Abstract
Objectives
To determine the contribution of cognitive impairment, prefracture functional impairment, and treatment as predictors of functional status and mobility 6 months after discharge from rehabilitation for older adults with hip fracture.
Design
Longitudinal.
Setting
Inpatient rehabilitation units of two community hospitals.
Participants
Adults with hip fractures aged 65 and older who were discharged from a rehabilitation unit and had been living in the community before the fracture (N = 133).
Measurements
Mini‐Mental State Examination (MMSE) score at discharge from rehabilitation was used to identify the presence and severity of cognitive impairment. Outcomes were measured using questions from two subscales of the Functional Independence Measure (Self‐Care Function and Functional Mobility) and the New Mobility Scale (NMS). Measurements were made at discharge from a rehabilitation setting and 3 and 6 months after discharge.
Results
Prefracture functional impairment was associated with worse outcomes throughout the 6 months after discharge and with lower rates of improvement, or in some cases decline, after discharge. Cognitive impairment was associated with worse outcomes throughout the 6 months after discharge but was only weakly associated with lower rates of improvement or decline. The Patient Centered Rehabilitation Model of care targeting persons with cognitive impairment (PCRM‐CI) intervention group had higher NMS scores after discharge than a usual care group.
Conclusion
Although cognitive impairment and prefracture functional impairment contribute to poor outcomes, prefracture functional impairment was more strongly associated with poor outcomes than cognitive impairment. There is evidence to show that individuals with cognitive impairment are able to regain their mobility, which suggests a need for postdischarge targeted interventions that include a focus on activities of daily living for older adults with cognitive impairment and functional impairment to stabilize gains from inpatient rehabilitation.
Keywords: hip fracture; person‐centered models of care; cognitive impairment; dementia, rehabilitation models of care; long‐term rehabilitation outcomes
Approximately 50% of older adults who sustain a hip fracture experience functional decline and become increasingly unable to perform activities of daily living (ADLs).1, 2 The sequelae of hip fracture are often so debilitating that up to 20% of older adults with hip fracture will be placed in institutionalized care 3 months after hospital discharge.3
Rehabilitation interventions aim to improve function and mobility in individuals who have sustained a hip fracture,4 but individuals with cognitive impairment are often excluded from participating in active inpatient rehabilitation.5 The Patient Centered Rehabilitation Model of Care targeting persons with cognitive impairment (PCRM‐CI) was developed and implemented as an interdisciplinary intervention to educate and mentor staff on an active rehabilitation unit to provide person‐centered interventions targeting older adults with complex medical conditions, particularly those with cognitive impairment.6 Enrolled staff were provided with specialized education and supplementary support to care for older persons with comorbidities, including cognitive impairment secondary to dementia or delirium. Evaluation of the PCRM‐CI revealed that individuals with cognitive impairment in the intervention group were more likely than those in the control group to be discharged home irrespective of the presence of cognitive impairment.6
Recent studies provide conflicting evidence regarding the factors that influence recovery in older adults with hip fracture after discharge from inpatient rehabilitation. Factors such as prefracture cognitive and functional status,7, 8 cognitive impairment,9, 10, 11, 12, 13, 14, 15, 16 age,17 sex,18, 19, 20 medical co morbidities,21 and pain22 have been found to influence recovery, function, and mobility outcomes over time in older adults after hip fracture,12, 14, 15, 16 yet two systematic reviews indicated that individuals with cognitive impairment made gains that were similar to those of individuals without cognitive impairment.16, 23 Albeit informative, these studies were unclear as to how many individuals with complex needs were offered active rehabilitation, the type and approaches used during rehabilitation, and the extent to which inpatient care influenced long‐term outcomes. Given the inconsistency of extant evidence, the potential and relative effect of predictors of recovery in older adults after hip fracture is unclear. Addressing this knowledge gap is a necessary first step in increasing understanding of the factors influencing decline in this complex and vulnerable population, which will inform management considerations in determining treatments appropriate for older adult recovery after discharge.
The purpose of this study was to determine the contribution of the severity of cognitive impairment, level of prefracture functional impairment, and treatment in the PCRM‐CI as predictors of functional status and mobility 6 months after discharge from rehabilitation for older adults with hip fracture. Based on the literature, it was hypothesized that prefracture functional impairment and cognitive impairment would affect outcomes after discharge from rehabilitation.
Methods
Participants and Setting
This was a prospective 6‐month postdischarge follow‐up evaluation of participants initially enrolled in a study comparing the PCRM‐CI with usual care.6 The PCRM‐CI protocol and results to time of discharge from inpatient rehabilitation have been described in detail.6, 24 Inclusion criteria were aged 65 and older, had undergone surgery for hip fracture, admitted to inpatient rehabilitation directly from an acute care hospital, living in the community in a private home or residential setting (that did not provide 24‐hour nursing care) at the time of the hip fracture, English speaking, and had a collateral informant (family member or close friend) who was familiar with the individual's prefracture condition. Individuals with a previous hip fracture, pathological hip fracture, or hip fracture associated with multiple traumas were excluded. Recruitment took place at two inpatient rehabilitation units in two community hospitals in Ontario, Canada. The institutional ethics review boards at the research sites approved this study.
Explanatory Variables
Participant Characteristics
Personal characteristics such as age, sex, marital status, and education level as a proxy for socioeconomic status were collected at admission.25
Participant Health Status
Cognitive function was measured at admission and discharge using the Mini‐Mental State Examination (MMSE).26, 27 Participants were classified into three cognitive groups depending on their score: severe impairment (<15), mild to moderate impairment (15–23), and no impairment (≥24).28 MMSE score at discharge was used to better understand the influence of cognitive impairment on recovery after discharge. Residual delirium was not excluded when the MMSE was administered. Cognitive function 1 year before the hip fracture was estimated using the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE),29 but these data were not used because the IQCODE was highly correlated with MMSE at discharge. Comorbidities and prefracture functional status were measured using the Older American Resources and Service Instrument (OARS) upon admission. Pain status was measured using the Pain Reported Scale,30 and use of a gait aid (wheelchair, walker, cane) was documented at admission and discharge.
Outcome Variables
A research assistant who was a registered nurse on the rehabilitation unit collected data at the time of discharge. Three and 6 months after discharge, the nurse conducted telephone interviews with participants' collateral informants to collect follow up data.
Independence in ADLs
The self‐care functions of older adults with hip fractures are likely to be affected during physical recovery. The self‐care items of the Functional Independence Measure (FIMS) were used to monitor changes in eating, grooming, bathing, dressing, toileting, and continence. This tool has been used in individuals with cognitive impairment after hip fracture to measure their independence in ADLs.31
Functional Mobility
Because hip fracture affects the lower extremities, specifically locomotion and transferring abilities, the study focused on the mobility items of the Functional Independence Measure (FIMM). This subscale measures the ability to walk, climb stairs, transfer in and out of bed, toilet, and bathe. The FIMM has well‐established reliability and validity.32, 33, 34
Environmental Mobility
The New Mobility Score (NMS) was used to evaluate environmental mobility and captures the influence of environmental factors that individuals encounter in the community on their mobility.35 The NMS is a composite score of the individual's ability to walk indoors, walk outdoors, and shop.35
Analyses
The predictors of longitudinal change in outcomes during the first 6 months after discharge were analyzed using multilevel mixed‐effects multivariate regression in which within‐individual errors were considered to have an autoregressive structure of order 1 from discharge through 6 months after discharge. Multilevel models were needed because each outcome was measured repeatedly on the same participant over time. Level 1 units were the repeated measures for each participant, and the Level 2 unit was the participant. Participants were treated as a Level 2 random effect. Participant characteristics, participant health status variables, participant impairment, and whether the PCRM‐CI intervention or usual care was received during rehabilitation were each treated as Level 2 fixed effects. The influence of the intervention over the postdischarge period was evaluated by testing the interaction of the intervention with each measurement time. The influence of cognitive impairment over the postdischarge period was evaluated by testing the interaction of each level of cognitive impairment with each measurement time. The influence of prefracture functional impairment over the postdischarge period was evaluated by testing the interaction of the impairment with each measurement time. It was possible to use all available data in the regressions while accounting for missing values, which was an advantage of this analysis plan because data were incomplete for 18 participants who died during the 6‐month postdischarge study period.
Results
Characteristics of the study sample are shown in Table 1 according to level of cognitive impairment. Seventy‐seven percent of participants were female, 41% were married, 50% were living with another person, 16% had a diagnosis of dementia, 83% had three or more chronic conditions, and 68% had a history of falls. Average MMSE score at the time of discharge was 25.5 ± 4.6; 76% had no cognitive impairment, 17% mild to moderate cognitive impairment, and 7% severe cognitive impairment.
Table 1.
Characteristics of Study Population According to Level of Cognitive Impairment
| Characteristic | Combined, n = 133 | No Cognitive Impairment, n = 101 | Mild to Moderate Cognitive Impairment, n = 23 | Severe Cognitive Impairment, n = 9 |
|---|---|---|---|---|
| Age, n (%) | ||||
| 64–74 | 33 (25) | 26 (26) | 7 (30) | 0 (0) |
| 75–84 | 50 (38) | 41 (41) | 6 (26) | 3 (33) |
| ≥85 | 50 (38) | 34 (43) | 10 (28) | 6 (67) |
| Age, mean ± SD | 81.0 ± 7.9 | 80.8 ± 8.1 | 80.2 ± 8.5 | 84.6 ± 3.7 |
| Female, % | 77 | 81 | 57 | 88 |
| Education <12 years, % | 17 | 15 | 26 | 11 |
| Married or common‐law partner, % | 41 | 35 | 52 | 33 |
| Living with others % | 50 | 53 | 39 | 44 |
| Health status and physical function, % | ||||
| Diagnosed dementia | 16 | 7 | 39 | 56 |
| ≥3 chronic conditions | 83 | 82 | 91 | 78 |
| History of falls | 68 | 63 | 83 | 78 |
| Previous fall with injury | 55 | 52 | 68 | 67 |
| MMSE score at admission, mean ± SD | 24.6 ± 4.6 | 26.3 ± 2.5 | 20.6 ± 3.3 | 14.6 ± 7.9 |
| MMSE score at discharge, mean ± SDa | 25.5 ± 4.6 | 27.6 ± 1.7 | 21.6 ± 1.6 | 12.9 ± 5.5 |
| Older American Resources and Service Instrument score, mean ± SD | 23.7 ± 5.4 | 25.1 ± 4.2 | 20.9 ± 3.8 | 15.2 ± 9.4 |
| Type of hip fracture, % | ||||
| Intertrochanteric | 39 | 43 | 39 | 0 |
| Intracapsular | 49 | 45 | 48 | 100 |
| Subtrochanteric | 2 | 2 | 4 | 0 |
| Other | 10 | 11 | 9 | 0 |
| Wheelchair required at discharge, % | 13 | 11 | 22 | 11 |
| Reported pain at discharge, % | 22 | 22 | 26 | 11 |
| Site 1 (of two alternative sites), % | 42 | 44 | 39 | 33 |
| Intervention care, % | 46 | 46 | 48 | 44 |
N = 133 because 12 participants had missing data.
SD = standard deviation; MMSE = Mini‐Mental State Examination.
Figure 1 details the number of participants in the study from admission to rehabilitation through the 6‐month period after discharge and loss of follow‐up due to participant death. The sample for the analysis was a subset of the 133 participants (90% of participants) for whom MMSE scores at discharge were available, and the results are based on this sample. Figure 1 includes the 12 participants missing MMSE scores at discharge that were excluded from the analysis where it was required. At the beginning of the postdischarge period, the study included 70 participants who had received PCRM‐CI care and 75 who had received usual care. In the first 3 months after discharge, four participants from the usual care group and five from the PCRM‐CI group died. Between 3 and 6 months after discharge, two participants each from the PCRM‐CI group and the usual care group died, leaving 63 PCRM‐CI participants and 69 usual care participants at 6 months after discharge.
Figure 1.
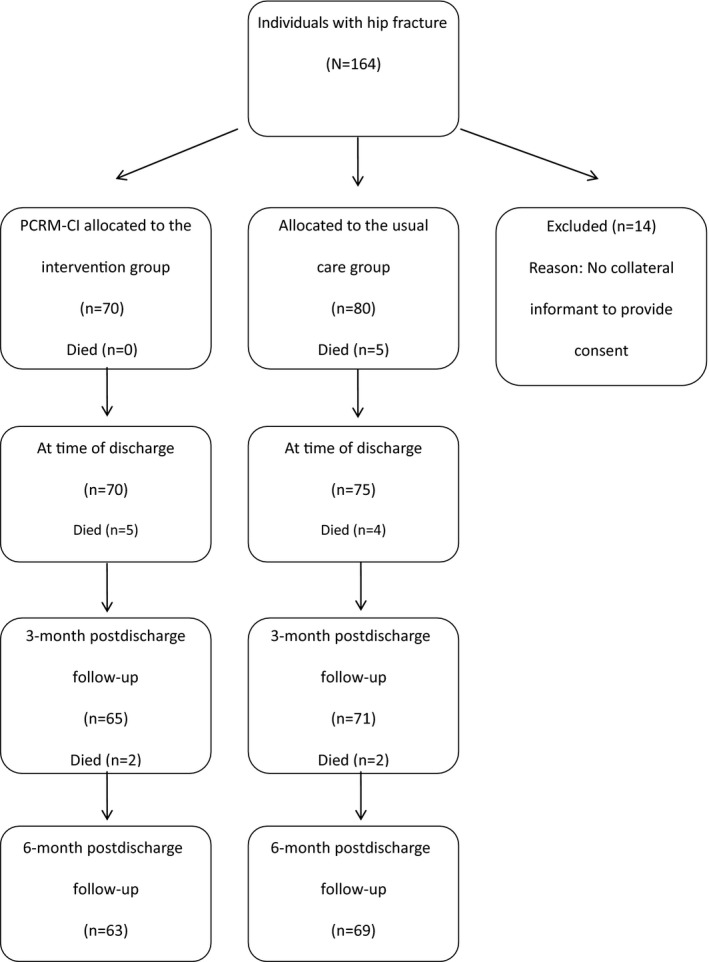
Patient Centered Rehabilitation Model‐Cognitive Impairment model of care (PCRM‐CI) participant study flow diagram.
Influence of Cognitive Impairment Severity on Outcomes
Table 2 shows mean FIMM, FIMS, and NMS scores at admission; at discharge from inpatient rehabilitation; and at 3‐ and 6‐month follow‐up for all participants, categorized according to level of cognitive impairment. In general, participants with no cognitive impairment were discharged with higher FIMS, FIMM, and NMS scores than those with cognitive impairment. Mobility and independence in ADLs for participants with no cognitive impairment increased during the first 3 months after discharge and less so during the subsequent 3 months.
Table 2.
Change in Outcomes from Admission Through 6 Months After Discharge for Each Category of Cognitive Impairment at Discharge
| Outcome | No Cognitive Impairment, n = 101 | Mild to Moderate Cognitive Impairment, n = 23 | Severe Cognitive Impairment, n = 9 |
|---|---|---|---|
| Mean ± Standard Deviation | |||
| Independence in activities of daily living (FIM Self‐care Subscale; possible range 8–56) | |||
| Admission | 41.5 ± 8.6 | 39.2 ± 8.7 | 32.4 ± 11.5 |
| Discharge | 51.6 ± 4.7 | 49.0 ± 8.3 | 37.2 ± 13.2 |
| 3 months after discharge | 52.7 ± 7.0 | 43.1 ± 13.4 | 29.3 ± 16.1 |
| 6 months after discharge | 53.2 ± 4.6 | 46.5 ± 11.1 | 35.8 ± 15.6 |
| Functional mobility (FIM Mobility Subscale; possible range 5–35) | |||
| Admission | 13.5 ± 5.3 | 12.3 ± 5.2 | 11.0 ± 6.5 |
| Discharge | 25.2 ± 4.9 | 24.1 ± 6.0 | 17.0 ± 8.2 |
| 3 months after discharge | 28.3 ± 5.2 | 22.6 ± 7.9 | 18.2 ± 9.4 |
| 6 months after discharge | 29.0 ± 4.7 | 25.5 ± 7.6 | 19.8 ± 9.0 |
| Environmental Mobility (New Mobility Scale; possible range 0–9 | |||
| Admission | 3.4 ± 1.2 | 3.0 ± 1.4 | 2.2 ± 1.1 |
| Discharge | 4.3 ± 1.0 | 4.1 ± 1.3 | 3.6 ± 1.3 |
| 3 months after discharge | 6.2 ± 2.1 | 5.0 ± 2.8 | 4.6 ± 2.2 |
| 6 months after discharge | 6.7 ± 1.9 | 5.8 ± 3.0 | 4.7 ± 2.1 |
FIM = Functional Independence Measure.
Table 3 compares the multilevel mixed‐effects multivariate regression results for outcomes 3 and 6 months after discharge with those at discharge. Participants with mild to moderate cognitive impairment at discharge had discharge FIMS, FIMM, and NMS scores similar to those of participants with no cognitive impairment, although participants with mild to moderate cognitive impairment improved less after discharge in FIMS and FIMM than those with no cognitive impairment. In contrast, participants with severe cognitive impairment were discharged with lower FIMS and FIMM scores than participants with no cognitive impairment, but FIMS, FIMM, and NMS scores improved after discharge at least as much as they improved for participants with no cognitive impairment.
Table 3.
Multilevel Mixed‐Effects Multivariate Regression Results Comparing Outcomes 3 and 6 Months After Discharge with Those at Discharge (Repeated Measures on N = 133 Participants)
| Predictor | Independence in Activities of Daily Living (FIM Self‐care Subscale) | Functional Mobility (FIM Mobility Subscale) | Environmental Mobility (New Mobility Scale) |
|---|---|---|---|
| Unstandardized Beta (95% Confidence Interval) | |||
| Average effect on outcome from discharge to 6 months after discharge | |||
| Participant characteristics | |||
| Age | –0.01 (–0.14–0.11) | –0.08 (–0.17–0.01) | 0.01 (–0.01–0.02) |
| Female | 1.89 (–0.55–4.34) | 1.81 (0.01–3.60)a | 0.24 (–0.14–0.62) |
| Married or partner | –1.43 (–3.46–0.61) | 0.74 (–0.75–2.23) | 0.27 (–0.04–0.59) |
| <High school education | –0.07 (–2.74–2.60) | –1.88 (–3.83–0.07) | –0.14 (–0.56–0.28) |
| Participant health status at admission | |||
| Number of comorbidities | –0.40 (–1.07–0.27) | –0.39 (–0.87–0.10) | 0.03 (–0.07–0.14) |
| Prefracture functional impairment | –0.12 (–0.35–0.11) | –0.25 (–0.43 to –0.06)b | –0.11 (–0.14 to –0.07)c |
| Participant health status at discharge | |||
| Required wheelchair at discharge | –5.41 (–8.32 to –2.51)c | –3.54 (–5.68 to –1.41)c | –0.99 (–1.45 to –0.54)c |
| Pain reported at discharge | –0.29 (–0.72–0.14) | –0.44 (–0.75 to –0.12)b | –0.08 (–0.15 to –0.02)a |
| Severity of cognitive impairment at discharge | |||
| Severe cognitive impairment | –12.94 (–17.44 to –8.44)c | –5.43 (–9.10 to –1.76)b | 0.26 (–0.41–0.93) |
| Mild to moderate cognitive impairment | –0.74 (–3.56–2.09) | 0.88 (–1.42–3.18) | 0.34 (–0.08–0.76) |
| Patient Centered Rehabilitation Model‐Cognitive Impairment model of care | –0.42 (–2.33–1.48) | –0.47 (–1.87–0.92) | 0.30 (0.00–0.59)a |
| Site difference | –0.37 (–2.32–1.57) | 0.95 (–0.46–2.36) | 0.07 (–0.23–0.37) |
| Pattern of change over time: interactions with each measurement time | |||
| Interaction between each category of cognitive impairment and each measurement time (reference discharge) | |||
| No cognitive impairment × 3 months after discharge | 3.93 (1.94–5.92)c | 4.44 (2.96–5.93)c | 2.54 (2.10–2.98)c |
| No cognitive impairment × 6 months after discharge | 3.28 (1.37–5.19)c | 4.38 (2.77–5.98)c | 2.76 (2.28–3.24)c |
| Mild to moderate cognitive impairment × 3 months after discharge | –3.25 (–6.91–0.41) | –2.76 (–5.60–0.00)a | –0.28 (–1.08–0.51) |
| Mild to moderate cognitive impairment × 6 months after discharge | –3.46 (–7.04–0.12) | –1.79 (–4.78–1.20) | –0.24 (–1.15–0.66) |
| Severe cognitive impairment × 3 months after discharge | 0.70 (–7.56–6.16) | 1.59 (–3.36–6.53) | 0.09 (–1.30–1.49) |
| Severe cognitive impairment × 6 months after discharge | 1.42 (–5.08–7.92) | 0.65 (–4.69–6.00) | –0.27 (–1.81–1.27) |
| Interaction between prefracture functional impairment and each measurement time (reference discharge) | |||
| Prefracture functional impairment × 3 months after discharge | –0.67 (–0.97 to –0.37)c | –0.36 (–0.58 to –0.14)b | –0.14 (–0.20 to –0.07)c |
| Prefracture functional impairment × 6 months after discharge | –0.53 (–0.82 to –0.24)c | –0.27 (–0.51 to –0.06)a | –0.12 (–0.20 to –0.05)c |
| Constant | 53.65 (42.86–64.44) | 30.55 (22.65–38.46) | 3.69 (2.00–5.37) |
| Random‐effects parameters | |||
| SD among repeated measures within participants | 4.02 (3.14–5.14) | 2.53 (1.78–3.61) | 0.69 (0.49–0.96) |
| SD of residual variation at discharge | 3.96 (3.06–5.14) | 3.88 (3.20–4.71) | 0.48 (0.25–0.93) |
| SD of residual variation at 3 months after discharge | 6.49 (5.49–7.68) | 3.94 (3.22–4.83) | 1.66 (1.45–1.90) |
| SD of residual variation at 6 months after discharge | 5.45 (4.31–6.87) | 4.18 (3.42–5.10) | 1.65 (1.43–1.90) |
| Correlation between repeated measures at discharge and 3 months after discharge | 0.12 (–0.08–0.32) | 0.05 (–0.15–0.25) | 0.29 (0.05–0.49) |
| Correlation between repeated measures 3 months and 6 months after discharge | 0.72 (0.57–0.83) | 0.68 (0.51–0.79) | 0.74 (0.65–82) |
Cognitive impairment measured according to Mini‐Mental State Examination; prefracture functional impairment measured according to Older Americans Resources and Services instrument.
P < a.05, b.01, c.001.
FIM = Functional Independence Measure; SD = standard deviation.
Influence of Prefracture Functional Impairment on Outcomes
The influence of prefracture functional impairment (OARS) on outcomes was investigated. Table 3 illustrates that FIMM and NMS scores but not FIMS scores were lower from discharge to 6 months after discharge in those with prefracture functional impairment. Further postdischarge changes in each of the outcomes were inversely related to levels of functional impairment to the extent that participants with mild, moderate, and greater levels of prefracture functional impairment experienced declines in all three outcomes after discharge.
Influence of Prefracture Functional Impairment and Cognitive Impairment on Outcomes
Prefracture functional impairment and cognitive impairment often influence outcomes, so the relationship between the two was explored by focusing on the patterns of recovery in the three outcomes (independence in ADLs, functional mobility, environmental mobility) from admission to 6 months after discharge from rehabilitation. Figure 2 illustrates the relative contributions of prefracture functional impairment and cognitive impairment by adjusting values to control for the influence of prefracture functional impairment. The trajectories with the black markers depict the unadjusted changes (combined effect of cognitive impairment and prefracture impairment) of FIMS, FIMM, and NMS scores, and the trajectories with white markers depict their adjusted changes (removed effect of prefracture functional impairment) to illustrate the influence of cognitive impairment alone. Comparing the two sets of trajectories, Figure 2 shows that functional impairment was much more strongly associated with poor functional and environmental mobility than was cognitive impairment. After accounting for prefracture functional impairment, level of mobility as measured using the NMS and its change after discharge did not differ between cognitive impairment categories (i.e., the adjusted trajectories are remarkably similar) (Figure 2a). Mobility as measured using FIMM showed a similar pattern (Figure 2b). In contrast, cognitive impairment and prefracture functional impairment contributed to independence in ADLs (Figure 2c), indicating that prefracture functional impairment was more strongly associated with poor mobility outcomes than cognitive impairment.
Figure 2.
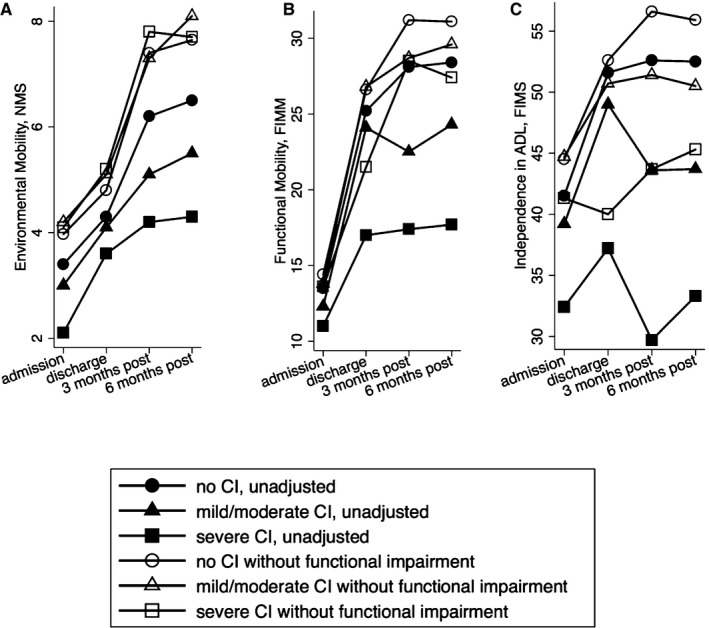
Change in outcomes from admission through 6 months after discharge for each category of cognitive impairment. Black markers present unadjusted values and show the contribution of cognitive impairment and prefracture functional impairment. White markers depict the adjusted changes (removed effect of prefracture functional impairment) to illustrate the influence of cognitive impairment alone. FIMS = Functional Independence Measure Self‐care Subscale; FIMM = Functional Independence Measure Mobility Subscale; NMS = New Mobility Scale.
Influence of PCRM‐CI Intervention and Usual Care on Outcomes
Table 3 shows that NMS scores improved significantly more in the PCRM‐CI group than in the usual care group from discharge to 6 months after discharge. PCRM‐CI participants were more likely to be able walk outdoors at 3 and 6 months, although similar results were not seen for functional mobility (P = .65) or independence in ADLs (P = .62). Regression analyses that included the interaction of PCRM‐CI with time found that no postdischarge longitudinal changes in any of the outcomes differed significantly between the PCRM‐CI and usual care groups. These interactions were therefore not included in the regression analyses reported here.
Influence of Variables Related to Health Status at Discharge on Outcomes
The analysis also showed that participants requiring a wheelchair at discharge had significantly worse postdischarge outcomes than those who did not. Greater pain reported at discharge was also associated with poorer recovery after discharge (Table 3).
Discussion
Prefracture functional impairment was more strongly associated with poor function and mobility outcomes than was cognitive impairment in older adults with hip fracture. Prefracture functional impairment was associated with poorer outcome scores and lower rates of improvements through the 6‐month follow‐up period after discharge. These findings also suggest different recovery trends over time for participants based on their level of cognitive impairment, prefracture functional status, pain status, and use of a wheelchair at the time of discharge from rehabilitation and their involvement in the PCRM‐CI model of care. Therefore, when examining long‐term mobility outcomes for this population, prefracture functional status limits recovery more than cognitive impairment.
When combining individuals from the usual care and intervention groups to determine factors influencing outcomes for all participants, consistent with findings from the intervention cohort, individuals with mild to moderate cognitive impairment did not improve their functional mobility as much as those with no cognitive impairment. Participants with severe cognitive impairment had less independence in ADLs and functional mobility than those with mild to moderate cognitive impairment. The results indicate that regardless of the severity of their cognitive impairment, the discharge scores of all participants with cognitive impairment in independence of ADLs and functional mobility remained almost identical 6 months after discharge from rehabilitation as they were 3 months earlier. The findings of this study indicate that, if inpatient rehabilitation benefits are to persist after discharge, there is a need for rehabilitation interventions deliverable in the home and customized to the individual. The results show that functional and environmental mobility improve over time, whereas independence in ADL recovery patterns have a comparatively distinct trajectory, with less improvement over time. Although other studies have found cognitive impairment to be a predictor of decline,12, 36 the current findings show that prefracture functional impairment is the main predictor of decline. If persons have severe cognitive impairment and low levels of prefracture functional impairment, they tend to recover. The focus of concern for clinicians needs to be on older adults with higher levels of functional impairment rather than those with cognitive impairment after a hip fracture. Therefore, the results present preliminary evidence that persons with various levels of cognitive impairment can benefit from inpatient rehabilitation and have some long‐term effects and thus should be provided access to care.
Prefracture functional impairment was the most significant predictor of decline in independence in ADLs and in mobility. The finding that prefracture functional status is an important predictor of functional recovery in older adults with hip fracture is consistent with previous work.37, 38, 39 A previous study found that prefracture mobility and ability to perform ADLs independently predicted mortality and preserved walking ability at 4 months after discharge and absolute FIM gain.39 This finding is of concern given the recent evidence of increased incidence of comorbidities among hip fracture patients.40 This may influence prefracture functional status, which in turn may put individuals at increased risk for poor outcomes after discharge from inpatient rehabilitation.41 Finally, although there is evidence to suggest that pre‐hip fracture status is more important than cognitive impairment for the prediction of regaining functional mobility after rehabilitation, both of these variables have been identified as important predictors of regaining functional independence.39, 42, 43 Both should therefore be assessed in persons receiving rehabilitation after hip fracture. For persons with hip fracture, an evidence‐based community or home‐based intervention targeting those with cognitive impairment or prefracture functional impairment is the next important step in the clinical pathway for this vulnerable population. Based on the current study results, outpatient rehabilitation interventions may need to consider ways to provide more assistance to support ADL independence when persons with cognitive impairment are discharged from inpatient rehabilitation rather than a sole focus on maintaining their mobility. Further investigation is required to understand how family caregivers are managing the burden of care placed on them of caring for persons with cognitive impairment while trying to keep them as independent as possible.
These findings support that rehabilitation in the PCRM‐CI was effective in improving independence in environmental mobility over the postdischarge period, although no benefit was seen for the PCRM‐CI care group in postdischarge ADL independence or functional mobility. The results also indicate that pain is an important predictor of outcomes in older adults after hip fracture. It has been report that pain control has been poorly managed in older adults with hip fracture,44 especially in those with cognitive impairment. The results of this study show that a high pain rating score at discharge is significantly associated with lower independence in ADLs and functional mobility at discharge. The latter is consistent with findings that participants who report higher levels of pain after surgery and during rehabilitation are slower to mobilize after hip fracture.22, 45 These results suggest a need for specific strategies for pain assessment and management during rehabilitation for individuals with cognitive impairment, especially just before discharge, and with more postdischarge follow‐up to monitor and alleviate pain.
Study Limitations
This study has several potential limitations. The sample size was small, particularly the number of participants with low MMSE scores, which may have affected the ability to detect some independent predictors of outcomes and differences between various subgroups. Another limitation is that the amount of rehabilitation therapy delivered after discharge was not monitored, so this could not be accounted for in the analyses. Despite these limitations, the results of this study contribute to understanding of the predictors of long‐term outcomes in persons with hip fracture and the need to provide postrehabilitation care for vulnerable individuals.
Conclusions
Many variables influence long‐term recovery from rehabilitation for older adults with hip fracture. Older adults with prefracture functional impairment entering inpatient rehabilitation, as well as individuals with severe cognitive impairment, are at risk of poor long‐term outcomes and may require additional interventions after discharge from inpatient rehabilitation.
Acknowledgments
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Dr. Naglie was supported by the George, Margaret and Gary Hunt Family Chair in Geriatric Medicine, University of Toronto. Dr. McGilton was supported by a Mid‐Career Award from the Ontario Ministry of Health & Long‐Term Care.
This study was supported by a demonstration grant from the Canadian Institutes of Health Research—Institute of Aging (DPA–93049).
Author Contributions: McGilton, Davis, Naglie, Chu, Stewart, van Wyk: study concept and design, data interpretation, manuscript preparation. McGilton: literature review, data collection, preparation of manuscript. Stewart: statistical analysis. All authors: critical revisions to the final manuscript.
Sponsor's Role: None.
J Am Geriatr Soc 64:1601‐1609, 2016.
References
- 1. Sahota O, Curie C. Hip fracture care: All change. Age Ageing 2008;37:128–129. [DOI] [PubMed] [Google Scholar]
- 2. Freter S, Koller K. Hip Fractures and Alzheimer's disease. The Canadian Review of Alzheimer's Disease and Other Dementias [on‐line]. Available at http://www.stacommunications.com/customcomm/back-issue_pages/ad_review/adPDFs/2008/september2008/pg15.pdf Accessed January 10, 2015.
- 3. Cree M, Soskolne CL, Belseck E et al. Mortality and institutionalization following hip fracture. J Am Geriatr Soc 2000;48:283–288. [DOI] [PubMed] [Google Scholar]
- 4. Cameron I. Coordinated multidisciplinary rehabilitation after hip fracture. Disabil Rehabil 2005;27:1081–1090. [DOI] [PubMed] [Google Scholar]
- 5. Wiktorowicz ME, Goeree R, Papaioannou A et al. Economic implications of hip fracture: Health service use, institutional care and cost in Canada. Osteoporos Int 2001;12:271–278. [DOI] [PubMed] [Google Scholar]
- 6. McGilton KS, Davis A, Naglie G et al. Evaluation of patient‐centered rehabilitation model targeting older persons with a hip fracture, including those with cognitive impairment. BMC Geriatr 2013;13:136–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pretto M, Spirig R, Kaelin R et al. Outcomes of elderly hip fracture patients in the Swiss healthcare system. A survey prior to the implementation of DRGs and prior to the implementation of a Geriatric Fracture Centre. Swiss Med Wkly 2010;140(w13086):1–7. [DOI] [PubMed] [Google Scholar]
- 8. Naglie G, Tansey C, Kirkland JL et al. Interdisciplinary inpatient care for elderly people with hip fracture: A randomized controlled trial. Can Med Assoc J 2002;167:25–32. [PMC free article] [PubMed] [Google Scholar]
- 9. Al‐Ani AN, Flodin L, Söderqvist A et al. Does rehabilitation matter in patients with femoral neck fracture and cognitive impairment? A prospective study of 246 patients. Arch Phys Med Rehabil 2010;91:51–57. [DOI] [PubMed] [Google Scholar]
- 10. Kristensen MT. Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med 2011;47:257–264. [PubMed] [Google Scholar]
- 11. Adunsky A, Fleissig Y, Levenkrohn S et al. A comparative study of Mini‐Mental Test, Clock Drawing task and Cognitive‐FIM in evaluating functional outcome of elderly hip fracture patients. Clin Rehabil 2002;16:414–419. [DOI] [PubMed] [Google Scholar]
- 12. Heruti R, Lusky A, Barell V et al. Cognitive status at admission: Does it affect the rehabilitation outcome of elderly patients with hip fracture? Arch Phys Med Rehabil 1999;80:432–436. [DOI] [PubMed] [Google Scholar]
- 13. Rapp MA, Schnaider‐Beeri M, Wysocki M et al. Cognitive decline in patients with dementia as a function of depression. Am J Geriatr Psychiatry 2011;19:357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Givens J, Snaft T, Marcantonio E. Functional recovery after hip fracture: The combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc 2008;6:1075–1079. [DOI] [PubMed] [Google Scholar]
- 15. Samuelsson B, Hedström M, Ponzer S et al. Gender differences and cognitive aspects on functional outcome after hip fracture—a 2 years' follow‐up of 2,134 patients. Age Ageing 2009;38:686–692. [DOI] [PubMed] [Google Scholar]
- 16. Allen J, Koziak A, Buddingh S et al. Rehabilitation in patients with dementia following hip fracture: A systematic review. Physiother Can 2012;64:190–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arinzon Z, Fidelman Z, Zuta A et al. Functional recovery after hip fracture in old‐old elderly patients. Arch Gerontol Geriatr 2005;40:327–336. [DOI] [PubMed] [Google Scholar]
- 18. Kirke PN, Sutton M, Burke H et al. Outcome of hip fracture in older Irish women: A 2‐year follow‐up of subjects in a case–control study. Injury 2002;33:387–391. [DOI] [PubMed] [Google Scholar]
- 19. Rolland Y, Pillard F, Lauwers‐Cances V et al. Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 2004;26:425–431. [DOI] [PubMed] [Google Scholar]
- 20. Fredman L, Hawkes WG, Black S et al. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc 2006;54:1074–1081. [DOI] [PubMed] [Google Scholar]
- 21. Patrick K, Knoefel F, Gaskowski P et al. Medical comorbidity and rehabilitation efficiency in geriatric inpatients. J Am Geriatr Soc 2002;49:1471–1477. [DOI] [PubMed] [Google Scholar]
- 22. Herrick C, Steger‐May K, Sinacore DR et al. Persistent pain in frail older adults after hip fracture repair. J Am Geriatr Soc 2004;52:2062–2068. [DOI] [PubMed] [Google Scholar]
- 23. Muir SW, Yohannes AM. The impact of cognitive impairment on rehabilitation outcomes in elderly patients admitted with a femoral neck fracture: A systematic review. J Geriatr Phys Ther 2009;32:24–32. [DOI] [PubMed] [Google Scholar]
- 24. McGilton KS, Davis A, Mahomed N et al. An inpatient rehabilitation model of care targeting patients with cognitive impairment. BMC Geriatr 2012;12:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. American Psychological Association, Task Force on Socioeconomic Status, 2007 . Report of the APA Task Force on Socioeconomic Status. Washington, DC: American Psychological Association [on‐line] Available at https://www.apa.org/pi/ses/resources/publications/task-force-2006.pdf Accessed January 25, 2015. [Google Scholar]
- 26. Folstein MF, Folstein SE, McHugh PR. ‘Mini‐mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 27. Mungas D. In‐office mental status testing: A practical guide. Geriatrics 1991;46:54–58,63,66. [PubMed] [Google Scholar]
- 28. Cockwell JR, Folstein MF. Mini‐Mental State Exam. Principles and practice of geriatric psychiatry In: Copeland JRM, Abou‐Saleh MT, Blazer DG, eds. Principles and Practice of Geriatric Psychiatry, 2nd Ed. Chichester: Wiley, 2002, pp 140–156 [on‐line]. Available at http://xa.yimg.com/kq/groups/27461618/536209845/name/geraitry_psyquiatry-2002.pdf#page=150 Accessed January 11, 2015. [Google Scholar]
- 29. Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross‐validation. Psychol Med 1994;24:145–153. [DOI] [PubMed] [Google Scholar]
- 30. Williams SW, Williams CS, Zimmerman S et al. Characteristics associated with mobility limitation in long‐term care residents with dementia. Gerontologist 2005;1:62–67. [DOI] [PubMed] [Google Scholar]
- 31. Chaudhry H, Devereaux PJ, Bhandari M. Cognitive dysfunction in hip fracture patients. Orthop Clin North Am 2013;44:153–162. [DOI] [PubMed] [Google Scholar]
- 32. McGilton K, Calabrese S, Davis A et al. Outcomes for older adults following hip fracture surgery in an inpatient rehabilitation facility. Arch Gerontol Geriatr 2008;49:23–31. [DOI] [PubMed] [Google Scholar]
- 33. Siu AL, Boockvar KS, Penrod JD et al. Effect of inpatient quality of care on functional outcomes in patients with hip fracture. Med Care 2006;44:862–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Eastwood EA, Magaziner J, Wang J et al. Patients with hip fracture: Subgroups and their outcomes. J Am Geriatr Soc 2002;50:1240–1249. [DOI] [PubMed] [Google Scholar]
- 35. Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br 1993;75:797–798. [DOI] [PubMed] [Google Scholar]
- 36. Gruber‐Baldini AL, Zimmerman S, Morrison RS et al. Cognitive impairment in hip fracture patients: Timing of detection and longitudinal follow‐up. J Am Geriatr Soc 2003;51:1227–1236. [DOI] [PubMed] [Google Scholar]
- 37. Young Y, Brant L, German P et al. A longitudinal examination of functional recovery among older people with subcapital hip fractures. J Am Geriatr Soc 1997;45:288–294. [DOI] [PubMed] [Google Scholar]
- 38. Magaziner J, Simonsick EM, Kashner TM et al. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J Gerontol 1990;45:101–107. [DOI] [PubMed] [Google Scholar]
- 39. Dubljanin‐Raspopovic E, Markovic‐Denic L, Matanovic D et al. Is pre‐fracture functional status better than cognitive level in predicting short‐term outcome of elderly hip fracture patients? Arch Med Sci 2012;8:115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Portegijs E, Buurman BM, Essink‐Bot ML et al. Failure to regain function at 3 months after acute hospital admission predicts institutionalization within 12 months in older patients. J Am Med Dir Assoc 2012;13(569–567):e1–e7. [DOI] [PubMed] [Google Scholar]
- 41. Brauer CA, Coca‐Perraillon M, Cutler DM et al. Incidence and mortality of hip fractures in the United States. JAMA 2009;302:1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rozzini R, Frisoni GB, Barbisoni P et al. Dementia does not prevent the restoration of safe gait after hip fracture. J Am Geriatr Soc 1997;45:1406–1407. [DOI] [PubMed] [Google Scholar]
- 43. Beloosesky Y, Grinblat J, Epelboym B et al. Dementia does not significantly affect complications and functional gain in elderly patients operated on for intracapsular hip fracture. Arch Orthop Trauma Surg 2001;121:257–260. [DOI] [PubMed] [Google Scholar]
- 44. Gracia De San Roman R. Assessment of the relationship between a high level of dependence and the incidence of perioperative complications in elderly patients admitted for hip fracture. Eur Geriatr Med 2011;2:20–21. [Google Scholar]
- 45. Morrison RS, Magaziner J, McLaughlin MA et al. The impact of post‐operative pain on outcomes following hip fracture. Pain 2003;103:303–311. [DOI] [PubMed] [Google Scholar]


