To the Editor: Sunburn is a biologic indicator of acute overexposure to ultraviolet (UV) radiation, and sunburn at any age is associated with an increased risk for melanoma.1 Tracking changes in the national prevalence of sunburn over time can provide insight to our nation’s progress toward increasing adequate use of sun protection and reducing skin cancer risk at a population level.2 We examined changes over time in sunburn among US adults during 2005–2015.
We analyzed data from the 2005, 2010, and 2015 National Health Interview Survey, a cross-sectional, nationally representative sample of the US civilian population aged ≥18 years (https://www.cdc.gov/nchs/nhis/). Respondents were asked to report the number of sunburns they experienced during the preceding 12 months. We estimated the percentage of adults who experienced ≥1 sunburn each year and the mean number of sunburns among those who were sunburned overall and by sex, age group, race/ethnicity, and US region. We assessed differences in sunburn between survey years by using logistic regressions to calculate adjusted prevalence ratios overall and for each demographic subgroup. Annual unconditional response rates were 55.2%−69.0%, and sample sizes were 27,157–33,672 persons. We used SAS-callable SUDAAN version 11.0 (Research Triangle Institute, Research Triangle Park, NC) for the analyses to account for the complex sampling design and for nonresponse.
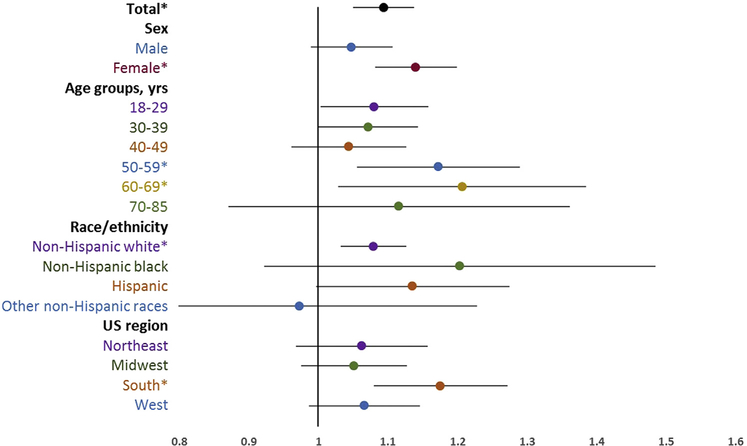
Each year, more than one third of adults experienced sunburn (Table I). The mean number of sunburns (among those reporting sunburn) ranged from 2.37 (95% confidence interval [CI] 2.25–2.48) in 2010 to 2.62 (95% CI 2.39–2.84) in 2015. A higher percentage of non-Hispanic white adults experienced sunburn compared with other racial/ethnic groups (P <.001), and the percentage of adults experiencing sunburn tended to decrease with increasing age (P < .001). Among all adults, sunburn increased significantly during 2005–2010 (adjusted prevalence ratio [APR] 1.13, 95% CI 1.09–1.17) and during 2005–2015 (APR 1.09, 95% CI 1.05–1.14). Sunburn did not change significantly during 2010–2015. Similar patterns occurred across most demographic subgroups. However, during 2005–2015, sunburn increased significantly only among females, 50–59-year-olds, 60–69-year-olds, non-Hispanic whites, and those living in the South (Fig 1). There were no significant changes in the mean number of sunburns over time.
Table I.
Estimated percentages (unadjusted) of US adults experiencing ≥1 sunburns in the past 12 months, National Health Interview Survey 2005, 2010, 2015
| 2005 | 2010 | 2015 | ||||
|---|---|---|---|---|---|---|
| Category | Sample size | % (95% CI) | Sample size | % (95% CI) | Sample size | % (95% CI) |
| Total | 29,250 | 34.2 (33.5–34.9) | 25,159 | 37.1 (36.3–37.9) | 31,399 | 34.1 (33.2–35.1) |
| Sex | ||||||
| Male | 12,762 | 36.2 (35.1–37.2) | 11,090 | 38.6 (37.5–39.7) | 14,056 | 34.8 (33.5–36.0) |
| Female | 16,488 | 32.4 (31.6–33.3) | 14,069 | 35.7 (34.7–36.7) | 17,343 | 33.5 (32.4–34.6) |
| Age group, years | ||||||
| 18–29 | 5434 | 45.6 (43.9–47.2) | 4949 | 50.1 (48.2–51.9) | 5331 | 47.2 (45.0–49.4) |
| 30–39 | 5543 | 43.6 (42.0–45.3) | 4557 | 45.8 (44.0–47.5) | 5229 | 44.2 (42.4–46.0) |
| 40–49 | 5715 | 40.2 (38.6–41.8) | 4455 | 42.7 (41.0–44.5) | 4866 | 38.5 (36.6–40.4) |
| 50–59 | 4983 | 28.6 (27.1–30.1) | 4249 | 33.7 (31.9–35.5) | 5447 | 31.7 (30.0–3.5) |
| 60–69 | 3421 | 19.4 (17.9–20.9) | 3431 | 22.1 (20.6–23.8) | 5143 | 22.5 (20.7–24.4) |
| ≥70 | 4154 | 9.2 (8.2–10.3) | 3518 | 11.5 (10.2–12.9) | 5383 | 10.0 (8.8–11.2) |
| Race/ethnicity | ||||||
| Non-Hispanic white | 19,059 | 41.2 (40.3–42.1) | 14,490 | 44.8 (43.9–45.7) | 19,784 | 42.4 (41.2–43.7) |
| Non-Hispanic black | 3986 | 8.2 (7.2–9.3) | 4093 | 11.0 (9.8–12.3) | 4157 | 9.7 (8.6–10.9) |
| Hispanic | 5106 | 22.4 (21.0–23.8) | 4779 | 27.0 (25.4–28.7) | 5208 | 24.5 (22.8–26.2) |
| Other non-Hispanic races* | 1029 | 19.5 (16.5–22.9) | 1710 | 21.1 (18.8–23.6) | 2074 | 18.2 (16.1–20.5) |
| US region | ||||||
| Northeast | 4921 | 34.3 (32.8–35.8) | 3982 | 36.5 (34.8–38.2) | 5175 | 33.0 (31.2–35.0) |
| Midwest | 6868 | 42.6 (41.1–44.1) | 5543 | 43.6 (42.0–45.2) | 6633 | 41.0 (38.7–43.4) |
| South | 10,828 | 27.7 (26.5–29.0) | 9240 | 32.7 (31.3–34.1) | 10,731 | 29.8 (28.3–31.4) |
| West | 6633 | 35.4 (34.0–36.9) | 6394 | 37.7 (36.0–39.5) | 8860 | 35.1 (33.3–36.9) |
CI, Confidence interval.
Includes non-Hispanic respondents who were American Indian, Alaska Native, Asian, or multiple races.
Fig 1.
APRs for ≥1 sunburns among US adults in 2015 versus 2005 overall and by sex, age, race/ethnicity, and US region. APRs were adjusted for demographic characteristics by using logistic regression models with predicted marginal probabilities. The APRs for total were adjusted for sex, age groups, race/ethnicity, and US region in the model. The APRs for male and female were adjusted for age groups, race/ethnicity, and US region in the model. The APRs for the 5 age groups were adjusted for sex, race/ethnicity, and US region in the model. The APRs for the racial/ethnic groups were adjusted for sex, age groups, and US region in the model. The APRs for the US regions were adjusted for sex, age groups, and race/ethnicity. The category other non-Hispanic races included non-Hispanic respondents who were American Indian, Alaska Native, Asian, or multiple races. APR, Adjusted prevalence ratio. *APR is statistically significant (P <.01).
Study limitations include reliance on self-reported information, which is subject to error, and generalizability to only the noninstitutionalized, civilian adult population. The large sample size warrants caution when interpreting statistically significant results with small absolute differences between years.
Overall, we found little change in sunburn prevalence during 2005–2015. Although sunburn is most prevalent among non-Hispanic white adults, heterogeneity in skin type exists within racial and ethnic groups, and these data indicate that all demographic groups experience preventable overexposure to UV radiation. Without future decreases in sunburn, skin cancer rates will likely continue to increase in the decades to come.3 Evidence-based interventions to reduce UV exposure and increase sun protection are available.2,4,5 However, more efforts are needed to help communities adapt and adopt these strategies and programs to meet their unique needs and maximize the likelihood of sustainability over time.
Footnotes
Conflicts of interest: None disclosed.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
REFERENCES
- 1.Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18(8):614–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer. Washington, DC: US: Dept of Health and Human Services, Office of the Surgeon General; 2014 [Google Scholar]
- 3.Guy GP Jr, Thomas CC, Thompson T, Watson M, Massetti GM, Richardson LC, Centers for Disease Control and Prevention. Vital signs: melanoma incidence and mortality trends and projections — United States, 1982–2030. MMWR Morb Mortal Wkly Rep. 2015;64(21):591–596. [PMC free article] [PubMed] [Google Scholar]
- 4.Community Preventive Services Task Force. The community guide: what works to promote health. The Guide to Community Preventive Services website. Avaliable at: http://www.thecommunityguide.org/index.html. Accessed October 4, 2017.
- 5.National Cancer Institute. Research tested intervention programs. Avaliable at: https://rtips.cancer.gov/rtips/index.do. Accessed January 29, 2018.