Abstract
Aims
The EuroQol five-dimension (EQ-5D) questionnaire is a widely used multiattribute general health questionnaire where an EQ-5D < 0 defines a state ‘worse than death’ (WTD). The aim of this study was to determine the proportion of patients awaiting total hip arthroplasty (THA) or total knee arthroplasty (TKA) in a health state WTD and to identify associations with this state. Secondary aims were to examine the effect of WTD status on one-year outcomes.
Patients and Methods
A cross-sectional analysis of 2073 patients undergoing 2073 THAs (mean age 67.4 years (sd 11.6; 14 to 95); mean body mass index (BMI) 28.5 kg/m2 (sd 5.7; 15 to 72); 1253 female (60%)) and 2168 patients undergoing 2168 TKAs (mean age 69.3 years (sd 9.6; 22 to 91); BMI 30.8 kg/m2 (sd 5.8; 13 to 57); 1244 female (57%)) were recorded. Univariate analysis was used to identify variables associated with an EQ-5D score < 0: age, BMI, sex, deprivation quintile, comorbidities, and joint-specific function measured using the Oxford Hip Score (OHS) or Oxford Knee Score (OKS). Multivariate logistic regression was performed. EQ-5D and OHS/OKS were repeated one year following surgery in 1555 THAs and 1700 TKAs.
Results
Preoperatively, 391 THA patients (19%) and 263 TKA patients (12%) were WTD. Multivariate analysis identified preoperative OHS, deprivation, and chronic obstructive pulmonary disease in THA, and OKS, peripheral arterial disease, and inflammatory arthropathy in TKA as independently associated with WTD status (p < 0.05). One year following arthroplasty EQ-5D scores improved significantly (p < 0.001) and WTD rates reduced to 35 (2%) following THA and 53 (3%) following TKA. Patients who were WTD preoperatively achieved significantly (p < 0.001) worse joint-specific Oxford scores and satisfaction rates one year following joint arthroplasty, compared with those not WTD preoperatively.
Conclusion
In total, 19% of patients awaiting THA and 12% awaiting TKA for degenerative joint disease are in a health state WTD. Although specific comorbidities contribute to this, hip- or knee-specific function, mainly pain, appear key determinants and can be reliably reversed with an arthroplasty.
Cite this article: Bone Joint J 2019;101-B:941–950.
Keywords: Hip arthroplasty, Knee arthroplasty, Health-related quality of life
In modern society, there is increasing demand for healthcare interventions to be economically viable and cost-effective. To quantify this, the number of quality-adjusted life-years (QALYs) delivered by the intervention is calculated, based on the EuroQol five-dimension (EQ-5D) score and population demographics such as life expectancy. The EQ-5D score measures five domains, scoring each at three levels of severity (mild, moderate, severe), giving 243 possible health profiles. These profiles can then be converted into a single absolute utility score. For the United Kingdom population, these scores range from -0.594 to 1, with a score of 1 representing full health and 0 death.1 Negative scores define, therefore, a state ‘worse than death’ (WTD). Of the 243 possible health states, 84 have negative utility scores and hence are deemed WTD. The ability to score health states WTD enables a broader description of severe disability and severely poor health, thereby lessening the floor effect of this score. The measure is reliable, responsive, and validated in a number of populations and conditions including arthropathy.2-4
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) for end-stage degenerative joint disease (DJD) are both extremely clinically and cost-effective: cost per QALY is £1372 and £2101 for THA and TKA, respectively.5 Both procedures are considerably cheaper than the £20 000 per QALY for a procedure to be defined as cost-effective. Despite this, in a financially pressured healthcare system there is pressure to reduce, and possibly even ration, their use. The assumption appears to be that leaving patients with DJD in pain to deteriorate is benign when compared with other healthcare needs.
The aim of this study was to identify the number of patients with end-stage DJD awaiting hip or knee arthroplasty surgery whose health state was defined as WTD by the EQ-5D score, and to identify associations with this state. Secondary aims included examining the influence of waiting times on WTD status and of WTD status on the outcome of joint arthroplasty surgery at one year.
Patients and Methods
Ethical approval was obtained for this cross-sectional study (Scotland (A) Research Ethics Committee 16/SS/0026). Between January 2014 and September 2017 data were recorded for 2206 consecutive patients undergoing primary THAs and 2394 primary TKAs. Data pertaining to the second arthroplasty in patients who underwent bilateral procedures during the study period were excluded, leaving study populations of 2073 patients undergoing THA and 2168 TKA.
Standard prostheses were cemented THAs utilizing an Exeter stem and a Contemporary acetabular component (Stryker Orthopaedics, Mahwah, New Jersey) and cemented, cruciate-retaining Triathlon TKAs (Stryker Orthopaedics), with surgery performed or supervised by 12 surgeons at a large orthopaedic teaching hospital. Patients followed standardized postoperative rehabilitation following THA and similarly following TKA. All patients followed a uniform departmental rehabilitation care plan.
Preoperatively, patients completed questionnaires including a detailed comorbidity questionnaire, general health (EQ-5D), and joint-specific (Oxford Hip Score (OHS) or Oxford Knee Score (OKS)) patient-reported outcome measures (PROMs). Specifically, the questionnaire asked about the presence of the following conditions: myocardial infarction, congestive heart failure, peripheral arterial disease (PAD), stroke with hemiplegia, dementia, chronic obstructive pulmonary disease (COPD), connective tissue disorder, diabetes, kidney disease and liver disease, back pain, and pain in other joints. Preoperative questionnaires were collected at a preassessment clinic two weeks prior to surgery, when additional demographical data including age, sex, body mass index (BMI), and postcode were recorded by the research team. At one year postoperatively, questionnaires included EQ-5D, OHS/OKS, and a measure of patient satisfaction using a five-point Likert scale with the options ‘very satisfied’, ‘satisfied’, ‘uncertain’, ‘dissatisfied’, and ‘very dissatisfied’. These were completed independently of routine care and were administered via post.
The EQ-5D score provides a validated and standardized measure of five health domains (mobility, self-care, ability to perform usual activities, pain/discomfort, and anxiety/depression), each rated 1 to 3 (no problems; moderate difficulties; severe difficulties) in addition to two visual analogue scales of health and pain (scale 0 to 100).6 The OHS and OKS are validated hip- and knee-specific outcome measures, respectively, where 12 questions (five possible answers) give scores from 0 to 48 (higher scores = better function).7,8 The patient’s postcode was used to assign Scottish Index of Multiple Deprivation (SIMD) quintiles.9 The SIMD ranks geographical areas based upon seven domains: income, employment, education, housing, health, crime, and geographical access. Data zones are defined by postcodes and once ranked nationally are divided into population-weighted quintiles with 1 representing the most deprived and 5 representing the least deprived.
Waiting list data were acquired from our local waiting list office. For patients who were placed on the waiting list at their first orthopaedic outpatient (OP) review, the time from primary care referral to orthopaedic review and the time from review to surgery were individually calculated. Patients who had been reviewed multiple times in OP clinics prior to listing were not included in the waiting time evaluation, as the basis of the delay to surgery was uncertain.
Statistical analysis
Data were analyzed using SPSS version 21.0 (IBM, Armonk, New York). Univariate analysis was performed using parametric (Student’s t-test: paired and unpaired) and nonparametric (Mann–Whitney U test, Wilcoxon’s signed-rank test) tests, as appropriate, to assess differences in continuous variables between groups (WTD and not WTD; responders and nonresponders; persistent and resolved WTD status). Nominal categorical variables were analyzed using chi-squared test or Fisher’s exact test. Pearson’s correlation coefficient was used to assess the relationship between linear variables. Variables found to be associated with a health state WTD at the 10% level or less were entered stepwise into a multivariate binary logistic regression analysis, using an enter methodology, to identify independent associations with WTD status. The same method was employed to identify associations with persistent postoperative WTD status. A p-value < 0.05 was considered statistically significant. Receiver operating characteristic (ROC) curve analysis was used to identify the threshold OHS or OKS associated with WTD status. The area under the ROC curve ranges from 0.5, indicating a test with no accuracy, to 1.0, indicating perfect accuracy. The threshold value is the point of maximal sensitivity and specificity in predicting WTD.
Results
Hips
Between January 2014 and September 2017, 2073 THAs were performed in 2073 consecutive patients: mean age, 67.4 years (sd 11.6; 14 to 95); mean BMI, 28.5 kg/m2 (sd 5.7; 15 to 72); 1253 patients (60.4%) were female, 1982 patients (95.6%) had primary osteoarthristis.
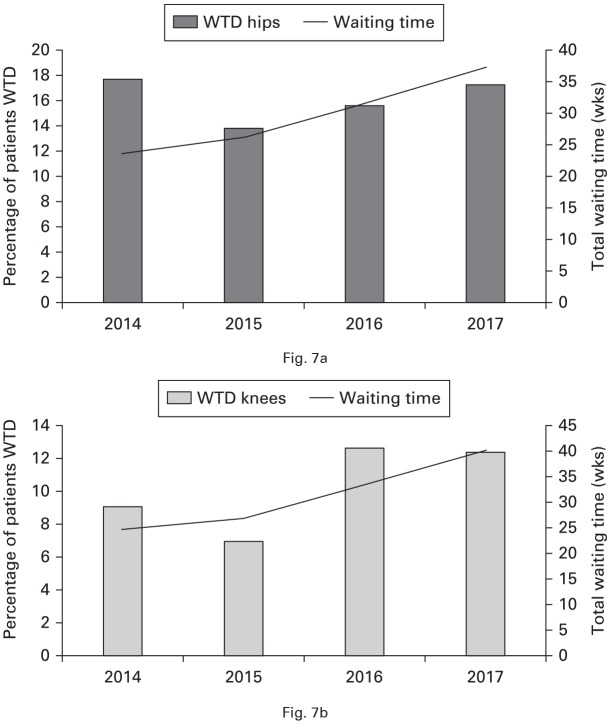
While awaiting THA, the median EQ-5D index was 0.364 (interquartile range (IQR) 0.06 to 0.69), six patients (0.3%) had an EQ-5D status of full health (EQ-5D index = 1.0), and 391 (18.9%) had negative scores WTD (Fig. 1). Of 391 patients with scores defined as WTD, 389 (99%) reported extreme levels of pain and 76 (20%) extreme levels of anxiety and depression. Univariate analysis identified a number of variables significantly (p < 0.05) associated with WTD status (Table I). Multivariate analysis identified the preoperative OHS and the presence of COPD to be independently associated with WTD status prior to hip arthroplasty (Table II).
Table I.
Univariate analysis of associations with ‘worse than death’ (WTD) status (EuroQol five-dimension (EQ-5D) < 0) prior to total hip arthroplasty (THA) and total knee arthroplasty (TKA)
| Variable | Hips | Knees | ||||
|---|---|---|---|---|---|---|
| WTD (n = 391) | Not WTD (n = 1682) | p-value | WTD (n = 260) | Not WTD (n = 1907) | p-value | |
| Mean age, yrs (sd) | 67.3 (12.8) | 67.4 (11.3) | 0.919* | 68.9 (10.3) | 69.4 (9.4) | 0.478* |
| Mean body mass index, kg/m2 (sd) | 29.9 (6.3) | 28.2 (5.5) | < 0.001*† | 32.3 (6.4) | 30.6 (5.7) | < 0.001*† |
| Sex, female, n (%) | 280 (72) | 973 (58) | < 0.001†‡ | 183 (68) | 1060 (55) | < 0.001†‡ |
| SIMD, n (%) | ||||||
| 1 | 40 (10) | 118 (7) | < 0.001†‡ | 31 (12) | 158 (8) | 0.006†‡ |
| 2 | 113 (29) | 266 (16) | 75 (29) | 364 (19) | ||
| 3 | 58 (15) | 304 (18) | 42 (16) | 368 (19) | ||
| 4 | 94 (24) | 390 (23) | 52 (20) | 443 (23) | ||
| 5 | 86 (22) | 604 (36) | 60 (23) | 574 (30) | ||
| Medical comorbidity, n (%) | ||||||
| Myocardial infarction | 15 (4) | 56 (3) | 0.620‡ | 11 (4) | 93 (5) | 0.621‡ |
| Heart failure | 5 (1) | 11 (1) | 0.204‡ | 3 (1) | 17 (1) | 0.692‡ |
| Peripheral arterial disease | 5 (1) | 25 (1) | 0.757‡ | 12 (5) | 31 (2) | 0.001†‡ |
| Stroke with hemiplegia | 17 (4) | 34 (2) | 0.007†‡ | 7 (3) | 49 (3) | 0.930‡ |
| Dementia | 11 (3) | 10 (1) | < 0.001†‡ | 1 (0.4) | 8 (0.4) | 0.926‡ |
| Chronic obstructive pulmonary disease | 38 (10) | 52 (3) | < 0.001†‡ | 15 (6) | 79 (4) | 0.244‡ |
| CTD/inflammatory arthropathy | 84 (21) | 153 (9) | < 0.001†‡ | 70 (27) | 296 (16) | < 0.001†‡ |
| Diabetes | 37 (9) | 131 (8) | 0.497‡ | 28 (11) | 241 (13) | 0.358‡ |
| Kidney disease | 10 (3) | 29 (2) | 0.275‡ | 7 (3) | 42 (2) | 0.638‡ |
| Liver disease | 14 (4) | 18 (1) | < 0.001†‡ | 4 (2) | 24 (1) | 0.724‡ |
| Median number of medical comorbidities (IQR) | 0 (0 to 5) | 0 (0 to 9) | < 0.001†§ | 1 (0 to 2) | 0 (0 to 1) | < 0.001†§ |
| Musculoskeletal comorbidity, n (%) | ||||||
| Back pain | 159 (41) | 566 (34) | < 0.001†‡ | 136 (52) | 731 (38) | < 0.001†‡ |
| Pain in other joints | 199 (51) | 822 (49) | < 0.001†‡ | 205 (78) | 1315 (69) | < 0.003†‡ |
| Bilateral joint arthroplasties | 31 (8) | 82 (5) | 0.017†‡ | 16 (6) | 133 (7) | 0.481‡ |
| Mean PROM (sd) | ||||||
| EQ-5D health | 52.6 (24.3) | 70.8 (20.14) | < 0.001†§ | 57.6 (22.8) | 71.4 (19.7) | < 0.001*† |
| EQ-5D pain | 39.9 (25.7) | 53.7 (22.1) | < 0.001*† | 44.5 (24.4) | 52.9 (22.1) | < 0.001*† |
| Preoperative Oxford score | 11.0 (5.6) | 21.7 (7.8) | < 0.001*† | 14.1 (7.2) | 21.0 (7.6) | < 0.001*† |
Unpaired Student’s t-test
Statistically significant
Chi-squared test
Mann–Whitney U test
SIMD, Scottish Index of Multiple Deprivation; CTD, connective tissue disorder; IQR, interquartile range; PROM, patient-reported outcome measure
Table II.
Multivariate logistic regression analysis of predictors of ‘worse than death’ (WTD) status prior to total hip arthroplasty (THA) and total knee arthroplasty (TKA)
| Predictors in the model | B | OR (95% CI) | p-value |
|---|---|---|---|
| Hips (R2 = 0.411) | |||
| Body mass index | -0.01 | 0.99 (0.96 to 1.0) | 0.521 |
| Sex, female | 0.10 | 1.1 (0.74 to 1.63) | 0.627 |
| Scottish Index of Multiple Deprivation | 0.08 | 1.1 (0.95 to 1.24) | 0.038 |
| Joint-specific PROM | |||
| Preoperative Oxford Hip Score | 0.20 | 1.21 (1.18 to 1.26) | < 0.001* |
| Medical comorbidities | |||
| Stroke with hemiplegia | 0.35 | 1.4 (0.50 to 4.0 | 0.515 |
| Dementia | 1.58 | 4.9 (0.81 to 29.3) | 0.084 |
| Chronic obstructive pulmonary disease | 1.49 | 4.4 (1.9 to 10.3) | 0.001* |
| CTD/inflammatory arthropathy | 0.56 | 1.7 (0.96 to 3.2) | 0.067 |
| Liver disease | 0.57 | 1.76 (0.49 to 6.4) | 0.400 |
| Total number of medical comorbidities | 0.11 | 1.11 (0.84 to 1.48) | 0.458 |
| Musculoskeletal comorbidities | |||
| Back pain | 0.40 | 1.5 (0.99 to 2.2) | 0.054 |
| Pain in other joints | 0.30 | 1.4 (0.80 to 2.3) | 0.265 |
| Bilateral THAs | -0.54 | 0.58 (0.29 to 1.16) | 0.126 |
| Knees (R2 = 0.382) | |||
| Body mass index | -0.04 | 0.99 (0.96 to 1.03) | 0.790 |
| Sex, female | 0.21 | 1.24 (0.82 to 1.87) | 0.309 |
| Scottish Index of Multiple Deprivation | 0.05 | 1.05 (0.91 to 1.22) | 0.505 |
| Year of surgery | -0.16 | 0.85 0.72 to 1.02) | 0.081 |
| Joint-specific PROM | |||
| Preoperative Oxford Knee Score | 0.23 | 1.26 (1.22 to 1.31) | < 0.001* |
| Medical comorbidities | |||
| Peripheral arterial disease | 1.57 | 4.79 (1.57 to 14.58) | 0.006* |
| CTD/inflammatory arthropathy | 0.72 | 2.05 (1.24 to 3.40) | 0.005* |
| Total number of medical comorbidities | 0.03 | 1.03 (0.84 to 1.26) | 0.774 |
| Musculoskeletal comorbidities | |||
| Back pain | 0.04 | 1.04 (0.69 to 1.55) | 0.856 |
| Pain in other joints | 0.35 | 1.41 (0.85 to 2.35) | 0.186 |
Statistically significant
OR, odds ratio; CI, confidence interval; PROM, patient-reported outcome measure; CTD, connective tissue disorder
Fig. 1.
Frequency density graph of preoperative EuroQol five-dimension (EQ-5D) index in patients awaiting total hip arthroplasty (THA) and at one year following THA.
The preoperative EQ-5D status correlated with the preoperative OHS (R = 0.698; p < 0.01, Pearson’s correlation coefficient), the EQ-5D health score (R = 0.394; p < 0.01), and the EQ-5D pain score (R = 0.312; p < 0.01). Preoperative OHSs were significantly worse in those with WTD status (Table I, Fig. 2).
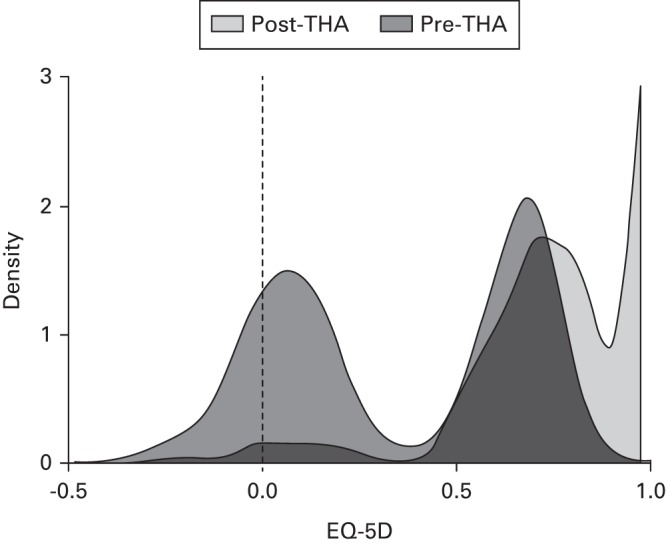
Fig. 2.
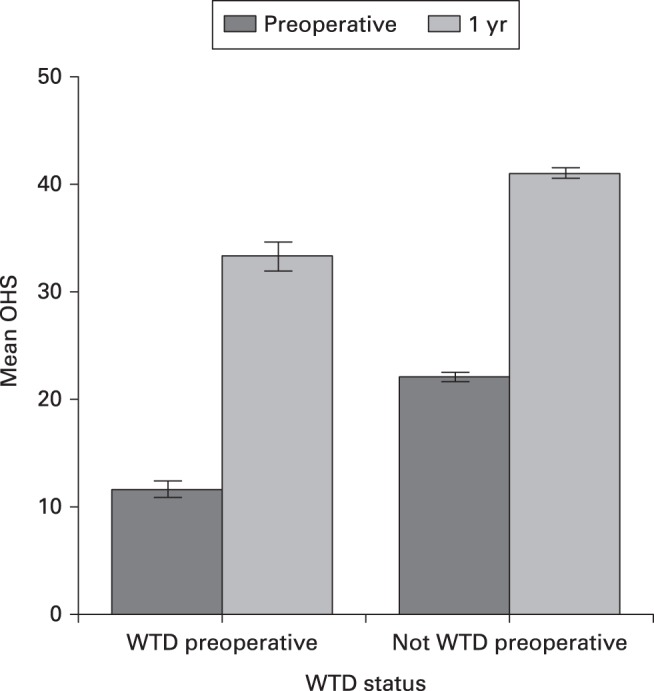
Chart showing Oxford Hip Scores (OHSs) prior to and one year following total hip arthroplasty (THA) in patients with preoperative ‘worse than death’ (WTD) status (EuroQol five-dimension (EQ-5D) < 0) and in those not WTD (EQ-5D > 0). Error bars represent 95% confidence intervals.
ROC analysis using the OHS to predict WTD status gave an area under the curve of 0.87 (95% confidence interval (CI) 0.85 to 0.88; p < 0.001; Fig. 3). A threshold OHS of 14.5 gave a sensitivity of 82% and a specificity of 75% for identifying those WTD. Significant differences were found in the responses to every individual question of the OHS preoperatively between those WTD and those not (p < 0.001, chi-squared test).
Fig. 3.
Receiver operating characteristic (ROC) curve for ‘worse than death’ (WTD) status and Oxford Hip Score prior to total hip arthroplasty (THA; area under curve = 0.87). Diagonal segments are produced by ties.
One year following THA, 16 patients had died and 1555/2046 surviving patients (76%) completed PROMs. Surviving responders and nonresponders are compared in Table III. In responders, the median EQ-5D index improved significantly to 0.796 (p < 0.001, Wilcoxon’s signed rank test): 615/1555 patients (40%) had an EQ-5D index of 1.0 (i.e. full health) and 35 patients (2%) had negative scores and were WTD. Patients WTD preoperatively achieved a significantly greater improvement in OHS following THA (Table IV), but their mean OHS remained significantly worse than those not WTD preoperatively at one year (33.3 (sd 10.4) vs 41.0 (sd 7.9); p < 0.001, Mann–Whitney U test; Fig. 2), a difference exceeding the minimal clinically important difference for this score of 5.10 Preoperative WTD status was significantly associated with satisfaction at one year: 206/242 WTD (85%) versus 1179/1286 not WTD (92%; p = 0.011, chi-squared test).
Table III.
Characteristics of responders and nonresponders to one-year patient-reported outcome measures (PROMs)
| Variable | Hips | Knees | ||||
|---|---|---|---|---|---|---|
| Nonresponder (n = 518) | Responder (n = 1555) | p-value | Nonresponder (n = 452) | Responder (n = 1697) | p-value | |
| Mean age, yrs (sd) | 65.6 (11.1) | 68.0 (11.7) | < 0.001*† | 68.1 (10.2) | 69.7 (9.3) | 0.002*† |
| Mean body mass index, kg/m2 (sd) | 29.5 (6.3) | 28.2 (5.5) | < 0.001*† | 31.7 (6.4) | 30.6 (5.6) | < 0.001*† |
| Sex, female, n (%) | 318 (61) | 935 (60) | 0.618‡ | 174 (38) | 753 (44) | 0.004†‡ |
| Medical comorbidity, n (%) | ||||||
| Myocardial infarction | 22 (4) | 49 (3) | 0.235‡ | 31 (7) | 73 (4) | 0.040†‡ |
| Heart failure | 5 (1) | 11 (1) | 0.561‡ | 3 (1) | 17 (1) | 0.466‡ |
| Peripheral arterial disease | 5 (1) | 25 (2) | 0.298‡ | 9 (2) | 34 (2) | 0.902‡ |
| Stroke with hemiplegia | 12 (2) | 39 (3) | 0.808‡ | 20 (4) | 36 (2) | 0.01†‡ |
| Dementia | 4 (1) | 17 (1) | 0.527‡ | 3 (1) | 6 (1) | 0.396‡ |
| Chronic obstructive pulmonary disease | 32 (6) | 58 (4) | 0.018†‡ | 28 (6) | 66 (4) | 0.052‡ |
| CTD/inflammatory arthropathy | 76 (15) | 161 (10) | 0.007†‡ | 97 (21) | 269 (16) | 0.014†‡ |
| Diabetes | 49 (9) | 119 (8) | 0.192‡ | 62 (14) | 207 (12) | 0.565‡ |
| Kidney disease | 8 (2) | 31 (2) | 0.515‡ | 13 (3) | 37 (2) | 0.455‡ |
| Liver disease | 8 (2) | 24 (1) | 0.999‡ | 8 (2) | 20 (1) | 0.374‡ |
| Median number of medical comorbidities (IQR) | 0 (0 to 1) | 0 (0 to 2) | < 0.001†§ | 2 (1 to 3) | 0 (0 to 1) | < 0.001†§ |
| Musculoskeletal comorbidity, n (%) | ||||||
| Back pain | 274 (53) | 725 (47) | < 0.013†‡ | 214 (47) | 653 (38) | 0.006†‡ |
| Pain in other joints | 358 (69) | 1020 (66) | < 0.015†‡ | 341 (75) | 1179 (69) | 0.202 |
| Preoperative PROM | ||||||
| Median EQ-5D index (IQR) | 0.16 (-0.02 to 0.62) | 0.516 (0.09 to 0.69) | < 0.001†§ | 0.20 (0.06 to 0.69) | 0.59 (0.16 to 0.69) | < 0.001†§ |
| Mean EQ-5D health (sd) | 63.4 (23.7) | 68.7 (21.5) | < 0.001*† | 67.0 (21.1) | 70.5 (20.4) | < 0.001*† |
| Mean EQ-5D pain (sd) | 47.5 (24.5) | 52.0 (23.2) | < 0.001*† | 50.2 (23.4) | 52.3 (22.3) | 0.076* |
| Mean preoperative Oxford score | 17.5 (8.5) | 20.4 (8.5) | < 0.001*† | 18.0 (7.8) | 20.7 (7.8) | < 0.001*† |
Unpaired Student’s t-test
Statistically significant
Chi-squared test
Mann–Whitney U test
CTD, connective tissue disorder; IQR, interquartile range
Table IV.
Improvement in patient-reported outcome measures (PROMs) at one year following total hip arthroplasty (THA; n = 1555) or total knee arthroplasty (TKA; n = 1697) in those ‘worse than death’ (WTD) preoperatively compared with those not WTD
| PROM improvement to 1 yr | WTD preoperative mean score (sd) | Not WTD preoperative mean score (sd) | p-value | 95% CI |
|---|---|---|---|---|
| Hips | n = 248 | n = 1307 | ||
| EQ-5D health | 13.3 (29.2) | 8.7 (22.8) | 0.023*† | 0.6 to 8.5 |
| EQ-5D pain | 24.8 (37.1) | 24.1 (33.4) | 0.301* | -4.3 to 5.9 |
| EQ-5D status | 0.67 (0.3) | 0.35 (0.3) | < 0.001*† | 0.28 to 0.36 |
| Oxford Hip Score | 21.6 (11.1) | 19.0 (9.4) | 0.001*† | 1.1 to 4.1 |
| Knees | n = 168 | n = 1529 | ||
| EQ-5D health | 14.4 (27.6) | 5.9 (22.5) | < 0.001*† | 4.1 to 12.9 |
| EQ-5D pain | 23.4 (35.0) | 21.1 (33.1) | 0.407* | -3.1 to 7.6 |
| EQ-5D status | 0.58 (0.35) | 0.29 (0.32) | < 0.001*† | 0.24 to 0.34 |
| Oxford Knee Score | 16.9 (10.8) | 15.0 (9.3) | 0.031*† | 0.17 to 3.6 |
Unpaired Student’s t-test
Statistically significant
CI, confidence interval; OHS, Oxford Hip Score; EQ-5D, EuroQol five-dimension; OKS, Oxford Knee Score
A total of 19 patients were persistently WTD at one year. Univariate analysis of those persistently WTD compared with those no longer WTD demonstrated significant differences in specific comorbidities and PROMs. Multivariate analysis of associations significant at the < 10% level (Table V) identified poor improvement in OHS to be the only independent association with persistent WTD status (p < 0.001). WTD rate at one year following THA was significantly higher in those WTD preoperatively: 19/248 (8%) versus 16/1307 (1%) (p < 0.001, chi-squared).
Table V.
Multivariate logistic regression analysis of predictors of persistent ‘worse than death’ (WTD) status in patients WTD preoperatively (hips, n = 19; knees, n = 24) compared with patients who were no longer WTD at one year following joint arthroplasty (total hip arthroplasty (THA), n = 248; total knee arthroplasty (TKA), n = 244). Only variables significant at < 10% level on univariate analysis were included
| Predictors in the model | B | OR (95% CI) | p-value |
|---|---|---|---|
| Hips (R2 = 0.516) | |||
| Liver disease | 1.43 | 4.18 (0.37 to 47.4) | 0.248 |
| Back pain | 0.84 | 2.30 (0.39 to 13.6) | 0.356 |
| Post-operative Oxford Hip Score | 0.07 | 1.07 (0.96 to 1.21) | 0.229 |
| Improvement in Oxford Hip Score | 0.13 | 1.14 (1.0 to 1.30) | 0.039* |
| Improvement in EQ-5D health | 0.02 | 1.02 (1.0 to 1.04) | 0.111 |
| Knees (R2 = 0.525) | |||
| Preoperative Oxford Knee Score | -0.05 | 0.95 (0.84 to 1.08) | 0.437 |
| Post-operative Oxford Knee Score | 0.22 | 1.26 (1.14 to 1.38) | < 0.001* |
| Improvement in EQ-5D pain | -0.003 | 1.00 (0.98 to 1.02) | 0.798 |
| Improvement in EQ-5D health | 0.02 | 1.02 (0.99 to 1.04) | 0.306 |
Statistically significant
OR, odds ratio; CI, confidence interval; EQ-5D, EuroQol five-dimension
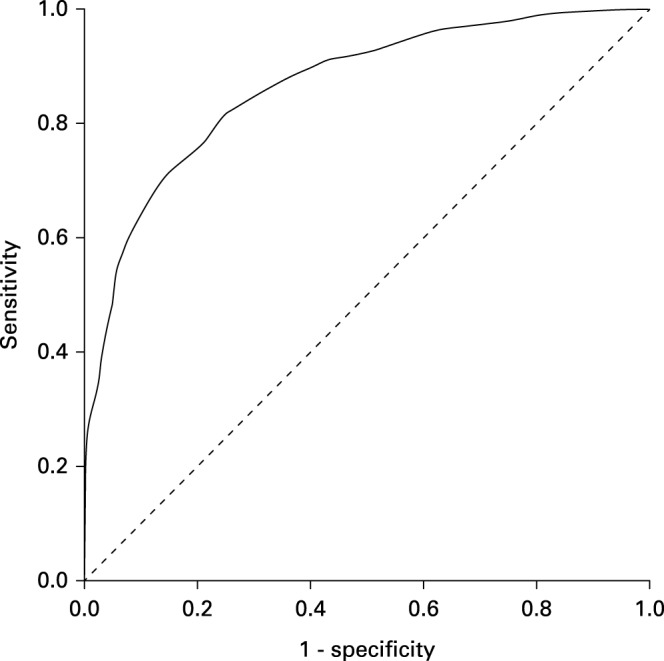
Waiting list data were available for 892 THA patients (141 WTD). Over the study period, the mean waiting time for both OP clinic review (p < 0.001, analysis of variance (ANOVA)) and surgery (p < 0.001, ANOVA) increased significantly. Between 2014 and 2017 mean OP waiting time increased from 10.8 weeks (sd 3.3) to 21.0 weeks (sd 11.0; p < 0.001, Student’s t-test); mean surgery waiting time increased from 13.0 weeks (sd 5.5) to 15.7 weeks (sd 6.5; p < 0.001, Student’s t-test). WTD status did not vary across the years studied (p = 0.713, chi-squared test). Patients reporting WTD status waited a mean shorter time for OP review (13.8 weeks (sd 8.1) vs 15.4 weeks (sd 7.5); p = 0.018) and for surgery (12.3 weeks (sd 5.0) vs 13.6 weeks (sd 5.8); p = 0.001).
Knees
Between January 2014 and September 2017, 2168 TKAs were performed in 2168 patients: mean age, 69.3 years (sd 9.6; 22 to 91); mean BMI, 30.8 kg/m2 (sd 5.8; 13 to 57); 1244 patients (57%) were female.
While awaiting TKA, the median EQ-5D index was 0.587 (IQR 0.29 to 0.88), five patients (0.3%) had an EQ-5D status of full health (EQ-5D index = 1.0), and 263 (12.1%) had negative scores WTD (Fig. 4). Of 263 patients with health states defined as WTD, all reported extreme levels of pain and 69 (26%) reported extreme levels of anxiety and depression. Univariate analysis confirmed a number of variables to be significantly (p < 0.05) associated with WTD status (Table I). Multivariate analysis identified the preoperative OKS and the presence of PAD or connective tissue disease (including inflammatory arthropathy) to be independently associated with WTD status prior to TKA (Table I).
Fig. 4.
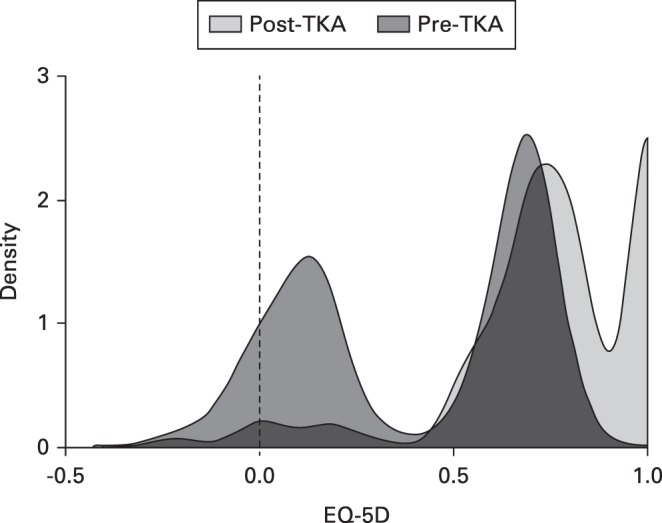
Frequency density graph of preoperative EuroQol five-dimension (EQ-5D) index in patients awaiting total knee arthroplasty (TKA) and at one year following TKA.
The preoperative EQ-5D status correlated with the preoperative OKS (R = 0.484; p < 0.01, Pearson’s correlation coefficient), the EQ-5D health score (R = 0.253; p < 0.01), and the EQ-5D pain score (R = 0.182; p < 0.01). Preoperative OKSs were significantly worse in those with WTD status (Table I, Fig. 5).
Fig. 5.
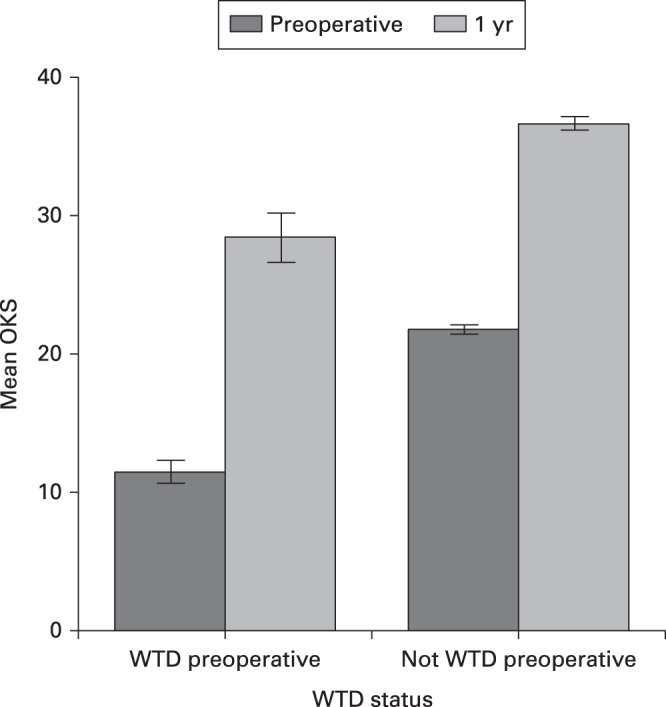
Oxford Knee Scores (OKSs) prior to and one year following total knee arthroplasty (TKA) in patients with preoperative ‘worse than death’ (WTD) status (EuroQol five-dimension (EQ-5D) < 0) and in those not WTD (EQ-5D > 0). Error bars represent 95% confidence intervals.
ROC analysis using the OKS to predict WTD status gave an area under the curve of 0.75 (0.72 to 0.78; p < 0.001; Fig. 6). A threshold OKS of 16.5 gave a sensitivity of 71% and a specificity of 64% for predicting those WTD. Significant differences were found in the responses to every individual question of the OKS preoperatively between those WTD and those not (p < 0.001, chi-squared test).
Fig. 6.
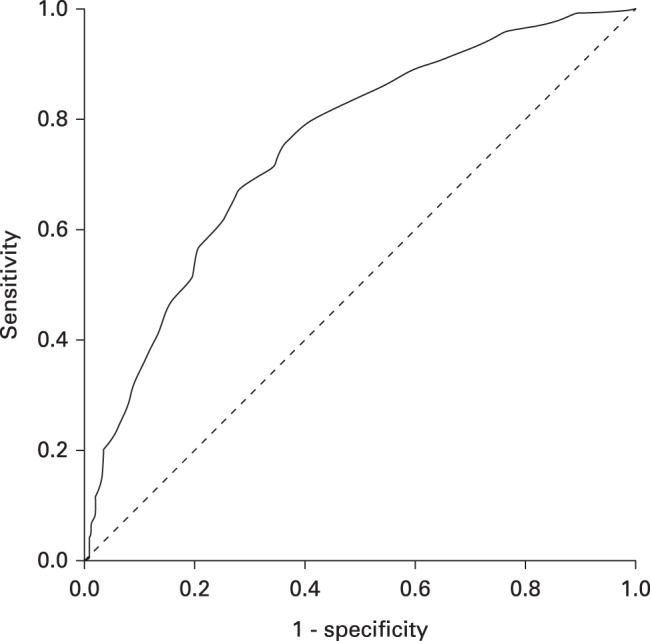
Receiver operating characteristic (ROC) curve for ‘worse than death’ (WTD) status and Oxford Knee Score prior to total knee arthroplasty (TKA; area under curve = 0.75). Diagonal segments are produced by ties.
One year following TKA, 19 patients had died and 1697/2149 surviving patients (79%) completed follow-up PROMs. Surviving responders and nonresponders are compared in Table III. In responders, the median EQ-5D index improved significantly to 0.760 (p < 0.001, Wilcoxon’s signed rank test): 493/1697 patients (29%) reported an EQ-5D status of 1.0 (i.e. full health) and 53 patients (3%) had negative scores and were WTD. Those WTD preoperatively achieved greater improvements in OKS following TKA (Table IV), although their OKS remained significantly worse than those not WTD preoperatively at one year (28.5 (sd 11.5) vs 36.7 (sd 9.1); p < 0.001, Mann–Whitney U test; Fig. 5), a difference that exceeds the minimal clinically important difference for this score of 5.10 Preoperative WTD status was significantly associated with satisfaction at one year: 125/164 WTD (73%) vs 1264/1506 not WTD (84%; p = 0.012, chi-squared test).
A total of 24 patients were persistently WTD at one year. Univariate analysis of those persistently WTD following TKA compared with those no longer WTD demonstrated no differences in demographics or comorbidities. Multivariate analysis of associations significant at the < 10% level (Table V) identified postoperative OKS to be the only independent association with persistent WTD status (p < 0.001). WTD rate at one year following TKA was significantly higher in those WTD preoperatively: 24/168 (14%) versus 32/1523 (2%; p < 0.001, chi-squared).
Waiting list data were available for 969 patients (79 WTD). Over the study period, the mean waiting time for both OP clinic review (p < 0.001, ANOVA) and surgery (p < 0.001, ANOVA) increased significantly: mean OP waiting time increased from 11.1 weeks (sd 2.9) to 23.1 weeks (sd 9.8; p < 0.001, Student’s t-test); mean surgery waiting time increased from 13.0 weeks (sd 6.2) to 17.1 weeks (sd 6.5; p < 0.001, Student’s t-test). The year of surgery affected the rate of WTD status (p = 0.013, chi-squared test) and was worst in 2016, when 55/437 patients (13%) were WTD (Fig. 7). There was no significant difference in waiting times between those reporting a health state WTD and those who did not: mean waiting time for new OP review (15.1 weeks (sd 7.4) vs 15.6 weeks (sd 5.4); p = 0.577); mean waiting time for surgery (14.2 weeks (sd 6.8) vs 14.1 weeks (sd 6.0); p = 0.797).
Fig. 7.
The percentage of patients awaiting a) total hip arthroplasty (THA) and b) total knee arthroplasty (TKA) defined as ‘worse than death’ (WTD) by year and the total annual wait for surgery (from referral to surgery in weeks).
Discussion
While awaiting lower limb arthroplasty, 19% of patients with DJD of the hip and 12% with DJD of the knee reported a health state ‘worse than death’, as expressed by the EQ-5D score. This was independently associated with joint specific function on multivariate analysis. Other associations with WTD status on multivariate analysis included COPD and deprivation in hip patients, and PAD and connective tissue disorder/inflammatory arthropathy in knee patients. Of the variables examined, restrictions resulting from joint disease and certain comorbidities leave a number of patients in a health state ‘worse than death’ as defined by the baseline dataset sampled from the general public of the United Kingdom. Patients who were WTD preoperatively achieved significantly worse joint-specific Oxford scores and satisfaction rates one year following joint arthroplasty, compared with those not WTD preoperatively. A trend of increasing waiting times over the study period was matched by a trend of an increasing proportion of patients WTD, although this was only statistically significant for knees.
These results must be interpreted in the context of how the EQ-5D score is calculated. The EQ-5D determines 243 health states using five domains. The specific score assigned to each of the 243 different health states differs by country reflecting different population preference weighting. This study of United Kingdom patients uses the United Kingdom value set. Results may differ with a different country’s preferences.4 The definition of WTD is researcher-generated and reflects the construction of the EQ-5D score.4 In the United Kingdom value set, one-third of the 243 health states are negative or WTD. These were defined by 3395 United Kingdom individuals valuing 45/243 states using the time trade-off method. Each individual scored 13 hypothetical heath states: the less time in the health state that could be endured, the lower the score.11 As such, these negative WTD scores are a hypothetical value statement made by the general public based on their beliefs of health-related quality of life. They do not mean that patients with negative scores would rather be dead (i.e. they are not experience-based valuations). A recent study of the general Swedish population aged more than 65 years found that 1.8% of the 6611 respondents defined a health state WTD using a hypothetical value set.11 WTD status was associated with female sex and older age reaching 5% in females more than 85 years of age,11 considerably lower than those of patients awaiting joint arthroplasty reported here. They also demonstrated that of patients classed as WTD, 15% were still satisfied with their life. This implies that using a hypothetical value set may underestimate actual quality of life and that experiential value sets may be more appropriate and accurate at this end of the spectrum. However, it is the general public in the United Kingdom who vote for the government, often with consideration of how they will fund the health service using their taxes, so their opinion of how severe illnesses and disabilities may be cared for in a societal context is highly relevant, especially when considering rationing and prioritization.
Health-related quality of life for a number of medical conditions has been studied using the EQ-5D health index (Table VI).3,12-14 It is notable how patients awaiting joint arthroplasty surgery score worse on the EQ-5D than patients with other chronic medical conditions such as heart failure, diabetes, and COPD (Table VI). This may reflect the influence of pain on this scoring system: 414/416 patients defined as WTD reported extreme pain in this domain of the EQ-5D. Few studies specifically examine patients with EQ-5D health indices < 0. Harrison et al3 investigated predictors of EQ-5D WTD status in 700 UK patients with inflammatory arthropathy, finding 9% to be in a health state WTD, associated mainly with pain. Similarly, Gaujoux-Viala et al4 reported EQ-5D scores in 813 patients with early inflammatory arthropathy, finding 11% were WTD, the key determinant of which was pain on multivariate regression analysis, although poor mental health scores (SF-12 MCS) and lower levels of education were also associated with a state WTD. Although our results support the influence of pain on EQ-5D heath status, social deprivation (as a proxy for educational level) was only associated with WTD status in hips.
Table VI.
EuroQol five-dimension (EQ-5D) index (United Kingdom value sets) for different medical conditions
| Condition | Reference | Mean (sd) | Median (IQR) |
|---|---|---|---|
| Awaiting THA | This study | 0.385 (0.32) | 0.516 (0.21 to 0.82) |
| Awaiting TKA | This study | 0.426 (0.30) | 0.587 (0.32 to 0.85) |
| Asthma | Pickard et al12 | 0.42 (0.3)* | N/A |
| COPD | Pickard et al12 | 0.52 (0.16)* | N/A |
| Inflammatory arthropathy | Harrison et al3 | N/A | 0.590 (0.52 to 0.69) |
| Heart failure | Gallagher et al13 | 0.64 (0.27) | N/A |
| Diabetes (type II) | Nauck et al14 | 0.78 (0.24) | N/A |
IQR, interquartile range; THA, total hip arthroplasty; TKA, total knee arthroplasty; COPD, chronic obstructive pulmonary disease; N/A, not applicable
COPD was independently associated with WTD status in patients prior to THA. Previous studies have shown significant lower limb arthritis to adversely affect cardiopulmonary function, and thus end-stage DJD may exacerbate COPD.15,16 This phenomenon has also been shown to be reversed following joint arthroplasty.16,17 Similarly, PAD was identified as an independent predictor of WTD status prior to TKA. Again, this is not surprising; arthritis increases the cardiovascular effort of walking and PAD reduces muscle strength in the limb, preventing maximum cardiovascular effort.18,19
Although individual waiting times did not predict WTD status, the increase in waiting times over the study period was mirrored by a rise in the proportion of patients defined as WTD, although this was only statistically significant for knee patients. Shorter overall waiting times in patients WTD is likely due to expedited review and urgent theatre scheduling for patients with the most severe disability.
Our study has quantified the extent to which quality of life is affected by end-stage DJD. Increasingly, referrals to secondary care for joint arthroplasty surgery are being limited by criteria such as BMI or Oxford score. Leaving patients to deteriorate to negative EQ-5D scores limits the outcome they can achieve following joint arthroplasty: patients WTD preoperatively had significantly worse Oxford scores one year following THA and TKA. Both multivariate and ROC analysis confirmed the importance of joint-specific function in determining this poor health state, with an OHS of ≤ 14.5 or an OKS of ≤ 16.5 associated with WTD status. If access to joint arthroplasty is restricted by Oxford score, this gives very narrow windows of opportunity in which to operate: OHS 14 to 24; and OKS 16 to 23. The low specificity of the ROC analysis, however, calls into question using the Oxford scores for this purpose. Discouraging referrals for joint arthroplasty by overzealous gatekeeping in primary care not only has a potentially negative effect on outcome, but may also contribute to the growing opiate epidemic, as patients with increasingly severe disease are managed nonoperatively in the community.
Limitations of this study include the loss to follow-up of nonresponders at one year. Nonresponders had significantly worse median EQ-5D indices prior to both THA and TKA than responders, and were younger and generally more comorbid. Although one-year outcomes were not our primary outcome, this may have affected our conclusions regarding improvement at one year. Although Oxford scores were significantly different statistically between responders and nonresponders, this difference did not reach the minimal clinically important difference. There may be other important covariates that we have not included in our analysis. To fully understand the deterioration in patient populations that leads to a WTD status, a controlled study design would be required. Robust waiting list data were not available for all patients. Despite multiple comorbidities being investigated specifically, depression and anxiety were not. These conditions are known to affect patient satisfaction following joint arthroplasty,20 and may affect symptom perception and thus EQ-5D index. Severe levels of self-reported anxiety and depression were present, however, in only 76/391 of WTD hip patients (20%) and 69/263 of WTD knee patients (26%). Using the anxiety and depression domain of the EQ-5D to predict WTD status is confounded by it being part of the score upon which WTD status is based and so was not reported. These data are from a United Kingdom population and analysis was performed using United Kingdom EQ-5D weighting. While our findings are generalizable to this population, they may not be translatable to other countries with different weightings and healthcare systems.
A total of 19% of patients with end-stage DJD of the hip reported a health state defined as WTD by the EQ-5D score. For the knee, this figure was 12%. This end-stage disease was effectively treated with joint arthroplasty surgery with significant benefits in both health-related quality of life and joint-specific function. WTD status was independently associated with poor joint function and specific comorbidities (COPD and PAD) rather than the demographic variables examined. Other unidentified confounders may contribute, with the regression models here explaining approximately 40% of the variance found. From the results presented here, when patients do deteriorate to WTD levels, the function they achieve following joint arthroplasty, although significantly better than preoperatively, is worse than that obtained in patients not WTD prior to surgery. Leaving patients in pain with end-stage hip or knee DJD has significant consequences on their health-related quality of life and ultimately on the outcome of their joint arthroplasty. Patients with negative EQ-5D scores should be a priority for healthcare delivery.
Take home message
- One-fifth of patients awaiting total hip arthroplasty and 12% of patients awaiting total knee arthroplasty are defined as in a health state ‘worse than death’ (WTD) by the EuroQol five-dimension (EQ-5D) score, a state independently associated with poor joint function measured using Oxford Hip and Knee Scores.
- When patients are in a health state WTD, outcomes are worse following arthroplasty.
- It is not benign to delay or deny patients arthroplasty surgery; patients with end-stage degenerative joint disease live with pain and disability that is more severe than many other chronic health conditions when measured using the EQ-5D.
Author contributions
C. E. H. Scott: Conceptualized the study, Analyzed and interpreted the data, Prepared and reviewed the manuscript
D. J. MacDonald: Collected and analyzed the data, Reviewed the manuscript.
C. R. Howie: Conceptualized the study, Interpreted the data, Prepared and reviewed the manuscript.
Funding statement
This study was supported by NHS Research Scotland (NRS), through C. E. H. Scott.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
C. E. H. Scott reports personal consultancy fees from Stryker not related to this study. C. E. H. Scott and C. R. Howie report an institutional grant paid to the Royal Infirmary of Edinburgh (Edinburgh, United Kingdom) by Stryker not related to this study.
Acknowledgements
The authors thank all orthopaedic surgeons whose patients were included in this study. The authors acknowledge the financial support of NHS Research Scotland (NRS), through C. E. H. Scott of NHS Lothian.
Ethical review statement
Ethical approval was obtained for this study (Scotland (A) Research Ethics Committee 16/SS/0026).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC BY-NC), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
This article was primary edited by P. Page.
Follow the authors @EdinburghKnee
References
- 1.Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-1108. [DOI] [PubMed] [Google Scholar]
- 2.Luo N, Chew LH, Fong KY, et al. . A comparison of the EuroQol-5D and the Health Utilities Index mark 3 in patients with rheumatic disease. J Rheumatol 2003;30:2268-2274. [PubMed] [Google Scholar]
- 3.Harrison MJ, Davies LM, Bansback NJ, et al. . Why do patients with inflammatory arthritis often score states “worse than death” on the EQ-5D? An Investigation of the EQ-5D classification system. Value Health 2009;12:1026-1034. [DOI] [PubMed] [Google Scholar]
- 4.Gaujoux-Viala C, Fautrel B, Guillemin F, et al. . Who are the patients with early arthritis with worse than death scores on the EQ-5D? Results from the ESPOIR cohort. Rheumatology 2013;52:832-838. [DOI] [PubMed] [Google Scholar]
- 5.Jenkins PJ, Clement ND, Hamilton DF, et al. . Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J 2013;95-B:115-121. [DOI] [PubMed] [Google Scholar]
- 6.EuroQol Group EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. [DOI] [PubMed] [Google Scholar]
- 7.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg [Br] 1996;78-B:185-190. [PubMed] [Google Scholar]
- 8.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg [Br] 1998;80-B:63-69. [DOI] [PubMed] [Google Scholar]
- 9.No authors listed The Scottish Index of Multiple Deprivation, 2016. Scottish Government. http://www.gov.scot/Topics/Statistics/SIMD (date last accessed 13 May 2019).
- 10.Beard DJ, Harris K, Dawson J, et al. . Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 2015;68:73-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernfort L, Gerdle B, Husberg M, Levin LA. People in states worse than dead according to the EQ-5D UK value set: would they rather be dead? Qual Life Res 2018;27:1827-1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pickard AS, Wilke C, Jung E, et al. . Use of a preference-based measure of health (EQ-5D) in COPD and asthma. Respir Med 2008;102:519-536. [DOI] [PubMed] [Google Scholar]
- 13.Gallagher AM, Lucas R, Cowie MR. Assessing health-related quality of life in heart failure patients attending an outpatient clinic: a pragmatic approach. ESC Heart Fail 2019;6:3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nauck MA, Buse JB, Mann JFE, et al. . Health-related quality of life in people with type 2 diabetes participating in the LEADER trial. Diabetes Obes Metab 2019;21:525-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ries MD, Philbin EF, Groff GD. Relationship between severity of gonarthrosis and cardiovascular fitness. Clin Orthop Relat Res 1995;313:169-176. [PubMed] [Google Scholar]
- 16.Macnicol MF, McHardy R, Chalmers J. Exercise testing before and after hip arthroplasty. J Bone Joint Surg [Br] 1980;62-B:326–331. [DOI] [PubMed] [Google Scholar]
- 17.Ries MD, Philbin EF, Groff GD, et al. . Effect of total hip arthroplasty on cardiovascular fitness. J Arthroplasty 1997;12:84–90. [DOI] [PubMed] [Google Scholar]
- 18.Baloch ZQ, Abbas SA, Marone L, Ali A. Cardiopulmonary exercise testing limitation in peripheral arterial disease. Ann Vasc Surg 2018;52:108–115. [DOI] [PubMed] [Google Scholar]
- 19.McDermott MM, Criqui MH, Greenland P, et al. . Leg strength in peripheral arterial disease: associations with disease severity and lower-extremity performance. J Vasc Surg 2004;39:523–530. [DOI] [PubMed] [Google Scholar]
- 20.Scott CE, Howie CR, MacDonald D, Biant LC. Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg [Br] 2010;92-B:1253–1258. [DOI] [PubMed] [Google Scholar]