Abstract
Arthritis remains a widespread and yet unsolved therapeutic dilemma. Cartilage grafting has proven to be difficult and satisfactory results are often elusive. There are several inherent difficulties. These include both chondrocyte migration and the lack of sufficient uptake of nutrients to allow for graft survival. With autografts, there is also the paucity of symptom-free donor sites. Accordingly, multiple alternative therapies for cartilage regeneration and/or substitution have been developed over time. In this article, the authors shall discuss the options for the treatment of damaged cartilage with a focus on the cartilage grafting techniques.
Keywords: arthritis, cartilage implantation, upper extremity
Arthritis is a leading cause of disability in the United States. It affects ∼54 million adults and treatment options are scarce. Generally, the repair of cartilage is difficult and most treatments are aimed at addressing symptoms rather than the actual repair of the damaged cartilage. In this article, we shall discuss the options for the treatment of damaged cartilage with a focus on the cartilage grafting techniques. 1
Skin, bone, and fat grafting are procedures common to the field of plastic surgery and have reliable results. In contrast, cartilage grafting has proven to be difficult and satisfactory results are often elusive. There are several inherent difficulties. These include both chondrocyte migration and the lack of sufficient uptake of nutrients to allow for graft survival. With autografts, there is also the paucity of symptom-free donor sites. Accordingly, multiple alternative therapies for cartilage regeneration and/or substitution have been developed over time. By far, the vast majority of data in cartilage grafting comes from its use in the knee.
Alternative Treatments
One of the most common joints where articular cartilage defects are found and treated via grafting techniques is in the knee, where symptomatic cartilage defects can cause disability comparable to advanced knee osteoarthritis. 2 3 It is important to note that not all articular cartilage defects are symptomatic; therefore, a thorough assessment of other potential etiologies for knee pain must be undertaken in patients who present with cartilage defects. 2 Many different treatment strategies have been proposed and utilized for cartilage defects in the knee. Conservative treatment in the form of physical therapy (particularly for defects in the patellofemoral compartment) is typically utilized for a period of at least 3 to 6 months. This is done in conjunction with weight loss and activity modification. A trial of intra-articular corticosteroid injection or viscosupplementation therapy is also often used, especially in patients who are within a few years of being “age-eligible” for knee replacement surgery. Surgical treatment is only considered after failure of the aforementioned conservative modalities in patients with symptomatic full-thickness (grade 3 or 4) cartilage defects. After any cartilage repair procedure, patients will likely undergo extensive rehabilitation and will have restrictions for a prolonged period of time. Therefore, preoperative patient counseling is important to establish realistic expectations. 2
Multiple studies have analyzed treatment strategies for cartilage repair and have concluded that the location and size of the defect are the most important considerations, followed by age as a second-tier consideration. 2 4 5 In the tibiofemoral compartment (femoral condyle), smaller lesions (< 4 cm 2 ) can be treated with either autologous chondrocyte implantation (ACI) or microfracture (which involves making multiple small holes in the surface of the joint to stimulate a healing response) with similar outcomes. 2 6 Abrasion arthroplasty is another technique used for small cartilage defects in the femoral condyle. This technique is thought to induce marrow stimulation and healing, but instead of drills or wires (as used in the microfracture technique), high-speed burrs are used to remove the damaged cartilage and reach the subchondral bone. 2 7 Larger lesions (> 4 cm 2 ) have shown poor results with microfracture/abrasion arthroplasty and tend to do better after ACI. 2 6 8 Another treatment modality which has shown good results for small cartilage lesions (< 4 cm 2 ) in the femoral condyle is osteochondral autograft transfer (which involves harvesting an osteochondral plug from a less–weight-bearing area of the patient's knee and placing it in the defect). 2 9 10 For larger lesions in the femoral condyle (> 4 cm 2 ), osteochondral autograft transfer can be associated with substantial donor-site morbidity; therefore, ACI or osteochondral allograft transplantation (OATS procedure) is often used. OATS involves an osteochondral plug allograft (as opposed to autograft) being used to fill the defect, thus eliminating the potential donor-site morbidity seen with autograft procedures ( Fig. 1 ). 2 7
Fig. 1.
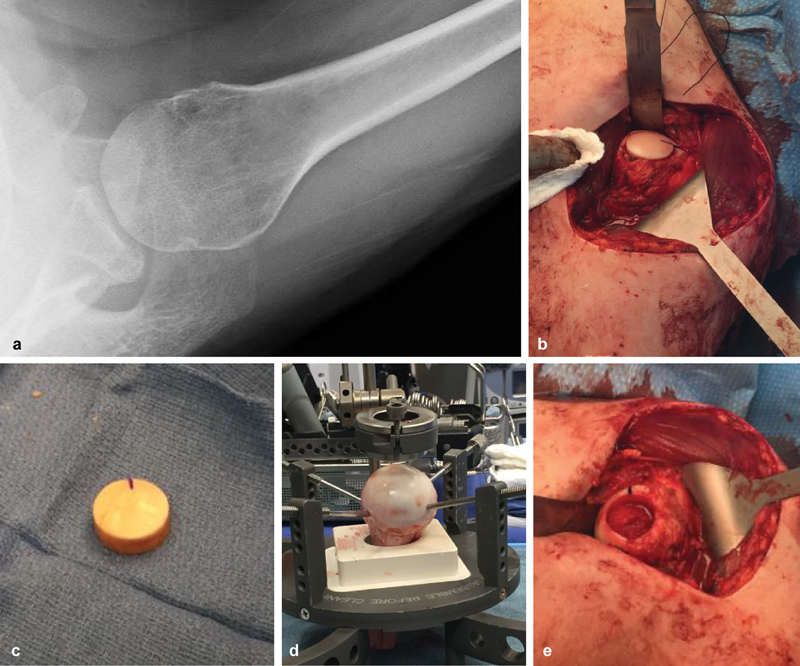
( a–e ) Humeral head osteochondral allograft.
In the patellofemoral compartment, results of microfracture, osteochondral autograft transfer, and osteochondral allograft transplantation have not been as good as in the femoral condyles. 2 4 5 Initially, ACI also showed poor results for cartilage defects in the patellofemoral compartment. 2 11 However, recent studies have shown successful outcomes of ACI in the patellofemoral compartment in > 80% of patients, likely due to better understanding of patellofemoral joint biomechanics and more aggressive treatment of patellar tracking abnormalities. 2 12 13
Finally, in older patients with pre-existing arthritis or multiple, wide-spread cartilage defects, arthroplasty (in the form of patellofemoral arthroplasty, unicompartmental knee arthroplasty, or total knee arthroplasty) may be the best surgical treatment modality. 2 14 The choice among these procedures is based primarily on the location of diseased cartilage.
Autologous Cartilage Implantation
Cartilage grafting attempts to solve the dilemma of cartilage damage by attempting to repair the cartilage defect. By taking autologous grafts, the theory is that there is a combination of both the requisite growth factors and viable mesenchymal stem cells to produce sufficient replacement cartilage ( Fig. 2 ). 15
Fig. 2.
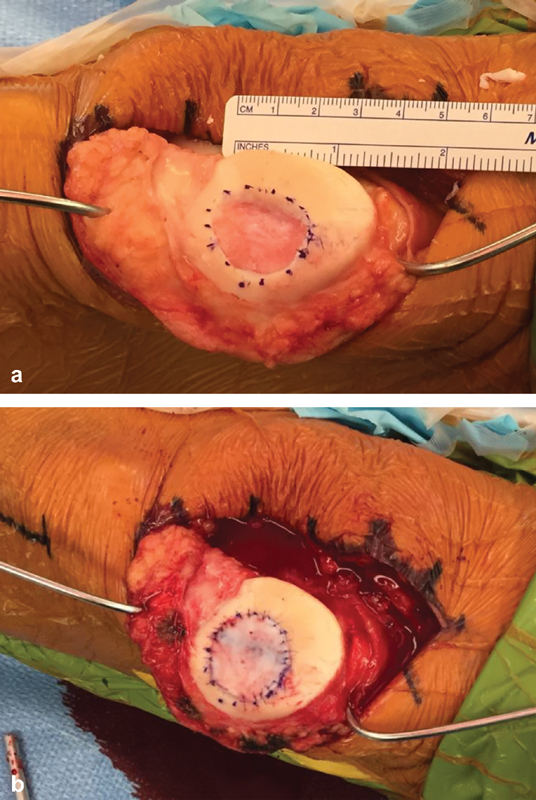
( a,b ) ACI of the patella.
Cultured autografts are familiar to plastic surgeons due to the frequent use of cultured epithelial autografts in burn care. Cartilage grafting outcomes were improved using a similar technique. Brittberg's landmark article in the New England Journal of Medicine had “good” or “excellent” outcomes in femoral condylar grafts in five out of seven patients. These patients experienced improved knee function after patellar grafting. Their technique including harvesting cartilage slices from a non–weight-bearing portion of the knee for culture. Two to three weeks after the initial surgery, a second surgery was performed where the cultured autografts were implanted into the knee. A periosteal flap was then used to cover the site of grafting. 11
There have been modifications to the technique since then. The periosteal flap has the disadvantage of requiring an open procedure and the added surgical pain to the patient. Minimal alteration of the native knee architecture would be ideal in the treatment algorithm. In an attempt to do this, a novel technique utilizing a collagen bilayer was evaluated in six patients. Results after at least 6-month follow-up revealed good results with no complications. 16 Yet another technique utilized hyaluronic acid support in combination with an arthoscopic, rather than open approach. Both techniques were found to decrease the length of surgery. 17
Another consideration is the addition of a matrix that is used to more evenly distribute the chondrocytes in the recipient site. This technique, called matrix-induced ACI (MACI), has been used with nice success.
The need for two surgeries has been challenged as well. There is a belief that the need for two surgeries will obviate the widespread use of the procedure. 18 Animal studies using minced cartilage have shown to treat chondral defects in just 6 months. This technique is being used in humans, though outcome studies are sparse. 19
Early results have been promising but sparse. Interestingly there has been data that show the cartilage in the regenerated tissue resembles hyaline. 20 There has been great interest in the combination of growth factors that are optimal for cartilage growth and repair. With a more refined application of this knowledge we may be able to create an ideal nonsurgical injectable to encourage the growth and repair in patients with cartilage defects and the risk of development of severe arthritis. 15
Conclusion
When there are a multitude of treatment options for a given disease, it generally means that a demonstrably superior method has not been discovered yet. Arthritis remains a widespread and yet unsolved therapeutic dilemma. While there is unlikely to be a magic bullet, cartilage grafting has promising initial results and additional basic science and clinical research is warranted. Its use has become more widespread in the treatment of cartilage defects about the knee, but applications for the upper extremity are likely to expand as we gain more knowledge and experience with the technology.
Footnotes
Conflict of Interest None declared.
References
- 1.Arthritis facts. Available at:https://www.arthritis.org/about-arthritis/understanding-arthritis/arthritis-statistics-facts.php. Accessed Feb 17, 2019
- 2.Gomoll A H, Farr J, Gillogly S D, Kercher J, Minas T. Surgical management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92(14):2470–2490. [PubMed] [Google Scholar]
- 3.Heir S, Nerhus T K, Røtterud J H et al. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med. 2010;38(02):231–237. doi: 10.1177/0363546509352157. [DOI] [PubMed] [Google Scholar]
- 4.Kreuz P C, Steinwachs M R, Erggelet C et al. Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage. 2006;14(11):1119–1125. doi: 10.1016/j.joca.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 5.Bentley G, Biant L C, Carrington R W et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2003;85(02):223–230. doi: 10.1302/0301-620x.85b2.13543. [DOI] [PubMed] [Google Scholar]
- 6.Knutsen G, Engebretsen L, Ludvigsen T C et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86-A(03):455–464. doi: 10.2106/00004623-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Godin J A, Sanchez G, Cinque M E, Chahla J, Kennedy N I, Provencher M T. Osteochondral allograft transplantation for treatment of medial femoral condyle defect. Arthrosc Tech. 2017;6(04):e1239–e1244. doi: 10.1016/j.eats.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basad E, Ishaque B, Bachmann G, Stürz H, Steinmeyer J. Matrix-induced autologous chondrocyte implantation versus microfracture in the treatment of cartilage defects of the knee: a 2-year randomised study. Knee Surg Sports Traumatol Arthrosc. 2010;18(04):519–527. doi: 10.1007/s00167-009-1028-1. [DOI] [PubMed] [Google Scholar]
- 9.Gudas R, Kalesinskas R J, Kimtys V et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21(09):1066–1075. doi: 10.1016/j.arthro.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Hangody L, Kish G, Kárpáti Z, Szerb I, Udvarhelyi I. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1997;5(04):262–267. doi: 10.1007/s001670050061. [DOI] [PubMed] [Google Scholar]
- 11.Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331(14):889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 12.Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463(463):187–194. [PubMed] [Google Scholar]
- 13.Minas T, Bryant T. The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res. 2005;(436):30–39. doi: 10.1097/01.blo.0000171916.40245.5d. [DOI] [PubMed] [Google Scholar]
- 14.Everhart J S, Abouljoud M M, Kirven J C, Flanigan D C. Full-thickness cartilage defects are important independent predictive factors for progression to total knee arthroplasty in older adults with minimal to moderate osteoarthritis: data from the osteoarthritis initiative. J Bone Joint Surg Am. 2019;101(01):56–63. doi: 10.2106/JBJS.17.01657. [DOI] [PubMed] [Google Scholar]
- 15.Fortier L A, Barker J U, Strauss E J, McCarrel T M, Cole B J. The role of growth factors in cartilage repair. Clin Orthop Relat Res. 2011;469(10):2706–2715. doi: 10.1007/s11999-011-1857-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cherubino P, Grassi F A, Bulgheroni P, Ronga M. Autologous chondrocyte implantation using a bilayer collagen membrane: a preliminary report. J Orthop Surg (Hong Kong) 2003;11(01):10–15. doi: 10.1177/230949900301100104. [DOI] [PubMed] [Google Scholar]
- 17.Marcacci M, Zaffagnini S, Kon E, Visani A, Iacono F, Loreti I. Arthroscopic autologous chondrocyte transplantation: technical note. Knee Surg Sports Traumatol Arthrosc. 2002;10(03):154–159. doi: 10.1007/s00167-001-0275-6. [DOI] [PubMed] [Google Scholar]
- 18.Lohmander L S.Tissue engineering of cartilage: do we need it, can we do it, is it good and can we prove it? Novartis Found Symp 20032492–10., discussion 10–16, 170–174, 239–241 [PubMed] [Google Scholar]
- 19.Lu Y, Dhanaraj S, Wang Z et al. Minced cartilage without cell culture serves as an effective intraoperative cell source for cartilage repair. J Orthop Res. 2006;24(06):1261–1270. doi: 10.1002/jor.20135. [DOI] [PubMed] [Google Scholar]
- 20.Peterson L, Minas T, Brittberg M, Nilsson A, Sjögren-Jansson E, Lindahl A. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res. 2000;(374):212–234. doi: 10.1097/00003086-200005000-00020. [DOI] [PubMed] [Google Scholar]


