Abstract
Background and Purpose
People with multiple sclerosis (PwMS) experience falls, usually when walking and transferring. The aim was to investigate if walking distance and patient overestimate of walking distance are predictors of falls in PwMS.
Methods
A prospective study was conducted, with a single test occasion followed by prospective registration of falls for 3 months. All PwMS in Region Örebro County with a previously registered Expanded Disability Status Scale score between 3.0 and 7.0 in the Swedish MS Registry were invited to participate (n = 149). Altogether, data from 49 PwMS being relapse free for at least 3 months and with a confirmed Expanded Disability Status Scale between 1.5 and 7.0 upon study entry were analysed.
Results
Twenty‐two PwMS (45%) fell during the study period, providing information of 66 falls. Walking distance or overestimate of one's walking distance, as compared with test results, did not predict falls in this MS sample.
Discussion
Walking and standing activities are associated with numerous falls in PwMS. Our data do not clearly support routine measurements of walking distance in assessing individual fall risk. © 2015 The Authors. Physiotherapy Research International published by John Wiley & Sons, Ltd.
Keywords: falls, multiple sclerosis, prediction, walking
Introduction
Many people with multiple sclerosis (PwMS) experience falls (Cattaneo et al., 2002; Finlayson et al., 2006; Nilsagard et al., 2009b; Kasser et al., 2011; Matsuda et al., 2011; Prosperini et al., 2011; Coote et al., 2013; Gunn et al., 2013a), and falls often occur when walking and transferring (Cattaneo et al., 2002; Finlayson et al., 2006; Nilsagard et al., 2009a; Matsuda et al., 2011). Gait impairment (Benedetti et al., 1999, Martin et al., 2006) and fall tendency are present early in the disease course (Moen et al., 2011). Reduced stride length, prolonged double support phase, altered muscular recruitment and reduced speed have been reported in people with mild MS, that is values between 0 and 2.5 according to the Expanded Disability Status Scale (EDSS) (Benedetti et al., 1999; Martin et al., 2006). Being able to walk longer distances is required for many everyday tasks and participation in society. Increased dependency in self‐care, mobility and domestic life are reported as associated with a shorter distance covered during the 6‐minute walk test (6MWT) (Paltamaa et al., 2007). The importance of walking distance is also recognized when determining MS severity using scales, such as EDSS (Kurtzke, 1983).
The presence of motor, sensor or cognitive symptoms have been suggested to be associated with falls in PwMS (Cattaneo et al., 2002; Finlayson et al., 2006; Nilsagard et al., 2009a; Nilsagard et al., 2009b; Cameron and Wagner, 2011; Kasser et al., 2011; Matsuda et al., 2011; Prosperini et al., 2011; Prosperini et al., 2013; Sosnoff et al., 2013), and these symptoms may also impact walking ability. Kasser and co‐workers reported that temporo‐spatial changes were frequent in recurrent fallers (Kasser et al., 2011), while D'Orio reported a significant correlation (r = 0.39) between walking speed and falls (D'Orio et al., 2012). Walking capacity is increasingly limited with more advanced MS, displayed as a changed gait pattern and reduced speed (Kelleher et al., 2010). Moreover, the need for a walking aid increases in the progressive phase of the disease. An association between use of mobility aid and falls has been reported in a recently published meta‐analysis (Gunn et al., 2013b).
Although falls and fall tendency are associated with disease severity (Nilsagard et al., 2009b; Moen et al., 2011; Prosperini et al., 2011; Sosnoff et al., 2012; Prosperini et al., 2013), people with moderate mobility restrictions are reported to fall more frequently than those with modest or severe mobility restrictions (Matsuda et al., 2012).
The high frequency of falls and fallers in the MS community stresses the need for accurate clinical assessment tools in identifying potential fallers. For example, a possible association between walking distance, as a measure of endurance, and fall risk is yet to be evaluated. Until now, the association between walking ability and fall risk has been investigated using different scales (Cattaneo et al. 2002; Nilsagard et al., 2009b) or by temporal–spatial parameters of gait (Kasser et al. 2011). Actual walking distance is rarely measured in clinical practise. Instead, one relies on patient self‐estimation. Reduced muscular endurance has been recognized by PwMS as an increasing fall risk and being aware of one's limits is identified as a strategy to prevent falls (Nilsagard et al., 2009a). In the present study, we investigated if walking distance and patient estimate of walking distance are possible predictors of fall in PwMS. We hypothesized that reduced walking distance and overestimation of walking distance would be associated with falls.
Methods
Design
A prospective study was conducted, with a single test occasion followed by prospective registration of falls for 3 months.
Outcome variable
Self‐reported falls defined as ‘any unexpected event resulting in the person landing on the floor or lower level’ (Lamb et al., 2005). A faller was defined by reporting ≥1 fall during a 3‐month period.
Predictor variables
The 6MWT has been recommended as a measure of performance of walking endurance in PwMS (Goldman et al., 2010; Motl et al., 2013). The distance covered reduces with increasing EDSS, but the test is well tolerated also with more severe walking disability (Goldman et al., 2008; Motl et al., 2012). The 6MWT incorporates both anaerobic and aerobic work, with steady state reached the last three minutes (Motl et al., 2012).The 6MWT correlates well with self‐reported perceived limitations of walking capacity (Goldman et al., 2008) and balance confidence (Wetzel et al., 2011), and intra‐rater and inter‐rater reliability are reported as excellent (Intraclass Correlation Coefficient 0.95 and 0.91, respectively). The study participants were encouraged to walk as fast they could back and forth in a quiet hallway with a 30‐m interval for a maximum of 15 minutes. No encouragement was given during the test procedure and sitting rest was not allowed, according to the description by Goldman et al. (Goldman et al., 2008). Distance was measured at 6 minutes (6MWT) and after 15 minutes (if able to walk ≥15 minutes) or when the participant had reached his or her maximal distance within the predetermined time limit. Walking distance was measured using a minimum of walking device in accordance with the EDSS grading. A correct patient self‐estimate of maximal walking distance was defined as an agreement between estimated and actually measured distance walked ±10% (Ringel and Zettl, 2006).
Ethical consideration
The study was approved by the Regional Ethics Committee in Uppsala, Sweden (2012/077), and followed the Helsinki Declaration. The participants gave written‐informed consent.
Subjects
All PwMS who were resident in Region Örebro County and with a previously registered EDSS between 3.0 and 7.0 in the Swedish MS Registry were invited to participate (n = 149). Inclusion criteria were the following: 1) relapse‐free for at least 3 months prior to study entry; 2) able to understand verbal and written information and 3) preserved ability to walk with or without use of walking devices. The exclusion criterion was the following: other diseases or conditions with impact on walking ability (for example other neurological diseases, severe ischemic heart disease and orthopaedic conditions).
Out of 149 eligible PwMS, 54 accepted to participate and were initially believed to fulfil the criteria. As discovered during the test procedure, two of them were not able to walk and one did not fulfil the diagnostic criteria for MS. Another two did not return any fall diaries. Thus, the final sample consisted of 49 PwMS (Table 1). Fall data were obtained for 49, 47 and 46 PwMS in the first, second and third month, respectively. Data regarding fall circumstances were missing in two cases.
Table 1.
Demographics and sample characteristics for the entire MS sample and for non‐fallers and fallers separately
| Variable | Total (n = 49) | Non‐faller (n = 27) | Faller (n = 22) | |
|---|---|---|---|---|
| Age, years : mean; | 55.6 (11) | 54.1 (11) | 57.5 (10) | |
| SD range | 22; 73 | 22; 70 | 32; 73 | |
| Sex (frequency) | Male | 11 (22%) | 7 (26%) | 4 (18%) |
| Female | 38 (78%) | 20 (74%) | 18 (82%) | |
| BMI : mean; SD | 26 (4) | 27 (5) | 26 (4) | |
| EDSS median, (25–75% IQR) | 4.5 (4.0–6.5) | 4.5 (4.0–6.5) | 5.0 (4.0–6.5) | |
| MS subtype (frequency) | RRMS | 21 (43%) | 13 (48%) | 8 (36%) |
| SPMS/PPMS | 28 (57%) | 14 (52%) | 14 (64%) | |
| SDMT score: | n = 48 | n = 26 | ||
| mean; SD | 41 (14) | 44 (15) | 38 (12) | |
| Cognitive dysfunction (PASAT): n = 44 | Yes | 22 (46%) | 12 (44%) | 10 (46%) |
| Cognitive dysfunction(FSMC): (frequency) | None or mild (≤52) | 7 (14%) | 2 (7%) | 5 (23%) |
| Moderate or Severe (≥53) | 42 (86%) | 25 (93%) | 17 (77%) | |
| Walk aid (frequency) | Yes | 17 (35%) | 8 (30%) | 9 (40%) |
| Maximal walk test (metres): | ||||
| mean; SD | 531 (452) | 607 (506) | 438 (366) | |
| median; range | 374 (5; 1530) | 381 (34; 1530) | 278 (5; 1239) | |
| 6‐minute walk test (metres): | n = 43 | n = 23 | n = 20 | |
| mean, SD | 316 (145) | 355 (154) | 272 (121) | |
| median; range | 314 (5; 616) | 374 (70; 616) | 270 (5; 513) | |
| Overestimated walking distance(frequency) | 10 (20%) | 5 (18%) | 5 (23%) | |
| MSWS‐12 score | ||||
| (0–100): mean, SD | 63 (28) | 60 (31) | 66 (23) | |
| median; range | 69 (42–88) | 69 (33–88) | 70 (47–83) | |
n = 49 (27:22) unless otherwise stated. EDSS = Expanded Disability Status Scale; IQR = inter‐quartile range; BMI = Body Mass Index; SPMS = secondary progressive MS; PPMS = primary progressive MS; FSMC = Fatigue Scale for Motor and Cognitive Functions; SDMT = Symbol Digit Modalities Test; PASAT = Paced Auditory Serial Addition Test; MSWS‐12 = 12‐item Multiple Sclerosis Scale; RRMS = Relapsing‐remitting MS.
Procedure
The testing procedure was performed at Örebro University Hospital using standardized protocols. Neurological examination was performed for re‐assessment and validation of the previously registered EDSS score. The neurologist asked the participants to estimate the distance they could walk at their best, in accordance with EDSS‐rating procedure, and noted the exact estimation. Furthermore, data on demographics and medical history, such as disease phenotype, were collected. To further describe the sample and to collect data on possible confounders, measures of cognitive processing speed previously related to falls in MS were used (D'Orio et al., 2012; Sosnoff et al., 2013). Firstly, the Symbol Digit Modality Test (SDMT) that measures the number of correct number–geometric symbol pairings provided for 90 seconds (Smith, 1982). Secondly, the Paced Auditory Serial Addition Test (PASAT‐3) that requires the person to add auditory presented digits to a proceeding given digit and verbally state the sum (Rao, 1990). The number of correct given answers forms a score. To describe the perceived limitations of walking due to MS, the 12‐item MS Walking Scale score (0–100) was used, and higher scores indicate more pronounced perceived limitations (Hobart et al., 2003). Finally, the Fatigue Scale for Motor and Cognitive Functions (FSMC) was used (Penner et al., 2009).
Thereafter, a physiotherapist experienced in neurology assessed the walking ability and handed out a falls diary with the instruction to register falls during a 3‐month period. Additional information (location, time of day, activity and injuries) was filled in for each fall. An upper limit for reporting was set to four falls per month for the participants' convenience. The diaries were returned on a monthly basis and if not received by the physiotherapist, reminder phone calls and letters were applied.
Statistical procedure
Logistic regression analyses were performed with fallen/not fallen as dependent variable and for each predictor variable. The results are presented as Odds ratios (OR) with 95% confidence intervals, p‐values and area under the receiving operating curve with 95% confidence intervals. ORs for continuous variables with large heterogeneity were calculated and divided with 100 to illustrate the risk if increased by one step (100 m) for walking test performance. p‐values, OR and area under the receiving operating curve are based on original values and not on stratified groups. The Statistical Package for the Social Sciences, version 15.0 (SPSS Inc., Chicago, IL, USA) was used to analyse the data.
Results
Altogether, 22 PwMS (47%) were classified as fallers, providing information of 66 falls in total. Fourteen (29%) reported two falls or more. The mean score of perceived limitation in walking measured using the MSWS‐12 was 63 (SD 28) (Table 1). Only two had primary progressive MS (one faller and one non‐faller), and only one used a unilateral walk aid (faller). Twenty‐one PwMS (43%) estimated their maximal walking distance correctly (within ±10%): 11 (41%) fallers and 10 (46%) non‐fallers, while 18 PwMS (37%) underestimated their maximal walking distance: 11 (41%) fallers and 7 (32%) non‐fallers.
Fifteen falls were reported to result in minor injuries (pain, bruise and wound). The majority of falls occurred in the afternoon (12.00–17.59 pm; n = 35), while falls were more rare in the hours 06.00–11.59 am (n = 17) and 18.00–23.59 pm (n = 10). Only one fall occurred between 24.00 and 05.59 am. Forty‐seven of the falls occurred at home (inside or outside). The most common activities performed when falling were walking (n = 17), turning (n = 12), transferring (n = 11) and standing (n = 6). The falls were primarily reported to be caused by loss of balance (n = 32), followed by legs gave away (n = 9), fatigue (n = 9), distraction (n = 6) and dizziness (n = 4). Three falls each were caused by stumbling, slipping, reduced vision or when affected by heat. Seven falls occurred in public buildings, six on driveway or lawn, three on the street and three in a shop.
Data were available for 43 PwMS who completed the 6MWT. The ORs for the investigated variables were non‐significant (Table 2 and Figure 1). The 6MWT was near significant (p = 0.066) suggesting that if the distance walked during 6 minutes increases with 100 metres, the risk of being classified as a faller is reduced by 36%.
Table 2.
Odds Ratio, p‐value and area under the receiving operating curve with 95% confidence intervals for walk test data and overestimation of walking distance
| Variable | Valuea | no. of fallers (%) | Faller OR (95%CI) | p‐value | AUROC (95%CI) |
|---|---|---|---|---|---|
| Maximal walk test (/100 m) | 0.05–<2.43 | 9 (53) | |||
| 2.43–<6.5 | 7 (44) | ||||
| 6.5–15.3 | 6 (38) | 0.92 (0.80–1.05) | 0.195 | 0.59 (0.43–0.75) | |
| 6MWT (/100 m) | 0.05–<2.46 | 8 (57) | |||
| 2.46–<3.81 | 8 (57) | ||||
| 3.81–6.16 | 4 (27) | 0.64 (0.40–1.03) | 0.066 | 0.67 (0.50–0.83) | |
| Overestimated maximal walking distance | 5 (50) | 1.27 (0.59–2.74) | 0.537 | 0.55 (0.40–0.70) |
OR = odds ratio; CI = confidence intervals; AUROC = Area under the Receiving Operating Curve; 6MWT = 6‐minute walk test.
Categories for categorical variables and subgroups for continuous variables.
Figure 1.
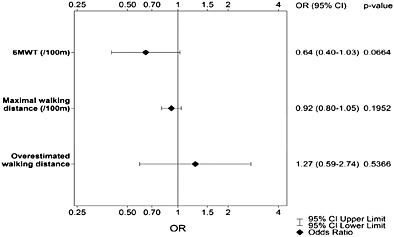
Forrest plot for the 6‐minute walk test, maximal walking distance and overestimated walking distance
Discussion
Aiming to examine putative predicators of fall risk in MS, we addressed walking performance and estimation of maximal walking distance. In the present MS sample, we did not obtain any significant differences comparing fallers and non‐fallers regarding the examined walking parameters. The investigated sample was considered to be representative in terms of fall frequency since 47% of the PwMS experienced falls during a 3‐month period, in line with previous studies (Cattaneo et al., 2002; Finlayson et al., 2006; Nilsagard et al., 2009b; Kasser et al., 2011; Matsuda et al., 2011; Prosperini et al., 2011; Coote et al., 2013; Gunn et al., 2013a). The sex distribution was also compatible of that expected in a MS population.
Several factors may impact walking, and it was believed that these factors may be reflected by testing walking capacity over a longer distance. Tests, such as the 6MWT, may also minimize the risk of overlooking motor fatigue or ceiling effects using shorter distances, especially for people with mild MS (van Winsen et al., 2010). Motor fatigue is described as a gradual decline of the maximal muscle strength during a constant mild to moderate exercise (Phan‐Ba et al., 2012), and the 6MWT is suggested to capture motor fatigue, that is reduced speed at the end of the test (Goldman et al., 2008).
Walking tests in general are mainly developed based on situations where falls are less likely to occur, that is performed during controlled environmental circumstances. Falls related to dual tasking or with environmental challenges are possibly insufficiently captured with such tests although concomitant cognitive tasks can be used (Shumway‐Cook et al., 2000). From a clinical perspective, a measure that combines endurance, dual tasking and environmental challenges would probably be more stringent as a predictor of falls. It would be interesting to use the 6MWT outdoors to meet these challenges.
Moreover, patients that overestimated their maximal walking distance were not overrepresented among fallers. The estimation of walking distance was done before the test procedure, and the participants were unaware of how long the corridor was during testing. This implies that they were neither helped in their estimation by having performed the test nor could adjust their actual walking distance to fit their estimation. In the present study, a larger proportion correctly estimated (43%) their actual walking distance compared with that reported by Ringel and co‐workers (21%) (Ringel and Zettl, 2006).
According to our knowledge, maximal walking distance rarely is included as an objective test in clinical practice. One plausible reason is that it is time consuming from both patients and the care givers perspectives and may be exhausting for the patients. The value of objective testing must be scrutinized before incorporated as standardized parameter in clinical assessment.
Despite the fact of a small sample (n = 49), our data suggest that the investigated parameters have limited clinical relevance in identifying fallers among individuals with MS. Further studies may yield additional information in terms of walking speed over longer distances, because we observed a predictive trend in 6MWT data analysis (p = 0.066). A post‐power size calculation was made for the 6MWT. Based on a clinically significant difference between groups at 60, the assumption of an equal standard deviation at 140, an allocation to a group of faller or non‐faller at 1:1 and a power at 80%, the sample size has to be 87 persons in each group.
A majority of falls in this study were perceived to be caused simply by loss of balance. An alternative approach in further examination of fall risk in MS may be to study other parameters which influence on walking ability, rather than focus on the maximal walking distance itself. The variation in maximal walking distance suggests difficulties finding clinically relevant cutoffs to predict who will fall or not. Although the most commonly reported activity performed when falling was “walking” in the present study, the results imply that maximal walking distance per se is not associated with falls. Instead, underlying factors affecting walking, that is spasticity, proprioception and muscular strength, are of greater importance. However, neither maximal walking distance nor patient overestimate of walking distance in PwMS was associated with falls.
Study limitations
There were several study limitations. Due to safety reasons, the physiotherapist supervising the walking tests in a few cases had to walk close behind the participant. Thus, walking speed may have been affected, also affecting the distance covered. For practical reasons, we set an upper time limit at 15 minutes. Several of the participants actually walked until their legs gave away, but they were not represented among those participants where the test was stopped at 15 minutes. In that sense, the latter participants did not reach their absolute maximal walking distance limit. It is possible that the maximal walking distance could have been longer if the instructions did not encourage them to walk fast. However, encouragement to walk fast is recommended in the literature for PwMS (Goldman et al., 2008). All falls were self‐reported, which is a limitation, but on the other hand, prospectively reported, which is strength. The sample size was small, considering the heterogeneity of the outcome variables.
Implications for physiotherapy practise:
People with MS often have impaired balance that may lead to falls.
Falls often occur during walking.
However, maximal walking distance and patient overestimate of walking capacity are not associated with falls.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
This study was supported financially by Biogen Idec and the Norrbacka‐Eugenia Foundation. The project was supported by the Örebro Research Committee, Sweden, the Norrbacka‐Eugenia Foundation, Sweden, Biogen Idec and Neuro Sweden (NHR). We thank physiotherapist Margareta Kånåhols for the participation in data collection.
Nilsagård, Y. , Westerdahl, E. , Wittrin, A. , and Gunnarsson, M. (2016) Walking Distance as a Predictor of Falls in People With Multiple Sclerosis. Physiother. Res. Int., 21: 102–108. doi: 10.1002/pri.1625.
Footnotes
[Correction added on 24 July 2015, after first online publication: The above Funding section was initially omitted and has now been added to this version.]
References
- Benedetti MG, Piperno R, Simoncini L, Bonato P, Tonini A, Giannini S. Gait abnormalities in minimally impaired multiple sclerosis patients. Multiple Sclerosis 1999; 5: 363–368. [DOI] [PubMed] [Google Scholar]
- Cameron MH, Wagner JM. Gait abnormalities in multiple sclerosis: pathogenesis, evaluation, and advances in treatment. Current Neurology and Neuroscience Reports 2011; 11: 507–515. [DOI] [PubMed] [Google Scholar]
- Cattaneo D, De Nuzzo C, Fascia T, Macalli M, Pisoni I, Cardini R. Risks of falls in subjects with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 2002; 83: 864–867. [DOI] [PubMed] [Google Scholar]
- Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Archives of Physical Medicine and Rehabilitation 2013; 94: 616–621. [DOI] [PubMed] [Google Scholar]
- D'Orio VL, Foley FW, Armentano F, Picone MA, Kim S, Holtzer R. Cognitive and motor functioning in patients with multiple sclerosis: neuropsychological predictors of walking speed and falls. Journal of the Neurological Sciences 2012; 316: 42–46. [DOI] [PubMed] [Google Scholar]
- Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 2006; 87: 1274–1279. [DOI] [PubMed] [Google Scholar]
- Goldman MD, Marrie RA, Cohen JA. Evaluation of the six‐minute walk in multiple sclerosis subjects and healthy controls. Multiple Sclerosis 2008; 14: 383–390. [DOI] [PubMed] [Google Scholar]
- Goldman MD, Motl RW, Rudick RA. Possible clinical outcome measures for clinical trials in patients with multiple sclerosis. Therapeutic Advances in Neurological Disorders 2010; 3: 229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn H, Creanor S, Haas B, Marsden J, Freeman J. Risk factors for falls in multiple sclerosis: an observational study. Multiple Sclerosis 2013a; 19: 1913–1922. [DOI] [PubMed] [Google Scholar]
- Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta‐analysis. Physical Therapy 2013b; 93: 504–513. [DOI] [PubMed] [Google Scholar]
- Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ. Measuring the impact of MS on walking ability: the 12‐Item MS Walking Scale (MSWS‐12). Neurology 2003; 60: 31–36. [DOI] [PubMed] [Google Scholar]
- Kasser SL, Jacobs JV, Foley JT, Cardinal BJ, Maddalozzo GF. A prospective evaluation of balance, gait, and strength to predict falling in women with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 2011; 92: 1840–1846. [DOI] [PubMed] [Google Scholar]
- Kelleher KJ, Spence W, Solomonidis S, Apatsidis D. The characterisation of gait patterns of people with multiple sclerosis. Disability and Rehabilitation 2010; 32: 1242–1250. [DOI] [PubMed] [Google Scholar]
- Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983; 33: 1444–1452. [DOI] [PubMed] [Google Scholar]
- Lamb SE, Jorstad‐Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. Journal of the American Geriatrics Society 2005; 53: 1618–1622. [DOI] [PubMed] [Google Scholar]
- Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, Galea MP. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Multiple Sclerosis 2006; 12: 620–628. [DOI] [PubMed] [Google Scholar]
- Matsuda PN, Shumway‐Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. Pm r 2011; 3: 624–632; quiz 632. [DOI] [PubMed] [Google Scholar]
- Matsuda PN, Shumway‐Cook A, Ciol MA, Bombardier CH, Kartin DA. Understanding falls in multiple sclerosis: association of mobility status, concerns about falling, and accumulated impairments. Physical Therapy 2012; 92: 407–415. [DOI] [PubMed] [Google Scholar]
- Moen SM, Celius EG, Nordsletten L, Holmoy T. Fractures and falls in patients with newly diagnosed clinically isolated syndrome and multiple sclerosis. Acta Neurol Scand 2011; 124(Suppl 191): 79–82. [DOI] [PubMed] [Google Scholar]
- Motl RW, Balantrapu S, Pilutti L, Dlugonski D, Suh Y, Sandroff BM, Lane A, Fernhall B. Symptomatic correlates of six‐minute walk performance in persons with multiple sclerosis. European Journal of Physical and Rehabilitation Medicine 2013; 49: 59–66. [PubMed] [Google Scholar]
- Motl RW, Suh Y, Balantrapu S, Sandroff BM, Sosnoff JJ, Pula J, Goldman MD, Fernhall B. Evidence for the different physiological significance of the 6‐ and 2‐minute walk tests in multiple sclerosis. BMC Neurology 2012; 12: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsagard Y, Denison E, Gunnarsson LG, Bostrom K. Factors perceived as being related to accidental falls by persons with multiple sclerosis. Disability and Rehabilitation 2009a; 31: 1301–1310. [DOI] [PubMed] [Google Scholar]
- Nilsagard Y, Lundholm C, Denison E, Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis — a longitudinal study. Clinical Rehabilitation 2009b; 23: 259–269. [DOI] [PubMed] [Google Scholar]
- Paltamaa J, Sarasoja T, Leskinen E, Wikstrom J, Malkia E. Measures of physical functioning predict self‐reported performance in self‐care, mobility, and domestic life in ambulatory persons with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 2007; 88: 1649–1657. [DOI] [PubMed] [Google Scholar]
- Penner IK, Raselli C, Stocklin M, Opwis K, Kappos L, Calabrese P. The Fatigue Scale for Motor and Cognitive Functions (FSMC): validation of a new instrument to assess multiple sclerosis‐related fatigue. Multiple Sclerosis 2009; 15: 1509–1517. [DOI] [PubMed] [Google Scholar]
- Phan‐Ba R, Calay P, Grodent P, Delrue G, Lommers E, Delvaux V, Moonen G, Belachew S. Motor fatigue measurement by distance‐induced slow down of walking speed in multiple sclerosis. PLoS One 2012; 7: e34744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosperini L, Fortuna D, Gianni C, Leonardi L, Pozzilli C. The diagnostic accuracy of static posturography in predicting accidental falls in people with multiple sclerosis. Neurorehabilitation and Neural Repair 2013; 27: 45–52. [DOI] [PubMed] [Google Scholar]
- Prosperini L, Kouleridou A, Petsas N, Leonardi L, Tona F, Pantano P, Pozzilli C. The relationship between infratentorial lesions, balance deficit and accidental falls in multiple sclerosis. Journal of the Neurological Sciences 2011; 304: 55–60. [DOI] [PubMed] [Google Scholar]
- Rao S, Society. TCFSGotNMS. A Manual for the Brief Repeatable Battery of Neuropsychological Tests in Multiple Sclerosis. Milwaukee, WI: Medical College of Wisconsin, 1990. [Google Scholar]
- Ringel I, Zettl UK. Estimates of the walking distance in multiple sclerosis patients and their effect on the EDSS. Journal of Neurology 2006; 253: 666–667. [DOI] [PubMed] [Google Scholar]
- Shumway‐Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community‐dwelling older adults using the Timed Up & Go Test. Physical Therapy 2000; 80: 896–903. [PubMed] [Google Scholar]
- Smith A. Symbol Digit Modalities Test (SDMT) Manual. Los Angeles: Western Psychological Services, 1982. [Google Scholar]
- Sosnoff JJ, Balantrapu S, Pilutti LA, Sandroff BM, Morrison S, Motl RW. Cognitive processing speed is related to fall frequency in older adults with multiple sclerosis. Archives of Physical Medicine and Rehabilitation 2013; 94: 1567–1572. [DOI] [PubMed] [Google Scholar]
- Sosnoff JJ, Sandroff BM, Pula JH, Morrison SM, Motl RW. Falls and physical activity in persons with multiple sclerosis. Mult Scler Int 2012; 2012: 315620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Winsen LM, Kragt JJ, Hoogervorst EL, Polman CH, Uitdehaag BM. Outcome measurement in multiple sclerosis: detection of clinically relevant improvement. Multiple Sclerosis 2010; 16: 604–610. [DOI] [PubMed] [Google Scholar]
- Wetzel JL, Fry DK, Pfalzer LA. Six‐minute walk test for persons with mild or moderate disability from multiple sclerosis: performance and explanatory factors. Physiotherapy Canada 2011; 63: 166–180. [DOI] [PMC free article] [PubMed] [Google Scholar]


