Abstract
Purpose
The aim of this prospective study was to evaluate quality of life (QoL) and sexual function of women affected by endometriosis pain treated with Dienogest (DNG) for 24 months.
Patients and methods
Fifty-four women constituted the study group and were given DNG 2 mg/daily; 38 women were given non-steroidal anti-inflammatory drugs (NSAIDs) and constituted the control group. To define endometriosis-associated pelvic pain, dysmenorrhea and dyspareunia the Visual Analogic Scale (VAS) was used. The Short Form-36 (SF-36), the Female Sexual Function Index (FSFI) and the Female Sexual Distress Scale (FSDS) were used to assess the QoL, sexual function and the sexual distress, respectively. The study included five follow-ups at 3, 6, 12, 18 and 24 months.
Results
Slight improvements in chronic pelvic pain, dysmenorrhea and dyspareunia were observed in the study group at 3 months (p<0.05) and improved more from 6 to 24 months of DNG treatment (p<0.001). QoL improved with a similar trend: at 3 months the improvement was significant in several categories (p<0.05), and from 6 to 24 months in all categories (p<0.001). The FSFI score did not change at the 3 month follow-up (p=not significant [NS]) but it improved from 6 to 24 months (p<0.001). A similar trend was observed for the FSDS score (p<0.001). No change was observed in the control group (p=NS).
Conclusion
Long-term treatment with DNG 2 mg once-daily in women with endometriosis-associated pelvic pain may have positive effects on the QoL and sexual life, confirming the observations of the previous study on the first 6 months of treatment.
Keywords: dyspareunia, endometriosis, chronic pelvic pain, long term dienogest, quality of life, sexual life
Introduction
Endometriosis-associated pelvic pain affects approximately 10% of women of reproductive age.1
Other than pelvic pain, women mainly experience dysmenorrhea with cyclical or peri-menstrual symptoms, dyspareunia, dyschezia, fatigue and infertility.2–4 Usually, drugs adopted to treat the chronic pelvic pain are not able to cure women with this problem. Progestins or hormonal contraceptives,3,5 GnRH agonists,6,7 aromatase inhibitors,8 etonogestrel subdermal implant,9 or levonorgestrel-releasing intrauterine devices10,11 are used to counteract the ovarian estrogenic secretion on the endometrium-like tissue developing outside the uterus.12 Even if each of these treatments may be effective and improve quality of life (QoL), pelvic pain usually reappears when women discontinue their usage, thus affecting their QoL. Moreover, women affected by chronic pelvic pain should use drugs having a continuous regimen, including hormonal contraceptives.13 Several women take on-demand non-steroidal anti-inflammatory drugs (NSAIDs) as first line agents to control their pelvic pain.14 Hormonal treatment is adopted only after a specialist diagnoses endometriosis as the cause of the pelvic pain. It is important to remark that women are different in their sensitivity to chronic pelvic pain. Thus, the first step in prescribing a drug for chronic pelvic pain is to understand the needs of each subject.
Dienogest (DNG) is a synthetic progestin that is currently used for clinical treatment of endometriosis with a dose of 2 mg daily.15 The steroid also has direct antiproliferative, immunologic and antiangiogenic activities that contribute to the reduction of endometriosis-associated symptoms and exhibits highly selective binding to the progesterone receptor.16,17
We previously investigated endometriosis-associated pelvic pain of women on DNG for 6 months and observed an improvement in pain, QoL and sexual function.18
The study aims to evaluate how many women rested on DNG at 24-month follow-up, and to measure the pain level (primary endpoint), sexual function and QoL (secondary endpoints).
Materials and methods
Ninety-two women aged 18–37 (mean age 28±8) where enrolled in this prospective study. All the women underwent physical and gynecological examinations and transvaginal ultrasound (TVS) to identify or rule out rectal endometriosis, deep endometriosis, ovarian endometrioma, or adenomyosis. On the basis of ESHRE guidelines,2 women affected by chronic pelvic pain with a clinical diagnosis of endometriosis (dysmenorrhea, noncyclical chronic pelvic pain, deep dyspareunia, and dyschezia) confirmed with gynecological examination and TVS, were enrolled.
Sexual life and function were also assessed: sexually active women having at least one sexual event during the month before the counselling were included.
Women with a history of non-organic sexual dysfunction, or having a partner affected by sexual dysfunction were excluded. Women under GnRH analog treatment during the last 6 months, or hormonal contraceptive treatment less than 3 months before, or choosing a surgical approach were excluded.
After having received counselling on the effects and benefits of DNG, 54 (58.7%) women accepted to take 2 mg DNG once-daily and constituted the study group. The remaining 38 (41.3%) women refused the use of DNG and any other hormonal treatment, preferring to continue their previous NSAIDs on-demand therapy. They were enrolled as the control group after receiving a counseling on the therapy they chose and having signed a new informed consent form.
All the women were asked the names of the NSAIDs they were usually taking to relieve their pelvic pain: paracetamol, ibuprofen, ketoprofen, ketorolac, diclofenac by oral route were the only medication used; patients were allowed to take only NSAIDs contained in this list. No opioids or other types of NSAIDs were used or prescribed.
The study protocol conformed to the ethical guidelines of the 1975 Helsinki Declaration and was approved by the Ethics Committee of the Department of General Surgery and Medical Surgical Specialties of University of Catania. Informed written consent was obtained from each woman before entering the study, and they did not receive payment of any kind.
Instruments
The Visual Analogic Scale (VAS) was used to define endometriosis-associated pain,19 nominally chronic pelvic pain, dysmenorrhea and dyspareunia.
The Short Form-36 (SF-36) validated questionnaire was used to assess QoL.20 Sexual behavior was assessed using the self-administered Female Sexual Function Index (FSFI) validated in the Italian gynecological population.21 An FSFI cut-off of ≤26.55 is usually accepted for diagnosis of sexual dysfunction in women within a wide age range. Moreover, for diagnosis of sexual dysfunction an essential element is the requirement that the condition causes significant personal distress for the woman. Therefore, the Female Sexual Distress Scale (FSDS) was used.22 The FSDS consists of 12 items, with a maximum score of 48. An FSDS score of ≥15 corresponds to clinically significant distress. We considered women with an FSFI score of ≤26.55 to be affected by sexual dysfunction if they also had an FSDS score of 15 or greater.
The study included five follow-ups at 3, 6, 12, 18 and 24 months. All questionnaires were administered to both the groups at the baseline evaluation, and at each follow-up. Moreover, each woman received a diary to record daily sexual events, satisfaction rate, as well as adverse events during treatment.
Statistical analysis
ANOVA was used to compare the demographic and clinical data between the two groups. Paired Student’s t-test was used to compare the values obtained at baseline with those of follow-ups from the VAS, SF-36 domains and FSDS. For comparisons of the values obtained from the FSFI items between baseline and the follow-ups, the nonparametric Wilcoxon rank-sum test with z values was used. Scores are presented as mean ± SD. The result was statistically significant when p<0.05. Statistical analysis was carried out using the Primer of Biostatistics statistical computer package (Glantz SA, New York, USA: McGraw-Hill, Inc.1997).
Results
Table 1 shows the demographic characteristics of the study group and the control group at baseline. At the 3rd and the 6th month follow-ups, 3 (5.6%) and 2 (3.7%) women of study group, respectively, discontinued treatment due to spotting. Those patients were prescribed combined oral contraceptive treatment in a continuous regimen. Moreover, at the 12th, and 18th month follow-ups, 2 (3.7%) and 4 (7.4%) women, respectively, discontinued DNG to plan a pregnancy. None of the patients from the study group underwent surgical treatment. Therefore, 43 (79.6%) women completed the study. Moreover, women reported mild adverse events at the 3rd month follow-up, which did not provoke discontinuation, namely spotting (9=16.6%), nausea (7=12.9%) or breast tenderness (8=14.3%). Finally, at the 3rd and the 6th month follow-ups, 10 (20.4%) and 39 (79.6%) women underwent amenorrhea, respectively. Amenorrhea rate was 88.3% at the 24th month follow-up. Eight women (21.1%) of the control group decided to undergo surgical treatment and 30 (78.9%) chose to continue using their previous on-demand NSAIDs. They reported mainly nausea (23=76.5%) during the usage of on-demand NSAIDs. Finally, 5 women (16.6%) chose to adopt a combined oral contraceptive during the period between the 6th and 18th month of the study, and 3 (10%) dropped out at the 24th month. Consequently, 22 (73.3%) women completed the study.
Table 1.
Demographic characteristic
| Treated group (n=54) | Control group (n=38) | p-value | |
|---|---|---|---|
| Age range (years) | 18–36 | 18–34 | 1 |
| Mean Age | 29.4±9.2 | 27.4±8.3 | 0.2 |
| Age at menarche | 12.4±2.4 | 12.6±3.1 | 0.8 |
| BMI kg/m2 | 23.2±4.8 | 24.1±3.5 | 0.7 |
| Menstrual cycle length (days) | 25–31 | 26–33 | 0.1 |
| Duration of menses (days) | 4.1±2.2 | 3.4±1.8 | 0.1 |
| Chronic Pelvic Pain | 54 (100%) | 48 (100%) | 1 |
| Dysmenorrhea | 40 (78.4%) | 29 (76.3%) | 0.5 |
| Dyspareunia | 35 (68.6%) | 27 (71.1%) | 0.5 |
| Parity | |||
| Nulliparous | 40 (78.4%) | 29 (76.3%) | 0.5 |
| One or more children | 11 (21.6%) | 9 (23.7%) | 0.6 |
| Systolic blood pressure (mmHg) | 107.5±10.5 | 112.4±9.7 | 0.02 |
| Diastolic blood pressure (mmHg) | 68.4±6.8 | 66.4±9.5 | 0.2 |
| Heart rate (per min) | 69.5±8.5 | 65.6±7.8 | 0.03 |
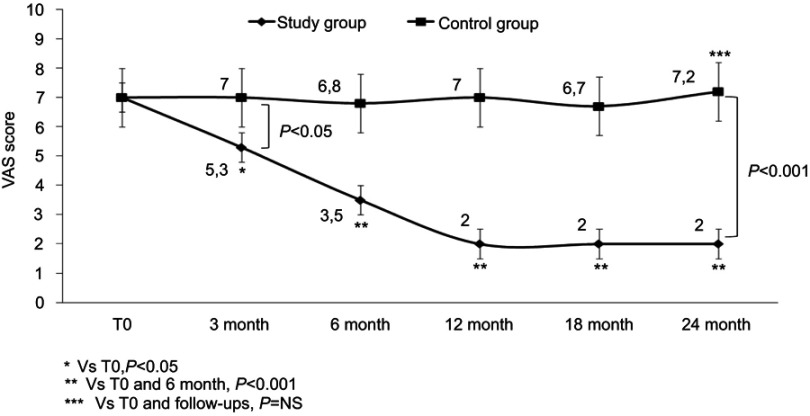
Figure 1 refers to the intra- and inter-group comparison of pelvic pain by VAS; the intra-group analysis showed an improvement of the VAS score at the 3rd month (p<0.05) that became even more evident from the 6th to 24th month follow-ups (p<0.001) of DNG usage. No change was observed in the control group from baseline to the 24th month follow-up (p=NS). The inter-group comparison between baseline values showed no differences (p=NS). On the contrary, the comparison was statistically significant at the 3rd month (p<0.05) and from the 6th to 24th month follow-ups (p<0.001).
Figure 1.
Visual Analog Scale (VAS) score of women affected by endometriosis-associated chronic pelvic pain during treatment with Dienogest 2 mg/die.
Abbreviation: NS, not significant.
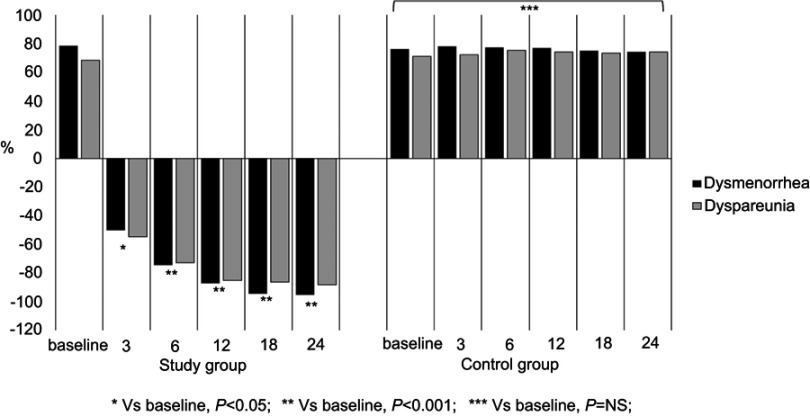
Figure 2 shows the improvement of dysmenorrhea and dyspareunia of the study and control groups. Women on DNG had a reduction of dysmenorrhea of 50.3, 74.5, 87.2, 94.6 and 95.5% at the 3, 6, 12, 18 and 24-month follow-ups compared to baseline, respectively. A similar trend was observed for dyspareunia; in fact, it improved gradually from baseline with a reduction of 74.4% at the 24-month follow-up (p<0.001). Finally, the control group did not show any change at each follow-up compared to the baseline value (p=NS).
Figure 2.
Dysmenorrhea and dyspareunia of women with endometriosis-associated pelvic pain before and during treatment with Dienogest 2 mg/die (study group) and women using on-demand non-steroidal anti-inflammatory drugs (control group).
Abbreviation: NS, not significant.
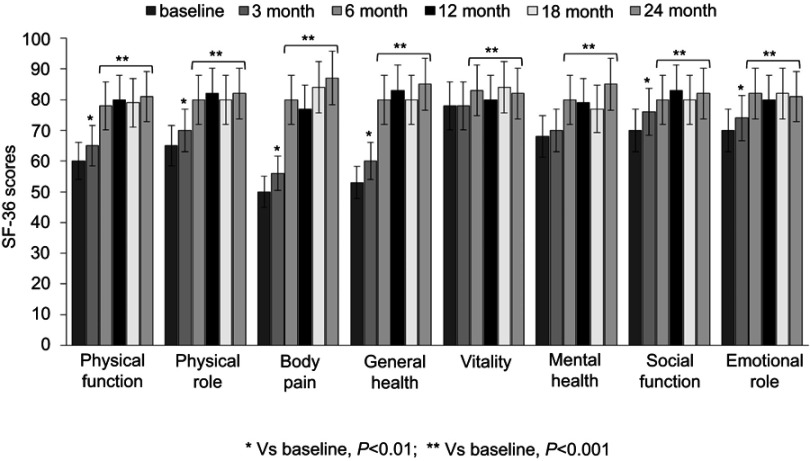
Figure 3 shows the changes of QoL of the study group. At the 3rd month follow-up, women reported QoL improvement in physical function, physical role, body pain, general health, social function and emotional role categories (p<0.01); from the 6th to the 24th month follow-ups, women reported improvement in all categories compared the baseline scores (p<0.001). On the contrary, the women of the control group did not have any QoL change during the study period (p=NS).
Figure 3.
Quality of life of women with endometriosis-associated pelvic pain before and during treatment with Dienogest 2 mg/die.
Table 2 shows the FSFI and FSDS scores obtained at baseline and during DNG intake. At the 3rd month follow-up, women had no benefit from treatment (p=NS). From the 6th to the 24th month follow-ups, the FSFI score rose (p<0.001) and the FSDS score decreased (p<0.001), meaning an improvement of the quality of sexual life. From the intergroup statistical comparison at baseline and at the 3rd month follow-up, no difference was observed between the study group and the control group (p= NS), except for dyspareunia (p<0.002). After this, the intergroup difference was statistically significant; in fact, the study group showed an improvement in all FSFI items (p<0.02), in FSFI total score (p<0.001) and in FSDS score (p<0.001), with respect to the control group scores.
Table 2.
Female Sexual Function Index (FSFI) and Female Sexual Distress Scale (FSDS) scores of women affected by endometriosis-associated pelvic pain during treatment with Dienogest 2 mg/die: long term management
| FSFI domains | Baseline (n=54) | 3 months (n=51) | 6 months (n=49) | 12 months (n=47) | 18 months (n=43) | 24 months (n=43) |
|---|---|---|---|---|---|---|
| Desire | 3.4±1.3 | 3.1±1.2* | 3.8±1.1* | 4.1±1.2** | 4.4±1.1** | 4.5±1.2** |
| Arousal | 4.1±1.1 | 4.1±1.2* | 4.6±1.2** | 4.9±1.2** | 4.9±1.6** | 5.1±1.2** |
| Lubrication | 4.1±1.2 | 4.2±1.1* | 4.5±1.3* | 4.6±1.3** | 4.9±1.3** | 4.7±1.3** |
| Orgasm | 3.9±1.1 | 4.1±1.3* | 4.8±1.2** | 5.1±1.3** | 5.1±1.2** | 5.2±1.3** |
| Satisfaction | 3.8±1.1 | 4.1±1.4* | 4.6±1.1** | 5.3±1.2** | 5.3±1.1** | 5.2±1.2** |
| Dyspareunia | 3.1±1.2 | 4.7±1.2** | 5.5±1.3** | 5.7±1.1** | 5.6±1.2** | 5.5±1.1** |
| FSFI score | 22.3±1.3 | 23.9±1.3* | 27.8±1.3** | 29.7±1.4** | 30.2±1.3** | 30.3±1.7** |
| FSDS score | 18.4±1.3 | 17.5±1.8* | 11.3±1.4*** | 10.1±1.6*** | 10.3±1.7*** | 9.8±1.5*** |
Notes: Values are expressed as means ± SD. *Vs Baseline, p=NS. **Vs Baseline, p<0.001 (by non parametric Wilcoxon’ s rank sum test). ***Vs Baseline, p<0.001 (by Paired Student’s t -test).
Abbreviation: NS, not significant.
The monthly frequency of sexual activity increased in women on DNG, from 2.1 at baseline, to 5.4 at the end of study (p<0.001). Finally, women reported to be satisfied (16=37.2%) and very satisfied (27=62.8%), mainly for pain relief when taking DNG. On the contrary, the control group did not have any change (p=NS).
Discussion
The aim of the current study was to evaluate the efficacy of DNG for a 24-month long-term treatment. The design of the study was based on a critical observation of the survey length. In fact, efficacy studies usually are limited in time; they commonly end within 3 to 6 months. By adopting such a design, we often cannot know what long-term effects and benefits progestin can have and how many subjects discontinue it. This was a limitation of our previous study.18
Firstly, the study group experienced a further improvement in pain syndrome, namely chronic pelvic pain, dysmenorrhea and dyspareunia, recorded by VAS at the 12-month follow-up compared to the previous follow-ups (primary endpoint). A reduction of pelvic pain without a relevant increase of concomitant pain medication was achieved in women on DNG; this benefit was maintained until the end of the study. Moreover, the progressive reduction of the pain syndrome reported by women over the treatment period could have contributed to improve their QoL and their sexual life further (secondary endpoint). Assessment of the QoL is a crucial parameter to take into account before concluding on the efficacy of treatment. Our study showed an improvement in some categories of the SF-36 at the 3-month follow-up, mainly those related to physical aspects, but not to mental aspects. All categories improved from the 6th month to the end of the study. Usually the first 3 months of assumption of a drug are connoted by objective and subjective adjustments and adaptation to its effects. However, to confirm the trend, a more prolonged observation is often necessary. Even if receptor binding studies have shown that DNG has some anti-androgenic properties23 which could affect the libido of long term users, recent studies showed that the quality of sexual life, particularly, improve during 6 months of DNG treatment of women with endometriosis.24 We observed a concomitant and gradual improvement of sexual function and a reduction of sexual distress starting from the 6th month follow-up until the 24-month follow-up. The low antiandrogenic effect showed by DNG on sexual desire could be due to psychosexual well-being related to the decrease in pain. Not all the benefits obtained by women on DNG were observed in women using on-demand NSAIDs.
It is interesting to note that DNG 2 mg daily provides ovulation inhibition, but ovarian activity is not completely suppressed;25 thus it has not been approved as a contraceptive.26 Moreover, circulating estradiol levels during treatment with DNG 2 mg daily are similar to those in the early follicular phase of the menstrual cycle.27 The moderate suppression of estradiol with DNG may represent a potential advantage over other therapies, such as GnRH agonists, which require estrogen add-back if used for more than 6 months.28
Currently, DNG is also used with ethinyl estradiol in a combined 21/7 regimen pill, but this regimen can fail in controlling pelvic pain; therefore, a so-called long-cycle regimen was introduced. In fact, women on conventional COCs may still experience headaches, pelvic pain and mood changes during the hormone-free interval, mainly due to the raised estradiol levels and increasing number of follicles induced by the increasing follicle-stimulating hormone levels during the hormone-free interval.29 On the contrary, the effectiveness of combined estradiol valerate in a 26/2 four-phase formulation pill has been observed.30
Our study performed a clinical diagnosis of endometriosis-associated pelvic pain, but it is necessary to point out that the gold standard investigation to a definitive diagnosis of most forms of endometriosis is laparoscopy for women presenting symptoms suggestive of endometriosis. This could be a limit of our study. However, pain symptoms suggestive of the disorder can be treated without a definitive diagnosis using a hormonal drug to reduce menstrual flow.31,32
The multidisciplinary nature of chronic pelvic pain may cause confusion for a correct diagnosis and treatment. To avoid this, women affected by chronic pelvic pain but also by dysmenorrhea and dyspareunia were enrolled in our current study. Another characteristic of pelvic pain due to endometriosis is its beginning during adolescence; in fact, women usually report a longer time and worse experience while obtaining a diagnosis. Thus, treatment is often started several years after use of NSAIDs.33 The delay of an appropriate treatment negatively affects the QoL of woman, often not restricting the progression of endometriosis.34
DNG represents a promising medication for the long-term management of endometriosis. Probably, a longer period without pelvic pain could lead to a greater awareness of being able to live their sexuality without discomfort and improve their QoL.
Conclusion
The long-term follow-up investigation has produced some very interesting results, proving that DNG has a good tolerability (79.6% completed the 24 months study) and a positive influence on the natural history of the symptoms related to the disease, while NSAIDs can reduce the pain transitory, with no effects on QoL and sexual function.
The current study has some limitations: endometriosis was not confirmed by laparoscopic exploration and biopsy also because the goal was to investigate about medical therapy and it’s not encouraged by the guidelines to perform laparoscopy without treating the lesions during the same surgery.2 The lack of randomization and the small size of the sample are further limits which will be addressed in future studies. For these reasons, the results must be interpreted with caution but however the long follow up confirmed the positive effects of the drug on pain and showed that QoL and sexual function continue to improve even after 6 months and 12 months of therapy; furthermore, the improvements are stable until 24 months.
The current study contributes to enrich literature about the advantages of using DNG in a long term to treat endometriosis-related pelvic pain, improving also QoL and sexual function.
Acknowledgments
The authors wish to thank the Scientific Bureau of the University of Catania, Italy, for language support.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Rogers PA, D’Hooghe TM, Fazleabas A, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci. 2009;16(4):335–346. doi: 10.1177/1933719109339217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunselman GAJ, Vermeulen N, Becker C, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014;29(3):400–412. doi: 10.1093/humrep/det457 [DOI] [PubMed] [Google Scholar]
- 3.Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261–275. doi: 10.1038/nrendo.2013.255 [DOI] [PubMed] [Google Scholar]
- 4.Laganà AS, La Rosa VL, Rapisarda AMC, et al. Anxiety and depression in patients with endometriosis: impact and management challenges. Int J Womens Health. 2017;9:323–330. doi: 10.2147/IJWH.S119729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casper RF. Progestin-only pills may be a better first-line treatment for endometriosis than combined estrogen-progestin contraceptive pills. Fertil Steril. 2017;107(3):533–536. doi: 10.1016/j.fertnstert.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 6.Bedaiwy MA, Allaire C, Alfaraj S. Long-term medical management of endometriosis with dienogest and with a gonadotropin-releasing hormone agonist and add-back hormone therapy. Fertil Steril. 2017;107(3):537–548. doi: 10.1016/j.fertnstert.2016.12.024 [DOI] [PubMed] [Google Scholar]
- 7.Ferrero S, Evangelisti G, Barra F. Current and emerging treatment options for endometriosis. Expert Opin Pharmacother. 2018;19(10):1109–1125. doi: 10.1080/14656566.2018.1494154 [DOI] [PubMed] [Google Scholar]
- 8.Ferrero S, Remorgida V, Maganza C, et al. Aromatase and endometriosis: estrogens play a role. Ann N Y Acad Sci. 2014;1317:17–23. doi: 10.1111/nyas.12411 [DOI] [PubMed] [Google Scholar]
- 9.Walch K, Unfried G, Huber J, et al. Implanon versus medroxyprogesterone acetate: effects on pain scores in patients with symptomatic endometriosis–a pilot study. Contraception. 2009;79(1):29–34. doi: 10.1016/j.contraception.2008.07.017 [DOI] [PubMed] [Google Scholar]
- 10.Yucel N, Baskent E, KaramustafaogluBalci B, Goynumer G. The levonorgestrel-releasing intrauterine system is associated with a reduction in dysmenorrhoea and dyspareunia, a decrease in CA 125 levels, and an increase in quality of life in women with suspected endometriosis. Aust N Z J Obstet Gynaecol. 2018;58(5):560–563. doi: 10.1111/ajo.12773 [DOI] [PubMed] [Google Scholar]
- 11.Caruso S, Cianci S, Vitale SG, Fava V, Cutello S, Cianci A. Sexual function and quality of life of women adopting the levonorgestrel-releasing intrauterine system (LNG-IUS 13.5 mg) after abortion for unintended pregnancy. Eur J Contracept Reprod Health Care. 2018;23(1):24–31. doi: 10.1080/13625187.2018.1433824 [DOI] [PubMed] [Google Scholar]
- 12.Bishop LA. Management of chronic pelvic pain. Clin Obstet Gynecol. 2017;60(3):524–530. doi: 10.1097/GRF.0000000000000299 [DOI] [PubMed] [Google Scholar]
- 13.Muzii L, Di Tucci C, Achilli C, et al. Continuous versus cyclic oral contraceptives after laparoscopic excision of ovarian endometriomas: a systematic review and metaanalysis. Am J Obstet Gynecol. 2016;214(2):203–211. doi: 10.1016/j.ajog.2015.08.074 [DOI] [PubMed] [Google Scholar]
- 14.Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev. 2015;30(7):CD001751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harada T, Taniguchi F. Dienogest: a new therapeutic agent for the treatment of endometriosis. Womens Health (Lond Engl). 2010;6(1):27–35. doi: 10.2217/WHE.09.72 [DOI] [PubMed] [Google Scholar]
- 16.Okada H, Nakajima T, Yoshimura T, Yasuda K, Kanzaki H. The inhibitory effect of dienogest, a synthetic steroid, on the growth of human endometrial stromal cells in vitro. Mol Hum Reprod. 2001;7(4):341–347. doi: 10.1093/molehr/7.4.341 [DOI] [PubMed] [Google Scholar]
- 17.Nakamura M, Katsuki Y, Shibutani Y, Oikawa T. Dienogest, a synthetic steroid, suppresses both embryonic and tumor cell-induced angiogenesis. Eur J Pharmacol. 1999;386(1):33–40. doi: 10.1016/S0014-2999(99)00765-7 [DOI] [PubMed] [Google Scholar]
- 18.Caruso S, Iraci M, Cianci S, Casella E, Fava V, Cianci A. Quality of life and sexual function of women affected by endometriosis‑associated pelvic pain when treated with dienogest. J Endocrinol Invest. 2015;38(11):1211–1218. doi: 10.1007/s40618-015-0383-7 [DOI] [PubMed] [Google Scholar]
- 19.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38(6):633–638. doi: 10.1067/mem.2001.118863 [DOI] [PubMed] [Google Scholar]
- 20.Bech P, Brazier J, Bullinger M, et al. The factor structure of the SF-36 health survey in 10 countries: results from the International Quality of Life Assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):1159–1165. doi: 10.1016/S0895-4356(98)00107-3 [DOI] [PubMed] [Google Scholar]
- 21.Nappi RE, Albani F, Vaccaro P, et al. Use of the Italian translation of the Female Sexual Function Index (FSFI) in routine gynecological practice. Gynecol Endocrinol. 2008;24(4):214–219. doi: 10.1080/09513590801925596 [DOI] [PubMed] [Google Scholar]
- 22.Derogatis LR, Rosen R, Leiblum S, Burnett A, Heiman J. The Female Sexual Distress Scale (FSDS): initial validation of a standardized scale for assessment of sexually related personal in distress women. J Sex Marital Ther. 2002;28(4):317–330. doi: 10.1080/00926230290001448 [DOI] [PubMed] [Google Scholar]
- 23.Sasagawa S, Shimizu Y, Kami H, et al. Dienogest is a selective progesterone agonist in transactivation analysis with potent endometrial activity due to this efficient pharmacokinetic profile. Steroids. 2008;73(2):222–231. doi: 10.1016/j.steroids.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 24.Morotti M, Sozzi F, Remorgida V, Venturini PL, Ferrero S. Dienogest in women with persistent endometriosis-related pelvic pain during norethisterone acetate treatment. Eur J Obstet Gynecol Reprod Biol. 2014;183:188–192. doi: 10.1016/j.ejogrb.2014.10.036 [DOI] [PubMed] [Google Scholar]
- 25.Klipping C, Duijkers I, Remmers A, et al. Ovulation-inhibiting effects of dienogest in a randomized, dose-controlled pharmacodynamic trial of healthy women. J Clin Pharmacol. 2012;52(11):1704–1713. doi: 10.1177/0091270011423664 [DOI] [PubMed] [Google Scholar]
- 26.Sitruk-Ware R, Nath A. The use of newer progestins for contraception. Contraception. 2010;82(5):410–417. doi: 10.1016/j.contraception.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 27.Foster RH, Wild MI. Dienogest. Drugs. 1998;56(5):825–833. doi: 10.2165/00003495-199856050-00007 [DOI] [PubMed] [Google Scholar]
- 28.Rafique S, Decherney AH. Medical management of endometriosis. Clin Obstet Gynecol. 2017;60(3):485–496. doi: 10.1097/GRF.0000000000000292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caruso S, Iraci M, Cianci S, Fava V, Casella E, Cianci A. Comparative, open-label prospective study on the quality of life and sexual function of women affected by endometriosis-associated pelvic pain on 2 mg dienogest/30 µg ethinyl estradiol continuous or 21/7 regimen oral contraceptive. J Endocrinol Invest. 2016;39(8):923–931. doi: 10.1007/s40618-016-0460-6 [DOI] [PubMed] [Google Scholar]
- 30.Grandi G, Xholli A, Napolitano A, Palma F, Cagnacci A. Pelvic pain and quality of life of women with endometriosis during quadriphasic estradiol valerate/dienogest oral contraceptive: a patient-preference prospective 24-week pilot study. Reprod Sci. 2015;22(5):626–632. doi: 10.1177/1933719114556488 [DOI] [PubMed] [Google Scholar]
- 31.Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20(10):2698–2704. doi: 10.1093/humrep/dei135 [DOI] [PubMed] [Google Scholar]
- 32.Vercellini P, Frattaruolo MP, Somigliana E, et al. Surgical versus low-dose progestin treatment for endometriosis-associated severe deep dyspareunia II: effect on sexual functioning, psychological status and health-related quality of life. Hum Reprod. 2013;28(5):1221–1230. doi: 10.1093/humrep/det071 [DOI] [PubMed] [Google Scholar]
- 33.The Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion. Fertil Steril. 2014;101(4):927–935. doi: 10.1016/j.fertnstert.2014.02.012 [DOI] [PubMed] [Google Scholar]
- 34.Márki G, Bokor A, Rigó J, Rigó A. Physical pain and emotion regulation as the main predictive factors of health-related quality of life in women living with endometriosis. Hum Reprod. 2017;32(7):1432–1438. doi: 10.1093/humrep/dex091 [DOI] [PubMed] [Google Scholar]