Abstract
Background:
Ozanimod, an oral immunomodulator, selectively targets sphingosine 1-phosphate receptors 1 and 5.
Objective:
Evaluate efficacy, safety, and tolerability of ozanimod in relapsing multiple sclerosis.
Methods:
In the RADIANCE Part A phase II study (NCT01628393), participants with relapsing multiple sclerosis were randomized (1:1:1) to once-daily ozanimod hydrochloride (0.5 or 1 mg) or placebo. After 24 weeks, participants could enter a 2-year, dose-blinded extension. Ozanimod-treated participants continued their assigned dose; placebo participants were re-randomized (1:1) to ozanimod hydrochloride 0.5 or 1 mg (equivalent to ozanimod 0.46 and 0.92 mg).
Results:
A total of 223 (89.6%) of the 249 participants completed the blinded extension. At 2 years of the extension, the percentage of participants who were gadolinium-enhancing lesion-free ranged from 86.5% to 94.6%. Unadjusted annualized relapse rate during the blinded extension (week 24—end of treatment) was 0.32 for ozanimod hydrochloride 0.5 mg → ozanimod hydrochloride 0.5 mg, 0.18 for ozanimod hydrochloride 1 mg → ozanimod hydrochloride 1 mg, 0.30 for placebo → ozanimod hydrochloride 0.5 mg, and 0.18 for placebo → ozanimod hydrochloride 1 mg. No second-degree or higher atrioventricular block or serious opportunistic infection was reported.
Conclusion:
Ozanimod demonstrated sustained efficacy in participants continuing treatment up to 2 years and reached similar efficacy in participants who switched from placebo; no unexpected safety signals emerged.
Keywords: Clinical trial, disease-modifying therapies, MRI, relapsing/remitting, T2 lesions, multiple sclerosis
Introduction
Multiple sclerosis (MS) is a complex inflammatory disease in which autoreactive lymphocytes infiltrate the central nervous system (CNS). Sphingosine 1-phosphate (S1P) is a phospholipid involved in lymphocyte migration and other physiological processes. The initial S1P receptor modulator approved for treating relapsing multiple sclerosis (RMS), fingolimod targets four of the five S1P receptors: S1P1, S1P3, S1P4, and S1P5.1,2 Functional antagonism of S1P1 prevents the release of immune cells from lymph nodes, while S1P5 modulation may be neuroprotective.3–5
Ozanimod is a once-daily, oral immunomodulator that selectively targets S1P1 and S1P5. In the placebo-controlled, phase II portion (Part A) of RADIANCE (NCT01628393), ozanimod hydrochloride (HCl) 0.5 and 1 mg were associated with significant reductions in mean cumulative number of gadolinium-enhancing lesions and new/enlarging T2-hyperintense lesions over weeks 12–24 relative to placebo, as well as numerical, dose-dependent decreases in annualized relapse rate (ARR) in participants with RMS.6 No serious cardiac events, serious infections, or macular edema were reported. We report results for an additional 2 years of participation in the blinded extension of RADIANCE Part A.
Methods
Study design and participants
The design of RADIANCE Part A was previously described.6 Briefly, RADIANCE Part A was a multicenter, randomized, double-blind, placebo-controlled, phase II study of participants with RMS diagnosed per the 2010 McDonald criteria.7 Study participants were aged 18–55 years, with an Expanded Disability Status Scale (EDSS) score 0–5.0 and ⩾1 relapse in the 12 months prior to enrollment or ⩾1 relapse in the prior 24 months plus ⩾1 gadolinium-enhancing magnetic resonance imaging (MRI) lesion in the previous 12 months. Those with progressive MS or disease duration >15 years and EDSS score ⩽2.0 were excluded.
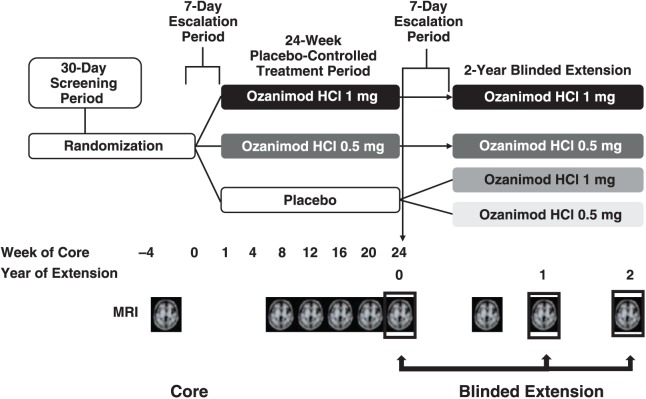
Eligible participants were randomized (1:1:1) to once-daily ozanimod HCl 0.5 mg (equivalent to ozanimod 0.46 mg), ozanimod HCl 1 mg (equivalent to ozanimod 0.92 mg), or placebo for 24 weeks. At week 24, study participants could enter a 2-year, dose-blinded extension in which participants originally randomized to ozanimod HCl continued their assigned dose (ozanimod HCl 0.5 mg → ozanimod HCl 0.5 mg and ozanimod HCl 1 mg → ozanimod HCl 1 mg groups), and those originally administered placebo were re-randomized (1:1) to ozanimod HCl 0.5 mg (placebo → ozanimod HCl 0.5 mg group) or 1 mg (placebo → ozanimod HCl 1 mg group), as shown in Figure 1. Randomization was stratified by country and performed centrally through an interactive voice response system using a computer-generated sequence programmed by an independent, unmasked, statistical team at the contract research organization (Pharmaceutical Product Development). During the extension, the sponsor and contract research organization were unblinded to treatment assignment, while investigators and participants remained blinded. A dual assessor approach, with separate treating and EDSS-examining investigators, was used to reduce potential unblinding. A core-imaging facility (NeuroRx Research, Montreal, Canada), blinded to treatment and other outcomes, performed MRI measurements.
Figure 1.
RADIANCE Part A design.
All participants, including those originally randomized to ozanimod HCl during the placebo-controlled period, underwent dose escalation with ozanimod HCl at week 24 (baseline for the blinded extension) over 7 days (0.25 mg on days 1–4, 0.5 mg on days 5–7, and then assigned dose starting on day 8) at the beginning of the blinded extension to maintain blinding.
Standard protocol approvals, registrations, and participant consents
The RADIANCE Part A extension was approved by the institutional review board/ethics committee at each participating site. The study protocol conformed to Good Clinical Practice guidelines and the principles outlined in the Declaration of Helsinki. All participants provided written informed consent. The study is registered at ClinicalTrials.gov (NCT01628393).
Assessments
During the blinded extension, participants were examined every 12 weeks. MRI was performed at entry to and at 6 months, 1 year, and 2 years of the blinded extension. A blinded treating physician supervised clinical management of the participant, including treatment-emergent adverse events (TEAEs). An independent, blinded EDSS evaluator performed the neurological examinations and completed the EDSS assessment. Efficacy endpoints included mean number of gadolinium-enhancing lesions, proportions of participants free of gadolinium-enhancing lesions, mean number of new or enlarging T2-hyperintense lesions on brain MRI, and unadjusted ARR.
Safety evaluations included the incidence and type of TEAEs, serious TEAEs, TEAEs leading to treatment discontinuation, pulmonary function tests, optical coherence tomography, and laboratory testing. TEAEs of special interest included infections, bradycardia, heart conduction abnormalities, abnormal pulmonary function tests, macular edema, hepatic effects, and malignancies.
At week 24 (baseline of the blinded extension), all participants were monitored for 6 hours after treatment (hourly vital signs and electrocardiograms before and 6 hours after treatment initiation in the blinded extension). Dermatologic exams were performed by the investigator at screening and every 6 months thereafter; any participant with suspicious findings was referred to a dermatologist.
Statistical analysis
Descriptive statistics were used to describe outcomes in the intent-to-treat population during the blinded extension. Demographic characteristics and safety data were pooled by ozanimod HCl-dose group (0.5 or 1 mg). Efficacy was examined in the dose subgroups as described above.
Results
Participant disposition
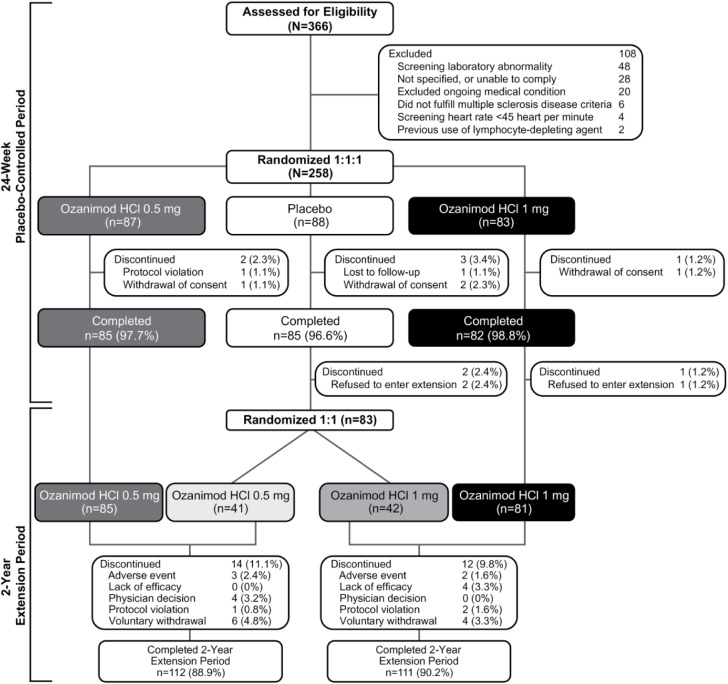
In total, 97.7% (252/258) of the participants completed the 24-week placebo-controlled period (ozanimod HCl 0.5 mg, n = 85; ozanimod HCl 1 mg, n = 82; placebo, n = 85). Three participants declined to enter the blinded extension. A total of 126 participants received ozanimod HCl 0.5 mg, and 123 received ozanimod HCl 1 mg during the blinded extension (Figure 2) between 1 May 2013 and 2 May 2016. Demographics and disease characteristics of participants in the blinded extension were similar to the baseline of the core period6 and across treatment groups (Table 1). Overall, 89.6% (223/249) of participants in RADIANCE Part A who continued to the blinded extension completed an additional 2 years, with 11.1% (14/126) and 9.8% (12/123) of those randomized to ozanimod HCl 0.5 and 1 mg, respectively, discontinuing study treatment prior to year 2. The reasons for treatment discontinuation are summarized in Figure 2.
Figure 2.
Disposition.
Table 1.
Demographics and disease characteristics of the blinded extension population at study entry.
| Placebo → ozanimod HCl 0.5 mg, (n = 41) | Ozanimod HCl 0.5 mg → ozanimod HCl 0.5 mg, (n = 85) | Placebo → ozanimod HCl 1 mg, (n = 42) | Ozanimod HCl 1 mg → ozanimod HCl 1 mg, (n = 81) | |
|---|---|---|---|---|
| Mean age (SD), years | 41 (8.01) | 38.1 (9.26) | 36.9 (8.69) | 38.5 (9.90) |
| Female, n (%) | 30 (73.2) | 58 (68.2) | 30 (71.4) | 57 (70.4) |
| White, n (%) | 41 (100) | 83 (97.6) | 42 (100) | 81 (100) |
| Eastern Europe, n (%) | 38 (92.7) | 78 (91.8) | 36 (85.7) | 74 (91.4) |
| Mean time since MS symptom onset (SD), years | 9.0 (7.05) | 6.0 (6.49) | 7.0 (7.05) | 6.2 (5.81) |
| Mean time since MS diagnosis (SD), years | 5.3 (5.19) | 2.8 (5.02) | 3.7 (5.11) | 3.6 (4.46) |
| Mean EDSS score (SD) | 2.7 (1.19) | 2.9 (1.29) | 2.9 (1.38) | 2.8 (1.18) |
| Mean relapses in the previous 12 months, n (SD) | 1.3 (0.68) | 1.4 (0.95) | 1.4 (0.62) | 1.3 (0.71) |
| Mean relapses in the previous 24 months, n (SD) | 2.0 (1.22) | 2.0 (1.69) | 1.7 (0.75) | 1.8 (1.05) |
| Mean gadolinium-enhancing lesions, n (SD) | 1.8 (3.73) | 0.9 (1.43) | 0.6 (1.38) | 1.4 (2.78) |
| Participants free of gadolinium-enhancing lesions, n (%) | 28 (68.3) | 51 (60.0) | 30 (71.4) | 51 (63.0) |
| Participants who received prior MS medication, n (%) | 18 (43.9) | 19 (22.4) | 12 (28.6) | 18 (22.2) |
EDSS: Expanded Disability Status Scale; MS: multiple sclerosis; SD: standard deviation.
Demographic and baseline characteristics at entry into the double-blind, placebo-controlled phase of RADIANCE Part A.
Efficacy
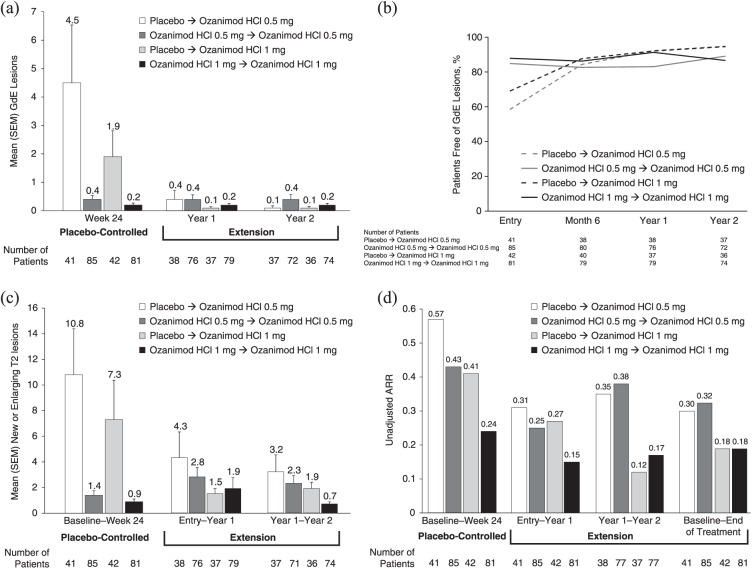
The mean number of gadolinium-enhancing lesions remained low in participants who continued ozanimod HCl throughout the placebo-controlled6 and blinded extension periods (Figure 3(a)). Among participants initially assigned to placebo who were re-randomized to ozanimod HCl, the mean number of gadolinium-enhancing lesions decreased between entry into the blinded extension at year 1 and remained low at year 2. At entry into the blinded extension, the proportion of participants free of gadolinium-enhancing lesions was 84.7% for ozanimod HCl 0.5 mg → ozanimod HCl 0.5 mg, 87.7% for ozanimod HCl 1 mg → ozanimod HCl 1 mg, 58.5% for placebo → ozanimod HCl 0.5 mg, and 69.0% for placebo → ozanimod HCl 1 mg; the proportions of participants free of gadolinium-enhancing lesions ranged from 91.1% to 92.9% at year 1 and from 86.5% to 94.6% at year 2 (Figure 3(b)). Ozanimod HCl showed a dose-dependent trend in reducing the mean number of new or enlarging T2 lesions (Figure 3(c)) from entry into the blinded extension to year 1 and from year 1 to year 2. The effects of ozanimod HCl on the unadjusted ARR seen during the placebo-controlled period were maintained during the blinded extension (Figure 3(d)) for participants continuing ozanimod HCl and decreased over the study period for those participants initially randomized to placebo (Figure 3(d)). Unadjusted ARR during the blinded extension was 0.32 for ozanimod HCl 0.5 mg → ozanimod HCl 0.5 mg, 0.18 for ozanimod HCl 1 mg → ozanimod HCl 1 mg, 0.30 for placebo → ozanimod HCl 0.5 mg, and 0.18 for placebo → ozanimod HCl 1 mg. Mean EDSS remained stable during the blinded extension period. Mean (standard deviation) change from baseline of the blinded extension at year 2 was 0.2 (0.85) for the ozanimod HCl 0.5 mg → ozanimod HCl 0.5 mg group, 0.1 (0.64) for the ozanimod HCl 1 mg → ozanimod HCl 1 mg group, 0.3 (0.76) for the placebo → ozanimod HCl 0.5 mg group, and 0.2 (0.67) for the placebo → ozanimod HCl 1 mg group.
Figure 3.
Efficacy outcomes: (a) mean number of gadolinium-enhancing lesions at year 1 and year 2 of the blinded extension, (b) proportions of participants free of gadolinium-enhancing lesions during the blinded extension, (c) mean number of new or enlarging T2 lesions over the entire study, and (d) unadjusted ARR over the entire study.
ARR: annualized relapse rate; GdE: gadolinium-enhancing; SEM: standard error of the mean.
Safety
Safety data are summarized in Table 2 and Supplementary Table 1. The most common TEAEs associated with ozanimod HCl were nasopharyngitis, upper respiratory tract infection, and increased alanine aminotransferase (ALT). A total of 4.9% (12/247) of participants had increases in ALT ⩾3-times the upper limit of normal (ULN; ozanimod HCl 0.5 mg, n = 4; ozanimod HCl 1 mg, n = 8). Of these participants, two (ozanimod HCl 0.5 mg, n = 1; ozanimod HCl 1 mg, n = 1) had concurrent aspartate aminotransferase (AST) elevations, while one participant, treated with ozanimod HCl 1 mg, had an isolated AST elevation. There were no reports of serious opportunistic infections during the blinded extension. No clinically significant abnormalities in pulmonary function tests and no cases of macular edema or malignancy were reported during the blinded extension. Four participants discontinued treatment due to a TEAE during the 2-year blinded extension (Table 2). These discontinuations were all attributable to increased transaminases and were protocol-specified (participants with confirmed ALT or AST levels >5-times the ULN were required to permanently discontinue study treatment). All four participants recovered after discontinuation of ozanimod HCl.
Table 2.
Safety summary.
| Core period and blinded
extension |
||
|---|---|---|
| Ozanimod HCl 0.5 mg, (n = 126) | Ozanimod HCl 1 mg, (n = 123) | |
| Participants with ⩾1 TEAE, n (%) | 99 (78.6) | 93 (75.6) |
| Participants with ⩾1 treatment-related TEAE, n (%) | 5 (4.0) | 4 (3.3) |
| Participants with ⩾1 serious TEAE, n (%) | 12 (9.5) | 9 (7.3) |
| Participants with ⩾1 TEAE leading to treatment discontinuation, n (%) | 3 (2.4) | 1 (0.8) |
| Treatment-related deaths, n (%) | 0 (0) | 0 (0) |
TEAE: treatment-emergent adverse event.
A total of 12 participants receiving ozanimod HCl 0.5 mg experienced ⩾1 serious TEAE, including acute myocardial infarction, (n = 1; 18 months after first dose in a participant who was 43 years old at randomization and had a medical history of lupus and hypertension) and hepatitis (n = 1; in a participant with a recent history of multiple bee stings and who was negative for viral hepatitis etiologies and anti-nuclear antibodies; Table 2; Supplementary Table 2). Nine participants receiving ozanimod HCl 1 mg reported a serious TEAE, including a case of moderate pancytopenia that resolved without interruption of treatment. No serious TEAE occurred in more than one participant, and none was considered related to ozanimod HCl.
The maximum mean decrease in heart rate from pre-dose baseline of the extension was 0.6 bpm, which was observed at 4 hours post-treatment on the first day of dose escalation at entry into the blinded extension in the placebo → ozanimod HCl 0.5 mg group; in participants continuing ozanimod HCl, mean heart rate did not decrease relative to baseline. One participant, randomized to placebo → ozanimod HCl 1 mg, experienced a decline in heart rate per vital sign measurement to below 45 bpm (specifically, 44 bpm), which was asymptomatic; this participant had a baseline pre-dose heart rate of 55 bpm. No participant who switched from placebo to ozanimod HCl had a decrease in heart rate of >20 bpm from pre-dose baseline during hours 1‒6 on the first day of the blinded extension. There were no reports of second-degree or higher atrioventricular block.
Hypertension was reported in 7.9% (10/126) of participants in the ozanimod HCl 0.5 mg group and 3.3% (5/123) of participants in the 1 mg group, with one case in the 0.5 mg group considered to be possibly related to study drug. There was one case of hypertension that was considered serious but unrelated to study drug in a participant (ozanimod HCl 0.5 mg group) with pre-existing hypertension who was hospitalized for further cardiac evaluation and medication adjustment. Herpes zoster was reported in five participants (ozanimod HCl 0.5 mg, n = 3; ozanimod HCl 1 mg, n = 2), although immunity was a requirement for enrollment. No case was serious and none led to permanent discontinuation of study drug. No seizures were reported during the study. No dermatologic cancers were observed.
During ozanimod exposure, four participants (all treated with ozanimod HCl 1 mg) had absolute lymphocyte counts <200 cells/µL, which were observed at weeks 12 and 48 (n = 1), 24 (n = 1), and 72 (n = 2) of the blinded extension (no participant had absolute lymphocyte counts <200 cells/µL during the core period of the study8). The absolute lymphocyte count reductions below 200 cells/µL were transient, with none associated with infection or leading to study discontinuation. Three participants, all treated with ozanimod HCl 0.5 mg, had absolute neutrophil counts <1000 cells/µL, one at baseline, one at week 48, and one at week 96 of the blinded extension.
Discussion
In the blinded extension of the phase II portion of RADIANCE, both doses of ozanimod HCl (0.5 and 1 mg) demonstrated continued efficacy over 2 years, as shown by low levels of MRI lesion activity and low unadjusted ARR, with apparent greater efficacy on both MRI and clinical disease measures for ozanimod HCl 1 mg versus ozanimod HCl 0.5 mg. In addition, the efficacy observed in participants who initially received placebo approximated that observed in participants who received ozanimod HCl continuously throughout the placebo-controlled portion of the study and the blinded extension. Consistent with the 24-week placebo-controlled treatment period,6 gadolinium-enhancing and new or enlarging T2 lesion numbers remained low in all four treatment groups during the 2-year blinded extension.
Safety plays a major role in treatment preference among individuals with MS,9 and adverse events (e.g. injection reactions and flu-like symptoms with injectable therapies and gastrointestinal side effects, headache, heart rate effects, and macular edema with oral therapies) are among the most common reasons for the discontinuation of MS treatments.10 The use of ozanimod HCl for over 2 years was well tolerated, with few participants discontinuing for side effects or safety reasons. TEAEs during the 2-year blinded extension were consistent with those seen during the placebo-controlled period, with no apparent increase over time or differences between ozanimod HCl 0.5 and 1 mg. In the blinded extension period, 4.9% of participants receiving ozanimod HCl experienced increases in ALT ⩾3-times the ULN, with the majority of ALT elevations occurring in participants who switched from placebo. Most cases of elevated liver enzymes were transient and did not require discontinuation of ozanimod HCl. Based on protocol requirements, four participants discontinued from the study with an ALT ⩾5-times ULN; all recovered after drug discontinuation.
Ozanimod was administered in a dose escalation regimen. In the RADIANCE Part A blinded extension, there were no reports of clinically significant cardiac conduction abnormalities associated with ozanimod HCl, including no second-degree or higher atrioventricular block, and no clinically meaningful bradycardia was observed, consistent with the results of the placebo-controlled period.6 It should be noted that individuals with certain clinically relevant cardiovascular conditions were excluded from the study,6 and <20% of participants had a history of cardiovascular disorders. Additional studies will help to further define the safety profile of ozanimod.
Results of extension studies are sometimes biased by participant attrition. However, this analysis benefited from high retention, with 88.9% of participants randomized to ozanimod HCl 0.5 mg and 90.2% of participants administered ozanimod HCl 1 mg completing 2 years of treatment. The participant population in this study was similar to that of other phase II trials of participants with MS administered other selective S1P receptor modulators.11 Limitations of these data include lack of a control arm during the blinded extension, relatively small sample size, and a predominantly white, Eastern European population. The phase III portion of RADIANCE (Part B, NCT02047734) is larger, comprising 1313 participants with RMS randomized (1:1:1) to ozanimod HCl 0.5 mg, ozanimod HCl 1 mg, or intramuscular interferon beta-1a for 24 months. In addition, SUNBEAM (NCT02294058), a similarly designed phase III study, enrolled 1346 participants with RMS. Those participating in SUNBEAM received ozanimod HCl 0.5 mg, ozanimod HCl 1 mg, or intramuscular interferon beta-1a for at least 12 months. Together, these two phase III studies will provide comprehensive data on the benefits and risks of this potential new treatment for RMS.
Supplemental Material
Supplemental material, MSJ789884_CONSORT_checklist for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal
Supplemental Material
Supplemental material, MSJ789884_data_supplement for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal
Supplemental Material
Supplemental material, MSJ789884_supplementary_appendix for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal
Acknowledgments
CodonMedical, an Ashfield Company, part of UDG Healthcare plc, provided editorial assistance for this manuscript, which was funded by Celgene Corporation.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J.A.C. received personal compensation for consulting for Adamas, Celgene Corporation, Novartis, and PendoPharm and as a co-editor of Multiple Sclerosis Journal – Experimental, Translational and Clinical. G.C. received compensation for consulting services and/or speaking activities from Almirall, Biogen, Celgene Corporation, EXCEMED Forward Pharma, Medday, Merck, Novartis, Roche, Sanofi, Sanofi Genzyme, and Teva. D.L.A. received personal fees for consulting from Acorda Therapeutics, Biogen, Genzyme, the Immune Tolerance Network, Novartis, and Sanofi-Aventis; grants from Biogen and Novartis; and holds an equity interest in NeuroRx Research. A.B.-O. received personal compensation for consulting from Biogen, Celgene Corporation, EMD Serono, Medimmune, Novartis, Roche, and Sanofi Genzyme. K.W.S. served as a consultant for Biogen Idec, Celgene Corporation, Genzyme, Merck, Novartis, Ono Pharma, Roche, Synthon, and Teva. L.S. served as a consultant for Abbvie, Atreca, Celgene Corporation, Coherus, EMD Serono, Novartis, Teva, and Tolerion; and received research support from Atara, Biogen, Celgene Corporation, and Coherus. E.K.H. received personal compensation for consulting and speaking for Actelion, Biogen, Celgene Corporation, Merck, Novartis, Sanofi, Roche, and Teva and was supported by Czech Ministry of Education, project PROGRES Q27/LF1. B.A.C.C. received personal compensation for consulting from Abbvie, Biogen, EMD Serono, GeNeuro, Novartis, and Sanofi Genzyme. X.M. received speaking honoraria and travel expenses for scientific meetings or participated in steering committees or in advisory boards for clinical trials with Almirall, Bayer, Schering Pharma, Biogen, Genentech, Genzyme, GSK, Merck Serono, MS International Federation, National Multiple Sclerosis Society, Novartis, Roche, Sanofi-Aventis, and Teva; for serving as an editor for Clinical Cases for MSJ. H.-P.H. received fees for consulting, serving on steering committees, and speaking from Bayer HealthCare, Biogen, GeNeuro, Genzyme, Merck, Medimmune, Novartis, Octapharma, Opexa, Roche, Sanofi, and Teva. V.H. is a current employee of Celgene Corporation and is a stockholder in Celgene Corporation. P.F. is a former employee of Celgene Corporation (at the time of the study and analysis) and is currently employed by Bioniz Therapeutics, Inc. B.E.S. is a current employee of Celgene Corporation and is also a stockholder in Celgene Corporation. L.K.’s institution (University Hospital Basel) has received in the last 3 years and used exclusively for research support: steering committee, advisory board, and consultancy fees (Actelion, Addex, Bayer HealthCare, Biogen Idec, Biotica, Celgene Corporation, Genzyme, Lilly, Merck, Mitsubishi, Novartis, Ono Pharma, Pfizer, Sanofi, Santhera, Siemens, Teva, UCB, and Xenoport); speaker fees (Bayer HealthCare, Biogen Idec, Merck, Novartis, Sanofi, and Teva); support for educational activities (Bayer HealthCare, Biogen, CSL Behring, Genzyme, Merck, Novartis, Sanofi, and Teva); license fees for Neurostatus products; and grants (Bayer HealthCare, Biogen Idec, European Union, Merck, Novartis, Roche Research Foundation, Swiss MS Society, and Swiss National Research Foundation).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was sponsored by Celgene Corporation.
Contributor Information
Jeffrey A Cohen, Mellen Center for MS Treatment and Research, Cleveland Clinic, Cleveland, OH, USA.
Giancarlo Comi, Department of Neurology, San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Italy.
Douglas L Arnold, NeuroRx Research and Montreal Neurological Institute, McGill University, Montreal, QC, Canada.
Amit Bar-Or, Center for Neuroinflammation and Experimental Therapeutics and Department of Neurology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA.
Krzysztof W Selmaj, Center for Neurology, Łódź, Poland.
Lawrence Steinman, Department of Neurology & Neurological Sciences, Beckman Center for Molecular Medicine, Stanford University Medical Center, Stanford, CA, USA.
Eva K Havrdová, Department of Neurology and Center for Clinical Neuroscience, First Faculty of Medicine, Charles University, Prague, Czech Republic.
Bruce AC Cree, UCSF Weill Institute for Neurosciences and Department of Neurology, University of California, San Francisco, San Francisco, CA, USA.
Xavier Montalbán, Division of Neurology and St. Michael’s Hospital, University of Toronto, Toronto, ON, Canada/Cemcat, Vall d’Hebron University Hospital and Universitat Autònoma de Barcelona, Barcelona, Spain.
Hans-Peter Hartung, Department of Neurology, Medical Faculty, Heinrich Heine University, Düsseldorf, Germany.
Vivian Huang, Biostatistics, Celgene Corporation, San Diego, CA, USA.
Paul Frohna, Clinical Development, Celgene Corporation, San Diego, CA, USA.
Brett E Skolnick, Clinical Development, Celgene Corporation, San Diego, CA, USA.
Ludwig Kappos, Neurologic Clinic and Polyclinic, University Hospital of Basel and University of Basel, Basel, Switzerland.
References
- 1. Brinkman V, Billich A, Baumruker T, et al. Fingolimod (FTY720): Discovery and development of an oral drug to treat multiple sclerosis. Nat Rev Drug Discov 2010; 9: 883–897. [DOI] [PubMed] [Google Scholar]
- 2. Novartis Pharmaceuticals Corporation. Fingolimod (GILENYA) prescribing information. East Hanover, NJ: Novartis Pharmaceuticals Corporation, 2016. [Google Scholar]
- 3. Choi JW, Gardell SE, Herr DR, et al. FTY720 (fingolimod) efficacy in an animal model of multiple sclerosis requires astrocyte sphingosine 1-phosphate receptor 1 (S1P1) modulation. Proc Natl Acad Sci U S A 2011; 108: 751–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miron VE, Jung CG, Kim HJ, et al. FTY720 modulates human oligodendrocyte progenitor process extension and survival. Ann Neurol 2008; 63: 61–71. [DOI] [PubMed] [Google Scholar]
- 5. Miron VE, Ludwin SK, Darlington PJ, et al. Fingolimod (FTY720) enhances remyelination following demyelination of organotypic cerebellar slices. Am J Pathol 2010; 176: 2682–2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cohen JA, Arnold DL, Comi G, et al. Safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ozanimod in relapsing multiple sclerosis (RADIANCE): A randomised, placebo-controlled, phase 2 trial. Lancet Neurol 2016; 15: 373–381. [DOI] [PubMed] [Google Scholar]
- 7. Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011; 69: 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sanna MG, Vincent KP, Repetto E, et al. Bitopic sphingosine 1-phosphate receptor 3 (S1P3) antagonist rescue from complete heart block: Pharmacological and genetic evidence for direct S1P3 regulation of mouse cardiac conduction. Mol Pharmacol 2016; 89: 176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arroyo R, Sempere A, Ruiz-Beato E, et al. Conjoint analysis to understand preferences of patients with multiple sclerosis for disease-modifying therapy attributes in Spain: A cross-sectional observational study. BMJ Open 2017; 7: e014433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Longbrake EE, Cross AH, Salter A. Efficacy and tolerability of oral versus injectable disease-modifying therapies for multiple sclerosis in clinical practice. Mult Scler J Exp Transl Clin 2016; 2: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Olsson T, Boster A, Fernandez O, et al. Oral ponesimod in relapsing-remitting multiple sclerosis: A randomised phase II trial. J Neurol Neurosurg Psychiatry 2014; 85: 1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, MSJ789884_CONSORT_checklist for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal
Supplemental material, MSJ789884_data_supplement for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal
Supplemental material, MSJ789884_supplementary_appendix for Efficacy and safety of ozanimod in multiple sclerosis: Dose-blinded extension of a randomized phase II study by Jeffrey A Cohen, Giancarlo Comi, Douglas L Arnold, Amit Bar-Or, Krzysztof W Selmaj, Lawrence Steinman, Eva K Havrdová, Bruce AC Cree, Xavier Montalbán, Hans-Peter Hartung, Vivian Huang, Paul Frohna, Brett E Skolnick and Ludwig Kappos in Multiple Sclerosis Journal