Abstract
Chronic physical illness is associated with significant vulnerability for emotional disorders. Some studies suggest anxiety and depression are common comorbidities in individuals with alpha-1 antitrypsin deficiency (AATD). Many aspects of AATD contribute to quality of life impairment. Delays in diagnosis, high costs of disease treatment, and inherited genetic risk add to the symptom burden of lung or liver disease to alter quality of life. Whether anxiety and depression independently contribute to quality of life impairment remains unproven. In this article, we aim to review current literature examining the impact of anxiety and depression on the quality of life of AATD-affected individuals. Multifaceted approaches may best meet the needs of a heterogeneous population and are the best future strategies to minimize these emotional impacts and assure highest quality of life possible. More research studies are needed to achieve this ambitious goal and make life of AATD-affected individuals better by minimizing the effects of anxiety and depression.
Keywords: anxiety, depression, alpha-1 antitrypsin deficiency
Introduction
Alpha-1 antitrypsin deficiency (AATD) is the most common genetically recognized cause of COPD. Because it is rare, AATD remains underdiagnosed with resulting impact on patients.1,2 While emphysema is the most common pulmonary manifestation in AATD, bronchitis, asthma, and bronchiectasis phenotypes of COPD also occur. AATD-associated COPD presents at a younger age compared to usual COPD, likely because of the enhanced susceptibility to effects of tobacco smoke, dusts, and fumes.3 Other conditions associated with AATD include cirrhosis, hepatocellular carcinoma, necrotizing panniculitis, and granulomatosis with polyangiitis.
Over three decades ago, it was observed that individuals with chronic illnesses had worse psychosocial status than comparable populations that did not have chronic illnesses.4 Although this seems self-evident, the first trials that targeted anxiety and depression defined new targets for promising therapies. Over these 30 years, more evidence has emerged to describe the complicated relationships between chronic disease, anxiety/depression, and patient-centered outcomes.5 One result has been an examination of anxiety and depression by disease state, since therapies applied to some patients do not always translate to other chronic disease populations. Therefore, the focus of the present article is to discuss anxiety and depression in the AATD population.
Studies vary on measurements and criteria to define depression and anxiety disorders in the COPD population. Some studies have used self-reported data, while others require diagnostic interviews performed by trained clinicians. Depression encompasses somatic and cognitive domains that include feelings of worthlessness, sadness, sleep disturbance, altered appetite, impaired sexual drive, and decreased interest in activities. A clinical diagnosis of depression is usually established when aforementioned symptoms persist for over 2 weeks.
Excessive and persistent worrying is the main feature of a generalized anxiety disorder. Most individuals present with somatic symptoms of muscle tension, autonomic hyperactivity and hyperarousal. Many affected patients complain of poor sleep, inability to relax, fatigue, headaches, and pain in the neck, shoulders, or back. Anxiety is common associated with increased use of health services, and leads to a greater functional impairment if coexistent with depression.
Prevalence and impact of depression and anxiety in usual COPD
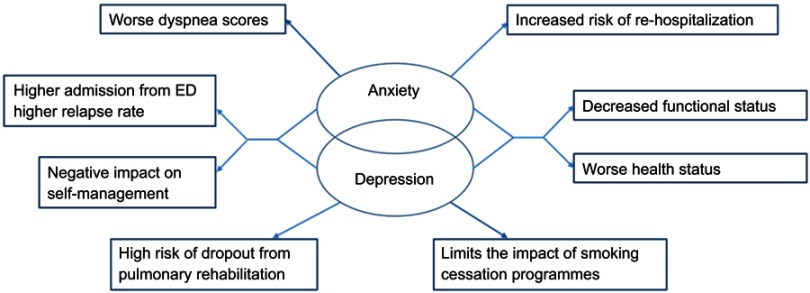
In COPD from all causes, depression and/or anxiety are common with an estimated prevalence of 65%, resulting in severe limitations and quality of life impairments.6 In one study, anxiety and depression in COPD were treated in a minority of affected individuals. The presence of depression as a COPD comorbidity leads to an increased mortality risk, worsened quality of life and increased health care burden.7,8 Numerous studies have evaluated the profound impact of anxiety and depression in COPD (Figure 1).9–11 COPD associated depression is associated with poor exercise performance and more severe BODE index score which is correlated with mortality.12
Figure 1.
The impact of depression and anxiety in COPD. Anxiety and depression often overlap in COPD. This figure aims to show the complex effects of both anxiety and depression on patient-centered outcomes such as dyspnea scores, health status, higher admission rates, and decreased participation in programs aimed at rehabilitation and smoking cessation.
Anxiety and depression in AATD
The genetic abnormalities of AATD produce a risk for COPD that is interactive with environmental exposures. Therefore, in the absence of environmental exposures, individuals may be minimally symptomatic into the 8th decade of life. However, individuals can present with the need for lung transplantation in the 4th decade of life if they smoke cigarettes or have an excessive environmental burden. Therefore, the marked heterogeneity in lung disease presentation makes the disease difficult to study.
At one extreme, AATD is a progressive, debilitating disease resulting in significant decline in quality of life from dyspnea. The disease is associated with very high costs of care since the only-specific therapies may cost >US$100,000 yearly. Diagnosis is usually made after detecting liver or lung disease, and occasionally after AATD has been diagnosed in the family. Numerous studies confirm that some AATD-affected individuals have low quality of life, more comorbidities, and a higher mortality rate than the usual population.13 Dyspnea and fatigue are the most common clinical manifestations.
However, despite severe genetic deficiency of AAT, the development and progression of symptoms can be highly variable with some individuals having no symptoms into the 8th decade of life. In these individuals, the risk of a debilitating disease in themselves or family members may still increase the incidence of anxiety and depression.
Compared to usual COPD, AATD-associated COPD presents approximately 10 years earlier, often during the working lives of affected individuals. The timing of disease development is an important component of the experience of living with a chronic condition. Unlike older individuals, younger age at presentation can alter the perceptions of disease. Prognosis in AATD can be difficult to objectively define since AATD can progress slowly. In one prospective study, ambiguity, reflecting uncertainty about symptoms and physical cues in AATD was associated with worse quality of life, dyspnea, and altered mood.14,15
Risk factors for anxiety and depression in AATD
We hypothesize that numerous risk factors play a role in the development of emotional disorders in AATD (Table 1). Some of these risk factors are common to COPD and some are unique to AATD. Reactions to the disease state can be different by a variety of variables that include symptom severity, gender, age, employment status, income, sleep quality, race, education, and marital status. However, the inherited genetic risk and younger age at the time of diagnosis are unique to the AATD disease state. High costs associated with AATD therapies are common.16 Guilt concerning the passing of deficiency genes from one generation to the next can be present. With the diagnostic delay averaging 6–8 years,17 the opportunity for misdiagnosis and delayed diagnosis is high.2
Table 1.
Causes of anxiety and depression in AATD
| Intrinsic | Extrinsic |
|---|---|
| Genetic disease | High cost of therapies |
| Under recognition and diagnostic delay | Potential loss of employment/income |
| No cure | Potential loss of insurance coverage |
| High burden of symptoms | Denial of insurance |
| Decrease in functional status | Augmentation therapy may not be available/few countries reimburse it |
| Limitations inflicted by disease: Professional/personal life choices | Limited health care providers with expertise |
| Illness unpredictability and uncertainty | |
| Necessity for self-management skills |
Abbreviation: AATD, alpha-1 antitrypsin deficiency.
The vast majority of primary care practitioners do not have enough knowledge about AATD. Even subspecialty-trained physicians may not be familiar enough with the disease, and certainly lack expertise in this rare disease management.
Despite years of research and found answers, many more questions surfaced and the quest for cure in AATD continues. Successful available therapies for AATD primarily focus on augmentation therapy to normalize AAT levels and transplantation approach. Both are of a high cost, limited availability, present burden to the patient and do not prolong life span as desired. Studies of gene therapies for AATD are underway and if successful would be of a lower cost, fewer risks, and hopefully wide availability.18 Augmentation therapy is not a covered benefit worldwide. In many countries, even developed ones with high social economic index, local health authorities do not recommend this therapy. In Poland, AATD individuals do not have access to augmentation therapy. Belgium stopped reimbursement several years ago leaving patients without treatment. In the Netherlands, this therapy is only reimbursed for a selected group of patients.
Despite some studies evaluating composite scores associated with mental disorders and symptoms of anxiety and depression in the alpha-1 population, we are not aware of studies evaluating the prevalence of physician-diagnosed anxiety and depression.
Screening for alpha-1 antitrypsin deficiency: benefits, consequences, and psychosocial effects
The earliest experience with newborn screening for AATD occurred in 1972–1974 in Sweden, the country where AATD was discovered. For the 127 individuals found to be PiZZ at birth, the parents were told that their children should not smoke and that a liver disease was possible. Little else was known. The potential advantages of early diagnosis included parental and childhood behavior modifications, including a clean air future professional choice.19 In the early days of alpha-1 screening, studies confirmed significant and long-lasting negative psychosocial consequences to the parents of the tested children (fear and anxiety),20 partially due to the paucity of information available about the disease at the time.21,22 Reassuringly, later manuscripts revealed no differences in parental worrying about the child’s future and health and increased consciousness of smoking and dusty environments. Yet, mothers of AATD children had more anxiety as compared to controls.23 Long-term follow-up studies also confirmed that the affected individuals as adults had no negative psychosomatic complaints related to the knowledge of alpha-1 status as neonates. These individuals “unanimously” felt that screening should be recommended.24
Anxiety and depression effects on patient-reported outcomes in AATD
Earlier onset of pulmonary disease in AATD-COPD may lead to worse clinical and psychological outcomes. In a study of AATD-affected individuals, developing illness at a younger age, particularly in singles, was linked to more symptoms of depression, worse quality of life, and more dyspnea.25
A high burden of symptoms in chronic diseases has been associated with additional anxiety and depression. Interestingly, the effect is bidirectional since anxiety and depression can clearly worsen symptoms. Analyses of AATD cohorts receiving specific therapy of intravenous augmentation therapy noted that subjects with more COPD exacerbations had a statistically lower mental composite score of the short form-36 (SF-36) questionnaire, a general quality of life instrument. Therefore, a focus on the exacerbating AATD population may allow particular focus on the burden of both anxiety and depression in a targeted population.26
Adjustment to chronic health conditions is challenging for affected individuals. Most AATD individuals are diagnosed while in a highly productive stage of life with career pursuits or raising a family. In a study of AATD individuals, however, the presence of additional resources (higher education, and being a part of the couple) counterbalanced the risk associated with the younger age.27 The high prevalence and inverse relationship between age and symptoms of both anxiety and depression have previously been demonstrated in many chronic conditions.28 Life adjustments are commonly made by AATD-affected individuals to accommodate the illness. Reportedly, 75.3% of individuals living with AATD had a major change in their life: early retirement, change to a physically easier job, or a loss of one.2
It is important to mention that stress starts at the time of AATD diagnosis, but often transitions into areas of chronic illness that are different from diagnostic uncertainties. These transitions in stress may require further psychological adjustments that are necessary during the course of the disease. For example, some of the other areas causing stress to the AATD community include the genetic risks for family members, disease unpredictability, need for life-long treatment, integrating weekly infusions into life, limiting life choices due to the need for frequent infusions, coping with treatment failures, side effects, and potential complications.
Genetic testing has been suggested to require informed consent since results may impact other family members. Because genetic diseases may have more risks of discrimination and stigmatization than other kinds of tests, research evaluated the effects of genetic testing on anxiety in AATD. General anxiety about the test results and stress induced by testing did not differ between those who agreed to the testing as compared to non-responders.29 Another study confirmed that information about the testing did not raise mean anxiety levels helping alleviate concerns about post-testing issues in chronic diseases such as cystic fibrosis and AATD.30
Anxiety in a population tested for alpha-1 antitrypsin deficiency
The Alpha Coded Testing (ACT) study offers confidential testing for AATD in individuals with physician-diagnosed COPD and in AATD families. Along with genetic testing psychosocial surveys, demographic data, income and smoking status are collected. In our analyses of 726 individuals who were severely deficient or carriers, we found elevated Beck Anxiety Inventory (BAI) scores in over 9% suggesting significant anxiety in this subgroup. Lower incomes and current smoking status correlated with increased BAI scores whereas age and AATD genotype did not affect those correlations. In addition, the SF-12 questionnaire that reflects quality of life showed a good correlation with BAI scores in this cohort, which was primarily driven by the Mental Health Composite Scale score component of SF-12.
Management of anxiety and depression in AATD
The course of anxiety and depression in AATD varies, depending on severity of illness, the progression of the disease, family support availability, and amount of resources available. Understandably, some of these are fluid and may change inadvertently affecting either anxiety or depression. According to most of the studies, anxiety and depression remain overlooked in case of AATD individuals. Even when diagnosed, treatment at times is omitted for various reasons.
The Big Fat Reference Guide (BFRG) is a web resource for individuals and families who have AATD that was written by AATD-affected individuals. The BFRG (www.alphanetbfrg.org) has a chapter on “Coping with Alpha-1” that acknowledges the stress of the diagnosis and disease process. The outlined recommendations provide individuals with some tools to manage and achieve a good state of emotional well-being.
The 2019 GOLD COPD guidelines stress that both anxiety and depression are common comorbidities in COPD leading to poor prognosis. In usual COPD, specific risk factors have been implicated for anxiety and depression: younger age, female sex, smoking status, lower FEV1, presence of cough, higher SGRQ score and a history of cardiovascular disease. Importantly, GOLD states that both COPD and anxiety/depression should be treated as usual. Pulmonary rehabilitation once again is the strongest recommendation as physical exercise has a beneficial effect on depression.
The utility of a pharmacological approach to treat depression as a comorbidity in COPD remains unclear. Recent literature found the use of serotonergic antidepressants to be associated with small increases in morbidity and mortality among older individuals with COPD.31 More research is needed to determine whether these observations are the result of unresolved confounding or a potentially causative.
More research is available in other chronic medical conditions with a comorbidity of depression. Even though found to be safe, treatment with SSRIs did not result in improvement of depression in cardiovascular disease.32,33
Conclusion
Anxiety and depression are common and underappreciated comorbidities in the AATD population. Both are associated with worse patient-centered outcomes, lead to high costs of health care, and increase burden on patients, families, and providers. Guidelines should continue advocating for proper diagnosis and management of both conditions. We propose ongoing studies to evaluate the true prevalence. These should study the influence of anxiety and depression on patient-centered outcomes in order to identify potential strategies to minimize the impact. Potential treatment options are available and will require future-focused clinical trials.
Disclosure
Dr Charlie Strange reports grants from Alpha-1 Foundation, during the conduct of the study; grants and personal fees from Grifols, CSL Behring, Vertex and Adverum, outside the submitted work; personal fees from Shire/Takeda, and grants from MatRx, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Tejwani V, Nowacki AS, Fye E, Sanders C, Stoller JK. The impact of delayed diagnosis of alpha-1 antitrypsin deficiency: the association between diagnostic delay and worsened clinical status. Respir Care. 2019. doi: 10.4187/respcare.06555. [DOI] [PubMed] [Google Scholar]
- 2.Stoller JK, Smith P, Yang P, Spray J. Physical and social impact of alpha 1-antitrypsin deficiency: results of a survey. Cleve Clin J Med. 1994;61(6):461–467. [DOI] [PubMed] [Google Scholar]
- 3.Zacherle E, Noone JM, Runken MC, Blanchette CM. Health care cost and utilization associated with alpha-1 antitrypsin deficiency among a cohort of medicare beneficiaries with COPD. Value Health. 2015;18(7):A664. doi: 10.1016/j.jval.2015.09.2419 [DOI] [Google Scholar]
- 4.Cassileth BR, Lusk EJ, Strouse TB, et al. Psychosocial status in chronic illness. A comparative analysis of six diagnostic groups. N Engl J Med. 1984;311(8):506–511. doi: 10.1056/NEJM198408233110805. [DOI] [PubMed] [Google Scholar]
- 5.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127(4):1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 7.Jennings JH, Digiovine B, Obeid D, Frank C. The association between depressive symptoms and acute exacerbations of COPD. Lung. 2009;187(2):128–135. doi: 10.1007/s00408-009-9135-9. [DOI] [PubMed] [Google Scholar]
- 8.Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217–223. doi: 10.1093/fampra/cmm009. [DOI] [PubMed] [Google Scholar]
- 9.Dahlen I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–1637. doi: 10.1378/chest.122.5.1633 [DOI] [PubMed] [Google Scholar]
- 10.Gudmundsson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: role of health status, anxiety and depression. Eur Respir J. 2005;26(3):414–419. doi: 10.1183/09031936.05.00078504. [DOI] [PubMed] [Google Scholar]
- 11.Dowson CA, Town GI, Frampton C, Mulder RT. Psychopathology and illness beliefs influence COPD self-management. J Psychosom Res. 2004;56(3):333–340. doi: 10.1016/S0022-3999(03)00040-0. [DOI] [PubMed] [Google Scholar]
- 12.Al-shair K, Dockry R, Mallia-Milanes B, Kolsum U, Singh D, Vestbo J. Depression and its relationship with poor exercise capacity, BODE index and muscle wasting in COPD. Respir Med. 2009;103(10):1572–1579. doi: 10.1016/j.rmed.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Stallberg B, Janson C, Larsson K, et al. Real-world retrospective cohort study ARCTIC shows burden of comorbidities in Swedish COPD versus non-COPD patients. NPJ Prim Care Respir Med. 2018;28(1):33. doi: 10.1038/s41533-018-0101-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoth KF, Wamboldt FS, Strand M, et al. Prospective impact of illness uncertainty on outcomes in chronic lung disease. Health Psychol. 2013;32(11):1170–1174. doi: 10.1037/a0032721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Worthington AK, Parrott RL, Smith RA. Spirituality, illness unpredictability, and math anxiety effects on negative affect and affect-management coping for individuals diagnosed with alpha-1 antitrypsin deficiency. Health Commun. 2018;33(4):363–371. doi: 10.1080/10410236.2016.1266576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mullins CD, Huang X, Merchant S, Stoller JK. Alpha one foundation research network registry I. The direct medical costs of alpha(1)-antitrypsin deficiency. Chest. 2001;119(3):745–752. doi: 10.1378/chest.119.3.745. [DOI] [PubMed] [Google Scholar]
- 17.Stoller JK, Sandhaus RA, Turino G, Dickson R, Rodgers K, Strange C. Delay in diagnosis of alpha1-antitrypsin deficiency: a continuing problem. Chest. 2005;128(4):1989–1994. doi: 10.1378/chest.128.4.1989. [DOI] [PubMed] [Google Scholar]
- 18.Chiuchiolo MJ, Crystal RG. Gene therapy for alpha-1 antitrypsin deficiency lung disease. Ann Am Thorac Soc. 2016;13(Suppl 4):S352–S69. doi: 10.1513/AnnalsATS.201506-344KV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sveger T, Thelin T. A future for neonatal alpha1-antitrypsin screening? Acta Paediatr. 2000;89(3):259–261. [PubMed] [Google Scholar]
- 20.Thelin T, McNeil TF, Aspegren-Jansson E, Sveger T. Psychological consequences of neonatal screening for alpha 1-antitrypsin deficiency. Parental reactions to the first news of their infants’ deficiency. Acta Paediatr Scand. 1985;74(5):787–793. [DOI] [PubMed] [Google Scholar]
- 21.McNeil TF, Sveger T, Thelin T. Psychosocial effects of screening for somatic risk: the Swedish alpha 1 antitrypsin experience. Thorax. 1988;43(7):505–507. doi: 10.1136/thx.43.7.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNeil TF, Thelin T, Aspegren-Jansson E, Sveger T, Harty B. Psychological factors in cost-benefit analysis of somatic prevention. A study of the psychological effects of neonatal screening for alpha 1-antitrypsin deficiency. Acta Paediatr Scand. 1985;74(3):427–432. [DOI] [PubMed] [Google Scholar]
- 23.Sveger T, Thelin T, McNeil TF. Neonatal alpha1-antitrypsin screening: parents’ views and reactions 20 years after the identification of the deficiency state. Acta Paediatr. 1999;88(3):315–318. [DOI] [PubMed] [Google Scholar]
- 24.Sveger T, Thelin T, McNeil TF. Young adults with alpha 1-antitrypsin deficiency identified neonatally: their health, knowledge about and adaptation to the high-risk condition. Acta Paediatr. 1997;86(1):37–40. [DOI] [PubMed] [Google Scholar]
- 25.Holm KE, Plaufcan MR, Ford DW, et al. The impact of age on outcomes in chronic obstructive pulmonary disease differs by relationship status. J Behav Med. 2014;37(4):654–663. doi: 10.1007/s10865-013-9516-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campos MA, Alazemi S, Zhang G, et al. Exacerbations in subjects with alpha-1 antitrypsin deficiency receiving augmentation therapy. Respir Med. 2009;103(10):1532–1539. doi: 10.1016/j.rmed.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 27.Holm KE, Borson S, Sandhaus RA, et al. Differences in adjustment between individuals with alpha-1 antitrypsin deficiency (AATD)-associated COPD and non-AATD COPD. COPD. 2013;10(2):226–234. doi: 10.3109/15412555.2012.719049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Angermann CE, Ertl G. Depression, anxiety, and cognitive impairment: comorbid mental health disorders in heart failure. Curr Heart Fail Rep. 2018;15(6):398–410. doi: 10.1007/s11897-018-0414-8. [DOI] [PubMed] [Google Scholar]
- 29.Dickson MR, Carter CL, Carpenter MJ, et al. Barriers to genetic testing among persons at risk for alpha-1 antitrypsin deficiency. Genet Test. 2008;12(4):501–505. doi: 10.1089/gte.2008.0028. [DOI] [PubMed] [Google Scholar]
- 30.Coors ME, Levinson AH, Huitt GA. Anxiety related to genetic testing for alpha-1 antitrypsin deficiency and cystic fibrosis in COPD and/or bronchiectasis patients. Community Genet. 2008;11(3):135–140. doi: 10.1159/000113875. [DOI] [PubMed] [Google Scholar]
- 31.Vozoris NT, Wang X, Austin PC, et al. Serotonergic antidepressant use and morbidity and mortality among older adults with COPD. Eur Respir J. 2018;52(1). doi: 10.1183/13993003.00475-2018. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor CM, Jiang W, Kuchibhatla M, et al. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline against depression and heart disease in chronic heart failure) trial. J Am Coll Cardiol. 2010;56(9):692–699. doi: 10.1016/j.jacc.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Angermann CE, Gelbrich G, Stork S, et al. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683–2693. doi: 10.1001/jama.2016.7635. [DOI] [PubMed] [Google Scholar]