Abstract
Background: Experiences during the birth hospitalization affect breastfeeding outcomes. In the United States, hospital policies and practices supportive of breastfeeding are routinely assessed through the Maternity Practices in Infant Nutrition and Care (mPINC) survey; however, mPINC does not capture data on breastfeeding outcomes.
Materials and Methods: Data from the 2015 mPINC survey were linked to 2015 data from the Joint Commission (TJC), a major accreditor of health care systems in the United States (n = 1,305 hospitals). Each hospital participating in mPINC is given a total score, which is the average of seven subscores; all ranging from 0 to 100. TJC has hospital-specific data on the percentage of infants exclusively breastfeeding at hospital discharge. We used linear regression to estimate differences between quartiles of (1) total mPINC score and (2) each mPINC subscore with rates of exclusive breastfeeding at hospital discharge, adjusting for hospital type, teaching status, and number of annual births. We additionally used linear models to test for trend across quartiles of mPINC score.
Results: The mean percentage of in-hospital exclusive breastfeeding increased from 39.0% for hospitals in the lowest mPINC total score quartile (<75) to 60.4% for hospitals in the highest mPINC total score quartile (≥89), an adjusted difference of 21.1 percentage points (95% confidence interval 18.6–23.6). The mean percentage of in-hospital exclusive breastfeeding significantly increased (p < 0.0001) as mPINC scores increased for total mPINC score and for each mPINC subscore.
Conclusions: Higher mPINC scores were associated with higher rates of in-hospital exclusive breastfeeding. Hospitals can make improvements to their maternity care practices and policies to support breastfeeding.
Keywords: maternity care practices, breastfeeding, mPINC
Introduction
The American Academy of Pediatrics recommends infants be exclusively breastfed for about the first 6 months of life.1 Exclusive breastfeeding has numerous benefits for both mother and infant, and longer durations of exclusive breastfeeding have been associated with greater health benefits.2 National data demonstrate that 83.2% of newborns initiate breastfeeding and 64.7% are exclusively breastfeeding at 7 days of age.1 This discrepancy is in large part due to 17.2% of breastfeeding newborns being supplemented with infant formula before they reach 2 days of age,1 which often occurs in the hospital.3 Infants who are supplemented with formula while in the hospital are three times less likely to be receiving any breast milk at day 60.4
Practices such as initiating breastfeeding within 1 hour of birth, no formula supplementation during the hospital stay unless medically indicated, rooming-in, on-demand breastfeeding, and postdischarge breastfeeding support have been associated with increased rates of breastfeeding initiation,5 duration,6–8 and exclusivity.5,6,9 As such, improving maternity care practices and policies supportive of breastfeeding has been a key effort of national and international organizations.
In 2007, the Centers for Disease Control and Prevention (CDC) launched the Maternity Practices in Infant Nutrition and Care (mPINC) survey to monitor hospital-level practices and polices related to infant feeding and care.10 Although mPINC survey data have been used to document improved trends in maternity care practices in the United States,11–14 the survey does not collect information on breastfeeding outcomes. A prior study that linked mPINC to the Pregnancy Assessment Monitoring System (PRAMS) found higher mPINC scores to be associated with better breastfeeding outcomes (any and exclusive breastfeeding at 8 weeks), but this study did not assess in-hospital exclusive breastfeeding rates that are needed to gain a more complete picture of what is happening during the birth hospitalization.6
In-hospital breastfeeding outcomes are measured by the Joint Commission (TJC), an independent nonprofit organization that accredits and certifies ∼88% of accredited U.S. hospitals.15 TJC collects data on exclusive breastfeeding at hospitals providing maternity care in the United States as part of its perinatal care quality measures.16 By linking mPINC and TJC data, another previous study found an association between hospital practices and improved exclusive breastfeeding rates; however, this study used Baby-Friendly designation as their exposure17 and currently only about 26% of births occur in Baby-Friendly facilities.1
To our knowledge, no studies have examined hospital-reported maternity care practices and hospital-reported breastfeeding outcomes on a national level. Therefore, the purpose of this study was to assess whether maternity care practices (as determined by mPINC score) were associated with in-hospital exclusive breastfeeding rates (as reported to TJC).
Materials and Methods
Data sources
Data for this analysis were obtained from CDC's 2015 mPINC survey (data collected from August 2015 through February 2016) and 2015 TJC data (data collected from January 2015 through December 2015). Detailed data collection methods of the mPINC survey are published elsewhere.18 In brief, mPINC is a biennial census of all birth hospitals and birth centers in the United States and territories. Since birth centers do not report to TJC, they were excluded from this analysis (n = 170). The 2015 mPINC survey was sent to the person(s) at each hospital most knowledgeable about routine infant feeding practices and policies, who was most frequently the mother–baby unit manager. Information about hospital-level practices and polices related to infant feeding and care were collected. Starting in 2010, TJC began collecting data on exclusive breastfeeding at United States hospitals with maternity care by voluntary reporting. Beginning January 1, 2014, hospitals with at least 1,100 births per year were required to report exclusive breastfeeding to retain their accreditation and smaller hospitals could continue to voluntarily report this measure. During 2015, TJC announced the threshold for mandatory reporting was changing to 300 births effective January 1, 2016, thus more smaller hospitals may have been reporting the measure in 2015.19
Data from the 2015 mPINC survey were linked to 2015 TJC data by hospital name and postal address. In 2015, the mPINC response rate was 82%, and included 2,412 participating hospitals. TJC database included 1,748 hospitals; 411 of these were hospitals that did not participate in the 2015 mPINC survey, enabling us to link 1,337 hospitals. Hospitals in the mPINC database may not have been in TJC database because they are accredited by another organization, or did not report on the exclusive breastfeeding measure (in 2015 only required of hospitals with >1,100 births per year). Of the 1,337 linked hospitals, 32 were missing information on hospital characteristics collected in mPINC, resulting in a final analytic sample of 1,305. The number of hospitals varies slightly for subscore analyses because some hospitals were missing data on individual subscores.
Our exposure of interest was hospital practices and policies supportive of breastfeeding, as measured by mPINC scores. The CDC organized information collected in mPINC into seven maternity care practice subdomains: (1) labor and delivery care, (2) feeding of breastfed infants, (3) breastfeeding assistance, (4) contact between mother and infant, (5) hospital discharge care, (6) staff training, and (7) structural and organizational aspects of care. CDC calculated scores on a scale from 0 to 100 for each of the seven maternity care practice subdomains, and these seven subscores were averaged to calculate the hospital's total mPINC score.20 Higher scores denote better maternity care practices and policies. mPINC scores were treated as a continuous variable (0–100). Scores were categorized into quartiles, except for the feeding of breastfed infants subscore, which was categorized into tertiles due to a more limited distribution of scores.
We obtained data from TJC for our outcome, in-hospital exclusive breastfeeding rates. TJC defines exclusive breast milk feeding as “a newborn receiving only breast milk and no other liquids or solids except for drops or syrups consisting of vitamins, minerals, or medicines.”16 In-hospital exclusive breast milk feeding was reported as an overall percentage of newborns who were exclusively fed breast milk during their entire hospitalization from a sample of eligible infants.16 Details about TJC sampling methods are published elsewhere.21 In brief, hospitals are given detailed instructions on how to sample for the measure. This includes information on the minimum sample that must be randomly sampled for larger hospitals, or all records are taken for smaller hospitals. Suggested data sources for this measure include feeding flow sheets, physician notes, a discharge summary, or nursing notes from the medical record. Hospitals reported this information to TJC in one of two ways: (1) through an intermediary company who sent patient-level data to TJC, from which TJC produced rates using an established algorithm, or (2) hospitals reported data to TJC's direct data submission platform. The denominator for this percentage comprised single, term newborns discharged alive from the hospital.16 The numerator for this percentage comprised eligible newborns who were fed breast milk only since birth. This measure excludes infants who were admitted to the neonatal intensive care unit, diagnosed with galactosemia, on parenteral infusion, with a hospital stay >120 days, enrolled in clinical trials, with documented reasons for not exclusively feeding breast milk, transferred to another hospital, or those born preterm.16
Statistical analysis
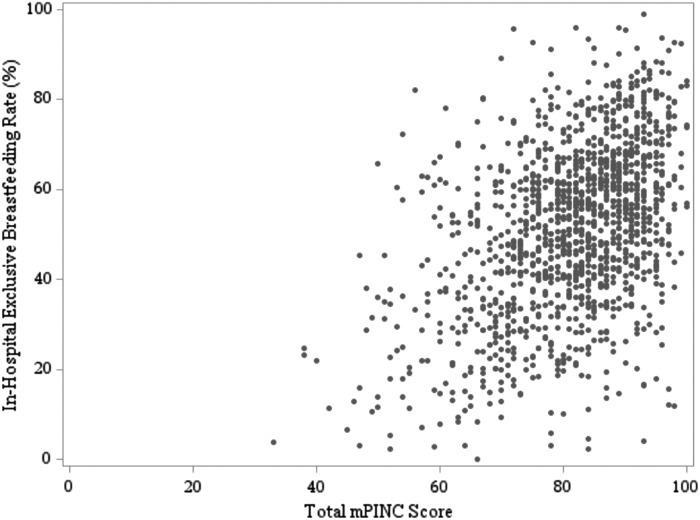
We calculated the prevalence of the following hospital characteristics: hospital type (nonprofit, private, government, or military), teaching status (no, yes), hospital size (annual number of births), and average mPINC total score and subscores (mean and range). In-hospital exclusive breastfeeding rate was plotted compared with the total mPINC score, as a continuous variable (0–100). We used linear regression models to estimate differences in mean exclusive breastfeeding rate by quartile of (1) total mPINC score and (2) each mPINC subscore, adjusting for hospital type, teaching status, and size. We additionally used linear regression models to test for trend across mPINC total score and subscore. Analyses were conducted using SAS v. 9.4 (Cary, NC).
Results
Table 1 illustrates the hospital characteristics and mPINC scores of the 1,305 hospitals included in the sample. The majority of the hospitals were nonprofit (70.8%), followed by private (15.3%), government (12.4%), and military (1.4%). About 12% of the hospitals were teaching hospitals. Hospitals with <250 births per year represented the smallest group of the study population (3.6%), and hospitals with 1,000–1,999 births represented the largest group of the study population (30.1%). The mean total mPINC score was 81 (range 33–100). Mean mPINC subscores ranged from 69 (range 0–100) for the discharge care subdomain to 91 (range 47–100) for the breastfeeding assistance subdomain.
Table 1.
Characteristics of Hospitals That Participated in the 2015 mPINC Survey and Reported Exclusive Breastfeeding Rates to the joint Commission
| Hospital characteristic | N (%) or mean [range] |
|---|---|
| Total | 1,305 |
| Hospital type | |
| Nonprofit | 924 (70.8%) |
| Private | 199 (15.3%) |
| Government | 162 (12.4%) |
| Military | 20 (1.5%) |
| Teaching hospital | |
| No | 1,143 (87.6%) |
| Yes | 162 (12.4%) |
| Size (annual number of births) | |
| 1–249 | 47 (3.6%) |
| 250–499 | 201 (15.4%) |
| 500–999 | 239 (18.3%) |
| 1,000–1,999 | 393 (30.1%) |
| 2,000–4,999 | 375 (28.7%) |
| ≥5,000 | 50 (3.8%) |
| mPINC score | |
| Total score | 81 [33–100] |
| Subscores | |
| Labor and delivery care | 86 [6–100] |
| Feeding of breastfed infants | 87 [23–100] |
| Breastfeeding assistance | 91 [47–100] |
| Contact between mother and infant | 83 [20–100] |
| Discharge care | 69 [0–100] |
| Staff training | 71 [0–100] |
| Structural and organizational aspects of care delivery | 82 [3–100] |
mPINC, Maternity Practices in Infant Nutrition and Care.
There was a positive linear correlation between total mPINC score and exclusive breastfeeding at hospital discharge (Pearson's r = 0.45, p < 0.0001) (Fig. 1). The mean percentage of in-hospital exclusive breastfeeding was 51.2% overall, and improved with each increasing quartile of mPINC total score: 39.0% for hospitals in Quartile 1 (<75), 50.4% for hospitals in Quartile 2 (75–82), 53.8%, for hospitals in Quartile 3 (83–88), and 60.4% for hospitals in Quartile 4 (≥89) (Table 2). After adjusting for hospital characteristics, hospitals with total mPINC scores in Quartiles 2, 3, and 4 had exclusive breastfeeding rates that were, on average, 11.3, 14.3, and 21.1 percentage points higher, respectively, compared with Quartile 1 (Table 2). Mean percentage of in-hospital breastfeeding rates were higher in higher score quartiles (compared with Quartile 1) for all seven subscores (Table 2). The greatest difference in breastfeeding across centiles among the subscores was for the labor and delivery care subdomain; hospitals with mPINC scores in the lowest quartile (<80) had a mean percentage of in-hospital exclusive breastfeeding of 39.0% and hospitals in the highest quartile (100) had a mean percentage of in-hospital exclusive breastfeeding of 59.1%, an adjusted increase of 19.1 percentage points (95% CI 16.8–21.5) (Table 2). When testing for trend, mean percentage of in-hospital exclusive breastfeeding significantly increased (p < 0.0001) across quartiles of mPINC total and all subscores.
FIG. 1.
Association between 2015 total mPINC scores and exclusive breastfeeding at hospital discharge. mPINC, Maternity Practices in Infant Nutrition and Care.
Table 2.
Association Between 2015 mPINC Scores and Exclusive Breastfeeding at Hospital Discharge
| Quartile/tertile of mPINC score | No. of hospitals | Mean % exclusive breastfeedinga | β | (95% CI) | p |
|---|---|---|---|---|---|
| Overall | 1,305 | 51.2 | — | — | — |
| Total score | |||||
| Quartile 1 (<75) | 317 | 39.0 | — | — | — |
| Quartile 2 (75–82) | 322 | 50.4 | 11.3 | 8.8 to 13.8 | <0.0001 |
| Quartile 3 (83–88) | 306 | 53.8 | 14.3 | 11.8 to 16.9 | <0.0001 |
| Quartile 4 (≥89) | 360 | 60.4 | 21.1 | 18.6 to 23.6 | <0.0001 |
| Labor and delivery care | |||||
| Quartile 1 (<80) | 299 | 39.0 | — | ||
| Quartile 2 (80–93) | 331 | 49.5 | 9.3 | 6.8 to 11.9 | <0.0001 |
| Quartile 3 (94–99) | 218 | 53.8 | 13.8 | 10.9 to 16.6 | <0.0001 |
| Quartile 4 (100) | 454 | 59.1 | 19.1 | 16.8 to 21.5 | <0.0001 |
| Feeding of breastfed infants | |||||
| Tertile 1 (<83) | 322 | 41.9 | — | — | — |
| Tertile 2 (83–92) | 219 | 45.3 | 3.1 | 0.3 to 6.0 | 0.0306 |
| Tertile 3 (≥93) | 737 | 57.1 | 14.1 | 12.0 to 16.3 | <0.0001 |
| Breastfeeding assistance | |||||
| Quartile 1 (<86) | 261 | 43.6 | — | — | — |
| Quartile 2 (86–95) | 362 | 48.2 | 4.7 | 2.0 to 7.5 | 0.0007 |
| Quartile 3 (96–99) | 223 | 55.7 | 11.7 | 8.6 to 14.8 | <0.0001 |
| Quartile 4 (100) | 456 | 55.7 | 11.6 | 9.0 to 14.3 | <0.0001 |
| Mother-infant contact | |||||
| Quartile 1 (<74) | 304 | 41.0 | — | — | — |
| Quartile 2 (74–87) | 284 | 49.6 | 8.6 | 5.8 to 11.4 | <0.0001 |
| Quartile 3 (88–93) | 139 | 53.1 | 12.1 | 8.6 to 15.6 | <0.0001 |
| Quartile 4 (≥94) | 577 | 56.9 | 16.0 | 13.5 to 18.4 | <0.0001 |
| Discharge care | |||||
| Quartile 1 (<55) | 195 | 41.4 | — | — | — |
| Quartile 2 (55–67) | 255 | 49.6 | 7.9 | 4.7 to 11.2 | <0.0001 |
| Quartile 3 (68–87) | 394 | 52.6 | 9.8 | 6.8 to 12.9 | <0.0001 |
| Quartile 4 (≥88) | 456 | 55.2 | 11.6 | 8.6 to 14.7 | <0.0001 |
| Staff training | |||||
| Quartile 1 (<58) | 311 | 48.5 | — | — | — |
| Quartile 2 (58–74) | 261 | 48.5 | 0.8 | −2.1 to 3.7 | 0.5806 |
| Quartile 3 (75–87) | 285 | 52.3 | 4.3 | 1.4 to 7.2 | 0.0034 |
| Quartile 4 (≥88) | 422 | 54.3 | 7.1 | 4.4 to 9.8 | <0.0001 |
| Structural and organizational aspects of care delivery | |||||
| Quartile 1 (<72) | 317 | 44.2 | — | — | — |
| Quartile 2 (72–83) | 330 | 50.0 | 5.5 | 2.8 to 8.1 | <0.0001 |
| Quartile 3 (84–95) | 323 | 51.7 | 7.2 | 4.4 to 9.9 | <0.0001 |
| Quartile 4 (≥96) | 335 | 59.7 | 14.0 | 11.2 to 16.8 | <0.0001 |
β reflects estimated difference in exclusive breastfeeding rate from the referent group, adjusted for hospital type, teaching status, and size.
The number of hospitals vary (n = 1,278–1,305) for subscore analyses because some hospitals were missing data on individual subscores.
CI, confidence interval.
Discussion
As total mPINC score increased, rates of in-hospital exclusive breastfeeding were significantly higher, suggesting that newborns who are delivered in hospitals with practices and policies supportive of breastfeeding have better in-hospital breastfeeding outcomes, as measured by exclusive breastfeeding. We observed this relationship for the total mPINC score as well as across all seven subdomains.
The mean exclusive in-hospital breastfeeding rate in this analysis (51.2%) was lower than the national rate for exclusive breastfeeding at 7 days of age (64.7%)1; this was true even among hospitals in Quartile 4, which had the highest total mPINC scores (60.4%). This may be due to a difference in how the data are collected. National data are collected retrospectively from respondents with children 19–35 months old through the National Immunization Survey (NIS) and may be subject to recall bias or reporting error, including the mother not knowing or not accounting for supplementation her infant may have received in the hospital. In addition, NIS data are from a nationally representative sample of infants and data for this study are from a subsample of hospitals that participated in mPINC and reported to TJC.
National data collection on maternity care practices as well as hospital-level breastfeeding outcomes can serve as an interventional driver toward improvement of practices. In addition to monitoring hospital practices, CDC sends each hospital that participates in mPINC an individualized benchmark report highlighting how the hospital is doing in comparison with hospitals of similar size, hospitals within the same state, and all hospitals that participated in the survey. Hospitals can use this report to identify areas of care that are strengths as well as improvement opportunities.10 The inclusion of exclusive breastfeeding in the perinatal core measure set may also contribute to improvements in hospital practices that support breastfeeding. In 2016, TJC expanded their requirement of reporting on exclusive breast milk feeding to hospitals with >300 births per year.22 Expanding reporting of this measure to smaller hospitals may help to increase awareness of the importance of exclusive breast milk feeding and further drive hospitals to improve their maternity care practices supportive of breastfeeding.
Our findings are consistent with the previous studies in the United States that found improved maternity care practices associated with increased breastfeeding rates. One study that linked 2009 mPINC and PRAMS data found improved breastfeeding outcomes for any and exclusive breastfeeding at 8 weeks with increased mPINC total score.6 Another study linked data from TJC and Baby-Friendly USA and found the Baby-Friendly hospital designation to be associated with significantly higher exclusive breastfeeding rates.17 The Baby-Friendly designation indicates that a hospital is implementing the Ten Steps to Successful Breastfeeding and the International Code of Marketing of Breast-milk Substitutes.23 Although the Baby-Friendly designation is a marker of hospital practices and policies supportive of breastfeeding, not all hospitals implementing such practices go through the designation process. Therefore, Baby-Friendly designation does not encompass the full spectrum of adherence to breastfeeding-supportive practices.
Strengths of this study include that mPINC is a census of all maternity facilities and has a high response rate. By linking mPINC data with data from TJC, we were able to examine maternity care practices and policies and breastfeeding outcomes at >1,300 hospitals. Limitations of this study include that mPINC is a self-reported survey, and although a standard protocol is implemented to identify a key informant at each hospital, responses may not accurately represent all hospital practices. Our study sample disproportionately included larger hospitals because they were more likely to report data on exclusive breastfeeding rates to TJC due to reporting requirements by hospital size. For example, the mean hospital-level number of annual births was 1,754 in our analytic sample, versus 1,274 in the full 2015 mPINC sample. Larger hospitals tend to have better maternity care practices24 and as a result, hospitals in our sample had a slightly higher average total mPINC score than all hospitals that completed the 2015 mPINC survey (81 versus 79). In addition, hospitals included in our sample had a slightly higher mean breastfeeding rate than the 411 hospitals that were excluded due to not completing the 2015 mPINC survey (51.2% versus 48.6%).
Conclusion
Facilities with higher mPINC scores had higher rates of in-hospital exclusive breastfeeding for the total mPINC score and for each mPINC subdomain score. Higher mPINC scores demonstrate hospital practices and policies supportive of breastfeeding; therefore, our data provide further evidence for the effects of maternity care practices on breastfeeding outcomes.
Authors' Contributions
C.M.B. contributed to the analytic study design, conducted the analysis, and drafted and revised the final article. J.L.B., J.M.N., and C.G.P. contributed to the analytic study design and provided critical review of the article. All authors approved the final article as submitted and agree to be accountable for all aspects of the study.
Disclosure Statement
The authors have no conflicts of interest to disclose. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1. Centers for Disease Control and Prevention. 2018 Breastfeeding report card. Available at https://www.cdc.gov/breastfeeding/data/reportcard.htm (accessed August24, 2018)
- 2. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev 2012:Cd003517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Contraindications to breastfeeding or feeding expressed breast milk to infants. Updated March 21, 2018. Available at https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/Contraindications-to-breastfeeding.html (accessed June28, 2018)
- 4. Chantry CJ, Dewey KG, Peerson JM, et al. . In-hospital formula use increases early breastfeeding cessation among first-time mothers intending to exclusively breastfeed. J Pediatr 2014;164:1339–1345.e1335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Merewood A, Mehta SD, Chamberlain LB, et al. . Breastfeeding rates in US Baby-Friendly hospitals: Results of a national survey. Pediatrics 2005;116:628–634 [DOI] [PubMed] [Google Scholar]
- 6. Nelson JM, Perrine CG, Freedman DS, et al. . Infant feeding-related maternity care practices and maternal report of breastfeeding outcomes. Birth 2018;45:424–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ahluwalia IB, Morrow B, D'Angelo D, et al. . Maternity care practices and breastfeeding experiences of women in different racial and ethnic groups: Pregnancy risk assessment and monitoring system (PRAMS). Matern Child Health J 2012;16:1672–1678 [DOI] [PubMed] [Google Scholar]
- 8. DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics 2008;122 Suppl 2:S43–S49 [DOI] [PubMed] [Google Scholar]
- 9. Perrine CG, Scanlon KS, Li R, et al. . Baby-friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012;130:54–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Maternity practices in infant nutrition and care (mPINC). Updated December 1, 2017. Available at www.cdc.gov/breastfeeding/data/mpinc/index.htm (accessed February6, 2018)
- 11. Perrine CG, Galuska DA, Dohack JL, et al. . Vital signs: Improvements in maternity care policies and practices that support breastfeeding—United States, 2007–2013. MMWR Morb Mortal Wkly Rep 2015;64:1112–1117 [DOI] [PubMed] [Google Scholar]
- 12. Nelson JM, Li R, Perrine CG. Trends of US hospitals distributing infant formula packs to breastfeeding mothers, 2007 to 2013. Pediatrics 2015;135:1051–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Barrera CM, Nelson JM, Boundy EO, et al. . Trends in rooming-in practices among hospitals in the United States, 2007–2015. Birth 2018;45:432–439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boundy EO, Perrine CG, Barrera CM, et al. . Trends in maternity care practice skin-to-skin contact indicators: United States, 2007–2015. Breastfeed Med 2018;13:381–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. The Joint Commission. Facts about hospital accreditation. Updated 2018. Available at https://www.jointcommission.org/facts_about_hospital_accreditation/ (accessed June12018)
- 16. The Joint Commission. Specifications Manual for Joint Commission National Quality Measures (v2015A1). 2015. https://manual.jointcommission.org/releases/TJC2015A1/index.html (accessed May23, 2018)
- 17. Patterson JA, Keuler NS, Olson BH. The effect of baby-friendly status on exclusive breastfeeding in U.S. hospitals. Matern Child Nutr 2018;14:e12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Methods: Maternity care practices. Updated December 1, 2017. Available at https://www.cdc.gov/breastfeeding/data/mpinc/methods.html Accessed May23, 2018
- 19. The Joint Commission. Improving performance on perinatal care measures. Benchmark 2013;11:16–19 [Google Scholar]
- 20. Centers for Disease Control and Prevention. Scoring: Maternity practices. Updated December 1, 2017. Available at https://www.cdc.gov/breastfeeding/data/mpinc/scoring.htm (accessed May23, 2018)
- 21. The Joint Commission. Specifications manual for joint commission national quality measures (v2017B2). Population and sampling method. Available at https://manual.jointcommission.org/releases/TJC2017B2/SamplingChapterTJC.html (accessed July17, 2018)
- 22. The Joint Commission. Expanded threshold for reporting perinatal care measure set. 2015. Available at https://www.jointcommission.org/assets/1/23/jconline_June_24_2015.pdf (accessed June4, 2018)
- 23. World Health Organization and UNICEF. Baby-friendly hospital initiative. Revised, updated, and expanded for integrated care. 2009. Available at http://whqlibdoc.who.int/publications/2009/9789241594967_eng.pdf (accessed October18, 2017) [PubMed]
- 24. Centers for Disease Control and Prevention. mPINC survey results: Maternity practices. Table 0a. Updated December 1, 2017. Available at https://www.cdc.gov/breastfeeding/data/mpinc/results-tables.htm (accessed July17, 2018)