Abstract
Objective
To investigate whether public knowledge, attitudes, desire for social distance and reported contact in relation to people with mental health problems have improved in England during the Time to Change (TTC) programme to reduce stigma and discrimination 2009–2015.
Methods
Using data from an annual face‐to‐face survey of a nationally representative sample of adults, we analysed longitudinal trends in the outcomes with regression modelling using standardised scores of the measures overall and by age and gender subgroups.
Results
There were improvements in all outcomes. The improvement for knowledge was 0.17 standard deviation units in 2015 compared to 2009 (95% CI 0.10, 0.23); for attitudes 0.20 standard deviation units (95% CI 0.14, 0.27) and for social distance 0.17 standard deviation units (95% CI 0.11, 0.24). Survey year for 2015 vs. 2009 was associated with a higher likelihood of reported contact (OR 1.32, 95% CI 1.13, 1.53). Statistically significant interactions between year and age suggest the campaign had more impact on the attitudes of the target age group (25–45) than those aged over 65 or under 25. Women's reported contact with people with mental health problems increased more than did men's.
Conclusion
The results provide support for the effectiveness of TTC.
Keywords: social stigma, public opinion, attitude, social distance, discrimination
Significant outcomes.
During the course of the Time to Change programme to reduce stigma and discrimination in England over 2009–2015, improvements among representative samples of the adult population were observed initially in attitudes, desire for social distance and reported contact; these were followed by improvements in stigma‐related knowledge.
Lived experience of a mental health problem had the strongest positive association with all outcomes out of the variables measured.
The effects of survey year on attitudes and reported contact were modified by age and gender. This suggests that the campaign had more impact on the attitudes of the target age group (25–45) than those aged over 65 or under 25 and that women's reported contact with people with mental health problems increased more than did men's.
Limitations.
There was no control group. TTC is a long‐term, national programme, and it was not possible to conduct the same survey in another part of the UK.
As data are collected via self‐report, we cannot be sure to what extent social desirability and agreement bias affected responses
The evaluation does not distinguish responses regarding common mental disorders, with which respondents are more likely to be familiar, from responses to less prevalent illnesses. It cannot therefore be assumed that the changes in the outcomes observed over time apply equally to disorders such as depression and those such as schizophrenia.
Introduction
Stigma and discrimination against people with mental health problems have substantial public health impact in England, creating and maintaining inequalities 1 including the following: poor access to mental and physical health care 2; reduced life expectancy 3, 4; exclusion from higher education 5, 6 and employment 7; increased risk of contact with criminal justice systems; victimisation 8; poverty and homelessness.
Typically, research on stigma has focussed on the measurement of knowledge and attitudes. It could be argued that these are less important than the actual experiences of stigma among people with mental health problems as reported by Corker et al. in this supplement 9; however, research suggests that there is a link between public stigma and these individual experiences 10. Internationally, public attitude data suggest that there has been little improvement in stigma over time 11 where there have been no specific programmes to reduce stigma. Indeed, relative to Scotland, which initiated the national antistigma initiative ‘See Me’ in 2002, attitudes in England showed relative worsening between 2000 and 2003 12.
In some high‐income countries, there is growing investment in and evidence for the effectiveness of antistigma interventions, both national programmes and those targeted to specific groups 13. The National Institute for Health and Clinical Excellence emphasises the inclusion of knowledge, attitude and behavioural components when developing and evaluating behaviour change interventions 14. Applying this to antistigma interventions requires the evaluation of: lack of knowledge and misinformation such as stereotypes; prejudicial attitudes and emotional reactions such as fear and anger; and discriminatory behaviour 15, 16.
In England, the current national programme against stigma and discrimination is Time to Change (TTC) 17, 18, delivered by the charities Mind and Rethink Mental Illness. Its first phase ran from 2007 to 2011, including a social marketing campaign launched in January 2009 19 and work with target groups 20, 21. TTC's targets for this first phase included a 5% positive shift in public attitudes towards mental health problems and a 5% reduction in discrimination by 2012. The first of these targets was assessed using the national Attitudes to Mental Illness survey 22, which is also the survey we report on here. Since 2009, this has also included measures of stigma‐related knowledge 23; desire for social distance, and reported contact with someone with a mental illness 24. Between 2009 and 2012, there was a significant improvement in desire for social distance and a trend towards more positive attitudes (P = 0.08), but no change in knowledge or reported contact 25. There was greater evidence for a reduction in discrimination as reported by mental health service users across a number of areas of life, particularly in informal relationships, although the proportion reporting no discrimination in any life area did not increase by 5% as per the target 26.
The second phase of TTC was funded for 2011–2015. During this phase, the UK Department (Ministry) of Health applied three outcome measures used for the TTC evaluation to monitor the impact of an objective of its mental health policy, ‘No Health Without Mental Health’, that ‘fewer people will experience stigma and discrimination’ 27, 28. Two measures were among those reported here: public attitudes and mental health‐related knowledge. The third was mental health service users’ experiences of discrimination, as reported in pages xx‐xx of this issue 9. The same targets of 5% improvements in public attitudes and service users’ experiences of discrimination, as fro Phase 1, were also chosen for Phase 2.
Aims of the study
This study examines longitudinal trends in mental health‐related knowledge, attitudes to mental illness, desire for social distance and reported contact with people with mental illness among the general public in England over the course of Time to Change (TTC). We investigate whether these outcomes have improved as the inception of TTC and if so at what time point and for which demographic groups.
Material and methods
Data source
The Attitudes to Mental Illness survey is conducted by the agency Taylor Nelson Sofres as part of an Omnibus Survey and has been carried out annually since 2008 as a part of the TTC evaluation. TTC received funding in October 2007, and the first events were run in October 2008, coinciding with World Mental Health Day. The measures of knowledge, desire for social distance and reported contact were added to the pre‐existing attitude measure in 2009, shortly before the start of the social marketing campaign activity. The baseline for attitudes is therefore 2008, and for the other outcomes 2009. Thus, the survey provides baseline and follow‐up indicators of mental health‐related knowledge, attitudes, desire for social distance and reported contact among a nationally representative sample of adults residing in England. There were approximately 1700 respondents surveyed each year from 2008 to 2015. The survey is carried out using a quota sample, with sample points selected by a random location methodology. Census small area statistics and the Postcode Address File were used to define sample points which were stratified by Government Office Region and social status.
The whole sample had slightly higher representation of individuals in lower socio‐economic classes compared to individuals from middle and upper socio‐economic classes; this has been corrected through sample weighting. The sample included 46.5% men and 53.5% women, and the mean age was approximately 48 years, ranging from 16 to 98 years of age (SD = 19.3).
Interviews were carried out in participants’ homes by fully trained personnel using computer‐assisted personal interviewing and demographic information was collected at the end of the interview. Additional information regarding the survey methods can be found at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsStatistics/DH_114795.
Measures
Mental health‐related knowledge
Mental health‐related knowledge was measured by the Mental Health Knowledge Schedule (MAKS) 23. The MAKS comprises six items covering stigma‐related mental health knowledge areas: help seeking, recognition, support, employment, treatment, and recovery, and six items that inquire about classification of various conditions as mental illnesses 29. Overall test–retest reliability of the MAKS is 0.71 (Lin's concordance statistic), and the overall internal consistency among items is 0.65 (Cronbach's α) 23. The total score is calculated so that higher MAKS scores indicate greater knowledge.
Mental health‐related attitudes
The UK Department of Health Attitudes to Mental Illness questionnaire was developed in 1993 based on previous research in Toronto, Canada and the West Midlands, England. It includes 26 items from the 40‐item Community Attitudes towards the Mentally Ill scale (CAMI) 30 and an added item on employment‐related attitudes. Items refer to attitudes about social exclusion, benevolence, tolerance and support for community mental health care and were rated from 1 (strong disagreement) to 5 (strong agreement). The total score is calculated so that higher CAMI scores indicate less stigmatising attitudes. Its overall internal consistency in these data measured using Cronbach's α is 0.87.
Desire for social distance and reported contact
These were measured using the Reported and Intended Behaviour Scale (RIBS) 24. We assessed changes for four different contexts (domains comprised: living with, working with, living nearby and continuing a relationship with someone with a mental health problem) which were derived from the Star Social Distance Scale 31, 32. Four items assessed the level of desired future contact with people with mental health problems, and an additional four items assessed past or current contacts. Overall test–retest reliability of the RIBS is 0.75 (Lin's concordance statistic). The overall internal consistency of the scale is 0.85 (Cronbach's α). The total social distance score is calculated so that higher scores indicate less desire for social distance; likewise, for reported contact, higher scores indicate more types of contact.
Socio‐economic status
Socio‐economic status (SES) of the respondent was categorised into one of four categories (i.e. AB, C1, C2 and DE) according to the Market Research Society's classification system 33. Classification was based on the occupation of the chief income earner in the household. Category AB represents individuals with professional/managerial occupations, C1 represents individuals with other non‐manual occupations, C2 represents individuals having skilled manual occupations and DE represents individuals with semi‐/unskilled manual occupations and people dependent on state benefits.
Familiarity with mental health problems
Previous research demonstrates that knowing someone with a mental health problem/familiarity with mental illness is strongly associated with mental health‐related knowledge, attitudes and desire for social distance 19, 25, 34, 35. We measured familiarity using the following item: Who is the person closest to you who has or has had some kind of mental illness? Potential response options included the following: immediate family (spouse/child/sister/brother/parent etc.), partner (living with you), partner (not living with you), other family (uncle/aunt/cousin/grandparent etc.), friend, acquaintance, work colleague, self, other and no one known. Responses were then categorised into three groups: self, other and none.
Statistical analysis
We calculated basic descriptive statistics for participant characteristics in addition to all knowledge, attitude, social distance and contact items by year. All statistical analyses were weighted by gender, age and ethnicity to reflect population characteristics in England available from the UK Government's Office for National Statistics (ons.gov.uk). To avoid inflation of type I error due to multiple testing, statistical tests for annual changes were only performed on total instrument scores rather than for each item. Three separate multiple linear regression models examined the following: (i) total knowledge (as measured by total standardised MAKS score based on the first six items); (ii) attitudes (as measured by total standardised CAMI score); and (iii) desire for social distance (as measured by total standardised RIBS score), using survey data between the start of the TTC programme in 2009 and the completion of phase two of TTC in 2015. As the CAMI has been used in the survey since its inception, we used 2008 as the reference year. To measure changes in reported contact in any of the four contexts, logistic regression was used. As all the models used the standardised scores of the measures as the dependent variables, the interpretation of the outputs was equivalent to that when running standardised regression models, where the amount of change in the dependent variable in standard deviation units is denoted by one standard deviation unit change in the independent variable. All of the models included year as a fixed effect in the form of a categorical variable. We chose this as opposed to a continuous variable to assess change year by year; this is more informative for studying a programme such as TTC, the content of which has changed over time, both in terms of the content of the social marketing campaign and the relative emphasis on other components of the programme. Covariates included in each regression model included the following: gender (female vs. male), age (categorical: 16–24, 25–44, 45–64 and 65+), ethnicity (categorical: Asian, Black, other and White), SES (categorical: AB, C1, C2 and DE) and familiarity with mental health problems (categorical: self, other none). Interactions were tested between the covariates and survey year by adding interaction terms separately to the original models to test whether the change in knowledge, attitude, desire for social distance and reported contact by year differed depending on subgroups of the survey population. Two specific hypotheses were tested based on the target group for the social marketing campaign, namely that change over time would appear earlier and/or be greater for people aged 25–45 and in the income groups AB, C1 and C2. Although the target group does not include the highest SES subgroup A, it was not possible to separate these respondents from SES B from the data collection. We also included exploratory analyses undertaken to assess whether there is any evidence that TTC may have had a differential impact on different demographic groups year by year; such information can then be used to further develop aspects of the programme. However, survey sampling weights were applied in all analyses so that respondents reflected a nationally representative sample in terms of sociodemographic characteristics within each region of England. Analyses were carried out using STATA version 11.2 (StataCorp LP College Station, Texas USA).
This study was classified as exempt from the need for research ethics committee approval by the King's College London, Psychiatry, Nursing and Midwifery Research Ethics Subcommittee.
Results
Sample characteristics and stigma item responses by year
Table 1 provides details of the sample participants in terms of sociodemographic characteristics, stratified by year. Further detail of the stigma‐related knowledge, attitudes, social distance and reported contact responses can be found in the Appendix S1–S3, at the item level.
Table 1.
Participant characteristics by survey year, unweighted frequency and weighted per cent
| 2009 (n = 1751) | 2010 (n = 1745) | 2011 (n = 1741) | 2012 (n = 1717) | 2013 (n = 1727) | 2014 (n = 1714) | 2015 (n = 1736) | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| F | 939 (51.5) | 939 (51.7) | 912 (51.5) | 924 (51.3) | 926 (51.0) | 893 (50.9) | 919 (51.6) |
| M | 812 (48.5) | 806 (48.3) | 829 (48.5) | 793 (48.7) | 801 (49.0) | 821 (49.1) | 817 (48.4) |
| Age mean (SD) | 46.0 (18.8) | 46.5 (18.4) | 46.4 (19.2) | 46.4 (19.1) | 45.9 (18.3) | 46.0 (18.8) | 46.4 (19.2) |
| Age group | |||||||
| 16–24 | 247 (14.3) | 240 (14.6) | 235 (14.4) | 258 (14.6) | 289 (14.6) | 221 (14.4) | 242 (14.1) |
| 25–44 | 633 (35.9) | 540 (35.1) | 545 (35.4) | 580 (34.8) | 568 (36.1) | 514 (36.2) | 528 (35.3) |
| 45–64 | 512 (31.3) | 549 (31.5) | 499 (30.6) | 506 (31.3) | 486 (31.1) | 506 (30.6) | 488 (31.5) |
| 65+ | 359 (18.5) | 416 (19.4) | 462 (19.5) | 373 (19.3) | 384 (18.3) | 473 (18.7) | 478 (19.0) |
| Ethnicity | |||||||
| Asian | 112 (6.2) | 136 (8.5) | 134 (8.1) | 160 (9.7) | 127 (7.9) | 105 (6.6) | 120 (6.7) |
| Black | 63 (3.4) | 88 (4.9) | 64 (3.8) | 67 (3.8) | 66 (3.7) | 69 (4.0) | 99 (5.3) |
| Other | 26 (1.4) | 18 (1.1) | 20 (1.1) | 31 (1.8) | 44 (2.6) | 26 (1.6) | 39 (2.3) |
| White | 1542 (89.0) | 1496 (85.5) | 1504 (87.0) | 1449 (84.7) | 1474 (85.9) | 1507 (87.8) | 1472 (85.7) |
| SES | |||||||
| AB (high‐SES) | 279 (19.4) | 300 (20.2) | 322 (20.5) | 292 (19.3) | 302 (20.5) | 353 (21.4) | 335 (22.2) |
| C1 | 454 (32.2) | 464 (31.7) | 450 (29.8) | 456 (31.0) | 445 (30.4) | 457 (29.2) | 432 (28.4) |
| C2 | 389 (20.8) | 342 (19.2) | 340 (21.1) | 368 (21.6) | 362 (20.8) | 333 (20.5) | 354 (20.4) |
| DE (low‐SES) | 629 (27.6) | 639 (28.8) | 629 (28.6) | 601 (28.1) | 618 (29.1) | 571 (29.0) | 615 (29.1) |
| Familiarity with mental health problems | |||||||
| Self | 92 (5.0) | 75 (4.2) | 90 (5.6) | 111 (6.4) | 120 (6.6) | 126 (7.4) | 124 (6.9) |
| Other | 902 (54.0) | 892 (53.0) | 896 (53.5) | 926 (55.9) | 963 (57.9) | 953 (57.5) | 963 (58.1) |
| None | 718 (41.0) | 738 (42.8) | 706 (41.0) | 645 (37.7) | 610 (35.5) | 606 (35.1) | 632 (35.0) |
SES, socio‐economic status.
Changes in public knowledge
There were significant improvements in overall knowledge score in 2014 and 2015 compared to 2009 (see Table 2); respondents in 2014 and 2015 scored 0.12 and 0.17 standard deviation units higher on the MAKS respectively. There was also a pattern of increasing levels of agreement with all items, including those that are incorrect regarding help‐seeking behaviour and whether grief and stress and mental illnesses. Figure 1 (blue squares) shows the predicted margins (predicted standardised scores holding all other variables at their means) and their confidence intervals, for each survey year, corresponding to the standardised effects estimated in the linear regression models. There were no significant interactions between year and the model covariates in relation to the MAKS score. There were also no significant interactions between year and SES for any of the outcomes; although this covariate is consistently a significant predictor, the change in scores over time does not differ depending on the SES subgroup.
Table 2.
Regression analysis of predictors of mental health‐related knowledge, attitudes and behaviour among the general public, as measured by standardised MAKS (first six items), CAMI and RIBS scores
| Predictors | Standardised MAKS score (n = 11824) | Standardised CAMI score (n = 13432) | Standardised RIBS (intended behaviour) score (n = 11824) | Standardised RIBS (reported behaviour) score (n = 12058) | ||||
|---|---|---|---|---|---|---|---|---|
| Standardised effect sizeb (95% CI) | P‐value | Standardised effect sizeb (95% CI) | P‐value | Standardised effect sizeb (95% CI) | P‐value | Adjusted odds ratioc (95% CI) | P‐value | |
| Year | ||||||||
| 2015 | 0.17a (0.10, 0.23) | <0.001 | 0.20a (0.14, 0.27) | <0.001 | 0.17a (0.11, 0.24) | <0.001 | 1.32a (1.13, 1.53) | <0.001 |
| 2014 | 0.12a (0.06, 0.19) | <0.001 | 0.18a (0.12, 0.24) | <0.001 | 0.18a (0.12, 0.24) | <0.001 | 1.18a (1.02, 1.37) | 0.025 |
| 2013 | 0.03 (−0.04, 0.10) | 0.383 | 0.09a (0.03, 0.15) | 0.006 | 0.11a (0.05, 0.17) | <0.001 | 1.20a (1.04, 1.40) | 0.014 |
| 2012 | 0.03 (−0.03, 0.10) | 0.309 | 0.06 (−0.01, 0.12) | 0.075 | 0.08a (0.01, 0.14) | 0.020 | 1.01 (0.88, 1.17) | 0.848 |
| 2011 | −0.01 (−0.08, 0.06) | 0.767 | 0.02 (−0.04, 0.09) | 0.465 | 0.03 (−0.03, 0.10) | 0.337 | 0.95 (0.82, 1.10) | 0.462 |
| 2010 | −0.02 (−0.09, 0.04) | 0.470 | 0.07a (0.01, 0.14) | 0.024 | 0.09a (0.03, 0.16) | 0.003 | 0.95 (0.82, 1.10) | 0.482 |
| 2009 (ref) | – | – | 0.00 (−0.06, 0.06) | 0.993 | – | – | – | – |
| 2008 (CAMI ref) | – | – | ||||||
| Gender | ||||||||
| F | 0.15a (0.11, 0.19) | <0.001 | 0.16a (0.13, 0.19) | <0.001 | −0.03 (−0.06, 0.00) | 0.087 | 1.38a (1.27, 1.49) | <0.001 |
| M (ref) | – | – | – | – | – | – | – | – |
| Age | ||||||||
| 16–24 | 0.02 (−0.04, 0.08) | 0.416 | 0.00 (−0.05, 0.05) | 1.00 | 0.51a (0.46, 0.57) | <0.001 | 0.94 (0.83, 1.08) | 0.390 |
| 25–44 | 0.15a (0.10, 0.20) | <0.001 | 0.13a (0.09, 0.18) | <0.001 | 0.46a (0.41, 0.50) | <0.001 | 1.50a (1.36, 1.67) | <0.001 |
| 45–64 | 0.23a (0.18, 0.28) | <0.001 | 0.25a (0.20, 0.29) | <0.001 | 0.40a (0.36, 0.45) | <0.001 | 2.04a (1.84, 2.27) | <0.001 |
| 65+ (ref) | – | – | – | – | – | – | – | – |
| Ethnicity | ||||||||
| Asian | −0.11a (−0.18, −0.05) | 0.001 | −0.55a (−0.60, −0.49) | <0.001 | −0.46a (−0.53, −0.39) | <0.001 | 0.25a (0.21, 0.29) | <0.001 |
| Black | −0.07 (−0.15, 0.02) | 0.128 | −0.50a (−0.58, −0.43) | <0.001 | −0.35a (−0.44, −0.26) | <0.001 | 0.61a (0.50, 0.74) | <0.001 |
| Other | 0.03 (−0.16, 0.10) | 0.687 | −0.33a (−0.45, −0.20) | <0.001 | −0.25a (−0.37, −0.13) | <0.001 | 0.70a (0.53, 0.94) | 0.017 |
| White (ref) | – | – | – | – | – | – | – | |
| SES | ||||||||
| AB (high‐SES) | 0.31a (0.26, 0.37) | <0.001 | 0.36a (0.32, 0.41) | <0.001 | 0.27a (0.22, 0.31) | <0.001 | 1.79a (1.60, 2.01) | <0.001 |
| C1 | 0.18a (0.14, 0.23) | <0.001 | 0.26a (0.22, 0.30) | <0.001 | 0.18a (0.14, 0.22) | <0.001 | 1.27a (1.14, 1.40) | <0.001 |
| C2 | 0.10a (0.05, 0.15) | <0.001 | 0.14a (0.09, 0.18) | <0.001 | 0.12a (0.07, 0.17) | <0.001 | 1.10a (0.99, 1.23) | 0.073 |
| DE (low‐SES) (ref) | – | – | – | – | – | – | – | – |
| Familiarity with mental health problems | ||||||||
| Self | 0.76a (0.68, 0.84) | <0.001 | 0.85a (0.79, 0.91) | <0.001 | 0.82a (0.76, 0.88) | <0.001 | NA | NA |
| Other | 0.45a (0.40, 0.49) | <0.001 | 0.54a (0.51, 0.57) | <0.001 | 0.54a (0.51, 0.58) | <0.001 | NA | NA |
| None (ref) | – | – | – | – | – | – | NA | NA |
MAKS, Mental Health Knowledge Schedule; CAMI, Community Attitudes towards the Mentally Ill; RIBS, Reported and Intended Behaviour Scale; SES, socio‐economic status.
Statistically significant at the P < 0.05 level.
Multiple linear regression.
Logistic regression.
Figure 1.
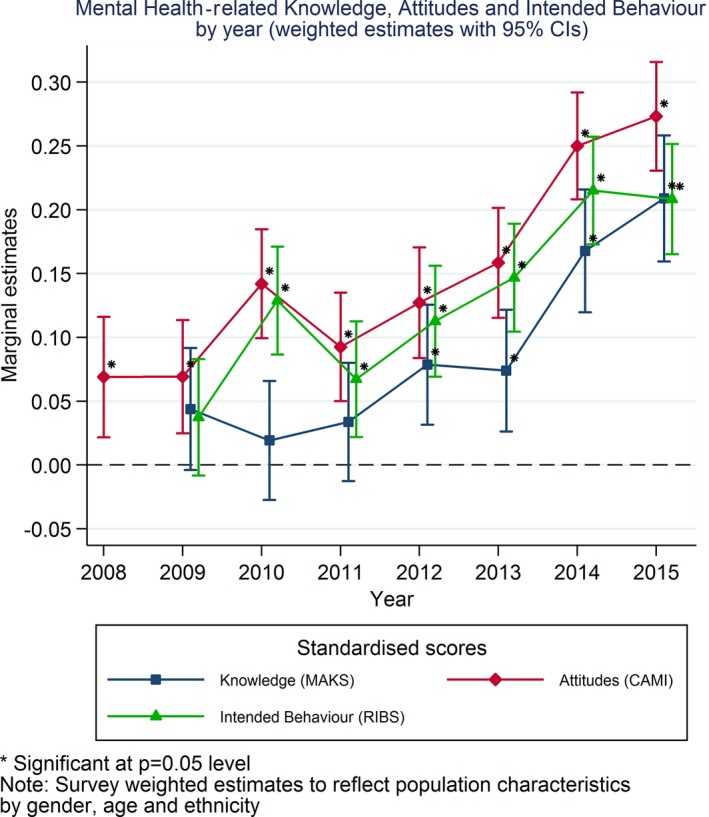
Mental health related knowledge, attitudes and intended behaviour by year (weighted estimates with 95% CIs). Significant at P = 0.05 level. Note: Survey weighted estimates to reflect population characteristics by gender, age and ethnicity.
Changes in public attitudes
Attitudes showed significant improvement in 2010, and again in 2013–2015. Relative to 2008, respondents in 2010 and 2013–2015 scored 0.07, 0.09, 0.18 and 0.20 standard deviation units higher on the CAMI (see Fig. 1‐ red diamond). These improvements were also tested for both factors of the CAMI score as it is considered to have two dimensions; prejudice/exclusion and tolerance/support for community care. Figure 2 shows that the improvements were indeed relevant to both of these subscales within CAMI. There was a significant interaction between year and age for the CAMI score (adjusted Wald test P = 0.002). Figure 3a shows the margins by age group at all follow‐up years. This shows a main effect of age whereby the youngest and eldest groups started off with lower scores at baseline. However, there were varying patterns of change over time among age groups; the two eldest groups had the least change over time. In the last few years, the target group 11, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43 has showed a stronger improvement, and the youngest group has bridged the gap to mid‐age individuals.
Figure 2.
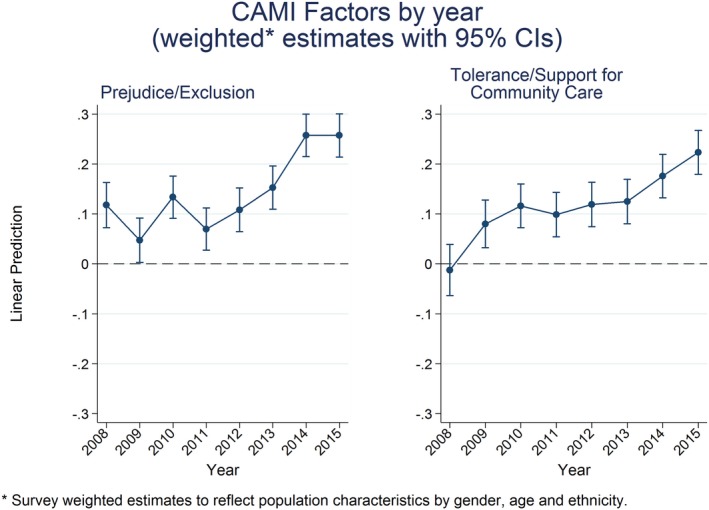
Community Attitudes towards the Mentally Ill factors by year weighted* estimates with 95% CIs). *Survey weighted estimates to reflect population characteristic by gender, age and ethnicity.
Figure 3.
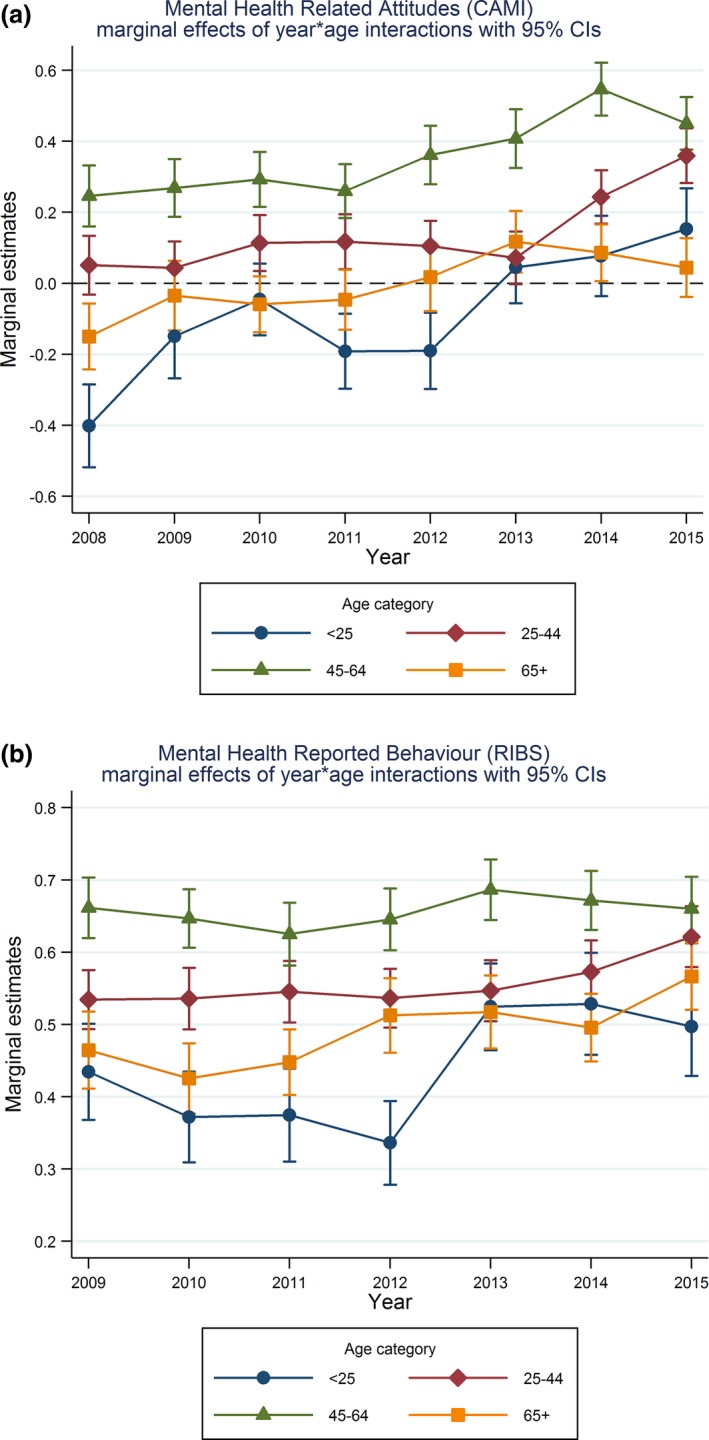
(a) Mental health related attitudes (Community Attitudes towards the Mentally Ill) marginal effects of year*age interactions with 95% CIs. (b) Mental health related behaviour (Reported and Intended Behaviour Scale) marginal effects of year*age interactions with 95% CIs.
Changes in desire for social distance
Responses regarding social distance improved significantly from 2009 to 2010 and to 2012–2015; respectively, respondents scored 0.09, 0.03, 0.11, 0.18 and 0.17 standard deviation units higher on the RIBS intended behaviour subscale. There were no significant interactions between year of follow‐up and the model covariates in relation to the RIBS intended behaviour score.
Changes in reported contact
Figure 4 shows odds ratios with confidence intervals for each year compared to 2009 on the RIBS reported behaviour score. There was a significant positive change in reported contact in 2013–2015 compared with 2009. There were significant interactions between year and sex for the RIBS reported behaviour score (adjusted Wald tests P = 0.01), and an indication of a possible interaction between year and age (Wald P = 0.08). Figure 3b shows the differential pattern of change by age which is similar to that of the CAMI score, with the eldest and youngest groups starting on lower scores and showing limited improvement. The target group 25–44 benefited best in the last years, with 45‐ to 64‐year‐old individuals managing the least change over time. Figure 5 suggests that females have responded better to the campaign fairly consistently each year compared to males, whose scores remain unchanged throughout follow‐up.
Figure 4.
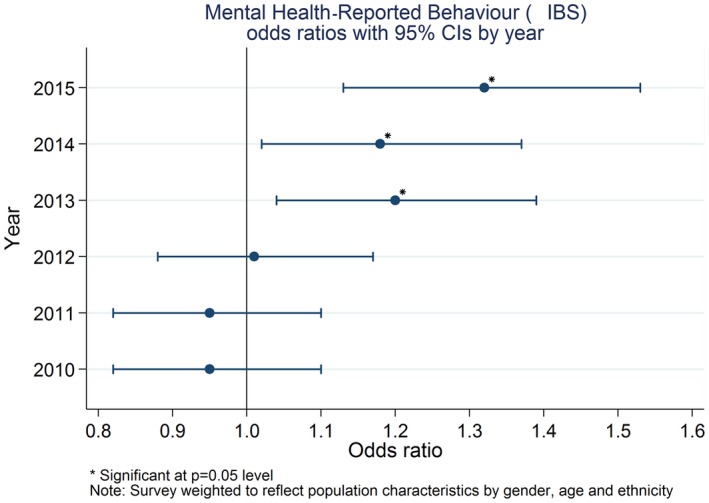
Mental health reported behaviour (Reported and Intended Behaviour Scale) odds ratios with 95% CIs by year. Significant at P = 0.05 level. Note: Survey weighted to reflect population characteristics by gender, age and ethnicity.
Figure 5.
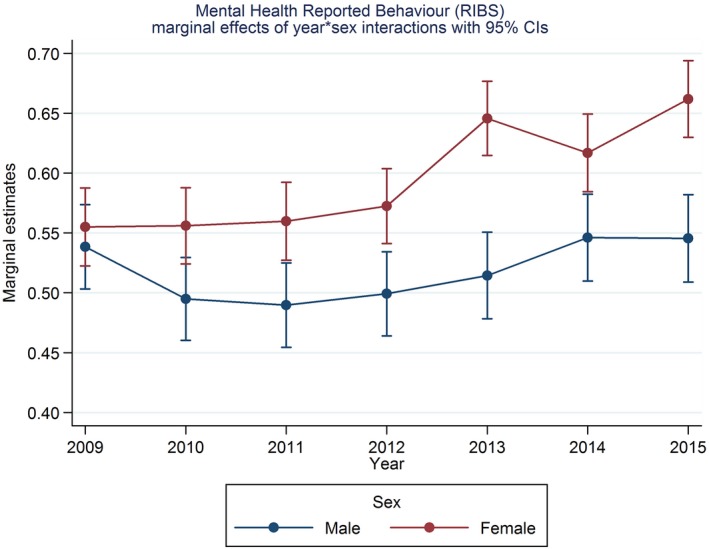
Mental health related behaviour (Reported and Intended Behaviour Scale) marginal effects of year*sex interactions with 95% CIs.
Discussion
Our findings indicate that between 2009 and 2015, there were improvements in all of: knowledge, attitudes, desire for social distance and reported contact in relation to people with mental illness. While early improvements were seen in attitudes and social distance, the latter has been the more consistent and has been followed by an increase in reported contact with people with mental health problems. These results are consistent with the evidence for a reduction in discrimination as reported by mental health service users over the course of TTC 9, 36. In contrast to attitudes, desire for social distance and reported contact, the improvement in knowledge from 2009 is only evident since 2014. Thus, in comparison with the mixed results apparent at the end of the first phase of TTC 24, the outcomes at the end of its second phase show a more consistent positive pattern.
While the pattern of an initial impact on attitudes, desire for social distance and reported contact rather than stigma‐related knowledge is consistent with the content of the social marketing campaign, it is nonetheless worth noting that changes in attitudes and behaviour are not dependent upon and may occur prior to changes in knowledge. The increases observed for all items regarding what is conceived of as a mental illness may be having a mixed effect on the other outcomes; agreement that stress and grief are mental illnesses may be associated with more negative attitudes and greater desire for social distance, while agreement regarding depression, bipolar disorder and schizophrenia is associated with more positive attitudes and reduced desire for social distance 29. It is also worth noting that incorrect responses to the help‐seeking question are increasing along with correct responses to the other questions in the first section of the MAKS. The positive phrasing of all these items, while increasing their comprehensibility, may also increase problems due to agreement bias 37, but it is not clear why this might increase over time. Alternatively, the response to the help‐seeking question may reflect an increasingly positive attitude to professional help seeking.
The differing response patterns for different age categories for attitudes and reported contact are also consistent with the social marketing campaign, which from 2009 has targeted people aged 25–45. This age group has shown a steady improvement in these outcomes, in contrast to a more recent positive change among younger people and little change among older people. The lack of change among men compared to women in terms of reported contact suggests that while there may be an impact on men's behaviour of the campaign, this is not detectable to other men; for example, they may disclose only to female friends or partners, so that only women report an increase in contact. A more tailored campaign may therefore be needed to affect behaviour in relation to men. This finding did not emerge until the end of the second phase of TTC, as during the first phase no significant change in reported contact was observed; this illustrates the need for long antistigma programmes to be not only prolonged but also responsive to continued evaluation.
Our results are consistent with those of the survey carried out in Sweden over the course of the antistigma campaign Hjärnkoll 38; this survey also used the MAKS and RIBS along with another version of the CAMI, but used online data collection instead of face to face. The results of our study and the Swedish one are in contrast to surveys in other countries lacking antistigma campaigns (at the time points when data were collected) which have generally shown no change or even a negative trend in attitudes and desire for social distance, despite improvements in public knowledge 11, 39. However, knowledge in these studies is measured as endorsement of causal explanations for mental illness and types of treatment, while the MAKS covers only the latter but also focuses on stigma‐related knowledge 23.
Strengths and limitations of the study
This study used a large nationally representative dataset which included baseline measures specifically targeted and developed for the evaluation of the TTC programme. Despite these strengths, there are some limitations associated with this study. Because there was no control group, it is impossible to know what would have happened without the TTC programme and how much of the change can be attributed to the TTC programme. We have established that following a deterioration in attitudes between 2000 and 2003 12, from 2003 attitudes were improving and that improvement above this trend is only evident for the prejudice and exclusion factor of CAMI 40, but we do not have data on knowledge or behaviour to study pre‐existing trends in these outcomes. However, results of a Cochrane systematic review 11 to assess the effects of mass media interventions on reducing stigma compared to inactive and other controls indicate that mass media interventions may have a small‐to‐medium effect in decreasing prejudice. TTC includes a mass media element in addition to other components, suggesting that the changes observed may reflect a similar response to that seen in the controlled studies. It is also possible that the economic downturn and policies which have been implemented in response may have influenced the outcomes. An additional limitation is that we did not collect information about awareness or engagement with the TTC campaign in years 2009–2011 of this survey, and thus, we only know the extent to which campaign awareness is associated with knowledge, attitudes and behaviour in the later years 41. This information was later added to the end of the survey so as not to risk biasing the outcome measures. As data are collected via face‐to‐face interviews, we cannot be sure to what extent social desirability affected responses 37; further, awareness of TTC may increase the effect on the measures of social desirability. Last, the evaluation does not distinguish responses regarding common mental disorders, with which respondents are more likely to be familiar, from responses to less prevalent illnesses.
Implications
These findings provide support for the effectiveness of the TTC national antistigma programme in improving reported and intended behaviour, attitudes and mental health‐related knowledge. They further suggest that local and national activities such as those delivered by TTC may work together to address a range of antistigma outcomes. Additional research is needed to better understand the relative contributions of different types of interventions when delivered locally vs. nationally via mass media and how to deliver them according to best practices, that is in a targeted, local, credible and repeated manner 42, 43. Differences in stigma‐related outcomes and in change over time by sociodemographic characteristics noted in the results suggest potential target groups for future antistigma work. Men have been suggested to be particularly affected by stigma in terms of being deterred from seeking treatment 44, 45. Qualitative findings suggest the importance of considering culture and beliefs in the development of antistigma interventions and that tailored interventions might improve engagement 46, 47. TTC included specific local projects with members of the South Asian and African Caribbean communities, and during Phase 2, the social marketing campaign used media which are relatively more effective in reaching Black and ethnic minority groups, including radio. So far, the social marketing campaign has been targeted towards the mid‐age range; middle‐income groups 48. Furthermore, evaluation of programme outcomes locally as well as nationally may be important as there may be differences in local needs, and reception of and reactions to different campaign messages. Finally, further work is required to understand the effective ingredients of TTC and other programmes and to determine whether their impact is sustained beyond the duration of the interventions.
Funding
Time to Change programme, grants from UK Department of Health and Comic Relief.
Declaration of interest
GT has received grants for stigma‐related research in the past 5 years from the National Institute for Health Research and has acted as a consultant to the UK Office of the Chief Scientist. SEL and CH have received consulting fees from Lundbeck. The other authors declare no conflict of interest. No authors participated in the planning or execution of Time to Change.
Supporting information
Appendix S1. Responses to MAKS Items by Year (strongly or slightly agree), weighted percentages.
Appendix S2. Responses to CAMI Items by Year (strongly or slightly agree), weighted percentages.
Appendix S3. Responses to RIBS Items by Year (strongly or slightly agree), weighted percentages.
Acknowledgements
The Time to Change evaluation was funded by the UK Government Department of Health, Comic Relief and Big Lottery Fund.
We are grateful for collaboration on the evaluation by: Sue Baker, Paul Farmer and Paul Corry. During Phase 1 of TTC GT, DR and CH were funded in relation to a National Institute for Health Research (NIHR) Applied Programme grant awarded to the South London and Maudsley NHS Foundation Trust (GT). CH, SEL and EC were supported during phases 1 and 2 by the grants to Time to Change from Big Lottery, the UK Department of Health and Comic Relief and ER during phase 2. CH was also funded by grants from the NIHR, Maudsley Charity and Guy's and St Thomas's Charity. GT is supported by the European Union Seventh Framework Programme (FP7/2007‐2013) Emerald project. GT and DR acknowledge financial support from the Department of Health via the National Institute for Health Research (NIHR) Biomedical Research Centre and Dementia Unit awarded to South London and Maudsley NHS Foundation Trust in partnership with King's College London and King's College Hospital NHS Foundation Trust. GT and DR acknowledge support from the NIHR Collaboration for Leadership in Applied Health Research and Care South London at King's College London Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Henderson C, Robinson E, Evans‐Lacko S, Corker E, Rebollo‐Mesa I, Rose D, Thornicroft G. Public knowledge, attitudes, social distance and reported contact regarding people with mental illness 2009–2015.
References
- 1. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103:813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mai Q, D'arcy C, Holman J, Sanfilippo FM, Emery JD, Preen DB. Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population‐based longitudinal study. BMC Med 2011;9:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Laursen TM, Munk‐Olsen T, Nordentoft M, Mortensen PB. Increased mortality among patients admitted with major psychiatric disorders: a register‐based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry 2007;68:899–907. [DOI] [PubMed] [Google Scholar]
- 4. Gissler M, Laursen TM, Ösby U, Nordentoft M, Wahlbeck K. Patterns in mortality among people with severe mental disorders across birth cohorts: a register‐based study of Denmark and Finland in 1982–2006. BMC Public Health 2013;13:834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Suhrcke M, De Paz Nieves C. The impact of health and health behaviours on educational outcomes in high‐income countries: a review of the evidence. Copenhagen: WHO Regional Office for Europe, 2011. [Google Scholar]
- 6. Lee S, Tsang A, Breslau J et al. Mental disorders and termination of education in high‐income and low‐ to middle‐income countries: epidemiological study. Br J Psychiatry 2009;194:411–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Social Exclusion Unit . Mental Health and Social Exclusion. London: Office of the Deputy Prime Minister; 2004. [Google Scholar]
- 8. Clement S, Brohan E, Sayce L, Pool J, Thornicroft G. Disability hate crime and targeted violence and hostility: a mental health and discrimination perspective. J Ment Health 2011;20:219–225. [DOI] [PubMed] [Google Scholar]
- 9. Corker E, Hamilton S, Robinson E et al. Viewpoint survey of mental health service users' experiences of discrimination in England 2008–2014. Acta Psychiatr Scand 2016;134:6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Evans‐Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self‐stigma among individuals with mental illness in 14 European countries. Psychol Med 2012;42:1741–1752. [DOI] [PubMed] [Google Scholar]
- 11. Schomerus G, Schwahn C, Holzinger A et al. Evolution of public attitudes about mental illness: a systematic review and meta‐analysis. Acta Psychiatr Scand 2012;125:440–452. [DOI] [PubMed] [Google Scholar]
- 12. Mehta N, Kassam A, Leese M, Butler G, Thornicroft G. Public attitudes towards people with mental illness in England and Scotland, 1994–2003. Br J Psychiatry 2009;194:278–284. [DOI] [PubMed] [Google Scholar]
- 13. Borschmann RG, Jones N, Henderson RC. Campaigns to reduce mental illness stigma in Europe: a scoping review. Die Psychiatr 2014;11:43–50. [Google Scholar]
- 14. National Institute for Health and Clinical Excellence . Behaviour Change. London: NICE, 2007. [DOI] [PubMed] [Google Scholar]
- 15. Thornicroft G. Shunned: Discrimination against People with Mental Illness. Oxford: Oxford University Press; 2006. [Google Scholar]
- 16. Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry 2007;190:192–193. [DOI] [PubMed] [Google Scholar]
- 17. Henderson C, Thornicroft G. Evaluation of the Time to Change programme in England 2008–2011. Br J Psychiatry 2013;202(Suppl 55):s45–s48. [DOI] [PubMed] [Google Scholar]
- 18. Henderson C, Thornicroft G. Stigma and discrimination in mental illness: Time to Change. Lancet 2009;373:1928–1930. [DOI] [PubMed] [Google Scholar]
- 19. Evans‐Lacko S, Malcolm E, West K et al. Influence of Time to Change's social marketing interventions on stigma in England 2009–2011. Br J Psychiatry 2013;202:s77–s88. [DOI] [PubMed] [Google Scholar]
- 20. Friedrich B, Evans‐Lacko S, London J, Rhydderch D, Henderson C, Thornicroft G. Anti‐stigma training for medical students – the Education Not Discrimination project. Br J Psychiatry 2013;202:s89–s94. [DOI] [PubMed] [Google Scholar]
- 21. Henderson C, Williams P, Little K, Thornicroft G. Mental health problems in the workplace: changes in employers’ knowledge, attitudes and practices in England 2006–2010. Br J Psychiatry 2013;202:s70–s76. [DOI] [PubMed] [Google Scholar]
- 22. Department of Health . Attitudes to Mental Illness Summary Report 2008. London: Department of Health; 2008. [Google Scholar]
- 23. Evans‐Lacko S, Little K, Meltzer H et al. Development and psychometric properties of the Mental Health Knowledge Schedule. Can J Psychiatry 2010;55:440–448. [DOI] [PubMed] [Google Scholar]
- 24. Evans‐Lacko S, Rose D, Little K, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of a stigma related behaviour measure. Epidemiol Psychiatr Sci 2011;20:263–271. [DOI] [PubMed] [Google Scholar]
- 25. Evans‐Lacko S, Henderson C, Thornicroft G. Public knowledge, attitudes and behaviour regarding people with mental illness in England 2009–2012. Br J Psychiatry 2013;202:s51–s57. [DOI] [PubMed] [Google Scholar]
- 26. Corker E, Hamilton S, Henderson C et al. Experiences of discrimination among people using mental health services in England 2008–2011. Br J Psychiatry 2013;202(s55):s58–s63. [DOI] [PubMed] [Google Scholar]
- 27. Department of Health . No health without mental health: a cross‐government mental health outcomes strategy of all ages. London: Department of Health; 2011. [Google Scholar]
- 28. Department of Health . No health without mental health: implementation framework. London: Department of health; 2012. [Google Scholar]
- 29. Rüsch N, Evans‐Lacko S, Thornicroft G. What is a mental illness? Public views and their effects on attitudes and disclosure. Aust N Z J Psychiatry 2012;46:641–650. [DOI] [PubMed] [Google Scholar]
- 30. Taylor SM, Dear MJ. Scaling community attitudes toward the mentally ill. Schizophr Bull 1981;7:225–240. [DOI] [PubMed] [Google Scholar]
- 31. Phillips D. Identification of mental illness: its consequences for rejection. Community Ment Health J 1967;3:262–266. [DOI] [PubMed] [Google Scholar]
- 32. STAR SA . What the Public Thinks about Mental Health and Mental Illness. Indianapolis, Indiana: Paper presented at the annual meeting of the National Association of Mental Health; 1952. [Google Scholar]
- 33. Market Research Society . Occupation Groupings: A Job Dictionary, 7th edn 2010: Market Research Society, London. [Google Scholar]
- 34. Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta‐analysis of outcome studies. Psychiatr Serv 2012;63:963–973. [DOI] [PubMed] [Google Scholar]
- 35. Al Ramiah A, Hewstone M. Intergroup contact as a tool for reducing, resolving, and preventing intergroup conflict: evidence, limitations, and potential. Am Psychol 2013;68:527–542. [DOI] [PubMed] [Google Scholar]
- 36. Henderson RC, Corker E, Hamilton S et al. Viewpoint survey of mental health service users’ experiences of discrimination in England 2008–12. Soc Psychiatry Psychiatr Epidemiol 2014;49:1599–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Henderson C, Evans‐Lacko S, Flach C, Thornicroft G. Responses to mental health stigma questions: the importance of social desirability and data collection method. Can J Psychiatry 2012;57:152–160. [DOI] [PubMed] [Google Scholar]
- 38. Hansson L, Stjernswärd S, Svensson B. Changes in attitudes, intended behaviour, and mental health literacy in the Swedish population 2009–2014: an evaluation of a national antistigma programme. Acta Psychiatr Scand 2016;134:71–79. [DOI] [PubMed] [Google Scholar]
- 39. Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. “A disease like any other”? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry 2010;167:1321–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Evans‐Lacko S, Corker E, Williams P, Henderson C, Thornicroft G. Trends in public stigma among the English population in 2003–2013: influence of the Time to Change anti‐stigma campaign. Lancet Psychiatry 2014;1:121–128. [DOI] [PubMed] [Google Scholar]
- 41. Henderson C, Evans‐Lacko S, Thornicroft G. Mental illness stigma, help seeking and public health programmes. Am J Public Health 2013;103:777–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Knaak S, Patten S. Building and Delivering Successful Anti‐stigma Programs for Healthcare Providers: Results of a Qualitative Study. Ottawa: Mental health Commission of Canada, 2014. [Google Scholar]
- 43. Corrigan PW. Best practices: strategic stigma change (SSC): five principles for social marketing campaigns to reduce stigma. Psychiatr Serv 2011;62:824–826. [DOI] [PubMed] [Google Scholar]
- 44. Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol 2003;58:5–14. [DOI] [PubMed] [Google Scholar]
- 45. Galdas PM, Cheater F, Marshall P. Men and health help‐seeking behaviour: literature review. J Adv Nurs 2005;49:616–623. [DOI] [PubMed] [Google Scholar]
- 46. Knifton L, Gervais M, Newbigging K et al. Community conversation: addressing mental health stigma with ethnic minority communities. Soc Psychiatry Psychiatr Epidemiol 2010;45:497–504. [DOI] [PubMed] [Google Scholar]
- 47. Shefer G, Rose D, Nellums L, Thornicroft G, Henderson C, Evans‐Lacko S. ‘Our community is the worst’: the influence of cultural beliefs on stigma, relationships with family and help‐seeking in three ethnic communities in London. Int J Soc Psychiatry 2012;59:535–554. [DOI] [PubMed] [Google Scholar]
- 48. Evans‐Lacko S, Henderson C, Thornicroft G, Mccrone P. Economic evaluation of the anti‐stigma social marketing campaign in England 2009–2011. Br J Psychiatry Suppl 2013;55:s95–s101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Responses to MAKS Items by Year (strongly or slightly agree), weighted percentages.
Appendix S2. Responses to CAMI Items by Year (strongly or slightly agree), weighted percentages.
Appendix S3. Responses to RIBS Items by Year (strongly or slightly agree), weighted percentages.


