Abstract
Background
Increased basal metabolic index (BMI) is associated with decreased levels of B-type natriuretic peptide (BNP). This makes the diagnosis of the congestive heart failure challenging in the obese population. We sought to determine the association and strength of the relationship between the two variables.
Methods
The association between BMI and BNP was examined in 405 patients utilizing a retrospective chart review in a single center study. Pearson correlation and regression analyses were performed to identify trends. BNP trends were also correlated with age.
Results
The mean age of patients was 77 years with 45% men and 55% women. Mean BNP level was 1,158 standard deviation (SD) ± 1,537. Mean BMI was 33 SD ± 28. BNP levels were found to be inversely related to increasing BMI (P value < 0.001). Using a cut-off of 3,500 pg/mL, there was a linear negative correlation on the dotted graph. In regression analysis the measure of effect of BMI on BNP levels was -0.90 pg/mL. There was no significant association between age and BNP levels (P = 0.90).
Conclusions
Irrespective of age, obese patients have lower BNP levels, complicating the diagnosis of heart failure exacerbation in such patients. Our results suggest that BNP levels in patients with BMI greater than 33 should be adjusted 9 pg/mL per unit increase in BMI.
Keywords: Obesity, Heart failure exacerbation, Diagnostic biomarkers
Introduction
The diagnosis of acute heart failure (HF) is based primarily on clinical judgment, supported by diagnostic testing. This challenge is accentuated in patients having a high basal metabolic index (BMI), as obesity not only obscures the physical examination findings of acute HF, but also diagnostic biomarker B-type natriuretic peptide (BNP). This is further complicated by a rising trend in obesity around the world. BNP levels were recently found to be inversely related to BMI in HF patients [1-3]. However, these studies had small patient populations with a limited range of BNP levels compared to a small range of BMI. We included patients with an extensive range of continuous variables in an effort not only to clarify the association but also to quantify the relationship between BMI and BNP in acute HF patients. Furthermore, we also took efforts to establish the effect of age on the BNP levels, as it is believed that increasing age is associated with higher BNP levels [4].
Materials and Methods
A retrospective chart review was performed at Abington Hospital-Jefferson Health from 2015 to 2019. Four hundred four patients with the diagnosis of HF exacerbation on admission were included. The initial diagnosis of HF exacerbation was made clinically, based on signs, symptoms and echocardiographic findings. For all patients with confirmed HF exacerbation, we retrospectively searched for the BNP and BMP on the time of presentation to the emergency room. Patients having false elevation of BNP due to other causes were excluded such as sepsis, pulmonary embolism, and chronic kidney disease.
Data was collected into an excel sheet by two independent authors and was cross-checked by the third author. The demographic characteristics like age and gender were also retrieved. The continuous data was reported as means and standard deviations (SD). The association between the two continuous variables was performed utilizing a Pearson correlation test and the relationship between the same variables was assessed using a regression analysis model. The alpha criteria for significance were set at a value less than 0.05. Analysis was performed using the SPSS v22.
For ethical compliance with human/animal study, IRB was approved by the ethical committee of the institution.
Results
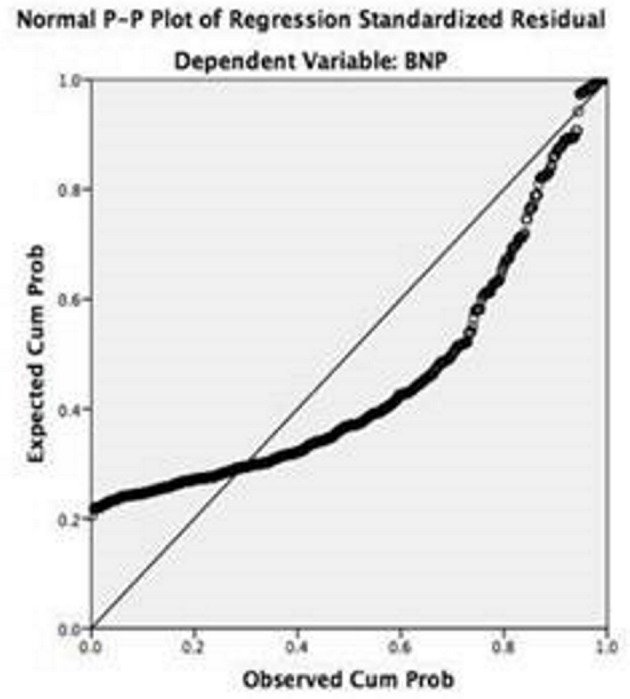
Mean BNP for all 404 patients was 1,158 SD ± 1,537. Mean BMI was 33 SD ± 28. The mean data was distributed in a bell-shaped normal distribution curve as shown in Figure 1.
Figure 1.
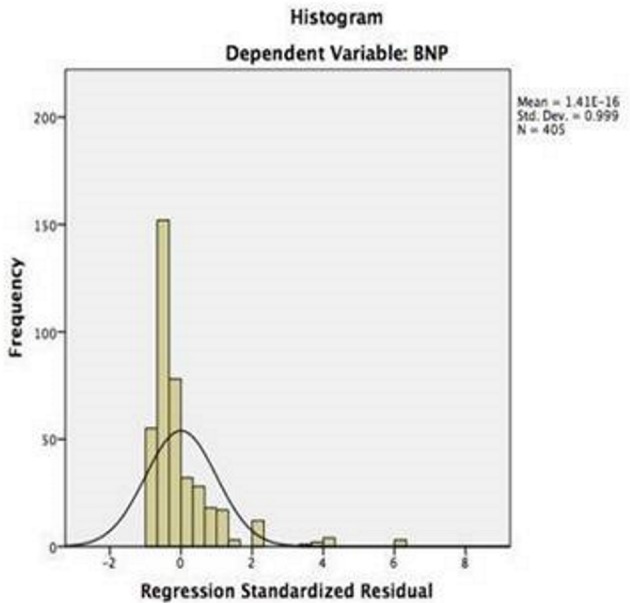
Normal distribution curve for the BNP across the central tendency.
Association between BNP and BMI was determined using a Pearson correlation test. There was an inverse Pearson correlation value (r) between BNP and BMI (r = -0.16), which was statistically significant with a P value of 0.001 (< 0.05). The coefficient of determination was determined by calculating the variance (i.e. r-squared, r2). The adjusted r2 value was comparable to the conventional r2 indicating that the sample size was large enough and the study had significant large power to detect the relationship between the two variables. These measures are shown in Table 1 and Figure 2.
Table 1. The Measure of Central Tendency and Pearson Correlation of the BMI and BNP.
| Mean | Standard deviation | r | r2 | P value | Adjusted r2 | Standard error | |
|---|---|---|---|---|---|---|---|
| BNP | 1,158.27 | 1,536.81 | 0.16 | 0.028 | 0.001 | 0.025 | 1,517.2 |
| BMI | 33.31 | 28.19 |
Figure 2.
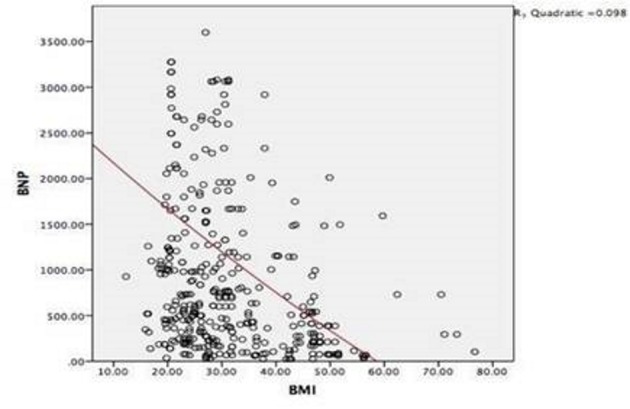
Inverse Pearson correlation of BNP levels with the rising BMI.
The relationship between the BNP and BMI was also determined using a linear regression model. The purpose was to gauge the effect of change in the BMI on the amount of variation in BNP. The analysis of variance (ANOVA) through regression model showed a value (F) of 11.4 with a statistically significant P value of 0.001, degree of freedom (df) 1. The strength of the relationship was calculated using coefficient values. It showed that for every unit increase in BMI, there is an associated BNP decrease of 9.07 pg/mL (beta coefficient, -0.16). This relationship between the two variables had a T value of -3.38 and P value of 0.001 (confidence interval (CI), -14.3 to -3.7). The narrow CI depicts the large sample size and decreased variance in the mean BNP of the included population. The mean residual value (0.00) further validated the analysis. This is shown in Figure 3 and Table 2.
Figure 3.
Regression analysis model showing the negative association between BNP and BMI.
Table 2. Regression Model Analysis of BMI and BNP Quantifying the Measure of Relationship.
| Model | Unstandardized coefficients | Standardized coefficients | t | Sig. | 95.0% CI | ||
|---|---|---|---|---|---|---|---|
| B | Standard error | Beta | Lower | Upper | |||
| BMI | -9.06 | 2.68 | -0.16 | -3.38 | .001 | -14.335 | -3.795 |
The mean age of patients was 77 SD ± 10 (41 - 98) years. We also checked the association between the age and BNP levels. We found that age has a very weak inverse correlation with the BNP levels (r = -0.006) which was not statistically significant (P = 0.45). On ANOVA testing, F value was 0.15 with a nonsignificant P value of 0.90 and df 1. This is shown in Figure 4 and Table 3.
Figure 4.
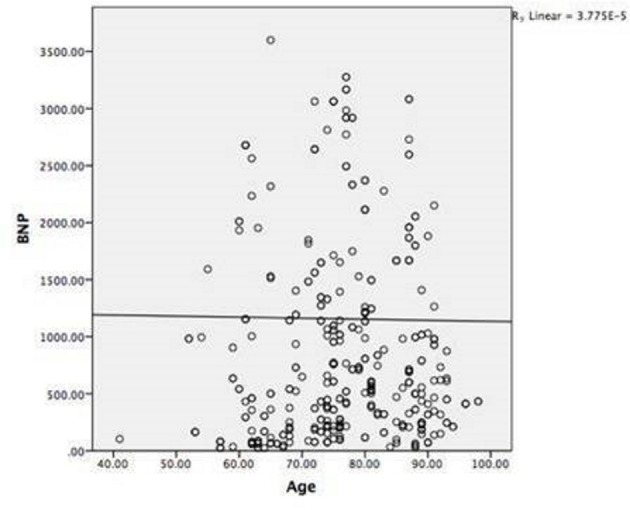
Non-linear association of increasing age with the BNP trend.
Table 3. Mean and Pearson Correlation of the Age Against BNP.
| Mean | Standardized deviation | r | P value | r2 | Adjusted r2 | |
|---|---|---|---|---|---|---|
| BNP | 1,155.7259 | 1,535.76869 | -0.006 | 0.451 | 0.000 | -0.002 |
| Age | 76.5136 | 10.19527 |
Coefficient analysis revealed that for every 1-year increase in the age, there is an associated BNP fall of about 9.26 (beta coefficient, -0.006), T value of -0.123 and P value of 0.902 (CI of -15.6 to 13.8). The narrow CI depicts the large sample size and decreased variance in the mean BNP of the included population. The mean residual value (0.00) further validated the analysis as shown in Table 4.
Table 4. Regression Analysis Model Showing a Weak Relationship of Old Age With BNP Levels.
| Model | Unstandardized coefficients | Standardized coefficients | t | Sig. | 95.0% CI | ||
|---|---|---|---|---|---|---|---|
| B | Standard error | Beta | Lower | Upper | |||
| Age | -0.92 | 7.50 | -0.006 | -0.12 | 0.90 | -15.67 | 13.82 |
Discussion
BNP is a natriuretic peptide secreted by cardiac myocytes in response to the stretch and high ventricular filling pressure. The plasma concentration of BNP aids in the diagnosis of HF exacerbations when used in concert with physical examination and clinical imaging [5]. BNP levels can increase drastically in severe cardiac dysfunction. A BNP value less than 100 pg/mL has a high negative predictive value to rule out an HF diagnosis. Most patients with HF presenting as dyspnea have a BNP level more than 400 pg/mL [6, 7].
Plasma BNP concentrations can be affected by many variables including age, gender and BMI. Prior studies suggest a positive correlation of age and BNP levels. Gender differences showed higher BNP in women as compared to men [8]. Our study is unique in a sense that we found a very weak inverse linear correlation of age with BNP levels (r = -0.006), which was not statistically significant (P = 0.45). Our study showed that for 1-year increase in the age, there is an associated BNP fall of about 9.26 (beta coefficient, -0.006), but it was nonsignificant (T value of -0.12, P value of 0.90, CI of -15.6 to 13.8). The regression analysis in our study showed a very weak relationship of old age with BNP levels. Thus, older age does have some weak inverse effect on BNP levels. Our patients, however, had no pediatric population and the mean age was 76 years with a range of 41 - 98 years, signifying that middle- and old-aged population was included.
Another modifiable variable of BNP level is BMI. Obese patients have a lower BNP levels as compared to people with normal BMI [9]. In 2004, Wang et al were the first ones to demonstrate an inverse relationship between BMI and BNP in 3,389 non-HF subjects from the original Framingham Heart Study offspring cohort. Multivariable regression analysis was adjusted for left atrial size and left ventricular mass. The mean plasma BNP levels were 12.7, 15.5 and 21.4 in obese, overweight and lean participants, respectively. This study was unable to conclude causation of low BNP given the cross-sectional design [10]. This result was further supported by a large population-based cohort of the Dallas Heart Study, demonstrating an inverse relationship of BMI, BNP, and an additional marker, N-terminal pro-brain natriuretic peptide (NT-proBNP). The study included a random sample of 2,707 patients aged 30 to 65. Multivariable regression analysis adjusted for ethnicity, age, gender, hypertension, left ventricular mass and end diastolic volume demonstrated high BMI level with low BNP and NT-proBNP levels (P < 0.001) [9]. Our study also shows an inverse relationship between BMI and BNP, but it is unique in the sense that measurement of BMI and BNP was in acute congestive heart failure (CHF) patients. In our study, the Pearson correlation value (r) between the BNP and BMI was found to be inverse (r = -0.16), which was statistically significant with a P value of 0.001 (< 0.05). The relationship between the BNP and BMI was also determined using a linear regression model. The purpose was to gauge the effect of change in the BMI on the amount of variation in the BNP. ANOVA demonstrated a value (F) of 11.4, with a statistically significant P value (0.001, df 1). The strength of relationship using the coefficient values showed that for every unit increase in the BMI, there is an associated BNP fall of 9.07 (B of -0.16, T value of -3.38, P value of 0.001 and CI of -14.3 to -3.7). The narrow CI depicts the large sample size and decreased variance in the mean BNP of the included population.
A variety of explanations were proposed to explain inverse relationship between BMI and BNP. Some of the organs involved to explain this physiology include the kidney, adipose tissue and heart. Regarding the role of the kidney, one hypothesis is that obesity increases the glomerular filtration rate thereby increasing the clearance of BNP [11]. Regarding the role of adipose tissue, several studies have suggested that obese patients have low levels of BNP due to alterations of BNP clearance and degradation. Receptors that facilitate removal of BNP from the circulation in obese patients include natriuretic peptide clearance receptors (NPR-C) [12-14]. This increased clearance of BNP linked to the decreased inhibition of renin-angiotensin system, decreased natriuretic effect and enhanced sodium retention in obese patients [15, 16]. Fasting and weight loss are known to decrease expression of adipose cellular NPR-C which can lead to increased BNP levels [17]. Regarding the role of the heart, the inverse relationship of BMI with BNP is thought to be due to decreased production rather than decreased clearance. This is supported by data from animal studies that find both BNP and NT-proBNP were more closely related to the muscle mass rather than fat mass. A study performed in rats by Cabiati et al reported significantly lower levels of mRNA of BNP in obese rats as compared to control rats [18]. A human study by Shah et al also suggested decreased production of BNP in obese people with low levels of coronary sinus BNP, as evidence of production [19].
Obesity is one of the major risk factors for HF. It can cause HF through lipoapoptosis, impaired fatty acid oxidation, or increased cardiopulmonary volume due to enhance vasodilation [15, 20, 21]. Researchers have theorized a “bidirectional relationship” between BNP and adiposity. Lipolysis in adipocytes has been shown to be caused by BNP. A lower BNP level decreases lipolysis.
Limitations
We did not study other factors which could have falsely elevated the BNP levels such as end-stage renal disease, sepsis and pulmonary embolism. The pediatric and younger population populations were not included.
Conclusions
Patients with high BMI have lower BNP levels, making the diagnosis of HF exacerbation more difficult in such patients. Based on our data we suggest adjusting BNP levels in patients with BMI greater than 33 kg/m2. Their BNP should be adjusted 9 pg/mL per unit increase in BMI, provided the patient has no other confounding factors. Larger scale studies including all population groups with consideration of their comorbidities can confirm these findings. We believe that this study will provide direction for these future studies.
Acknowledgments
We want to thank our program director Dr. Margot Boigon for providing research opportunities at Abington Hospital.
Financial Disclosure
The authors report no financial relationship regarding the content herein.
Conflict of Interest
The authors report no conflict of interest regarding the content herein.
Informed Consent
Informed consent was waived via IRB.
Author Contributions
WU contributed to the conception, analysis, and methodology; AA wrote the Introduction; YS wrote the Discussion; US contributed to the resources and data collection; HMAA contributed to literature search; MAC contributed to data collection; VF contributed to critical review and supervision.
References
- 1.Wang TJ, Larson MG, Levy D, Leip EP, Benjamin EJ, Wilson PW, Sutherland P. et al. Impact of age and sex on plasma natriuretic peptide levels in healthy adults. Am J Cardiol. 2002;90(3):254–258. doi: 10.1016/S0002-9149(02)02464-5. [DOI] [PubMed] [Google Scholar]
- 2.Li AM, Au CT, Zhu JY, Chan KC, Chan MH, Lee DL, Wing YK. Plasma natriuretic peptides in children and adolescents with obstructive sleep apnea and their changes following intervention. Front Pediatr. 2014;2:22. doi: 10.3389/fped.2014.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krauser DG, Lloyd-Jones DM, Chae CU, Cameron R, Anwaruddin S, Baggish AL, Chen A. et al. Effect of body mass index on natriuretic peptide levels in patients with acute congestive heart failure: a ProBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. Am Heart J. 2005;149(4):744–750. doi: 10.1016/j.ahj.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Hill SA, Booth RA, Santaguida PL, Don-Wauchope A, Brown JA, Oremus M, Ali U. et al. Use of BNP and NT-proBNP for the diagnosis of heart failure in the emergency department: a systematic review of the evidence. Heart Fail Rev. 2014;19(4):421–438. doi: 10.1007/s10741-014-9447-6. [DOI] [PubMed] [Google Scholar]
- 5.Luchner A, Stevens TL, Borgeson DD, Redfield M, Wei CM, Porter JG, Burnett JC Jr. Differential atrial and ventricular expression of myocardial BNP during evolution of heart failure. Am J Physiol. 1998;274(5):H1684–1689. doi: 10.1152/ajpheart.1998.274.5.H1684. [DOI] [PubMed] [Google Scholar]
- 6.Maisel A. B-type natriuretic peptide levels: diagnostic and prognostic in congestive heart failure: what's next? Circulation. 2002;105(20):2328–2331. doi: 10.1161/01.CIR.0000019121.91548.C2. [DOI] [PubMed] [Google Scholar]
- 7.Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT. Does this dyspneic patient in the emergency department have congestive heart failure? JAMA. 2005;294(15):1944–1956. doi: 10.1001/jama.294.15.1944. [DOI] [PubMed] [Google Scholar]
- 8.Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40(5):976–982. doi: 10.1016/S0735-1097(02)02059-4. [DOI] [PubMed] [Google Scholar]
- 9.Das SR, Drazner MH, Dries DL, Vega GL, Stanek HG, Abdullah SM, Canham RM. et al. Impact of body mass and body composition on circulating levels of natriuretic peptides: results from the Dallas Heart Study. Circulation. 2005;112(14):2163–2168. doi: 10.1161/CIRCULATIONAHA.105.555573. [DOI] [PubMed] [Google Scholar]
- 10.Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Wilson PW, Vasan RS. Impact of obesity on plasma natriuretic peptide levels. Circulation. 2004;109(5):594–600. doi: 10.1161/01.CIR.0000112582.16683.EA. [DOI] [PubMed] [Google Scholar]
- 11.Griffin KA, Kramer H, Bidani AK. Adverse renal consequences of obesity. Am J Physiol Renal Physiol. 2008;294(4):F685–696. doi: 10.1152/ajprenal.00324.2007. [DOI] [PubMed] [Google Scholar]
- 12.Sengenes C, Berlan M, De Glisezinski I, Lafontan M, Galitzky J. Natriuretic peptides: a new lipolytic pathway in human adipocytes. FASEB J. 2000;14(10):1345–1351. doi: 10.1096/fasebj.14.10.1345. [DOI] [PubMed] [Google Scholar]
- 13.Sarzani R, Dessi-Fulgheri P, Paci VM, Espinosa E, Rappelli A. Expression of natriuretic peptide receptors in human adipose and other tissues. J Endocrinol Invest. 1996;19(9):581–585. doi: 10.1007/BF03349021. [DOI] [PubMed] [Google Scholar]
- 14.Horwich TB, Hamilton MA, Fonarow GC. B-type natriuretic peptide levels in obese patients with advanced heart failure. J Am Coll Cardiol. 2006;47(1):85–90. doi: 10.1016/j.jacc.2005.08.050. [DOI] [PubMed] [Google Scholar]
- 15.Frohlich ED, Messerli FH, Reisin E, Dunn FG. The problem of obesity and hypertension. Hypertension. 1983;5(5 Pt 2):III71–78. doi: 10.1161/01.HYP.5.5_Pt_2.III71. [DOI] [PubMed] [Google Scholar]
- 16.Dessi-Fulgheri P, Sarzani R, Rappelli A. The natriuretic peptide system in obesity-related hypertension: new pathophysiological aspects. J Nephrol. 1998;11(6):296–299. [PubMed] [Google Scholar]
- 17.Sarzani R, Paci VM, Zingaretti CM, Pierleoni C, Cinti S, Cola G, Rappelli A. et al. Fasting inhibits natriuretic peptides clearance receptor expression in rat adipose tissue. J Hypertens. 1995;13(11):1241–1246. doi: 10.1097/00004872-199511000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Cabiati M, Raucci S, Liistro T, Belcastro E, Prescimone T, Caselli C, Matteucci M. et al. Impact of obesity on the expression profile of natriuretic peptide system in a rat experimental model. PLoS One. 2013;8(8):e72959. doi: 10.1371/journal.pone.0072959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah Z, Wiley M, Sridhar AM, Masoomi R, Biria M, Lakkireddy D, Dawn B. et al. Inverse correlation of venous brain natriuretic peptide levels with body mass index is due to decreased production. Cardiology. 2017;137(3):159–166. doi: 10.1159/000464111. [DOI] [PubMed] [Google Scholar]
- 20.Messerli FH, Sundgaard-Riise K, Reisin ED, Dreslinski GR, Ventura HO, Oigman W, Frohlich ED. et al. Dimorphic cardiac adaptation to obesity and arterial hypertension. Ann Intern Med. 1983;99(6):757–761. doi: 10.7326/0003-4819-99-6-757. [DOI] [PubMed] [Google Scholar]
- 21.Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L. et al. Lipotoxic heart disease in obese rats: implications for human obesity. Proc Natl Acad Sci U S A. 2000;97(4):1784–1789. doi: 10.1073/pnas.97.4.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]


