Abstract
Background
This study aims to determine if repetitive sphenopalatine ganglion (SPG) blockades with 0.5% bupivacaine delivered with the Tx360® device results in long‐term improvement in chronic migraine (CM). The SPG is a small concentrated structure of neuronal tissue that resides within the pterygopalatine fossa in close proximity to the sphenopalatine foramen and is innervated by the maxillary division of the trigeminal nerve. In a previous article, these authors reported repetitive SPG blockades with 0.5% bupivacaine delivered by the Tx360® device, which was an effective and well‐tolerated intervention to incrementally decrease baseline headache intensity of subjects with CM.
Methods
This was a double‐blind, parallel‐arm, placebo‐controlled, randomized pilot study using a novel intervention for acute treatment in CM. A total of 41 subjects were enrolled at two headache specialty clinics in the USA. Eligible subjects were between 18 and 80 years of age and had a history of CM defined by International Classification of Headache Disorders‐II definition. Subjects were allowed a stable dose of migraine preventive medications that was maintained throughout the study. Following a 28‐day baseline period, subjects were randomized by computer‐generated lists 2:1 to receive 0.3 cc of 0.5% bupivacaine or saline, respectively, delivered with the Tx360® twice a week for 6 weeks. Secondary end‐points reported in this manuscript include post‐treatment measures including number of headache days and quality of life measures.
Results
The final data set included 38 subjects: 26 in the bupivacaine group and 12 in the saline group. Our primary end‐point for the study, difference in numeric pain rating scale scores, was met and reported in a previous article. The supplemental secondary end‐points reported in this manuscript did not reach statistical significance. When looking collectively at these end‐points, trends were noticed and worthy of reporting. Subjects receiving bupivacaine reported a decrease in the number of headache days 1 month post‐treatment (Mdiff = −5.71), whereas those receiving saline only saw a slight improvement (Mdiff = −1.93). Headache Impact Test 6 scores were decreased in the bupivacaine group at 1 month (Mdiff = −5.13) and 6 months (Mdiff = −4.78) post‐treatment, but only a modest reduction was seen for those receiving saline at 1 and 6 months, respectively (Mdiff = −2.08, Mdiff = −1.58). Furthermore, subjects receiving bupivacaine reported a reduction in acute medication usage and improved quality of life measures (average pain in the previous 24 hours, mood, normal work, and general activity) up to 6 months post‐treatment. The changes in these measures for the saline group were minimal.
Conclusions
Data from this exploratory pilot study suggest that there may be long‐term clinical benefits with the use of repetitive SPG blockades with bupivacaine delivered with the simple to use Tx360® device. These include a sustained reduction of headache days and improvement in several important quality of life assessments. The SPG blockades were not associated with any significant or lasting adverse events. Further research on SPG blockade is warranted.
Keywords: chronic migraine, episodic migraine, sphenopalatine ganglion block, Tx360®
Abbreviations
- CM
chronic migraine
- EM
episodic migraine
- MOH
medication overuse headache
- HIT‐6
Headache Impact Test‐6
- NRS
numeric rating scale
- PGIC
Patient's Global Impression of Change
- ANOVA
analysis of variance
- SPG
sphenopalatine ganglion
Episodic migraine (EM) is a self‐limited recurrent pain syndrome with the potential to evolve into chronic migraine (CM). CM is a leading cause of neurological disease‐related disability and is considered to be, in most cases, a complication of EM.1 Although individual attacks of migraine can produce severe self‐limited disability,2 the true disease burden of migraine is largely a consequence of the accumulated disability associated with repeated attacks of migraine spanning decades.3 CM is associated with increased symptom intensity and duration, numerous comorbidities, and increased healthcare utilization relative to EM.4 As a result, patients with CM carry a greater migraine‐related disease burden than those with EM.5, 6
Numerous risk factors implicated in the transformation of EM to CM include frequency of attacks, failure to have acute treatment optimized, overuse of acute migraine medications, obesity, lower socio‐economic status, and female gender.7, 8 In an effort to prevent medication overuse headache (MOH) and transformation of EM into CM, patients and clinicians face a dilemma: even though benefiting from optimized acute treatment, there are frequency and/or quantity limits being imposed on acute medications. In a recent study, patients reporting their acute treatment to be very poorly optimized as measured by the Migraine Treatment Optimization Questionnaire, 6.8% developed CM within 1 year compared with 1.9% of patients reporting optimized acute treatment.9 This underscores the need for new effective treatment strategies that can be employed in the CM population that do not increase, or at least minimize, the risk of MOH.
To date, there are few clinical trials of acute or preventative pharmacological therapies in treatment of CM. The only Food and Drug Administration‐approved pharmacological treatment for prevention of CM is onabotulinumtoxinA.10 Although numerous other drugs are commonly used to reduce headache days in CM, few have been specifically studied in this indication. Oddly, there are essentially no clinical trials that have been conducted on efficacy of acute pharmacological interventions in CM despite the CM population having significant acute treatment needs. Perhaps this reflects the earlier understanding of migraine as existing primarily as an episodic condition.11, 12
Overall, these factors emphasize the need to develop evidence based data for both acute and preventative treatment in CM. Ideally, an acute treatment for CM should rapidly terminate headache and migraine‐associated symptoms, sustain a pain‐free response for at least 24 hours, and have few, if any, significant adverse events, including the development of MOH. In addition, an ideal acute intervention would protect the nervous system from future attacks of migraine and potentially modify the disease of CM.
The sphenopalatine ganglion (SPG) is the largest network of neurons outside the central and possibly the enteric nervous system. Anatomically, it is accessible through the middle turbinate where it is covered by a thin layer of mucosa overlying the pterygopalatine fossa. The SPG is composed of branches from V1 and V2 of the trigeminal nerve and is richly interconnecting with sympathetic and parasympathetic autonomic fibers. The historical association of the SPG with autonomic function has been used to explain autonomic symptoms of cluster headache. Indeed, data suggest that SPG blockade may be effective in cluster headache. However, numerous autonomic symptoms also occur in migraine; generally observed with the misdiagnosis of “sinus headache.13, 14, 15 Further case reports and small trials suggested that SPG blockade might be of benefit in migraine.16, 17, 18
The Tx360® device (Tian Medical Inc., Lombard, IL, USA) used in this study to anesthetize the SPG facilitates the passage of a small catheter below the middle turbinate of the nose to a distance slightly beyond the pterygopalatine fossa. The catheter is then rotated on an internal tract, allowing 0.5% bupivacaine to be deposited in a retrograde direction onto the mucosa covering over the SPG.
A previous article reported that repetitive SPG blockades with 0.5% bupivacaine delivered by the Tx360® device was an effective and well‐tolerated intervention to incrementally decrease baseline headache intensity of subjects with CM.19 Further, repetitive SPG blockades produced a statistically significant decrease of headache intensity at 15 and 30 minutes postprocedure that was sustained to the 24 hours end‐point. A total of 12 SPG blocks provided over a 6‐week time period demonstrated statistical superiority for 0.5% bupivacaine vs saline. In this article, we expand the original report to include results of the 1‐ and 6‐month follow‐up of this study population and report on the secondary study end‐points. We hypothesized that repetitive SPG blockades would result in long‐term modification of CM. Although this pilot study failed to demonstrate statistically significant differences between active and sham procedures, the overall trends support the use of SPG blockades with bupivacaine delivered with the Tx360® device in treatment of CM deserve further study.
Methods
A double‐blind, parallel‐arm, placebo‐controlled, randomized pilot study was conducted at two headache centers in the USA. Due to lack of comparator studies available and the pilot design of this study, the sample size was estimated and a power analysis was not completed.
Protocol Approvals, Registrations, and Patient Consents
This study was conducted in accordance with the Declaration of Helsinki, all relevant US federal regulations, and in compliance with the International Conference on Harmonization guideline for Good Clinical Practice. The study protocol, informed consent forms, and any other appropriate study‐related documents were reviewed and approved by Sterling Institutional Review Board/Ethics Committee. Written, informed consent was obtained from each subject prior to any protocol‐related activities. The study was a sponsor‐initiated study funded by Tian Medical Inc. and reported on Clinicaltrials.gov (NCT01709708).
Design
Subjects were recruited through the use of flyers, web postings, radio advertisements, and current clinic patients at headache specialty clinics located in Springfield, MO and Ann Arbor, MI. All subjects were screened using international review board‐approved phone scripts. Subjects had a history of CM defined by the International Classification of Headache Disorders, 2nd edition definition 2006, and by history had experienced CM for at least 3 months prior to enrollment. They were allowed to remain on migraine preventive and abortive medications, provided that the dose was stable for 30 days prior to screening and agreed to not start, stop, or change medication and/or dosage during the study period. All headaches associated with the spectrum of CM were treated regardless of pain severity at the time of treatment.
Following a 28‐day baseline period, subjects meeting inclusion and exclusion criteria were randomized at each study site by a supervisory individual who was not associated with the study subjects or visits. The randomization scheme was generated using the web site: (http://www.randomization.com). A total of 41 subjects were randomized 2:1 to receive 0.5% bupivacaine or saline, respectively. The supervisory individual numbered and assigned study medication, based on the randomization plan, in a blinded fashion to subject, coordinator, and investigator (Table 2).
Table 2.
Subject Demographics
| Total (N = 41) | Bupivacaine (N = 27) | Saline (N = 14) | |
|---|---|---|---|
| Gender | |||
| Male | n = 10 (24.4%) | n = 7 (25.9%) | n = 3 (21.4%) |
| Female | n = 31 (75.6%) | n = 20 (74.1%) | n = 11 (78.6%) |
| Age (years) | |||
| Mean | 41.30 | 40.96 | 41.97 |
| Standard deviation | 12.59 | 11.63 | 14.71 |
| Range (min, max) | 18, 67 | 22, 63 | 18, 67 |
| Ethnicity | |||
| Caucasian | n = 34 (82.9%) | n = 20 (74.1%) | n = 14 (100%) |
| African American | n = 4 (9.8%) | n = 4 (14.8%) | n = 0 (0%) |
| Other | n = 3 (7.3%) | n = 3 (11.1%) | n = 0 (0%) |
Study Population
A total of 55 subjects were screened for study inclusion, and 49 met inclusion/exclusion criteria and were required to complete a daily headache diary for 28 days to confirm an accurate diagnosis of CM. Of the 49 subjects, 41 met diagnostic criteria for CM and were randomized 2:1 to receive a series of 12 SPG blocks with either 0.3 cc of 0.5% bupivacaine or saline delivered with the Tx360® over a 6‐week period (2 SPG blocks/week). Pretreatment baseline headache pain scores for randomized headache subjects were determined at visit 2 prior to their first SPG block.
Visits 2 through 13, vital signs and changes in medical, headache, and medication history were collected. Subjects completed the numeric rating scale (NRS) prior to treatment. At visit 2, and visit 14, subjects completed a Headache Impact Test (HIT‐6) questionnaire.
At each treatment visit, subjects were administered an SPG block through each nostril by the investigator or study coordinator using the Tx360® device. This device contains a small, flexible, soft plastic tube that is advanced below the middle turbinate just past the pterygopalatine fossa. The plastic tube can then be rotated laterally on a preset track and extended into the intranasal space. A total of 0.3 cc of anesthetic (0.5% bupivacaine) is injected through the tube and directed to the mucosa covering the SPG.20 Dosing and anesthetic type were determined per device manufacture's recommendations. The procedure is performed similarly in each nostril. All subjects were given a piece of lemon candy as a taste distractor in an effort to maintain blinding prior to each procedure.
After each procedure, subjects completed the NRS at 15 and 30 minutes. At 30 minutes, subjects completed the Patient's Global Impression of Change (PGIC). Subjects also completed the NRS, PGIC, and questions regarding the subject's average pain, general activity interference, mood, and normal work interference for the 24 hours prior to the visit. Daily diaries were completed throughout the active treatment period and 1 month post‐treatment. HIT‐6 scores and quality of life questionnaires were collected by phone at 6 months post‐treatment.
The end‐points addressed below are not a comprehensive list, as many of the study end‐points were previously reported in a previous article.19 This manuscript reports the sustained post‐treatment outcomes of the study. All end‐points in this manuscript are supplemental secondary end‐points.
Secondary End‐Points
To compare change in the number of headache days from the 28‐day baseline period to the last 28 days of the treatment period and 1 month post‐treatment.
To compare average pain, general activity interference, mood, and normal work interference from pretreatment, immediately prior to the last treatment, 1 month post‐treatment, and 6 months post‐treatment.
HIT‐6 scores from pretreatment, immediately prior to the last treatment, 1 month post‐treatment, and 6 months post‐treatment.
Acute medications usage from 28 days baseline period to the last 28 days of the treatment period and 1 month post‐treatment.
Adverse events reported by all subjects.
Table 1.
Inclusion and Exclusion Criteria
| Inclusion Criteria |
|---|
|
| Exclusion Criteria |
|---|
|
Statistical Analysis
Data were collected analyzed using JMP, Version 8 (SAS Institute Inc., Cary, NC, USA) utilizing a repeated measures mixed‐design analysis of variance (ANOVA), including a within‐subjects factor of time (pretreatment, before the final treatment, 1 month post‐treatment, and 6 months post‐treatment), and a between‐subject factor of treatment groups (bupivacaine/sham saline) was also used to analyze data for statistical significance. Post‐hoc analyses were conducted using two sample Wilcoxon rank sums as appropriate. To control for multiple comparisons, Sidak corrections were calculated, and a cut‐off of P = .01 was used to determine statistical significance for all post‐hoc analyses. Missing data were reviewed and found to be missing completely at random and less than 5% for any one subject or one variable. All data collected were included in data analysis if eligibility criteria were met, making this a per protocol analysis. Due to lack of significant findings for these supplemental secondary end‐points using the repeated measures mixed‐design ANOVA, only descriptive statistics and effect sizes were reported in this manuscript. Effect sizes of Cohen's d were calculated using measure of the effect (.2 = “small,” .5 = “medium,” and .8 = “large”).21
Results
A total of 41 subjects were randomized 2:1 for this study (27 to bupivacaine and 14 to saline), which includes 10 males and 31 females with a mean age of 41.3 and a diagnosis of CM (Fig. 1, Table 3). Of the study population, 83% were Caucasian, 10% African American, and 7% Other. A total of 40 subjects completed treatment in the bupivacaine and sham saline groups, 27 and 13, respectively. During the treatment period, one subject withdrew consent in the saline group due to lack of efficacy; however, this subject's data remained in the analysis. Three subjects, one in the bupivacaine group and two in the sham saline group, were removed from data analysis due to being incorrectly randomized. Based on re‐analysis of their 28‐day baseline diaries, they did not meet the definition of CM during the baseline period. Consequently, the final data set included 38 subjects, 26 in the bupivacaine group and 12 in the sham saline group (including one subject that did not complete treatment) (Fig. 2). Subjects were diagnosed with CM on an average of 8.58 years prior to the start of the study and had an average of 23.63 headache days per month with 15.24 of them being classified with a migraine phenotype. (Table 3).
Figure 1.
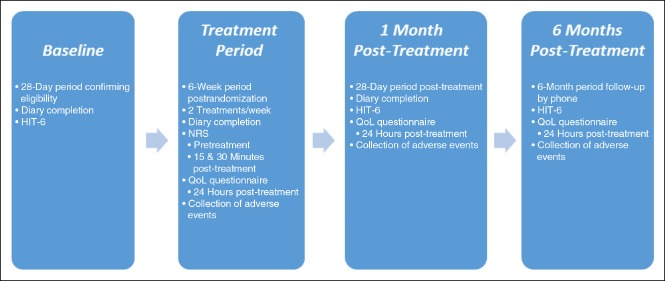
Study timeline. HIT‐6, Headache Impact Test‐6; QoL, quality of life.
Table 3.
Migraine Characteristics
| Total (M) | Bupivacaine (M) | Saline (M) | |
|---|---|---|---|
| Chronic migraine diagnosis duration (years) | 8.58 | 8.78 | 8.20 |
| Baseline migraine days | 15.2 | 15 | 15.8 |
| Baseline headache days | 23.6 | 23.1 | 24.8 |
Figure 2.
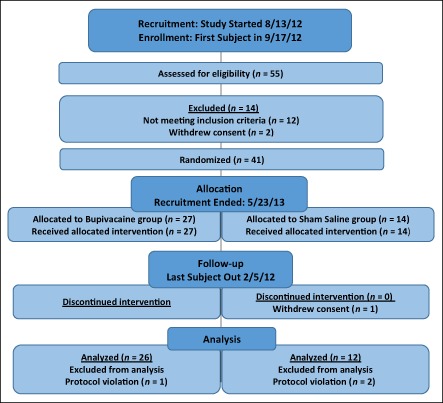
Study flow diagram.
Primary End‐Point
Although not the focus of this manuscript and previously reported in another manuscript, the primary end‐point of the study was to compare NRS scores at baseline, and 15 minutes, 30 minutes, and 24 hours post‐treatment between SPG blockades with 0.5% bupivacaine vs sham saline.19 When pooling all of the treatments 1 through 12, a repeated measures ANOVA showed a statistically significant interaction of time and group NRS scores over time, F(3, 438) = 4.90, P = .002. Results also revealed a statistically significant main effect of time (F(3, 438) = 29.34, P < .001) and group (F(1, 440) = 18.61, P < .001).
Headache Days
Comparing the number of headache days during the baseline period, the last 28 days of the treatment period, and 1 month post‐treatment differences between groups were not found to be significant. A decrease in the number of headache days for the bupivacaine group was found when comparing baseline, treatment, and 1 month post‐treatment (Fig. 3 and Table 4). Those in the saline group had only a modest reduction in headache days.
Figure 3.
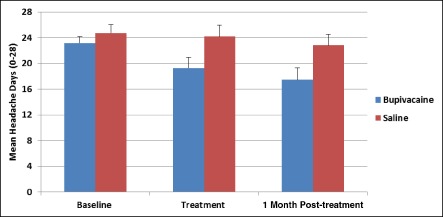
Headache days. The number of headache days were consistently lower at the end of treatment and 1 month post‐treatment for the bupivacaine group compared to the saline group.
Table 4.
Headache Days
| Bupivacaine | Saline | Effect Size | |||
|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | d | |
| Baseline | 25 | 23.15 (5.12) | 11 | 24.75 (4.35) | .33 |
| Treatment | 25 | 19.27 (8.39) | 11 | 24.17 (5.89) | .63 |
| 1 Month post‐treatment | 25 | 17.44 (9.08) | 11 | 22.82 (5.36) | .66 |
SD, standard deviation.
Average Pain
There was no significant difference in average pain between the bupivacaine and saline group at any time point. However, average pain rating for the 24 hours prior to a visit showed that the bupivacaine group had a decrease in pain rating when compared with pretreatment levels at the end of treatment, 1 month post‐treatment, and 6 months post‐treatment (Fig. 4, Table 5). The saline group showed a less robust decrease.
Figure 4.
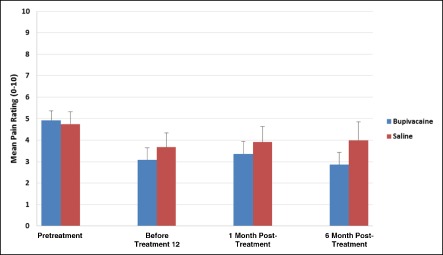
Average pain last 24 hours. Average pain scores were lower for the bupivacaine group compared with the saline group at treatment 12, 1 month post‐treatment, and 6 months post‐treatment.
Table 5.
Average Pain Previous 24 hours
| Bupivacaine | Saline | Effect Size | ||||
|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | d | ||
| Average pain | Pretreatment | 22 | 4.92 (2.23) | 8 | 4.75 (1.91) | .08 |
| Before treatment 12 | 22 | 3.08 (2.78) | 8 | 3.67 (2.23) | .22 | |
| 1 Month post‐treatment | 22 | 3.36 (2.87) | 8 | 3.91 (2.30) | .20 | |
| 6 Months post‐treatment | 22 | 2.86 (2.62) | 8 | 4.00 (2.27) | .45 | |
SD, standard deviation.
Quality of Life Measures
General Activity
Interference ratings of general physical activity were not found to significantly differ between groups at treatment 12, 1 month post‐treatment, or 6 months post‐treatment. Ratings of general physical activity reported by subjects over the duration of the study showed a sustained decrease in interference for bupivacaine group when comparing pretreatment, before treatment 12, 1 month post‐treatment, and 6 months post‐treatment (Table 6). The saline group initially decreased before treatment 12, but then interference ratings increased 1 and 6 months post‐treatment.
Table 6.
General Activity, Mood, and Normal Work Interference in the Previous 24 hours
| Bupivacaine | Saline | Effect Size | ||||
|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | d | ||
| General activity | Pretreatment | 22 | 3.96 (2.99) | 7 | 5.00 (3.10) | .34 |
| Before treatment 12 | 22 | 2.52 (3.31) | 7 | 2.50 (2.50) | .01 | |
| 1 Month post‐treatment | 22 | 2.64 (2.91) | 7 | 3.91 (2.81) | .44 | |
| 6 Months post‐treatment | 22 | 2.68 (2.87) | 7 | 4.00 (3.32) | .44 | |
| Mood | Pretreatment | 22 | 4.85 (3.16) | 7 | 5.33 (2.96) | .15 |
| Before treatment 12 | 22 | 2.44 (3.38) | 7 | 3.17 (2.89) | .22 | |
| 1 Month post‐treatment | 22 | 2.96 (3.43) | 7 | 3.82 (3.40) | .25 | |
| 6 Months post‐treatment | 22 | 3.18 (3.26) | 7 | 5.71 (3.68) | .75 | |
| Normal work | Pretreatment | 22 | 4.12 (3.10) | 7 | 5.17 (3.19) | .34 |
| Before treatment 12 | 22 | 2.64 (3.33) | 7 | 2.50 (2.75) | .04 | |
| 1 Month post‐treatment | 22 | 2.52 (3.14) | 7 | 3.45 (2.94) | .30 | |
| 6 Months post‐treatment | 22 | 2.59 (2.77) | 7 | 3.71 (3.50) | .38 | |
SD, standard deviation.
Mood
Ratings of mood interference within the last 24 hours revealed no between group differences. The bupivacaine group mood interference ratings improved when comparing pretreatment, to end of treatment, 1 month post‐treatment, and 6 months post‐treatment (Table 6). The saline group improved initially in mood interference ratings, however at 6 months post‐treatment increased compared with pretreatment ratings.
Normal Work
Significance between group differences was not found for normal work interference ratings within the last 24 hours. Subjects treating with bupivacaine showed improvements in their ability to perform normal work when comparing pretreatment, end of treatment, 1 month post‐treatment, and 6 months post‐treatment (Table 6). Those in the saline group experienced a modest improvement.
HIT‐6
Significance between group scores for the HIT‐6 was not detected. HIT‐6 scores improved over pretreatment scores at both 1 and 6 months post active treatment for the bupivacaine group and were sustained through 6 months. (Fig. 5, Table 7). Modest improvement was observed in the saline group.
Figure 5.
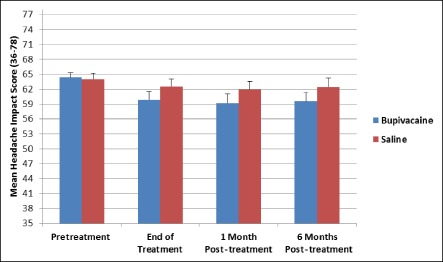
Headache Impact Test‐6 (HIT‐6 scores). HIT‐6 scores subjects receiving bupivacaine were decreased throughout the study and were found to be consistently lower than saline scores.
Table 7.
HIT‐6 Scores
| Bupivacaine | Saline | Effect Size | |||
|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | d | |
| Pretreatment | 26 | 64.36 (4.93) | 12 | 64.00 (3.92) | .08 |
| End of treatment | 26 | 59.85 (8.33) | 12 | 62.50 (4.96) | .36 |
| 1 Month post‐treatment | 26 | 59.23 (8.97) | 12 | 61.92 (5.45) | .33 |
| 6 Months post‐treatment | 26 | 59.58 (9.14) | 12 | 62.42 (5.96) | .34 |
HIT‐6, Headache Impact Test‐6; SD, standard deviation.
Acute Medication Usage
When analyzing the average number of times a subject used any acute medication for migraine treatment during the study, the bupivacaine group reported a decrease in the number of medications used when comparing baseline, treatment, and 1 month post‐treatment (Fig. 6 and Table 8). The saline group reported a less robust decrease.
Figure 6.
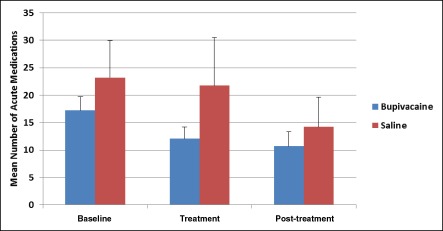
Acute medication usage. Although acute medication usage did not significantly differ between groups at any time point, subjects receiving bupivacaine generally reported lower usage of acute medication than those treated with saline.
Table 8.
Acute Medication Usage
| Bupivacaine | Saline | Effect Size | |||
|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | d | |
| Baseline | 26 | 17.23 (12.29) | 12 | 23.25 (22.13) | .38 |
| Treatment | 26 | 12.08 (10.86) | 12 | 21.75 (28.90) | .53 |
| Post‐treatment | 26 | 10.73 (12.70) | 12 | 14.25 (17.73) | .24 |
SD, standard deviation.
Discussion
In an earlier paper, it was demonstrated that subjects with CM receiving repetitive SPG blockades using the Tx360® device with 0.5% bupivacaine experienced statistically superior headache relief at 15 and 30 minutes to subjects receiving saline and that this benefit was maintained at 24 hours post‐treatment.19 In this paper, we report on the study population results at 1 and 6 months following active treatment with repetitive SPG blockades. Although statistical significance was not reached, the authors suggest that the culmination of all end‐points supports potential for long‐term benefits at 1 and 6 months for subjects with CM after receiving a series of 12 SPG blocks over a 6‐week period with bupivacaine vs saline. Due to the lack of statistical findings, the exploratory nature of this pilot study, and the modest effect size, it is hypothesized that the sample size (N = 38) may have played a role in limiting the significance of the statistical comparisons conducted. A post‐hoc power analysis revealed that on the basis of the mean, between‐groups comparison effects size observed for headache day reduction at the end of treatment (d = .63), an n of approximately 92 would be needed to obtain statistical power at the recommend .80 level.22 This calculation further supports that this study was underpowered.
However, multiple trends in these data are worth noting. There was a 5.7 reduction in headache days for the bupivacaine group vs a 1.9‐day reduction for the saline group at 1 month post‐treatment. The difference in the reduction in headache days between active and sham procedures is similar to the reduction noted for onabotulinumtoxinA in the Phase III Research Evaluating Migraine Prophylaxis Therapy studies and for topiramate in CM.23, 24 HIT‐6 scores were lower at 6 months vs baseline for the bupivacaine group, but only slightly decreased for the saline group. In addition, relative to baseline scores, subjects receiving bupivacaine reported less normal work interference at 6 months post‐treatment vs baseline. The bupivacaine group also showed a reduction in mood interference and general activity interference. There was a reduction of average headache pain over a 24‐hour period observed for the bupivacaine group over baseline. Additionally, a reduction of acute medications usage at 1 month post‐treatment vs baseline was found. There were only slight changes in all of these measures for the group receiving SPG blockades with saline. Considering these data collectively suggests that there could be a long‐lasting clinical benefit for repetitive SPG blockades with bupivacaine. Important to note and given the small sample size, the actual clinical significance of the quality of life measures and medication usage require further study. Clearly, there is a suggestion of disease modification for this procedure.
The use of prophylactic medications was allowed in this study except for onabotulinumtoxinA. Whether refinement of prophylactic regimens or the use of onabotulinumtoxinA might provide a synergistic benefit is a topic warranting further investigation.
There are numerous limitations to this study. The sample size is relatively small combined with a 2:1 bupivacaine vs saline randomization, statistical comparisons of the two groups is challenging due to differences in statistical power between groups. In addition, the treatment scheme and schedule used in this study is arbitrary. Refinement of the active treatment scheme or selection of patients based on subsets of CM such as medication overuse, location of headache, or comorbidities was not conducted. SPG blockades have been reported in small studies as effective in anatomically remote medical disorders such as back pain, complex regional pain syndromes, and myofascial pain syndromes underscoring the potential role of SPG in various migraine comorbidities.25 A further limitation reported in the previous paper is that the most common adverse events reported in the bupivacaine group were taste disturbances, lacrimation, and oral numbing. We considered whether these adverse events may have disrupted study blinding. However, there were no differences in response for subjects reporting or not reporting any of these specific adverse events and most subjects experienced these events with only some, but not all treatments. In addition, the data observed at 1 and 6 months were likely less affected by this bias, if it did exist.
Regardless, the use of repetitive SPG blockades with bupivacaine delivered by the Tx360® device has the potential to be an effective and novel short‐ and long‐term treatment for CM and warrants further investigation. It may be an attractive alternative to acute or prophylactic systemic pharmacology in this challenging clinical population. Of particular note was the significant reduction in headache days and the sustained reduction in the use of acute medications observed in 1 month post‐treatment for SPG blockade with bupivacaine. This suggests the possibility that repetitive SPG blockade with bupivacaine may have disease‐modifying benefits. This too merits further study.
Conclusion
Data from this exploratory pilot study does not establish efficacy, but suggests the possibility there may be long‐term clinical benefits in the use of repetitive SPG blockade with bupivacaine delivered with the Tx360® device vs sham with saline. These include a sustained reduction of headache days and improvement in several important quality of life assessments. Finally, the long‐term reduction in headache days suggests that possibly, there might be a disease‐modifying benefit for SPG blockade with bupivacaine, but not saline. Clearly, a more complete study of this novel treatment modality is warranted, as well as more studies to determine the role of the SPG in the physiology in migraine and its treatment.
Statement of Authorship
Category 1
-
(a)
Conception and Design
Roger Cady, Joel Saper
-
(b)
Acquisition of Data
Roger Cady, Joel Saper, Kent Dexter, Ryan Cady
-
(c)
Analysis and Interpretation of Data
Roger Cady, Heather Manley, Joel Saper
Category 2
-
(a)
Drafting the Manuscript
Roger Cady, Joel Saper, Heather Manley, Ryan Cady
-
(b)
Revising It for Intellectual Content
Roger Cady, Joel Saper, Heather Manley, Kent Dexter, Ryan Cady
Category 3
-
(a)
Final Approval of the Completed Manuscript
Roger Cady, Joel Saper, Heather Manley, Kent Dexter, Ryan Cady
Supporting information
Table S1.—CONSORT 2010 checklist of information to include when reporting a randomized trial.
Study approved by Sterling Institutional Review Board/Ethics Committee.
Conflict of Interest: Dr. Roger K. Cady currently serves on several advisory boards: Allergan, Avanir, Boston Scientific, DepoMed, Novartis, OptiNose US Inc., Pfizer, and Zogenix. He also receives research grants from Allergan, Amgen, AstraZeneca, Boston Scientific, Bristol Myers, ElectroCore, Labrys Biologics, OptiNose, Pharmalyte Solutions LLC, Tian Medical LLC, and Vivid Pharma Inc. Dr. Cady provided consulting services for Aerocrine, Allergan, Avanir, Becker Pharma Consulting, Duke University, DepoMed, Evidera, Inc., Impax Pharmaceuticals, Teva Pharmaceuticals, and Zogenix.
Dr. Joel Saper receives research grants from Achelios, Alder, Allergan, Amgen, Astellas, AstraZeneca, GlaxoSmithKline, Electrocore, Innovative Medical Concepts, Labrys Biologics, Neuraxon, Novartis, OptiNose, Osmotica, Pfizer Inc., Tian Medical, and Vanda & Winston Laboratories. Dr. Saper receives consultant/honorarium from Allergan, NuPathe, Johnson & Johnson (Ethicon), Purdue Pharma, Supernus, Medscape, Tian Medical, and Migraine Research Foundation. Dr. Kent Dexter, Ryan J. Cady, and Heather R. Manley have nothing to disclose.
Financial Support: This research study supported by a grant from Tian Medical Inc. (Lombard, IL, USA).
Trial Registration: ClinicalTrials.gov (NCT01709708).
References
- 1. Silberstein SD, Lipton RB, Saper JR. Chronic daily headache including transformed migraine, chronic tension‐type headache, and medication overuse headache In: Silberstein SD, Lipton RB, Dodick DW, eds. Wolff's Headache and Other Head Pain, 8th edn New York: Oxford University Press; 2008:315‐377. [Google Scholar]
- 2. Bigal ME, Lipton RB. The prognosis of migraine. Curr Opin Neurol. 2008;21:301‐308. [DOI] [PubMed] [Google Scholar]
- 3. Bigal ME, Lipton RB. Concepts and mechanisms of migraine chronification. Headache. 2008;48:7‐15. [DOI] [PubMed] [Google Scholar]
- 4. Hazard E, Muakata J, Bigal ME, Rupnow MFT, Lipton RB. The burden of migraine in the United States: Current and emerging perspectives on disease management and economic analysis. Value Health. 2009;12:55‐64. [DOI] [PubMed] [Google Scholar]
- 5. Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: Results from the International Burden of Migraine Study (IBMS). Cephalalgia. 2011;31:301‐315. [DOI] [PubMed] [Google Scholar]
- 6. Stokes M, Becker WJ, Lipton RB, et al. Cost of health care among patients with chronic and episodic migraine in Canada and the USA: Results from the International Burden of Migraine Study (IBMS). Headache. 2011;51:1058‐1077. [DOI] [PubMed] [Google Scholar]
- 7. Katsarava Z, Buse DC, Manack AN, Lipton RB. Defining the differences between episodic migraine and chronic migraine. Curr Pain Headache Rep. 2012;16:86‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lipton RB. Chronic migraine, classification, differential diagnosis, and epidemiology. Headache. 2011;51(Suppl. 2):77‐83. [DOI] [PubMed] [Google Scholar]
- 9. Lipton RB, Fanning KM, Serrano D, Reed ML, Cady R, Buse DC. Ineffective acute treatment of episodic migraine (EM) is associated with new‐onset chronic migraine (CM): Results of the American Migraine Prevalence and Prevention (AMPP) Study. Neurology. 2015;84:688‐695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. BOTOX® (onabotulinumtoxinA) Prescribing Information. Irvine, CA: Allergan, Inc.; 2011. [Google Scholar]
- 11. Haut SR, Bigal ME, Lipton RB. Chronic disorders with episodic manifestations: Focus on epilepsy and migraine. Lancet Neurol. 2006;5:148‐157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bigal ME, Rapoport AM, Lipton RB, et al. Chronic daily headache in a tertiary care population. Correlation between the International Headache Society diagnostic criteria and proposed revisions of criteria for chronic daily headache. Cephalalgia. 2002;22:432‐438. [DOI] [PubMed] [Google Scholar]
- 13. Cady RK, Schreiber CP. Sinus headache or migraine. Neurology. 2002;58:S10‐S14. [DOI] [PubMed] [Google Scholar]
- 14. Schreiber CP, Hutchinson S, Webster CJ, Ames M, Richardson MS, Powers C. Prevalence of migraine in patients with a history of self‐reported or physician‐diagnosed “sinus” headache. Arch Intern Med. 2004;164:1769‐1772. [DOI] [PubMed] [Google Scholar]
- 15. Barbanti P, Fabbrini G, Pesare M, Vanacore N, Cerbo R. Unilateral cranial autonomic symptoms in migraine. Cephalalgia. 2002;22:256‐259. [DOI] [PubMed] [Google Scholar]
- 16. Maizels M, Geiger AM. Intranasal lidocaine for migraine: A randomized trial and open‐label follow‐up. Headache. 1999;39:543‐551. [DOI] [PubMed] [Google Scholar]
- 17. Obah C, Fine PG. Intranasal sphenopalatine ganglion block: Minimally invasive pharmacotherapy for refractory facial and headache pain. J Pain Palliat Care Pharmacother. 2006;20:57‐59. [PubMed] [Google Scholar]
- 18. Láinez MJ, Puche M, Garcia A, Gascón F. Sphenopalatine ganglion stimulation for the treatment of cluster headache. Ther Adv Neurol Disord. 2014;7:162‐168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cady RK, Saper J. A double‐blind, placebo‐controlled study of repetitive transnasal sphenopalatine ganglion blockade with TX360® as acute treatment for chronic migraine. Headache. 2015;55:101‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Candido KD, Massey ST, Sauer R, Darabad RR, Knezevic NN. A novel revision to the classical transnasal topical sphenopalatine ganglion block for the treatment of headache and facial pain. Pain Physician. 2013;16:E769‐E778. [PubMed] [Google Scholar]
- 21. Buchanan EM, Valentine KD, Cota L, Derringer C, Melia M. Effect sizes should be easy: A Windows program to calculate effect sizes and their confidence intervals. Paper presented at: 54th Annual Meeting Psychonomic Society; 2013; Toronto, Ontario, Canada.
- 22. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149‐1160. [DOI] [PubMed] [Google Scholar]
- 23. Aurora SK, Dodick DW, Turkel CC, et al. OnabotulinumtoxinA for treatment of chronic migraine: Results from the double‐blind, randomized placebo‐controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793‐803. [DOI] [PubMed] [Google Scholar]
- 24. Diener HC, Dodick DW, Aurora SK, et al. OnabotulinumtoxinA for treatment of chronic migraine: Results from the double‐blind, randomized, placebo‐controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30:804‐814. [DOI] [PubMed] [Google Scholar]
- 25. Malinowski MN, Day MR. Sphenopalatine ganglion block In: Waldman SD, ed. Pain Management. Philadelphia, PA: Saunders Elsevier; 2011:1054‐1061. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.—CONSORT 2010 checklist of information to include when reporting a randomized trial.


