Abstract
Background and Objectives:
Skin cancer incidence rates are highest among U.S. older adults. However, little is known about sun protection behaviors and sunburn among adults aged 65 years and older.
Research Design and Methods:
We used data from the 2015 National Health Interview Survey to examine the association between sun protection behaviors (sun avoidance, wearing protective clothing, and sunscreen use) and likelihood of having experienced sunburn in the past year.
Results:
Just over one in ten older adults (13.2%) had experienced sunburn in the past year; sunburn prevalence was nearly twice as high (20.4%) among sun-sensitive older adults. Men, ages 65–69 years, non-Hispanic whites, and those with skin that burns or freckles after repeated sun exposure were more likely to have been sunburned in the past year compared with the respective comparison groups. The only sun protection behavior significantly associated with sunburn was sunscreen use. None of the sun protection behaviors were significantly associated with a decreased risk of sunburn.
Discussion and Implications:
The prevalence of sunburn among older adults suggests opportunities to reduce skin cancer risk within this demographic group by preventing overexposure to the sun. The lack of reduced sunburn risk among those who regularly used sun protection may be related to inadequate or inconsistent use of sun protection or the way the sun protection behaviors were measured. Multi-sector approaches to facilitate sun-safety among older adults are warranted and could include targeted efforts focused on those most likely to get sunburned, including men and those with sun-sensitive skin.
Keywords: Skin cancer, Sun safety, Sunscreen, Shade, Health promotion
Incidence rates for both melanoma and nonmelanoma skin cancers have steadily increased in the United States in recent years (Holman, Freeman, & Shoemaker, 2018b; Paulson et al., 2018; Rogers, Weinstock, Feldman, & Coliron, 2015). An increase in both the number of people treated for skin cancer and the per-person costs of treatment has led to a substantial increase in average annual treatment costs for skin cancer, which are currently estimated to be about US$8.1 billion per year (Guy, Machlin, Ekwueme, & Yarbroff, 2015). Most skin cancers are diagnosed among non-Hispanic white adults aged 65 years and older (referred to as older adults throughout this paper), and the observed increases are driven largely by increases in incidence rates among this demographic group (Holman, Freeman, & Shoemaker, 2018b; Rogers et al., 2015). Overexposure to ultraviolet radiation (UVR) is a major risk factor for most skin cancers. UVR damage to the skin accumulates over one’s lifetime, and age-related changes in the skin may make older adults more susceptible to UVR-induced cellular DNA damage (Syrigos, Tzannou, Katirtzoglou, & Georgiou, 2005). Although overexposure to UVR does not always result in a sunburn, sunburn is a biological indicator of both the intensity of UVR expo-sure and the individual’s susceptibility to skin damage from UVR exposure.
Sunburn at any age is associated with an increased skin cancer risk (Dennis et al., 2008) and is often used as a proxy outcome measure in skin cancer prevention studies (U.S. Department of Health and Human Services, 2014). U.S. adults are living longer than ever, and individuals who reach the age of 65 can expect to have, on average, two more decades of life ahead of them (Arias, Heron, & Xu, 2017). Furthermore, older adults are at greater risk for skin cancer compared with younger age groups (Holman, Freeman, & Shoemaker, 2018b; Paulson et al., 2018; Rogers et al., 2015). Efforts to reduce overexposure to UVR and prevent sunburn among older adults would likely reduce the incidence of skin cancer in these later decades, potentially reducing skin cancer–related morbidity, mortality, and medical expenditures (Guy, Machlin, Ekwueme, & Yarbroff, 2015a; Guy et al., 2015b).
Guidance from major public health organizations encourages using a combination of clothing, a wide-brimmed hat, broad spectrum sunscreen with a sun protection factor (SPF) of at least 15 or 30, and shade to adequately protect skin from the sun when spending time outdoors (American Academy of Dermatology, 2018; American Cancer Society, 2017; U.S. Department of Health and Human Services, 2014). When used in combination, these sun protection measures can prevent sunburn and reduce future skin cancer risk. Efforts to promote sun safety, reduce UVR exposure, and prevent sunburn among older adults are important components of a comprehensive approach to skin cancer prevention at a population level. However, this demographic group has rarely been the focus of skin cancer prevention research, and sun-safety interventions targeting older adults would benefit from a better understanding of the factors that influence sunburn risk among this population.
Conceptual Framework
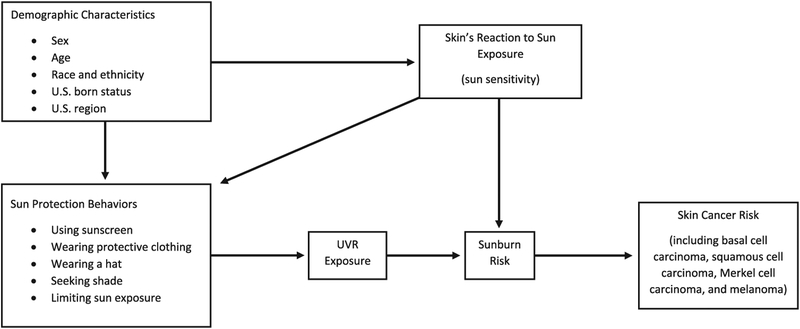
The conceptual framework guiding this study (Figure 1) is shaped by previous research regarding the relationship between sun protection behaviors and risk of sunburn and ultimately skin cancer among the general adult population. As depicted in the figure, previous research findings indicate that certain demographic characteristics may influence use of sun protection, which, in turn, influences UVR expo-sure and subsequent sunburn risk (Holman et al., 2018a; Holman et al., 2015). Sun sensitivity may also influence a person’s use of sun protection (independent of other demographic characteristics) as well as their sunburn risk (Holman et al., 2018a). As the number of sunburns a person experiences goes up, so does their risk for developing skin cancer (Dennis et al., 2008).
Figure 1.
Conceptual framework depicting the relationship between the study variables of interest. UVR = ultraviolet radiation.
Prior research findings lend insights into some of the nuances of the relationship between use of sun protection and risk for sunburn and subsequently skin cancer. For example, sunscreen trials have demonstrated that regular sunscreen use in adults may prevent melanoma (Green, Williams, Logan, & Strutton, 2011) and squamous cell carcinoma (van der Pols, Williams, Pandeya, Logan, & Green, 2006). However, behavioral research findings suggest a complex relationship in which adults who routinely use sunscreen when spending time outdoors are more likely to have been sunburned in the past year (Holman et al., 2018a). Some sunscreen users may use sunscreen on some but not all exposed skin (Holman et al., 2015), fail to apply sunscreen early enough prior to sun exposure, or fail to reapply it frequently enough (Wright, Wright, & Wagner, 2001). Additionally, some sunscreen users may use sun-screen in an attempt to get a suntan without burning, use sunscreen with a low SPF, and/or use sunscreen to stay in the sun longer than they would otherwise (Autier, Boniol, & Dore, 2007; Jansen et al., 2013; Wright et al., 2001). These potential patterns of use can result in more total UVR exposure than when sunscreen is used as directed on the product label. Findings from a recent study of patterns of sun-protective behaviors indicate that individuals who rely on sunscreen alone for sun protection are the most likely to get sunburned, whereas those engaging a combination of sun protection behaviors are the least likely to get sun-burned (Morris & Perna, 2018).
Behavioral research findings suggest that sun avoidance strategies such as seeking shade or not spending long periods of time in the sun are associated with a slight reduction in sunburn risk (Holman et al., 2018a). Shade does not provide complete UVR protection but can reduce total UVR exposure (Parisi & Turnbull, 2014). The amount of UVR protection conferred by shade depends on many factors, including the height, size, shape, and material of the shade as well as the reflectivity of surrounding surfaces (Parisi & Turnbull, 2014).
Although some behavioral research studies have failed to find an association between wearing protective clothing and sunburn prevalence (Holman et al., 2018a), findings from the previously mentioned study of patterns of sun-protective behaviors suggest that clothing can play an important role in sunburn prevention (Morris & Perna, 2018). Like shade, clothing typically does not confer complete UVR protection. The amount of protection depends primarily on the type of fabric and the percentage of total skin surface area that is covered (U.S. Department of Health and Human Services, 2014).
Age, race, ethnicity, foreign-born status, and U.S. region are demographic characteristics that have been associated with likelihood of experiencing sunburn in previous research among U.S. adults (Holman et al., 2018a). Adults aged 65 years and older are less likely to get sunburned compared with younger age groups. Non-Hispanic whites are more likely to experience sunburn compared with other racial/ethnic groups. Individuals who were born in the United States are more likely to experience sunburn compared with those who were born elsewhere. Those who live in the Midwest are more likely to experience sunburn compared with those living in other U.S. regions. Sex is another important demographic characteristic to consider. Although recent research does not indicate variation in sunburn by sex among U.S. adults, there is evidence to suggest that the types of sun protection used regularly tend to vary by sex (Holman et al., 2018a). Women are more likely to use sunscreen and stay in the shade compared with men, and men are more likely to wear protective clothing (Holman et al., 2018a).
Recent research has also highlighted the influence of a person’s sensitivity to sun exposure, as those with more sun-sensitive skin are more likely to experience sunburn, even when adjusting for race and ethnicity (Holman et al., 2018a). Researchers often measure this construct by asking about the skin’s reaction to sun exposure in two scenarios. The first scenario is one in which the person goes out in the sun for an hour without sun protection after several months of not being in the sun very much (short exposure). The second scenario is one in which the person goes out in the sun repeatedly, such as every day for 2 weeks, without sun protection (repeated exposure). Research findings indicate that sensitivity to repeated sun exposure is associated with likelihood of sunburn even when analyses are limited to adults classified as sun-sensitive based on the short exposure assessment (Holman et al., 2018a).
Hypotheses
For the current study, we used national surveillance data to examine the association between sun protection behaviors and having had at least one sunburn in the past 12 months among U.S. older adults. We hypothesized that after con-trolling for appropriate covariates, regular use of sun protection, including sun avoidance behaviors (staying in the shade and avoiding extended time outdoors), wearing protective clothing, and using sunscreen, would be associated with a decreased likelihood of having experienced sunburn.
Methods
We used data from the 2015 National Health Interview Survey (NHIS) to examine our hypotheses (National Center for Health Statistics, 2015). NHIS is an annual, cross-sectional household interview survey of a nationally representative sample of the U.S. noninstitutionalized civilian population that collects demographic and health-related information. Sampling and interviewing are continuous throughout each year. Interviews are conducted in person, with follow-up by telephone when needed. Information is collected about the household and each household member. A household may consist of more than one family. One adult aged 18 years or older in each family is randomly selected for additional detailed questions. More information about the sample design and data collection procedures is available online (National Center for Health Statistics, 2015).
In 2015, total of 33,672 sample adults were interviewed, with a final, unconditional response rate of 55.2% (National Center for Health Statistics, 2015). Our analyses included 7,765 respondents after excluding adults under the age of 65 years, those with a personal history of melanoma, and those with unknown or missing responses to questions about sun protection behaviors or sunburn. This study was exempt from review by the CDC Human Subject Institutional Review Board because we used existing publicly available deidentified data.
Measures
Sunburn was measured by a question asking respondents how many times they had a sunburn in the past 12 months. Sun protection behaviors were measured by a series of questions asking respondents how often they engage in certain behaviors when outside on a warm sunny day for more than 1 hr. The behaviors included staying in the shade; wearing a hat that shades the face, ears, and neck such as a hat with a wide brim all around; wearing a long-sleeved shirt, wearing long pants, or other clothing that reaches the ankles; and using sunscreen. Respondents who reported using sun-screen were also asked about the SPF of the sunscreen they use most often. Individuals who reported engaging in a given behavior “always” or “most of the time” were coded as regularly using that form of sun protection. Those who reported engaging in the behavior “sometimes,” “rarely,” or “never” were coded as not regularly using that form of sun protection. Some individuals responded to one or more of the sun protection questions by saying that they do not go in the sun for more than 1 hr. We coded this response as an additional sun protection behavior. These sun protection data were then recoded into three general categories of sun protection: sun avoidance (staying in the shade and/or not going in the sun for more than 1 hr), protective clothing (wearing a wide brimmed hat, long-sleeved shirt, and/or clothing to the ankles), and sunscreen with an SPF of at least 15. Those who reported not going in the sun were coded as “yes” for the sun avoidance composite variable and were coded as “no” for sunscreen use and protective clothing in the analyses unless they specifically reported using one of those protective strategies “always” or “most of the time.” We also created a separate variable to assess the total number of sun protection behaviors respondents used “always” or “most of the time.” Previous research findings indicate that survey questions about usual use of sun protection have high validity and agreement with more objective measures (Glanz et al., 2009; O’Riordan et al., 2009).
The other measures included in the analyses were sex, 5-year age groups, race, ethnicity, foreign-born status, U.S. region, and two measures of sun sensitivity. The first measure asked about 1 hr of unprotected sun exposure after not being in the sun very much for several months. Individuals who said they would “get a severe sunburn with blisters,” “have a moderate sunburn with peeling,” or “burn mildly with some or no darkening/tanning” were categorized as sun-sensitive. Those who said their skin would “turn darker without sunburn” or that “nothing would happen to [their] skin” were categorized as not sun-sensitive. The second sun-sensitivity question asked about repeated sun exposure over 2 weeks without sun protection. We dichotomized this variable as those who would burn repeatedly or freckle versus those who would develop a mild, moderate, or dark tan.
Analyses
A total of 7,765 older adults, including 3,204 men (41.3%) and 4,561 women (58.7%), were included in the analyses. Just under half (3,659; 47.8%) were classified as being sun-sensitive because their skin would burn after 1 hr of unprotected sun exposure (after not having been in the sun much for several months). We calculated weighted, unadjusted percentages to describe demographic characteristics and sun protection behaviors among U.S. older adults overall, and among older adult men, older adult women, and sun-sensitive older adults. We used multivariable logistic regression to calculate adjusted prevalence ratios for experiencing one or more sunburns in the past 12 months by sex, 5-year age groups, race and ethnicity, foreign-born status, U.S. region, sensitivity to repeated sun exposure, sun avoidance, use of protective clothing, and use of sunscreen (SPF 15+). Analyses were conducted overall and among sun-sensitive individuals only. We also repeated the regression analyses with the three sun protection category variables replaced with the single measure of number of sun protection behaviors regularly used. We used SAS-callable SUDAAN (Research Triangle Institute; Research Triangle Park, NC, Version 11.0) to calculate all weighted estimates and used the stratum and primary sampling unit variables provided with the NHIS data file to account for the complex survey design. We considered statistical tests with p values less than 0.05 statistically significant.
Results
Table 1 summarizes the demographic characteristics and sun protection behaviors of U.S. older adults, overall and among older adult men, older adult women, and sun-sensitive older adults in 2015. Nearly 80% of U.S. older adults were non-Hispanic white, and most (86.2%) were born in the United States. Just under 20% had skin that would burn repeatedly or freckle after repeated sun exposure, whereas more than half had skin that would develop a mild (29.0%), moderate (26.0%), or very dark (7.8%) tan after repeated sun exposure. Just under 20% did not directly answer the question about repeated sun exposure but rather stated that they do not go in the sun. Among sun-sensitive older adults, 29.2% had skin that would burn repeatedly or freckle after repeated sun exposure, and more than two-thirds would develop a mild (33.9%), moderate (26.7%), or very dark (5.2%) tan. Only 5.1% of sun-sensitive older adults responded to the question about their skin’s reaction to repeated sun exposure by saying that they do not go in the sun.
Table 1.
Weighted, Unadjusted Demographic Characteristics, Sun Protection Behaviors, and Sunburn Among U.S. Older Adults—National Health Interview Survey, 2015
| All older adults (n = 7,765) |
Older adult men (n = 3,204) |
Older adult women (n = 4,561) |
Sun-sensitive older adults* (n = 3,659) |
|
|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Age, years | ||||
| 65–69 | 33.3 (31.9, 34.7) | 35.2 (33.2, 37.3) | 31.7 (29.9, 33.6) | 36.5 (34.5, 38.5) |
| 70–74 | 25.8 (24.5, 27.1) | 27.1 (24.9, 29.3) | 24.7 (23.0, 26.5) | 27.1 (25.2, 29.2) |
| 75–79 | 17.3 (16.2, 18.5) | 16.4 (14.8, 18.1) | 18.0 (16.5, 19.6) | 16.5 (14.9, 18.2) |
| 80–84 | 12.3 (11.4, 13.3) | 12.0 (10.5, 13.5) | 12.6 11.4, 14.0) | 10.3 (9.2, 11.5) |
| 85+ | 11.4 (10.5, 12.3) | 9.4 (8.2, 10.7) | 13.0 (11.7, 14.4) | 9.7 (8.5, 10.9) |
| Race and ethnicity | ||||
| Non-Hispanic white | 78.1 (76.7, 79.3) | 78.9 (77.0, 80.6) | 77.4 (75.5, 79.1) | 90.3 (89.1, 91.4) |
| Non-Hispanic black | 8.9 (8.1, 9.8) | 8.1 (7.1, 9.3) | 9.5 (8.4, 10.7) | 2.3 (1.8, 2.9) |
| Hispanic | 8.1 (7.4, 9.0) | 7.9 (6.8, 9.2) | 8.3 (7.3, 9.5) | 5.0 (4.2, 5.9) |
| Other (non-Hispanic) | 4.9 (4.3, 5.6) | 5.1 (4.3, 6.1) | 4.8 (3.9, 5.7) | 2.5 (1.9, 3.2) |
| U.S. born | ||||
| Yes | 86.2 (85.0, 87.3) | 86.6 (84.8, 88.1) | 85.9 (842, 87.3) | 91.3 (90.0, 92.5) |
| No | 13.8 (12.7, 15.0) | 13.4 (11.9, 15.2) | 14.2 (12.7, 15.8) | 8.7 (7.6, 10.0) |
| U.S. Region | ||||
| Northeast | 19.1 (17.5, 20.7) | 19.8 (17.5, 22.2) | 18.5 (16.5, 20.7) | 19.4 (17.4, 21.5) |
| Midwest | 22.0 (22.0, 23.6) | 21.5 (19.1, 24.0) | 22.4 (20.7, 24.3) | 22.6 (20.7, 24.7) |
| South | 38.5 (36.6, 40.4) | 37.9 (35.2, 40.6) | 38.9 (36.6, 41.3) | 36.0 (33.4, 38.7) |
| West | 20.5 (19.2, 21.9) | 20.9 (18.9, 23.1) | 20.1 (18.3, 22.0) | 21.9 (20.2, 23.8) |
| Skin’s reaction after repeated sun exposure* | ||||
| Burn repeatedly or freckle | 18.6 (17.3, 19.9) | 15.1 (13.3, 17.1) | 21.3 (19.7, 23.1) | 29.2 (27.2, 31.4) |
| Mild tan | 29.0 (27.6, 30.4) | 30.4 (28.2, 32.6) | 27.9 (26.1, 29.9) | 33.9 (31.9, 36.0) |
| Moderate tan | 26.0 (24.6, 27.5) | 31.8 (29.5, 34.2) | 21.5 (19.9, 23.2) | 26.7 (24.7, 28.8) |
| Very dark tan | 7.8 (7.1, 8.6) | 10.0 (8.8, 11.3) | 6.1 (5.3, 7.1) | 5.2 (4.3, 6.2) |
| Do not go in the sun† | 18.6 (17.3, 20.0) | 12.8 (11.4, 14.3) | 23.2 (21.4, 25.1) | 5.1 (4.1, 6.2) |
| Regularly stays in the shade‡ | ||||
| Yes | 42.2 (40.7, 43.8) | 36.5 (34.1, 38.9) | 46.8 (44.8, 48.8) | 49.3 (43.8, 48.5) |
| No | 45.2 (43.6, 46.9) | 55.5 (52.7, 57.5) | 37.5 (35.6, 39.5) | 46.2 (43.8, 48.5) |
| Does not go out in the sun† | 12.5 (11.4, 13.7) | 8.6 (7.3, 9.9) | 15.6 (14.1, 17.4) | 4.6 (3.6, 5.7) |
| Regularly wears a wide-brimmed hat‡ | ||||
| Yes | 21.7 (20.4, 23.0) | 22.7 (20.7, 24.7) | 20.9 (19.4, 22.6) | 26.4 (24.4, 28.4) |
| No | 65.6 (64.0, 67.2) | 69.2 (67.0, 71.4) | 62.8 (60.7, 64.8) | 69.4 (67.2, 71.5) |
| Does not go out in the sun† | 12.7 (11.6, 13.9) | 8.1 (7.0, 9.4) | 16.3 (14.7, 8.1) | 4.3 (3.4, 5.3) |
| Regularly wears a long-sleeved shirt‡ | ||||
| Yes | 19.3 (18.2, 20.4) | 19.2 (17.4, 21.1) | 19.4 (17.9, 20.9) | 22.8 (21.0, 24.7) |
| No | 68.0 (66.5, 69.5) | 73.0 (70.9, 75.0) | 64.1 (61.9, 66.2) | 72.7 (70.7, 74.6) |
| Does not go out in the sun† | 12.7 (11.6, 13.9) | 7.9 (6.8, 9.1) | 16.6 (15.0, 18.3) | 4.6 (3.7, 5.7) |
| Regularly wears clothing to the ankles‡ | ||||
| Yes | 37.2 (35.6, 38.7) | 44.2 (41.8, 46.6) | 31.6 (29.8, 33.4) | 40.1 (37.9, 42.4) |
| No | 50.2 (48.5, 51.8) | 47.9 (45.5, 50.3) | 52.0 (49.9, 54.0) | 55.3 (53.0, 57.6) |
| Does not go out in the sun† | 12.7 (11.6, 13.9) | 7.9 (6.8, 9.2) | 16.5 (14.8, 18.2) | 4.6 (3.7, 5.7) |
| Regularly uses sunscreen (SPF 15+)‡ | ||||
| Yes | 26.5 (25.0, 28.0) | 19.4 (17.5, 21.6) | 32.1 (30.1, 34.1) | 38.1 (35.9, 40.3) |
| No | 60.6 (59.0, 62.3) | 72.1 (69.7, 74.4) | 51.6 (49.5, 53.6) | 57.2 (54.8, 59.5) |
| Does not go out in the sun† | 12.9 (11.8, 14.0) | 8.5 (7.3, 9.9) | 16.4 (14.9, 17.9) | 4.8 (3.9, 5.8) |
| Regularly uses sun avoidance§ | ||||
| Yes | 55.0 (53.4, 56.7) | 45.3 (42.8, 47.8) | 62.8 (60.8, 64.6) | 54.0 (51.7, 56.3) |
| No | 45.0 (43.4, 46.6) | 54.7 (52.2, 57.2) | 37.3 (35.4, 39.2) | 45.9 (43.7, 48.3) |
| Regularly wears protective clothing∥ | ||||
| Yes | 48.3 (46.7, 49.9) | 55.2 (52.7, 57.6) | 42.9 (40.9, 44.9) | 54.1 (51.8, 56.4) |
| No | 51.7 (50.1, 53.3) | 44.9 (42.5, 47.3) | 57.1 (55.1, 59.1) | 45.9 (43.6, 48.2) |
| Number of sun protection behaviors regularly used‡,¶ | ||||
| 0 | 17.9 (16.7, 19.2) | 20.6 (18.7, 22.6) | 15.8 (14.4, 17.4) | 14.9 (13.3, 16.7) |
| 1 | 26.9 (25.5, 28.4) | 30.4 (28.4, 32.6) | 24.1 (22.2, 26.1) | 29.5 (27.5, 31.6) |
| 2 | 20.1 (18.9, 21.4) | 21.0 (19.2, 22.9) | 19.4 (17.8, 21.2) | 22.5 (20.7, 24.4) |
| 3 | 11.9 (11.0, 12.9) | 11.5 (10.1, 12.9) | 12.2 (11.0, 13.6) | 15.3 (13.8, 17.0) |
| 4 | 8.6 (7.7, 9.6) | 7.0 (5.8, 8.4) | 9.9 (8.6, 11.4) | 10.2 (8.8, 11.7) |
| 5 | 14.6 (13.4, 15.8) | 9.6 (8.3, 11.1) | 18.5 (17.0, 20.1) | 7.6 (6.6, 8.8) |
| Sunburn in the past 12 months | ||||
| 0 | 86.8 (85.6, 88.0) | 85.1 (83.3, 86.7) | 88.2 (86.6, 89.6) | 79.6 (77.6, 81.4) |
| 1 or more | 13.2 (12.1, 14.3) | 14.9 (13.3, 16.7) | 11.8 (10.5, 13.4) | 20.4 (18.6, 22.4) |
| 1 | 7.4 (6.6, 8.3) | 8.7 (7.5, 10.1) | 6.3 (5.3, 7.6) | 11.5 (10.1, 13.1) |
| 2 | 3.7 (3.1, 4.3) | 3.9 (3.2, 4.9) | 3.5 (2.8, 4.3) | 5.8 (4.8, 7.0) |
| 3 or more | 2.1 (1.8, 2.6) | 2.3 (1.6, 3.1) | 2.0 (1.6, 2.6) | 3.1 (2.5, 3.8) |
Notes: SPF = sun protection factor. Percentages are weighted to the civilian, noninstitutionalized population.
Sun-sensitive individuals are those whose skin would burn after an hour of unprotected sun exposure after several months without much sun exposure. This measure differs from skin’s reaction to repeated sun exposure, and the two variables are independently associated with likelihood of sunburn.
Although not stated by the interviewer as a response option, some respondents answered the question about their skin’s reaction to the sun after repeated exposure and/or questions about sun protection behaviors by stating that they “do not go in the sun.”
Always or most of the time when outdoors on a warm sunny day for more than 1 hr.
Stays in the shade and/or does not go in the sun always or most of the time on warm sunny days.
Wears a wide-brimmed hat, long-sleeved shirt, and/or clothing to the ankles always or most of the time when outdoors on a warm sunny day for more than 1 hr. All others, including those who reported not going in the sun, were coded as “no.”
Includes shade, sunscreen, wide-brimmed hat, long-sleeved shirt, and other clothing to the ankles.
The most frequently used sun protection behaviors among U.S. older adults overall were staying in the shade (42.2%) and wearing long clothing to the ankles (37.2%). Among older men, staying in the shade (36.5%) and wearing clothing to the ankles (44.2%) were the most frequently used sun protection behaviors, followed by wearing a wide-brimmed hat (22.7%). Use of sunscreen (19.4%) and long-sleeved shirts (19.2%) were least prevalent among older men. Among older women, staying in the shade (46.8%) was the most frequently used sun protection behavior, followed by use of sunscreen (32.1%) and clothing to the ankles (31.6%). Wearing a wide-brimmed hat (20.9%) and wearing a long-sleeved shirt (19.4%) were the least prevalent sun protection behaviors among older women. Among sun-sensitive older adults, shade (49.3%) and clothing to the ankles (40.1%) were most prevalent, followed by sunscreen use (38.1%). Only 14.6% of older adults and 7.6% of sun-sensitive older adults regularly used all five sun protection behaviors (shade, sunscreen, wide-brimmed hat, long-sleeved shirt, and clothing to the ankles), whereas 17.9% of older adults and 14.9% of sun-sensitive older adults did not regularly use any of the five sun protection behaviors. Within the three sun protection categories (sun avoidance, protective clothing, and sunscreen), protective clothing was the most prevalent among older men (55.2%) and sun-sensitive older adults (54.1), and sun avoidance (62.8%) was the most prevalent among older women.
A total of 13.2% of U.S. older adults had experienced at least one sunburn in the past year, with 7.4% experiencing 1 sunburn, 3.7% experiencing 2 sunburns, and 2.1% experiencing 3 or more sunburns (Table 1). Among men, 14.9% had experienced sunburn, among women, 11.8% had experienced sunburn, and among sun-sensitive individuals, 20.4% had experienced sunburn.
Table 2 shows results from multivariable logistic regression analyses examining the likelihood of experiencing one or more sunburns in the past 12 months overall and among sun-sensitive individuals. Women were significantly less likely to have been sunburned compared with men (adjusted prevalence ratio [aPR] = 0.83, confidence interval [CI] = 0.71, 0.98). Likelihood of having been sunburned in the past year decreased with increasing age, and compared with the youngest age group (65–69 years old), all other age groups were significantly less likely to have been sunburned (aPRs = 0.38–0.73). Compared with non-Hispanic whites, non-Hispanic blacks (aPR = 0.51; CI = 0.36, 0.72) and non-Hispanics of other races (aPR = 0.42; CI = 0.22, 0.77) were significantly less likely to have been sunburned. Those whose skin burns repeatedly or freckles after repeated sun exposure were significantly more likely to have been sunburned (aPR = 1.39; CI=1.14, 1.70) compared with those whose skin would develop a mild tan. Those who do not go in the sun were less likely to have been sunburned (aPR = 0.60; CI = 0.42, 0.86) compared with those whose skin would develop a mild tan.
Table 2.
Multivariable Logistic Regression Predicting 1 or More Sunburns in the Past 12 Months Among All U.S. Older Adults and Among Sun-Sensitive Older Adults—National Health Interview Survey, 2015
| All older adults (n = 7,765) |
Sun-sensitive older adults* (n = 3,659) |
|
|---|---|---|
| aPR (95% CI) | aPR (95% CI) | |
| Sex | ||
| Male | ref | ref |
| Female | 0.83 (0.71, 0.98) | 0.81 (0.68, 0.96) |
| Age, years | ||
| 65–69 | ref | ref |
| 70–74 | 0.73 (0.60, 0.89) | 0.69 (0.56, 0.86) |
| 75–79 | 0.43 (0.33, 0.56) | 0.48 (0.36, 0.64) |
| 80–84 | 0.40 (0.30, 0.54) | 0.42 (0.30, 0.58) |
| 85+ | 0.38 (0.26, 0.55) | 0.36 (0.23, 0.55) |
| Race and ethnicity | ||
| Non-Hispanic white | ref | ref |
| Non-Hispanic black | 0.51 (0.36, 0.72) | 1.01 (0.60, 1.71) |
| Hispanic | 0.69 (0.47, 1.01) | 0.77 (0.48, 1.23) |
| Other (non-Hispanic) | 0.42 (0.22, 0.77) | 0.60 (0.29, 1.28) |
| U.S. born | ||
| Yes | ref | ref |
| No | 0.93 (0.68, 1.26) | 0.91 (0.61, 1.35) |
| U.S. region | ||
| Northeast | ref | ref |
| Midwest | 1.11 (0.86, 1.45) | 1.11 (0.83, 1.48) |
| South | 0.91 (0.71, 1.17) | 0.92 (0.71, 1.20) |
| West | 0.95 (0.73, 1.25) | 0.91 (0.69, 1.20) |
| Skin’s reaction after repeated sun exposure* | ||
| Burn repeatedly or freckle | 1.39 (1.14, 1.70) | 1.26 (1.02, 1.43) |
| Mild tan | ref | ref |
| Moderate tan | 1.13 (0.92, 1.40) | 1.13 (0.90, 1.42) |
| Very dark tan | 1.10 (0.81, 1.50) | 1.50 (1.05, 2.15) |
| Do not go in the sun† | 0.60 (0.42, 0.86) | 0.74 (0.37, 1.47) |
| Regularly uses sun avoidance‡ | ||
| Yes | 0.91 (0.76, 1.09) | 0.86 (0.71, 1.03) |
| No | ref | ref |
| Regularly wears protective clothing§ | ||
| Yes | 1.00 (0.84, 1.18) | 1.07 (0.90, 1.28) |
| No | ref | ref |
| Regularly uses sunscreen (SPF 15+)∥ | ||
| Yes | 1.27 (1.05, 1.52) | 1.08 (0.90, 1.31) |
| No | ref | ref |
Notes: aPR = adjusted prevalence ratio; CI = confidence interval; SPF = sun protection factor. Bolded aPR’s are statistically significant (p < 0.05).
Sun-sensitive individuals are those whose skin would burn after an hour of unprotected sun exposure. This measure differs from skin’s reaction to repeated sun exposure, and the two variables are independently associated with likelihood of sunburn.
Although not stated by the interviewer as a response option, some respondents answered the question about their skin’s reaction to the sun after repeated exposure by stating that they “do not go in the sun.”
Stays in the shade and/or does not go in the sun always or most of the time on warm sunny days.
Wears a wide-brimmed hat, long-sleeved shirt, and/or clothing to the ankles always or most of the time when outdoors on a warm sunny day for more than 1 hr. All others, including those who reported not going in the sun, were coded as “no.”
Uses sunscreen always or most of the time when outdoors on a warm sunny day for more than 1 hr. All others, including those who reported not going in the sun, were coded as “no.”
We found similar relationships between these individual characteristics and sunburn prevalence among sun-sensitive older adults with some exceptions. Among sun-sensitive individuals, we found no significant differences in sun-burn prevalence across racial/ethnic groups. Additionally, among sun-sensitive individuals, those who had skin that would develop a very dark tan after repeated sun exposure were significantly more likely to have been sunburned compared with those whose skin would develop a mild tan (aPR = 1.50; CI = 1.05, 2.15).
Contrary to our hypotheses, the only sun protection behavior for which we found a significant association with sunburn was sunscreen use. Among all older adults, those who regularly use sunscreen were more likely to have been sunburned in the past year compared with those who did not regularly use sunscreen (aPR = 1.27; CI = 1.05, 1.52). None of the sun protection behaviors were significantly associated with sunburn when we limited the analyses to sun-sensitive older adults. When we reran the regression models with a single measure of number of sun protection behaviors included in place of the three measures of sun protection categories, we found no significant association between sunburn and the number of sun protection behaviors used (data not shown).
Discussion and Implications
In this study, we used national surveillance data to examine the relationship between use of sun protection and likelihood of experiencing sunburn in the past year among U.S. older adults. Just over one in ten U.S. older adults had experienced sunburn in the past year, and the prevalence of sunburn was nearly twice as high among sun-sensitive older adults. Contrary to our hypothesis, we found no association between regular use of sun avoidance behaviors or regular use of protective clothing and likelihood of having experienced sunburn in the past year. We also found no association between the number of sun protection behaviors used and likelihood of sunburn. Similar to previous findings among all U.S. adults, the lack of a protective effect for sun protection behaviors may be related to multiple factors, including inadequate use of reported sun protection behaviors (Holman et al., 2018a). For example, some individuals may regularly wear a long-sleeved shirt or pants when outdoors in the sun but still have some unprotected skin exposed to the sun.
Also counter to our hypothesis, we found that those who regularly used sunscreen were more likely to have experienced sunburn in the past year. Some individuals who routinely use sunscreen may not apply it thickly enough or reapply it as recommended, may use a lower-than-recommended SPF, may fail to apply it early enough prior to sun exposure, or may intentionally use sunscreen to stay in the sun longer or to develop a suntan without burning (Autier et al., 2007; Jansen et al., 2013; Wright et al., 2001). Given the cross-sectional nature of the data, the temporal relationship between sunscreen use and the reported sunburns is unknown. As such, this finding may also reflect more frequent sunscreen use among those with a recent history of sunburn. The association between sunscreen use and sun-burn was not statistically significant when we limited the analyses to sun-sensitive individuals, which suggests that the finding may also be related to a higher use of sunscreen among those whose skin has a tendency to sunburn.
Implications for Research and Public Health Practice
Given the lack of reduced sunburn risk among those who regularly used sun protection and the limitations of the current data, additional research is warranted to examine the specific contexts in which sunburns typically occur. For example, additional research could examine which sun protection strategies (if any) are most frequently in use when sunburn occurs. This type of data might shed light on improper or ineffective use of sun protection. Furthermore, data on the types of activities and outdoor settings most frequently associated with sunburn occurrence could shape and inform intervention approaches. Such research would likely be most informative if it were stratified by age group and inclusive of older adults.
The prevalence of sunburn among older adults indicates a need for efforts to increase adequate use of sun protection among this demographic group to ensure that older adults experience the full protection of the protective measures used. To date, there has been a dearth of attention given to the topic of sun safety promotion for older adults, as demonstrated by the lack of studies focused on older adults described in the recent literature reviews conducted by the Community Preventive Services Task Force (The Community Guide, 2018). However, skin cancer risk is greatest for adults aged 65 years and older (Holman, Freeman, & Shoemaker, 2018b; Paulson et al., 2018; Rogers et al., 2015), and individuals who reach the age of 65 can expect to have, on average, two more decades of life ahead of them (Arias, Heron, & Xu, 2017). Efforts to reduce overexposure to UVR among older adults would likely reduce the incidence of skin cancer in these later decades, potentially reducing skin cancer–related morbidity, mortality, and medical expenditures (Guy, Machlin, Ekwueme, & Yarbroff, 2015; Guy, et al., 2015). Current guidance from the U.S. Preventive Services Task Force concludes that more research is needed to assess the balance of benefits and harms of visual skin examination by a clinician to screen for skin cancer in asymptomatic adults who do not have a history of premalignant or malignant skin lesions (US Preventive Services Task Force, 2016). In the Discussion section of the recommendation statement webpage, the U.S. Preventive Services Task Force notes that “targeted research among populations with the highest burden of disease would be helpful.”
We found that among U.S. older adults, men, individuals under the age of 75, non-Hispanic whites, and those with skin that burns repeatedly or freckles upon repeated sun exposure were the most likely to report sunburn. These groups may also be the most likely to benefit from sun-safety interventions. Similar to previous findings, the high likelihood of sunburn among those with sun-sensitive skin suggests potential value in using sun-sensitivity, rather than race or ethnicity, to identify those at greatest risk for skin cancer, particularly given the growing racial/ethnic diversity in the United States (Holman et al., 2018a). Some participants had skin that would develop a sunburn after 1 hr unprotected in the sun (after several months of not being in the sun) and then develop a “very dark tan” after repeated sun exposure. We found a high prevalence of sun-burn among these individuals. Past research findings suggest that individuals whose skin burns and then tans often experience repeated sunburns over time as the perceived harms of a sunburn are outweighed by the perceived benefits of having a tan (Clarke, Williams, & Arthey, 1997). Misconceptions about sun-tanned skin may also lead these individuals to have lower perceived susceptibility to sun damage and skin cancer.
Older adults are a heterogeneous group, and in addition to the genetic and phenotypic risk factors for skin cancer, some other characteristics may put certain older adults at a higher risk for skin cancer. For example, some older adults may engage in frequent outdoor activities, have out-door occupations such as construction or farming, or live in parts of the United States with greater total solar UVR (Richards et al., 2011), potentially leading to high levels of UVR exposure. Some may be taking prescription medications (e.g., certain antibiotics, antifungals, antihistamines, cholesterol lowering drugs, diuretics, and nonsteroidal anti-inflammatories) or using topical skin products (e.g., retinoids and alpha-hydroxy acids) that make their skin more sensitive to UVR exposure (U.S. Food and Drug Administration, 2018). Additionally, low levels of financial well-being among some older adults may create barriers to the purchase and use of certain forms of sun protection (Holman et al., 2015; Tucker-Seeley & Thorpe, 2019). For example, previous research indicates that individuals with household incomes below US$60,000 are significantly less likely to regularly use sunscreen when outdoors on a sunny day for an hour or more, even when accounting for other relevant demographic characteristics such as race and ethnicity (Holman et al., 2015).
Sun-safety interventions are warranted for older adults to reduce their risk of developing skin cancer late in life. However, very little research has been conducted to identify targeted strategies that are effective among this age group. In spite of the higher skin cancer rates among older adults, data from the Health Information National Trends Survey indicate that, compared with young adults, older adults are more likely to believe their skin cancer risk is low (Buster et al., 2012). Those aged 75 years and older reported less worry about developing skin cancer and more often agreed that there is not much one can do to prevent it (Buster et al., 2012). Messaging strategies could counter these beliefs and empower adults to take action to protect the future health of their skin. More research is warrented to determine how to frame messages in ways that resonate with older adults. Further research could also identify environmental change strategies that are most effective in reducing overexposure to UVR and supporting sun safety in this age group. Given the higher prevalence of shade use relative to the other sun protection behaviors, strategic placement of shade in out-door community settings is a promising approach.
In 2014, the U.S. Surgeon General released a Call to Action to Prevent Skin Cancer (U.S. Department of Health and Human Services, 2014). An overarching theme within the document was that all community sectors can play a role in efforts to promote sun safety, reduce overexposure to UVR, and ultimately, decrease skin cancer incidence rates. For example, communities can increase shade in outdoor public spaces, promote use of sun protection (e.g., sunscreen and protective clothing) during outdoor recreation, and encourage employers to provide sun protection gear for outdoor employees. In line with the themes from the Call to Action, successful efforts to promote sun safety among older adults will likely require a coordinated effort within communities and nationwide. Key partners will include many of the sectors already engaged in efforts targeting younger age groups such as clinicians, employers, and policy-makers but will also include new partners such as gerontologists and other groups whose work focuses specifically on older adults.
Although evidence suggests that sunburns that occur during adulthood increase one’s lifetime risk of developing melanoma (Dennis et al., 2008), there limited information in the published literature on the latency period for skin cancer development. Further research regarding the process of skin cancer development and the corresponding latency period could shed light on the degree to which sunburns that occur during older adulthood increase subsequent skin cancer risk and help us to clarify the potential benefits of minimizing UVR exposure later in life.
Strengths and Limitations
This study is the first of its kind to delve into the sun protection behaviors and prevalence of sunburn among older adults. The use of national surveillance data provides a large sample size and allows us to generalize the findings to the noninstitutionalized civilian U.S. older adult population. However, the study has limitations, which should be considered when interpreting the results. Measures of sun-sensitivity, sunburn, and sun protection behaviors were based on self-reports and are subject to error. Some adults (particularly those who do not go outside in sun for long periods of time) may be unaware of or unsure of their skin’s sensitivity to the sun. The survey question about sunburn did not include details about the severity of the sunburn or context in which the sunburn occurred, including whether the respondent was using sun protection when the sun-burn occurred. The survey questions about sun protection lacked sufficient detail to allow us to differentiate between adequate and inadequate use of such protective measures, and adults who reported “not going in the sun” could have still gone in the sun daily for up to an hour. Given the cross-sectional nature of the data, the temporal relationship between the use of the reported sun protection behaviors and the occurrence of the reported sunburns is unknown.
Conclusions
The prevalence of sunburn among older adults, particularly among 65–74 years old, men, non-Hispanic whites, and those with sun-sensitive skin, suggests that there may be opportunities to reduce skin cancer risk later in life. More work is needed to identify effective interventions to promote and facilitate adequate sun protection among older adults. A comprehensive approach to skin cancer risk reduction that engages many different community sectors and takes advantage of prevention opportunities throughout older adulthood is warranted.
Funding
This work was supported by the Division of Cancer Prevention and Control at the National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. D. M. Holman is a federal employee. H. Ding is a contractor with DB Consulting Group Inc. assigned to the Centers for Disease Control and Prevention’s Division of Cancer Prevention and Control. This research was supported in part by appointments (Ms. Shoemaker and Ms. Freeman) to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention. This paper was published as part of a supplement sponsored and funded by the Centers for Disease Control and Prevention (CDC).
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of Interest
None declared.
References
- American Academy of Dermatology. (2018). Say yes to sun protection; say no to skin cancer. Retrieved from https://www.aad.org/public/spot-skin-cancer/learn-about-skin-cancer/prevent/say-yes-to-sun-protection. Accessed July 23, 2018.
- American Cancer Society. (2017). How do I protect myself from UV rays? Retrieved from https://www.cancer.org/cancer/skin-cancer/prevention-and-early-detection/uv-protection.html. Accessed July 23, 2018.
- Arias E, Heron M, & Xu J (2017). United States life tables, 2014. National Vital Statistics Reports, 66, 2017–1120. [PubMed] [Google Scholar]
- Autier P, Boniol M, & Doré JF (2007). Sunscreen use and increased duration of intentional sun exposure: Still a burning issue. International Journal of Cancer, 121, 1–5. doi: 10.1002/ijc.22745 [DOI] [PubMed] [Google Scholar]
- Buster KJ, You Z, Fouad M, & Elmets C (2012). Skin cancer risk perceptions: A comparison across ethnicity, age, education, gender, and income. Journal of the American Academy of Dermatology, 66, 771–779. doi: 10.1016/j.jaad.2011.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke VA, Williams T, & Arthey S (1997). Skin type and optimistic bias in relation to the sun protection and suntanning behaviors of young adults. Journal of Behavioral Medicine, 20, 207–222. [DOI] [PubMed] [Google Scholar]
- Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, & Coughlin JA (2008). Sunburns and risk of cutaneous melanoma: Does age matter? A comprehensive meta-analysis. Annals of Epidemiology, 18, 614–627. doi: 10.1016/j.annepidem.2008.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, McCarty F, Nehl EJ, O’Riordan DL, Gies P, Bundy L, … Hall DM (2009). Validity of self-reported sunscreen use by parents, children, and lifeguards. American Journal of Preventive Medicine, 36, 63–69. doi: 10.1016/j.amepre.2008.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green AC, Williams GM, Logan V, & Strutton GM (2011). Reduced melanoma after regular sunscreen use: Randomized trial follow-up. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 29, 257–263. doi: 10.1200/JCO.2010.28.7078 [DOI] [PubMed] [Google Scholar]
- Guy GP Jr, Machlin SR, Ekwueme DU, & Yabroff KR (2015a). Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. American Journal of Preventive Medicine, 48, 183–187. doi: 10.1016/j.amepre.2014.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy GP Jr, Thomas CC, Thompson T, Watson M, Massetti GM, & Richardson LC; Centers for Disease Control and Prevention (CDC). (2015b). Vital signs: Melanoma incidence and mortality trends and projections - United States, 1982–2030. MMWR. Morbidity and Mortality Weekly Report, 64, 591–596. [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Berkowitz Z, Guy GP Jr, Hawkins NA, Saraiya M, & Watson M (2015). Patterns of sunscreen use on the face and other exposed skin among US adults. Journal of the American Academy of Dermatology, 73, 83–92.e1. doi: 10.1016/j.jaad.2015.02.1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Ding H, Guy GP Jr, Watson M, Hartman AM, & Perna FM (2018a). Prevalence of sun protection use and sunburn and association of demographic and behaviorial characteristics with sunburn among US Adults. JAMA Dermatology, 154, 561–568. doi: 10.1001/jamadermatol.2018.0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Shoemaker M, & Freeman MB (2018b). Trends in melanoma incidence among non-Hispanic whites in the United States, 2005–2014. JAMA Dermatology, 154, 361–362. doi: 10.1001/jamadermatol.2017.5541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen R, Osterwalder U, Wang SQ, Burnett M, & Lim HW (2013). Photoprotection, part II: Sunscreen: Development, efficacy, and controversies. Journal of the American Academy of Dermatology, 69, 867, e861–e814. doi: 10.1016/j.jaad.2013.08.022 [DOI] [PubMed] [Google Scholar]
- Morris KL & Perna FM (2018). Decision tree model vs traditional measures to identify patterns of sun-protective behaviors and sun sensitivity associated with sunburn. JAMA Dermatology, 154, 8, 897–902. doi: 10.1001/jamadermatol.2018.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2015). Survey description. Hyattsville, MD: National Health Interview Survey, 2015. [Google Scholar]
- O’Riordan DL, Nehl E, Gies P, Bundy L, Burgess K, Davis E, & Glanz K (2009). Validity of covering-up sun-protection habits: Association of observations and self-report. Journal of the American Academy of Dermatology, 60, 739–744. doi: 10.1016/j.jaad.2008.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parisi AV, & Turnbull DJ (2014). Shade provision for UV minimization: A review. Photochemistry and Photobiology, 90, 479–490. doi: 10.1111/php.12237 [DOI] [PubMed] [Google Scholar]
- Paulson KG, Park SY, Vandeven NA, Lachance K, Thomas H, Chapuis AG,…Nghiem P (2018). Merkel cell carcinoma: Current US incidence and projected increases based on changing demographics. Journal of the American Academy of Dermatology, 78, 457–463.e2. doi: 10.1016/j.jaad.2017.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Pols JC, Williams GM, Pandeya N, Logan V, & Green AC (2006). Prolonged prevention of squamous cell carcinoma of the skin by regular sunscreen use. Cancer Epidemiology, Biomarkers & Prevention, 15, 2546–2548. doi: 10.1158/1055-9965.EPI-06-0352 [DOI] [PubMed] [Google Scholar]
- Richards TB, Johnson CJ, Tatalovich Z, Cockburn M, Eide MJ, Henry KA,…Ajani UA (2011). Association between cutaneous melanoma incidence rates among white US residents and county-level estimates of solar ultraviolet exposure. Journal of the American Academy of Dermatology, 65, S50–S57. doi: 10.1016/j.jaad.2011.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers HW, Weinstock MA, Feldman SR, & Coldiron BM (2015). Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatology, 151, 1081–1086. doi: 10.1001/jamadermatol.2015.1187 [DOI] [PubMed] [Google Scholar]
- Syrigos KN, Tzannou I, Katirtzoglou N, & Georgiou E (2005). Skin cancer in the elderly. In vivo (Athens, Greece), 19, 643–652. [PubMed] [Google Scholar]
- The Community Guide. Cancer. (2018). Retrieved from https://www.thecommunityguide.org/topic/cancer. Accessed February 7, 2018.
- Tucker-Seeley R & Thorpe R. Material-psychosocial-behavioral aspects of financial well-being: A conceptual model applied to cancer prevention research . The Gerontologist, Suppl X:SX–X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2014). The surgeon general’s call to action to prevent skin cancer. Washington, DC: U.S. Dept of Health and Human Services, Office of the Surgeon General; 2014. [PubMed] [Google Scholar]
- U.S. Food and Drug Administration. (2018). The sun and your medicine. Retrieved from https://www.fda.gov/Drugs/ResourcesForYou/SpecialFeatures/ucm464195.htm. Accessed February 7, 2018.
- U.S. Preventive Services Task Force. (2016). Screening for skin cancer: U.S. Preventive Services Task Force recommendation statement. Journal of the American Medical Association, 316, 429–435. doi: 10.1001/jama.2016.8465 [DOI] [PubMed] [Google Scholar]
- Wright MW, Wright ST, & Wagner RF (2001). Mechanisms of sunscreen failure. Journal of the American Academy of Dermatology, 44, 781–784. doi: 10.1067/mjd.2001.113685 [DOI] [PubMed] [Google Scholar]