Abstract
Objective:
To investigate the success rate (technical precision) of ultrasound-guided lumbar transforaminal epidural steroid injection, which was validated by conventional fluoroscopic technique.
Methods:
A total of 20 patients with unilateral single-level lumbar foraminal disc protrusion causing radiculopathy were enrolled. Using transforming route, the needle location was determined by an axial (transvers) view of the ultrasound with fluoroscopic confirmation. We determined the needle placement accuracy of ultrasound- guided lumbar transforaminal injections approach.
Results:
The accuracy of ultrasound-guided interventions was 90% as confirmed by fluoroscopy. There were 2 failed cases at the L4-L5 level in the US-guided. The success rate in L5-S1 level was 100%, in L4-L5 level was 80% and in L3-L4 level was 100%. No complications were noted.
Conclusion:
Ultrasound-guided lumbar transforaminal epidural injections are accurate and feasible in clinical setting with an accuracy of 90% and no complications.
Key Words: Epidural injection, Fluoroscopy, Chronic pain management, Radiculopathy
Introduction
Low back pain and radiculopathy are among the most common diseases, and lumbar transforaminal epidural injection (TFEI), is one of the frequently used approaches for pain control and management of these diseases [1]. However, risks and severe adverse effects, such as paraplegia, quadriplegia, and cerebellar infarction, may be inevitable [2-6]. Complications may result from mechanical injury to the spine due to direct needle insertion, radiculomedullary arteries, and accidental intra-arterial injection of corticosteroid particles which may result in arterial embolism [7,8]. In order to provide anatomic precision and accuracy and also to minimize the associated risks, lumbar TFEI is normally performed under the guide of fluoroscopy or computed tomography [9-13] which make it the standard method for lumbar TFEI [1,14,15].
Fluoroscopy is most commonly imaging guide which is used in interventional spine procedures4 and is frequently performed to confirm the location of epidural needle. Radiation exposure is the major concern associated with obtaining fluoroscopic images which can be diminished using proper shields. Although fluoroscopy provide accurate real-time and continuous images, but this increases the overall exposure time, which puts both physician and patient at the risk of radiation exposure during the procedure.
The use of ultrasound (US) to perform injections for chronic pain has significantly increased in the past decade [16]. This increase is attributed to its multiple advantages over other imaging modalities including ease of performance, absence of ionizing radiation, better visualization of soft tissue (i.e., muscle, ligament) and blood vessels, real time visualization of needle advancement and, at times, the ability to observe the spread of injectate [3]. By using ultrasound, the need for use of contrast agents which can be associated with allergic reactions and renal damage is reduced. It can be performed portable, and is cost effective. However, several concerns such as accuracy and precision, reliability and patient safety should be addressed. To the best of our knowledge, only one study has been conducted in cadavers to evaluate accuracy and feasibility of US-guided lumbar TFEI.31 In this study, we investigated the accuracy (technical precision) of ultrasound guided lumbar transforaminal epidural injection, which was confirmed by conventional fluoroscopic technique.
Materials and Methods
Study population
This non-randomized clinical feasibility study was performed on 20 patients in a tertiary health care center during November and December 2017. Study population were all patients with unilateral single-level lumbar foraminal disc protrusion causing radiculopathy referring to department of pain whose diagnosis were previously confirmed by MRI and were candidate to undergo lumbar transforaminal epidural steroid injections. Study protocol was reviewed and approved by the institutional review board of Shahid Beheshti University of Medical Sciences (Tehran, Iran), and the hospital ethics committee. Patients were informed about the study procedure and informed consent was signed by all of them prior to the study. Written informed consent to publish the details was also obtained from the participant or parent/guardian. Inclusion criteria were age ≥18 years, ASA class I-II, and single level foraminal disc protrusion at either levels of L3-L4, L4-L5 or L5-S1. Patients with local or systemic infections; spinal stenosis, central disc herniation with axial pain, herniated degenerative disc, spinal deformity, vertebral fracture, inflammatory spondylopathy, duration of symptoms for more than six months, contraindication of lumbar surgery, failure to respond to traditional treatments (physical therapy, anti-inflammatories, or analgesics); history of lumbar spine surgery or previous epidural injection; opioid abuse, hyperextension pain, pregnancy (regarding female patients) neoplastic diseases, neurological defects, coagulopathy; apparent mental disorders; corticosteroid or contrast agent allergies were excluded from the study.
Study protocol
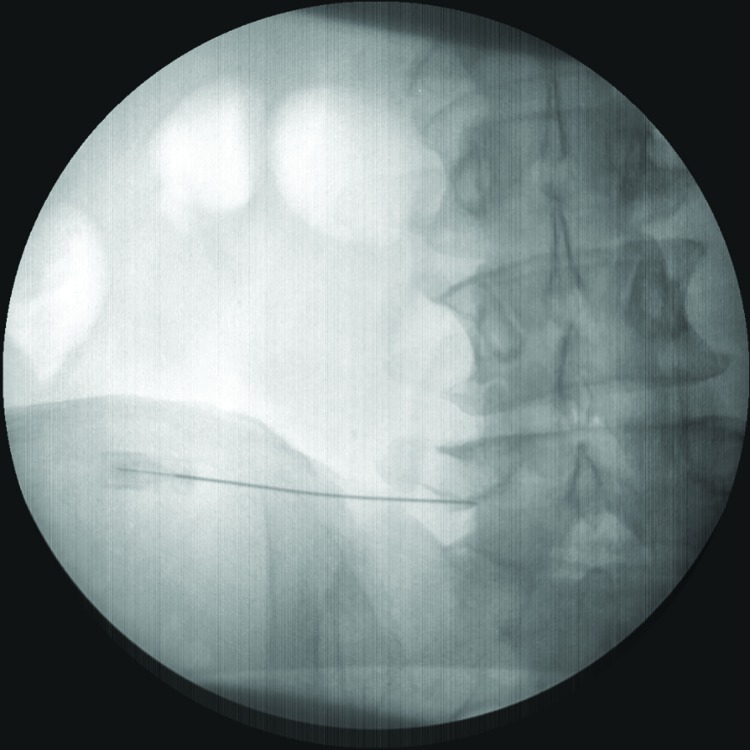
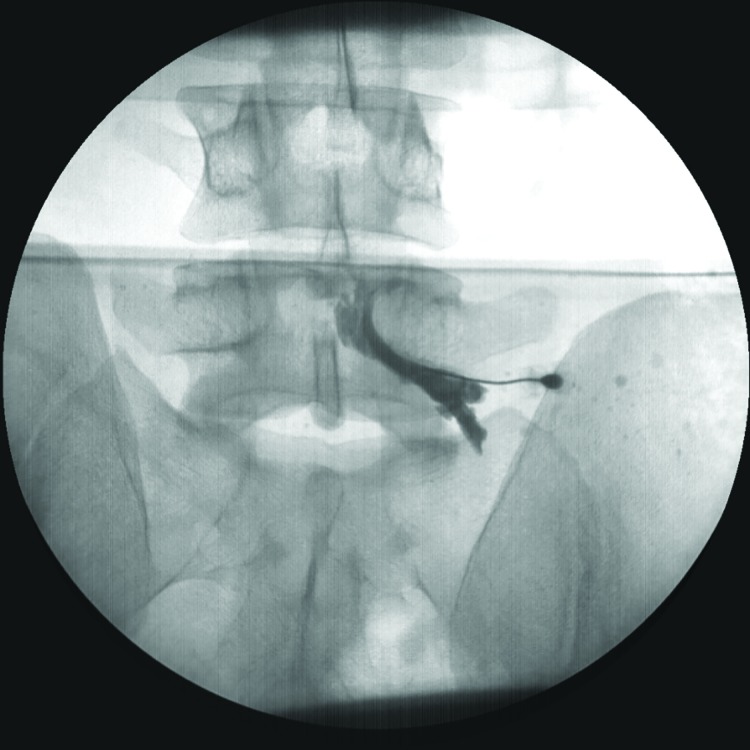
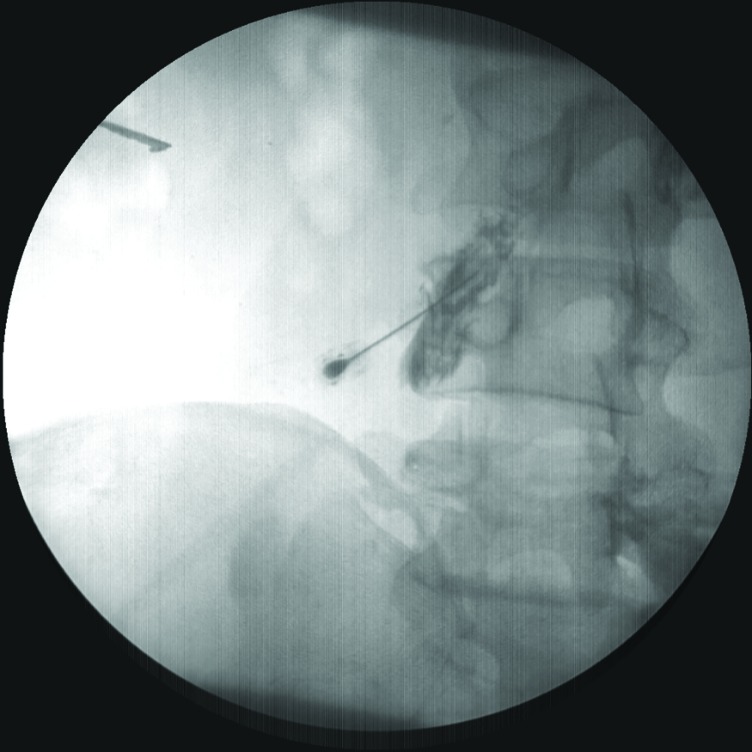
For all patients, standard monitoring (noninvasive blood pressure, pulse oximetry and electrocardiography) was applied upon arrival to the operating room. Procedural sedation was achieved using 1mg/ml of intravenous midazolam and patients were placed in a prone position. After sterilization and preparation of the site, the skin was anesthetized by subcutaneous injection of 3mL 1% lidocaine. A 22-gauge, 3.5 inch, Quincke-tipped spinal needle was used for all injections. The needle location was determined by an axial (transvers) view of ultrasound (Figure 1). In the lateral view and in-plane approach, the needle was placed under the pedicle on the ventral foramen between the vertebrae and in the anterior-posterior view, the needle was just placed under the middle of the corresponding pedicle. The needle was then pushed forward in the pathologic foramen under the guide of ultrasound. Once the needle was in position, and after negative aspiration for cerebrospinal fluid or blood, 1 mL of contrast dye (OMNIPAQUE ™, GE Healthcare, UK) was injected in the most medially visible shadow of the vertebral body and epidurogram results were recorded in the fluoroscope for evaluation of the contrast distribution pattern. During injection, an ultrasound image was taken to determine the distribution of the contrast dye in the posterior and lateral anterior aspect, which was confirmed by conventional fluoroscopic technique. The distribution of contrast dye was them evaluated (Figures 2 and 3). After validation of the correct placement of the needle, 2 ml of bupivacaine 2% mixed with 2 ml of dexamethasone 4 mg/ml was injected. In case of failure, repositioning of the needle was done by the guide of fluoroscopy. Any complications were noted.
Fig. 1.
Ultrasonographic image – Transverse view at L3-L4 foramen
Fig. 2.
Fluoroscope verification of needle placement at L5-S1
Fig. 3.
Fluoroscope verification of dye spread at L5-S1
Outcome measures
The main outcome of the study was to evaluate the accuracy of ultrasound in needle placement which was defined as the correct needle placement under the guide of ultrasound in the foraminal area. Specifically, accuracy of the spinal segment identification and pattern of radiopaque contrast spread were evaluated. Images were reported by two physicians who were not aware of each other's reports. In case of disagreement upon an image, that participant was excluded from the study.
Statistical analysis
Data analysis was performed using statistical package for social sciences (SPSS Inc., Chicago, Illinois, USA) for Windows, version 19.0. Results were reported as mean ± SD for quantitative variables and percentages for categorical variables.
Results
The mean age of patients was 48.7 ± 8.5 (35-64) years old. Eleven patients were male (55%) and 9 (45%) were female. Treatment level included the following cases: L5-S1: 9 cases (45%), L4-L5: 10 cases (50%) and L3-L4: 1 case (5%), including 12 cases (60%) on the right side and 8 cases (40%) on the left side. The accuracy of US-guided interventions was 90% as confirmed by fluoroscopy. There were 2 failed cases at the L4-L5 level in the US-guided (Figure 4). The success ratio in L5-S1 level was 100%, in L4-L5 level was 80% and in L3-L4 level was 100%. In the two failed cases, the needle tip was positioned inappropriately way too close to the midline. Therefore, the needle had to be repositioned. Repositioning was done under US guidance, and correct replacement was then confirmed by fluoroscopy. No complications were noted.
Fig. 4.
Anteroposterior fluoroscopy demonstrated aberrant (Psoas Muscle) contrast flow
Discussion
Interventional pain managements play a significant role in the treatment of different painful conditions and Image-guided interventional procedures have arisen as an alternative for management of back pain [17,18]. Lumbar TFEI is associated with minimal risk of dural puncture and better efficacy on pain relief, compared to posterior median and paramedian injection approaches [15, 19-21]. Transforaminal injections are performed under the guide of fluoroscopy/CT/MRI [22,23]. Though sonographic imaging has been revealed to be reliable and accurate in needle placement for TF approaches.
In our study, the accuracy of the lumbar TFEI under US guidance was 90%, and the accuracy of needle-tip on each lumbar level under US guidance was 80%-100%, without complications in any of the patients. Hashemi et al. reported that the accuracy of ultrasound in caudal epidural injections was 95.8% [24]. They also showed that the accuracy of ultrasound guided needle placement for Lumbar medial branch nerve block was 98% [25]. Yang G et al. have reported an accuracy of 85% for the US-guided interventions in lumbar TFEI [26]. According to the findings of Chumnanvej et al., when the lumbar injection was performed with midline approach, the accuracy of needle-tip on lumbar nerve root under ultrasound guidance was 62.82% and the accuracy of needle-tip on each lumbar nerve root under ultrasound guidance with fluoroscopic confirmation ranged from 7.14% to 80.95% [27].
In another study, it has been reported that in lumbosacral selective nerve root block by ultrasound guidance, the accuracy of needle-tip localization was 80% [28]. For rapid visualization of the target position, the needle is guided toward the target structure within a few seconds under real-time, safe and controlled conditions. Therefore, a rapid US-guided injection is not surprising. The US-guided lumbar TFEI is a complicated technique. Due to the high acoustic impedance of bone, and visualization interruption due to bony artifacts, the anatomic landmarks of the lumbar region are poorly determined by US-guidance [29].
In this study, we used an in-plane approach in which the needles were advanced strictly parallel to the long axis of the transducer to keep them along with the echoes. In-plane approach provides real-time monitoring of the inserted needle along its entire length. In fact, the needle appears as a single distinct line-shaped echo pattern, which is different with only a few dot-like reflections when other techniques are used. Nonetheless, precise and accurate management of the transducer is compulsory to get the best visualization of the complete needle. Other studies have reported several benefits of sonography as a useful adjunct during various forms of injection applications such as: imaging of individual anatomic parts, real-time needle guidance, visualization of the spread of local anesthetics, minimal risk of complications, dose reduction of local anesthetics, and shortening of onset time. In our study, ultrasound guidance was accurate and reliable in correct needle placement for lumbar TFEI. Moreover, it was an affordable and safe technique for approaching the lumbar TFEI using ultrasound. Several benefits of using ultrasound guidance as an adjunct technique during different forms of injection applications have been previously reported, including feasibility, repeatability, real-time needle advancement, imaging of the individual anatomic parts, reduction of dose of drug injection, reduction of the risk of complications and visualization of the spread of agent, soft tissues, nerves and blood vessels [15, 30-33].
In conclusion, ultrasound-guided lumbar transforaminal epidural injections are accurate and feasible in clinical setting with advantages in delineating anatomy and lack of ionizing radiation.
Conflict of Interest:
The author reports no financial/non-financial conflicts of interest regarding this work.
References
- 1.Ziai WC, Ardelt AA, Llinas RH. Brainstem stroke following uncomplicated cervical epidural steroid injection. Arch Neurol. 2006;63(11):1643–6. doi: 10.1001/archneur.63.11.1643. [DOI] [PubMed] [Google Scholar]
- 2.Suresh S, Berman J, Connell DA. Cerebellar and brainstem infarction as a complication of CT-guided transforaminal cervical nerve root block. Skeletal Radiol. 2007;36(5):449–52. doi: 10.1007/s00256-006-0215-0. [DOI] [PubMed] [Google Scholar]
- 3.McMillan MR, Crumpton C. Cortical blindness and neurologic injury complicating cervical transforaminal injection for cervical radiculopathy. Anesthesiology. 2003;99(2):509–11. doi: 10.1097/00000542-200308000-00038. [DOI] [PubMed] [Google Scholar]
- 4.Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003;103(1-2):211–5. doi: 10.1016/s0304-3959(02)00343-3. [DOI] [PubMed] [Google Scholar]
- 5.Bose B. Quadriparesis following cervical epidural steroid injections: case report and review of the literature. Spine J. 2005;5(5):558–63. doi: 10.1016/j.spinee.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Silbergleit R, Mehta BA, Sanders WP, Talati SJ. Imaging-guided injection techniques with fluoroscopy and CT for spinal pain management. Radiographics. 2001;21(4):927–39; discussion 940-2. doi: 10.1148/radiographics.21.4.g01jl15927. [DOI] [PubMed] [Google Scholar]
- 7.Chang A, Pochert S, Romano C, Brook A, Miller T. Safety of 1000 CT-guided steroid injections with air used to localize the epidural space. AJNR Am J Neuroradiol. 2011;32(9):E175–7. doi: 10.3174/ajnr.A2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashemi SM, Aryani MR, Momenzadeh S, Razavi SS, Mohseni G, Mohajerani SA, et al. Comparison of Transforaminal and Parasagittal Epidural Steroid Injections in Patients With Radicular Low Back Pain. Anesth Pain Med. 2015;5(5):e26652. doi: 10.5812/aapm.26652v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hashemi M, Mofrad MK, Mohajerani SA, Kazemi SM, Radpey B, Zali A. Anatomical Flow Pattern of Contrast in Lumbar Epidural Space: A Human Study with a Midline vs Parasagittal Interlaminar Approach under Fluoroscopy. Pain Physician. 2015;18(4):317–24. [PubMed] [Google Scholar]
- 10.Hashemi SM, Dadkhah P, Taheri M, Abootorabi HS. Effects of Percutaneous Laser Disc Decompression (PLDD) on Clinical Outcome of Teared Vs Intact Protruded Intervertebral Discs: A Prospective Cohort Study. Orthopaedic Surgery and Traumatology. 2018;2(1):279–85. [Google Scholar]
- 11.Kim PS. Role of injection therapy: review of indications for trigger point injections, regional blocks, facet joint injections, and intra-articular injections. Curr Opin Rheumatol. 2002;14(1):52–7. doi: 10.1097/00002281-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Carrino JA, Morrison WB, Parker L, Schweitzer ME, Levin DC, Sunshine JH. Spinal injection procedures: volume, provider distribution, and reimbursement in the US medicare population from 1993 to 1999. Radiology. 2002;225(3):723–9. doi: 10.1148/radiol.2253011401. [DOI] [PubMed] [Google Scholar]
- 13.Kothari K, Sahu DK. Ultrasonography versus fluoroscopy in modern pain management. Indian Journal of Pain. 2016;30(2):71. [Google Scholar]
- 14.Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005;24(1):33–8. doi: 10.7863/jum.2005.24.1.33. [DOI] [PubMed] [Google Scholar]
- 15.Greher M, Scharbert G, Kamolz LP, Beck H, Gustorff B, Kirchmair L, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004;100(5):1242–8. doi: 10.1097/00000542-200405000-00028. [DOI] [PubMed] [Google Scholar]
- 16.Gelinimoghaddam A, Hashemi M, Dadkhah P, Taheri M. Comparative studies on the success level of sonographic guided epidural steroid injection and its effectiveness with fluoroscopy techniques in treating lumbar radicular pain. Bioscience Biotechnology Research Communications. 2017;10(2):148–54. [Google Scholar]
- 17.Grau T, Leipold RW, Fatehi S, Martin E, Motsch J. Real-time ultrasonic observation of combined spinal-epidural anaesthesia. Eur J Anaesthesiol. 2004;21(1):25–31. doi: 10.1017/s026502150400105x. [DOI] [PubMed] [Google Scholar]
- 18.Cansever T, Kabatas S, Civelek E, Kircelli A, Yilmaz C, Musluman M, et al. Transforaminal epidural steroid injection via a preganglionic approach for the treatment of lumbar radicular pain. Turk Neurosurg. 2012;22(2):183–8. doi: 10.5137/1019-5149.JTN.5151-11.3. [DOI] [PubMed] [Google Scholar]
- 19.Derby R, Kine G, Saal JA, Reynolds J, Goldthwaite N, White AH, et al. Response to steroid and duration of radicular pain as predictors of surgical outcome. Spine (Phila Pa 1976) 1992;17(6 Suppl):S176–83. doi: 10.1097/00007632-199206001-00020. [DOI] [PubMed] [Google Scholar]
- 20.Gangi A, Dietemann JL, Mortazavi R, Pfleger D, Kauff C, Roy C. CT-guided interventional procedures for pain management in the lumbosacral spine. Radiographics. 1998;18(3):621–33. doi: 10.1148/radiographics.18.3.9599387. [DOI] [PubMed] [Google Scholar]
- 21.Nikooseresht M, Hashemi M, Mohajerani SA, Shahandeh F, Agah M. Ultrasound as a screening tool for performing caudal epidural injections. Iran J Radiol. 2014;11(2):e13262. doi: 10.5812/iranjradiol.13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hashemi M, Jazayeri SM, Niaki AS, Nikooseresht M, Hosseinpanah A, Razavi SS, et al. Ultrasound guidance for interventional pain management of lumbar facet joint pain: an anatomical and clinical study. Iranian Journal of Radiology. 2017;14(1) [Google Scholar]
- 23.Yang G, Liu J, Ma L, Cai Z, Meng C, Qi S, Zhou H. Ultrasound-guided Versus Fluoroscopy-controlled Lumbar Transforaminal Epidural Injections: A Prospective Randomized Clinical Trial. Clin J Pain. 2016;32(2):103–8. doi: 10.1097/AJP.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 24.Chumnanvej S, Wetchagama N, Kounsongtham V. Accuracy of needle-tip localization by ultrasound guidance lumbar selective nerve root block: a prospective clinical study of 78 lumbar nerve roots block. J Med Assoc Thai. 2011;94(12):1451–6. [PubMed] [Google Scholar]
- 25.Chumnanvej S, Kittayapirom K, Chumnanvej S. Visualization of Needle-Tip Localization by Ultrasound Guidance with Contrast Bubble in Lumbar Selective Nerve Root Block: Clinical Pilot Study. World Neurosurg. 2018;111:e418–e423. doi: 10.1016/j.wneu.2017.12.079. [DOI] [PubMed] [Google Scholar]
- 26.Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: an alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000;25(6):600–4. doi: 10.1053/rapm.2000.18184. [DOI] [PubMed] [Google Scholar]
- 27.Galiano K, Obwegeser AA, Bodner G, Freund MC, Gruber H, Maurer H, et al. Ultrasound-guided facet joint injections in the middle to lower cervical spine: a CT-controlled sonoanatomic study. Clin J Pain. 2006;22(6):538–43. doi: 10.1097/01.ajp.0000202977.98420.27. [DOI] [PubMed] [Google Scholar]
- 28.Galiano K, Obwegeser AA, Bodner G, Freund MC, Gruber H, Maurer H, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005;30(4):391–6. doi: 10.1016/j.rapm.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 29.Provenzano DA, Narouze S. Sonographically guided lumbar spine procedures. J Ultrasound Med. 2013;32(7):1109–16. doi: 10.7863/ultra.32.7.1109. [DOI] [PubMed] [Google Scholar]
- 30.Marhofer P, Schrögendorfer K, Wallner T, Koinig H, Mayer N, Kapral S. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med. 1998;23(6):584–8. doi: 10.1016/s1098-7339(98)90086-4. [DOI] [PubMed] [Google Scholar]
- 31.Cotti E, Campisi G, Ambu R, Dettori C. Ultrasound real-time imaging in the differential diagnosis of periapical lesions. Int Endod J. 2003;36(8):556–63. doi: 10.1046/j.1365-2591.2003.00690.x. [DOI] [PubMed] [Google Scholar]
- 32.Gofeld M, Bristow SJ, Chiu SC, McQueen CK, Bollag L. Ultrasound-guided lumbar transforaminal injections: feasibility and validation study. Spine (Phila Pa 1976) 2012;37(9):808–12. doi: 10.1097/BRS.0b013e3182340096. [DOI] [PubMed] [Google Scholar]
- 33.Kim PS. Role of injection therapy: review of indications for trigger point injections, regional blocks, facet joint injections, and intra-articular injections. Curr Opin Rheumatol. 2002;14(1):52–7. doi: 10.1097/00002281-200201000-00010. [DOI] [PubMed] [Google Scholar]