Key Points
Question
What are the geographic limitations faced by US veterans in accessing cochlear implant care within the Veterans Health Administration system?
Findings
In this analysis of census tract–level data on 19.9 million US veterans, more than 80% of veterans in 7 states resided more than 180 miles from the nearest Veterans Health Administration facility providing cochlear implant services, including sites that offer only audiologic services. Veterans living in both rural and large urban population centers face several geographic limitations in accessing cochlear implant care.
Meaning
This study suggests that additional avenues to provide cochlear implant services within the Veterans Health Administration system may help provide adequate and accessible care to veterans with hearing loss.
Abstract
Importance
Veterans are at high risk for developing sensorineural hearing loss leading to cochlear implant (CI) candidacy; however, the ability to care for these patients is limited by the number and location of Veterans Health Administration (VHA) facilities that provide specialized CI services.
Objective
To investigate geographic disparities in access to CI care within the VHA system for US veterans.
Design, Setting, and Participants
An analysis of census tract–level data including US veterans was conducted using the nationwide American Community Survey data collected by the US Census Bureau from January to December 2016, which were accessed in 2017.
Main Outcomes and Measures
Maps showing the geographic variability in need for specialized CI services, estimated as a function of the number of veterans and the distance to the nearest established VHA-based CI surgical or audiologic facilities.
Results
A total of 19.9 million veterans within the continental United States resided at a median distance of 80 miles (interquartile range [IQR], 30.1-140.9 miles; mean [SD], 1002 [465.8] miles) from the nearest VHA facility offering CI care; of these, 3.98 million (20.0%) resided more than 160.7 miles from the nearest VHA facility. When considering only comprehensive facilities offering both surgical and audiologic care, the median distance was 101.3 miles (IQR, 39.4-178.7 miles; mean [SD], 126.0 [448.4] miles), but 20.0% of veterans had to travel more than 201.0 miles to a VHA facility. Veterans residing in urban areas (74.0%) lived a median distance of 61.2 miles (IQR, 23.7-121.3 miles; mean [SD], 83.8 [477.1] miles) from the nearest VHA facility, with 2.9 million (20.0%) living the farthest at 140.7 miles. Veterans residing in rural areas (26.0%) lived a median distance of 119.8 miles (IQR, 79.0-182.4 miles; mean [SD], 146.9 [431.0] miles) from their nearest VHA facility, with 1.04 million (20.0%) living more than 206.2 miles from the nearest VHA facility.
Conclusions and Relevance
This study’s findings suggest that large disparities exist in the distance to the nearest VHA-based CI facilities. Veterans face considerable geographic barriers to obtaining VHA-based CI care in many parts of the country, including some large metropolitan areas. Those requiring only audiologic services face similar geographic barriers as those requiring surgery. Thoughtful placement of new facilities, along with upcoming advances in remote programming of implants, may help ensure appropriate care for this high-risk population.
This analysis uses census tract–level data from the nationwide American Community Survey to investigate geographic disparities for US veterans in accessing cochlear implant facilities within the Veterans Health Administration system.
Introduction
The Veterans Health Administration (VHA) hospital system provides US veterans with access to both primary and specialty health care. It provides more than 1000 community-based outpatient clinics,1 whereas specialized care is concentrated in larger VHA facilities typically located in major cities, thereby simplifying access to tertiary care in the most densely populated areas. Larger urban VHA facilities are also often affiliated with major academic centers that provide specialist faculty, sometimes via a shared appointment. The relatively small number of tertiary care facilities, however, risks an uneven availability of specialized services and poorer care overall.
Cochlear implantation (CI) is an example of a specialized service and represents the best treatment available for people with severe to profound sensorineural hearing loss.2 Cochlear implants can restore hearing when conventional amplification is not sufficient to enable communication. This treatment involves using specialized surgical facilities, often located at large-volume hospitals, and audiologists who are responsible for preoperative candidacy evaluations and postoperative programming and follow-up. Cochlear implant facilities within the VHA system include those providing surgical and audiologic services (comprehensive centers) and those providing specialty CI audiologic services without surgical capabilities (audiology-only sites). This is an important distinction because surgical procedures are necessary only for the placement of the device(s) and any potential surgical sequelae. Audiology appointments are typically required 3 or more times in the first postoperative year and then annually thereafter.3 Cochlear implant device programming, however, requires that a patient consult with an audiologist routinely in the first year after receiving the device and annually thereafter.
Given that hearing loss is the second-most common service-connected disability within the VHA system,4 the number of veterans who could benefit from implantation is high. However, the burden of traveling hundreds of miles to receive care poses an obstacle for veterans who do not live near a VHA-based CI facility. Ideally, veteran access to specialized care, such as cochlear implantation, should be equally balanced with regard to serving densely populated urban regions but in a geographic distribution such that no large regions of the country go uncovered.
In recent years, frustration among veterans regarding long wait times and poor access to care has increased and garnered the attention of politicians, media, and the general public.5 In response, the VHA has focused on reducing delays in obtaining treatment.6 Geographic barriers to care have been less well publicized. However, rapidly developing spatial mapping techniques have recently been used to highlight and improve inequities of care in fields such as organ transplantation, bariatric surgery, and multiple sclerosis within the VHA system.7,8 Policy makers and health care professionals alike have expressed interest in easing access to CI care,9 but detailed information regarding the obstacles faced by veterans has not been previously published to our knowledge.
In the present study, we used geographic information system (GIS) mapping techniques to identify the regions that are in greatest need of CI care within the VHA system.
Methods
Locations of VHA facilities providing CI services (as of February 2017) were provided by the VHA Cochlear Implant Advisory Board (Nancy Cambron, AuD, written communication, February 24, 2017). The Oregon Health & Science University Institutional Review Board, Portland, determined that this study was exempt from institutional review board requirements and granted a waiver of review.
The 2016 American Community Survey data from the US Census Bureau were used to estimate the number of individuals with veteran status within each census tract.10 Census tracts are relatively stable geographic areas that usually contain a population between 2500 and 8000 persons, with an optimal population of 4000 persons. Although census tracts never cross county lines, their spatial size may vary considerably depending on the population density of a given geographic area. Geometric centroids of each census tract were used as an approximate location for all veterans residing within each respective tract since the census does not provide individual address-level data to the public.
The American Community Survey data were used instead of another source of data about veterans’ health, the VHA Corporate Data Warehouse, which has been used to study barriers to care in patients with transplants and multiple sclerosis.7,8 We were concerned that data from the Corporate Data Warehouse might underrepresent veteran CI candidates because they might not be enrolled in the VHA system or their workup might not include current audiometric data. The 2016 American Community Survey’s 5-year estimates of the total number of veterans per census tract were used. Alaska and Hawaii have no VHA-based CI services and are at a considerably large distance from existing VHA facilities offering CI services; therefore, these states were excluded from this analysis. In addition, 25 census tracts were excluded from the analysis because their geographic definitions (shape or name) changed during the process of the 2010-2016 survey.
Metropolitan statistical areas (MSAs), which are defined by the US federal government,11 were used to identify large urban regions of the country for reporting purposes. To understand how geography affected the veterans residing in urban vs rural areas differentially, MSA definitions from the US Census’s 2018 classification system were used to categorize census tracts as either belonging to an MSA or being rurally located. Secondary analyses were then performed to assess the disparities in distance for veterans in urban and rural areas.
Veteran access was defined as a combination of veteran population within each census tract and the straight-line distance in miles from the census tract geometric centroid to the nearest VHA facility providing CI care in the contiguous United States. Equal weighting was accorded to people and distance to form an analysis unit of “veteran-miles.” ArcGIS, the mapping tool developed by ESRI, was used to calculate the veteran-miles for each census tract in the continental United States using the list of VHA-based CI comprehensive centers and audiology-only sites. For reporting purposes within the tables and figures, distances calculated from each census tract centroid were summed to the county level. That is, all census tract distances within a county were added to create areas with sufficient size to be seen on a small map of the United States and to create areas of more relatively consistent geographic size.
Results
As of 2017, 48 VHA facilities provided specialized CI care, of which 33 centers offered comprehensive surgical and audiologic CI services and the remaining 15 offered only audiologic services, including evaluation, counseling, and device programming. Nineteen of the facilities providing comprehensive care were located east of the Mississippi River divide and 14 were located west, closely following the country’s overall population statistics.
According to the 2016 American Community Survey, an estimated 19.9 million veterans resided within the continental United States. Of them, an estimated 13.7 million veterans (68.8%) resided more than 40 miles from the nearest VHA facility providing access to CI care, whereas 14.9 million veterans (74.8%) resided more than 40 miles from a comprehensive CI center. For all veterans, the median distance to the nearest VHA facility providing access to CI care was 80.0 miles (interquartile range [IQR], 30.1-140.9 miles). The distribution of distances to the nearest VHA facility providing CI services was strongly right-skewed, with a mean (SD) distance of 100.2 (465.8) miles. Approximately 3.98 million veterans (20.0% of the total) lived more than 160.7 miles from the nearest facility providing any form of CI care. When considering only comprehensive CI centers, the median distance was 101.3 miles (IQR, 39.4-178.7 miles; mean [SD], 126.0 [448.4] miles). In addition, 3.98 million veterans (20.0% of the total) had to travel more than 201.0 miles.
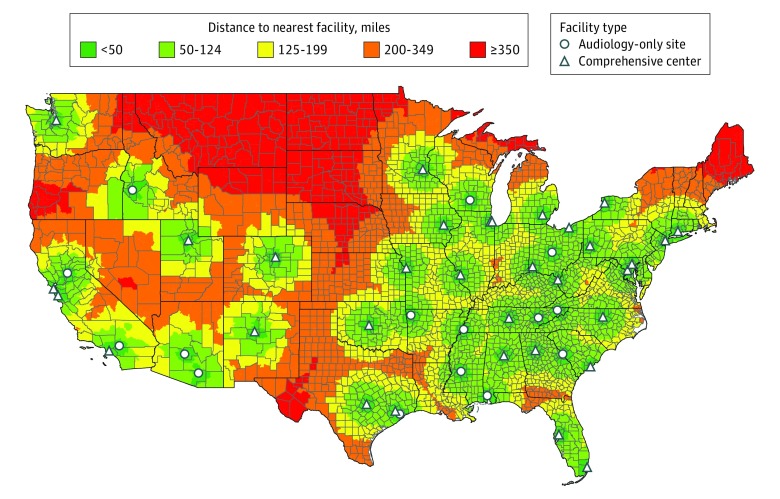
The distance that veterans had to travel to receive CI care varied widely among states. In the well-served states of Connecticut, Maryland, Tennessee, Arizona, and Ohio, 80% of the veterans lived less than 90 miles from a VHA-based CI facility. Eighty percent of the veterans in 31 states lived less than 180 miles from a VHA-based CI facility. In comparison, in 14 states (Idaho, Kansas, Louisiana, Maine, Montana, Nebraska, Nevada, New Hampshire, North Dakota, Oregon, South Dakota, Texas, Vermont, and Wyoming), more than 80% of the veteran population lived more than 90 miles from the nearest VHA facility offering any CI services. In Maine, Montana, North Dakota, South Dakota, Nebraska, Oregon, and Vermont, more than 80% of the veteran population lived more than 180 miles from the nearest VHA facility offering CI services.
Figure 1 shows the straight-line distance to the closest VHA facility providing any form of CI services. The greatest distances are predominantly located in low-density areas, including northern Maine, western Texas, southern Oregon, the upper peninsula of Michigan, the high plains, and the northern Rockies.
Figure 1. Straight-Line Distance to Nearest Veterans Health Administration Cochlear Implant Facility by Census Tract.
States are outlined in black and counties in gray. Distances are calculated from the nearest facility address to each census tract’s geometric centroid. To convert distances to kilometers, multiply miles by 1.6.
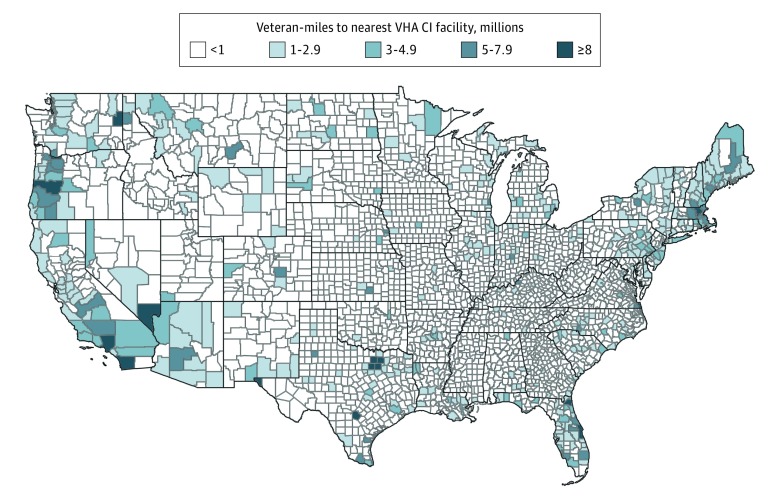
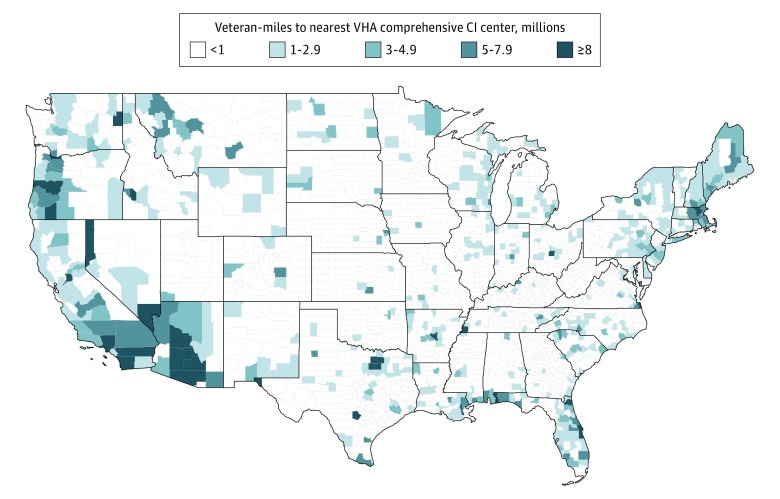
Figure 2 weights the data from Figure 1 according to the number of veterans and the straight-line distance each person must travel to reach the nearest VHA facility providing any form of CI services. Values are weighted as the product of the number of veterans and the number of miles each veteran must travel to obtain care (veteran-miles) to represent the overall burden to access CI services. In this figure, veteran-miles are observed to be generally greatest in large metropolitan areas, such as Los Angeles, California; Dallas-Fort Worth, Texas; and Boston, Massachusetts. However, some less dense areas, such as southern Oregon and northern Maine, are located so far from the nearest facility providing CI services that, despite having lower population densities, these areas still have a considerable need. Figure 3 is similar to Figure 2 but weights the data by the distance to comprehensive CI centers providing surgical CI services.
Figure 2. Population-Weighted Distance to Nearest Veterans Health Administration (VHA) Cochlear Implant (CI) Facility Offering Any Form of CI Services.
Geographic Information System mapping tools (ArcGIS; ESRI) were used to calculate veteran-miles for each census tract. States are outlined in black and counties in gray. To convert distances to kilometers, multiply miles by 1.6.
Figure 3. Population-Weighted Distance to Nearest Veterans Health Administration (VHA)–Based Cochlear Implant (CI) Comprehensive Center Offering Both Surgical and Audiologic CI Services.
Geographic Information System mapping tools (ArcGIS; ESRI) were used to calculate veteran-miles for each census tract. States are outlined in black and counties in gray. To convert distances to kilometers, multiply miles by 1.6.
Table 1 lists the 15 most underserved counties, sorted by veteran-miles, as they relate to access to any type of VHA-based CI care. Overall access for surgical services is considerably poorer given that 15 CI facilities are audiology-only sites (Table 2).
Table 1. Most Underserved Counties Based on Distance From Veterans Health Administration Facilities Offering Cochlear Implant Services.
| Rank | County | State | Veteran-Milesa | No. of Veterans | Metropolitan Statistical Area |
|---|---|---|---|---|---|
| 1 | Clark | Nevada | 34 479 312 | 150 177 | Las Vegas–Henderson–Paradise |
| 2 | Tarrant | Texas | 23 622 475 | 112 758 | Dallas–Fort Worth–Arlington |
| 3 | San Diego | California | 22 854 435 | 233 863 | San Diego–Carlsbad |
| 4 | Dallas | Texas | 21 997 849 | 101 226 | Dallas–Fort Worth–Arlington |
| 5 | Spokane | Washington | 18 339 485 | 44 662 | Spokane–Spokane Valley |
| 6 | Duval | Florida | 15 318 408 | 82 862 | Jacksonville |
| 7 | El Paso | Texas | 13 430 100 | 49 850 | El Paso |
| 8 | Bexar | Texas | 12 399 382 | 153 129 | San Antonio–New Braunfels |
| 9 | Virginia Beach Cityb | Virginia | 11 741 161 | 60 088 | Virginia Beach–Norfolk–Newport News |
| 10 | Middlesex | Massachusetts | 10 745 013 | 67 017 | Boston–Cambridge–Newton |
| 11 | Lane | Oregon | 10 215 475 | 28 683 | Eugene |
| 12 | Los Angeles | California | 9 206 888 | 304 534 | Los Angeles–Long Beach–Anaheim |
| 13 | Collin | Texas | 8 769 290 | 42 388 | Dallas–Fort Worth–Arlington |
| 14 | Multnomah | Oregon | 8 623 619 | 41 730 | Portland–Vancouver–Hillsboro |
| 15 | Denton | Texas | 8 198 796 | 40 841 | Dallas–Fort Worth–Arlington |
For information on how veteran-miles were calculated, see the Methods section.
Virginia Beach City is independent, not belonging to any county.
Table 2. Most Underserved Counties Based on Distance From Veterans Health Administration Comprehensive Cochlear Implant Centers.
| Rank | County | State | Veteran-Milesa | No. of Veterans | Metropolitan Statistical Area |
|---|---|---|---|---|---|
| 1 | Maricopa | Arizona | 104 537 671 | 264 835 | Phoenix–Mesa–Scottsdale |
| 2 | Clark | Nevada | 43 133 998 | 150 177 | Las Vegas–Henderson–Paradise |
| 3 | Pima | Arizona | 32 618 384 | 85 042 | Tucson |
| 4 | San Diego | California | 24 004 039 | 233 863 | San Diego–Carlsbad |
| 5 | Tarrant | Texas | 23 622 475 | 112 758 | Dallas–Fort Worth–Arlington |
| 6 | Dallas | Texas | 21 997 849 | 101 226 | Dallas–Fort Worth–Arlington |
| 7 | Duval | Florida | 15 318 408 | 82 862 | Jacksonville |
| 8 | Spokane | Washington | 15 247 112 | 44 662 | Spokane–Spokane Valley |
| 9 | Shelby | Tennessee | 14 797 932 | 54 847 | Memphis |
| 10 | El Paso | Texas | 13 430 100 | 49 850 | El Paso |
| 11 | Pinal | Arizona | 13 370 154 | 35 005 | Phoenix–Mesa–Scottsdale |
| 12 | Bexar | Texas | 12 399 382 | 153 129 | San Antonio–New Braunfels |
| 13 | Ada | Idaho | 12 202 348 | 29 930 | Boise City |
| 14 | Virginia Beach Cityb | Virginia | 11 741 161 | 60 088 | Virginia Beach–Norfolk–Newport News |
| 15 | Pulaski | Arkansas | 11 061 484 | 30 554 | Little Rock–North Little Rock–Conway |
For information on how veteran-miles were calculated, see the Methods section.
Virginia Beach City is independent, not belonging to any county.
Urban vs Rural
To understand the geographic disparities for veterans residing in urban and rural areas, an additional analysis was performed. Of the 19.9 million veterans residing within the continental United States, 14.7 million (74.0%) lived within defined MSAs. For these veterans, the median distance to a VHA-based CI facility was 61.2 miles (IQR, 23.7-121.3 miles; mean [SD], 83.8 [477.1] miles), and 2.9 million veterans (20.0%) living the farthest within MSAs had to travel more than 140.7 miles. When considering only comprehensive centers, the median distance was 81.9 miles (IQR, 30.9-159.4 miles; mean [SD], 109.3 [460.0] miles), and 2.9 million veterans (20.0%) who lived the farthest had to travel 182.7 miles. Of the 5.2 million veterans (26.0%) living outside the MSAs, the median distance to a facility providing CI services was 119.8 miles (IQR, 79.0-182.4 miles; mean [SD], 146.9 [431.0] miles), with 1.04 million veterans (20.0%) living the farthest having to travel 206.2 miles. When we considered only comprehensive centers for these veterans, the median distance was 143.8 miles (IQR, 92.2-229.3 miles; mean [SD], 173.3 [412.7] miles), with the 1.04 million veterans (20.0%) living the farthest having to travel more than 252.5 miles.
Discussion
Veterans are at high risk for developing hearing loss associated with noise exposure and hence need CIs.12,13 This need has been emphasized by recent findings showing that hearing loss can be correlated with mental health disorders, such as depression14 and anxiety,15 which are high priorities for the VHA.16 Benefits from CIs depend on both surgical care and the ongoing availability of evaluation and programming services by specialized audiologists. In addition, previous work has shown that distance to a VHA facility has a considerable influence on the likelihood of returning for care.17 The results of the present study suggest wide geographic disparities for veterans in access to CI care and provide an argument for the creation of new facilities and development of technologies to assist veterans living far from existing VHA-based CI facilities.
Weighting of Distance vs Population
Neither the number of veterans in a particular location nor their distance to an existing VHA-based CI facility can be used in isolation when considering where services are disproportionally deficient. Here, we chose to balance these 2 variables by weighting the number of veterans and distance in miles equally. In this weighting scheme, 500 veteran-miles equate to 500 veterans having to travel 1 mile for care with 1 veteran having to travel 500 miles for care (Figures 2 and 3). Given this scenario, some areas that appear underserved based on distance alone, such as Portland, Maine, and Duluth, Minnesota (Figure 1), may not seem so deficient once the number of veterans is considered. On the other hand, Los Angeles is shown to have a large need (>8 million veteran-miles), but this need results from the large number of veterans rather than an excessive distance to a VHA-based CI facility. A different ratio may be considered to direct resources according to policy priorities. Prioritizing reduction in distance barriers, for example, may help the veterans who live at exceptional distances, whereas prioritizing efficiency and high throughput may most help those who already live within a short distance of a VHA-based CI facility.
Urban vs Rural
Veterans in rural areas face several geographic barriers to accessing CI care. While there are exceptions (such as some parts of southern Illinois that have access to a large center in St Louis, Missouri), much of the high plains, Rocky Mountain states, and northern border areas, such as the upper peninsula of Michigan and northern Maine, have little access to CI care. These areas correspond to some degree with areas previously identified by the federal government as being medically underserved.18 This status may motivate policy makers to consider CI services along with other medical care that must be improved in these regions of the country. Of note, we found that veterans in many urban centers also lacked access to VHA-based CI facilities. These urban centers included both smaller cities, such as Eugene, Oregon; El Paso, Texas; and Virginia Beach, Virginia, and larger population centers, such as Boston, Massachusetts; Dallas, Texas; Las Vegas, Nevada; and Jacksonville, Florida (none of which have CI centers).
Implications of Data and Considerations for Enacting Policy Changes
In planning how to address the inequities demonstrated here, several variables must be considered. The importance of clinical volume to patient safety and effective outcomes is well recognized,19,20 favoring a few well-placed, high-volume facilities.21 Along similar lines, the cost of setting up a few larger centers with dedicated staff, collaborative training, and shared equipment may be lower than that for several smaller sites.22 It could be argued that facilitating travel from rural areas to existing high-volume centers would be more logical rather than opening new facilities in areas of relatively low population density.
Patients rarely see their surgeons after the immediate perioperative period, whereas audiologic care is required indefinitely. Access to audiology-only sites may remain a more important barrier overall than access to surgical centers. In some areas, such as Tennessee, audiology sites are currently placed to maximize coverage. In other areas, such as Houston, Texas, an audiology site is located quite close to a comprehensive center, leading to a risk of redundancy and reduced efficiency in services and poor coverage elsewhere. Telemedicine, which involves remote or automated programming of implants, is gaining interest among patients and providers23 because the number of audiologists able to program implants is not necessarily able to care for an increasing number of implantees.24 Future deployment of this technology in VHA-based CI facilities will help minimize the burden of the geographic barriers identified in this study.
The Veterans Choice Program was instituted in 2014 to decrease wait times and travel burden for veterans who cannot be offered an appointment within 30 days or who reside 40 miles or more from a VHA facility. This program includes coverage for CI services at non-VHA facilities. However, there are multiple reasons why the Veterans Choice Program may not be used for cochlear implantation even when a veteran meets the distance criterion. Cochlear implantation requires significant coordination of care among audiologists identifying potential candidates and implant surgeons. This team approach requires ease of communication, which is difficult to coordinate between a VHA audiologist and an outside surgeon. When a center provides only audiologic services, it is easier for the audiologist to coordinate care with the nearest comprehensive VHA implant center rather than establish communication with an implant surgeon in the community because of Health Insurance Portability and Accountability Act (HIPPA) compliance issues and differences in the electronic medical record. This communication gap could also affect the need for coordinating the ordering of devices (done through the VHA) for use in an outside facility and for providing the indefinite audiology follow-up services that implantees require. Last, non–VHA-based CI programs may not always be able to accommodate a patient for assessment of candidacy more quickly than the nearest VHA center. The data collected here can help optimize use of the Veterans Choice Program in areas identified as posing a particularly high risk of access issues.
Limitations
The specific results of this study depend on several assumptions. We used absolute distance as a measure of accessibility, whereas the actual travel time would be another possible measure, as was done previously when access to care was studied among veterans with multiple sclerosis.8 Programs such as the Veterans Transportation Service and VHA-sponsored lodging may make care relatively easier to access for some veterans despite living at a long distance from medical care facilities. We also included veterans living at any distance from a CI facility, although previous work has suggested that a distance less than 30 miles or 30 minutes offers essentially a negligible barrier to accessing care.25,26 A distance threshold such as this could be considered in future analyses to underscore the true burden of distance on an individual level. Distances to facilities with particular characteristics, such as wait times, device types offered, clinician experience, surgical outcomes (eg, hearing preservation rates), audiologic outcomes, and availability of vestibular diagnostics, could be considered separately in future analyses.
We also assumed that the prevalence of severe to profound hearing loss among veterans is comparable to that of the general population, as has been previously reported in a cohort of veterans.13 However, a different estimate was made by the Centers for Disease Control and Prevention, which suggested that veterans are 30% more likely than nonveterans to have severe hearing impairment after adjustment for age and current occupation.27 Our analysis likely underestimates the true burden of hearing loss among veterans.
Conclusions
This study contributes to existing literature examining access to health care as a function of distance by using modern GIS technology.7,8,28 This tool enables visualization of large amounts of spatial information with high granularity, which allows policy makers, health care professionals, and patients to have optimal insights into the current state of care, identify areas that require improvement, and follow changes over time.28 An analysis similar to the one performed here could also be applied to civilian access to CI care, in which other important variables, such as availability of pediatric audiologic and anesthesiology services, could be considered. However, many more civilian CI facilities are available; consequently, the geographic barriers to access described here may not extrapolate accurately to nonveterans.
References
- 1.US Department of Veterans Affairs Planning and operating outpatient sites of care. VHA Directive 1229. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5439. Published July 7, 2017. Accessed February 5, 2019.
- 2.O’Donoghue G. Cochlear implants—science, serendipity, and success. N Engl J Med. 2013;369(13):1190-1193. doi: 10.1056/NEJMp1310111 [DOI] [PubMed] [Google Scholar]
- 3.Adunka OF, Gantz BJ, Dunn C, Gurgel RK, Buchman CA. Minimum reporting standards for adult cochlear implantation. Otolaryngol Head Neck Surg. 2018;159(2):215-219. doi: 10.1177/0194599818764329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Department of Veterans Affairs; Veterans Benefits Administration Compensation. https://www.benefits.va.gov/REPORTS/abr/docs/FY17-Compensation.pdf. Published 2018. Accessed February 13, 2019.
- 5.Penn M, Bhatnagar S, Kuy S, et al. . Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs Medical Centers. JAMA Netw Open. 2019;2(1):e187096. doi: 10.1001/jamanetworkopen.2018.7096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helfand M; VA Evidence Synthesis Program. An evidence-based wait time threshold. https://www.hsrd.research.va.gov/publications/esp/WaitTimesMemo.pdf. Published August 2014. Accessed May 16, 2019.
- 7.Goldberg DS, French B, Forde KA, et al. . Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014;311(12):1234-1243. doi: 10.1001/jama.2014.2520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Culpepper WJ II, Cowper-Ripley D, Litt ER, McDowell TY, Hoffman PM. Using geographic information system tools to improve access to MS specialty care in Veterans Health Administration. J Rehabil Res Dev. 2010;47(6):583-591. doi: 10.1682/JRRD.2009.10.0173 [DOI] [PubMed] [Google Scholar]
- 9.Sorkin DL. Access to cochlear implantation. Cochlear Implants Int. 2013;14(suppl 1):S1. doi: 10.1179/1467010013Z.00000000081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States Census Bureau 2016 American Community Survey. American fact finder. https://www.census.gov/programs-surveys/acs/data.html. Published 2016. Accessed February 20, 2017.
- 11.Office of Information and Regulatory Affairs 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas. Washington DC: Office of Information & Regulatory Affairs; 2010:37252. [Google Scholar]
- 12.Theodoroff SM, Lewis MS, Folmer RL, Henry JA, Carlson KF. Hearing impairment and tinnitus: prevalence, risk factors, and outcomes in US service members and veterans deployed to the Iraq and Afghanistan wars. Epidemiol Rev. 2015;37(1):71-85. doi: 10.1093/epirev/mxu005 [DOI] [PubMed] [Google Scholar]
- 13.Wilson RH, Noe CM, Cruickshanks KJ, Wiley TL, Nondahl DM. Prevalence and degree of hearing loss among males in Beaver Dam cohort: comparison of veterans and nonveterans. J Rehabil Res Dev. 2010;47(6):505-520. doi: 10.1682/JRRD.2009.10.0169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li CM, Zhang X, Hoffman HJ, Cotch MF, Themann CL, Wilson MR. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005-2010. JAMA Otolaryngol Head Neck Surg. 2014;140(4):293-302. doi: 10.1001/jamaoto.2014.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carmen R, Uram S. Hearing loss and anxiety in adults. Hear J. 2002;55(4):48,50,52-54. doi: 10.1097/01.HJ.0000293358.79452.49 [DOI] [Google Scholar]
- 16.Blazer DG, Gray BH, eds. Evaluation of the Department of Veterans Affairs Mental Health Services. Washington, DC: National Academies Press; 2018. doi: 10.17226/24915 [DOI] [PubMed] [Google Scholar]
- 17.Elnitsky CA, Andresen EM, Clark ME, McGarity S, Hall CG, Kerns RD. Access to the US Department of Veterans Affairs health system: self-reported barriers to care among returnees of Operations Enduring Freedom and Iraqi Freedom. BMC Health Serv Res. 2013;13:498. doi: 10.1186/1472-6963-13-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health Resources and Services Administration Medically underserved areas and populations (MUA/Ps). https://bhw.hrsa.gov/shortage-designation/muap. Updated October 2016. Accessed February 5, 2019.
- 19.Morche J, Mathes T, Pieper D. Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. 2016;5(1):204. doi: 10.1186/s13643-016-0376-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pagedar NA. Surgical volumes and outcomes—does practice make perfect? JAMA Otolaryngol Head Neck Surg. 2019;145(1):70-71. doi: 10.1001/jamaoto.2018.3171 [DOI] [PubMed] [Google Scholar]
- 21.Vila PM, Hullar TE, Buchman CA, Lieu JEC. Is there a need for performance measures for cochlear implant centers? Otolaryngol Head Neck Surg. 2015;153(4):484-487. doi: 10.1177/0194599815575006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crowson MG, Chen JM, Tucci D. Provincial variation of cochlear implantation surgical volumes and cost in Canada. Otolaryngol Head Neck Surg. 2017;156(1):137-143. doi: 10.1177/0194599816668325 [DOI] [PubMed] [Google Scholar]
- 23.Bush ML, Sprang R. Management of hearing loss through telemedicine. JAMA Otolaryngol Head Neck Surg. 2019;145(3):204-205. doi: 10.1001/jamaoto.2018.3885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization Multi-country assessment of national capacity to provide hearing care. https://www.who.int/pbd/publications/WHOReportHearingCare_Englishweb.pdf. Published 2013. Accessed February 5, 2019.
- 25.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976-993. doi: 10.1007/s10900-013-9681-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Probst JC, Laditka SB, Wang JY, Johnson AO. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC Health Serv Res. 2007;7:40. doi: 10.1186/1472-6963-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Groenewold MR, Tak S, Masterson E; Centers for Disease Control and Prevention (CDC) . Severe hearing impairment among military veterans—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60(28):955-958. [PubMed] [Google Scholar]
- 28.Bearak JM, Burke KL, Jones RK. Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. Lancet Public Health. 2017;2(11):e493-e500. doi: 10.1016/S2468-2667(17)30158-5 [DOI] [PMC free article] [PubMed] [Google Scholar]