Abstract
Objective:
Mindfulness interventions have been shown to reduce stress; however, the mechanisms driving stress resilience effects are not known. Mindfulness interventions aim to teach individuals how to: (i) use attention to monitor present moment experiences; with (ii) an attitude of acceptance and equanimity. A randomized controlled dismantling trial (RCT) was conducted to test the prediction that the removal of acceptance skills training would eliminate stress-reduction benefits of a mindfulness intervention.
Methods:
This pre-registered RCT randomly assigned stressed community adults to one of three conditions: (i) Monitor & Accept (MA) mindfulness training, a standard 8-week MBSR intervention that provided explicit instruction in developing both monitoring and acceptance skills; (ii) Monitor Only (MO) mindfulness training, a well-matched 8-week MBSR intervention that taught monitoring skills only; or (iii) No Treatment (NT) control. Stress and non-judgment were measured using ecological momentary assessment (EMA) for three days at baseline and three days at post-intervention.
Results:
Consistent with predictions, MA participants increased in non-judgment and decreased in both stress ratings and the proportion of assessments that they reported experiencing feelings of stress in daily life, relative to both MO and NT participants.
Conclusions:
This RCT provides one of the first experimental tests of the mechanisms linking mindfulness interventions with stress resilience. These findings suggest that acceptance skills training may be a necessary active ingredient and support the value of integrating acceptance skills training into stress-reduction interventions.
Trial registration:
clinicaltrials.gov; Identifier:
Keywords: mindfulness, stress, ecological momentary assessment (EMA), randomized controlled trial (RCT), acceptance
There has been a dramatic increase in research examining mindfulness training programs over the past twenty years. Over 350 mindfulness randomized controlled trials (RCTs) have been published in the previous decade alone (2006–2016; Creswell, 2017). One possible reason for this widespread interest is that mindfulness interventions have shown promise for improving a broad range of mental and physical health outcomes (Creswell, 2017; Kuyken et al., 2016; Ludwig & Kabat-Zinn, 2008). One pathway through which mindfulness interventions are thought to produce these salutary effects is by buffering individuals against the negative consequences of stress (Creswell & Lindsay, 2014). Consistent with this possibility, mindfulness interventions such as the Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990) program have consistently been shown to decrease self-reported distress and stress post-intervention (meta-analysis by Khoury, Sharma, Rush, & Fournier, 2015). Despite this evidence, the active mechanisms for these effects are not known. It is possible that the stress-reducing benefits are driven by the training of specific psychological skills taught in mindfulness interventions. If this were the case, removing the training of these critical skills from mindfulness interventions would either attenuate or altogether eliminate stress reduction benefits. Here we report the results of a randomized controlled dismantling trial explicitly testing active psychological mechanisms of mindfulness interventions for reducing stress, measured using ecological momentary assessment (EMA) in daily life. Participants were randomly assigned to complete either: (i) a full 8-week MBSR training program that taught the standard combination of monitoring and acceptance skills; or (ii) a modified but structurally equivalent MBSR intervention that removed acceptance skills training and taught attention monitoring skills only.
Mindfulness is commonly described as the act of purposefully attending to the present moment experience with an attitude of acceptance and equanimity (Kabat-Zinn, 2009). Most mindfulness definitions used in contemporary empirical research contexts include two components: (i) intentionally guided attention to monitor present moment experiences; and (ii) adopting an attitude of acceptance toward these experiences. Monitor and Acceptance Theory (MAT) is one recent mechanistic account of mindfulness training which posits that both attention monitoring and acceptance skills play important roles in improving a broad range of outcomes in mindfulness training interventions (Lindsay & Creswell, 2017). Specifically, this account suggests that acceptance is an emotion regulation skill that fosters non-reactivity and openness to present moment experiences, and that the removal of acceptance skills training may eliminate the stress-buffering benefits of mindfulness interventions. Based on experimental evidence from an initial smartphone-based dismantling trial showing that acceptance skills training is necessary for reducing reactivity to a laboratory stress challenge (Lindsay, Young, Smyth, Brown, & Creswell, 2018), it was hypothesized that removing acceptance skills training from a mindfulness intervention would attenuate or eliminate reductions in stress during daily life measured using EMA.
EMA is particularly well-suited to study dynamic processes such as stress in daily life (Smyth & Stone, 2003) and provides several advantages compared to traditional recall-based measures. Compared to such measures, EMA is thought to minimize recall bias and maximize ecological validity (Shiffman, Stone, & Hufford, 2008). EMA measures have, at least in some contexts, also been shown to be more predictive of future outcomes than recall-based questionnaire measures (e.g., Kamarck, Muldoon, Shiffman, & Sutton-Tyrrell, 2007). EMA measures may also be more sensitive to training-related changes. For example, one study found that EMA measures provided greater sensitivity than questionnaire measures to detect changes in depression and anxiety symptoms following an 8-week MBSR intervention (Moore, Depp, Wetherell, & Lenze, 2016).
The primary aim of this RCT was to test theory-guided predictions about whether the removal of acceptance skills training attenuates or eliminates the stress-buffering benefits of an 8-week MBSR intervention (Lindsay & Creswell, 2017). This study experimentally manipulated whether participants learned both monitoring and acceptance skills or monitoring skills only, with the aim of testing whether removing acceptance skills training attenuated the stress buffering benefits of mindfulness interventions. To do this, stressed community adults were randomly assigned to one of three conditions: (i) Monitor & Accept (MA) training; (ii) Monitor Only (MO) training; or (iii) a no treatment (NT) control condition. Stress was assessed five times daily on three consecutive days at both baseline and post-intervention using EMA. The primary pre-registered hypothesis for this study was that 8-week MA training would reduce psychological stress during daily life compared to both MO training and NT control. To test this, participants (i) rated their momentary level of stress at each assessment and (ii) indicated whether or not they had experienced any feelings of stress since completing the previous assessment. Finally, the MAT account posits that acceptance skills training can increase non-judgment toward one’s momentary experiences. As a manipulation check for the experimental dismantling approach used in this study, participants provided momentary ratings of the degree to which they had been judging the self, thoughts and feelings, momentary experiences, and other people. It was predicted, as a secondary hypothesis, that MA training would increase daily life non-judgmental perceptions compared to MO training and NT control.
Methods
Participants.
Participants were 137 stressed community adults between the ages of 18–67 (M=37 years1, SD=13.4). The sample was 67.2% female, 66.4% white, 15.3% African-American, 10.2% Asian, and 8.0% other ethnicities. Recruitment was conducted via participant registries, community advertisements, and mass emails to local organizations for a study testing 8-week training programs for stress reduction and well-being. Eligible participants were fluent English-speaking smartphone owners (Android or iPhone) between the age of 18–70 years in good mental and physical health, who scored >5 on the 4-item Perceived Stress Scale2 (S. Cohen & Williamson, 1988; Sheldon Cohen, Kamarck, & Mermelstein, 1983). Participant exclusion criteria included: chronic mental or physical disease; hospitalization in the past 3 months; medication use that interferes with HPA axis or immune system functioning; current oral contraceptive use; current pregnancy; current antibiotic, antiviral, or antimicrobial treatment; recreational drug use or excessive alcohol or tobacco use; and travel to countries on the CDC travel alert list in the past 6 months. Finally, individuals with significant experience with or daily practice of mindfulness meditation or related mind-body practices (defined as >2 times per week or >90 minutes of weekly practice) were also excluded. All participants provided written informed consent and all study procedures were approved by the Carnegie Mellon University IRB. Study data were collected at Carnegie Mellon University in Pittsburgh, Pennsylvania between August 2015 and November 2016. Recruitment was halted once the target sample size had been reached.
G*Power was used to calculate an a priori target sample size needed to test primary study aims. These calculations were based upon previous 8-week mindfulness intervention studies typically demonstrating medium-large effect sizes (~η2=.06-.18) for both daily stress and stress-reactivity outcomes relative to no treatment (e.g., Creswell, Pacilio, Lindsay, & Brown, 2014). Using a two-tailed Type I error rate of .05, a desired power of .90, an estimated ICC for time of .6, and a design of 3 groups measured at 2 time points, the required calculated sample size for an omnibus test of primary study aims was 120.
Intervention Programs.
Participants were randomly assigned to one of three study conditions: (i) 8-week Monitor & Acceptance (MA) MBSR training program; (ii) 8-week Monitor Only (MO) adapted-MBSR training program; or (iii) No Treatment control group (NT). Briefly, MBSR is a standardized group-based program consisting of 8 weekly 2.5–3-hour sessions, 1 day-long retreat during the sixth week, and approximately 45-minutes of daily home practice of meditation and informal mindfulness in daily life (Kabat-Zinn, 1990). The MA program adhered to the standard MBSR curriculum although the length of the sessions was shortened to 2 hours. The MO program, which also included 2 hour sessions, adapted MBSR by emphasizing the concentration/observing aspects of MBSR and removing acceptance/non-judgment language and practices. The MA and MO programs were taught in counterbalanced order by a certified MBSR instructor and a qualified MBSR instructor, both of whom had completed teacher trainings through the UMass Center for Mindfulness. The MO program was adapted from standard MBSR curriculum by c-authors in consultation with a former senior teacher at the UMass Center for Mindfulness (see Author Contributions and Acknowledgements) along with supporting mindfulness training sources (e.g., Foust, 2014; Goenka, 1994; Trungpa, 2003). The NT control group received minimal contact from study personnel during the intervention period, and completed all other study activities and assessments.
Monitor & Accept (MA; Standard MBSR program).
During each group session, an MBSR instructor leads guided mindfulness meditations intended to help foster the ability to come into direct contact with, and monitor one’s current body sensations, mental images, emotions, and thoughts with an accepting, allowing attitude. As the sessions proceed, participants are invited to acknowledge their habitual reactions to stressful situations, eventually discovering that mindful awareness allows for additional choices in response to stress. Acceptance, or a non-judgmental, matter-of-fact attitude, is encouraged in the MA condition only. All class sessions and home practice audios include instructions for focusing and returning attention using language that encourages a gentle and accepting attitude towards sensory experiences and the fact that human minds wander. This attitudinal quality was also reinforced during instructor-led class discussions. Monitoring, or focusing and returning attention, is also included in the MA training program because developing this skill is an important early building block for learning to meditate. During class activities, MA participants are encouraged to “invite in” experiences with curiosity and interest, and to adopt a non-judgmental and accepting attitude towards their monitored experiences regardless of whether they are positive, negative, or neutral. Participants attend a seven-hour retreat during the sixth week of MBSR that is focused on integrating and elaborating upon the mindfulness skills learned throughout the course. Finally, participants are asked to complete approximately 40–45-minutes of daily home practice six days per week during the eight-week course (4.0–4.5 hours of practice per week). Daily home practice consists of recordings from the classroom instructor guiding participants through meditations such as body scanning, mindful movement, and sitting meditation, as well as informal mindfulness practice during daily life.
Monitor Only (MO; Adapted MBSR).
Monitoring, or training to sense into and observe one’s experience, is explicitly taught in standard MBSR and in the MO condition of this project. Participants are taught to focus their attention on an aspect of their present moment experience, such as sensations of breathing or other body sensations. They are asked to notice when their attention wanders and return it to the direct perception of the focal sensory object, and to monitor their present moment experiences during guided activities. The MO adaptations of the MBSR program primarily consisted of 1) changes in language, and 2) emphasizing concentration practices, specifically regarding body awareness. Changes in language included avoiding use of the words: accept, acceptance, allow, being with, letting go of judgment, non-judgment, and instead referring to: direct perception, observe, monitor, return to the anchor (e.g., of breath sensation). Thus, acceptance language was not included in the MO class instruction or home practice audios, and was also avoided by the instructor as much as possible during group discussions. The MO program emphasized concentration and attention monitoring. One such practice consisted of anchoring attention to breath or other body sensation or sound in order to return to present moment experience. The MO program did not include some meditative practices that are typically included in standard MBSR, such as open awareness meditation without a focal object. Like MA, MO participants completed a retreat day and the same amount of guided home practice. As a conservative test of study hypotheses, it is important to note that although the language and practices associated with acceptance were excised as much as was possible from MO, the teachers still embodied the acceptance and inclusion that are considered essential to cultivating a safe and effective learning environment for participants in the MBSR program. Moreover, focusing and returning attention can result in a greater sense of clarity and reduced distraction and distress, so it is also possible that some participants developed a more accepting attitude over time on their own as they continued to practice MO meditation.
Measures.
Stress and non-judgmental perceptions were assessed via signal-prompted assessment five times daily for three days at baseline and three days post-intervention. To assess stress, participants were asked to indicate how much stress they were experiencing or feeling right now on a seven-point Likert scale with anchors at 1 (mild), 4 (moderate), and 7 (severe). To assess occasions stressed, participants were also asked to provide a yes/no response to indicate whether they had experienced stress in the time since they completed the previous assessment. Items assessing stress and occasions stressed were adapted from previously published studies (e.g., Neubauer, Smyth, & Sliwinski, 2018; Smyth & Heron, 2016). To assess perceptions of non-judgment, participants were asked to indicate the degree to which they agreed that they had been judging as good or bad each of four domains since the previous assessment: (i) themselves; (ii) their thoughts and feelings; (iii) situations they were in or events that occurred; and (iv) other people they interacted with or thought about, on a six-point scale from 1 (strongly disagree) to 6 (strongly agree). Items assessing perceptions of non-judgment were adapted from existing trait mindfulness and acceptance scales (e.g., Baer, Smith, & Allen, 2004; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). These items were intended to measure nonjudgment as conceptualized in the mindfulness literature. Responses to all four items were reverse scored such that higher values indicated greater non-judgment and were averaged to create a single value representing overall non-judgment (α=.883).
Participants assigned to either the MA or MO MBSR conditions (n=107) completed the 6-item Credibility/Expectancy Questionnaire (CEQ; Devilly & Borkovec, 2000) which asked participants to rate the degree to which they believed the MBSR classes would be beneficial. This measure was included to ensure that any differences in how MA and MO training affected stress and non-judgmental perceptions were not due to differences in positive treatment expectancies (i.e., placebo effects). Responses across all six items were averaged to create a single value representing treatment expectancies (α=.912).
Procedures.
This study was a three-arm randomized controlled trial preregistered with Clinical Trials identifier NCT02502227. This manuscript reports pre-registered primary (daily life stress assessed using EMA), secondary (daily life state acceptance assessed using EMA), and other (treatment expectancies) outcome measures from this trial. All outcome measures reported here remained unanalyzed until data collection was complete.
Interested participants were screened for eligibility both via telephone and at an in-person baseline appointment by trained research assistants and staff. During this baseline appointment, eligible participants provided a dried blood spot (DBS) sample, completed a questionnaire and task battery, and were oriented to the study’s schedule and activities. Participants then completed three consecutive days of pre-intervention EMA and daily diary assessments. Next, participants were randomized into one of three study conditions using a random number generator in a 3–3-2 randomization sequence generated by a study statistician who was not involved with participant enrollment (for every 8 participants randomized, 3 were assigned to Monitor & Accept, 3 to Monitor Only, 2 to No Treatment). To maintain allocation concealment, only essential study personnel (e.g., the MBSR instructors) had knowledge of participant allocation and all assessors were blind to condition assignment. Following the 8-week intervention period, participants completed three consecutive days of post-intervention EMA and diary assessments before returning to the laboratory for a post-intervention appointment. At this appointment, condition-blind research staff directed participants as they provided a DBS sample and completed a questionnaire and task battery. Finally, all participants were debriefed, informed of the study’s primary aims, and compensated for their participation.
Ecological Momentary Assessment.
EMA surveys were administered using participants’ personal smartphones using Qualtrics surveys delivered through SurveySignal text links and MetricWire surveys. Participants were prompted to complete five EMA surveys daily at quasi-random times each day (30 surveys total across the baseline and post-intervention periods). Text links were sent during each of five 2-hour blocks distributed between 9:00 am and 7:00 pm, with links expiring after 45 minutes. Although not reported here, participants were also prompted to complete daily diary assessments at 8:30 pm each day (6 daily diary assessments total across the baseline and post-intervention periods); links were sent at exactly 8:30 pm and remained active until 11:30 pm. Participants were trained to complete all EMA assessments during the baseline study appointment. To encourage adherence, participants received $60 base compensation plus an additional maximum of $40 for compliance with the EMA protocols. At both baseline and post-intervention, EMA assessments began on a Wednesday and concluded on a Friday.
Data Analysis.
Mixed models were used as a primary data analytic approach, given that they model all available data and follow intention-to-treat principles4. Specifically, 3-level multilevel models nesting EMA observations (Level-1) within days (Level-2) within individuals (Level-3) were used to test for Time x Condition differences using the mixed command in Stata software (Version 15.1, StataCorp, College Station, Texas). For the dichotomous outcome (occasions stressed), identical 3-level models were tested using Stata’s melogit command. All multilevel mixed effect linear regressions used restricted maximum likelihood estimation with an identity covariance matrix. The multilevel logistic regression used an unstructured random-effects covariance matrix. Time, condition, the time × condition interaction, and observation number within day were modeled as fixed effects. Random intercepts were included in the model for both participant and day of assessment. The use of multilevel models in this analytic approach is considered optimal because they provide relatively unbiased model estimates that account for missing data (Allison, 2012).
Although multilevel models in longitudinal studies typically include an autoregressive term (ρ) to account for serial autocorrelation between proximal observations, this could not be done here because the continuous term for time since study entry was collinear with the categorical predictor for time (baseline, post-intervention). Instead, 3-level models nesting observations within day of assessment (coded 0–2) were used to account for autocorrelation between consecutive measurements. To further account for potential autocorrelation, a fixed- effect term was included in the model for observation number within day (coded 0–4). Examining the residuals produced from these models indicated that these steps successfully detrended the data.
Results
Preliminary Analysis
Of the 137 randomized participants, 125 completed the post-intervention assessment, and 125 completed at least one post-intervention EMA survey (see CONSORT flow chart in Figure 1). Of the 107 individuals assigned to one of the 8-week MBSR classes, 98 completed the intervention (91.6%). Success of randomization on major demographic characteristics in the full randomized sample (N=137) was evaluated. There were no baseline differences across conditions in age, sex, race, or education (see Table 1). There were also no condition differences in compliance with EMA protocols at baseline. Among the 125 participants who completed post-intervention EMA, there were also no condition differences in adherence to the EMA protocol at post-intervention. Overall, participants completed 69.2% of all possible EMA surveys across baseline and post-intervention.
Figure 1.
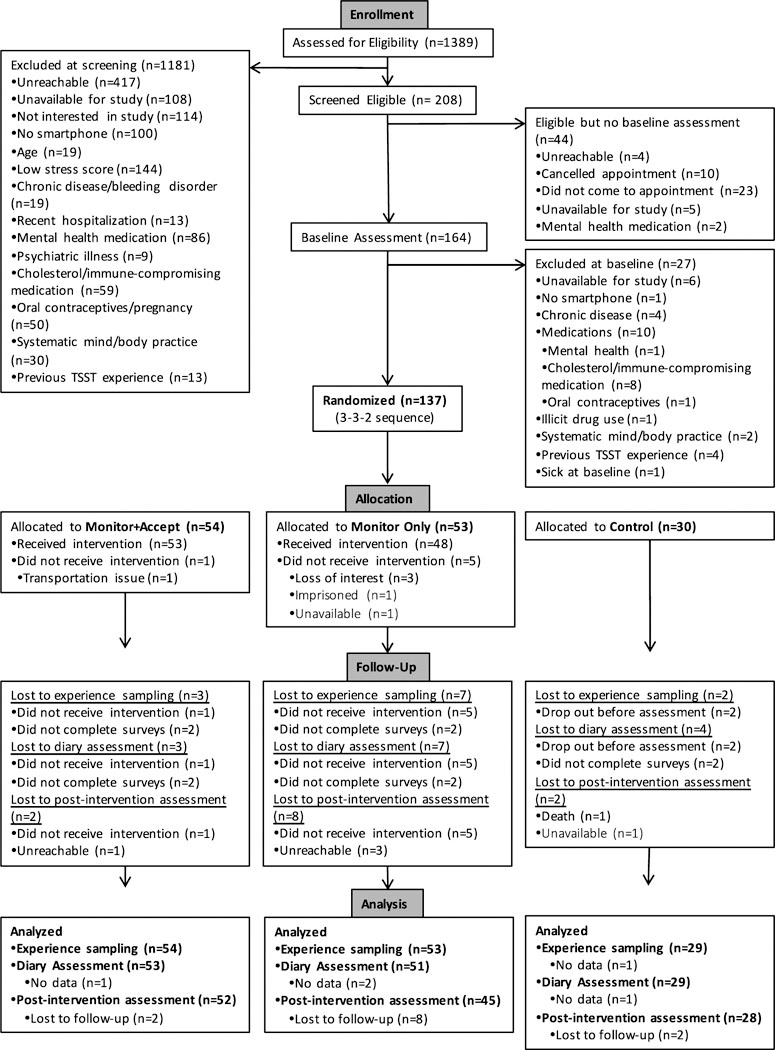
CONSORT Flow Chart
Table 1.
Baseline characteristics of participants (N=137) by study condition
| Characteristic | Full Sample (N=137)a |
Monitor + Accept (N=54) |
Monitor Only (N=53) |
No Treatment (N=30) |
Condition Difference |
|---|---|---|---|---|---|
| Age in yearsb | 37.68 (13.43) | 36.02 (14.40) | 37.58 (12.60) | 40.83 (13.00) | F(2,133)=1.25 |
| Sex | χ2(2)=0.96 | ||||
| Female | 92 (67.15%) | 34 (62.96%) | 36 (67.92%) | 22 (73.33%) | |
| Male | 45 (32.85%) | 20 (37.04%) | 17 (32.08%) | 8 (26.67%) | |
| Race | χ2(8)=7.56 | ||||
| American Indian/Alaska Native | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (00.0%) | |
| Asian | 14 (10.22%) | 7 (12.96%) | 6 (11.32%) | 1 (3.33%) | |
| Black/African American | 21 (15.33%) | 10 (18.52%) | 7 (13.21%) | 4 (13.33%) | |
| White/Caucasian | 91 (66.42%) | 33 (61.11%) | 36 (67.92%) | 22 (73.33%) | |
| Bi- or Multi-Racial | 6 (4.38%) | 2 (3.70%) | 1 (1.89%) | 3 (10.00%) | |
| Other | 5 (3.65%) | 2 (3.70%) | 3 (5.66%) | 0 (0.00%) | |
| Ethnicityc | χ2(2)=1.70 | ||||
| Not Hispanic or Latino | 130 (95.59%) | 3 (5.56%) | 3 (5.66%) | 0 (0.00%) | |
| Hispanic or Latino | 6 (4.41%) | 51 (94.44%) | 50 (94.34%) | 29 (96.67%) | |
| Education Level | χ2(16)= 11.18 | ||||
| No High School Diploma | 1 (0.73%) | 0 (0.00%) | 1 (1.89%) | 0 (0.00%) | |
| GED | 2 (1.46%) | 1 (1.85%) | 1 (1.89%) | 0 (0.00%) | |
| High School Diploma | 10 (7.30%) | 4 (7.41%) | 3 (5.66%) | 3 (10.00%) | |
| Technical Training | 2 (1.46%) | 0 (0.00%) | 1 (1.89%) | 1 (3.33%) | |
| Some College, no degree | 18 (13.14%) | 9 (16.67%) | 4 (7.55%) | 5 (16.67%) | |
| Associate Degree | 10 (7.30%) | 3 (5.56%) | 5 (9.43%) | 2 (6.67%) | |
| Bachelor’s Degree | 41 (29.93%) | 19 (35.19%) | 17 (32.08%) | 5 (16.67%) | |
| Master’s Degree | 40 (29.20%) | 12 (22.22%) | 17 (32.08%) | 11 (36.67%) | |
| MD, PhD, JD, PharmD | 13 (9.49%) | 6 (11.11%) | 4 (7.55%) | 3 (10.00%) | |
Note: Data are reported as means (SD) or percentages (%).
Of the 137 participants randomized, 12 did not complete the post-intervention assessment (8.8%). Those who dropped out did not differ in age (F(1,134)=0.20,p=.652), sex (χ2(1)=0.46, p=.496), race (χ2(4)=5.62,p=.229), or ethnicity (χ2(1)=0.48, p=.488). However, dropouts were more likely to have lower educational attainment (χ2(8)=21.25, p=.007).
Age missing from one participant in the Monitor Only condition (N= 136).
Ethnicity missing from one participant in the No Treatment condition (N=136).
p<.05
Next, condition differences in treatment expectancies at Week 1, Week 4, and Week 8 of the intervention were tested using all available data from individuals assigned to one of the two study interventions (n=107). There were no differences between the two training conditions in positive treatment expectancies at any time (all ps>.53). Finally, condition differences in treatment adherence were tested among the 98 individuals who completed their assigned intervention. There were no differences between the two training conditions in the number of classes attended. There was also no difference between the two training conditions in number of minutes of home practice5 (F(1,96)=2.97, p=.088) or number of home practice sessions (F(1,96)=1.72, p=.193). On average, MA participants completed 13.57 hours of home practice (SD=7.97; range: 0–29.94) across 27.1 sessions (SD=10.9, range: 0–42) whereas MO participants completed 10.72 hours of practice (SD=8.41; range: 0.02–26.31 hours) across 24.2 sessions (SD=10.5, range: 2–41) during the eight week intervention. However, adding minutes of home practice as a person-level covariate (with a value of zero for NT participants) to all primary analyses did not appreciably change any of the reported results. Moreover, minutes of home practice were not associated with baseline to post-intervention changes in momentary stress (MA: b=−.099, SE<001, p=.501; MO: b=−.057, SE<001, p=.712) or non-judgment (MA: b=.006, SE<001, p=.970; MO: b=.086, SE<.001, p=.577). Finally, there were also no baseline differences across conditions for any study outcome reported below (all ps>.20) indicating successful randomization.
Condition differences in change in non-judgment over time were examined as a manipulation check for the experimental dismantling approach used in this study. It was hypothesized that MA training would increase non-judgment relative to both MO training and NT control. To test this hypothesis, 3-level MLMs were used to evaluate the hypothesized time by condition interaction. There was no main effect of condition (χ2(2)=4.90, p=.0865) but there was a main effect of time (χ2(1)=255.50, p<.0001). Consistent with predictions, this was qualified by an interaction between time and condition (χ2(2)=30.82, p<.0001). Participants across all conditions showed an increase in daily life non-judgmental perceptions from baseline to post-intervention (MA: 3.83(12) to 4.58(.12), d=88; MO: 3.64(.12) to 4.25(.12), d=73; NT: 3.65(.17) to 3.92(.16), d=.31); however as predicted, this increase was significantly greater for MA participants compared to both MO (χ2(1)=4.40, p=.0360, d=.16) and NT participants (χ2(1)=30.82,p<.0001, d=. 56). This increase was also significantly greater for MO participants compared to NT participants (χ2(1)=14.25, p=.0002, d=.39).
EMA Stress
Stress Ratings.
It was hypothesized that MA participants would have greater reductions in momentary stress than MO or NT participants. To test this hypothesis, 3-level MLMs were used to evaluate the hypothesized time by condition interaction. There were main effects of condition (χ2(2)=6.72, p=.0347) and time (χ2(1)=128.12, p<.0001). Consistent with predictions, these effects were qualified by an interaction between time and condition (χ2(2)=9.89, p=.0071) (see Figure 2). Although participants across all conditions showed a decrease in stress ratings from baseline to post-intervention (MA mean change = .85, p<.0001, d=.85; MO mean change = .58, p<.0001, d=.59; NT mean change = .45, p<.0001, d=.44), this decrease was significantly greater for MA participants compared to both MO (χ2(1)=5.57,p=.0183, d=.27) and NT participants (χ2(1)=7.91, p=.0049, d=.40). There was no difference in stress reduction over time between MO and NT participants (χ2(1)=0.79, p=.3741, d=.13). (See Table 2 for condition means).
Figure 2.
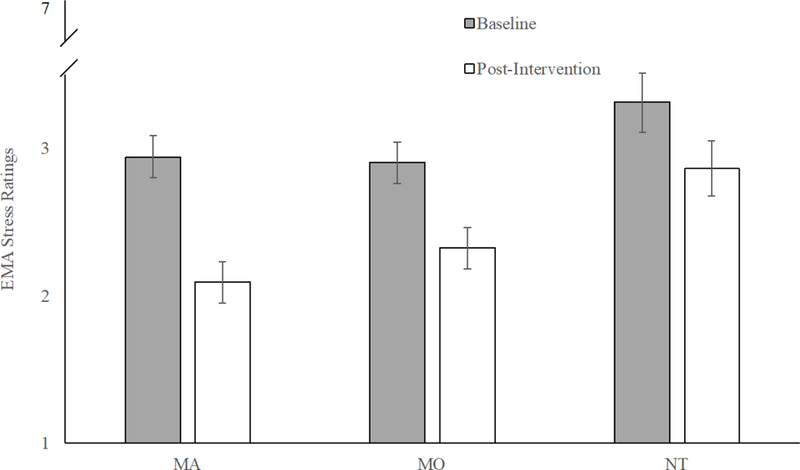
EMA stress ratings at baseline and post-intervention by study condition
Table 2.
Primary study outcomes at baseline and post-intervention by study condition
| Monitor + Accept | Monitor Only | No Treatment Control | Time x | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | (Pre and Post N=51) | (Pre N=51; Post N=46) | (Pre N=26;Post N=28) | Condition | ||||||
| Pre | Post | d | Pre | Post | d | Pre | Post | d | Difference | |
| Stress Ratings | 2.94 (.14) | 2.09 (.14) | .85 | 2.90 (.14) | 2.32 (.14) | .59 | 3.31 (.20) | 2.86 (.19) | .44 | χ2(2)=9.89, p=.007 |
| Occasions Stressed | 0.66 (.04) | 0.45 (.04) | .72 | 0.62 (.04) | 0.52 (.04) | .36 | 0.72 (.05) | 0.68 (.05) | .16 | χ2(2)=13.34, p=.001 |
| Non-judgment | 3.83 (.12) | 4.58 (.12) | .88 | 3.65 (.12) | 4.25 (.12) | .72 | 3.65 (.17) | 3.92 (.16) | .31 | χ2(2)=30.82, p<.001 |
Note: Data are reported as means (SE) adjusted for observation number within day (coded 0–4). d = Cohen’s d effect size estimate.
Occasions Stressed.
It was also hypothesized that MA participants would have greater reductions in the proportion of assessments in which they reported experiencing any feelings of stress compared to MO or NT participants. To test this hypothesis, we used 3-level MLMs to evaluate the time by condition interaction. Across all 2721 assessment responses, this high stress participant sample reported feeling stressed on 1565 occasions (57.52%). There was no main effect of condition (χ2(2)=5.50, p=.0641), but there was a main effect of time (χ2(1)=34.17, p<.0001). Consistent with prediction, these effects were qualified by an interaction between time and condition (χ2(2)=13.34, p=.0013). Although participants across all conditions showed a decrease from baseline to post-intervention in the proportion of assessments that they reported experiencing any feelings of stress (MA participants: .66 to .45, d=.73; MO participants: .62 to .52, d=.36; NT participants: .72 to .68, d=.16), this decrease was significantly greater for MA participants compared to both MO (χ2(1)=8.53, p=.0035, d=.38) and NT participants (χ2(1)=9.85, p=.0017, d=.62). There was no difference in change in occasions stressed between MO and NT participants (χ2(1)=0.93, p=.3356, d=.22).
When participants reported experiencing stress since the last assessment, they were prompted to answer three additional exploratory questions. These items assessed how much of the time participants were feeling stressed, how severe their feelings of stress were, and how successful they believed they were in coping with stress. As these items were only sampled in a subset of measurement occasions (57.5% of total measurement occasions) and because there were condition differences in the number of times participants indicated stress at post-intervention due to intervention effects (primary analyses described above: MA=45%, MO=52%, NT=68%), these items are treated as exploratory and underpowered, and reported in the supplemental online materials for interested readers.
Discussion
This dismantling RCT provides one of the first experimental tests of the mechanisms linking mindfulness interventions with reduced stress. Consistent with hypotheses, MA participants had greater reductions in both stress ratings and occasions stressed compared to both MO and NT participants. These findings add to a growing body of research examining the stress- reducing benefits of mindfulness interventions by providing evidence that these benefits may be driven by acceptance skills training.
This study experimentally demonstrates the important role of acceptance skills training in mindfulness interventions and also provides data consistent with the notion that increases in non-judgment may drive stress-reduction benefits. Specifically, MA participants had greater increases in non-judgmental perceptions during daily life at post-intervention compared to both MO and NT participants. This study provides the first evidence that increased non-judgment towards experiences in daily life may be one mechanism through which mindfulness training interventions reduce stress. One interesting implication of these findings is that training individuals to adopt an accepting attitude toward present moment experience reduces the tendency to construct evaluative and judgment-laden narratives about these experiences. Consistent with this notion, this type of evaluative attention has been shown to be associated with negative psychological outcomes such as depression and anxiety (Mor & Winquist, 2002). Moreover, our present measure of non-judgment was focused on measuring a more general orientation of non-judgment towards aspects of daily life including perceptions of the self, others, one’s thoughts and feelings, and everyday situations, suggesting that training acceptance skills in relation to momentary experiences may also help foster a broader non-evaluative lens toward one’s self and one’s current situation.
Monitor and Acceptance Theory (MAT) is one mechanistic account of mindfulness training which predicts that removing acceptance skills training from mindfulness interventions will attenuate both their stress reduction benefits and their protective effects against a host of stress-related diseases (Lindsay & Creswell, 2017). This RCT extends initial work demonstrating that acceptance training is necessary to reduce biological stress reactivity in the laboratory (Lindsay et al., 2018) by showing that acceptance skills training may also be the critical mechanism for stress reduction benefits in daily life measured by EMA. One potentially surprising finding was that participants completing the 8-week MO training did not show declines in psychological stress relative to NT participants. However, this result is consistent with the prediction made by Monitor and Acceptance Theory (MAT; Lindsay & Creswell, 2017) that attention monitoring alone is not sufficient for reducing psychological stress.
It is possible that acceptance skills training provides a behavioral approach for improving how one copes with difficult or stressful experiences, fostering non-judgment and reducing primary threat appraisals and negative affective reactions to daily life stressors (Slutsky, Rahl, Lindsay, & Creswell, 2016). The MA intervention class activities and home practice recordings invited participants to notice their thoughts, feelings, and sensations without attempting to suppress, avoid, or reject them. These instructions were intended to cultivate and support an attitude of acceptance and non-reactivity towards noticed experiences, even those that were unpleasant or uncomfortable. This attitude of acceptance was further reinforced during group discussions where class instructors modeled an attitude of non-judgment as participants reflected upon their experiences during meditation practice and daily life. During the course of the 8-week intervention, participants learn that judging or trying to control the uncontrollable increases stress while acknowledgement or acceptance of the uncontrollable creates more ease and less stress. By reducing the habitual tendency to negatively judge and reject stressful events and experiences, developing acceptance skills may allow individuals to respond to such situations in a less reactive and more deliberate and adaptive manner.
The health psychology literature has long focused on how stress can increase risk for a broad range of negative psychological (e.g., depression) and physical health (e.g., cardiovascular disease) outcomes (Cohen, Janicki-Deverts, & Miller, 2007). This study contributes to a growing stress management intervention literature showing how specific elements of interventions (i.e., acceptance skills training) may be key mechanisms for promoting stress resilience (cf. Antoni et al., 2006). One potential implication of this work which should be tested in future studies is that the stress reduction benefits of acceptance skills training observed here may foster better stress- related psychological and physical health outcomes over time. Indeed, acceptance skills training may be a key health protective factor for stressed and at risk patient populations, and may help explain the stress-related health benefits of mindfulness interventions among a wide range of patient groups (e.g., HIV, depression, addictive disorders) (Creswell, 2017; Creswell, Villalba, Lindsay, & Chin, in press).
These findings are consistent with correlational work suggesting that high levels of selfreported experiential acceptance are associated with lower psychological distress and improved psychological health (Ford, Lam, John, & Mauss, 2017). One important consideration, which is not explored here, is that acceptance skills can be trained in other types of behavioral interventions besides mindfulness meditation training. For example, there are other interventions centered around the development of acceptance skills such as Acceptance and Commitment Therapy (ACT; Hayes, 2004). Future work is also needed to test methods for training acceptance skills alone and the impact of these intervention approaches on psychological stress.
There are several potential limitations to the current study. One is that monitoring and acceptance skills were not manipulated in a full 2 × 2 factorial design that included an acceptance only training condition. Although this possibility was considered, it was ultimately determined that training in attention monitoring is a necessary skill for learning how to accept monitored experiences within the context of a mindfulness intervention. Specifically, using one’s attention to monitor present experiences is a critical prerequisite to implementing any type of behavioral skills training, and it is difficult to conceive of a mindfulness-based acceptance skills training program that does not require participants to use their attention. Second, another limitation of this study was that the concurrent measurement of non-judgmental perceptions and momentary stress did not provide the temporal precedence necessary to conduct mediation analyses. Future work is necessary to more carefully test the causal role of non-judgment as a mediating mechanism for mindfulness training effects. Moreover, it is also possible that the MA and MO training programs differed on additional components besides the training of acceptance skills despite the dismantling approach used to construct these interventions. Third, an additional limitation of this study is that the learning of acceptance skills was not directly measured. One important direction for future research is to develop new measures which assess the learning of acceptance skills. Fourth, while one significant strength of this study is that it compares two well-matched active mindfulness interventions which were equivalent in terms of increasing positive treatment expectancies, it is important to acknowledge that the third arm was an inactive no treatment group. Although the use of a non-active control group suggests that improvements in stress among MA participants were not simply due to an effect of time, this feature of the study does not permit inferences about the stress buffering benefits of mindfulness interventions compared to other stress management programs. However, initial research suggests that mindfulness interventions have benefits above and beyond some other stress management interventions (Creswell et al., 2016; Lindsay et al., 2018). Next, the EMA items used to assess stress and non-judgment in this study were adapted from previously validated measures, but like most in the field have not been extensively tested or validated. Finally, because this study examined a sample that was predominantly white, female, and highly educated, it is important to test the degree to which these results are generalizable to other populations.
These findings raise broader questions about the implications of MA effects for stress- related health outcomes. Previous work has linked stress, assessed using EMA, with outcomes such as positive affect, negative affect, and health behaviors (e.g., Smyth et al., 2009), suggesting that including acceptance skills training in mindfulness interventions may potentially confer similar benefits in these populations. Indeed, previous RCTs of mindfulness interventions provide promising initial evidence for a broad range of stress-related health benefits, such as reducing depression relapse among at risk individuals (Kuyken et al., 2016), reducing experimentally-induced inflammation (Rosenkranz et al., 2013), and decreasing symptom severity among patients with irritable bowel syndrome (Garland et al., 2012). Although the effect sizes for analyses comparing changes among MA and MO participants over time are relatively small, it is important to acknowledge that these interventions were structurally equivalent 8-week training programs that produced equivalent positive treatment expectancies. By comparing the stress-reduction effects of two well-matched interventions, this dismantling study contributes to a new wave of mechanistically-focused mindfulness RCTs which allow investigators to evaluate the contributions of specific intervention components (e.g., Britton et al., 2018).
Conclusions
This theoretically-driven dismantling RCT tested the mechanisms of mindfulness training for stress-reduction. Consistent with predictions, participants trained to both monitor and accept present moment experiences showed greater reductions in daily life stress compared to participants trained in monitoring skills only. A notable strength of this study is the use of a highly ecologically valid EMA measurement strategy to assess changes in state stress. These findings provide evidence that acceptance skills training is an important and perhaps understudied mechanism of mindfulness interventions (Lindsay & Creswell, 2017). Furthermore, this RCT work highlights the value of conducting dismantling studies of mindfulness interventions to evaluate mechanistic pathways linking behavioral interventions with stress and health.
Supplementary Material
Acknowledgements.
The authors gratefully acknowledge Melissa Myozen Blacker, MA, Roshi, former senior teacher at UMass Center for Mindfulness for her contributions to the development and design of the intervention programs; Deanna Burkett for contributions to the development, design, and teaching of the intervention programs; and Jeffrey DeBoer, Hayley Rahl, and Lauren Simicich for help with study management.
Funding Sources. Research reported in this publication was supported by grants from the National Center For Complementary & Integrative Health (NCCIH) of the National Institutes of Health (NIH) (R21AT008493; R01AT008685) awarded to JDC. Recruitment for this study was supported by the NIH (UL1TR000005). Contributions to this manuscript made by EL were supported by a grant from the NIH (F32AT009508). The funding sources had no involvement in study design; manuscript preparation; data collection, analysis, or interpretation; or the decision to submit this article for publication. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Age was missing from one participant; age based on n=136 participants.
The 4-item PSS is a validated measure and this short form was used to minimize participant burden during the phone screening. PSS-4 scores at baseline in this study (M=8.22, SD=1.85, n=132) were appreciably higher than previously reported population means for this scale (M=4.49, SD=2.96 by Cohen & Williamson, 1988; M=6.11, SD=3.14 by Warttig, Forshaw, South, & White (2013).
Cronbach’s alpha was calculated by averaging reliability values computed at each time point.
There were no appreciable changes to any result in secondary analyses which examined only participants who completed the intervention (n=98).
While home practice audios were 40–45 minutes in duration, participants would occasionally receive credit for additional practice time due to issues with the software platform. To correct these outliers, any home practice session greater than 45 minutes in duration were recoded to 45 minutes.
References
- Allison PD (2012). Handling missing data by maximum likelihood In SAS global forum (Vol. 2012). Statistical Horizons, Havenford, PA. [Google Scholar]
- Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, ... Carver CS (2006). How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology, 74(6), 1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer RA, Smith GT, & Allen KB (2004). Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment, 11(3), 191–206. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. [DOI] [PubMed] [Google Scholar]
- Britton WB, Davis JH, Loucks EB, Peterson B, Cullen BH, Reuter L, ... Lindahl JR (2017). Dismantling Mindfulness-Based Cognitive Therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour Research and Therapy https://doi.org/10.10167j.brat.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, & Williamson G (1988). Perceived stress in a probability sample of the US In Spacapam S& Oskamp S(Eds.), The social psychology of health: Claremont symposium on applied social psychology (pp. 31–67). Newbury Park, CA: Sage. [Google Scholar]
- Cohen Sheldon, Janicki-Deverts D, & Miller GE (2007). Psychological stress and disease. Journal of the American Medical Association, 298(14), 1685–1687. [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396. [PubMed] [Google Scholar]
- Creswell JD (2017). Mindfulness Interventions. Annual Review of Psychology, 68(1), 491–516. 10.1146/annurev-psych-042716-051139 [DOI] [PubMed] [Google Scholar]
- Creswell JD, & Lindsay EK (2014). How does mindfulness training affect health? A mindfulness stress buffering account. Current Directions in Psychological Science, 23(6), 401–407. [Google Scholar]
- Creswell JD, Pacilio LE, Lindsay EK, & Brown KW (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44(2014), 1–12. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Taren AA, Lindsay EK, Greco CM, Gianaros PJ, Fairgrieve A, ... Rosen RK (2016). Alterations in resting-state functional connectivity link mindfulness meditation with reduced interleukin-6: a randomized controlled trial. Biological Psychiatry, 80(1), 53–61. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Villalba D, Lindsay EK, & Chin B (n.d.). Mindfulness interventions for physical health: mechanisms and outcomes. Psychosomatic Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devilly GJ, & Borkovec TD (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry, 31(2), 73–86. [DOI] [PubMed] [Google Scholar]
- Ford BQ, Lam P, John OP, & Mauss IB (2017). The Psychological Health Benefits of Accepting Negative Emotions and Thoughts: Laboratory, Diary, and Longitudinal Evidence. Journal of Personality and Social Psychology. 10.1037/pspp0000157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foust J (2014). Body-Centered Inquiry: Meditation Training to Awaken Your Inner Guidance, Vitality, and Loving Heart. Louisville, CO: Sounds True. [Google Scholar]
- Garland EL, Gaylord SA, Palsson O, Faurot K, Douglas Mann J, & Whitehead WE (2012). Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine, 35(6), 591–602. 10.1007/s10865-011-9391-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenka SN (1994). Discourse Summaries: Evening Discourses by S.N. Goenka from a Ten- Day Course of Vipassana Onalaska, WA: Pariyatti Publishing. [Google Scholar]
- Hayes SC (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35(4), 639–665. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: The program of the stress reduction clinic at the University of Massachusetts Medical Center. New York: Delta. [Google Scholar]
- Kabat-Zinn J (2009). Wherever you go, there you are: Mindfulness meditation in everyday life. Hachette UK. [Google Scholar]
- Kamarck TW, Muldoon MF, Shiffman SS, & Sutton-Tyrrell K (2007). Experiences of demand and control during daily life are predictors of carotid atherosclerotic progression among healthy men. Health Psychology, 26(3), 324–332. 10.1037/0278-6133.26.3.324 [DOI] [PubMed] [Google Scholar]
- Khoury B, Sharma M, Rush SE, & Fournier C (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. 10.1016/jjpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G, ... Dalgleish T (2016). Efficacy of Mindfulness-Based Cognitive Therapy in Prevention of Depressive Relapse: An Individual Patient Data Meta-analysis From Randomized Trials. JAMA Psychiatry, 73(6), 565 10.1001/jamapsychiatry.2016.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review, 51, 48–59. https://doi.org/10.10167j.cpr.2016.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Smyth JM, Brown KW, & Creswell JD (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology, 87, 63–73. [DOI] [PubMed] [Google Scholar]
- Ludwig DS, & Kabat-Zinn J (2008). Mindfulness in medicine. The Journal of the American Medical Association, 300(11), 1350–1352. [DOI] [PubMed] [Google Scholar]
- Moore RC, Depp CA, Wetherell JL, & Lenze EJ (2016). Ecological momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. Journal of Psychiatric Research, 75, 116–123. https://doi.org/10.10167j.jpsychires.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor N, & Winquist J (2002). Self-focused attention and negative affect: a meta-analysis. Psychological Bulletin, 128(4), 638. [DOI] [PubMed] [Google Scholar]
- Neubauer AB, Smyth JM, & Sliwinski MJ (2018). Age differences in proactive coping with minor hassles in daily life. The Journals of Gerontology: Series B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenkranz MA, Davidson RJ, MacCoon DG, Sheridan JF, Kalin NH, & Lutz A(2013). A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity, 27C, 174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological Momentary Assessment. Annual Review of Clinical Psychology, 4(1), 1–32. 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Slutsky J, Rahl H, Lindsay EK, & Creswell JD (2016). Mindfulness, emotion regulation, and social threat. Mindfulness in Social Psychology. [Google Scholar]
- Smyth JM, & Heron KE (2016). Is providing mobile interventions” just-in-time” helpful? an experimental proof of concept study of just-in-time intervention for stress management. In Wireless Health (pp. 89–95). [Google Scholar]
- Smyth JM, & Stone AA (2003). Ecological Momentary Assessment Research in Behavioral medicine. Journal of Happiness Studies, 4(1), 35–52. 10.1023/A:1023657221954 [DOI] [Google Scholar]
- Smyth JM, Wonderlich SA, Sliwinski MJ, Crosby RD, Engel SG, Mitchell JE, & Calogero RM (2009). Ecological momentary assessment of affect, stress, and binge- purge behaviors: Day of week and time of day effects in the natural environment. International Journal of Eating Disorders, 42(5), 429–436. 10.1002/eat.20623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trungpa C (2003). Training the Mind and Cultivating Loving-Kindness. Shambhala Publications. [Google Scholar]
- Warttig SL, Forshaw MJ, South J, & White AK (2013). New, normative, English- sample data for the Short Form Perceived Stress Scale (PSS-4). Journal of Health Psychology, 18(12), 1617–1628. 10.1177/1359105313508346 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


