Abstract
This study investigated whether insecure attachment is associated with poorer outcomes at 6‐month follow‐up in adolescents who self‐harm. At baseline the Child Attachment Interview was administered to 52 adolescents (13‐17 years) referred to specialist child and adolescent mental health services and with a recent history of self‐harm. Participants also completed self‐report measures of self‐harm, peer attachment, anxiety, and depression and were administered the means end problem‐solving task. Self‐harm behavior and problem‐solving skills were assessed again at 6‐month follow‐up. At baseline, 14 (27%) were securely attached to their mothers. In the 49 (94%) adolescents followed‐up, those with insecure maternal attachment and insecure peer attachment were more likely to have repeated self‐harm. In addition, securely attached adolescents showed greater improvement in problem‐solving skills. These findings indicate that secure maternal and peer attachments may help recovery from self‐harm, possibly by supporting the acquisition of problem‐solving skills, and highlights the importance of social connections and attachments for youth with a history of self‐harm.
Self‐harm refers to intentional self‐poisoning or self‐injury with a nonfatal outcome, irrespective of whether the individual intends to die (National Collaborating Centre for Mental Health, 2011). This definition recognizes that suicidal intent may be low but not absent in many acts of self‐harm (Hjelmeland et al., 2002) and that suicidal intentions underlying some self‐harm behaviors may be mixed, unclear, or even unknown to individuals (Hawton, Cole, O'Grady, & Osborn, 1982). Self‐harm is a significant public health problem across the world and has considerable impact on the lives of the individual, their family, and on health services.
At present, rates of self‐harm are highest in young people (Bergen, Hawton, Waters, Cooper, & Kapur, 2010). Large community‐based surveys within Europe reveal that approximately 10% of adolescents report having self‐harmed in their lifetime (Hawton, Rodham, Evans, & Weatherall, 2002; Madge et al., 2008). Furthermore, these surveys indicate repetition of self‐harm is common; over half of adolescents who had self‐harmed reported multiple episodes. There are, however, limits to the inferences that can be made from such cross‐sectional or retrospective studies. Prospective studies are likely to provide more robust and reliable information about repetition of self‐harm (Hawton, Bergen, et al., 2012). In one of the few studies to prospectively examine the prevalence of self‐harm in the community, O'Connor, Rasmussen, and Hawton (2009) found that 6.2% of 15‐ to 16‐year‐olds reported self‐harm over 6 months, with 2.6% having self‐harmed for the first time, and 3.6% with a repeat episode. Prospective studies monitoring adolescent presentations of self‐harm in hospitals suggest that approximately 15% of adolescents carry out a further act within the following year (Hawton, Hall, et al., 2003), with up to 27% repeating self‐harm when followed‐up over a minimum of 2 years (Hawton, Bergen, et al., 2012). However, findings from hospital‐admission studies are based on records of individuals who have reattended hospital following self‐harm and are likely to reflect an underestimate (Hawton, Saunders, & O'Connor, 2012).
It is crucial to consider why some adolescents repeat self‐harm as repetition may reflect ongoing or recurrent distress and places greater demands on clinical services (Hawton, Kingsbury, Steinhardt, James, & Fagg, 1999), and importantly, a history of self‐harm is the strongest predictor of completed suicide (Hawton, Zahl, & Weatherall, 2003). The need to reduce the risk of suicide in key high‐risk groups, such as those with a history of self‐harm, is a target outlined in the most recent UK government suicide prevention strategy (Department of Health, 2012). However, relatively few studies have prospectively investigated the extent to which psychosocial and psychological factors are predictive of repeat self‐harm behavior among adolescents (Fliege, Lee, Grimm, & Klapp, 2009). Prospective research suggests that family dysfunction and poor parental mental health are risk factors for repeated self‐harm (Chitsabesan, Harrington, Harrington, & Tomenson, 2003; O'Connor et al., 2009); however, little attention has been paid to the role of attachment in repetition of self‐harm.
Attachment theory argues that infants are biologically programmed to form an emotional bond with their caregiver (Bowlby, 1969/1982), and an attachment figure should act to provide physical security and comfort to an otherwise helpless infant. For securely attached infants, the caregiver will be available and responsive in times of stress and the caregiver provides a “secure base” from which to explore the environment. This exploration promotes the development of emotion‐regulation, self‐confidence, and problem‐solving skills. Furthermore, favorable interactions with the attachment figure lead to the development of positive representations of the self, of others, and of relationships (Bowlby, 1973). These competencies are believed to increase children's adaptation to the world around them and are thought to continue to influence adjustment throughout the life span.
It is proposed that an insecure attachment style can develop when a primary caregiver is insensitive or inconsistent in responding to the child in times of need, predisposing children to become either preoccupied with maintaining contact or disengaging with the caregiver. Insecure attachment styles can, therefore, impede socioemotional development and the development of effective coping strategies and problem‐solving skills needed in challenging situations (Mikulincer, Shaver, & Pereg, 2003).
Although Bowlby's early work was criticized for potentially blaming mothers (Mead, 1954), careful longitudinal research has confirmed the contribution of the quality of the child's attachment relationship with the caregiver to children's long‐term developmental outcomes (Sroufe, Egeland, Carlson, & Collins, 2005). Studies investigating the contribution of genetic and environmental influences to individual differences in attachment in infants and toddlers have found evidence for an environmental, rather than genetic, influence on attachment, as predicted by attachment theory (e.g., O'Connor & Croft, 2001). A recent twin study (Fearon, Shmueli‐Goetz, Viding, Fonagy, & Plomin, 2014), however, has confirmed a significant genetic influence on adolescent attachment; for attachment classification (secure vs. insecure), 35% of the variability was found to be attributable to genes. These findings suggest that a child's inherited characteristics play a role in their attachment status in adolescence; it is possible that the child's temperamental characteristics evoke changes in the sensitivity of care provided by the caregiver, which influences security of attachment in the child–caregiver relationship. Hence, parent effects, child effects, and bi‐directional parent–child effects may all play a role.
Insecure attachment has been related with self‐harm behavior in adolescent clinical samples (Adam, Sheldon‐Keller, & West, 1996), and prospective, longitudinal research has shown insecure attachment to be a significant risk factor for self‐harm in community samples of adolescents (Fergusson, Woodward, & Horwood, 2000; Salzinger, Rosario, Feldman, & Ng‐Mak, 2007) and young adults (Sroufe et al., 2005). Adolescents with insecure attachment styles demonstrate more dysfunctional anger and avoidance of problem solving during discussions with parents (Kobak, Cole, Ferenz‐Gillies, Fleming, & Gamble, 1993) and develop maladaptive ways of coping with negative emotions (Seiffge‐Krenke, 2006). Furthermore, adolescent self‐harm is associated with poorer problem‐solving skills (Pollock & Williams, 2004).
To our knowledge, however, no published research has explored longitudinally the role of attachment in relation to the course of self‐harm in a clinical sample of young people with a history of self‐harm. If self‐harm can be seen as “extreme attachment behavior” (Adam et al., 1996, p. 265) produced in response to threats in order to signal distress and the need for caregiving, it can be theorized that adolescents with secure attachment will have caregivers and peers who will recognize this distress and therefore this behavior will elicit appropriate concern, help, and support. That is, following an incident of self‐harm, sensitive caregivers may become more attentive to their child's needs, or more protective, creating a “safe” environment and encouraging the child to develop more adaptive methods of coping with distress. Thus, securely attached adolescents would be expected to have better outcomes in terms of self‐harm behavior and problem solving.
In this study we aimed to investigate the role of insecure parental and peer attachment in relation to outcomes for self‐harm over a 6‐month period among a high‐risk group of clinically referred adolescents with a history of self‐harm. We also examined whether adolescents classified as having insecure parental attachment have poorer outcomes in terms of problem solving and attendance with clinic appointments at 6‐month follow‐up.
Method
Participants
Adolescents aged 12 to 17 years referred to specialist child and adolescent mental health services (CAMHS), with a history of self‐harm behavior within the last year were eligible. Those adolescents referred following accidental self‐harm were excluded from the study.
Design and Recruitment
This was a longitudinal study with assessments at baseline and 6‐month follow‐up. Participants were invited to take part in the study before a routine psychosocial assessment conducted by a specialist CAMHS professional following emergency treatment for self‐harm or at a CAMHS clinic appointment. If the researcher was unable to meet with participants, CAMHS staff gave out information packs and collected contact details on the researcher's behalf.
Baseline Measures
Attachment
The Child Attachment Interview (CAI; Target, Fonagy, & Shmueli‐Goetz, 2003) was administered. This semistructured interview asks about current experiences with, and perceptions of, attachment figures. Questions are designed to tap into the adolescent's self‐representation and representation of his or her caregivers, particularly during situations in which the attachment system is thought to be activated (e.g., emotional upset, conflict, distress, illness, hurt, separation, and loss).
The interview, conducted by a trained rater, is filmed and later transcribed verbatim; relevant nonverbal behaviors are noted where appropriate (e.g., marked anxiety and maintenance of eye contact). Transcripts of the interview and nonverbal behavior are coded according to nine scales (Preoccupied Anger, Idealization, Dismissal, Disorganization, Overall Coherence, Emotional Openness, Use of Examples, Balance of Positive/Negative References to Attachment Figures, and Resolution of Conflict) and based on these ratings a main attachment style can be assigned for the mother and father independently: secure attachment or an insecure attachment style (dismissing, preoccupied, or disorganized). All interviews were conducted and coded by the same accredited researcher (KG), who was trained by the developers to 85% agreement over 20 cases for the secure–insecure split for maternal attachment (κ = .7).
The CAI was originally designed for use with individuals aged 8 to 12 years but has since been adapted and used with adolescents up to 17 years of age (Scott, Briskman, Woolgar, Humayun, & O'Connor, 2011) using age appropriate language. For participants in foster care, the modified CAI for adolescents in care was administered. The CAI has demonstrated sound psychometric properties, with good criterion validity, discriminant validity, and test–retest reliability at 1 year (Shmueli‐Goetz, Target, Fonagy, & Datta, 2008).
To establish peer attachment styles, participants completed The Attachment Questionnaire for Children (AQC; Muris, Mayer, & Meesters, 2000). This consists of three descriptions relating to relationships with close friends. Respondents endorse the description that matches their peer relationships most closely giving classifications of secure, insecure‐avoidant, or insecure‐ambivalent peer attachment. Muris, Meesters, van Melick, and Zwambag (2001) found this brief measure has demonstrated good concurrent validity with the Inventory of Parent and Peer Attachment (Armsden & Greenberg, 1987).
Anxiety and Depression
Participants completed the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983). The HADS is a well‐validated measure of anxiety and depression in clinically referred adolescents (White, Leach, Sims, Atkinson, & Cottrell, 1999). It has 14 items (seven for anxiety, e.g., “I feel tense or wound up”; seven for depression, e.g., “I feel as if I am slowed down”) each with a 4‐point verbal rating scale scored from 0 to 3, giving total scores ranging from 0 to 21 for each subscale. Negative items are recoded so that high scores indicate high levels of distress. The HADS demonstrates sound internal consistency; Cronbach's α of between .78 and .93 have been reported for the anxiety subscale and between .82 and .90 for the depression subscale (Mykletun, Stordal, & Dahl, 2001).
Self‐Harm
The self‐harm questionnaire was developed from the questions used in Hawton et al.'s (2002) large school‐based survey investigating self‐harm in adolescence. In the original school study, participants were asked to describe in their own words what they had done to harm themselves. From this, the authors were able to determine whether this met one of the predetermined criteria for self‐harm. In this study, we used the same criteria and created a list of self‐harm behaviors. Instructions asked participants to indicate yes or no as to whether they have engaged in the methods of self‐harm behaviors with the intention to harm (e.g., “Have you ever poisoned yourself?” “Have you ever taken more than the recommended dose of a drug?” “Have you ever burned yourself with something?”). Participants were also asked to indicate how frequently they had engaged in self‐harm in their lifetime (once/2–5 times/6–10 times/11–15 times/over 15 times).
Informal and Formal Support
Participants were asked to indicate whom they felt they go to talk about things that really bother them (mother/father/brother or sister/another relative/friends/teacher/member of staff at CAMHS/somebody else [e.g., a boyfriend or girlfriend]). The number of sources of support selected was summed and higher scores indicated a greater number of perceived individuals available for help. This measure was also used in Hawton et al.'s large school survey (Evans, Hawton, & Rodham, 2005) but was adapted for the clinical sample in this study to include the response option “a member of staff at CAMHS.”
Problem‐Solving Abilities
The means end problem‐solving task (MEPS; Platt & Spivack, 1975), a performance‐based test of general social problem solving, was used. Participants are presented with scenarios that begin with a protagonist needing or wanting something and end with this need being satisfied by him or her. Participants complete the story by generating potential solutions that could have occurred between the goal being presented and being reached. Individuals are assessed on their ability to appraise the given problem and identify steps or “means” that would adequately result in the given resolution. The MEPS has been used to assess problem solving in adolescents with a history of self‐harm (Orbach et al., 2007).
This study used a shortened version of the MEPS designed for use with adolescents (Hawton et al., 1999). Solutions were scored according to the guidelines developed by Steinhardt, Hawton, and Kingsbury (1999). We present findings from the “total relevant means” subscale, which refers to the sum of all steps in the story that are relevant to the story process. The MEPS was scored by one of two independent coders. To assess interrater reliability, both coded approximately 10% of the MEPS and across the five stories intra‐class correlations ranged from .74–.93 for the “total relevant means” scores.
Participants also completed questions on their current living situation, previous living situation, and family affluence (Family Affluence Scale II, Boyce, Torsheim, Currie, & Zambon, 2006).
Outcome Measures
Self‐Harm
The self‐report self‐harm behavior measure was adapted to collect information about self‐harm in the 6 months since baseline.
Problem‐Solving Abilities
The MEPS was readministered at 6‐month follow‐up. Differences in scores from baseline to follow‐up were calculated for total relevant means scores to give “change in total relevant means” as an outcome variable.
Attendance at Clinical Services
The proportion of scheduled CAMHS appointments (including assessment and treatment sessions) attended during the 6‐month follow‐up period was recorded from RiO, the mental health electronic patient record system.
Procedure
At the baseline assessment, informed parental consent and participant assent from adolescents under 16 years of age were obtained. Participant consent was obtained for adolescents aged 16 or older. The CAI was then administered and subsequently participants completed the measures of peer attachment, anxiety and depression, sources of help, and self‐harm behaviors via a computer‐assisted self interview, as research has shown that adolescents feel more comfortable revealing sensitive information, such as mental health problems, to a computer (Parkin, 2000). Lastly, participants completed the MEPS, which was administered face‐to‐face by the researcher.
At the follow‐up assessment, 6 months later, participants completed the problem‐solving task again as well as the self‐harm measure adapted for follow‐up.
Attachment interviews were coded blind to outcomes. Repeat referrals to CAMHS following emergency treatment for self‐harm and appointment attendance were recorded from RiO once the coding of the CAIs was complete.
This study received ethical approval from the “East Midlands—Nottingham 2” NHS Research Ethics Committee.
Statistical Analyses
Maternal attachment and peer attachment classifications were dichotomized into secure attachment (0) and insecure attachment (1) for univariate and multivariate analyses. The self‐harm variable was dichotomized into no self‐harm behavior (0) and self‐harm behavior (1). Multivariable logistic regression (enter method) was used to examine those factors that independently and most strongly predicted self‐harm behavior at 6‐month follow‐up. Covariates were age, gender, maternal attachment, peer attachment, and levels of previous self‐harm at baseline and baseline levels of anxiety and depression. Multicollinearity checks were run on all predictor variables used in the regression analyses. Correlations between variables were less than .7, variation inflation factor scores were below 2.2, and tolerance statistic values were above .5, indicating that there were no strong correlations between predictors in the regression model.
Results
During the study period of April 20, 2010–June 29, 2011, 91 adolescents agreed to receive information about the study and supplied contact details, of whom 52 (3 males) consented and were recruited to the study. Consenters were older (median age 15 [IQR = 15–16] vs. 15 [IQR = 14–15]; Z = −2.63, p = .009), although there was no difference in gender between consenters and dissenters. As recruitment was through CAMHS staff, it is not known how many young people were approached who declined to supply contact information.
The final sample consisted of 49 young people who had been assessed following emergency treatment for self‐harm and three young people who had been referred to Tier three Community CAMHS and had disclosed a history of self‐harm (see Table 1 for sample demographics).
Table 1.
Baseline Sample Demographics
| Total sample (N = 52) | |
|---|---|
| Gender | |
| Female n (%) | 49 (94) |
| Median age (IQR) | 15 (15–16) |
| Mean Family Affluence Scale score (SD) | 4.37 (1.75) |
| Parental separation | |
| Yes n (%) | 39 (75) |
| Living situation | |
| With both parents n (%) | 12 (23) |
| With one parent n (%) | 30 (58) |
| With relative n (%) | 5 (10) |
| In foster care n (%) | 4 (7) |
| Other n (%) | 1 (2) |
| Currently or previously spent time living with someone other than a birth parent (e.g., relative and family friend) | |
| Yes n (%) | 20 (39) |
| History with services | |
| Total referrals to tier 3 specialist CAMHS at baseline assessment | |
| One n (%) | 26 (50) |
| Two n (%) | 10 (19) |
| Three or more n (%) | 16 (31) |
| Total referrals to tier 3 specialist CAMHS for assessment following emergency treatment for self‐harm at baseline assessment (%) | |
| None n (%) | 2 (4) |
| One n (%) | 41 (80) |
| Two n (%) | 2 (12) |
| Three or more n (%) | 2 (4) |
SD, standard deviation; IQR, interquartile range; CAMHS, child and adolescent mental health services.
The most frequently endorsed methods of self‐harm were self‐poisoning (n = 44, 85%), self‐cutting (n = 39, 77%), and battering or hitting oneself (n = 29, 57%). Three quarters of participants (n = 39, 75%) had scores of 8 or above on the anxiety subscale of the HADS, indicating probable clinical anxiety, while a third (n = 17, 33%) had scores of 8 or above on the depression subscale of the HADS, indicating probable clinical depression. A third of participants (n = 17, 33%) met the criteria for probable clinical depression and anxiety.
Parental Attachment Style
Thirty‐seven participants (71%) were classified as insecurely attached to their mother. One participant did not provide sufficient information to be able to assign an attachment style for maternal attachment.
The Relationship Between Maternal Attachment Style and Study Variables at Baseline
At the time of interview, many participants (40%) had infrequent or no contact with their biological father. No participants classified as insecurely attached to their mother had a secure attachment to someone else (including father, a grandparent, or foster carer). Therefore, attachment style to the mother (secure/insecure) was used as the independent variable. Participants classified as securely attached did not differ in terms of age, gender, and self‐reported family affluence from those classified as insecurely attached.
Securely attached participants had greater levels of social support (Z = −2.34, p = .019) and were more likely to report having their mother, χ2(1) = 12.4, p ≤ .001, a sibling, χ2(1) = 4.01, p = .045, and their friends, χ2(1) = 5.26, p = .022, as a source of support, compared to insecurely attached participants. Insecurely attached participants reported greater levels of current depression, t(49) = −1.72, p = .035, and a greater frequency of previous self‐harm behavior, median = 2–5 times vs. 6–10 times; χ2(1) = 4.44, p = .034. Over half of the sample (n = 28, 56%) reported having attempted suicide. Securely attached adolescents were as likely as insecurely attached adolescents to endorse having made a suicide attempt. There were no differences between the groups in terms of self‐reported secure peer attachment [n = 5 (36%) vs. n = 17 (46%)]. There were also no differences between the securely attached group and the insecurely attached group in terms of “total mean” scores on the MEPS (Table 2).
Table 2.
The Relationship Between Attachment Style and Study Variables at Baseline
| Secure attachment (n = 14) | Insecure attachment (n = 37) | Significance level | |
|---|---|---|---|
| Hospital Anxiety and Depression Scale | |||
| Median anxiety score (IQR) | 10.5 (5.75–12) | 11.73 (8.5–14.5) | .165 |
| Mean depression score (SD) | 4.85 (2.34) | 6.84 (4.10) | .035* |
| Sources of support endorsed | |||
| Mother n (%) | 11 (79) | 9 (24) | <.001*** |
| Father n (%) | 2 (14) | 4 (11) | .731 |
| Brother/sister n (%) | 6 (43) | 6 (16) | .045* |
| Another relative n (%) | 6 (43) | 16 (43) | .980 |
| Friends n (%) | 13 (93) | 22 (60) | .022* |
| Teacher n (%) | 2 (14) | 7 (19) | .699 |
| Member of staff at CAMHS n (%) | 4 (29) | 9 (24) | .756 |
| Somebody else n (%) | 7 (50) | 25 (68) | .247 |
| Median Total Support (IQR) | 3.5 (2.75–4.25) | 3 (2–3) | .019* |
| Peer attachment | |||
| Secure n (%) | 5 (36) | 17 (46) | .510 |
| Means end problem‐solving task | |||
| Mean total means score (SD) | 3.53 (0.91) | 3.76 (1.92) | .664 |
Note. CAMHS, child and adolescent mental health services; IQR, interquartile range.
***p < .001; *p ≤ .05.
Six‐Month Follow‐up
Forty‐nine (94%) participants completed the study tasks at Time 2. The three nonresponders were females with two classified as having secure maternal attachment and another insecure maternal attachment at baseline. None of these participants had been assessed by CAMHS following emergency treatment for self‐harm in the 6‐month follow‐up period.
The Role of Attachment in Repetition of Self‐Harm
Two thirds of participants engaged in one or more episodes of self‐harm at follow‐up and significantly more were classified as having insecure maternal attachment at baseline, χ2(1) = 5.46, p = .019. Therefore, 78% (28/36) of all participants classified as insecurely attached repeated self‐harm behavior during the study period. In comparison, 42% (5/12) of the securely attached group went on to repeat self‐harm (see Figure 1). A slightly greater proportion of insecurely attached participants had been assessed following emergency treatment for self‐harm during the study period [n = 6 (17%), vs. n = 1 (8%)], although this difference was not statistically significant.
Figure 1.
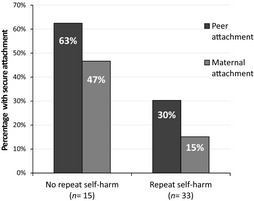
Proportion of secure maternal and peer attachments among those who did not self‐harm during follow‐up and those who did self‐harm.
Bivariate associations indicate that repeated self‐harm was related to greater levels of baseline self‐harm, χ2(1) = 5.10, p = .024; depression, t(44.7) = −2.52, p = .015; and anxiety (Z = −2.12, p = .034) and peer attachment, χ2(1) = 4.62, p = .032, but was not related to age and gender.
In the multivariable logistic regression model, insecure maternal attachment (OR = 7.80, 95% CI 1.15, 52.91) and poor peer attachment (OR = 8.01, 95% CI 1.00, 64.20) independently predicted self‐harm at follow‐up (Table 3). Age, gender, previous self‐harm, and levels of anxiety and depression at baseline were not independently associated with the outcome.
Table 3.
Multivariate Logistic Regression Predicting Repetition of Self‐Harm at Time 2
| B | Unadjusted odds ratio | Adjusted odds ratio (95% confidence interval) | p value | |
|---|---|---|---|---|
| Age | −0.07 | 0.83 (0.48–1.44) | 0.93 (0.46–1.91) | .850 |
| Gender | −20.50 | 0.00 | 0.00 | .999 |
| Self‐harm at baseline | −0.02 | 1.66 (1.05–2.01) | 0.98 (0.52–1.84) | .941 |
| Maternal attachment at baseline a | 2.06 | 4.90 (1.22–19.69) | 7.80 (1.15–52.91) | .035* |
| Peer attachment at baseline a | 2.08 | 3.83 (1.09–13.45) | 8.01 (1.00–64.20) | .050* |
| Levels of anxiety at baseline | −0.004 | 1.19 (1.00–1.43) | 1.00 (0.75–1.32) | .977 |
| Levels of depression at baseline | 0.10 | 1.23 (1.00–1.52) | 1.01 (0.82–1.47) | .520 |
Note. R 2 = .29 (Cox & Snell), .41 (Nagelkerke). Model χ2(2) = 16.57, p = .020.
*p ≤ .05.
aHigher score indicates insecure attachment.
The Role of Attachment in Improvement in Problem Solving
Overall, participants classified as having secure attachment showed greater improvement in problem‐solving skills at follow‐up, producing on average one extra step toward the resolution of the problem, t(43) = 2.33, p = .027 (Table 4).
Table 4.
Outcome Variables at 6‐Month Follow‐up
| Secure attachment group (n = 12) | Insecure attachment group (n = 36) | Significance level | |
|---|---|---|---|
| Self‐harm behavior | |||
| Yes n (%) | 5 (42) | 28 (78) | .019* |
| Means end problem‐solving task | |||
| Mean change in total means score n (SD) | 1.0 (1.78) | −0.05 (1.70) | .027* |
| Scheduled CAMHS appointments | |||
| Median number of appointments planned (IQR) | 4.0 (1.0–5.5) | 7.5 (3.25–15.5) | .029* |
| Median proportion of appointments attended (IQR) | 0.79 (0.25–1.0) | 0.75 (0.53–1.0) | .872 |
Note. CAMHS, child and adolescent mental health services; IQR, interquartile range.
*p ≤ .05.
The Role of Attachment in Attendance at Clinical Services
Participants with insecure maternal attachment had a greater number of appointments (which included both assessment and treatment sessions) scheduled with specialist CAMHS during the 6‐month study period (Z = −2.18, p = .029; Table 4). However, there was no difference in the proportion of sessions attended by participants with and without secure maternal attachment. Findings show that those participants with insecure maternal attachment were more likely to be in contact with specialist CAMHS at follow‐up [n = 18 (50%) vs. n = 1 (8%); p = .016].
Discussion
During this study we investigated the role of attachment in predicting outcomes for clinically referred adolescents who have self‐harmed; a hitherto neglected area of research. The findings demonstrated that both insecure maternal and peer attachments independently predicted repeated self‐harm at follow‐up, while other known correlates of self‐harm behavior (age and levels of previous self‐harm, anxiety, and depression symptoms) were not associated with repetition of self‐harm once attachment was accounted for. Furthermore, of the seven participants who required clinical assessment by CAMHS following emergency treatment for self‐harm during the follow‐up period, six were classified as having insecure attachment. In addition, participants who were insecurely attached were more likely to be in contact with specialist CAMHS at follow‐up, perhaps indicating ongoing distress. These findings build on previous prospective longitudinal research that has demonstrated insecure attachment is associated with self‐harm behavior in young people (Fergusson et al., 2000; Salzinger et al., 2007; Sroufe et al., 2005).
While there were no differences between securely and insecurely attached participants in problem‐solving skills at baseline, participants classified as having secure attachment showed improvements in problem solving at follow‐up. They produced on average one whole extra step toward the resolution of the problems presented. It is possible that participants with secure attachments had caregivers who recognized their self‐harm as a signal of distress and this behavior elicited appropriate concern, help, and support, including encouraging the child to develop more adaptive methods of coping. Adolescents report that the behavior of parents can influence further self‐harming (Yip, Ngan, & Lam, 2003) and future research could use qualitative methods to explore adolescents' perceptions of caregivers' role in aiding the development of constructive problem‐solving skills following self‐harm.
Furthermore, research has shown that genes may play a significant role in adolescent attachment (Fearon et al., 2014) and it is possible that the child's genetic propensities and temperament evoke changes in the sensitivity of care provided by the caregiver. It is therefore important to consider that the relationship between attachment and outcomes for self‐harm and problem solving may not just be accounted for by parent effects, but also child effects and bidirectional parent–child effects.
Our findings indicate that insecurely attached adolescents could particularly benefit from problem‐solving therapy and attachment‐based therapy in combination. Problem‐solving therapy has been shown to improve problem‐solving skills in adults who self‐harm (Townsend et al., 2001) and a recent randomized controlled trial (RCT) has indicated that dialectical behavior therapy for adolescents (DBT‐A), which in part aims to enhance skills to cope with intense emotions that may precede self‐harm, is effective for adolescent self‐harm behavior (Mehlum et al., 2014). To date, few RCTs of family‐based interventions have been conducted for adolescents who self‐harm; however, results from these are promising. Attachment‐based family therapy (ABFT) focuses on strengthening parent–adolescent attachment bonds to create a protective and secure base for adolescent development. It works to improve parent–adolescent communication and the adolescent's confidence in the parent's availability and support. Furthermore, it aims to improve the family's capacity for problem solving, affect regulation, and organization in an attempt to strengthen family cohesion. An RCT by Diamond et al. (2010) demonstrated that adolescents who received ABFT reported significantly greater and more rapid reductions in suicidal ideation during the treatment period compared with those adolescents receiving Enhanced Usual Care (a facilitated referral process with ongoing clinical monitoring). This was supported by clinician ratings of the adolescents' suicidal ideation. Furthermore, while there was no difference between the two groups in rate of change from the endpoint (12 weeks) to follow‐up (24 weeks), those in the ABFT group still reported significantly less suicidal ideation at follow‐up. In addition, mentalization‐based treatment (MBT), which is grounded in attachment theory, has been shown to be more effective than routine care in reducing repeat self‐harm in a clinical sample of adolescents; MBT produced a recovery rate of 44% versus 17% for the treatment‐as‐usual group (Rossouw & Fonagy, 2012). The mechanism of change was attributable to improved mentalization and reduced attachment avoidance.
No relationship was found between attachment style and the number of scheduled clinical appointments attended but it may be that electronic records of service uptake, although more accurate than participant recall, are not a sensitive marker for engagement with treatment. However, clinical record data revealed that participants with insecure maternal attachment had more appointments scheduled with specialist CAMHS during the follow‐up period compared to those with secure attachment. This could be indicative of greater clinical need or a slower response to treatment.
A large proportion (67%) of participants reported repeated self‐harm behavior during the 6‐month study period. However, only seven participants were assessed by specialist CAMHS following emergency treatment for self‐harm during this period, suggesting that episodes are often unknown to clinical services. Many of the studies that have prospectively studied self‐harm among adolescents who have received emergency treatment for self‐harm have relied on hospital records to determine repetition of self‐harm. The discrepancy between self‐report data and hospital admissions for self‐harm found in this study illustrates the limitations of relying on hospital data alone.
Baseline data also suggested a difference between the securely and insecurely attached participants in frequency of previous self‐harm behavior. Furthermore, analysis of individual sources of support revealed that securely attached individuals were more likely than insecurely attached participants to report their mother, their siblings, and their friends as someone they could talk to. This is in line with previous research that indicates that adolescents who have self‐harmed on only one occasion are more able to talk to relatives and friends than adolescents who have engaged in multiple episodes of self‐harm (Evans et al., 2005). It is possible that in this study having a greater range of individuals to turn to for help among securely attached participants contributed toward better outcomes in terms of self‐harm behavior. Furthermore, the greater endorsement of maternal support by participants classified as securely attached provides validity for the secure–insecure attachment classifications assigned.
To date, no published research has explored the role of attachment in a clinical sample of adolescents who have self‐harmed using an attachment interview that is suitable for adolescents. The attachment interview is considered the “gold standard” in attachment research; however, previous research in this domain has relied on assessing attachment styles through a self‐report measure of attachment (e.g., West, Spreng, Rose, & Adam, 1999) or an attachment interview designed for adults (e.g., Adam et al., 1996). One novel aspect of this study, therefore, was that adolescent attachment classifications were assigned based on narratives produced during a reliable and valid interview specifically designed for young people.
Furthermore, a considerable strength of this study was the high number of participants (94%) retained at 6‐month follow‐up. Longitudinal studies are necessary to investigate the course of complex behavior patterns such as self‐harm, yet research with psychologically vulnerable or transient populations is often limited by high rates of attrition (Kleschinsky, Bosworth, Nelson, Walsh, & Shaffer, 2009). Attrition can compromise the external validity of study findings and high follow‐up rates allow greater confidence that the findings are representative of the whole sample and more generalizable.
Limitations
The longitudinal design of this observational study allows inferences to be made regarding the association between attachment and outcomes for self‐harm and problem solving. However, without a randomized experimental design, it is not possible to infer a causal relationship. It was not possible to measure, and control for, all factors that may have affected the outcome of self‐harm and problem solving, and it is possible that there may be some residual confounding.
The present study was limited by a modest sample size and the possibility that participants may not be representative of all adolescents who self‐harm. In particular, there were very few males in this study and the findings might not generalize to males. The female:male ratio among adolescents assessed by the CAMHS self‐harm team during the study period was 10:1. The ratio in this sample was 17:1; therefore, males were further under represented. This research should be repeated with a sample of males to determine whether these findings are generalizable to both genders.
A single researcher (KG) administered the Child Attachment Interviews and coded all transcripts. Although the researcher is a certified reliable coder, having passed the reliability test, this does not protect against rater drift in reliability. Furthermore, as this sample of adolescents contained individuals with elevated levels of depression and anxiety, there is the potential that level of distress impacted attachment classification. It is noted, however, that unlike self‐report measures of attachments, the CAI does not directly assess participants' interpretations of their caregivers and examines coherence, inconsistencies, and contradictions within the narrative. Furthermore, the CAI was developed for use with clinical samples. In addition, actual distress was not the strongest predictor of self‐harm (as measured by levels of anxiety and depression), which would be expected if it played a greater contribution than attachment styles to repeated self‐harm.
Implications for Future Research and Clinical Practice
The finding that insecure maternal attachment and insecure peer attachment are associated with future self‐harm has important implications in research and clinical work. Future research could build on these findings by investigating the relationship between attachment and future self‐harm in a large cohort study. Within such a study, it would be important to examine outcomes for those with high levels of repeat self‐harm behavior and those who have experienced living in foster care or residential care homes. Furthermore, an attachment‐based intervention study with people who have self‐harmed for the first time could help shed light on causal relationships.
Peer and maternal attachment classifications could also be routinely used to help inform assessment and treatment for adolescents who have self‐harmed. Insecure attachment is a potentially useful marker of risk of future self‐harm and it could be that combined attachment‐based and problem‐solving interventions are particularly effective for insecurely attached adolescents who have self‐harmed, but this requires further investigation.
Conclusion
This study offers novel insights into the role of attachment in outcomes for self‐harm and problem solving among clinically referred adolescents who have self‐harmed. There were high rates of insecure attachment within this sample and this is of concern as insecurely attached participants were found to be at greater risk of repeated self‐harm and showed less improvement in problem solving.
We thank the young people for their participation, and Marie Armstrong and CAMHS staff who assisted with recruitment.
References
- Adam, K. S. , Sheldon‐Keller, A. , & West, M. (1996). Attachment organization and history of suicidal behavior in clinical adolescents. Journal of Consulting and Clinical Psychology, 64, 264–272. [DOI] [PubMed] [Google Scholar]
- Armsden, G. C. , & Greenberg, M. T. (1987). The Inventory of Parent and Peer Attachment: Individual differences and their relationship to psychological well‐being in adolescence. Journal of Youth and Adolescence, 16, 427–454. [DOI] [PubMed] [Google Scholar]
- Bergen, H. , Hawton, K. , Waters, K. , Cooper, J. , & Kapur, N. (2010). Epidemiology and trends in non‐fatal self‐harm in three centres in England: 2000–2007. The British Journal of Psychiatry, 197, 493–498. [DOI] [PubMed] [Google Scholar]
- Bowlby, J. (1969/1982). Attachment and loss: Vol.1. Attachment (2nd ed.). New York: Basic Books. (Original work published 1969) [Google Scholar]
- Bowlby, J. (1973). Attachment and loss: Vol. 2. Separation: Anxiety and anger. New York, NY: Basic Books. [Google Scholar]
- Boyce, W. , Torsheim, T. , Currie, C. , & Zambon, A. (2006). The Family Affluence Scale as a measure of national wealth: Validation of an adolescent self‐report measure. Social Indicators Research, 78, 473–487. [Google Scholar]
- Chitsabesan, P. , Harrington, R. , Harrington, V. , & Tomenson, B. (2003). Predicting repeat self‐harm in children. European Child and Adolescent Psychiatry, 12, 23–29. [DOI] [PubMed] [Google Scholar]
- Department of Health . (2012). Preventing suicide in England: A cross‐government outcomes strategy to save lives. London: Author. [Google Scholar]
- Diamond, G. S. , Wintersteen, M. B. , Brown, G. K. , Diamond, G. M. , Gallop, R. , Shelef, K. , & Levy, S. (2010). Attachment‐based family therapy for adolescents with suicidal ideation: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 49, 122–131. [DOI] [PubMed] [Google Scholar]
- Evans, E. , Hawton, K. , & Rodham, K. (2005). In what ways are adolescents who engage in self‐harm or experience thoughts of self‐harm different in terms of help‐seeking, communication and coping strategies? Journal of Adolescence, 28, 573–587. [DOI] [PubMed] [Google Scholar]
- Fearon, R. , Shmueli‐Goetz, Y. , Viding, E. , Fonagy, P. , & Plomin, R. (2014). Genetic and environmental influences on adolescent attachment. Journal of Child Psychology and Psychiatry, 55, 1033–1041, doi: 10.1111/jccp.12171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson, D. M. , Woodward, L. J. , & Horwood, L. J. (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine, 30, 23–39. [DOI] [PubMed] [Google Scholar]
- Fliege, H. , Lee, J. R. , Grimm, A. , & Klapp, B. F. (2009). Risk factors and correlates of deliberate self‐harm behavior: A systematic review. Journal of Psychosomatic Research, 66, 477–493. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Bergen, H. , Kapur, N. , Cooper, J. , Steeg, S. , Ness, J. , & Waters, K. (2012). Repetition of self‐harm and suicide following self‐harm in children and adolescents: Findings from the Multicentre Study of Self‐harm in England. Journal of Child Psychology and Psychiatry, 53, 1212–1219. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Cole, D. , O'Grady, J. , & Osborn, M. (1982). Motivational aspects of deliberate self‐poisoning in adolescents. The British Journal of Psychiatry, 141, 286–291. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Hall, S. , Simkin, S. , Bale, L. , Bond, A. , Codd, S. , & Stewart, A. (2003). Deliberate self‐harm in adolescents: A study of characteristics and trends in Oxford, 1990–2000. Journal of Child Psychology and Psychiatry, 44, 1191–1198. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Kingsbury, S. , Steinhardt, K. , James, A. , & Fagg, J. (1999). Repetition of deliberate self‐harm by adolescents: The role of psychological factors. Journal of Adolescence, 22, 369–378. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Rodham, K. , Evans, E. , & Weatherall, R. (2002). Deliberate self harm in adolescents: Self report survey in schools in England. British Medical Journal, 325, 1207–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton, K. , Saunders, K. E. A. , & O'Connor, R. C. (2012). Self‐harm and suicide in adolescents. The Lancet, 379, 2373–2382. [DOI] [PubMed] [Google Scholar]
- Hawton, K. , Zahl, D. , & Weatherall, R. (2003). Suicide following deliberate self‐harm: Long‐term follow‐up of patients who presented to a general hospital. The British Journal of Psychiatry, 182, 537–542. [DOI] [PubMed] [Google Scholar]
- Hjelmeland, H. , Hawton, K. , Nordvik, H. , Bille‐Brahe, U. , Leo, D. D. , Fekete, S. , et al. (2002). Why people engage in parasuicide: A cross‐cultural study of intentions. Suicide and Life‐Threatening Behavior, 32, 380–393. [DOI] [PubMed] [Google Scholar]
- Kleschinsky, J. H. , Bosworth, L. B. , Nelson, S. E. , Walsh, E. K. , & Shaffer, H. J. (2009). Persistence pays off: Follow‐up methods for difficult‐to‐track longitudinal samples. Journal of Studies on Alcohol and Drugs, 70, 751–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak, R. R. , Cole, H. E. , Ferenz‐Gillies, R. , Fleming, W. S. , & Gamble, W. (1993). Attachment and emotion regulation during mother‐teen problem solving: A control theory analysis. Child Development, 64, 231–245. [PubMed] [Google Scholar]
- Madge, N. , Hewitt, A. , Hawton, K. , Wilde, E. J. , Corcoran, P. , Fekete, S. , et al. (2008). Deliberate self‐harm within an international community sample of young people: Comparative findings from the Child & Adolescent Self‐harm in Europe (CASE) Study. Journal of Child Psychology and Psychiatry, 49, 667–677. [DOI] [PubMed] [Google Scholar]
- Mead, M. (1954). Some theoretical considerations on the problem of mother‐child separation. American Journal of Orthopsychiatry, 24, 471. [DOI] [PubMed] [Google Scholar]
- Mehlum, L. , Tørmoen, A. J. , Ramberg, M. , Haga, E. , Diep, L. M. , Laberg, S. , et al. (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self‐harming behavior: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53, 1082–1091. [DOI] [PubMed] [Google Scholar]
- Mikulincer, M. , Shaver, P. R. , & Pereg, D. (2003). Attachment theory and affect regulation: The dynamics, development, and cognitive consequences of attachment‐related strategies. Motivation and Emotion, 27(2), 77–102. [Google Scholar]
- Muris, P. , Mayer, B. , & Meesters, C. (2000). Self‐reported attachment style, anxiety, and depression in children. Social Behavior and Personality, 28(2), 157–162. [Google Scholar]
- Muris, P. , Meesters, C. , van Melick, M. , & Zwambag, L. (2001). Self‐reported attachment style, attachment quality, and symptoms of anxiety and depression in young adolescents. Personality and Individual Differences, 30, 809–818. [Google Scholar]
- Mykletun, A. , Stordal, E. , & Dahl, A. A. (2001). Hospital Anxiety and Depression (HAD) scale: Factor structure, item analyses and internal consistency in a large population. The British Journal of Psychiatry, 179, 540–544. [DOI] [PubMed] [Google Scholar]
- National Collaborating Centre for Mental Health . (2011). Self‐harm: Longer term management. NICE Clinical Guidance 133. London: National Institute for Clinical Excellence. [Google Scholar]
- O'Connor, T. G. , & Croft, C. M. (2001). A twin study of attachment in preschool children. Child Development, 72, 1501–1511. [DOI] [PubMed] [Google Scholar]
- O'Connor, R. , Rasmussen, S. , & Hawton, K. (2009). Predicting deliberate self‐harm in adolescents: A 6‐month prospective study. Suicide and Life‐Threatening Behavior, 39, 364–375. [DOI] [PubMed] [Google Scholar]
- Orbach, I. , Blomenson, R. , Mikulincer, M. , Gilboa‐Schechtman, E. , Rogolsky, M. , & Retzoni, G. (2007). Perceiving a problem‐solving task as a threat and suicidal behavior in adolescents. Journal of Social and Clinical Psychology, 26, 1010–1034. [Google Scholar]
- Parkin, A. (2000). Computers in clinical practice: Applying experience from child psychiatry. British Medical Journal, 321, 615–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt, J. J. , & Spivack, G. (1975). Manual for the Means‐End Problem‐Solving Procedure (MEPS): A measure of interpersonal cognitive problem‐solving skill. Philadelphia, PA: Department of Mental Health Sciences, Hahnemann Medical College and Hospital. [Google Scholar]
- Pollock, L. R. , & Williams, J. M. G. (2004). Problem‐solving in suicide attempters. Psychological Medicine, 34, 163–167. [DOI] [PubMed] [Google Scholar]
- Rossouw, T. I. , & Fonagy, P. (2012). Mentalization‐based treatment for self‐harm in adolescents: A randomized controlledtrial. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 1304–1313. [DOI] [PubMed] [Google Scholar]
- Salzinger, S. , Rosario, M. , Feldman, R. S. , & Ng‐Mak, D. S. (2007). Adolescent suicidal behavior: Associations with preadolescent physical abuse and selected risk and protective factors. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 859–866. [DOI] [PubMed] [Google Scholar]
- Scott, S. , Briskman, J. , Woolgar, M. , Humayun, S. , & O'Connor, T. G. (2011). Attachment in adolescence: Overlap with parenting and unique prediction of behavioural adjustment. Journal of Child Psychology and Psychiatry, 52, 1052–1062. [DOI] [PubMed] [Google Scholar]
- Seiffge‐Krenke, I. (2006). Coping with relationship stressors: The impact of different working models of attachment and links to adaptation. Journal of Youth and Adolescence, 35, 24–38. [Google Scholar]
- Shmueli‐Goetz, Y. , Target, M. , Fonagy, P. , & Datta, A. (2008). The Child Attachment Interview: A psychometric study of reliability and discriminant validity. Developmental Psychology, 44, 939–956. [DOI] [PubMed] [Google Scholar]
- Sroufe, L. A. , Egeland, B. , Carlson, E. , & Collins, W. A. (2005). The development of the person: The Minnesota study of risk and adaptation from birth to adulthood. New York, NY: Guilford. [Google Scholar]
- Steinhardt, K. , Hawton, K. , & Kingsbury, S. (1999). The Means‐End Problem Solving Procedure (MEPS) for assessing problem‐solving skills: The development of scoring guidelines. Unpublished manuscript.
- Target, M. , Fonagy, P. , & Shmueli‐Goetz, Y. (2003). Attachment representations in school‐age children: The development of the Child Attachment Interview (CAI). Journal of Child Psychotherapy, 29, 171–186. [Google Scholar]
- Townsend, E. , Hawton, K. , Altman, D. , Arensman, E. , Gunnell, D. , Hazell, P. , et al. (2001). The efficacy of problem‐solving treatments after deliberate self‐harm: Meta‐analysis of randomized controlled trials with respect to depression, hopelessness and improvement in problems. Psychological Medicine, 31, 979–988. [DOI] [PubMed] [Google Scholar]
- West, M. , Spreng, S. W. , Rose, S. M. , & Adam, K. S. (1999). Relationship between attachment‐felt security and history of suicidal behaviours in clinical adolescents. Canadian Journal of Psychiatry, 44, 578–582. [DOI] [PubMed] [Google Scholar]
- White, D. , Leach, C. , Sims, R. , Atkinson, M. , & Cottrell, D. (1999). Validation of the Hospital Anxiety and Depression Scale for use with adolescents. The British Journal of Psychiatry, 175, 452–454. [DOI] [PubMed] [Google Scholar]
- Yip, K. , Ngan, M. , & Lam, I. (2003). A qualitative study of parental influence and response to adolescents' self‐cutting in Hong Kong. Families in Society, 84, 405–416. [Google Scholar]
- Zigmond, A. S. , & Snaith, R. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. [DOI] [PubMed] [Google Scholar]


