosphere. 2002;46(9-10): 1485–1489. [DOI] [PubMed] [Google Scholar]
- 34.Mendonca K, Hauser R, Calafat AM, Arbuckle TE, Duty SM. Bisphenol A concentrations in maternal breast milk and infant urine. Int Arch Occup Environ Health. 2014;87(1): 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ye X, Bishop AM, Needham LL, Calafat AM. Automated on-line column-switching HPLC-MS/MS method with peak focusing for measuring parabens, triclosan, and other environmental phenols in human milk. Anal Chim Acta. 2008;622(1-2):150–156. [DOI] [PubMed] [Google Scholar]
- 36.Fisher M, MacPherson S, Braun JM, et al. Paraben concentrations in maternal urine and breast milk and its association with personal care product use. Environ Sci Technol. 2017;51(7):4009–4017. [DOI] [PubMed] [Google Scholar]
- 37.Gee RH, Charles A, Taylor N, Darbre PD. Oestrogenic and androgenic activity of triclosan in breast cancer cells. J Appl Toxicol. 2008;28(1):78–91. [DOI] [PubMed] [Google Scholar]
- 38.Hardefeldt PJ, Edirimanne S, Eslick GD. Deodorant Use and Breast Cancer Risk. Epidemiology. 2013;24(1):172. [DOI] [PubMed] [Google Scholar]
- 39.Taylor KW, Troester MA, Herring AH, et al. Associations between personal care product use patterns and breast cancer risk among white and black women in the Sister Study. Environ Health Perspect. 2018;126(2):027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trabert B, Falk RT, Figueroa JD, et al. Urinary bisphenol A-glucuronide and postmenopausal breast cancer in Poland. Cancer Causes Control. 2014;25(12):1587–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang M, Ryu J-H, Jeon R, Kang D, Yoo K-Y. Effects of bisphenol A on breast cancer and its risk factors. Arch Toxicol. 2009;83(3):281–285. [DOI] [PubMed] [Google Scholar]
- 42.Linhart C, Talasz H, Morandi EM, et al. Use of underarm cosmetic products in relation to risk of breast cancer: a case-control study. EBioMedicine. 2017;21:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gammon MD, Neugut AI, Santella RM, et al. The Long Island Breast Cancer Study Project: description of a multi-institutional collaboration to identify environmental risk factors for breast cancer. Breast Cancer Res Treat. 2002;74(3):235–254. [DOI] [PubMed] [Google Scholar]
- 44.Parada H, Gammon MD, Chen J, et al. Urinary phthalate metabolite concentrations and breast cancer incidence and survival following breast cancer: The Long Island Breast Cancer Study Project. Environ Health Perspect. 2018; 126(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. National Death Index. http://www.cdc.gov/nchs/ndi.htm. Published 2017. Accessed June 26, 2018.
- 46.Hornung RW, Reed LD. Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg. 1990;5(1):46–51. [Google Scholar]
- 47.Mcpherson K, Steel C, Dixon J. ABC of breast diseases: breast cancer-epidemiology, risk factors, and genetics. BMJ. 2000;321:624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McPherson K, Steel CM, Dixon JM. Breast cancer—epidemiology, risk factors, and genetics. BMJ. 2000;321:624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Allison P Survival Analysis Using SAS: A Practical Guide. 2nd ed. Cary, NC; 2010. [Google Scholar]
- 50.Darbre PD. Underarm cosmetics and breast cancer. J Appl Toxicol. 2003;23(2):89–95. [DOI] [PubMed] [Google Scholar]
- 51.Fakri S, Al-Azzawi A, Al-Tawil N. Antiperspirant use as a risk factor for breast cancer in Iraq. East Mediterr Heal J. 2006;12(3-4):478–482. [PubMed] [Google Scholar]
- 52.Mirick DK, Davis S, Thomas DB. Antiperspirant use and the risk of breast cancer. J Natl Cancer Inst. 2002;94(20):1578–1580. [DOI] [PubMed] [Google Scholar]
- 53.Wolff MS, Pajak A, Pinney SM, et al. Associations of urinary phthalate and phenol biomarkers with menarche in a multiethnic cohort of young girls. Reprod Toxicol. 2017;67:56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gray JM, Rasanayagam S, Engel C, Rizzo J. State of the evidence 2017: an update on the connection between breast cancer and the environment. Environ Heal. 2017; 16(94): 1–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Byford JR, Shaw LE, Drew MGB, Pope GS, Sauer MJ, Darbre PD. Oestrogenic activity of parabens in MCF7 human breast cancer cells. J Steroid Biochem Mol Biol. 2002;80(1):49–60. [DOI] [PubMed] [Google Scholar]
- 56.Wróbel AM, Gregoraszczuk EŁ. Actions of methyl-, propyl- and butylparaben on estrogen receptor-α and -β and the progesterone receptor in MCF-7 cancer cells and non-cancerous MCF-10A cells. Toxicol Lett. 2014;230(3):375–381. [DOI] [PubMed] [Google Scholar]
- 57.Wróbel A, Gregoraszczuk EŁ. Effects of single and repeated in vitro exposure of three forms of parabens, methyl-, butyl- and propylparabens on the proliferation and estradiol secretion in MCF-7 and MCF-10A cells. Pharmacol Rep. 2013;65(2):484–493. [DOI] [PubMed] [Google Scholar]
- 58.Pan S, Yuan C, Tagmount A, et al. Parabens and human epidermal growth factor receptor ligand cross-talk in breast cancer cells. Environ Health Perspect. 2016;124(5):563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sun L, Yu T, Guo J, et al. The estrogenicity of methylparaben and ethylparaben at doses close to the acceptable daily intake in immature Sprague-Dawley rats. Sci Rep. 2016;6(1):25173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wróbel AM, Gregoraszczuk EŁ. Action of methyl-, propyl- and butylparaben on GPR30 gene and protein expression, cAMP levels and activation of ERK1/2 and PI3K/Akt signaling pathways in MCF-7 breast cancer cells and MCF-10A non-transformed breast epithelial cells. Toxicol Lett. 2015;238(2): 110–116. [DOI] [PubMed] [Google Scholar]
- 61.Hu P, Overby H, Heal E, et al. Methylparaben and butylparaben alter multipotent mesenchymal stem cell fates towards adipocyte lineage. Toxicol Appl Pharmacol. 2017;329:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taxvig C, Dreisig K, Boberg J, et al. Differential effects of environmental chemicals and food contaminants on adipogenesis, biomarker release and PPARγ activation. Mol Cell Endocrinol. 2012;361 (1-2): 106–115. [DOI] [PubMed] [Google Scholar]
- 63.Pereira-Fernandes A, Demaegdt H, Vandermeiren K, et al. Evaluation of a screening system for obesogenic compounds: screening of endocrine disrupting compounds and evaluation of the PPAR dependency of the effect. PLoS One. 2013;8(10):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kostadinova R, Wahli W, Michalik L. PPARs in diseases: control mechanisms of inflammation. Curr Med Chem. 2005;12(25):2995–3009. [DOI] [PubMed] [Google Scholar]
- 65.Chen J, Ahn KC, Gee NA, Gee SJ, Hammock BD, Lasley BL. Antiandrogenic properties of parabens and other phenolic containing small molecules in personal care products. Toxicol Appl Pharmacol. 2007;221(3):278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Patel SM, Ratcliffe SJ, Reilly MP, et al. Higher serum testosterone concentration in older women is associated with insulin resistance, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2009;94(12):4776–4784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Oh J-Y, Barrett-Connor E, Wedick NM, Wingard DL. Endogenous sex hormones and the development of type 2 diabetes in older men and women: the Rancho Bernardo Study. Diabetes Care. 2002;25(1):55–60. [DOI] [PubMed] [Google Scholar]
- 68.Laughlin GA, Goodell V, Barrett-Connor E. Extremes of endogenous testosterone are associated iwth increased risk of incident coronary events in older women. J Clin Endocrinol Metab. 2010;95(2):740–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rexrode KM, Manson JAE, Lee IM, et al. Sex hormone levels and risk of cardiovascular events in postmenopausal women. Circulation. 2003;108(14):1688–1693. [DOI] [PubMed] [Google Scholar]
- 70.Grodin JM, Siiteri PK, MacDonald PC. Source of estrogen production in postmenopausal women. J Clin Endocrinol Metab. 1973;36(2):207–214. [DOI] [PubMed] [Google Scholar]
- 71.Lønning PE, Dowsett M, Powles TJ. Postmenopausal estrogen synthesis and metabolism: Alterations caused by aromatase inhibitors used for the treatment of breast cancer. J Steroid Biochem. 1990;35(3-4):355–366. [DOI] [PubMed] [Google Scholar]
- 72.Key TJ, Appleby PN, Reeves GK, et al. Circulating sex hormones and breast cancer risk factors in postmenopausal women: reanalysis of 13 studies. Br J Cancer. 2011;105(5):709–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang YW, Stern B, Rebar RW. Endocrine comparison of obese menstruating and amenorrheic women. J Clin Endocrinol Metab. 1984;58(6):1077–1083. [DOI] [PubMed] [Google Scholar]
- 74.Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354(3):270–282. [DOI] [PubMed] [Google Scholar]
- 75.Hatch EE, Nelson JW, Stahlhut RW, Webster TF. Association of endocrine disruptors and obesity: perspectives from epidemiologic studies. Int J Androl. 2011;33(2):324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Du X, Goodwin JS. Increase of chemotherapy use in older women with breast carcinoma from 1991-1996. Cancer. 2001;92(4):730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Meeker JD, Cantonwine DE, Rivera-González LO, et al. Distribution, variability, and predictors of urinary concentrations of phenols and parabens among pregnant women in Puerto Rico. Environ Sci Technol. 2013;47(7):3439–3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Philippat C, Wolff MS, Calafat AM, et al. Prenatal exposure to environmental phenols: concentrations in amniotic fluid and variability in urinary concentrations during pregnancy. Environ Health Perspect. 2013;121(10):1225–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Smith KW, Braun JM, Williams PL, et al. Predictors and variability of urinary paraben concentrations in men and women, including before and during pregnancy. Environ Health Perspect. 2012;120(11):1538–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Engel LS, Buckley JP, Yang G, et al. Predictors and variability of repeat measurements of urinary phenols and parabens in a cohort of Shanghai women and men. Environ Health Perspect. 2014;122(7):733–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.