Abstract
This article reviews updated advice and factual material from the Swedish National Board of Health and Welfare on reducing the risk of sudden infant death syndrome. Issues covered by the guidance for parents and healthcare professionals include sleeping positions, smoking, breastfeeding, bed sharing and using pacifiers.
Conclusion
The guidelines conclude that infants under three months of age are safest sleeping in their own cot and that a pacifier can be used when they are going to sleep.
Keywords: Apparent life‐threatening event, bed sharing, pacifier, prevention, Sudden infant death syndrome
Key Notes.
This article reviews updated advice and factual material from the Swedish National Board of Health and Welfare on reducing the risk of sudden infant death syndrome.
Issues covered by the guidance include sleeping positions, smoking, breastfeeding, bed sharing and using pacifiers.
The guidelines conclude that infants under three months of age are safest sleeping in their own cot and that a pacifier can be used when they are going to sleep.
In the winter of 2013–2014, the Swedish National Board of Health and Welfare published updated advice for parents on ways to reduce the risk of sudden infant death syndrome (SIDS) 1. The aims were to maintain the current low Swedish incidence of SIDS and reduce it still further. A few months later, the National Board of Health and Welfare supplemented the advice with a comprehensive publication on SIDS called Reducing the risk of cot death – a guide for healthcare professionals 2, 3. This review presents, and comments on, the new advice for parents and the guide for healthcare professionals. For definition of SIDS, see Box 1.
Box 1.
Sudden infant death syndrome (SIDS) denotes the sudden and unexpected death of an infant where the cause of death cannot be determined despite a thorough history, inspection of place of death or forensic autopsy.
Historical Perspective
What we call SIDS has always existed. The first known description of a case of SIDS can be found in the Old Testament, in the First Book of Kings. In a story that illustrates the wisdom of King Solomon as a judge, it says: ‘And this woman's child died in the night; because she overlaid it’ 4. The view that the deaths were caused by the mother lying on top of her infant is also reflected in the old Swedish provincial laws from the 13th and 14th centuries. A woman who had laid on her child could be punished 5.
When child mortality due to infections became rare in the mid‐20th century, it became more obvious that some infants died suddenly and unexpectedly. In Sweden, cot deaths started to attract attention in the 1960s 6. The incidence of cot deaths was around one per 2000 live births from 1960 to the beginning of the 1970s. The incidence then started to rise during the 1970s 7. During the 1980s, the increase in SIDS incidence became worrying both in the Scandinavian countries and in other Western countries (Fig. 1).
Figure 1.
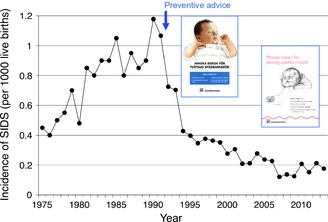
Incidence of SIDS in Sweden, 1975–2013. Statistics from the Swedish National Board of Health and Welfare from 1990 to 2013. The cover pages of previous parental brochures from the National Board of Health and Welfare, Reducing the risk of cot death [Minska risken för plötslig spädbarnsdöd], are inserted. Figure from (ref. 2).
Appearance of Preventive Advice
A change in childcare practices that occurred at the beginning of the 1970s was that babies were no longer put on their backs or sides to sleep but in a prone position. Unfortunately, the possible consequence of a prone sleeping position in terms of the increased risk of SIDS did not start to be understood until the second half of the 1980s 8, 9, 10.
The breakthrough in reducing SIDS came around 1990. Two pivotal case–control studies, one in England and the other in New Zealand, convincingly demonstrated that prone sleeping increased the risk of SIDS 11, 12. This insight rapidly spread throughout the Western world and parents started to place their babies on their backs to sleep. In early 1992, the National Board of Health and Welfare in Sweden issued advice against prone sleeping for infants 13. It resulted in a rapid decline in the incidence of SIDS (Fig. 1). Maternal smoking during pregnancy was shown to be another important risk factor for SIDS 12, 14, 15, 16, 17, 18. The welcome reduction in smoking during pregnancy in the last two decades has certainly contributed to the continued reduction in the incidence of SIDS even when few infants sleep prone.
Today, SIDS is uncommon in Sweden. The number of SIDS cases has decreased from 146 cases in 1990 to 24 cases in 2012 and 20 cases in 2013. This means that the incidence has gone down from 12 infants per 10 000 live births to two infants per 10 000 births. Since 1992, the National Board of Health and Welfare has provided advice to reduce the risk of SIDS 13. As time has passed, the advice has been updated. The preventive SIDS advice has been very successful. However, in recent years, new knowledge has appeared, making a new update necessary.
A systematic review of the literature on SIDS led to six pieces of advice to parents, fully referenced in the following sections, to reduce the risk of SIDS (see also Box 2):
Box 2.
The new advice from the Swedish National Board of Health and Welfare on reducing the risk of SIDS 1, 2:
The infant should sleep on its back.
Smoking and nicotine should be avoided.
The infant's face should be kept free, overheating should be avoided, and movement should not be restrained.
The safest place to sleep for an infant under three months is in its own cot.
Mothers should breastfeed if possible.
A pacifier (dummy) can be used when the infant is going to sleep.
The infant should sleep on its back.
Smoking and nicotine should be avoided.
The infant's face should be kept free, overheating should be avoided, and movement should not be restrained.
The safest place for an infant under three months to sleep is in its own cot.
Mothers should breastfeed if possible.
A pacifier (dummy) can be used when the infant is going to sleep.
The Baby Should Sleep on Its Back
A large number of studies show that the back is the safest sleeping position for babies 11, 12, 19, 20, 21. Moreover, being placed on their side involves a greater risk than being placed supine. A side position as such does not appear to carry an increased risk of SIDS, but the side is a less stable position 22. The increased risk occurs if the baby rolls into a prone position 23.
Smoking and Nicotine Should Be Avoided
It is well known that smoking during pregnancy increases the risk of SIDS 24 and that the relationship is dose dependent 18. Due the possible dangers of other nicotine‐containing products, such as snuff and nicotine chewing gums, these should also be avoided during pregnancy.
One mode of action appears to be that babies who have been exposed to smoking when they were foetuses appear to have impaired arousability 25, 26. Impaired arousal of this kind could explain why the risk of SIDS is greater in the babies of smoking mothers, when the mother and the baby sleep in the same bed 23, 27. Maternal smoking also appears to affect the autonomic nervous control of cardiovascular function and blood pressure 28. This impairs the baby's ability to maintain autonomic balance, that is homeostasis.
The Safest Place for an Infant under Three Months to Sleep is in Its Own Cot
This statement has strong scientific support. An extensive study based on individual data from a large number of studies demonstrated that this also applies to breastfed infants and when the mother does not smoke 27. The mechanism can be that the baby's breathing may be obstructed if its face lies against the skin of the adult or is covered by an arm or by bedclothes. Furthermore, it has been speculated that there is a risk of thermal stress for a baby lying next to a warm sleeping adult.
However, we acknowledge that this advice has been questioned. One criticism has been that it makes breastfeeding more difficult. One option is to breastfeed in bed and then place the baby in a cot next to the parent's bed. The baby should sleep in the same room as the parents, as this carries a lower risk of SIDS than if the baby sleeps in a room by itself 23, 29, 30, 31.
Another criticism has been that the risk of bed sharing is linked to specific hazardous circumstances. In a recent analysis based on two case–control studies conducted in the UK, Blair et al. found that the risk associated with bed sharing was not significant in the absence of hazards like bed sharing with a smoker or with a person who had consumed alcohol or sleeping together on a sofa 32. This applied to infants of less than three months old as well.
If the mother chooses to keep the baby in her bed, bed sharing should be made as safe as possible, by creating a space of its own for the baby, for example. Furthermore, bed sharing should always be avoided during obviously hazardous circumstances, such as when the parents have consumed alcohol.
Mothers Should Breastfeed if Possible
Breastfeeding is associated with a reduced risk of SIDS 33, 34. The mechanism mediating the effect is not totally clear. One possible explanation is that breast milk via its antibodies reduces the risk of virus infection, a factor that is often present in cases of SIDS 35. It has recently been demonstrated that interleukin‐1β, which is produced during infection, induces the release of prostaglandin E2, which impairs respiration via receptors in the brainstem 36, 37.
A Pacifier (Dummy) can be Used When the Infant is Going to Sleep
Many studies have found that the use of a pacifier when the baby is going to sleep reduces the risk of SIDS 38, 39. One possible explanation could be that the sucking activates muscles in the mouth and pharynx, thereby promoting the patency of the upper airways. Another mechanism could be that the pacifier keeps the airways open mechanically 40. It has also been suggested that use of a pacifier increases arousability from sleep 41. This was, however, not found in later studies 42, 43.
A recent review of pacifier use and SIDS from the Physiology and Epidemiology Working Groups of the International Society for the Study and Prevention of Perinatal and Infant Death (ISPID) supported the consistent evidence that pacifier use reduces the risk of SIDS 44. However, the review questioned the explanations of how pacifiers confer protection because the pacifier often falls out of the infant's mouth, often within minutes of the infant going to sleep 41. The authors of the ISPID review asked whether the association between the lack of a pacifier being used by the infant for the final sleep and SIDS could be a marker for something as yet unmeasured 44.
The use of pacifiers has been criticised, as pacifiers have been said to affect breastfeeding negatively. It is, however, difficult to say whether the use of a pacifier per se is negative for breastfeeding. It could be that the pacifier merely satisfies the baby's need to suck, especially if the baby is not breastfed.
Adverse Effects
The use of a supine sleeping position has increased the incidence of acquired cranial asymmetry, nonsynostotic plagiocephaly 45, 46, 47. The asymmetry falls into three main groups: plagiocephaly (skewed occipital flattening), brachycephaly (symmetric occipital flattening) and combined plagiocephaly–brachycephaly. The advice for parents and the factual material for healthcare professionals focus on how to prevent the development of acquired cranial asymmetry. The most important factor is that the position of the head is varied. The risk of acquiring skull asymmetry is also further reduced if the baby spends time awake in the prone position 48.
How to Communicate Preventive Advice
Effective communication on ways to reduce the risk is essential for the successful prevention of SIDS. This information is primarily provided at child welfare centres. One chapter in the guide for healthcare professionals deals with the best way for the nurse at the clinic to inform parents about ways of reducing the risk of SIDS. The guide also discusses ways of talking to parents who have lost their babies.
Apparent Life‐Threatening Events
The guide for healthcare professionals also addresses related conditions like apparent life‐threatening events (ALTE). In recent years, there have been several reports of ALTE affecting newborn babies in the maternity ward 49, 50, 51, 52. Many of the events have occurred immediately after birth during early breastfeeding attempts. When placed skin‐to‐skin, the newborn baby can have problems keeping its airways free. This has resulted in suffocation accidents. To avoid these accidents, it should be stressed that, when a newly born baby is placed skin‐to‐skin to promote breastfeeding, checks must be made to ensure that breathing is free.
Best Hypothesis of SIDS Pathogenesis
As a result of epidemiological research, the incidence of SIDS has been drastically reduced. In spite of this, we still do not know the exact mechanism, or mechanisms that cause the deaths. The guide for healthcare professionals has a chapter that discusses previous and current hypotheses of the cause of SIDS at length 2, 53. The best explanation of SIDS pathogenesis appears to be offered by the triple‐risk model originally proposed by Filiano and Kinney 54, and more recently highlighted in other papers 55, 56. In this model, findings from different epidemiological studies are brought together to form a plausible pathophysiological scenario.
According to this model, interaction between different risk factors is needed to result in SIDS: (i) a critical developmental period; (ii) a vulnerable infant and (iii) an exogenous stressor (extrinsic risk factor). In a model of this kind, one hypothetical scenario could be a three‐month‐old baby boy, with a mother who smoked during pregnancy, who sleeps prone with his face towards the mattress. Breathing is obstructed and oxygenation deteriorates, but the expected arousal does not occur, as nicotine exposure has led to a blunted arousal response. A vicious circle with apnoea, bradycardia and asystole is initiated.
Conclusion
Updated Swedish advice and guidance on reducing the risk of SIDS conclude that infants under three months of age are safest sleeping in their own cot and that a pacifier can be used when they are going to sleep.
References
- 1. Socialstyrelsen [National Board of Health and Welfare] . Minska risken för plötslig spädbarnsdöd [Reducing the risk of cot death]. 11 Dec 2013 [cited 2015 Feb 14]. Available from URL: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19486/2014-8-2.pdf.
- 2. Socialstyrelsen [National Board of Health and Welfare] . Minska risken för plötslig spädbarnsdöd. En vägledning för hälso‐ och sjukvårdspersonal [Reducing the risk of cot death – a guide for healthcare professionals]. Stockholm: Socialstyrelsen, 2014. Artikel‐nr 2014‐3‐3. 8 May 2014 [cited 2014 Nov 12]. Available from URL: http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19370/2014-3-3.pdf. [Google Scholar]
- 3. Wennergren G. Nya råd för att minska risken för plötslig spädbarnsdöd. »Trippelriskmodellen« ger grund för prevention [New guidelines for reducing the risk of sudden infant death. “Triple risk model” provide the basis for prevention]. Läkartidningen 2014; 111: 1564–5. [PubMed] [Google Scholar]
- 4. 1 Kings , 3:19. The Official King James Bible Online. [cited 2014 Nov 12]. Available from URL: http://www.kingjamesbibleonline.org/1-Kings-Chapter-3/.
- 5. Norvenius SG. Some medico‐historic remarks on SIDS. Acta Paediatr 1993; 82(Suppl 389): 3–9. [DOI] [PubMed] [Google Scholar]
- 6. von Sydow G. Plötslig, oväntad spädbarnsdöd: Socialmedicinsk värdering av några fall [Sudden unexpected death in infancy. Social medical evaluations of some cases]. Läkartidningen 1969; 66: 683–9. [PubMed] [Google Scholar]
- 7. Norvenius SG. Sudden infant death syndrome in Sweden in 1973‐1977 and 1979. Acta Paediatr Scand 1987; 76(Suppl 333): 1–138. [DOI] [PubMed] [Google Scholar]
- 8. Davies DP. Cot death in Hong Kong: a rare problem? Lancet 1985; 2: 1346–9. [DOI] [PubMed] [Google Scholar]
- 9. Beal S. Sleeping position and SIDS. Lancet 1988; 2: 512. [DOI] [PubMed] [Google Scholar]
- 10. Engelberts AC, de Jonge GA. Choice of sleeping position for infants: possible association with cot death. Arch Dis Child 1990; 65: 462–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fleming PJ, Gilbert R, Azaz Y, Berry PJ, Rudd PT, Stewart A, et al. Interaction between bedding and sleeping position in the sudden infant death syndrome: a population based case‐control study. BMJ 1990; 301: 85–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mitchell EA, Scragg R, Stewart AW, Becroft DM, Taylor BJ, Ford RP, et al. Results from the first year of the New Zealand cot death study. N Z Med J 1991; 104: 71–6. [PubMed] [Google Scholar]
- 13. Socialstyrelsen [National Board of Health and Welfare] . Skall spädbarn ligga på mage eller rygg? Finns det ett samband mellan magläge och plötslig spädbarnsdöd? [Should infants be placed prone or supine? Is there a connection between prone position and cot death?] Stockholm: Socialstyrelsens meddelandeblad, 1992. [Google Scholar]
- 14. Steele R, Langworth JT. The relationship of antenatal and postnatal factors to sudden unexpected death in infancy. Can Med Assoc J 1966; 94: 1165–71. [PMC free article] [PubMed] [Google Scholar]
- 15. Rintahaka PJ, Hirvonen J. The epidemiology of sudden infant death syndrome in Finland in 1969‐1980. Forensic Sci Int 1986; 30: 219–33. [DOI] [PubMed] [Google Scholar]
- 16. Mitchell EA, Ford RP, Stewart AW, Taylor BJ, Becroft DM, Thompson JM, et al. Smoking and the sudden infant death syndrome. Pediatrics 1993; 91: 893–6. [PubMed] [Google Scholar]
- 17. Blair PS, Fleming PJ, Bensley D, Smith I, Bacon C, Taylor E, et al. Smoking and the sudden infant death syndrome: results from 1993‐5 case‐control study for confidential inquiry into stillbirths and deaths in infancy. Confidential Enquiry into Stillbirths and Deaths Regional Coordinators and Researchers. BMJ 1996; 313: 195–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alm B, Milerad J, Wennergren G, Skjaerven R, Øyen N, Norvenius G, et al. A case‐control study of smoking and sudden infant death syndrome in the Scandinavian countries, 1992 to 1995. The Nordic Epidemiological SIDS Study. Arch Dis Child 1998; 78: 329–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ponsonby AL, Dwyer T, Kasl SV, Cochrane JA. The Tasmanian SIDS Case‐Control Study: univariable and multivariable risk factor analysis. Paediatr Perinat Epidemiol 1995; 9: 256–72. [DOI] [PubMed] [Google Scholar]
- 20. Wennergren G, Alm B, Øyen N, Helweg‐Larsen K, Milerad J, Skjaerven R, et al. The decline in the incidence of SIDS in Scandinavia and its relation to risk‐intervention campaigns. Nordic Epidemiological SIDS Study. Acta Paediatr 1997; 86: 963–8. [DOI] [PubMed] [Google Scholar]
- 21. Brooke H, Gibson A, Tappin D, Brown H. Case‐control study of sudden infant death syndrome in Scotland, 1992‐5. BMJ 1997; 314: 1516–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Skadberg BT, Morild I, Markestad T. Abandoning prone sleeping: effect on the risk of sudden infant death syndrome. J Pediatr 1998; 132: 340–3. [DOI] [PubMed] [Google Scholar]
- 23. Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet 2004; 363: 185–91. [DOI] [PubMed] [Google Scholar]
- 24. Mitchell EA, Milerad J. Smoking and the sudden infant death syndrome. Rev Environ Health 2006; 21: 81–103. [DOI] [PubMed] [Google Scholar]
- 25. Horne RS, Franco P, Adamson TM, Groswasser J, Kahn A. Influences of maternal cigarette smoking on infant arousability. Early Hum Dev 2004; 79: 49–58. [DOI] [PubMed] [Google Scholar]
- 26. Richardson HL, Walker AM, Horne RS. Maternal smoking impairs arousal patterns in sleeping infants. Sleep 2009; 32: 515–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carpenter R, McGarvey C, Mitchell EA, Tappin DM, Vennemann MM, Smuk M, et al. Bed sharing when parents do not smoke: is there a risk of SIDS? An individual level analysis of five major case‐control studies. BMJ Open 2013; 3: e002299. doi: 10.1136/bmjopen-2012-002299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cohen G, Jeffery H, Lagercrantz H, Katz‐Salamon M. Longterm reprogramming of cardiovascular function in infants of active smokers. Hypertension 2010; 55: 722–8. [DOI] [PubMed] [Google Scholar]
- 29. Scragg RK, Mitchell EA, Stewart AW, Ford RP, Taylor BJ, Hassall IB, et al. Infant room‐sharing and prone sleep position in sudden infant death syndrome. New Zealand Cot Death Study Group. Lancet 1996; 347: 7–12. [DOI] [PubMed] [Google Scholar]
- 30. Tappin D, Ecob R, Brooke H. Bedsharing, roomsharing, and sudden infant death syndrome in Scotland: a case‐control study. J Pediatr 2005; 147: 32–7. [DOI] [PubMed] [Google Scholar]
- 31. Blair PS, Sidebotham P, Evason‐Coombe C, Edmonds M, Heckstall‐Smith EM, Fleming P. Hazardous cosleeping environments and risk factors amenable to change: case‐control study of SIDS in south west England. BMJ 2009; 339: b3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blair PS, Sidebotham P, Pease A, Fleming PJ. Bed‐sharing in the absence of hazardous circumstances: is there a risk of sudden infant death syndrome? An analysis from two case‐control studies conducted in the UK. PLoS ONE 2014; 9: e107799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ip S, Chung M, Raman G, Trikalinos TA, Lau J. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med 2009; 4(Suppl 1): S17–30. [DOI] [PubMed] [Google Scholar]
- 34. Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta‐analysis. Pediatrics 2011; 128: 103–10. [DOI] [PubMed] [Google Scholar]
- 35. Helweg‐Larsen K, Lundemose JB, Øyen N, Skjaerven R, Alm B, Wennergren G, et al. Interactions of infectious symptoms and modifiable risk factors in sudden infant death syndrome. The Nordic Epidemiological SIDS study. Acta Paediatr 1999; 88: 521–7. [DOI] [PubMed] [Google Scholar]
- 36. Hofstetter AO, Saha S, Siljehav V, Jakobsson PJ, Herlenius E. The induced prostaglandin E2 pathway is a key regulator of the respiratory response to infection and hypoxia in neonates. Proc Natl Acad Sci U S A 2007; 104: 9894–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Siljehav V, Olsson Hofstetter A, Jakobsson PJ, Herlenius E. mPGES‐1 and prostaglandin E2: vital role in inflammation, hypoxic response, and survival. Pediatr Res 2012; 72: 460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta‐analysis Pediatrics 2005; 116: e716–23. [DOI] [PubMed] [Google Scholar]
- 39. Mitchell EA, Blair PS, L'Hoir MP. Should pacifiers be recommended to prevent sudden infant death syndrome? Pediatrics 2006; 117: 1755–8. [DOI] [PubMed] [Google Scholar]
- 40. Tonkin SL, Lui D, McIntosh CG, Rowley S, Knight DB, Gunn AJ. Effect of pacifier use on mandibular position in preterm infants. Acta Paediatr 2007; 96: 1433–6. [DOI] [PubMed] [Google Scholar]
- 41. Franco P, Scaillet S, Wermenbol V, Valente F, Groswasser J, Kahn A. The influence of a pacifier on infants’ arousals from sleep. J Pediatr 2000; 136: 775–9. [PubMed] [Google Scholar]
- 42. Hanzer M, Zotter H, Sauseng W, Pfurtscheller K, Müller W, Kerbl R. Pacifier use does not alter the frequency or duration of spontaneous arousals in sleeping infants. Sleep Med 2009; 10: 464–70. [DOI] [PubMed] [Google Scholar]
- 43. Odoi A, Andrew S, Wong FY, Yiallourou SR, Horne RS. Pacifier use does not alter sleep and spontaneous arousal patterns in healthy term‐born infants. Acta Paediatr 2014; 103: 1244–50. [DOI] [PubMed] [Google Scholar]
- 44. Horne RS, Hauck FR, Moon RY, L'Hoir MP, Blair PS. Physiology and Epidemiology Working Groups of the International Society for the Study and Prevention of Perinatal and Infant Death . Dummy (pacifier) use and sudden infant death syndrome: potential advantages and disadvantages. J Paediatr Child Health 2014; 50: 170–4. [DOI] [PubMed] [Google Scholar]
- 45. van Vlimmeren LA, van der Graaf Y, Boere‐Boonekamp MM, L'Hoir MP, Helders PJ, Engelbert RH. Risk factors for deformational plagiocephaly at birth and at 7 weeks of age: a prospective cohort study. Pediatrics 2007; 119: e408–18. [DOI] [PubMed] [Google Scholar]
- 46. McKinney CM, Cunningham ML, Holt VL, Leroux B, Starr JR. A case‐control study of infant, maternal and perinatal characteristics associated with deformational plagiocephaly. Paediatr Perinat Epidemiol 2009; 23: 332–45. [DOI] [PubMed] [Google Scholar]
- 47. Cavalier A, Picot MC, Artiaga C, Mazurier E, Amilhau MO, Froye E, et al. Prevention of deformational plagiocephaly in neonates. Early Hum Dev 2011; 87: 537–43. [DOI] [PubMed] [Google Scholar]
- 48. Bialocerkowski AE, Vladusic SL, Wei NgC. Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol 2008; 50: 577–86. [DOI] [PubMed] [Google Scholar]
- 49. Dageville C, Pignol J, De Smet S. Very early neonatal apparent life‐threatening events and sudden unexpected deaths: incidence and risk factors. Acta Paediatr 2008; 97: 866–9. [DOI] [PubMed] [Google Scholar]
- 50. Andres V, Garcia P, Rimet Y, Nicaise C, Simeoni U. Apparent life‐threatening events in presumably healthy newborns during early skin‐to‐skin contact. Pediatrics 2011; 127: e1073–6. [DOI] [PubMed] [Google Scholar]
- 51. Poets A, Urschitz MS, Steinfeldt R, Poets CF. Risk factors for early sudden deaths and severe apparent life‐threatening events. Arch Dis Child Fetal Neonatal Ed 2012; 97: F395–7. [DOI] [PubMed] [Google Scholar]
- 52. Pejovic NJ, Herlenius E. Unexpected collapse of healthy newborn infants: risk factors, supervision and hypothermia treatment. Acta Paediatr 2013; 102: 680–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lagercrantz H. Mängder av hypoteser om plötslig spädbarnsdöd … men inget genomslag [Numerous hypotheses about sudden infant death… but no impact]. Läkartidningen 2014; 111: 1572–4. [PubMed] [Google Scholar]
- 54. Filiano JJ, Kinney HC. A perspective on neuropathologic findings in victims of the sudden infant death syndrome: the triple‐risk model. Biol Neonate 1994; 65: 194–7. [DOI] [PubMed] [Google Scholar]
- 55. Trachtenberg FL, Haas EA, Kinney HC, Stanley C, Krous HF. Risk factor changes for sudden infant death syndrome after initiation of Back‐to‐Sleep campaign. Pediatrics 2012; 129: 630–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bergman NJ. Proposal for mechanisms of protection of supine sleep against sudden infant death syndrome: an integrated mechanism review. Pediatr Res 2015; 77: 10–9. [DOI] [PubMed] [Google Scholar]


