Abstract
Aims
A prolonged corrected QT interval (QTc) ≥500 ms is associated with high all-cause mortality in hospitalized patients. We aimed to explore any difference in short- and long-term mortality in patients with QTc ≥500 ms compared with patients with QTc <500 ms after adjustment for comorbidity and main diagnosis.
Methods and results
Patients with QTc ≥500 ms who were hospitalized at Telemark Hospital Trust, Norway between January 2007 and April 2014 were identified. Thirty-day and 3-year all-cause mortality in 980 patients with QTc ≥500 ms were compared with 980 patients with QTc <500 ms, matched for age and sex and adjusting for Charlson comorbidity index (CCI), previous admissions, and main diagnoses. QTc ≥500 ms was associated with increased 30-day all-cause mortality [hazard ratio (HR) 1.90, 95% confidence interval (CI) 1.38–2.62; P < 0.001]. There was no significant difference in mortality between patients with QTc ≥500 ms and patients with QTc <500 ms who died between 30 days and 3 years; 32% vs. 29%, P = 0.20. Graded CCI was associated with increased 3-year all-cause mortality (CCI 1–2: HR 1.62, 95% CI 1.34–1.96; P < 0.001; CCI 3–4: HR 2.50, 95% CI 1.95–3.21; P < 0.001; CCI ≥5: HR 3.76, 95% CI 2.85–4.96; P < 0.001) but was not associated with 30-day all-cause mortality.
Conclusion
QTc ≥500 ms is a powerful predictor of short-term mortality overruling comorbidities. QTc ≥500 ms also predicted long-term mortality, but this effect was mainly caused by the increased short-term mortality. For long-term mortality, comorbidity was more important.
Keywords: Long QT syndrome, Risk factor, Arrhythmia, All-cause mortality, Charlson comorbidity index
What’s new?
A prolonged corrected QT interval (QTc) ≥500 ms is a powerful predictor of short-term mortality overruling comorbidities.
QTc ≥500 ms did also predict long-term mortality, but this effect was mainly caused by the increased short-term mortality.
The Charlson comorbidity index was a good predictor of mortality between 30 days and 3 years.
Introduction
A prolonged corrected QT interval (QTc) ≥500 ms on an electrocardiogram (ECG) is associated with high all-cause mortality in hospitalized patients, reflecting the morbidity and multipharmacy in these patients.1–4 It is also associated with increased risk of torsades de pointes (TdP) ventricular arrhythmias.5 We have previously described several predictors of mortality in hospitalized patients with QTc ≥500 ms and have also proposed a new QTc mortality score to improve the prediction of mortality in a clinical setting.4 The risk of QT prolongation depends on the underlying repolarization reserve. This reserve is a product of the interaction between different risk factors, including genetic predisposition.6,7 Several QT prolonging risk factors are identifiable and reversible, including transient QT prolongation during acute non-cardiac illness.8,9
The Charlson comorbidity index (CCI)10 is a widely used measurement of comorbidity, which is validated as a tool for prediction of mortality in a variety of clinical conditions including cardiac arrhythmias.11–13 Each comorbidity included in CCI is weighted (1, 2, 4, or 6) depending on the associated risk, with a weight of six being the most severe. The scores for each condition are summarized and the sum score can be used for prediction of mortality for the individual patient.
It is well documented that QTc ≥500 ms is associated with increased all-cause mortality. It is however not known if this is due to the acute condition or the chronic comorbidity of the patient. The impact of QTc ≥500 ms on short-term and long-term survival should also be elucidated.
The aim of this study was to explore any difference in short-term and long-term mortality between patients with a prolonged QTc interval ≥500 ms and patients with a QTc <500 ms after adjustment for differences in comorbidity and main diagnosis.
Methods
Study population
Telemark Hospital Trust is a general community hospital within the Norwegian National Health System, serving approximately 173 000, mostly Caucasian, inhabitants. There are no other clinics treating inpatients within this area.
Patients with a prolonged corrected QT interval (QTc) ≥500 ms were compared with patients with QTc <500 ms in a retrospective cohort study design.
Hospital administrative data
Data from the patient administrative system (PAS) from all patients admitted to Telemark Hospital Trust between January 2007 and April 2014 were used. Each data record comprised information for one patient stay at a ward and included type of admission (emergency or elective), coded medical diagnoses according to ICD-10,14 date and time for admission and discharge, in addition to gender and age. The Norwegian National Registry15 contains information on all patients registered with Norway as their past or present country of residence. For patients deceased during follow-up, date of death was imported from the Norwegian National Registry to the PAS database by use of the personal identity number that all permanent residents in Norway have. An encrypted personal identity number was replacing personal identity number before exporting PAS data to files used for analysis.
Patients with QTc ≥500 ms
The ECG database at Telemark Hospital Trust contained 225 117 ECGs from 63 286 unique patients collected throughout a period of 11 years (January 2004–December 2014). The ECG database was searched with the following criteria: QTc (Bazett’s formula) ≥500 ms, QRS width ≤120 ms, age ≥15 years, heart rate >30 and ≤100 b.p.m. (because of the limitations of Bazett’s formula), no acute ST-segment-elevation infarction, and no atrial fibrillation or atrial flutter. All ECGs identified with a QTc ≥500 ms were manually reviewed as described below.
The QT interval was measured manually in the lead showing the longest QT interval as the mean of three consecutive beats. We determined the end of the T wave by the tangent method, and U waves were not included if distinct from the T wave.16 The average heart rate over the entire recording was used if the rhythm was regular. Electrocardiograms with frequent premature ventricular beats or short runs of supraventricular tachycardia were excluded.4 For patients who had more than one ECG meeting the specified criteria, the first ECG with QTc ≥500 ms was chosen for inclusion (index ECG). After the manual review of the ECGs, a total of 1531 patients with at least one ECG with QTc ≥500 ms were identified in the ECG database. The patients with QTc ≥500 ms have been described previously.4,8
All medical records for these patients were searched manually for the following information: date of the first ECG with QTc ≥500 ms (index ECG), primary medical diagnosis for the hospital visit, type of visit (elective, emergency or outpatient), age, sex, and personal identity number.
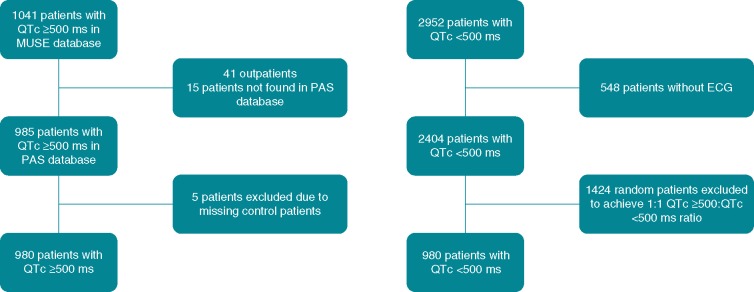
Personal identity numbers for all patients with QTc ≥500 ms were encrypted in the same manner as for the PAS database. Patients with QTc ≥500 ms hospitalized between January 2007 and April 2014 were identified in the PAS database according to the encrypted personal identity number. A total of 490 patients were included in the ECG database before January 2007 or after April 2014, and had no PAS data and were consequently excluded from the present study. All outpatients having an ECG examination at the hospital were included in the ECG database, but data from outpatient examinations were not included in the PAS database for this study. Consequently, 41 outpatients were excluded from the study. The PAS record which was closest to, and within 8 days of, the date and time registered for the index ECG examination was used, and 15 patients did not fulfil this criterium. Five patients with QTc ≥500 ms were excluded due to missing control patients, leaving 980 patients with QTc ≥500 ms to be included for the main study (Figure 1).
Figure 1.
Flow chart showing patients with a QTc ≥500 ms and patients with a QTc <500 ms identified at each stage of the selection process.
Sampling of patients with QTc <500 ms
Random sampling of matched control patients with QTc <500 ms was performed using the PAS database including all emergency admissions at Telemark Hospital Trust, excluding pregnant women. Three patients with QTc <500 ms were sampled per patient with QTc ≥500 ms. The sampling was performed outside the hospital by one author (D.T.K.) who was not involved in treatment of the patients. Matching was performed with respect to gender, age, year, and 4-month period of index ECG examination. For patients with QTc ≥500 ms aged 91 years or more, the patients with QTc <500 ms matched the age intervals 91–95 and 96–100. Two patients with QTc ≥500 ms had only one and two available controls in the PAS database. Consequently, a total of 2952 matched controls with QTc <500 ms were identified. As an extra quality control, the main author (C.G.) identified the selected controls to confirm that they had taken an ECG which did not meet inclusion criteria for cases, i.e. automatically measured QTc was <500 ms. A total of 548 (19%) controls were excluded because of missing ECG. After exclusion of these controls, a total of 980 patients with QTc ≥500 ms had up to three available matched controls, and finally one control with QTc <500 ms was randomly sampled for each patient with QTc ≥500 ms, resulting in 980 pairs for analysis (Figure 1).
Adjustment variables
Charlson comorbidity index
Charlson comorbidity index was calculated from previous admissions from the last 3 years prior to the index admission, but did not include the index admission. The index admission was excluded because a patient with a longer hospital stay is likely to have recorded more diagnoses than a patient who is discharged or dies within a few days. For patients included in 2007–2008, there were no complete 3-year period of previous admissions available. Charlson comorbidity index was pooled into categories: CCI 0, CCI 1–2, CCI 3–4, and CCI ≥5.
Number of admissions preceding year
The number of admissions the last year prior to index admission were pooled into categories 0–1 and ≥2.
Main diagnosis
All patients were categorized according to whether their main diagnosis was acute coronary syndrome (ICD 10-block I20-I22), newly diagnosed cancer (ICD-10 block C00-C97), new-onset heart failure (ICD-10 block I50), or stroke (ICD-10 block I60-I64). As newly diagnosed cancer and new-onset heart failure were detected during the index admission and not included in CCI, these covariates were included as separate variables in the analysis.
Cause of death
Cause of death was categorized into the following groups: cardiovascular, infectious, pulmonary, malignancy, gastrointestinal, neurology, endocrinology, renal, and other.
Statistical methods
Continuous data were described by mean and standard deviation or median and range, and compared by two-sample t-tests or the non-parametric Mann–Whitney U test, as appropriate. Categorical data were summarized by counts and proportions and analysed by the χ2 tests. P-values less than 0.05 were considered statistically significant, and no correction for multiple testing was done.
A Cox proportional hazards model was used to model the patient outcome of dead/alive after 30 days and 3 years, using the following covariates: number of previous admissions, CCI, and main diagnosis. Variables with fewer than 10 observations were excluded from the multivariate analysis. We analysed the variance inflation factor to exclude multicollinearity and explored whether the predictors satisfied the proportional hazard assumption. The final model compared patients with QTc ≥500 ms and patients with QTc <500 ms adjusting for number of previous admissions, CCI, and main diagnosis in a multivariate Cox regression analysis. The survival profiles for the patient groups were visualized by Kaplan–Meier curves for 30-day and 3-year mortality. Log-rank tests were used to compare the patient groups.
The analyses and random sampling were performed with R, versions 2.15.2 and 3.0.3 (free software available at http://www.r-project.org) and SPSS, version 23.0 (IBM, Armonk, NY, USA).
Sensitivity analysis was performed by analysing 985 patients with QTc ≥500 ms and 2952 patients with QTc <500 ms and demonstrated that we did not introduce any systematic errors. The results are shown in Supplementary material online, Table S1 and Figure S1.
Ethics
The study complies with the Declaration of Helsinki. The Norwegian Regional Committee for Medical and Health Research Ethics approved the study (2013/1090).
Results
Characteristics of the study population
A total of 1960 patients (41% males, median age 73 years, range 15–100 years) were included in the dataset and were available for analysis; 980 patients with QTc ≥500 ms and 980 patients with QTc <500 ms. Demographics of patients included in the study are shown in Table 1. The patients with QTc ≥500 ms had a higher number of previous admissions and a longer median length of stay compared with the patients with QTc <500 ms. There was no significant difference in median CCI score between patients with QTc ≥500 ms and patients with QTc <500 ms, within the groups of patients who died before or after 30 days.
Table 1.
Demographic data in 980 patients with QTc ≥500 ms and 980 patients with QTc <500 ms
| Patients with QTc <500 ms (n = 980) | Patients with QTc ≥500 ms (n = 980) | P-value | |
|---|---|---|---|
| Males, n (%) | 398 (41) | 398 (41) | |
| Age (years), median (range) | 73 (15–100) | 73 (15–97) | |
| ≤40, n (%) | 44 (4.5) | 44 (4.5) | |
| 41–60, n (%) | 186 (19) | 186 (19) | |
| 61–75, n (%) | 309 (32) | 309 (32) | |
| 76–85, n (%) | 280 (29) | 280 (29) | |
| 86+, n (%) | 161 (16) | 161 (16) | |
| Admissions preceding year, median (range) | 0 (0–208) | 0 (0–157) | <0.001 |
| 0–1, n (%) | 776 (79) | 720 (74) | <0.01 |
| ≥2, n (%) | 204 (21) | 260 (27) | <0.01 |
| Charlson comorbidity index score, median (range) | 0 (0–11) | 0 (0–11) | 0.06 |
| 0, n (%) | 684 (70) | 643 (66) | 0.053 |
| 1–2, n (%) | 184 (19) | 217 (22) | 0.07 |
| 3–4, n (%) | 66 (6.7) | 74 (7.6) | 0.54 |
| ≥5, n (%) | 46 (4.7) | 46 (4.7) | 1.0 |
Among the conditions included in CCI, mild liver disease and renal disease were more prevalent among the patients with QTc ≥500 ms compared with the patients with QTc <500 ms. For the other conditions, there were no significant differences (Table 2).
Table 2.
Conditions in Charlson comorbidity index among 980 patients with QTc ≥500 ms and 980 patients with QTc <500 ms
| Patients with QTc <500 ms | Patients with QTc ≥500 ms | P-value | |
|---|---|---|---|
| Congestive heart failure, n (%) | 91 (9.3) | 113 (12) | 0.12 |
| Dementia, n (%) | 26 (2.7) | 23 (2.4) | 0.77 |
| Chronic pulmonary disease, n (%) | 97 (9.9) | 93 (9.5) | 0.82 |
| Rheumatic disease, n (%) | 28 (2.9) | 30 (3.1) | 0.89 |
| Mild liver disease, n (%) | 11 (1.1) | 26 (2.7) | 0.02 |
| Diabetes with chronic complication, n (%) | 25 (2.6) | 28 (2.9) | 0.78 |
| Hemiplegia or paraplegia, n (%) | 3 (0.3) | 3 (0.3) | 1.0 |
| Renal disease, n (%) | 53 (5.4) | 89 (9.1) | <0.01 |
| Any malignancya, n (%) | 85 (8.7) | 81 (8.3) | 0.81 |
| Moderate or severe liver disease, n (%) | 7 (0.7) | 13 (1.3) | 0.26 |
| Metastatic solid tumour, n (%) | 31 (3.2) | 22 (2.3) | 0.26 |
| AIDS/HIV, n (%) | 0 (0) | 1 (0.1) | 1.0 |
| Charlson comorbidity index = 0 | 684 (70) | 643 (66) | 0.053 |
Including lymphoma and leukaemia, except malignant neoplasm of skin.
Among the main diagnoses, new-onset heart failure was more prevalent in patients with QTc ≥500 ms compared with patients with QTc <500 ms; 3.2% (n = 31) vs. 1.4% (n = 14), P = 0.01. Acute coronary syndrome was also more prevalent in patients with QTc ≥500 ms than in patients with QTc <500 ms; 14% (n = 138) vs. 6.1% (n = 60), P < 0.001. There were no significant differences in the prevalence of stroke; 3.4% (n = 33) vs. 3.0% (n = 29), P = 0.7 or newly diagnosed cancer; 3.1% (n = 30) vs. 4.4% (n = 43), P = 0.15, between patients with QTc ≥500 ms and patients with QTc <500 ms.
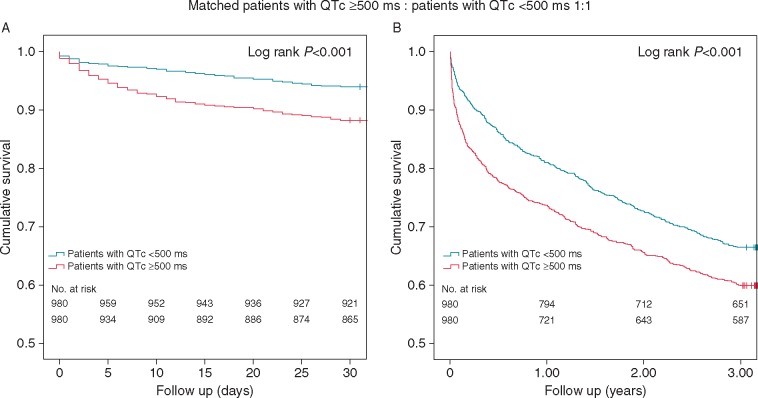
Mortality
The survival analysis showed that the patients with a QTc ≥ 500 ms had significantly lower 30-day and 3-year survival compared with the patients with QTc <500 ms (log rank P < 0.001 for both) (Figure 2). Thirty-day all-cause mortality was 12% (n = 115) in the group of patients with QTc ≥500 ms compared with 6.0% (n = 59) for the group of patients with QTc <500 ms (P < 0.001). Three year all-cause mortality was 40% (n = 393) in patients with QTc ≥500 ms compared with 34% (n = 329) in patients with QTc <500 ms (P < 0.01). There was no significant difference in mortality between patients with QTc ≥500 ms and patients with QTc <500 ms who died between 30 days and 3 years; 32% (n = 278) vs. 29% (n = 270), P = 0.20.
Figure 2.
Thirty-day (A) and 3-year (B) survival curves of 980 patients with QTc ≥500 ms compared with 980 patients with QTc <500 ms.
The Cox regression analyses are presented in Tables 3and4. In the multivariate analysis, a prolonged QTc ≥500 ms was associated with increased 30-day all-cause mortality with a hazard ratio (HR) of 1.90 [95% confidence interval (CI) 1.38–2.62; P < 0.001] and 3-year all-cause mortality with a HR of 1.29 (95% CI 1.11–1.50; P < 0.01) when adjusting for CCI, number of previous admissions and primary diagnosis. Graded CCI was associated with increased 3-year all-cause mortality, but not with 30-day all-cause mortality.
Table 3.
Multivariate Cox regression analysis for 30-day all-cause mortality in 980 patients with QTc ≥500 ms and 980 patients with QTc <500 ms
| Univariate analyses |
Multivariate analysesa |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| QTc ≥500 ms vs. QTc <500 ms | 2.01 | 1.47–2.76 | <0.001 | 1.90 | 1.38–2.62 | <0.001 |
| Charlson comorbidity index 0 | Ref | Ref | ||||
| Charlson comorbidity index 1–2 | 1.34 | 0.93–1.94 | 0.12 | 1.09 | 0.73–1.63 | 0.67 |
| Charlson comorbidity index 3–4 | 2.10 | 1.31–3.36 | <0.01 | 1.46 | 0.87–2.47 | 0.15 |
| Charlson comorbidity index ≥5 | 2.10 | 1.20–3.68 | <0.01 | 1.63 | 0.88–3.0 | 0.12 |
| Admissions preceding year 0–1 | Ref | Ref | ||||
| Admissions preceding year ≥2 | 2.09 | 1.54–2.83 | <0.001 | 1.86 | 1.29–2.69 | <0.01 |
| Acute coronary syndrome | 0.60 | 0.32–1.10 | 0.10 | 0.67 | 0.36–1.25 | 0.21 |
| Cerebral stroke | 3.33 | 1.99–5.56 | <0.001 | 4.31 | 2.53–7.33 | <0.001 |
| Newly diagnosed malignancy | 1.77 | 0.96–3.27 | 0.07 | 1.87 | 1.00–3.48 | 0.049 |
| New-onset heart failure | 3.25 | 1.77–5.99 | <0.001 | 3.37 | 1.80–6.30 | <0.001 |
CI, confidence interval; HR, hazard ratio; Ref, reference; QTc, corrected QT interval.
Adjusted when including all variables.
Table 4.
Multivariate Cox regression analysis for 3-year all-cause mortality in 980 patients with QTc ≥500 ms and 980 patients with QTc <500 ms
| Univariate analyses |
Multivariate analysesa |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| QTc ≥500 ms vs. QTc <500 ms | 1.3 | 1.12–1.50 | <0.01 | 1.29 | 1.11–1.50 | <0.01 |
| Charlson comorbidity index 0 | Ref | Ref | ||||
| Charlson comorbidity index 1–2 | 1.83 | 1.53–2.18 | <0.001 | 1.62 | 1.34–1.96 | <0.001 |
| Charlson comorbidity index 3–4 | 3.22 | 2.57–4.03 | <0.001 | 2.50 | 1.95–3.21 | <0.001 |
| Charlson comorbidity index ≥5 | 4.30 | 3.32–5.56 | <0.001 | 3.76 | 2.85–4.96 | <0.001 |
| Admissions preceding year 0–1 | Ref | Ref | ||||
| Admissions preceding year ≥2 | 2.10 | 1.80–2.45 | <0.001 | 1.35 | 1.13–1.62 | <0.01 |
| Acute coronary syndrome | 0.62 | 0.47–0.83 | <0.01 | 0.72 | 0.54–0.96 | 0.03 |
| Cerebral stroke | 2.04 | 1.46–2.85 | <0.001 | 2.70 | 1.92–3.80 | <0.001 |
| Newly diagnosed malignancy | 3.73 | 2.85–4.88 | <0.001 | 3.20 | 2.44–4.21 | <0.001 |
| New-onset heart failure | 1.43 | 0.92–2.34 | 0.11 | 1.59 | 1.01–2.49 | 0.045 |
CI, confidence interval; HR, hazard ratio; Ref, reference; QTc, corrected QT interval.
Adjusted when including all variables.
There were no significant differences in the distribution of causes of death within 30 days between patients with QTc ≥500 ms and patients with QTc <500 ms (Supplementary material online, Table S2). One patient with QTc ≥500 ms and one patient with QTc <500 ms were reported to die of cardiac arrhythmia (ICD-10 I49.0 and I49.9).
With respect to deaths between 30 days and 3 years, a higher proportion of the patients with QTc <500 ms died of malignancy compared with the patients with QTc ≥500 ms; 20% (n = 53 out of 270) vs. 13% (n = 35 out of 278); P = 0.03, otherwise there were no significant differences in the distribution of cause of death (Supplementary material online, Table S2). Two patients with QTc ≥500 ms, but no patients with QTc <500 ms, were reported to die of cardiac arrhythmia (ICD-10 I49.0 and I49.9).
Discussion
In the present study, the patients with a QTc ≥500 ms had twice as high 30-day all-cause mortality compared with the patients with a QTc <500 ms, matched for age and sex and independent of comorbidity. Beyond 30 days, the difference in mortality between the two groups remained constant. The difference in mortality remained significant both within 30 days and 3 years when adjusting for CCI, number of previous admissions, and main diagnosis. CCI predicted 3-year mortality, but did not predict mortality within 30 days. These findings indicate that QTc ≥500 ms in hospitalized patients is a powerful predictor of short-term mortality overruling comorbidities. QTc ≥500 ms was also a predictor of long-term mortality, but this effect was mainly caused by the increased short-term mortality in our population. CCI was a good predictor for long-term mortality, as shown by others.13
Only a small minority of the patients in our study had arrhythmia as registered cause of death, but the vast majority of patients did not have their heart rhythm monitored at the time of death. Furthermore, the patients were admitted according to their main clinical condition to relevant community hospital wards having low awareness of QT prolongation.4,8 Thus, the occurrence of life-threatening arrhythmias may have been underestimated in our population. We were consequently not able to determine to what degree the increased mortality among the patients with QTc ≥500 ms was due to QT-mediated arrhythmic deaths. In a previous study, Laksman et al.9 described the prognosis of a cohort of hospitalized patients with extreme QTc interval prolongation. The in-hospitalized mortality was high (29%), but only 4% of the patients experienced arrhythmic death, all of which were attributed to secondary causes. Yu et al.2 also described the prognosis of a cohort of hospitalized patients with QTc ≥500 ms and documented life-threatening arrhythmias in 3.8%. These results were similar to our short-term results and support the view that prolonged QTc ≥500 ms recorded in hospitalized patients may be a marker of severe illness, and that the cause of death may not necessarily be primarily arrhythmic. In a previous study, we demonstrated that the main predictors of mortality among the patients with QTc ≥500 ms were aborted cardiac arrest, cerebral stroke/head trauma, and heart failure. We speculate that cardiac ischaemia and structural changes, systemic inflammation, and other unknown factors that affect cardiac action potential and cause QT-prolongation may explain the increased mortality in our population, and that it might be these conditions, and not the QT-prolongation per se, that is responsible for the increased mortality in our population.
QT-prolonging drugs can be well tolerated under normal conditions, but may be potentially lethal when combined with other QT-prolonging drugs, electrolyte disturbances, or medical conditions.6,7,17 Although torsade de pointes may be a rare event,18,19 it is potentially avoidable. In patients with QTc ≥500 ms, important measures include removing QT-prolonging drugs, correcting electrolyte disturbances and other exacerbating factors to prevent TdP.17 However, to what degree elimination of these QT-prolonging risk factors influence all-cause mortality in our population is not known.
Assuming that our findings are representative for patients admitted to Norwegian hospitals, one would expect that among 100 patients with an ECG taken, two to three will have prolonged QTc ≥500 ms.4,8 A prolonged QTc is often missed or even ignored.4 It is important to recognize these high-risk patients since many of the QT prolonging factors are modifiable. Our retrospective study design does not allow us to draw any conclusions regarding causality. One could however speculate that the mortality rate among the patients with QTc ≥ 500 ms could have been lower if the QT prolongation had been acknowledged and appropriate measures had been taken. Future prospective studies should investigate how to reduce short-term mortality in these patients.
Study limitations
The study was performed at a single centre, which may reduce its generalizability. The retrospective design is a limitation due to a higher possibility of unknown biases. Biases may be related to non-uniform registrations of parameters, non-registered confounders, and missing data. For the diagnoses, there is a possibility of misclassification bias. Since the patients with QTc ≥500 ms and patients with QTc <500 ms are sampled from the same population, it is likely that any misclassification bias is equally distributed between patients with QTc ≥500 ms and patients with QTc <500 ms, which is a strength. QT-prolonging drugs and electrolyte disturbances were not available for the 980 patients with QTc <500 ms, and we could consequently not adjust for these variables in the analyses. Bazett’s formula overestimates QTc at high heart rates, and some of the patients may have lower QTc using other correction formulas. Future studies should explore the best cut-off value for QTc to predict mortality.
Conclusions
The patients with a QTc ≥500 ms had twice as high 30-day all-cause mortality compared with the patients with a QTc <500 ms, matched for age and sex and independent of comorbidity. Beyond 30 days, the difference in mortality between the two groups remained constant. Charlson comorbidity index was a predictor of 3-year mortality, but did not predict mortality within 30 days. Our findings indicate that QTc ≥500 ms in hospitalized patients is a powerful predictor of short-term mortality overruling comorbidities. QTc ≥500 ms did also predict long-term mortality, but this effect was mainly caused by the increased short-term mortality in our population. For long-term mortality, comorbidity was more important.
Supplementary Material
Acknowledgements
The authors thank Tomislav Dimoski at Norwegian Institute of Public Health, Oslo, Norway for his contribution by developing the software necessary for extracting PAS data from Telemark Hospital Trust, conducting the data collection and quality assurance of data in this project.
Funding
This work was supported by a grant from Telemark Hospital Trust (Skien, Norway).
Conflict of interest: none declared.
References
- 1. Haugaa KH, Bos JM, Tarrell RF, Morlan BW, Caraballo PJ, Ackerman MJ.. Institution-wide QT alert system identifies patients with a high risk of mortality. Mayo Clin Proc 2013;88:315–25. [DOI] [PubMed] [Google Scholar]
- 2. Yu H, Zhang L, Liu J, Liu Y, Kowey PR, Zhang Y. et al. Acquired long QT syndrome in hospitalized patients. Heart Rhythm 2017;14:974–8. [DOI] [PubMed] [Google Scholar]
- 3. Anderson HN, Bos JM, Haugaa KH, Morlan BW, Tarrell RF, Caraballo PJ. et al. Prevalence and outcome of high-risk QT prolongation recorded in the emergency department from an institution-wide QT alert system. J Emerg Med 2018;54:8–15. [DOI] [PubMed] [Google Scholar]
- 4. Gibbs C, Thalamus J, Heldal K, Holla OL, Haugaa KH, Hysing J.. Predictors of mortality in high-risk patients with QT prolongation in a community hospital. Europace 2018;20:f99–f107. [DOI] [PubMed] [Google Scholar]
- 5. Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J. et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Europace 2015;17:1601–87. [DOI] [PubMed] [Google Scholar]
- 6. Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med 2004;350:1013–22. [DOI] [PubMed] [Google Scholar]
- 7. Schwartz PJ, Woosley RL.. Predicting the unpredictable: drug-induced QT prolongation and torsades de pointes. J Am Coll Cardiol 2016;67:1639–50. [DOI] [PubMed] [Google Scholar]
- 8. Gibbs C, Thalamus J, Tveten K, Busk OL, Hysing J, Haugaa KH. et al. Genetic and phenotypic characterization of community hospital patients with QT prolongation. J Am Heart Assoc 2018;7:e009706.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Laksman Z, Momciu B, Seong YW, Burrows P, Conacher S, Manlucu J. et al. A detailed description and assessment of outcomes of patients with hospital recorded QTc prolongation. Am J Cardiol 2015;115:907–11. [DOI] [PubMed] [Google Scholar]
- 10. Charlson ME, Pompei P, Ales KL, MacKenzie CR.. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- 11. Konig S, Ueberham L, Schuler E, Wiedemann M, Reithmann C, Seyfarth M. et al. In-hospital mortality of patients with atrial arrhythmias: insights from the German-wide Helios hospital network of 161 502 patients and 34 025 arrhythmia-related procedures. Eur Heart J 2018;39:3947–57. [DOI] [PubMed] [Google Scholar]
- 12. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–82. [DOI] [PubMed] [Google Scholar]
- 13. Sharabiani MT, Aylin P, Bottle A.. Systematic review of comorbidity indices for administrative data. Med Care 2012;50:1109–18. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. http://www.who.int/classifications/icd/en/ (30 October 2018, date last accessed).
- 15.The Norwegian Tax Administration. The National Registry. http://www.skatteetaten.no/en/person/national-registry/this-is-the-national-registry/ (30 October 2018, date last accessed).
- 16. Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ. et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009;53:982–91. [DOI] [PubMed] [Google Scholar]
- 17. Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V. et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 2010;121:1047–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vandael E, Vandenberk B, Vandenberghe J, Pince H, Willems R, Foulon V.. Incidence of Torsade de Pointes in a tertiary hospital population. Int J Cardiol 2017;243:511–5. [DOI] [PubMed] [Google Scholar]
- 19. Sarganas G, Garbe E, Klimpel A, Hering RC, Bronder E, Haverkamp W.. Epidemiology of symptomatic drug-induced long QT syndrome and Torsade de Pointes in Germany. Europace 2014;16:101–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.