Summary
Pneumatic dilation (PD) of the lower esophageal sphincter (LES) in achalasia is a major palliative treatment. It is generally believed, although never substantiated, that therapeutic efficacy of ballooning in achalasia is the result of the disruption and tearing of the muscular layers of the LES. To clarify this issue, we investigated the frequency of muscular disruption at the LES, 24 hours after PD, by employing the endoscopic ultrasound (EUS), in a group of 43 consented patients with achalasia. Between July 2009 and March2012, 51 consecutive adult patients with tentative diagnosis of achalasia, some with recurrence of symptoms after an earlier treatment with balloon dilation, were evaluated and underwent PD, using Rigiflex balloon without major adverse effect. Out of the 51 evaluated, 43 eligible and consenting patients who underwent EUS, 24 hours after PD, using Olympus GF‐UE 160 echoendoscope and an Aloka Prosound probe at 7.5 MHZ, are the subjects of this study. The EUS in 43 eligible patients revealed an intact LES in 36 (83.7%), small area of muscular disruption in 5 (11.6%) and small hematoma in 2 patients (4.6%). Our data convincingly demonstrate that the clinical effectiveness of balloon dilation in achalasia is not the result of muscular disruption, but of circumferential stretching of the LES. Our findings on the mechanism of action of PD in achalasia could result in modifying the current method of dilation for a safer procedure, by slowing the rate of inflation and allowing the sphincter to slowly stretch itself to the distending balloon.
Keywords: achalasia, balloon dilation, LES stretching
Introduction
Because the etiology and the exact pathogenesis of achalasia are unknown,1, 2 there is no specific treatment to restore the normal motor function to the esophagus. The current therapeutic approaches in achalasia are essentially palliative and targeted at relieving the functional obstruction at the lower esophageal sphincter (LES), and let the swallowed food and liquid enter the stomach by their sheer weight. This is achieved either by partial relaxation of the LES or by breaking the resistance of the spastic LES. Relaxation of the spastic LES is achieved either by daily repeated doses of nitrates or calcium channel blockers, such as nifedipine (orally or sublingually prior to meals), which offer only partial and transient relief,3 or endoscopic injection of botulinum toxin in the LES. Botulinum toxin injection by blocking the release of acetylcholine from excitatory cholinergic neurons in the myenteric plexus confers partial relaxation to the LES2, 4 and symptomatic relief to the patient for a few months to a year in two thirds of treated patients.1, 4, 5
The functional obstruction of the LES can also be dealt with in a more aggressive manner,5, 6 either mechanically by forceful pneumatic dilation (PD), or surgically, by a 6‐ to 8‐cm longitudinal extra‐mucosal transection of muscular layer of the LES, introduced a century ago by Heller, a Swiss surgeon.7 Whereas symptomatic relief from PD is relatively short lasting (months to a few years), often necessitating repeated dilation, the therapeutic effect of Heller myotomy is more durable and longer lasting.5, 6, 8, 9, 10
It is generally believed, probably by analogy to the efficacy of Heller operation, that the therapeutic efficacy of PD is the result of rupture of the muscular layer of the LES.6, 8, 10, 11, 12, 13, 14 However, different clinical outcome and late complications of these two treatment modalities, bespeaks of two different basic mechanisms of action, and not just different grading of the effect by the same operative mechanism.
The rate of perforation of the esophagus in achalasic patients undergoing PD, performed by experienced gastroenterologists, is 1–5%9, 11, 13, 14. If muscular disruption of the LES was the basis for the observed clinical efficacy of PD in achalasia, one would have expected a much higher rate of esophageal perforation after PD, essentially a blind and inadequately controlled procedure.
Moreover, there is no scientific study to support the widely held, but never substantiated, view on the mechanism of action of PD in patients with achalasia.
To clarify this point, we undertook the challenge of evaluating the integrity of the muscular layers of the LES by endoscopic ultrasound (EUS), in 40–50 consecutive achalasic patients undergoing PD at Shiraz University of Medical Sciences (SUMS), in Shiraz, the Capital of Fars, a southern Province of Iran.
The Aims of the Study
The principle aim of our study was to determine the frequency of occurrence of muscular disruption at the LES in achalasic patients, by employing EUS 24 hours after PD.
In the absence of a systematic muscular disruption of circular muscle at the LES, supposedly to account for the clinical effectiveness of PD, what would be the alternative mechanism of action of PD to explain the observed clinical efficacy of PD in achalasia?
Our research protocol was reviewed and approved by the Research and Ethics Committee of Shiraz University of Medical Sciences.
Patients and methods
Between July 2009 and March 2012, 51 consecutive adult patients with tentative diagnosis of achalasia, referred by practicing gastroenterologists and internists from Fars and the neighboring provinces to the Section of Gastroenterology of Shiraz University for management, were prospectively studied and are the subjects of this investigation.
All referred patients were clinically assessed by the principal investigator (PI) according to a specially prepared questionnaire. After collecting demographic data, patients were thoroughly questioned about their symptoms including: dysphagia, regurgitation, retrosternal chest pain, weight loss, coughing when lying down, duration and severity of their symptoms, any special maneuvers alleviating their symptoms, presence of similar symptoms in any other member of their family and any previous work‐up and medical treatment of their disease by the local internist or PD by a gastroenterologist.
After establishing the diagnosis of achalasia and fully describing the nature of their illness and the aim of our study to the patients, they were invited to participate in the study. Those who agreed to participate in the study and to have EUS of the LES the day after PD looking for any induced injury from balloon dilation, signed the informed consents, and those who declined to participate received proper treatment.
Inclusion and exclusion criteria
All patients whose clinical history, radiological, esophagogastroduodenoscopy (EGD) and esophageal manometric findings were consistent with the diagnosis of achalasia, even those with a history of previous PD were included in the study. Those patients who were treated surgically for achalasia, or patients with any medical contraindication to PD, and those considered unable to tolerate any potential serious adverse effects of the procedure, were excluded from consideration.
Interventions
PD
The procedural details of PD, as recommended by Waechter and Pasricha in ‘Up to Date’, were carefully followed.15 Briefly, under conscious sedation, EGD was performed and careful inspection of the cardia by retroflexed scope was carried out to rule out any infiltrative process causing pseudo‐achalasia.16 The distance between the esophagogastric junction and the incisors of patient was measured by the endoscope and marked by a band of a narrow tape on the shaft of the dilating catheter from the middle of the balloon. Then a guide‐wire was passed through the biopsy channel of endoscope for directing the Rigiflex catheter (Boston Scientific, Boston, MA, USA). After removing the endoscope, threading the ballooned catheter and positioning the middle of the balloon at the LES under fluoroscopic guidance, the balloon was gradually inflated with air to observe development of the waist in the middle of the balloon, and its obliteration with more inflation pressure (between 7 and 15 psi). The balloon was kept under obliterating pressure for 60 seconds. Then the balloon was rapidly deflated, only to be re‐inflated for another 60 seconds, with a pressure of 3 psi less than the pressure of the first inflation.
In patients with no history of earlier PD the 3 cm balloon, and in patients with symptomatic recurrence(s), the 3.5 cm or the 4 cm diameter balloons were used.15
EUS evaluation
All post‐dilation EUS of the LES was performed by using an Olympus GF‐UE160 echoendoscope (Olympus Co, Tokyo, Japan) and an Aloka Prosound ά‐5 sv (ALKOA CO, LTD, Mure, Mitaka‐Shi, Tokyo, Japan) under conscious sedation with a 7.5 MHZ probe. The LES was identified endoscopically, and the whole length of it was scanned for any dilation injury, including rupture or hematoma. Patients were discharged home after EUS to be followed by the PI through periodic (every few weeks) phone calls or attending the clinic in person.
Statistical analysis
All results are expressed as percentage, mean ± standard deviation. The SPSS Statistical Software Program (Version 11.0, SPSS, Chicago, IL, USA) was used for analysis of data. The Student's t‐test was used to compare the difference of means between the groups.
Post‐dilation follow‐up
As expected, during the relatively short period of our follow‐up, most of our patients, particularly the older ones, demonstrated significant clinical improvement of their dysphagia and regurgitation for several months to even 2–3 years, but in about one out of four patients, particularly the young, recurrence of symptoms were early and severe enough to require repeat PD with a larger diameter balloon. Because we employed a standard PD technique, and in view of our short duration of follow‐up, analysis of clinical outcome in patients were deemed inconclusive, and irrelevant to the stated objectives of our study.
Results
There was no incidence of esophageal perforation in any of our study patients undergoing PD. Only one patient complained of a prolonged and moderate retro‐sternal chest pain after PD. Radiological examination with Gastrogrffin (Bracco Diagnostic Inc. Monroe Township, NJ, USA.) in this patient failed to demonstrate any extra‐mucosal or extra‐luminal leakage of contrast material. Incidentally, he was one of the five patients whose EUS evaluation revealed a small area of muscular disruption of the LES.
The range and the mean age of patients, duration of symptoms at presentation for men and women, and the statistical significance between the two groups are shown in Table 1.
Table 1.
Age and symptoms duration in men and women
| No. of patients | Mean age ± SD (years) | P value | Symptoms duration (years) Mean ± SD | P value | |
|---|---|---|---|---|---|
| Men | 25 | 48.08 ± 16.80 | 0.083 | 8.36 ± 7.48 | 0.025a |
| Women | 26 | 40.73 ± 12.69 | Assessed patients | 4.48 ± 3.53 | Assessed patients |
| All patients (19–78 years) | 51 | 44.33 ± 15.16 | Assessed patients | 6.38 ± 6.08 | Assessed patients |
There is a significant difference for duration of symptoms between men and women. SD, standard deviation.
EUS findings
The EUS of the LES in 43 studied patients, 24 hours after PD, demonstrated intact muscular layers in 36 patients (83.7%; Figure 1) and dilation injury in 7 patients (16.3 %). The injuries comprised a small area of muscular disruption in 5 patients (11.6%; Figure 2) and small hematoma in 2 other patients (4.6%).
Figure 1.
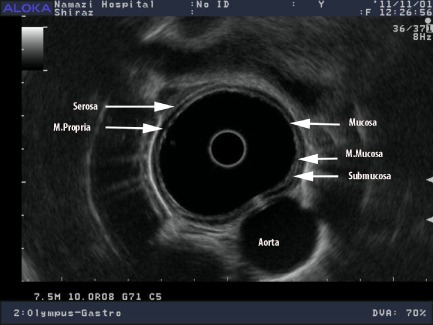
Intact post‐dilation muscular structure of the lower esophageal sphincter on endoscopic ultrasound.
Figure 2.
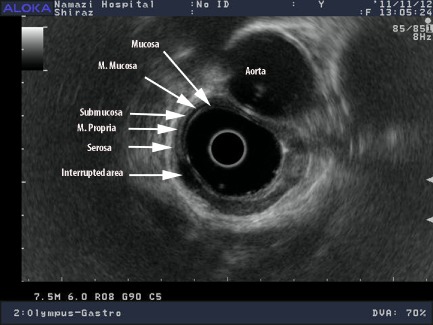
Minor disruption: muscularis propria is interrupted with a hypoechoic area.
Discussion
As stated earlier, although the exact mechanism of action of PD on the LES has never been investigated,17 it is generally believed that clinical efficacy of PD in achalasia is the result of rupture of the muscular layer of the LES. This view, although scientifically unsubstantiated, is expressed in all Textbooks of Gastroenterology,13, 14 original contributions,8, 10, 18 reviews,6, 11, 12, 15 editorials5, 19 and even in the Clinical Guideline for Diagnosis and Management of Achalasia 20 by the American College of Gastroenterology.
Meanwhile, Schiano et al., with no intention to challenge the prevalent view on post‐PD muscular disruption, assessed the state of the LES by high‐resolution EUS in 11 achalasic patients, before, immediately and 24 hours after PD and found only transient thickening (edema) of mucosa and submucosa, but ‘surprisingly’ no muscular damage observed.21
Based on the results of our investigation, one can conclude that therapeutic effectiveness of PD in achalasia is not the result of muscular disruption, but circumferential stretching of the wall of the LES. The relatively low rate of esophageal perforation in patients with achalasia undergoing PD is consistent with the concept of circumferential stretching as the basic mechanism of action of PD.
Thirty years ago, Vantrappen and Janssens, by dilating the LES in monkeys and dogs with balloons of increasing diameter, lowered the LES pressure to the level of 20% or less of pretreatment values. Histological examination of the LES in treated and control animals were virtually indistinguishable and there was no evidence of muscular rupture. Interestingly, Vantrappen and Janssens, for the first time, used the term of ‘stretching the cardia’ by forceful dilation.17
Can the concept of stretching of the LES results in modifying certain parameters of PD in achalasia?
Now, given the circumferential stretching of the nonrelaxing LES as the actual mechanism of action of PD, then we may have to question which variable(s) in the process of PD, including the size of the balloon (3, 3.5 and 4 cm), the rate of inflation (rarely if ever measured and reported), the inflation pressure required to efface the waist of the balloon at the LES (5–15 psi), the duration of keeping the balloon at the maximum pressure (6 seconds to 5 minutes) and finally the number of inflation per session, is(are) effectively involved and may contribute to a safer, more efficacious and durable stretching of the LES.
Among all the above variables, the rate of inflation of the balloon appears to be the critical factor for maintaining the integrity of the LES, whereas keeping the inflated balloon under pressure longer probably confers durability of clinical effectiveness of the procedure. With a rapid inflation of the balloon to the required pressure to obliterate the waist (8−15 psi), the circular muscle of the LES may not get enough time to adapt and accommodate to the expanding balloon, hence, the muscle layers may eventually yield and rupture. With a slower rate of inflation (2–3 minutes), we let the LES gradually stretch proportionate to the increasing caliber of the balloon and potentially prevent esophageal perforation.
Acknowledgement
The authors offer their sincere thanks to Mehrdad Vossoughi, PhD (Department of Biostatistics, Shiraz University of Medical Sciences), for statistical analysis of our data and Dr. Amir Anushirvani, the Chief Resident in Medicine (Department of Medicine, Shiraz University of Medical Sciences), for his assistance in the online submission of the manuscript. The authors also express their deep appreciation to Mr. Mike Wilson (Olympus Key Med, division of Key Med Ltd., Essex, UK) for supporting our research project on achalasia by donating 20 pieces of MH‐303 EUS Balloons.
This paper was partly presented at the Digestive Diseases Week at San Diego, CA, on May 19, 2012.
Specific author contributions: FBM: involved in the conception of the idea and the design of the study, writing the draft of the research protocol and submitting it to the Medical Research and Ethics Committee for approval, clinical and eligibility evaluation of patients, obtaining the informed consent, post‐PD follow‐up of the patients in clinic or by phone, collecting and analyzing the data with the statistician and drafting the manuscript with numerous revisions. MJK: critical review of the protocol and the final draft of the manuscript and selection and employment of the highly recommended technique of balloon dilation in patients. ART: critical evaluation of the research protocol and the manuscript and performing the endoscopic ultrasounds in all investigated patients.
Conflicts of interest: The authors have nothing to disclose.
[This article has been changed since originally published on 13 March 2015. In addition to minor typographical amendments, the following errors have been corrected: The author affiliations “1Department of Medicine, Section of Gastroenterology, Shiraz University of Medical Sciences Shiraz, Iran; and 2Department of Gastroenterology and 3Department of Medicine, Section of Gastroenterology, Shiraz University of Medical Sciences, Shiraz, Iran” have been changed to “1Shiraz University of Medical Sciences and 2Nemazee Hospital, Department of Medicine, Section of Gastroenterology, Shiraz, Iran”; References 9 and 10 have been deleted from the text and Reference list and succeeding references have been renumbered.]
References
- 1. Richter J E. Achalasia – an update. J Neurogastroenterol Motil 2010; 16: 232–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Park W, Vaezi M F. Etiology and pathogenesis of achalasia. The current understanding. Am J Gastroenterol 2005; 100: 404–414. [DOI] [PubMed] [Google Scholar]
- 3. Hoogerwerf W A, Pasricha P J. Pharmacologic therapy in treating achalasia. Gastrointest Endosc Clin N Am 2001; 11: 311–323. [PubMed] [Google Scholar]
- 4. Pasricha P J, Rai R, Ravich W J, Hendrix T R, Kalloo A N. Botulinum toxin for achalasia: long‐term outcome and predictors of response. Gastroenterology 1996; 110: 1410–1415. [DOI] [PubMed] [Google Scholar]
- 5. Pehlivanov N, Pasricha P J. Achalasia: botox, dilatation or laparoscopic surgery in 2006. Neurogastroenterol Motil 2006; 13: 799–804. [DOI] [PubMed] [Google Scholar]
- 6. Spiess A E, Kahrilas P J. Treating achalasia; from whalebone to laparoscope. JAMA 1998; 280: 638–642. [DOI] [PubMed] [Google Scholar]
- 7. Heller E. Extramukӧse cardiaplastik beim chronischen kardiospasmus mit dilatation des oesophagus. Mitt Grenzgeb Med Chir 1913; 27: 141–149. [Google Scholar]
- 8. Csendes A, Velasco N, Braghetto I, Henriquez A. A prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia of the esophagus. Gastroenterology 1981; 80: 789–795. [PubMed] [Google Scholar]
- 9. Lopushinsky S R, Urbach D R. Pneumatic dilation and surgical myotomy for achalasia. JAMA 2006; 296: 2227–2233. [DOI] [PubMed] [Google Scholar]
- 10. Csendes A, Braghetto I, Henriquez A, Cortes C. Late results of prospective randomized study comparing forceful dilatation and esophagomyotomy in patients with achalasia. Gut 1989; 30: 299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pohl D, Tutuian R. Achalasia: an overview of diagnosis and treatment. J Gastrointest Liver Dis 2007; 16: 297–303. [PubMed] [Google Scholar]
- 12. Nanson E. Treatment of achalasia of cardia. Gastroenterology 1966; 51: 236–241. [PubMed] [Google Scholar]
- 13. Clouse R E, Diamant N E. Esophageal motor and sensory function and motor disorders of the esophagus In: Feldman M, Friedman L S, Sleisenger M H. (eds) Sleisenger & Fortrand's Gastrointestinal and Liver Disease, 7th edn, Vol. 1 Philadelphia: Saunders, 2002; 561–584. [Google Scholar]
- 14. Kahrilas P J, Pandolfino J E. Esophageal neuromuscular function and motility disorders In: Yamada T, (ed.) Textbook of Gastroenterology, 4th edn, Vol. 1. Philadelphia: Lippincott, 2003; 677–704. [Google Scholar]
- 15. Waechter A, Pasricha P J. Pneumatic dilation and botulinum toxin injection for achalasia. Updated 02/11/2008. [Cited 23 Jun 2009.] Available from URL: http://www.uptodate.com
- 16. Gockel I, Eckardt V F, Schmitt T, Junginger T. Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroent 2005; 40: 378–385. [DOI] [PubMed] [Google Scholar]
- 17. Vantrappen G, Janssens J. To dilate or to operate? That is the question. Gut 1983; 24: 1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fellows I W, Ogilvie A L, Atkinson M. Pneumatic dilatation in achalasia. Gut 1983; 24: 1020–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Spechler S J. Pneumatic dilation and laparoscopic Heller's myotomy equally effective for achalasia. N Engl J Med 2011; 346: 1868–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vaezi M F, Pandolfino J E, Vela M F. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 2013; 108: 1238–1249. [DOI] [PubMed] [Google Scholar]
- 21. Schiano T D, Fisher R S, Parkman H P, Cohen S, Debezies M, Miller L S. Use of high‐resolution endoscopic ultrasonography to assess esophageal wall damage after pneumatic dilation and botulinum toxin injection to treat achalasia. Gastrointest Enosc 1996; 44: 151–157. [DOI] [PubMed] [Google Scholar]


