Abstract
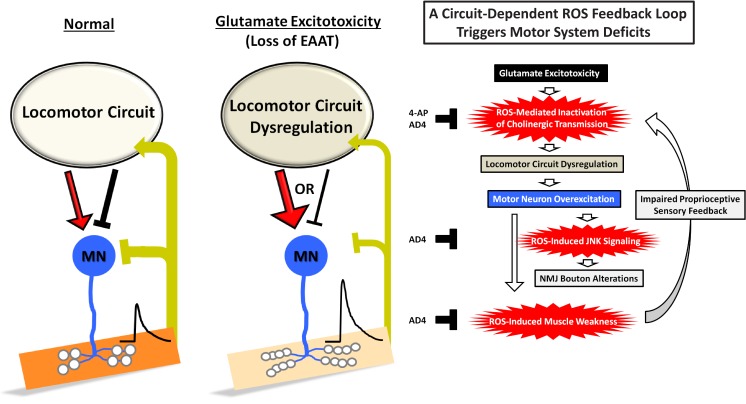
Overproduction of reactive oxygen species (ROS) is known to mediate glutamate excitotoxicity in neurological diseases. However, how ROS burdens can influence neural circuit integrity remains unclear. Here, we investigate the impact of excitotoxicity induced by depletion of Drosophila Eaat1, an astrocytic glutamate transporter, on locomotor central pattern generator (CPG) activity, neuromuscular junction architecture, and motor function. We show that glutamate excitotoxicity triggers a circuit-dependent ROS feedback loop to sculpt the motor system. Excitotoxicity initially elevates ROS, thereby inactivating cholinergic interneurons and consequently changing CPG output activity to overexcite motor neurons and muscles. Remarkably, tonic motor neuron stimulation boosts muscular ROS, gradually dampening muscle contractility to feedback-enhance ROS accumulation in the CPG circuit and subsequently exacerbate circuit dysfunction. Ultimately, excess premotor excitation of motor neurons promotes ROS-activated stress signaling that alters neuromuscular junction architecture. Collectively, our results reveal that excitotoxicity-induced ROS can perturb motor system integrity through a circuit-dependent mechanism.
Research organism: D. melanogaster
Introduction
Reactive oxygen species (ROS) are generated as the by-product of mitochondrial oxidative phosphorylation (Adam-Vizi, 2005). In the central nervous system, under physiological conditions, high energy demand results in higher levels of ROS production relative to those in other body parts. In the past, endogenously generated ROS were recognized as signaling molecules that regulate a range of nervous system processes, including neuronal polarity, growth cone pathfinding, neuronal development, synaptic plasticity, and neural circuit tuning (Li et al., 2016; Oswald et al., 2018a; Oswald et al., 2018b). By contrast, ROS overproduction and/or overwhelming the antioxidant machinery can generate ROS burdens, termed oxidative stress, in aging and diverse pathological conditions (Blesa et al., 2015; Bozzo et al., 2017; Liguori et al., 2018; Pollari et al., 2014; Wang et al., 2014; Zhao and Zhao, 2013). In turn, excess ROS causes the malfunction and overactivation of ROS-regulated cell signaling pathways. Moreover, the highly oxidative properties of ROS are damaging to nucleotides, proteins, and lipids, eventually leading to neuronal dysfunction or demise. Hence, advancing our understanding of the mechanisms underlying ROS-induced neurotoxicity should aid the development of potent therapeutic treatments for neurological disorders.
Glutamate acts as the major excitatory neurotransmitter that regulates nearly all activities of the nervous system, with a tight balance between glutamate release and reuptake keeping the micromolar concentration of extracellular glutamate low (Lewerenz and Maher, 2015). In diseases, accumulation of extrasynaptic glutamate results in glutamate-mediated excitotoxicity to the nervous system (Dong et al., 2009; Mehta et al., 2013; Van Den Bosch et al., 2006). Dysfunction of Na+/K+-dependent excitatory amino acid transporters (EAATs) is a key element of glutamate-mediated excitotoxicity (Lewerenz and Maher, 2015). In mammals, there are five EAAT subtypes, that is EAAT1 (GLAST), EAAT2 (GLT1), EAAT3 (EAAC1), EAAT4, and EAAT5 (Vandenberg and Ryan, 2013). EAAT3, EAAT4 and EAAT5 are expressed in neurons, whereas EAAT1 and EAAT2 are mainly present in astrocytes, where they are enriched in astrocyte terminal processes that form tripartite synapses with neurons and where they take up approximately 90% of released glutamate. Glutamate-mediated excitotoxicity can trigger bulk Ca2+ influx into postsynaptic neurons via NMDA receptors, which causes mitochondrial Ca2+ overload, along with other cellular responses, and which subsequently generates excess amounts of ROS (Peng and Jou, 2010; Prentice et al., 2015). Notably, it has emerged that dysregulation of neural circuit activity can initiate subsequent disruption of the integrity of other constituents in the same network, resulting in overall circuit dysfunction and even neurodegeneration (Fornito et al., 2015; Hussain et al., 2018; Palop and Mucke, 2010; Shababi et al., 2014). However, it still remains unclear whether and how excitotoxicity-induced ROS can influence the integrity of neural circuits.
Coordinated animal behaviors are linked to the activity of spinal cord central pattern generators (CPG), which are known to be specialized circuits that integrate inputs from the central brain and sensory neurons, and that subsequently generate rhythmic and patterned outputs to motor neurons (Kiehn, 2016). The Drosophila feed-forward locomotor circuit has served as an appropriate model for exploring the pathogenic network mechanisms that underlie neurodegenerative diseases (Held et al., 2019; Imlach et al., 2012; Lotti et al., 2012), because it has a relatively simple neural circuitry compared to mammals yet retains conserved functions (Clark et al., 2018; Kohsaka et al., 2017). In this study, we explored whether glutamate-mediated excitotoxicity impacts locomotor CPG activity, neuromuscular junction (NMJ) architecture, and motor function. Interestingly, we found that glutamate-mediated excitotoxicity due to depletion of Drosophila Eaat1, the sole Drosophila homolog of human EAAT2 (Besson et al., 2000), can induce a circuit-dependent ROS feedback loop that impairs the proper activities of the locomotor CPG circuit and muscles, ultimately leading to motor neuron overexcitation, abnormal NMJ growth and strength, and compromised movement. Together, our work reveals a circuit-dependent mechanism for increasing ROS, which mediates glutamate excitotoxicity to sculpt the Drosophila locomotion network.
Results
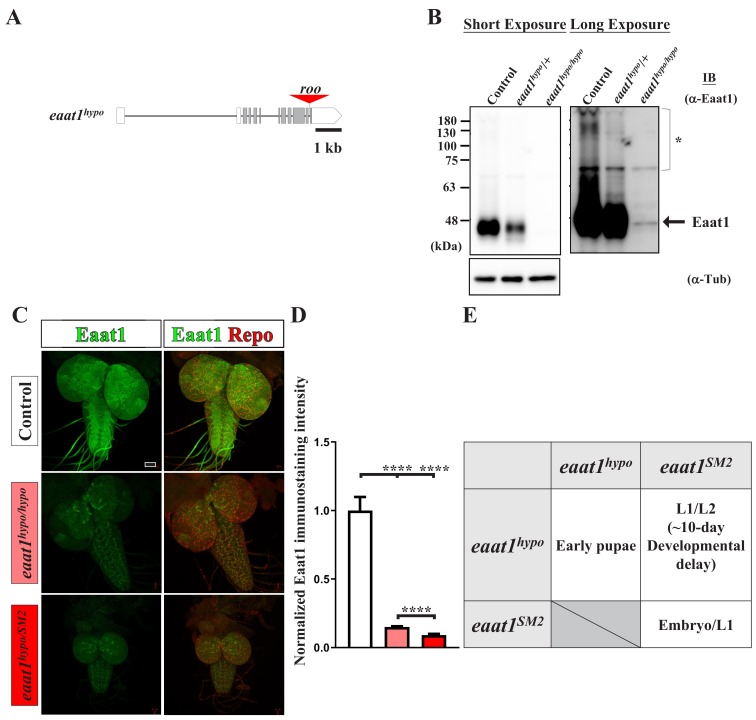
Loss of Drosophila Eaat1 causes motor-system deficits
Alterations in synaptic structure and function have been associated with a wide range of chronic neurodegenerative diseases (Chand et al., 2018; Dachs et al., 2011; Fischer et al., 2004; Kariya et al., 2008; Lepeta et al., 2016; Rocha et al., 2013; Sharma et al., 2016; Wishart et al., 2006). To explore the mechanisms underpinning these alterations, we collected the mutants that were previously characterized as having functional and/or developmental deficits in Drosophila photoreceptor cells (Hiesinger et al., 2005; Jafar-Nejad et al., 2005; Ohyama et al., 2007; Verstreken et al., 2003), and then conducted a secondary screen for mutations affecting synaptic bouton development of Drosophila third instar larval NMJs, with this latter system being broadly used to study the causes of neurodegenerative diseases (Jaiswal et al., 2012; McGurk et al., 2015). From this screen, we identified a hypomorphic mutation of Drosophila excitatory amino acid transporter 1 (eaat1). The mutant allele contained an insertion of a roo transposon in the last intron of the eaat1 locus, which results in a severe reduction of Eaat1 protein levels (Figure 1—figure supplement 1A–D). Hereafter, we term this mutant eaat1hypo. Although eaat1 null mutants (eaat1SM2/SM2) died before the first instar larval stage, as reported previously (Stacey et al., 2010), approximately 20% of eaat1hypo/hypo animals developed almost normally during the larval stages, but most of them died at early pupal stages (Figure 1—figure supplement 1E). We noted that a majority of eaat1hypo/SM2 mutants died between the first and second instar larval stages, whereas ~1% of the mutants could further develop until the third instar stage, but they exhibited a significant ~10-day developmental delay (Figure 1—figure supplement 1E). The protein level of Eaat1 that remained in these survivors was further reduced relative to that detected in eaat1hypo/hypo mutants (Figure 1—figure supplement 1C–D). These data indicate that the expression levels of Eaat1 are correlated with successful larval development.
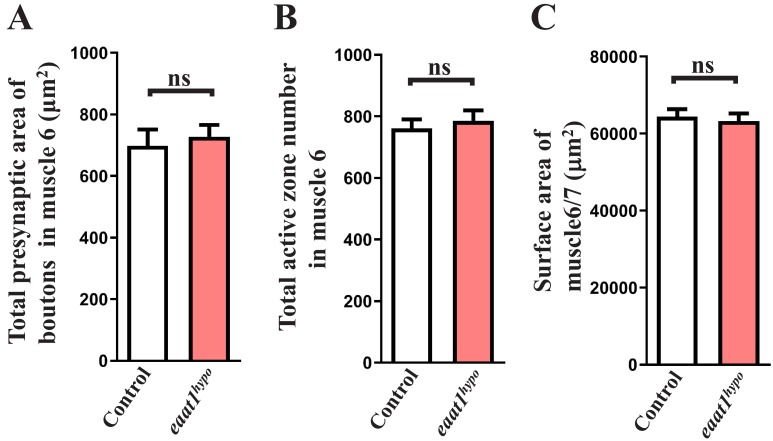
To examine NMJ bouton architecture, we outlined the presynaptic and postsynaptic membranes of boutons by immunostaining with anti-horseradish peroxidase and anti-Disc large (Dlg) antibodies. As shown in Figure 1A–D, eaat1hypo mutants displayed an ~50% increase in bouton number compared to wild-type controls, but their boutons were significantly smaller. Overall presynaptic area, active zone number per NMJ, and muscle surface area in controls and eaat1hypo mutants were indistinguishable (Figure 1—figure supplement 2A–C). We then assessed whether synaptic transmission differs in response to morphological changes. Evoked excitatory junctional potential (EJP) was recorded from muscles under low-frequency (0.2 Hz) nerve stimulation. Compared to controls, eaat1hypo mutants showed an increase in the EJP amplitude and quantal content (QC) (Figure 1E–G), whereas the amplitude and frequency of miniature EJPs were comparable between controls and eaat1 mutants (Figure 1H; not shown for frequency), suggesting that loss of eaat1 also abnormally increases neurotransmitter release.
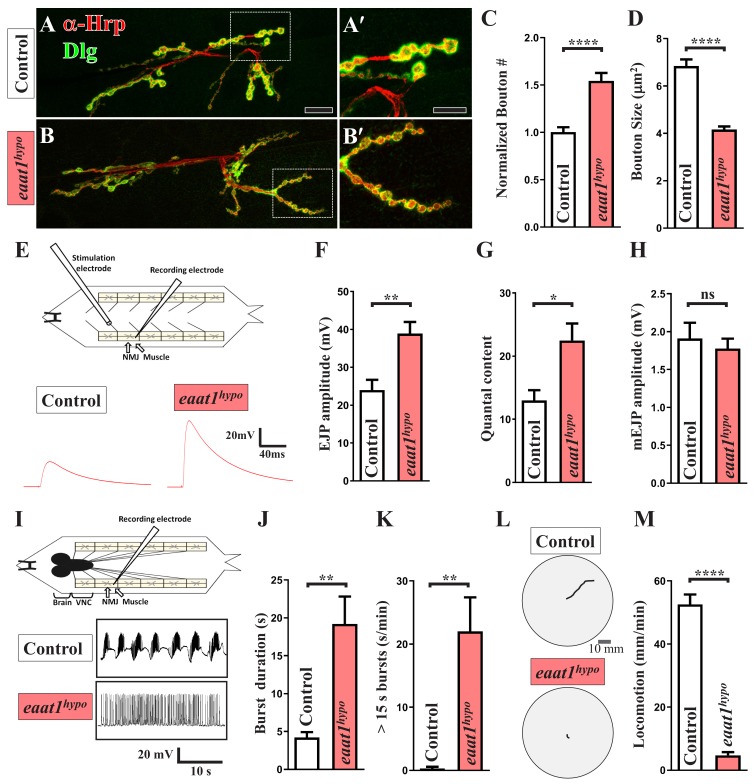
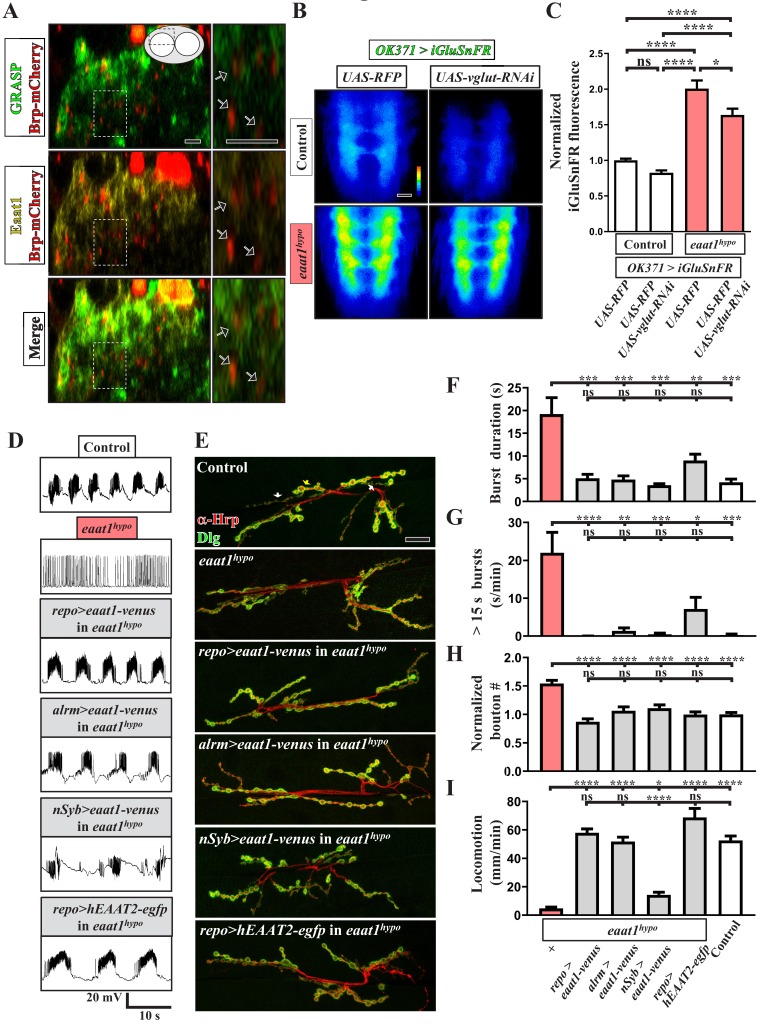
Figure 1. eaat1 mutants exhibit NMJ bouton abnormalities, motor neuron overexcitation, and motor deficits.
(A–D) Loss of eaat1 increases NMJ bouton number and reduces bouton size. (A–B) Confocal images of NMJs co-stained with α-HRP (red) and α-Dlg (green) from controls (w1118) and eaat1hypo/hypo mutants. The NMJ boutons outlined in panels (A,B) are shown in panels (A',B'). Scale bars: 20 µm in (A,B), 10 µm in (A',B'). (C) The number of NMJ boutons per muscle area was counted and normalized to the value of controls (n ≥ 15 NMJs derived from A2 muscles 6 and 7 for each genotype). (D) The sizes of type Ib boutons were calculated on the basis of the immunostaining of Cysteine string protein, a synaptic vesicle-associated protein (n ≥ 433 type Ib boutons from NMJs (n ≥ 8) of A2 muscles 6 and 7 for each genotype). (E–H) Evoked presynaptic responses are increased upon loss of eaat1. (E) Top panel: schematic of the recording setting for larval fillets in which brain and ventral nerve cord (VNC) had been removed. Bottom panel: representative EJP traces evoked from A3 muscle 6 with 0.2 Hz electric stimulation in 0.5 mM Ca2+-containing HL3 solution. (F–H) Quantification data for EJP amplitude, quantal content (QC), and miniature EJP amplitude (n ≥ 6 animals). Miniature EJPs were recorded in HL3 solution containing 0.5 mM Ca2+ and 5 μM tetrodotoxin (TTX). (I–K) eaat1hypo mutants receive excess premotor excitation. (I) Top panel: schematic of the recording setting for larval fillets in which the brain and VNC remain intact. Bottom panel: representative EJP traces evoked by spontaneous motor CPG activity during fictive locomotion. Recordings were obtained from A3 muscle 6 in HL3 solution containing 1 mM Ca2+. (J–K) Quantification data for burst duration and overall firing time (from bursts of >15 s) per recording minute (n ≥ 6 animals). (L–M) eaat1hypo mutants display compromised locomotion. (L) Representative locomotion tracks of third instar larvae. (M) Quantification data for larval locomotion (n ≥ 16 animals). P values: ns, no significance; *, p<0.05; **, p<0.01; ****, p<0.0001. n: replicate number. Error bars indicate the standard errors of the means (SEM). Statistics: Student's t-test.
Figure 1—figure supplement 1. Characterization of the eaat1hypo mutant allele.
Figure 1—figure supplement 2. Morphological analysis of eaat1hypo mutant NMJ boutons and muscles.
Figure 1—figure supplement 3. Analysis of the properties of the locomotor CPG output.
Drosophila larval feed-forward locomotion is driven by the rhythmic activity of the locomotor CPG located in the ventral nerve cord (VNC) (Cattaert and Birman, 2001), reminiscent of human and mouse spinal cords. This premotor network integrates inputs from the central brain (Cattaert and Birman, 2001) and proprioceptive sensory neurons (Hughes and Thomas, 2007; Song et al., 2007), and it subsequently sends outputs to motor neurons (Foran and Trotti, 2009; Shaw and Ince, 1997). It has been shown that motor neurons that are derived from dissected first instar larvae of the eaat1 null mutants receive sustained locomotor CPG output (Stacey et al., 2010). To corroborate this CPG phenotype, we generated third instar larval fillets of eaat1hypo mutants, in which the brain and VNC remain intact, and performed intracellular muscle recordings to measure spontaneous locomotor CPG activity during fictive locomotion. Wild-type control motor neurons were normally able to receive rhythmic CPG output bursts that lasted a few seconds (Figure 1I–J), consistent with previous reports (Cattaert and Birman, 2001; Imlach et al., 2012). By contrast, eaat1hypo motor neurons displayed a marked increase (~5 fold) in burst duration (Figure 1I–J). Moreover, burst frequency and intra-burst spike density were decreased in eaat1hypo mutants relative to those in controls (Figure 1—figure supplement 3A–B). To represent the degree of sustained excitation on motor neurons quantitatively, we calculated the overall firing time of extremely long bursts (e.g. >15 s) for each recording minute and found that control and eaat1hypo motor neurons were fired for 0.28 ± 0.28 s and 22 ± 5.38 s, respectively (Figure 1K). Consistent with these results, wild-type control larvae displayed coordinated peristalsis and locomotion activity, whereas eaat1hypo mutants barely exhibited peristalsis and showed sluggish movement (Figure 1L–M). Therefore, these data suggest that Eaat1 is required to maintain proper patterning of the locomotor CPG output, and its loss can alter the CPG output pattern, thereby eliciting excess stimulation of motor neurons.
Loss of Drosophila Eaat1 in astrocyte-like glia causes motor-system defects
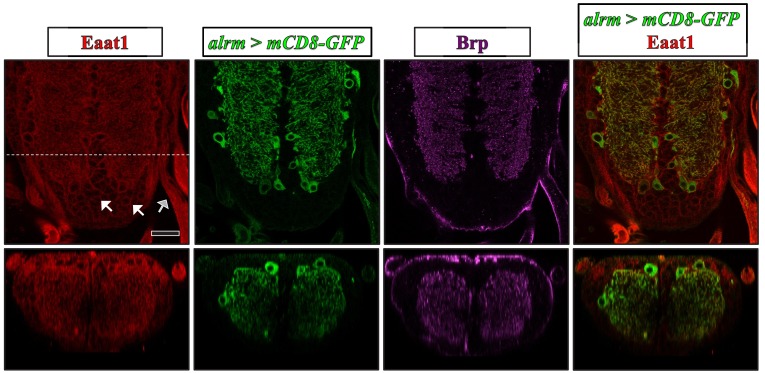
Drosophila Eaat1 has been shown to be abundant in astrocyte-like glia of the central nervous system (Besson et al., 2000) (see also Figure 2—figure supplement 1). Although glutamate is the major neurotransmitter utilized by Drosophila motor neurons, Eaat1 is not present in the NMJ-associated glia throughout embryonic and larval development (Rival et al., 2006). To examine the physical association between the astrocyte-like glia and glutamatergic synapses in the larval VNC, we performed a GRASP (GFP reconstitution across synaptic partners) analysis (Feinberg et al., 2008), in which the transgenes of two split green fluorescence proteins (GFPs), UAS-CD4::spGFP1-10 and lexAOP-CD4::spGFP11, were separately expressed in glutamatergic neurons and astrocyte-like glia using OK371-GAL4 (also known as vglut-GAL4) and repo-lexA. Concurrently, the presynaptic compartments of glutamatergic interneurons were labeled by expressing the mCherry fusion transgene of an active zone scaffold protein Bruchpilot (Brp). We did not observe any GRASP signal in the VNCs derived from the larvae of either OK371-GAL4/UAS-CD4::spGFP1-10 or repo-lexA/lexAOP-CD4::spGFP11 control (Figure 2—figure supplement 2). By contrast, the larvae of OK371-GAL4/UAS-CD4::spGFP1-10/repo-LexA/lexAOP-CD4::spGFP11 displayed high GRASP signals in neuropils of the dorsal part of the VNC (Figure 2—figure supplement 2; green in Figure 2A), which was tightly associated with Eaat1 expression (yellow in Figure 2A). However, we noted that the terminal processes of astrocyte-like glia were close to rather than part of the glutamatergic tripartite synapses, which is consistent with a previous transmission electron microscopy study (Stork et al., 2014). To investigate the function of Eaat1, we expressed UAS-iGluSnFR, a membrane-bound extracellular glutamate sensor (Chenji et al., 2016; Stork et al., 2014), at glutamatergic synapses of the VNC using OK371-GAL4 to measure the level of perisynaptic glutamate. As seen in Figure 2B–C (left panels), the control VNC exhibited low glutamate levels, whereas excess accumulation of glutamate was found upon Eaat1 depletion. Thus, Eaat1 maintains glutamate homeostasis efficiently through its close synaptic association in the Drosophila central nervous system.
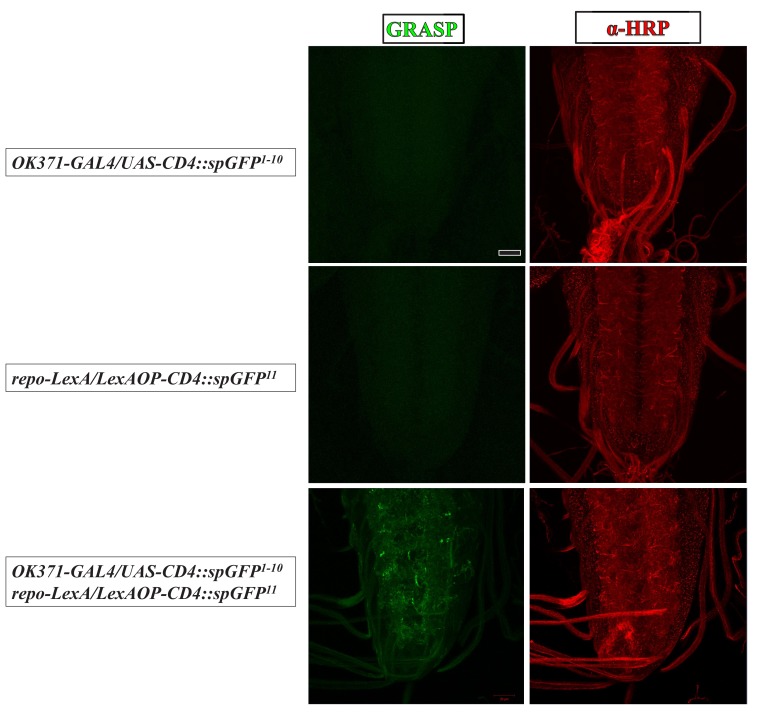
Figure 2. Eaat1 expressed in astrocyte-like glia plays a conserved role in maintaining motor system integrity.
(A) GRASP assay showing a close association between astrocyte-like glia and motor neurons. Confocal cross-section images captured from the dorsal sector of the VNC of third instar larvae (repo-LexA/LexAOP-CD4::spGFP11/OK371-GAL4/UAS-CD4::spGFP1-10/UAS-brp-mCherry). Among the different types of glia, astrocyte-like glia predominantly extend their cellular processes into neuropils of the VNC. Arrows indicate clustered Brp-mCherry-labeled presynaptic compartments of glutamatergic interneurons, which are closely surrounded by GRASP signals (green) and Eaat1 proteins (yellow). Higher magnifications of the outlined regions are shown in the panels on the right. (B,C) Loss of eaat1 elevates perisynaptic glutamate. (B) Pseudocolored images of the VNC-expressing iGluSnFR obtained from third instar larvae of the indicated genotypes. UAS-RFP was used as the control UAS transgene. Representative images were captured in zero calcium HL3 solution. (C) Quantification data for iGluSnFR signal intensity, normalized to the value of control (OK371 >iGluSnFR + RFP) (n ≥ 9 VNCs for each genotype). (D–I) Glial or astrocytic expression of the eaat1-venus transgene or of the human EAAT2-egfp transgene fully rescues the motor system defects in eaat1hypo mutants. Neuronal expression of the eaat1-venus transgene in eaat1 mutants can restore premotor circuit activity and NMJ bouton growth but not locomotion. (D) Representative traces of EJPs evoked by spontaneous motor CPG activity during fictive locomotion obtained from third instar larvae of controls (w1118) and the indicated genotypes. Recordings were obtained from A3 muscle 6 in HL3 solution containing 1 mM Ca2+. Quantification data for burst duration and overall firing time (for bursts of >15 s) for each recording minute are shown in panels (F,G) (n ≥ 6 animals for each genotype). (E) Confocal images of NMJs co-stained with α-HRP (red) and α-Dlg (green) obtained from third instar larvae of controls (w1118) and the indicated genotypes. Quantification data for NMJ bouton number for each muscle area, normalized to the value of controls, are shown in panel (H) (n ≥ 9 NMJs derived from A2 muscles 6 and 7 for each genotype). (I) Quantification data for the locomotion of third instar larvae of controls (w1118) and the indicated genotypes (n ≥ 10 animals for each genotype). P values: ns, no significance; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: one-way ANOVA with Tukey’s post hoc test. Scale bars: 5 μm in (A), 20 µm in (B), 20 µm in (E).
Figure 2—figure supplement 1. Expression pattern of Eaat1 in the larval VNC.
Figure 2—figure supplement 2. GRASP assay for the physical contact between astrocyte-like glia and glutamatergic neurons.
Figure 2—figure supplement 3. Phenotypic characterization of eaat1hypo/SM2 mutants.
To investigate whether the depletion of Eaat1 from astrocyte-like glia is causative of the observed motor system deficits, we first expressed the UAS transgene of the yellow fluorescent protein (Venus) fused to Eaat1 (UAS-eaat1-venus) in eaat1hypo mutants using repo-GAL4, a pan-glia GAL4 driver. This approach rescued the changes in locomotor CPG activity, NMJ boutons, and locomotion (Figure 2D–I and Figure 1—figure supplement 3A–B). In addition, a similar rescue effect was obtained with alrm-GAL4, an astrocyte-like glia-specific GAL4 driver (Doherty et al., 2009) (Figure 2D–I and Figure 1—figure supplement 3A–B). Thus, loss of Eaat1 in astrocyte-like glia leads to the defective motor system phenotypes. Interestingly, when we also tested the effect of neuronal expression of eaat1-venus, altered locomotor CPG output activity and NMJ boutons, but not impaired locomotion, were rescued (Figure 2D–I and Figure 1—figure supplement 3A–B). This evidence suggests that the ectopic expression of Eaat1 in neurons can partially restore function, but appropriate expression of Eaat1 in astrocytes is required to coordinate CPG activity between and/or within individual segments. Next, we determined whether the functions of Drosophila Eaat1 are conserved in its human homolog. Expression of the human EAAT2 (hEAAT2)-egfp transgene using repo-GAL4 rescued eaat1hypo mutant phenotypes (Figure 2D–I), except for the reduced CPG burst frequency (Figure 1—figure supplement 3A–B). Under the above-described conditions, most rescued animals could eclose as adult flies (not shown). Therefore, the functions of EAAT are conserved from fly to human.
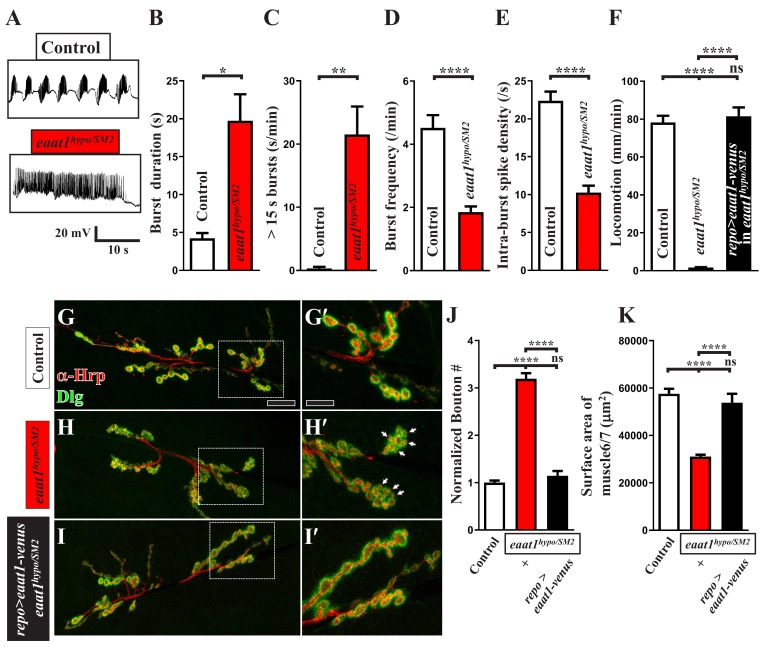
We further phenotypically characterized eaat1hypo/SM2 mutants that survived to the third instar stage. These larvae also exhibited alterations in locomotor CPG activity and locomotion (Figure 2—figure supplement 3A–F). In addition, they presented outgrown NMJ boutons (Figure 2—figure supplement 3G–J). However, eaat1hypo/SM2 mutant NMJs had numerous satellite boutons (Figure 2—figure supplement 3G–I) and reduced muscle size (Figure 2—figure supplement 3K), outcomes that are distinct from those found in eaat1hypo/hypo mutants. We speculate that this morphological difference may be partly attributable to a significant developmental delay in NMJ bouton growth (Figure 1—figure supplement 1E) (Sandoval et al., 2014). Furthermore, glial expression of eaat1-venus using repo-GAL4 robustly corrected these defects (Figure 2—figure supplement 3F and I–K). Hence, these results strengthen the causal role of the eaat1 mutation in altering the integrity of the motor system.
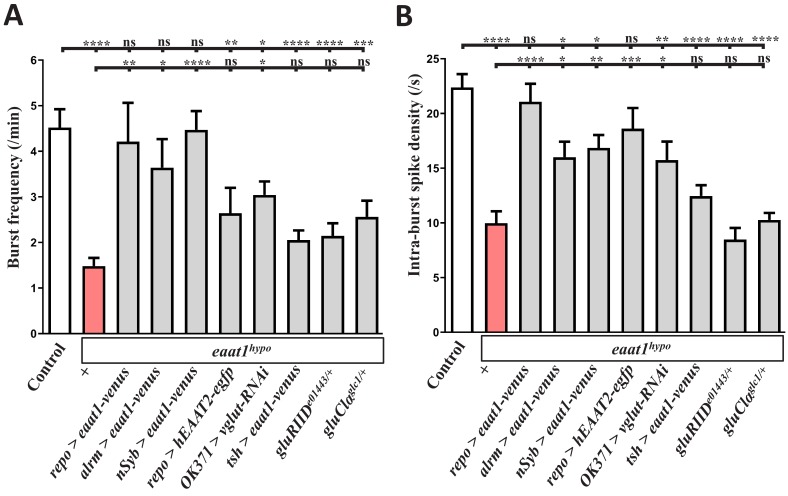
Glutamate-mediated excitotoxicity elicits premotor circuit dysfunction and motor neuron overexcitation upon loss of eaat1
In Drosophila, the locomotor CPG network activates motor neurons via cholinergic and GABAergic interneurons (Figure 4D, top panel) (Rohrbough and Broadie, 2002), and motor neurons do not receive direct excitatory glutamatergic inputs (Kohsaka et al., 2017). Moreover, Drosophila can utilize glutamate as an inhibitory neurotransmitter that activates glutamate-gated chloride channel α (GluClα) to elicit Cl– influx (Cully et al., 1996). Glutamatergic period-positive median segmental interneurons (PMSIs) are responsible for relaying sensory inputs to motor neurons (Clark et al., 2018; Kohsaka et al., 2014). Nonetheless, removal of one copy of gluClα did not modify the motor-system defects associated with eaat1hypo mutants (Figure 3—figure supplement 1), raising the interesting possibility that excess synaptic glutamate caused by loss of eaat1 may trigger excitotoxicity to alter locomotor CPG activity, which secondarily elicits excess stimulation of motor neurons. To test this possibility, we first neutralized the increased perisynaptic glutamate associated with eaat1hypo mutants by knocking down the vesicular glutamate transporter (vglut) in glutamatergic neurons, which is anticipated to reduce the glutamate loading of synaptic vesicles and hence glutamate release. Expression of vglut-RNAi using OK371-GAL4 lowered excess perisynaptic glutamate in eaat1hypo mutants (Figure 2B,C). Furthermore, it largely rescued the altered locomotor CPG activity and impaired locomotion of eaat1hypo mutants (Figure 3A–D; Figure 1—figure supplement 3A–B). It has been shown previously that the locomotor CPG circuit is assembled within the VNC (Cattaert and Birman, 2001). Consistently, when we expressed UAS-eaat1-venus solely in the VNC of eaat1hypo mutants using teashirt(tsh)-GAL4, it significantly reversed the prolonged CPG outputs (Figure 3A–C) and movement defects (Figure 3D). However, other CPG defects still remained (Figure 1—figure supplement 3A–B). Therefore, these results suggest that Eaat1 expressed in the VNC may modulate the locomotor CPG output pattern, especially burst duration, to protect motor neurons from excess premotor excitation. Eaat1 expressed in the central brain may be responsible for triggering the motor CPG and perhaps tuning intra-burst spike density. Therefore, the dual activities of Eaat1 control the speed and coordination of larval locomotion.
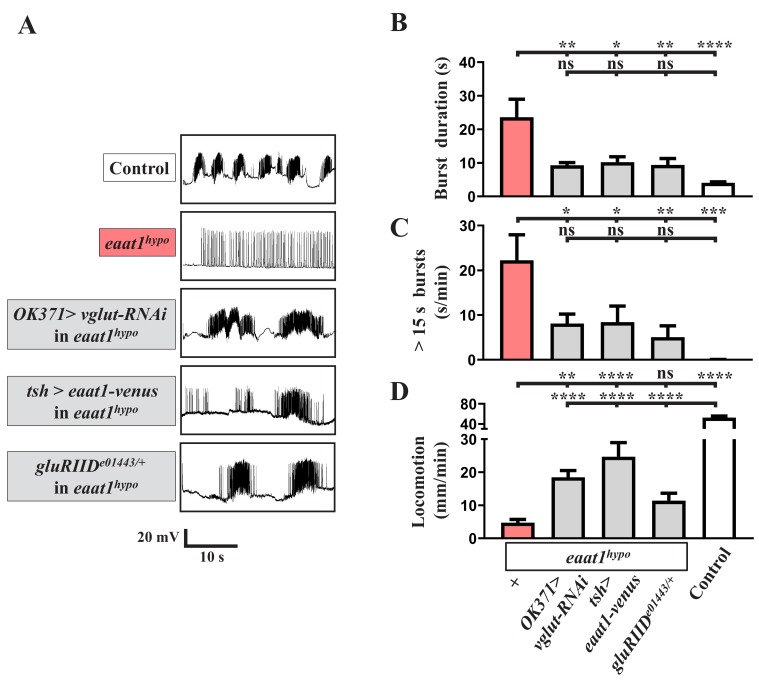
Figure 3. Glutamate-mediated excitotoxicity dysregulates premotor circuit activity in eaat1 mutants.
(A–D) Reducing glutamate release or inhibiting the postsynaptic glutamate receptor reverses prolonged burst duration in eaat1hypo mutants. (A) Representative traces of EJPs evoked by spontaneous motor CPG activity during fictive locomotion obtained from third instar larvae of controls (w1118) and the indicated genotypes. Quantification data for burst duration and overall firing time (for bursts of >15 s) per recording minute are shown in panels (B,C) (n ≥ 6 animals for each genotype). (D) Quantification data for locomotion of third instar larvae of controls (w1118) and the indicated genotypes (n ≥ 11 animals for each genotype). P values: ns, no significance; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: one-way ANOVA with Tukey’s post hoc test.
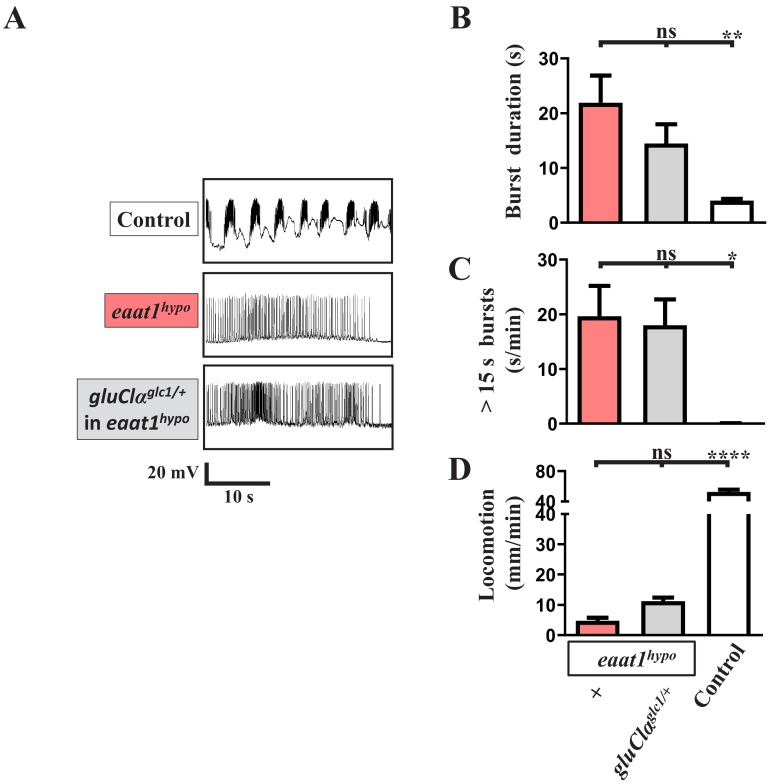
Figure 3—figure supplement 1. Removal of one copy of gluClα does not affect the motor-system deficits caused by eaat1 depletion.
The AMPA-like glutamate receptor GluRIID is expressed in the central nervous system and is required for rhythmic locomotor CPG activity (Featherstone, 2005). Interestingly, like the expression of eaat1-venus driven by tsh-GAL4, removing one copy of gluRIID from eaat1hypo mutants reversed the prolonged CPG outputs (Figure 3A–C) but did not rescue the reduced burst frequency and intra-burst spike density (Figure 1—figure supplement 3A–B). However, gluRIID reduction only slightly benefited mutant locomotion (Figure 3D). Accordingly, it seems likely that excess glutamate could also affect coordination between segmental CPG networks by activating other types of glutamate-gated receptors, thereby leading to the defective locomotion. Together, these results suggest that loss of eaat1 expression from the VNC leads to glutamate-mediated excitotoxicity, causing premotor circuit dysfunction and prolonged CPG output to motor neurons, and thereby gives rise to motor-system deficits.
Oxidative stress elicits premotor circuit dysfunction upon loss of eaat1
It is known that glutamate excitotoxicity triggers bulk Ca2+ influxes to promote mitochondrial Ca2+ overload, overproducing ROS (Zeeshan et al., 2016). To investigate whether excess ROS production occurs within the locomotor CPG circuit upon glutamate excitotoxicity, we stained dissected VNCs with CM-H2DCFDA, a fluorescent ROS-sensing dye (Nguyen et al., 2018), to monitor cytosolic ROS levels. Compared to controls, increased ROS levels were evident in neuropils of eaat1hypo VNCs (Figure 4A–B). After abrogating excitotoxicity by reducing gluRIID, the increased ROS were significantly neutralized (Figure 4A–B), suggesting that glutamate-mediated excitotoxicity increases oxidative stress in the locomotor CPG circuit.
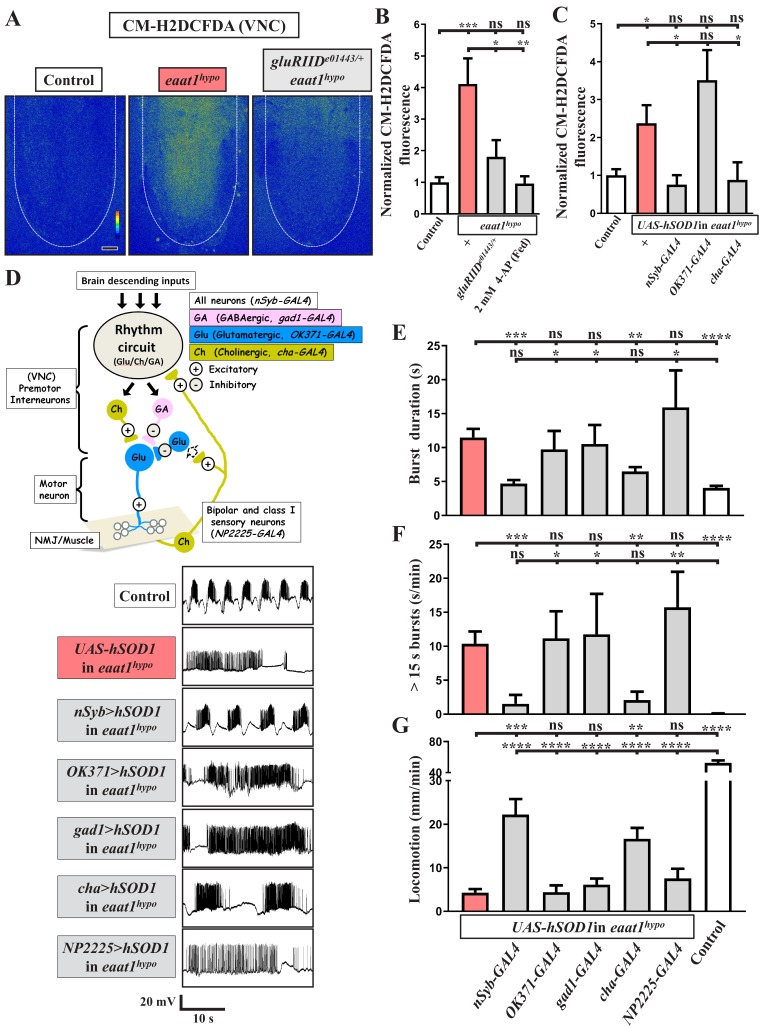
Figure 4. Loss of eaat1 elevates oxidative stress in cholinergic interneurons, leading to premotor circuit dysfunction.
(A–C) Loss of eaat1 elevates ROS in the VNC through excess activation of glutamate receptors. (A) Pseudocolored confocal images of the VNCs (outlined with white dotted lines) stained with CM-H2DCFDA obtained from third instar larvae of controls (w1118) and the indicated genotypes. Scale bar: 20 μm. (B) Averaged CM-H2DCFDA fluorescence intensity in VNCs was normalized to the value of controls (n ≥ 6 VNCs for each genotype). (C) Averaged CM-H2DCFDA fluorescence intensity in VNCs of third instar larvae of controls (w1118) and the indicated genotypes, normalized to the value of controls (n ≥ 5 VNCs for each genotype). (D–G) Increased oxidative stress in cholinergic interneurons contributes to dysregulated premotor circuit activity. Schematic of neuronal type and connectivity in the Drosophila larval locomotor circuit (top panel). Corresponding neurons expressing specific GAL4 drivers are indicated. Representative traces (bottom panel) of EJPs evoked by spontaneous motor CPG activity during fictive locomotion; these traces were obtained from third instar larvae of controls (w1118) and the indicated genotypes. (E–F) Quantification data for burst duration and overall firing time (for bursts > 15 s) per recording minute (n ≥ 6 animals for each genotype). (G) Quantification data for the locomotion of the third instar larvae of controls (w1118) and the indicated genotypes (n ≥ 10 animals for each genotype). P values: ns, no significance; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: one-way ANOVA with Tukey’s post hoc test.
To investigate the effect of increased oxidative stress on locomotor CPG activity, we expressed the UAS transgene of human copper-zinc superoxide dismutase (hSOD1) in eaat1hypo mutants. This manipulation has been used previously to erase excess ROS and to rescue ROS-triggered neuronal defects in Drosophila (Liu et al., 2015; Milton et al., 2011). Pan-neuronal expression of hSOD1 using nSyb-GAL4 eliminated the increased ROS in eaat1hypo mutants (Figure 4C) and also rescued the defects in locomotor CPG activity and larval movement (Figure 4D–G). These results provide evidence that excess ROS in neurons contributes to premotor circuit dysfunction in eaat1 mutants.
We then determined which population of neurons is potentiated and targeted by excess ROS. We first expressed hSOD1 in glutamatergic neurons in eaat1hypo mutants using OK371-GAL4. However, neither the increased ROS within the VNC nor those within the motor-system phenotypes were reversed (Figure 4C–G). Furthermore, no rescue was observed when hSOD1 was expressed in GABAergic neurons using gad1-GAL4 (Figure 4D–G). Remarkably, expression of hSOD1 in cholinergic neurons using cha-GAL4 led to a significant restoration of the ROS level, locomotor CPG activity, and locomotion, comparable to the effect of pan-neuronal hSOD1 expression (Figure 4C–G). Two subtypes of cholinergic sensory neurons, bipolar and class I, have been shown to deliver sensory feedback inputs to the locomotor CPG circuit during feed-forward locomotion (Cheng et al., 2010; Hughes and Thomas, 2007). However, targeted expression of hSOD1 in both these neuron subtypes using NP2225-GAL4 (Imlach et al., 2012) failed to affect the motor-system defects (Figure 4D–G). Hence, upon loss of eaat1, the excitotoxicity-induced ROS increase occurs in the cholinergic interneurons of the locomotor CPG network, dyregulating patterned locomotor CPG activity.
Excitotoxicity-induced oxidative stress hampers the excitability of cholinergic interneurons upon loss of eaat1
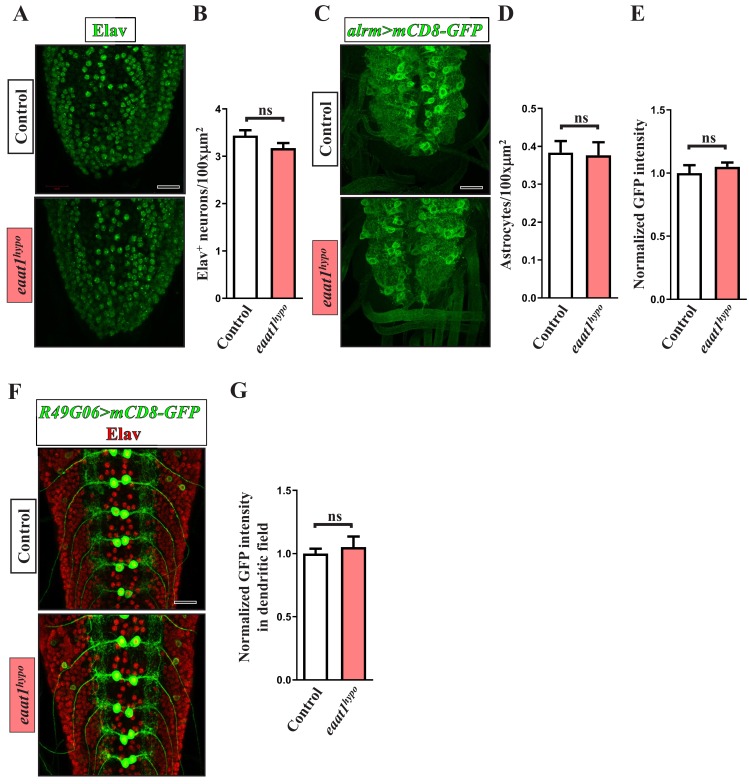
Premotor circuit dysfunction due to Eaat1 depletion may be attributable to either abnormal network assembly or dysregulated network activity. The Drosophila larval locomotor CPG circuit is assembled during the late embryonic stage (Kohsaka et al., 2012). Accordingly, we utilized the GAL4/GAL80ts system to control the expression of UAS-eaat1-venus spatiotemporally in the eaat1 mutant background. As shown in Figure 5A,B, the embryos of the control group (repo-GAL4/UAS-eaat1-venus/tub-GAL80ts in eaat1hypo mutants) were reared at 18°C to restrict the expression of eaat1-venus from 2 hr after egg laying to the late larval stage. As expected, the developed third instar (L3) larvae behaved like eaat1hypo mutants. When these embryos were reared at 29°C to allow expression of eaat1-venus throughout embryonic and larval development, the L3 larvae exhibited full restoration of movement (termed ‘full rescue’). However, restricted expression of eaat1-venus within the window of embryonic development (termed ‘embryonic rescue’) still resulted in defective locomotion. By contrast, the locomotion defect could be robustly normalized when the hatched larvae were reared at 29°C only during the larval stage (termed ‘L1–L3 rescue’). Thus, eaat1 is functionally required during the larval stage but not during embryonic development when the CPG circuit is assembled. Consistent with these results, we did not observe overt changes in VNC architecture in eaat1hypo mutants with regard to the number of neurons and astrocytes, the processes of astrocyte-like glia, and the dendritic field of motor neurons (Figure 5—figure supplement 1).
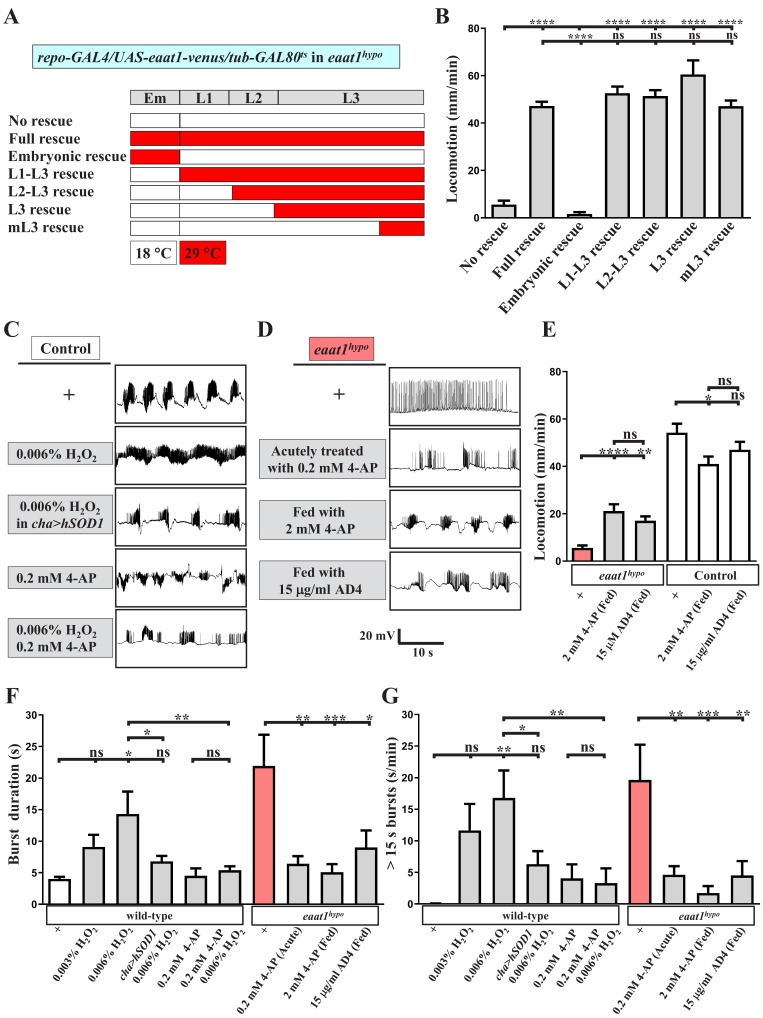
Figure 5. Increased excitotoxicity-induced ROS hampers the excitability of cholinergic interneurons.
(A–B) The locomotion defect caused by loss of eaat1 is rescued by expressing eaat1-venus at the late larval stage. (A) Schematic of the temporal expression of UAS-eaat1-venus controlled by the GAL80ts/GAL4 system during embryonic and larval stages. Animal genotypes are indicated. Developmental timescale of larvae at 18°C and 29°C: Em (embryo stage, 0–48 hr after egg laying (18°C) and 0–12 hr after egg laying (29°C)); L1 (first instar larvae, 0–48 hr after embryo hatching (18°C) and 0–12 hr after embryo hatching (29°C)); L2 (second instar larvae, 48–96 hr after embryo hatching (18°C) and 12–24 hr after embryo hatching (29°C)); and L3 (third instar larvae, 96–240 hr after embryo hatching (18°C) and 24–60 hr after embryo hatching (29°C)). Expression of eaat1-venus was restricted at 18°C (white boxes), but was switched on at 29°C (red boxes). (B) Quantification data for locomotion of third instar larvae (n ≥ 8 third instar larvae for each genotype). (C) Acute exposure of H2O2 phenocopies the prolonged burst duration of the motor CPG, which is reversed by expression of hSOD1 in cholinergic interneurons or by 0.2 mM 4-AP treatment. The representative traces show EJPs evoked by spontaneous motor CPG activity during fictive locomotion obtained from third instar wild-type controls (w1118) and third instar wild-type controls expressing hSOD1 with cha-GAL4. Larval fillets were acutely exposed to 0.006% H2O2-containing HL3 solution for 3 min, followed by 10 min recordings in the same solution. For 4-AP treatment, larval fillets were bathed in 0.2 mM 4-AP-containing HL3 solution for 5 min and then bathed in 0.2 mM 4-AP/0.006% H2O2-containing HL3 solution for 3 min, followed by 10 min recordings in the same solution. Quantification data for burst duration and overall firing time (for bursts of >15 s) per recording minute are shown in panels (F,G) (n ≥ 8 animals for each genotype). (D) Prolonged burst duration caused by loss of eaat1 can be rescued by acute treatment of 0.2 mM 4-AP or by long-term feeding of 2 mM 4-AP or 15 μg/ml AD4. Representative EJP traces evoked by spontaneous motor CPG activity during fictive locomotion obtained from third instar eaat1hypo/hypo mutants. Larval fillets were bathed in 0.2 mM 4-AP-containing HL3 solution for 5 min, followed by 10 min recordings in the same solution. For long-term drug treatment, eaat1hypo mutants were fed with 2 mM 4-AP or 15 μg/ml AD4 throughout the larval stage. Larval fillets were subjected to recordings in HL3 solution. Quantification data for burst duration and overall firing time (for bursts of >15 s) per recording minute are shown in panels (F,G) (n ≥ 7 animals for each genotype). (E) Long-term feeding of 2 mM 4-AP or 15 μg/ml AD4 improves locomotion of eaat1hypo mutants. 2 mM 4-AP but not 15 μg/ml AD4 slightly reduced locomotion of control (w1118) larvae. Locomotion of treated larvae was measured and quantified (n ≥ 17 animals for each genotype). P values: ns, no significance; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: one-way ANOVA with Tukey’s post hoc test.
Figure 5—figure supplement 1. No overt change in the structural integrity of the larval VNC upon loss of eaat1.
Intriguingly, when expression of eaat1-venus was switched on in eaat1hypo mutants progressively from L2, early L3, or even the middle L3 stage, all of these expression conditions provided robust rescue of locomotion (termed ‘L2-L3’, ‘L3’ and ‘mL3’ rescues, respectively, Figure 5A–B), suggesting that excitotoxicity-induced oxidative stress may result in temporal and reversible dysregulation of locomotor CPG activity, which can be normalized whenever the Eaat1 function is recovered. Accordingly, it is possible that acutely increasing oxidative stress in the locomotor CPG circuit would mimic the effect of the eaat1 mutation. To test this possibility, we exposed dissected wild-type larval fillets to low concentrations of H2O2 (0.003% and 0.006%) for ~5 min and measured locomotor CPG activity. Remarkably, H2O2 exposure could prolong CPG output duration in a dose-dependent manner (Figure 5C and F–G). By contrast, when the anti-oxidative ability of cholinergic neurons was enhanced by expressing hSOD1, the circuit effect of H2O2 was greatly diminished (Figure 5C and F–G). Together, these data suggest that, upon loss of eaat1, a mild level of ROS does not perturb the synaptic connectivity of the locomotor circuit but instead alters its activity by influencing cholinergic transmission.
Oxidization of voltage-gated potassium channels caused by excess ROS can attenuate their inactivation, resulting in neuronal silencing under disease conditions (Sahoo et al., 2014; Sesti et al., 2010). Therefore, we hypothesized that premotor circuit dysfunction upon loss of eaat1 may arise from ROS-mediated inactivation of cholinergic interneurons. The K+ channel blocker 4-aminopyridine (4AP) is a clinical treatment for multiple sclerosis (Chwieduk and Keating, 2010). We incubated dissected wild-type larval fillets with 0.2 mM 4-AP-containing media for 5 min and then recorded CPG activity in the setting of 0% or 0.006% H2O2 treatment. Administration of 4-AP slightly increased the CPG output duration in non-H2O2-treated animals (Figure 5C and F–G), presumably due to enhanced excitability of the locomotor circuit. Nonetheless, 4-AP administration reversed prolonged CPG outputs induced by 0.006% H2O2 treatment (Figure 5C and F–G). In addition, acute 4-AP treatment alleviated the CPG output defect associated with the eaat1 mutation (Figure 5D and F–G). Next, we fed eaat1hypo mutants with food containing 2 mM 4-AP throughout the larval stages. This manipulation also abrogated the locomotion defect (Figure 5E). Our CPG recordings revealed that ~70% (12/17) of 4-AP-treated mutants displayed normalized CPG output patterns (Figure 5D and F–G), whereas the remaining animals (5/17) still showed mutant-like alterations (not shown). This incomplete rescue could be due to insufficient drug penetration across the blood–brain barrier surrounding the VNC. Last, treatment of eaat1hypo mutants with 15 μg/ml N-acetylcysteine amide (AD4), a potent membrane penetrating antioxidant (Liu et al., 2015), also significantly corrected both premotor circuit dysfunction and compromised locomotion (Figure 5D–G). Notably, when wild-type controls were fed with the food containing either 2 mM 4-AP or 15 μg/ml AD4, only a slight reduction in locomotion activity was observed (Figure 5E), indicating that the above-described rescue effects do not result from an overall increase in locomotor CPG activity. Taken together, these findings strongly suggest that the excitotoxicity-induced increase in ROS upon loss of eaat1 hampers the excitability of cholinergic interneurons, leading to premotor circuit dysfunction.
ROS-induced muscle weakness feedback exacerbates premotor circuit dysfunction upon loss of eaat1
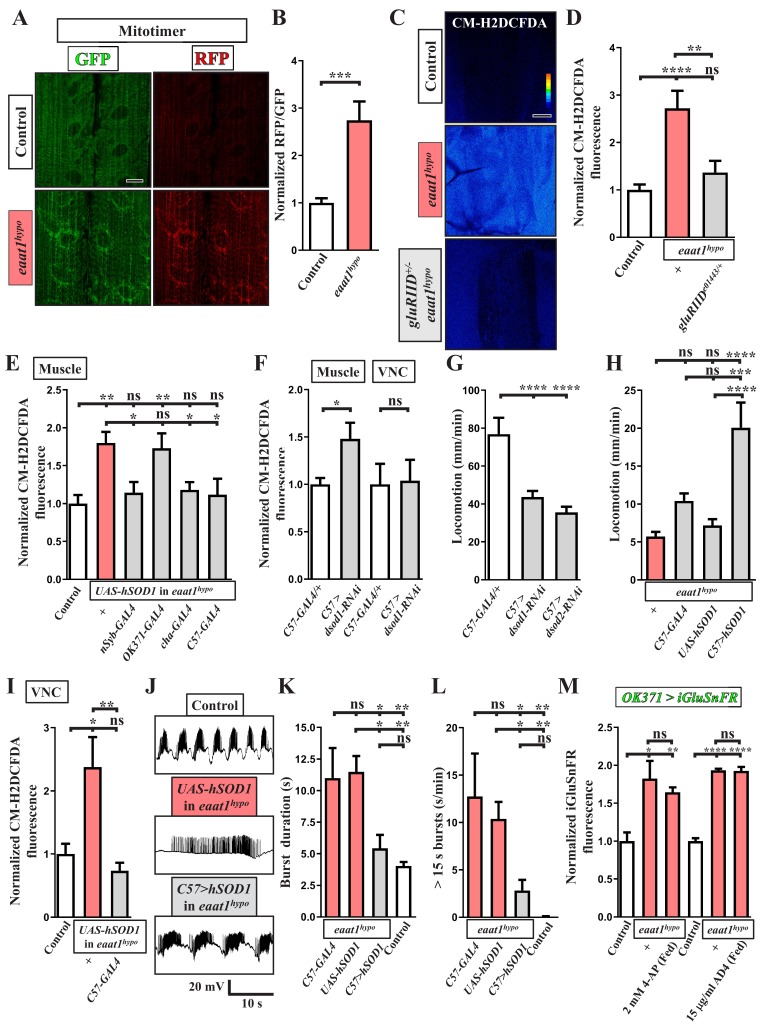
Given the impaired locomotion phenotype, we then investigated whether excess excitation of motor neurons upon Eaat1 depletion could boost mitochondrial ROS production in larval muscles and influence muscular physiology. Mitochondrial ROS in muscles was probed by expressing mitotimer using C57-GAL4, a muscle-specific GAL4 driver. Mitotimer is a mitochondria-targeted timer that switches its fluorescence from green fluorescence protein (GFP) to red fluorescence protein (RFP) upon oxidation (Laker et al., 2014). Compared to control muscles, the RFP/GFP ratio of mitotimer was significantly higher in eaat1hypo mutant muscles (Figure 6A,B), indicating an increased level of mitochondrial ROS. Note that the distribution of mitochondria in muscles is also slightly altered in eaat1 mutants. Consistent with this result from mitotimer, we detected elevated cytosolic ROS levels in eaat1hypo mutant muscles, as detected by CM-H2DCFDA staining (Figure 6C,D). The ROS increase was normalized after the increased inputs from motor neurons were abrogated by reducing gluRIID (Figure 3 and Figure 6C,D) or by expression of hSOD1 driven by nSyb-GAL4 or cha-GAL4 (Figure 4D–G and Figure 6E). By contrast, expression of hSOD1 driven by OK371-GAL4 failed to rescue altered locomotor CPG activity (Figure 4D–G) and excess muscular ROS (Figure 6E). Therefore, the altered locomotor CPG activity due to loss of eaat1 can overexcite motor neurons and muscles, promoting oxidative stress in muscles.
Figure 6. ROS-induced muscle weakness feedback maintains the increased premotor oxidative stress to exacerbate circuit dysfunction.
(A,B) Loss of eaat1 induces mitochondrial oxidative stress in muscles. (A) Confocal images of muscles 6 and 7 of third instar larvae expressing mitotimer using C57-GAL4 obtained from wild-type controls (w1118) and eaat1hypo/hypo mutants. Scale bar: 20 µm. (B) The RFP/GFP ratio of mitotimer is assessed and normalized to the value of controls (n ≥ 6 animals for each genotype). (C,D) Reducing gluRIID can normalize the increased oxidative stress resulting from loss of eaat1. (C) Pseudocolored confocal images of muscles 6 and 7 of the third instar larvae of controls (w1118) and the indicated genotypes stained with CM-H2DCFDA. Scale bar: 20 μm. (D) Averaged CM-H2DCFDA fluorescence intensity was quantified and normalized to the value of controls (n ≥ 13 A3 muscles 6 and 7 from (n ≥ 7) animals for each genotype). (E) Expression of hSOD1 using nSyb-GAL4, cha-GAL4 or C57-GAL4 but not OK371-GAL4 relieves the muscular oxidative stress of eaat1hypo mutants. CM-H2DCFDA fluorescence intensity of muscles 6 and 7 from the third instar larvae of controls (w1118) and the indicated genotypes is quantified and normalized to the value of controls (n ≥ 12 A3 muscles 6 and 7 from (n ≥ 7) animals for each genotype). (F) Muscular expression of dsod1-RNAi using C57-GAL4 promotes ROS production in muscles but not in VNCs. Quantification data for CM-H2DCFDA fluorescence are shown. (n ≥ 7 animals for each genotype.) (G) Muscular knockdown of dsod1 or dsod2 impairs larval locomotion. UAS-dsod1-RNAi or UAS-dsod2-RNAi is expressed by using C57-GAL4, and larval locomotion was quantified (n ≥ 21 animals for each genotype). (H) Expression of hSOD1 using C57-GAL4 improves eaat1hypo mutant locomotion. Locomotion of third instar larvae of the indicated genotypes is quantified (n ≥ 23 animals for each genotype). (I–L) Expression of hSOD1 using C57-GAL4 relieves premotor oxidative stress of eaat1hypo mutants and reverses premotor circuit dysregulation. (I) The CM-H2DCFDA fluorescence intensity of VNCs of thethird instar larvae of controls (w1118) and the indicated genotypes was quantified and normalized to the value of controls (n ≥ 6 animals for each genotype). (J) Representative traces of EJPs evoked by spontaneous motor CPG activity during fictive locomotion obtained from the third instar larvae of controls (w1118) and the indicated genotypes. (K–L) Quantification data for burst duration and overall firing time (for bursts of >15 s) per recording minute (n ≥ 7 animals for each genotype). (M) Either neuronal inactivation or relieving oxidative stress does not affect the levels of perisynaptic glutamate of glutamatergic interneurons in eaat1 mutants. Perisynaptic glutamate was detected by expression of the iGluSnFR reporter driven by OK371-GAL4. Averaged iGluSnFR fluorescence intensity was quantified and normalized to the value of controls (n ≥ 4 VNC for each genotype). P values: ns, no significance; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: one-way ANOVA with Tukey’s post hoc test.
Figure 6—figure supplement 1. Phenotypic characterization of dsod1 knockdown larvae.
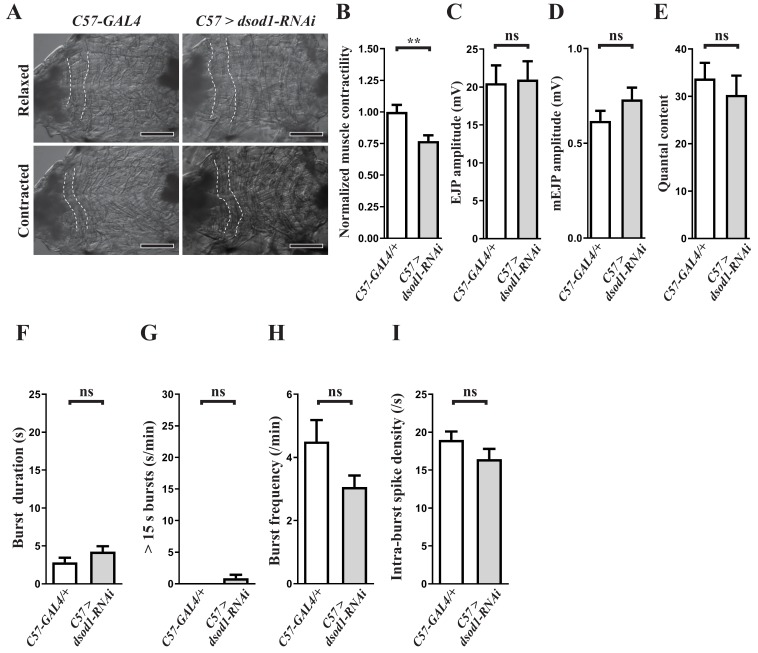
To assess whether excess ROS influences muscle strength, we boosted oxidative stress in muscles by knocking down Drosophila superoxide dismutase 1 (dsod1) before measuring muscle contractility and larval locomotion. Muscular expression of UAS-dsod1-RNAi using C57-GAL4 elevated ROS production in muscles but not in other tissues, such as the VNC (Figure 5F). The muscle contractility of larvae was measured during spontaneous peristaltic waving using a video-tracking system. Unlike GAL4 controls, muscles of dsod1 knockdown larvae could not contract properly (Figure 6—figure supplement 1A–B). As a result, these larvae also showed compromised locomotion (Figure 6G). A similar locomotion defect was obtained by knocking down dsod2 (Figure 6G), which encodes Drosophila mitochondrial Sod. Furthermore, when we expressed hSOD1 in eaat1hypo mutant muscles using C57-GAL4, the ROS increase was abrogated (Figure 6E) and larval locomotion significantly improved (Figure 6H). Note that muscular knockdown of dsod1 alone did not affect normal synaptic transmission (Figure 6—figure supplement 1C–E) or locomotor CPG activity (Figure 6—figure supplement 1F–I). Therefore, these results suggest that the increased oxidative stress triggered by tonic motor neuron stimulation upon loss of eaat1 weakens muscle contraction and larval movement.
However, this significant improvement in larval locomotion of the eaat1 mutants by muscular expression of hSOD1 was surprising, as we had expected that aberrant locomotor CPG pattern and impaired muscle contractility together contribute to the compromised locomotion. Previous studies have shown that the contractile status of muscles is coupled with the activation of proprioceptive sensory neurons, through which muscle contraction triggers sensory input to modulate or terminate locomotor CPG output to motor neurons (Hughes and Thomas, 2007; Kohsaka et al., 2017; Song et al., 2007). Therefore, this scenario raises the attractive possibility that inefficient muscle contraction upon loss of eaat1 may attenuate sensory feedback inhibition to exacerbate premotor circuit dysfunction. In support of this possibility, muscular expression of hSOD1 not only relieved the ROS increase in the locomotor CPG circuit (Figure 6I), but also reversed the prolonged circuit output (Figure 6J–L). We also treated eaat1 mutants with 2 mM 4-AP to re-activate cholinergic interneurons, which reversed aberrant locomotor CPG activity and defective locomotion (Figure 5D–E). Consistent with the effect of muscular expression of hSOD1, the ROS increase in the eaat1 mutant VNC was significantly relieved by means of 2 mM 4-AP treatment (Figure 4B). Interestingly, under this condition, the increase in perisynaptic glutamate in eaat1 mutants was not affected (Figure 6M). A similar result was obtained by treatment with the antioxidant AD4 (Figure 6M). Hence, these results indicate that excitotoxicity can induce oxidative stress in the locomotor CPG circuit and muscles and can lead to their dysfunction via a motor circuit-dependent mechanism, and that the feedback arising from inefficient muscle contraction sustains oxidative stress in the locomotor CPG circuit independently of glutamate release.
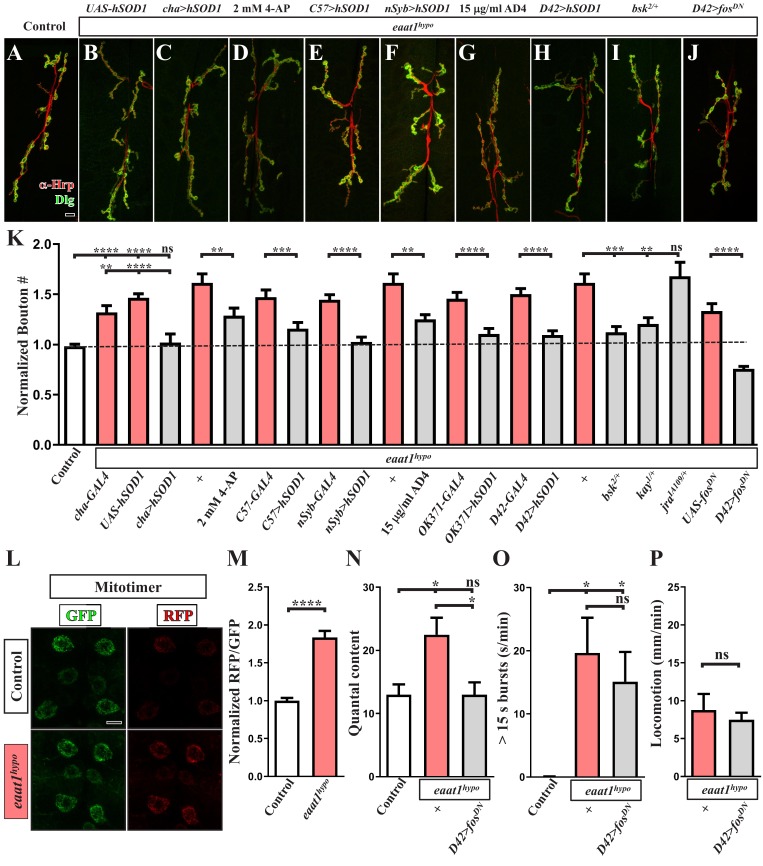
The ROS-induced JNK signaling pathway alters NMJ bouton architecture
Growth of Drosophila NMJ boutons is linked to the excitation status of motor neurons (Budnik et al., 1990; Oswald et al., 2018a; Tsai et al., 2012). In addition, elevated oxidative stress was previously shown to enhance the formation of NMJ boutons (Milton et al., 2011). Therefore, we postulated that, upon Eaat1 depletion, excess CPG stimulation of motor neurons may boost oxidative stress, altering NMJ bouton architecture. As shown in Figure 7L–M, eaat1hypo mutant motor neurons exhibited an increased RFP/GFP ratio of mitotimer compared to that in control motor neurons. This outcome suggests that motor neuron overexcitation does indeed elevate oxidative stress. Furthermore, when excess excitation of eaat1hypo mutant motor neurons was corrected by feeding larvae with 4-AP (Figure 5) or expressing hSOD1 using cha-GAL4 or C57-GAL4 (Figure 4 and Figure 6), the NMJ bouton phenotype was also partially or fully rescued (Figure 7A–E and K). Similarly, expression of hSOD1 in all neurons (using nSyb-GAL4), or specifically in glutamatergic neurons (using OK371-GAL4) or motor neurons (using D42-GAL4), resulted in robust phenotypic rescue (Figure 7F, H and K). Moreover, treatment with 15 μg/ml AD4 had the same effect (Figure 7G and K). However, expression of hSOD1 driven by OK371-GAL4 did not rescue prolonged CPG outputs (Figure 4). Hence, our data indicate that the excitotoxicity-induced ROS increase acts cell-autonomously to alter NMJ bouton formation upon loss of eaat1.
Figure 7. Premotor circuit dysfunction causes altered NMJ bouton architecture via ROS-dependent activation of the JNK signaling pathway upon loss of eaat1.
(A–J) Representative confocal images of NMJs co-stained with α-HRP (red) and α-Dlg (green) obtained from third instar larvae of controls (w1118) and the indicated genotypes. Scale bar: 10 µm. (K) Quantification data for the number of NMJ boutons per muscle area normalized to the value of controls (n ≥ 7 NMJs of A2 muscles 6 and 7 derived from n ≥ 7 animals for each genotype). (L–M) Loss of eaat1 increases mitochondrial ROS in motor neurons. (L) Representative confocal images of motor neurons of third instar larvae expressing mitotimer using D42-GAL4 obtained from controls (w1118) and eaat1hypo/hypo mutants. Scale bar: 5 µm. (M) The RFP/GFP ratio of mitotimer was quantified and normalized to the value of controls (n ≥ 10 animals for each genotype). (N,O) Expression of fosDN in motor neurons rescues the NMJ bouton phenotype based on normalized quantal content, but does not affect premotor circuit dysregulation in eaat1hypo mutants. (N) Quantification data for quantal content recorded from A3 muscle 6 of third instar larvae of controls (w1118) and the indicated genotypes with 0.2 Hz electric stimulation in 0.5 mM Ca2+-containing HL3 solution (n ≥ 6 animals for each genotype). (O) Quantification data for overall firing time (for bursts of >15 s) per recording minute (n ≥ 8 animals for each genotype). (P) Quantification data for larval locomotion of eaat1hypo mutants and eaat1hypo mutants who express fosDN in motor neurons (n ≥ 20 animals for each genotype). P values: ns, not significant; *, p<0.05; **, p<0.01; ***, p<0.001; ****, p<0.0001. n: replicate number. Error bars indicate SEM. Statistics: Student's t-test or one-way ANOVA with Tukey’s post hoc test.
The conserved c-JUN-N-terminal kinase (JNK) stress signaling pathway is activated by increased oxidative stress to mediate a variety of cellular events, including differentiation, survival, and apoptosis (Kim and Choi, 2010). It has also been shown that the ROS-JNK axis positively regulates NMJ bouton growth in Drosophila (Milton et al., 2011). To investigate whether ROS-dependent activation of JNK signaling drives the NMJ bouton change associated with Eaat1 depletion, we genetically reduced the levels of key components of the JNK signaling pathway in the eaat1hypo mutant background. Removal of one copy of bsk (encoding the Drosophila homolog of JNK) or kay (encoding the Drosophila homolog of c-FOS) from eaat1hypo mutants resulted in the restoration of normal NMJ bouton morphology (Figure 7I and K). Consistent with these results, motor-neuron-specific expression of the dominant-negative form of c-Fos (c-FosDN) rescued the bouton phenotype (Figure 7J–K). By contrast, reducing jra that encodes the Drosophila homolog of c-JUN had no effect (Figure 7K), which is consistent with a previous finding (Milton et al., 2011). Restoration of NMJ bouton morphology could further normalize the release probability of eaat1hypo mutant NMJs (Figure 7N), but it did not have an impact on CPG circuit dysregulation (Figure 7O) or compromised locomotion (Figure 7P). Hence, these findings indicate that ROS-activated JNK signaling cell-autonomously causes abnormal NMJ bouton formation in eaat1 mutants, and they support premotor circuit dysfunction as being the primary cause of NMJ bouton abnormalities and compromised locomotion upon loss of eaat1.
Discussion
In this work, we utilized a fly model of glutamate excitotoxicity induced by loss of Drosophila eaat1 to explore the impact of glutamate excitotoxicity on the integrity of the motor system. We report a circuit-dependent feedback mechanism for increasing ROS that mediates excitotoxicity to alter premotor circuit activity, NMJ architecture, and motor function. As summarized in Figure 8, glutamate excitotoxicity initially alters locomotor CPG activity and hence prolongs CPG output bursts onto motor neurons by ROS-mediated inactivation of the cholinergic interneurons constituting the CPG circuit. Then, tonic premotor stimulation triggers activity-dependent ROS overproduction in both motor neurons and muscles. In muscles, the increased ROS level gradually dampens muscle contractility and consequent sensory input back to the locomotor CPG circuit, with this feedback strengthening ROS accumulation within the CPG circuit to exacerbate circuit dysfunction. Thus, a positive feedback loop between ROS production in the CPG circuit and muscles is established. Finally, in motor neurons, the induced ROS activate JNK stress signaling to promote abnormal NMJ bouton outgrowth and strength. Apart from genetic rescue, pharmacological treatment with the antioxidant AD4 or the K+ channel blocker 4-AP can also significantly alleviate these motor-system deficits.
Figure 8. A schematic model of a circuit-dependent ROS feedback loop under glutamate excitotoxicity induced by loss of eaat1.
The details are presented in the discussion section.
Glutamatergic transmission regulates the Drosophila locomotor CPG circuit
The locomotor CPG circuit for Drosophila larval feed-forward locomotion is positioned in the VNC and is activated by input from the central brain (Cattaert and Birman, 2001). Furthermore, acute treatment of dissected Drosophila larvae with non-competitive NMDA antagonists has been shown to reduce the initial output burst duration of the locomotor CPG and eventually abolishes all output activity (Cattaert and Birman, 2001), suggesting that glutamatergic transmission drives locomotor CPG activity and positively controls its output burst duration during larval movement. Consistent with these latter results, we have shown herein that VNC-restricted expression of eaat1-venus using tsh-GAL4 could reverse the prolonged CPG output burst (Figure 3) but not the reduced CPG output frequency (Figure 1—figure supplement 3) in eaat1 mutants, indicating that central brain removal of eaat1 reduced burst frequency, whereas VNC removal markedly extended burst duration. The exact neuronal identity and network connections that build up the core components of the Drosophila larval locomotor CPG circuit remain unknown (Kohsaka et al., 2017; Ohyama et al., 2015). Intriguingly, the phenotype of prolonged CPG output has also been reported under conditions in which the motor neuron inputs from proprioceptive sensory neurons or period-positive median segmental interneurons (PMSI) are limited (Kohsaka et al., 2014; MacNamee et al., 2016; Song et al., 2007). Moreover, RNAi-mediated knockdown of eaat1 extends PMSI-evoked inhibitory postsynaptic currents in motor neurons (MacNamee et al., 2016). We also noticed an increase in extrasynaptic glutamate at the axonal synapses of PMSI when eaat1 is lost (unpublished data), raising an alternative possibility that excess extrasynaptic glutamate may desensitize GluClα to further diminish sensory inhibition feedback. However, we found that reducing gluRIID but not gluClα in the eaat1 mutant background shortened prolonged CPG output (Figure 3 and Figure 3—figure supplement 1). Hence, upon loss of eaat1, glutamate-mediated excitotoxicity mainly contributes to locomotor CPG circuit dysfunction. In this regard, the CPG outputs to motor neurons may be elongated and/or the potential inhibition from CPG output to PMSI or its upstream interneurons may be abrogated (Figure 8). Further experiments will be needed to unravel the detailed mechanism operating in the CPG circuit upon loss of eaat1.
ROS-mediated inactivation of cholinergic transmission underlies the locomotor CPG dysregulation in eaat1 mutants
Targeted relief of the increased ROS in cholinergic interneurons by genetic approaches could significantly alleviate altered CPG activity arising from either eaat1 mutation (Figure 4) or short-term exposure to H2O2 (Figure 5), indicating that a subset of cholinergic interneurons, which presumably constitutes the locomotor CPG circuit, is vulnerable to and influenced by the ROS increase. Our temporal rescue experiments further suggest that the effect of the ROS increase on circuit activity is acute and reversible (Figure 5). In support of the fact that ROS is known to reduce the inactivation of voltage-gated potassium channels in neurons (Sahoo et al., 2014; Sesti et al., 2010), long-term food-mediated feeding of (or even short-term exposure to) the K+ channel blocker 4-AP led to a restoration of CPG activity in eaat1 mutants (Figure 4 and Figure 5). Thus, temporal hypoexcitability of cholinergic interneurons most probably underlies ROS-induced locomotor CPG dysfunction upon eaat1 loss. Interestingly, immediate blockade of glutamatergic transmission shortens the burst duration of the CPG output (Cattaert and Birman, 2001). Under this scenario, it is expected that shortened rather than prolonged CPG burst durations should occur upon loss of eaat1. Thus, it is likely that the induced ROS may occur in a restricted way in a certain subset of cholinergic interneurons, resulting in uneven suppression of cholinergic transmission in the locomotor CPG circuit.
The GABA neurotransmitter has a crucial role in neuronal inhibition in the central nervous system through its actions on GABA receptors (Farrant and Nusser, 2005). Notably, regulation of GABAergic transmission by redox signaling is increasingly recognized (Beltrán González et al., 2019). ROS, especially those derived from mitochondrial respiration, act to strengthen the neuronal inhibition mediated by GABAA receptors (Accardi et al., 2014; Penna et al., 2014). Thus, we do not exclude an alternative possibility that, if those ROS-vulnerable cholinergic interneurons also receive GABAergic input, the increased ROS may silence cholinergic transmission of the locomotor CPG circuit by strengthening GABA-mediated inhibition.
ROS-induced muscle weakness initiates a circuit-dependent ROS feedback loop
The pathological roles of ROS in the regulation of skeletal muscles have been studied extensively (Barbieri and Sestili, 2012; Moylan and Reid, 2007; Powers et al., 2011), and most targets of redox signaling in skeletal muscle participate in muscle contraction. For instance, excess ROS can modulate SR calcium ATPase (SERCA) and ryanodine receptor (RyR) activity (Gutiérrez-Martín et al., 2004; Xu et al., 1997; Zima and Blatter, 2006), both of which control the Ca2+ homeostasis of sarcoplasmic reticulum. ROS exposure can also oxidize some myofilament proteins, such as myosin heavy chain and troponin C and, in turn, can impair their functions (Coirault et al., 2007; Plant et al., 2000; Yamada et al., 2006). Consistent with these findings, the ROS increase dampens the muscle contractility of Drosophila larvae. We found that mitochondrial and cytosolic ROS levels increase upon excess motor neuron stimulation when eaat1 is lost (Figure 6). Moreover, while increasing ROS by dsod1 knockdown reduced muscle contractility and movement velocity, relieving excess ROS in eaat1 mutant muscles improved locomotion (Figure 6). In the motor system, muscles are not only recognized as the end executive tissues for body movement, but also have a crucial role in triggering proprioceptive sensory feedback input to the central circuit (Hughes and Thomas, 2007; Kohsaka et al., 2017; Song et al., 2007). Recent studies in Drosophila have also revealed that proprioceptive sensory feedback plays a vital role in tuning locomotor circuit activity in the homeostatic adjustment of Drosophila larval crawling (Oswald et al., 2018a) and in a Drosophila model of amyotrophic lateral sclerosis (ALS) (Held et al., 2019). Unexpectedly, we found that, upon glutamate excitotoxicity, ROS-induced muscle weakness can cause inefficient sensory feedback input to worsen the ROS burden and can negatively impact the functioning of the central locomotor network. Therefore, under pathological conditions, impaired muscle activity can serve as a key mediator for initiating the ROS feedback loop between the CPG circuit and muscles, which may contribute to network dysfunction in excitotoxicity-associated diseases.
Excitotoxicity-induced premotor circuit dysfunction elicits activity-dependent synaptic changes
ROS are known to activate the JNK/AP-1 signaling pathway (Zhang et al., 2016) that regulates synaptic formation and strength in Drosophila (Collins et al., 2006; Milton et al., 2011; Sanyal et al., 2003; Sanyal et al., 2002; Shen and Ganetzky, 2009; West et al., 2015). The mutation in Drosophila spinster (spin), which encodes a late endosome and lysosome protein (Dermaut et al., 2005; Sweeney and Davis, 2002), causes impaired lysosomal activity and a consequent ROS burden, leading to synaptic bouton outgrowth by activating the JNK signaling pathway (Milton et al., 2011). Intriguingly, c-FOS but not c-JUN is important for bouton outgrowth under spin loss (Milton et al., 2011). Similarly, we found that the synaptic bouton phenotypes of eaat1 mutants are dependent on ROS and c-FOS activity (Figure 7). Interestingly, Milton et al., 2011) have shown that ‘constitutive’ boosting of mitochondria-derived ROS under loss of dsod2 or after paraquat treatment can also promote bouton growth, but in that case it requires both c-FOS and c-JUN activities. By contrast, in eaat1 mutants, the altered CPG pattern possibly elicits a pulsed increase of mitochondrial ROS. Thus, it may be postulated that different resources and temporal generation of ROS may be responsible for engaging different cellular signaling processes. In support of this notion, in addition to mitochondria, NADPH oxidases provide another major source of ROS to control diverse cellular processes (Brennan et al., 2009; Oswald et al., 2018b; Zhang et al., 2016). Recently, DJ-1β, a Parkinson’s disease-linked protein, has been identified as a redox sensor that mediates the mitochondrial ROS regulating activity-dependent synaptic plasticity at Drosophila NMJ (Oswald et al., 2018a). It will be interesting to further investigate the underlying mechanisms in detail.
Potential relevance of ROS-induced motor-circuit dysregulation for neurodegenerative diseases
Downregulation of EAAT2 has been demonstrated in patients with Alzheimer’s disease (Jacob et al., 2007; Li et al., 1997) or amyotrophic lateral sclerosis (ALS) (Rothstein et al., 1995), as well as in ALS rodent models (Bendotti et al., 2001; Bruijn et al., 1997; Howland et al., 2002; Tong et al., 2013). ALS is a fatal adult-onset disease that predominantly causes NMJ denervation, motor neuron degeneration, and compromised motor function (Taylor et al., 2016). Spinal removal of mouse EAAT2 is sufficient to elicit motor neuron death (Sugiyama et al., 2017; Sugiyama and Tanaka, 2018). Transgenic expression of EAAT2 (Guo et al., 2003) or treatment with the small compound LDN/OSU-0212320 (Kong et al., 2014), which mainly increases translation of EAAT2 mRNA, improves the motor performance of an ALS mouse model expressing hSOD1G93A. However, a recent clinical study testing ceftriaxone, an FDA-approved β-lactam antibiotic that can transcriptionally promote EAAT2 expression (Lee et al., 2008; Rothstein et al., 2005), in ALS patients concluded that this drug treatment had no therapeutic effect (Cudkowicz et al., 2014). Therefore, it is questionable whether increasing EAAT2 expression represents a feasible therapeutic strategy for ALS. It has been argued, however, that EAAT2 downregulation largely occurs at the posttranslational and not at the transcriptional level in ALS (Bristol and Rothstein, 1996; Kong et al., 2014). There was no evidence for increased EAAT2 in patients treated with ceftriaxone (Cudkowicz et al., 2014), and ceftriaxone treatment only slightly increases protein levels of EAAT2 in hSOD1G93A mice (Kong et al., 2014). In addition, the efficacy of ceftriaxone in hSOD1G93A mice is not consistent among different studies (Kong et al., 2012; Kong et al., 2014; Rothstein et al., 2005; Scott et al., 2008). Hence, more investigations will be needed to strengthen evidence for the pathogenic contribution of EAAT2 dysfunction in ALS.
Oxidative stress is known as a hallmark of Alzheimer’s disease (Wang et al., 2014; Zhao and Zhao, 2013), Parkinson’s disease (Blesa et al., 2015), and ALS (Barber and Shaw, 2010). During aging, neurons are thought to be susceptible to excitotoxicity (Lewerenz and Maher, 2015), and the nervous system and muscles are vulnerable to ROS accumulation because of high oxygen consumption demand (Jackson and McArdle, 2011; Liguori et al., 2018). Administration of antioxidants can improve the motor function of hSOD1G93A mice (Andreassen et al., 2000; Aoki et al., 2011; Crow et al., 2005; Gurney et al., 1996; Ito et al., 2008; Matthews et al., 1998) and ALS patients (Abe et al., 2014; The Writing Group, 2017). Nonetheless, how oxidative stress is produced in ALS and how this burden is involved in disease pathogenesis is not well understood. Interestingly, in our study, Drosophila Eaat1 depletion was shown to cause ALS-like characteristics, including motor neuron excitotoxicity, NMJ bouton abnormalities, muscle weakness, and compromised motor performance. In the future, it will be worth exploring whether ROS-induced motor circuit dysfunction might also participate in ALS progression and age-dependent motor system decline.
It has previously been shown that reduced excitability of proprioceptive sensory neurons and cholinergic interneurons is causative of locomotor CPG circuit dysfunction and compromised locomotion in Drosophila smn mutants, which are used as a Drosophila model of spinal muscular atrophy (SMA), a motor neuron disease of juveniles (Imlach et al., 2012; Lotti et al., 2012). Increasing neuronal excitability by 4-AP treatment reverses these motor system defects (Imlach et al., 2012; Lotti et al., 2012). Intriguingly, our data show that long-term food-mediated feeding of (or even short-term exposure to) the K+ channel blocker 4-AP also rescued altered locomotor CPG activity in eaat1 mutants (Figure 5). Notably, although the precise mechanisms are unknown, 4-AP has been used to treat several motor system-related disorders such as spinal cord injury (Hayes, 2007), Lambert-Eaton syndrome (Quartel et al., 2010), and hereditary canine spinal muscular atrophy (Pinter et al., 1997), and it is an FDA-approved therapy for multiple sclerosis (Chwieduk and Keating, 2010; Hayes, 2007). Thus, as supported by our findings, it seems plausible that neuronal hypoexcitability may be a shared mechanism underlying the motor-system defects displayed in motor-related disorders.
Materials and methods
Fly strains
Flies were reared in regular food at 25°C. To obtain third instar eaat1hypo mutants, eggs were laid on grape juice plates covered with yeast paste, and larvae were grown on a fresh plate with yeast paste at 25°C. The EMS-mutagenized mutants were kindly provided by Hugo J Bellen. Other fly stocks were obtained from the Bloomington Drosophila Stock Center (https://bdsc.indiana.edu/) and the Vienna Drosophila RNAi Center (https://stockcenter.vdrc.at/control/main): nSyb-GAL4 (Pauli et al., 2008); OK371-GAL4 (Mahr and Aberle, 2006); D42-GAL4 (Yeh et al., 1995); cha-GAL4 (Salvaterra and Kitamoto, 2001); gad1-GAL4 (Ng et al., 2002); repo-GAL4 (Sepp et al., 2001); alrm-GAL4 (Doherty et al., 2009); NP2222-GAL4 (Sugimura et al., 2003); tsh-GAL4 (Tomoyasu et al., 1998); C57-GAL4 (Packard et al., 2002); GMR49G06-GAL4 (Janelia GAL4) (Pfeiffer et al., 2008); tub-Gal80ts (McGuire, 2003); repo-LexA (Lai and Lee, 2006); UAS-CD4::spGFP1-10 and LexAOP-CD4::spGFP11 (Gordon and Scott, 2009); UAS-hSOD1 (Watson et al., 2008); UAS-fosDN and UAS-JunDN (Eresh et al., 1997); UAS-mitoTimer (Laker et al., 2014); UAS-vglut-RNAi (Vienna Drosophila RNAi Center, #v2574); UAS-dsod1-RNAi (Vienna Drosophila RNAi Center, #v31551); UAS-dsod2-RNAi (Bloomington Drosophila Stock Center, #32496); gluRIIDe01443 (Featherstone, 2005); kay1 and kay2 (Riesgo-Escovar and Hafen, 1997); jraIA109 (Hou et al., 1997); bsk2 (Sluss et al., 1996); UAS-eaat1-venus (Parinejad et al., 2016); eaat1SM2 (Stacey et al., 2010); UAS-iGluSnFR (Stork et al., 2014); and gluClαglc1 (Kane et al., 2000).
DNA cloning and genomic sequencing
The genomic DNA of third instar larvae of homozygous eaat1hypo mutants was extracted using a Gentra Puregene Tissue Kit (Qiagen). The primers were designed to cover 500–600 base pairs (bp) of the eaat1 locus. PCR-amplified products were sequenced. No mutation was found in exons of the eaat1 gene in the respective eaat1hypo chromosome. A 428-bp insertion of the long transcribed region (LTR) of the roo transposon was identified in intron 10 of the eaat1 gene. The sequence of human EAAT1-GFP was PCR-amplified from pGFAP-CITE-hEAAT2-EGFP plasmid, which was kindly provided by Dr. Chien-Liang Glenn Lin, using primers (forward primer GGGGTACCA CCATGGCATCTACGGAAGGTGCC; reverse primer TTTCTAGATTACTTGTACA GCTCGTCC). The PCR fragment was subcloned into the KpnI and XbaI sites of the pUAST vector. This construct was microinjected into early embryos according to a standard transgenesis protocol.
Immunohistochemistry and Western blotting
For α-Eaat1 immunostaining, we fixed the samples with Bouin’s fixative for 2 min. For other immunostaining, the samples were fixed with 4% paraformaldehyde for 20 min. Primary antibodies were used as follows: mouse α-Dlg (Developmental Studies Hybridoma Bank 4F3, 1:100); mouse α-Bruchpilot (Developmental Studies Hybridoma Bank nc82, 1:100); mouse α-dCSP2 (Developmental Studies Hybridoma Bank 6D6, 1:100); mouse α-Repo (Developmental Studies Hybridoma Bank 8D12, 1:100); rat α-Elav (Developmental Studies Hybridoma Bank 7E8A10, 1:400); chicken α-GFP (Abcam, 1:1000); rabbit α-RFP (Clontech, 1:200); rat α-RFP (Chromotek, 1:1000) and rabbit α-HRP conjugated with Alexa Fluor 488, Cy3 or Cy5 (Jackson ImmunoResearch Laboratories, 1:300). Secondary antibodies conjugated to Alexa Fluor 488, Alexa Fluor 555, and Alexa Fluor 647 (Invitrogen and Jackson ImmunoResearch) were used at 1:500. Images were captured with a Zeiss 780 confocal microscope and processed using LSM Zen and Image J software (National Institutes of Health). For Western blotting, we suspended ten L3 brains in 50 μl ice-cold 1xSDS sample buffer, followed by homogenization and boiling for 5 min. Five brain lysates were loaded into a 15% SDS-PAGE gel. We used rabbit α-Eaat1 (1:20,000) (Peco et al., 2016) and mouse α-tubulin (Sigma, 1:10,000) as primary antibodies. HRP-conjugated secondary antibodies (Jackson ImmunoResearch Laboratories) were used at 1:10,000.
Live imaging
Third instar larvae were dissected in zero calcium HL3 buffer (70 mM NaCl, 5 mM KCl, 10 mM MgCl2, 10 mM NaHCO3, 5 mM HEPES, 115 mM sucrose, 5 mM Trehalose, pH 7.2) at room temperature. Imaging was performed in zero calcium HL3 buffer and captured by a 60X water-immersion objective and EMCCD camera (iXon, Andor) mounted on a SliceScope Pro 6000 (Scientifica) microscope using MetaFlour software (Molecular Devices).
CM-H2DCFDA staining
Third instar larvae were dissected in zero calcium HL3 buffer. CM-H2DCFDA was detected as previously described (Nguyen et al., 2018). In brief, 1x PBS buffer containing 10 μM CM-H2DCFDA (ThermoFisher) and 2 mM Ca2+ was added to larval fillets, followed by orbital shaking for 15 min in the dark. Excess dyes were removed by several washes of zero calcium HL3 buffer. Subsequently, the samples were fixed with 60% methanol in 1 x PBS buffer for 10 min. The images were captured by Zeiss 780 confocal microscopy and analyzed using Image J.
Electrophysiology
Evoked excitatory junctional potential (EJP) was recorded as previously described (Yao et al., 2009). In brief, third instar larvae were dissected in zero calcium HL3 buffer at room temperature, followed by incubation in 0.5 mM Ca2+ HL3 solution for 5–10 min prior to recording. The mean resistance value for the recording electrode was ~40 MΩ when 3M KCl solution was used as the electrode solution. All recordings were obtained from A3 muscle 6. Resting membrane potentials of muscles were held at less than −60 mV. EJPs were amplified with an Axoclamp 900A amplifier (Axon Instruments, Foster City, CA) under bridge mode and filtered at 10 kHz. EJPs were analyzed using the pClamp 10.6 software (Axon Instruments). Averaged EJP amplitude was calculated from the amplitudes of 80 EJPs in one consecutive recording. Miniature EJP recordings were performed in HL3 solution containing 0.5 mM Ca2+ and 5 μM tetradotoxin (TTX), and analyzed using pClamp 10.6 software. Spontaneous motor central pattern generator (CPG) activity was measured as previously described (Imlach et al., 2012; McKiernan, 2013). Third instar larvae were dissected in zero calcium modified HL3 solution (70 mM NaCl, 5 mM KCl, 4 mM MgCl2, 10 mM NaHCO3, 5 mM HEPES, 5 mM Trehalose, and 115 mM sucrose, pH 7.2). Subsequently, EJPs were recorded from A3 muscle 6 in 1 mM Ca2+-containing HL3 solution for 10 min with a long sharp electrode. EJPs were analyzed using the pClamp 10.6 software. A successful burst was defined as a burst containing ≥15 consecutive EJPs with <1 s intervals between them. For H2O2 exposure, larval fillets were bathed in the HL3 solution containing 1 mM Ca2+ and 0.006% H2O2 for ~3 min after dissection, and recordings were done in the same solution for 10 min. For 4-AP treatment, we preincubated dissected larval fillets in HL3 solution containing 1 mM Ca2+ and 0.2 mM 4-AP, and recordings were conducted in new HL3 solution containing 0.2 mM 4-AP or/and 0.006% H2O2 for 10 min.
Larval locomotion
We adopted a previously described protocol for our locomotion assay (Aleman-Meza et al., 2015). In brief, third instar larvae were placed on a 6 mm Petri dish containing 1.0% agar for 10 min, during which time they were habituated and starved. One to five larvae were then transferred onto a new plate, and larval locomotion was traced for 30 s using a camera mounted on a SteREO DiscoveryV8 (Zeiss) stereomicroscope using AxioVision software (Zeiss). For data quantification, locomotion tracks were superimposed and analyzed using Image J.
Drug treatment
Embryos of wild-type controls and eaat1 mutants were placed on a grape juice plate topped with yeast paste containing 15 μg/ml AD4 (Sigma) or 2 mM 4-AP (Sigma). Hatched larvae were grown at 25°C on plates changed daily with the same concentrations of compounds throughout the larval stage.
Statistics
Paired and multiple datasets were compared by Student's t-test and one-way ANOVA, respectively. All data analyses were conducted using GraphPad Prism 8.0.
Acknowledgements
We are grateful to Hugo Bellen for sharing EMS-mutagenized fly stocks. We thank DJ van Meyel for sharing UAS-eaat1-venus flies and Eaat1 antibody. We appreciate the critical readings of Henry Sun, Ruey-Hwa Chen, Yijuang Chern, and Guang-Chao Chen. We thank Brian McCabe, Aaron Diantonio, Jimena Berni, Marc Freeman, Tzu-Yang Lin, Bloomington Stock Center, Vienna Drosophila RNAi Center, and the Developmental Studies Hybridoma Bank for reagents. We thank Tzu-Li Yen and Shiu-Hui Lin for assisting with the NMJ bouton screen; Chien-Liang Glenn Lin for providing human EAAT2-egfp cDNA; Hung-Lune Chen for assisting with DNA construction; Chiou-Yang Tang for aiding us with microinjections, and the Taiwan FlyCore for assistance. This work was supported by grants from the Ministry of Science and Technology (101–2311-B-001–015-MY3, 105–2311-B-001–076, 107–2311-B-001–003-MY3, 106-0210-01-15-02, and 107-0210-01-19-01) and Academia Sinica (AS-103-TP-B05).
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Chi-Kuang Yao, Email: ckyao@gate.sinica.edu.tw.
Patrik Verstreken, KU Leuven, Belgium.
Ronald L Calabrese, Emory University, United States.
Funding Information
This paper was supported by the following grants:
Academia Sinica AS-103-TP-B05 to Chi-Kuang Yao.
Ministry of Science and Technology, Taiwan 101-2311-B-001-015-MY3 to Chi-Kuang Yao.
Ministry of Science and Technology, Taiwan 105-2311-B-001-076 to Chi-Kuang Yao.
Ministry of Science and Technology, Taiwan 107-2311-B-001-003-MY3 to Chi-Kuang Yao.
Ministry of Science and Technology, Taiwan 106-0210-01-15-02 to Chi-Kuang Yao.
Ministry of Science and Technology, Taiwan 107-0210-01-19-01 to Chi-Kuang Yao.
Additional information
Competing interests
No competing interests declared.
Author contributions
Conceptualization, Resources, Data curation, Software, Formal analysis, Validation, Investigation, Visualization, Methodology, Project administration.
Conceptualization, Resources, Data curation, Software, Formal analysis, Supervision, Validation, Investigation, Visualization, Methodology, Project administration.
Formal analysis, Methodology.
Formal analysis, Methodology.
Formal analysis, Methodology.
Conceptualization, Resources, Data curation, Software, Formal analysis, Supervision, Funding acquisition, Validation, Investigation, Visualization, Methodology, Writing—original draft, Project administration, Writing—review and editing.
Additional files
Data availability
Source data files for all figures and figure supplements have been uploaded.
References
- Abe K, Itoyama Y, Sobue G, Tsuji S, Aoki M, Doyu M, Hamada C, Kondo K, Yoneoka T, Akimoto M, Yoshino H, on behalf of The Edaravone ALS Study Group Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2014;15:610–617. doi: 10.3109/21678421.2014.959024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accardi MV, Daniels BA, Brown PM, Fritschy JM, Tyagarajan SK, Bowie D. Mitochondrial reactive oxygen species regulate the strength of inhibitory GABA-mediated synaptic transmission. Nature Communications. 2014;5:3168. doi: 10.1038/ncomms4168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam-Vizi V. Production of reactive oxygen species in brain mitochondria: contribution by electron transport chain and non-electron transport chain sources. Antioxidants & Redox Signaling. 2005;7:1140–1149. doi: 10.1089/ars.2005.7.1140. [DOI] [PubMed] [Google Scholar]
- Aleman-Meza B, Jung SK, Zhong W. An automated system for quantitative analysis of Drosophila larval locomotion. BMC Developmental Biology. 2015;15:11. doi: 10.1186/s12861-015-0062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreassen OA, Dedeoglu A, Klivenyi P, Beal MF, Bush AI. N-acetyl-L-cysteine improves survival and preserves motor performance in an animal model of familial amyotrophic lateral sclerosis. NeuroReport. 2000;11:2491–2493. doi: 10.1097/00001756-200008030-00029. [DOI] [PubMed] [Google Scholar]
- Aoki M, Warita H, Mizuno H, Suzuki N, Yuki S, Itoyama Y. Feasibility study for functional test battery of SOD transgenic rat (H46R) and evaluation of edaravone, a free radical scavenger. Brain Research. 2011;1382:321–325. doi: 10.1016/j.brainres.2011.01.058. [DOI] [PubMed] [Google Scholar]
- Barber SC, Shaw PJ. Oxidative stress in ALS: key role in motor neuron injury and therapeutic target. Free Radical Biology and Medicine. 2010;48:629–641. doi: 10.1016/j.freeradbiomed.2009.11.018. [DOI] [PubMed] [Google Scholar]
- Barbieri E, Sestili P. Reactive oxygen species in skeletal muscle signaling. Journal of Signal Transduction. 2012;2012:1–17. doi: 10.1155/2012/982794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltrán González AN, López Pazos MI, Calvo DJ. Reactive oxygen species in the regulation of the GABA mediated inhibitory neurotransmission. Neuroscience. 2019 doi: 10.1016/j.neuroscience.2019.05.064. [DOI] [PubMed] [Google Scholar]
- Bendotti C, Tortarolo M, Suchak SK, Calvaresi N, Carvelli L, Bastone A, Rizzi M, Rattray M, Mennini T. Transgenic SOD1 G93A mice develop reduced GLT-1 in spinal cord without alterations in cerebrospinal fluid glutamate levels. Journal of Neurochemistry. 2001;79:737–746. doi: 10.1046/j.1471-4159.2001.00572.x. [DOI] [PubMed] [Google Scholar]
- Besson MT, Soustelle L, Birman S. Selective high-affinity transport of aspartate by a Drosophila homologue of the excitatory amino-acid transporters. Current Biology. 2000;10:207–210. doi: 10.1016/S0960-9822(00)00339-0. [DOI] [PubMed] [Google Scholar]
- Blesa J, Trigo-Damas I, Quiroga-Varela A, Jackson-Lewis VR. Oxidative stress and Parkinson's disease. Frontiers in Neuroanatomy. 2015;9:91. doi: 10.3389/fnana.2015.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzo F, Mirra A, Carrì MT. Oxidative stress and mitochondrial damage in the pathogenesis of ALS: new perspectives. Neuroscience Letters. 2017;636:3–8. doi: 10.1016/j.neulet.2016.04.065. [DOI] [PubMed] [Google Scholar]
- Brennan AM, Suh SW, Won SJ, Narasimhan P, Kauppinen TM, Lee H, Edling Y, Chan PH, Swanson RA. NADPH oxidase is the primary source of superoxide induced by NMDA receptor activation. Nature Neuroscience. 2009;12:857–863. doi: 10.1038/nn.2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bristol LA, Rothstein JD. Glutamate transporter gene expression in amyotrophic lateral sclerosis motor cortex. Annals of Neurology. 1996;39:676–679. doi: 10.1002/ana.410390519. [DOI] [PubMed] [Google Scholar]
- Bruijn LI, Becher MW, Lee MK, Anderson KL, Jenkins NA, Copeland NG, Sisodia SS, Rothstein JD, Borchelt DR, Price DL, Cleveland DW. ALS-linked SOD1 mutant G85R mediates damage to astrocytes and promotes rapidly progressive disease with SOD1-containing inclusions. Neuron. 1997;18:327–338. doi: 10.1016/S0896-6273(00)80272-X. [DOI] [PubMed] [Google Scholar]
- Budnik V, Zhong Y, Wu CF. Morphological plasticity of motor axons in Drosophila mutants with altered excitability. The Journal of Neuroscience. 1990;10:3754–3768. doi: 10.1523/JNEUROSCI.10-11-03754.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaert D, Birman S. Blockade of the central generator of locomotor rhythm by noncompetitive NMDA receptor antagonists in Drosophila larvae. Journal of Neurobiology. 2001;48:58–73. doi: 10.1002/neu.1042. [DOI] [PubMed] [Google Scholar]
- Chand KK, Lee KM, Lee JD, Qiu H, Willis EF, Lavidis NA, Hilliard MA, Noakes PG. Defects in Synaptic transmission at the neuromuscular junction precede motor deficits in a TDP-43Q331K transgenic mouse model of amyotrophic lateral sclerosis. The FASEB Journal. 2018;32:2676–2689. doi: 10.1096/fj.201700835R. [DOI] [PubMed] [Google Scholar]
- Cheng LE, Song W, Looger LL, Jan LY, Jan YN. The role of the TRP channel NompC in Drosophila larval and adult locomotion. Neuron. 2010;67:373–380. doi: 10.1016/j.neuron.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chenji S, Jha S, Lee D, Brown M, Seres P, Mah D, Kalra S. Investigating default mode and sensorimotor network connectivity in amyotrophic lateral sclerosis. PLOS ONE. 2016;11:e0157443. doi: 10.1371/journal.pone.0157443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chwieduk CM, Keating GM. Dalfampridine extended release: in multiple sclerosis. CNS Drugs. 2010;24:883–891. doi: 10.2165/11205910-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Clark MQ, Zarin AA, Carreira-Rosario A, Doe CQ. Neural circuits driving larval locomotion in Drosophila. Neural Development. 2018;13:6. doi: 10.1186/s13064-018-0103-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coirault C, Guellich A, Barbry T, Samuel JL, Riou B, Lecarpentier Y. Oxidative stress of myosin contributes to skeletal muscle dysfunction in rats with chronic heart failure. American Journal of Physiology-Heart and Circulatory Physiology. 2007;292:H1009–H1017. doi: 10.1152/ajpheart.00438.2006. [DOI] [PubMed] [Google Scholar]
- Collins CA, Wairkar YP, Johnson SL, DiAntonio A. Highwire restrains synaptic growth by attenuating a MAP kinase signal. Neuron. 2006;51:57–69. doi: 10.1016/j.neuron.2006.05.026. [DOI] [PubMed] [Google Scholar]
- Crow JP, Calingasan NY, Chen J, Hill JL, Beal MF. Manganese porphyrin given at symptom onset markedly extends survival of ALS mice. Annals of Neurology. 2005;58:258–265. doi: 10.1002/ana.20552. [DOI] [PubMed] [Google Scholar]
- Cudkowicz ME, Titus S, Kearney M, Yu H, Sherman A, Schoenfeld D, Hayden D, Shui A, Brooks B, Conwit R, Felsenstein D, Greenblatt DJ, Keroack M, Kissel JT, Miller R, Rosenfeld J, Rothstein JD, Simpson E, Tolkoff-Rubin N, Zinman L, Shefner JM, Ceftriaxone Study Investigators Safety and efficacy of ceftriaxone for amyotrophic lateral sclerosis: a multi-stage, randomised, double-blind, placebo-controlled trial. The Lancet Neurology. 2014;13:1083–1091. doi: 10.1016/S1474-4422(14)70222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cully DF, Paress PS, Liu KK, Schaeffer JM, Arena JP. Identification of a Drosophila Melanogaster glutamate-gated chloride channel sensitive to the antiparasitic agent avermectin. Journal of Biological Chemistry. 1996;271:20187–20191. doi: 10.1074/jbc.271.33.20187. [DOI] [PubMed] [Google Scholar]
- Dachs E, Hereu M, Piedrafita L, Casanovas A, Calderó J, Esquerda JE. Defective neuromuscular junction organization and postnatal myogenesis in mice with severe spinal muscular atrophy. Journal of Neuropathology & Experimental Neurology. 2011;70:444–461. doi: 10.1097/NEN.0b013e31821cbd8b. [DOI] [PubMed] [Google Scholar]
- Dermaut B, Norga KK, Kania A, Verstreken P, Pan H, Zhou Y, Callaerts P, Bellen HJ. Aberrant lysosomal carbohydrate storage accompanies endocytic defects and neurodegeneration in Drosophila benchwarmer. The Journal of Cell Biology. 2005;170:127–139. doi: 10.1083/jcb.200412001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty J, Logan MA, Taşdemir OE, Freeman MR. Ensheathing Glia function as phagocytes in the adult Drosophila brain. Journal of Neuroscience. 2009;29:4768–4781. doi: 10.1523/JNEUROSCI.5951-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong XX, Wang Y, Qin ZH. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacologica Sinica. 2009;30:379–387. doi: 10.1038/aps.2009.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eresh S, Riese J, Jackson DB, Bohmann D, Bienz M. A CREB-binding site as a target for decapentaplegic signalling during Drosophila endoderm induction. The EMBO Journal. 1997;16:2014–2022. doi: 10.1093/emboj/16.8.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrant M, Nusser Z. Variations on an inhibitory theme: phasic and tonic activation of GABA(A) receptors. Nature Reviews Neuroscience. 2005;6:215–229. doi: 10.1038/nrn1625. [DOI] [PubMed] [Google Scholar]
- Featherstone DE. An essential Drosophila glutamate receptor subunit that functions in both central neuropil and neuromuscular junction. Journal of Neuroscience. 2005;25:3199–3208. doi: 10.1523/JNEUROSCI.4201-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg EH, Vanhoven MK, Bendesky A, Wang G, Fetter RD, Shen K, Bargmann CI. GFP reconstitution across synaptic partners (GRASP) defines cell contacts and synapses in living nervous systems. Neuron. 2008;57:353–363. doi: 10.1016/j.neuron.2007.11.030. [DOI] [PubMed] [Google Scholar]
- Fischer LR, Culver DG, Tennant P, Davis AA, Wang M, Castellano-Sanchez A, Khan J, Polak MA, Glass JD. Amyotrophic lateral sclerosis is a distal axonopathy: evidence in mice and man. Experimental Neurology. 2004;185:232–240. doi: 10.1016/j.expneurol.2003.10.004. [DOI] [PubMed] [Google Scholar]
- Foran E, Trotti D. Glutamate transporters and the excitotoxic path to motor neuron degeneration in amyotrophic lateral sclerosis. Antioxidants & Redox Signaling. 2009;11:1587–1602. doi: 10.1089/ars.2009.2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornito A, Zalesky A, Breakspear M. The connectomics of brain disorders. Nature Reviews Neuroscience. 2015;16:159–172. doi: 10.1038/nrn3901. [DOI] [PubMed] [Google Scholar]
- Gordon MD, Scott K. Motor control in a Drosophila taste circuit. Neuron. 2009;61:373–384. doi: 10.1016/j.neuron.2008.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H, Lai L, Butchbach ME, Stockinger MP, Shan X, Bishop GA, Lin CL. Increased expression of the glial glutamate transporter EAAT2 modulates excitotoxicity and delays the onset but not the outcome of ALS in mice. Human Molecular Genetics. 2003;12:2519–2532. doi: 10.1093/hmg/ddg267. [DOI] [PubMed] [Google Scholar]
- Gurney ME, Cutting FB, Zhai P, Doble A, Taylor CP, Andrus PK, Hall ED. Benefit of vitamin E, riluzole, and gababapentin in a transgenic model of familial amyotrophic lateral sclerosis. Annals of Neurology. 1996;39:147–157. doi: 10.1002/ana.410390203. [DOI] [PubMed] [Google Scholar]
- Gutiérrez-Martín Y, Martín-Romero FJ, Iñesta-Vaquera FA, Gutiérrez-Merino C, Henao F. Modulation of sarcoplasmic reticulum ca(2+)-ATPase by chronic and acute exposure to peroxynitrite. European Journal of Biochemistry. 2004;271:2647–2657. doi: 10.1111/j.1432-1033.2004.04193.x. [DOI] [PubMed] [Google Scholar]
- Hayes KC. Fampridine-SR for multiple sclerosis and spinal cord injury. Expert Review of Neurotherapeutics. 2007;7:453–461. doi: 10.1586/14737175.7.5.453. [DOI] [PubMed] [Google Scholar]
- Held A, Major P, Sahin A, Reenan RA, Lipscombe D, Wharton KA. Circuit dysfunction in SOD1-ALS model first detected in sensory feedback prior to motor neuron degeneration is alleviated by BMP signaling. The Journal of Neuroscience. 2019;39:2347–2364. doi: 10.1523/JNEUROSCI.1771-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiesinger PR, Fayyazuddin A, Mehta SQ, Rosenmund T, Schulze KL, Zhai RG, Verstreken P, Cao Y, Zhou Y, Kunz J, Bellen HJ. The v-ATPase V0 subunit a1 is required for a late step in synaptic vesicle exocytosis in Drosophila. Cell. 2005;121:607–620. doi: 10.1016/j.cell.2005.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou XS, Goldstein ES, Perrimon N. Drosophila jun relays the jun amino-terminal kinase signal transduction pathway to the decapentaplegic signal transduction pathway in regulating epithelial cell sheet movement. Genes & Development. 1997;11:1728–1737. doi: 10.1101/gad.11.13.1728. [DOI] [PubMed] [Google Scholar]
- Howland DS, Liu J, She Y, Goad B, Maragakis NJ, Kim B, Erickson J, Kulik J, DeVito L, Psaltis G, DeGennaro LJ, Cleveland DW, Rothstein JD. Focal loss of the glutamate transporter EAAT2 in a transgenic rat model of SOD1 mutant-mediated amyotrophic lateral sclerosis (ALS) PNAS. 2002;99:1604–1609. doi: 10.1073/pnas.032539299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes CL, Thomas JB. A sensory feedback circuit coordinates muscle activity in Drosophila. Molecular and Cellular Neuroscience. 2007;35:383–396. doi: 10.1016/j.mcn.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain A, Pooryasin A, Zhang M, Loschek LF, La Fortezza M, Friedrich AB, Blais CM, Üçpunar HK, Yépez VA, Lehmann M, Gompel N, Gagneur J, Sigrist SJ, Grunwald Kadow IC. Inhibition of oxidative stress in cholinergic projection neurons fully rescues aging-associated olfactory circuit degeneration in Drosophila. eLife. 2018;7:e32018. doi: 10.7554/eLife.32018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imlach WL, Beck ES, Choi BJ, Lotti F, Pellizzoni L, McCabe BD. SMN is required for sensory-motor circuit function in Drosophila. Cell. 2012;151:427–439. doi: 10.1016/j.cell.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito H, Wate R, Zhang J, Ohnishi S, Kaneko S, Ito H, Nakano S, Kusaka H. Treatment with edaravone, initiated at symptom onset, slows motor decline and decreases SOD1 deposition in ALS mice. Experimental Neurology. 2008;213:448–455. doi: 10.1016/j.expneurol.2008.07.017. [DOI] [PubMed] [Google Scholar]
- Jackson MJ, McArdle A. Age-related changes in skeletal muscle reactive oxygen species generation and adaptive responses to reactive oxygen species. The Journal of Physiology. 2011;589:2139–2145. doi: 10.1113/jphysiol.2011.206623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob CP, Koutsilieri E, Bartl J, Neuen-Jacob E, Arzberger T, Zander N, Ravid R, Roggendorf W, Riederer P, Grünblatt E. Alterations in expression of glutamatergic transporters and receptors in sporadic alzheimer's disease. Journal of Alzheimer's Disease. 2007;11:97–116. doi: 10.3233/JAD-2007-11113. [DOI] [PubMed] [Google Scholar]
- Jafar-Nejad H, Andrews HK, Acar M, Bayat V, Wirtz-Peitz F, Mehta SQ, Knoblich JA, Bellen HJ. Sec15, a component of the exocyst, promotes notch signaling during the asymmetric division of Drosophila sensory organ precursors. Developmental Cell. 2005;9:351–363. doi: 10.1016/j.devcel.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Jaiswal M, Sandoval H, Zhang K, Bayat V, Bellen HJ. Probing mechanisms that underlie human neurodegenerative diseases in Drosophila. Annual Review of Genetics. 2012;46:371–396. doi: 10.1146/annurev-genet-110711-155456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane NS, Hirschberg B, Qian S, Hunt D, Thomas B, Brochu R, Ludmerer SW, Zheng Y, Smith M, Arena JP, Cohen CJ, Schmatz D, Warmke J, Cully DF. Drug-resistant Drosophila indicate glutamate-gated chloride channels are targets for the antiparasitics nodulisporic acid and ivermectin. PNAS. 2000;97:13949–13954. doi: 10.1073/pnas.240464697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariya S, Park GH, Maeno-Hikichi Y, Leykekhman O, Lutz C, Arkovitz MS, Landmesser LT, Monani UR. Reduced SMN protein impairs maturation of the neuromuscular junctions in mouse models of spinal muscular atrophy. Human Molecular Genetics. 2008;17:2552–2569. doi: 10.1093/hmg/ddn156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiehn O. Decoding the organization of spinal circuits that control locomotion. Nature Reviews Neuroscience. 2016;17:224–238. doi: 10.1038/nrn.2016.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EK, Choi E-J. Pathological roles of MAPK signaling pathways in human diseases. Biochimica Et Biophysica Acta (BBA) - Molecular Basis of Disease. 2010;1802:396–405. doi: 10.1016/j.bbadis.2009.12.009. [DOI] [PubMed] [Google Scholar]
- Kohsaka H, Okusawa S, Itakura Y, Fushiki A, Nose A. Development of larval motor circuits in Drosophila. Development, Growth & Differentiation. 2012;54:408–419. doi: 10.1111/j.1440-169X.2012.01347.x. [DOI] [PubMed] [Google Scholar]
- Kohsaka H, Takasu E, Morimoto T, Nose A. A group of segmental premotor interneurons regulates the speed of axial locomotion in Drosophila larvae. Current Biology. 2014;24:2632–2642. doi: 10.1016/j.cub.2014.09.026. [DOI] [PubMed] [Google Scholar]
- Kohsaka H, Guertin PA, Nose A. Neural circuits underlying fly larval locomotion. Current Pharmaceutical Design. 2017;23:1722–1733. doi: 10.2174/1381612822666161208120835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong Q, Carothers S, Chang Y, Glenn Lin CL. The importance of preclinical trial timing - a potential reason for the disconnect between mouse studies and human clinical trials in ALS. CNS Neuroscience & Therapeutics. 2012;18:791–793. doi: 10.1111/j.1755-5949.2012.00358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong Q, Chang L-C, Takahashi K, Liu Q, Schulte DA, Lai L, Ibabao B, Lin Y, Stouffer N, Mukhopadhyay CD, Xing X, Seyb KI, Cuny GD, Glicksman MA, Lin C-LG. Small-molecule activator of glutamate transporter EAAT2 translation provides neuroprotection. Journal of Clinical Investigation. 2014;124:1255–1267. doi: 10.1172/JCI66163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai SL, Lee T. Genetic mosaic with dual binary transcriptional systems in Drosophila. Nature Neuroscience. 2006;9:703–709. doi: 10.1038/nn1681. [DOI] [PubMed] [Google Scholar]
- Laker RC, Xu P, Ryall KA, Sujkowski A, Kenwood BM, Chain KH, Zhang M, Royal MA, Hoehn KL, Driscoll M, Adler PN, Wessells RJ, Saucerman JJ, Yan Z. A novel MitoTimer reporter gene for mitochondrial content, structure, stress, and damage in vivo. The Journal of Biological Chemistry. 2014;289:12005–12015. doi: 10.1074/jbc.M113.530527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SG, Su ZZ, Emdad L, Gupta P, Sarkar D, Borjabad A, Volsky DJ, Fisher PB. Mechanism of ceftriaxone induction of excitatory amino acid transporter-2 expression and glutamate uptake in primary human astrocytes. Journal of Biological Chemistry. 2008;283:13116–13123. doi: 10.1074/jbc.M707697200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepeta K, Lourenco MV, Schweitzer BC, Martino Adami PV, Banerjee P, Catuara-Solarz S, de La Fuente Revenga M, Guillem AM, Haidar M, Ijomone OM, Nadorp B, Qi L, Perera ND, Refsgaard LK, Reid KM, Sabbar M, Sahoo A, Schaefer N, Sheean RK, Suska A, Verma R, Vicidomini C, Wright D, Zhang XD, Seidenbecher C. Synaptopathies: synaptic dysfunction in neurological disorders - A review from students to students. Journal of Neurochemistry. 2016;138:785–805. doi: 10.1111/jnc.13713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewerenz J, Maher P. Chronic glutamate toxicity in neurodegenerative Diseases-What is the evidence? Frontiers in Neuroscience. 2015;9:469. doi: 10.3389/fnins.2015.00469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Mallory M, Alford M, Tanaka S, Masliah E. Glutamate transporter alterations in alzheimer disease are possibly associated with abnormal APP expression. Journal of Neuropathology and Experimental Neurology. 1997;56:901–911. doi: 10.1097/00005072-199708000-00008. [DOI] [PubMed] [Google Scholar]
- Li G, Gong J, Lei H, Liu J, Xu XZS. Promotion of behavior and neuronal function by reactive oxygen species in C. elegans. Nature Communications. 2016;7:13234. doi: 10.1038/ncomms13234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori I, Russo G, Curcio F, Bulli G, Aran L, Della-Morte D, Gargiulo G, Testa G, Cacciatore F, Bonaduce D, Abete P. Oxidative stress, aging, and diseases. Clinical interventions in aging. 2018;13:757–772. doi: 10.2147/CIA.S158513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Zhang K, Sandoval H, Yamamoto S, Jaiswal M, Sanz E, Li Z, Hui J, Graham BH, Quintana A, Bellen HJ. Glial lipid droplets and ROS induced by mitochondrial defects promote neurodegeneration. Cell. 2015;160:177–190. doi: 10.1016/j.cell.2014.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotti F, Imlach WL, Saieva L, Beck ES, Hao leT, Li DK, Jiao W, Mentis GZ, Beattie CE, McCabe BD, Pellizzoni L. An SMN-dependent U12 splicing event essential for motor circuit function. Cell. 2012;151:440–454. doi: 10.1016/j.cell.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacNamee SE, Liu KE, Gerhard S, Tran CT, Fetter RD, Cardona A, Tolbert LP, Oland LA. Astrocytic glutamate transport regulates a Drosophila CNS synapse that lacks astrocyte ensheathment. Journal of Comparative Neurology. 2016;524:1979–1998. doi: 10.1002/cne.24016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahr A, Aberle H. The expression pattern of the Drosophila vesicular glutamate transporter: a marker protein for motoneurons and glutamatergic centers in the brain. Gene Expression Patterns. 2006;6:299–309. doi: 10.1016/j.modgep.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Matthews RT, Yang L, Browne S, Baik M, Beal MF. Coenzyme Q10 administration increases brain mitochondrial concentrations and exerts neuroprotective effects. PNAS. 1998;95:8892–8897. doi: 10.1073/pnas.95.15.8892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire SE. Spatiotemporal rescue of memory dysfunction in Drosophila. Science. 2003;302:1765–1768. doi: 10.1126/science.1089035. [DOI] [PubMed] [Google Scholar]
- McGurk L, Berson A, Bonini NM. Drosophila as an in vivo model for human neurodegenerative disease. Genetics. 2015;201:377–402. doi: 10.1534/genetics.115.179457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKiernan EC. Effects of manipulating slowpoke calcium-dependent potassium channel expression on rhythmic locomotor activity in Drosophila larvae. PeerJ. 2013;1:e57. doi: 10.7717/peerj.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta A, Prabhakar M, Kumar P, Deshmukh R, Sharma PL. Excitotoxicity: bridge to various triggers in neurodegenerative disorders. European Journal of Pharmacology. 2013;698:6–18. doi: 10.1016/j.ejphar.2012.10.032. [DOI] [PubMed] [Google Scholar]
- Milton VJ, Jarrett HE, Gowers K, Chalak S, Briggs L, Robinson IM, Sweeney ST. Oxidative stress induces overgrowth of the Drosophila neuromuscular junction. PNAS. 2011;108:17521–17526. doi: 10.1073/pnas.1014511108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moylan JS, Reid MB. Oxidative stress, chronic disease, and muscle wasting. Muscle & Nerve. 2007;35:411–429. doi: 10.1002/mus.20743. [DOI] [PubMed] [Google Scholar]
- Ng M, Roorda RD, Lima SQ, Zemelman BV, Morcillo P, Miesenböck G. Transmission of olfactory information between three populations of neurons in the antennal lobe of the fly. Neuron. 2002;36:463–474. doi: 10.1016/S0896-6273(02)00975-3. [DOI] [PubMed] [Google Scholar]
- Nguyen TT, Vuu MD, Huynh MA, Yamaguchi M, Tran LT, Dang TPT. Curcumin Effectively Rescued Parkinson’s Disease-Like Phenotypes in a Novel Drosophila melanogaster Model with dUCH Knockdown. Oxidative Medicine and Cellular Longevity. 2018;2018:1–12. doi: 10.1155/2018/2038267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohyama T, Verstreken P, Ly CV, Rosenmund T, Rajan A, Tien AC, Haueter C, Schulze KL, Bellen HJ. Huntingtin-interacting protein 14, a palmitoyl transferase required for exocytosis and targeting of CSP to synaptic vesicles. The Journal of Cell Biology. 2007;179:1481–1496. doi: 10.1083/jcb.200710061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohyama T, Schneider-Mizell CM, Fetter RD, Aleman JV, Franconville R, Rivera-Alba M, Mensh BD, Branson KM, Simpson JH, Truman JW, Cardona A, Zlatic M. A multilevel multimodal circuit enhances action selection in Drosophila. Nature. 2015;520:633–639. doi: 10.1038/nature14297. [DOI] [PubMed] [Google Scholar]
- Oswald MC, Brooks PS, Zwart MF, Mukherjee A, West RJ, Giachello CN, Morarach K, Baines RA, Sweeney ST, Landgraf M. Reactive oxygen species regulate activity-dependent neuronal plasticity in Drosophila. eLife. 2018a;7:e39393. doi: 10.7554/eLife.39393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald MCW, Garnham N, Sweeney ST, Landgraf M. Regulation of neuronal development and function by ROS. FEBS Letters. 2018b;592:679–691. doi: 10.1002/1873-3468.12972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packard M, Koo ES, Gorczyca M, Sharpe J, Cumberledge S, Budnik V. The Drosophila wnt, wingless, provides an essential signal for pre- and postsynaptic differentiation. Cell. 2002;111:319–330. doi: 10.1016/S0092-8674(02)01047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palop JJ, Mucke L. Amyloid-beta-induced neuronal dysfunction in Alzheimer's disease: from synapses toward neural networks. Nature Neuroscience. 2010;13:812–818. doi: 10.1038/nn.2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parinejad N, Peco E, Ferreira T, Stacey SM, van Meyel DJ. Disruption of an EAAT-Mediated chloride channel in a Drosophila model of ataxia. Journal of Neuroscience. 2016;36:7640–7647. doi: 10.1523/JNEUROSCI.0197-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauli A, Althoff F, Oliveira RA, Heidmann S, Schuldiner O, Lehner CF, Dickson BJ, Nasmyth K. Cell-type-specific TEV protease cleavage reveals cohesin functions in Drosophila neurons. Developmental Cell. 2008;14:239–251. doi: 10.1016/j.devcel.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peco E, Davla S, Camp D, Stacey SM, Landgraf M, van Meyel DJ. Drosophila astrocytes cover specific territories of the CNS neuropil and are instructed to differentiate by Prospero, a key effector of notch. Development. 2016;143:1170–1181. doi: 10.1242/dev.133165. [DOI] [PubMed] [Google Scholar]
- Peng TI, Jou MJ. Oxidative stress caused by mitochondrial calcium overload. Annals of the New York Academy of Sciences. 2010;1201:183–188. doi: 10.1111/j.1749-6632.2010.05634.x. [DOI] [PubMed] [Google Scholar]
- Penna A, Wang DS, Yu J, Lecker I, Brown PM, Bowie D, Orser BA. Hydrogen peroxide increases GABAA receptor-mediated tonic current in hippocampal neurons. Journal of Neuroscience. 2014;34:10624–10634. doi: 10.1523/JNEUROSCI.0335-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer BD, Jenett A, Hammonds AS, Ngo TT, Misra S, Murphy C, Scully A, Carlson JW, Wan KH, Laverty TR, Mungall C, Svirskas R, Kadonaga JT, Doe CQ, Eisen MB, Celniker SE, Rubin GM. Tools for neuroanatomy and neurogenetics in Drosophila. PNAS. 2008;105:9715–9720. doi: 10.1073/pnas.0803697105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinter MJ, Waldeck RF, Cope TC, Cork LC. Effects of 4-aminopyridine on muscle and motor unit force in canine motor neuron disease. The Journal of Neuroscience. 1997;17:4500–4507. doi: 10.1523/JNEUROSCI.17-11-04500.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant DR, Lynch GS, Williams DA. Hydrogen peroxide modulates Ca2+-activation of single permeabilized fibres from fast- and slow-twitch skeletal muscles of rats. Journal of Muscle Research and Cell Motility. 2000;21:747–752. doi: 10.1023/A:1010344008224. [DOI] [PubMed] [Google Scholar]
- Pollari E, Goldsteins G, Bart G, Koistinaho J, Giniatullin R. The role of oxidative stress in degeneration of the neuromuscular junction in amyotrophic lateral sclerosis. Frontiers in Cellular Neuroscience. 2014;8:131. doi: 10.3389/fncel.2014.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers SK, Ji LL, Kavazis AN, Jackson MJ. Reactive oxygen species: impact on skeletal muscle. Comprehensive Physiology. 2011;1:941–969. doi: 10.1002/cphy.c100054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prentice H, Modi JP, Wu J-Y. Mechanisms of neuronal protection against excitotoxicity, endoplasmic reticulum stress, and mitochondrial dysfunction in stroke and neurodegenerative diseases. Oxidative Medicine and Cellular Longevity. 2015;2015:1–7. doi: 10.1155/2015/964518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quartel A, Turbeville S, Lounsbury D. Current therapy for Lambert-Eaton myasthenic syndrome: development of 3,4-diaminopyridine phosphate salt as first-line symptomatic treatment. Current Medical Research and Opinion. 2010;26:1363–1375. doi: 10.1185/03007991003745209. [DOI] [PubMed] [Google Scholar]
- Riesgo-Escovar JR, Hafen E. Common and distinct roles of DFos and DJun during Drosophila development. Science. 1997;278:669–672. doi: 10.1126/science.278.5338.669. [DOI] [PubMed] [Google Scholar]
- Rival T, Soustelle L, Cattaert D, Strambi C, Iché M, Birman S. Physiological requirement for the glutamate transporter dEAAT1 at the adult Drosophila neuromuscular junction. Journal of Neurobiology. 2006;66:1061–1074. doi: 10.1002/neu.20270. [DOI] [PubMed] [Google Scholar]
- Rocha MC, Pousinha PA, Correia AM, Sebastião AM, Ribeiro JA. Early changes of neuromuscular transmission in the SOD1(G93A) mice model of ALS start long before motor symptoms onset. PLOS ONE. 2013;8:e73846. doi: 10.1371/journal.pone.0073846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrbough J, Broadie K. Electrophysiological analysis of synaptic transmission in central neurons of Drosophila larvae. Journal of Neurophysiology. 2002;88:847–860. doi: 10.1152/jn.2002.88.2.847. [DOI] [PubMed] [Google Scholar]
- Rothstein JD, Van Kammen M, Levey AI, Martin LJ, Kuncl RW. Selective loss of glial glutamate transporter GLT-1 in amyotrophic lateral sclerosis. Annals of Neurology. 1995;38:73–84. doi: 10.1002/ana.410380114. [DOI] [PubMed] [Google Scholar]
- Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, Jin L, Dykes Hoberg M, Vidensky S, Chung DS, Toan SV, Bruijn LI, Su ZZ, Gupta P, Fisher PB. Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature. 2005;433:73–77. doi: 10.1038/nature03180. [DOI] [PubMed] [Google Scholar]
- Sahoo N, Hoshi T, Heinemann SH. Oxidative modulation of voltage-gated potassium channels. Antioxidants & Redox Signaling. 2014;21:933–952. doi: 10.1089/ars.2013.5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvaterra PM, Kitamoto T. Drosophila cholinergic neurons and processes visualized with Gal4/UAS-GFP. Gene Expression Patterns. 2001;1:73–82. doi: 10.1016/S1567-133X(01)00011-4. [DOI] [PubMed] [Google Scholar]
- Sandoval H, Yao C-K, Chen K, Jaiswal M, Donti T, Lin YQ, Bayat V, Xiong B, Zhang K, David G, Charng W-L, Yamamoto S, Duraine L, Graham BH, Bellen HJ. Mitochondrial fusion but not fission regulates larval growth and synaptic development through steroid hormone production. eLife. 2014;3:e03558. doi: 10.7554/eLife.03558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyal S, Sandstrom DJ, Hoeffer CA, Ramaswami M. AP-1 functions upstream of CREB to control synaptic plasticity in Drosophila. Nature. 2002;416:870–874. doi: 10.1038/416870a. [DOI] [PubMed] [Google Scholar]
- Sanyal S, Narayanan R, Consoulas C, Ramaswami M. Evidence for cell autonomous AP1 function in regulation of Drosophila motor-neuron plasticity. BMC Neuroscience. 2003;4:20. doi: 10.1186/1471-2202-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S, Kranz JE, Cole J, Lincecum JM, Thompson K, Kelly N, Bostrom A, Theodoss J, Al-Nakhala BM, Vieira FG, Ramasubbu J, Heywood JA. Design, power, and interpretation of studies in the standard murine model of ALS. Amyotrophic Lateral Sclerosis. 2008;9:4–15. doi: 10.1080/17482960701856300. [DOI] [PubMed] [Google Scholar]
- Sepp KJ, Schulte J, Auld VJ. Peripheral Glia direct axon guidance across the CNS/PNS transition zone. Developmental Biology. 2001;238:47–63. doi: 10.1006/dbio.2001.0411. [DOI] [PubMed] [Google Scholar]
- Sesti F, Liu S, Cai SQ. Oxidation of potassium channels by ROS: a general mechanism of aging and neurodegeneration? Trends in Cell Biology. 2010;20:45–51. doi: 10.1016/j.tcb.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Shababi M, Lorson CL, Rudnik-Schöneborn SS. Spinal muscular atrophy: a motor neuron disorder or a multi-organ disease? Journal of Anatomy. 2014;224:15–28. doi: 10.1111/joa.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A, Lyashchenko AK, Lu L, Nasrabady SE, Elmaleh M, Mendelsohn M, Nemes A, Tapia JC, Mentis GZ, Shneider NA. ALS-associated mutant FUS induces selective motor neuron degeneration through toxic gain of function. Nature Communications. 2016;7:10465. doi: 10.1038/ncomms10465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw PJ, Ince PG. Glutamate, excitotoxicity and amyotrophic lateral sclerosis. Journal of Neurology. 1997;244 Suppl 2:S3–S14. doi: 10.1007/BF03160574. [DOI] [PubMed] [Google Scholar]
- Shen W, Ganetzky B. Autophagy promotes synapse development in Drosophila. The Journal of Cell Biology. 2009;187:71–79. doi: 10.1083/jcb.200907109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sluss HK, Han Z, Barrett T, Goberdhan DC, Wilson C, Davis RJ, Ip YT. A JNK signal transduction pathway that mediates morphogenesis and an immune response in Drosophila. Genes & Development. 1996;10:2745–2758. doi: 10.1101/gad.10.21.2745. [DOI] [PubMed] [Google Scholar]
- Song W, Onishi M, Jan LY, Jan YN. Peripheral multidendritic sensory neurons are necessary for rhythmic locomotion behavior in Drosophila larvae. PNAS. 2007;104:5199–5204. doi: 10.1073/pnas.0700895104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey SM, Muraro NI, Peco E, Labbé A, Thomas GB, Baines RA, van Meyel DJ. Drosophila glial glutamate transporter Eaat1 is regulated by fringe-mediated notch signaling and is essential for larval locomotion. Journal of Neuroscience. 2010;30:14446–14457. doi: 10.1523/JNEUROSCI.1021-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stork T, Sheehan A, Tasdemir-Yilmaz OE, Freeman MR. Neuron-glia interactions through the heartless FGF receptor signaling pathway mediate morphogenesis of Drosophila astrocytes. Neuron. 2014;83:388–403. doi: 10.1016/j.neuron.2014.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugimura K, Yamamoto M, Niwa R, Satoh D, Goto S, Taniguchi M, Hayashi S, Uemura T. Distinct developmental modes and lesion-induced reactions of dendrites of two classes of Drosophila sensory neurons. The Journal of Neuroscience. 2003;23:3752–3760. doi: 10.1523/JNEUROSCI.23-09-03752.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiyama K, Aida T, Nomura M, Takayanagi R, Zeilhofer HU, Tanaka K. Calpain-Dependent degradation of nucleoporins contributes to motor neuron death in a mouse model of chronic excitotoxicity. The Journal of Neuroscience. 2017;37:8830–8844. doi: 10.1523/JNEUROSCI.0730-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiyama K, Tanaka K. Spinal cord-specific deletion of the glutamate transporter GLT1 causes motor neuron death in mice. Biochemical and Biophysical Research Communications. 2018;497:689–693. doi: 10.1016/j.bbrc.2018.02.132. [DOI] [PubMed] [Google Scholar]
- Sweeney ST, Davis GW. Unrestricted synaptic growth in spinster-a late endosomal protein implicated in TGF-beta-mediated synaptic growth regulation. Neuron. 2002;36:403–416. doi: 10.1016/S0896-6273(02)01014-0. [DOI] [PubMed] [Google Scholar]
- Taylor JP, Brown RH, Cleveland DW. Decoding ALS: from genes to mechanism. Nature. 2016;539:197–206. doi: 10.1038/nature20413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Writing Group Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. The Lancet. Neurology. 2017;16:505–512. doi: 10.1016/S1474-4422(17)30115-1. [DOI] [PubMed] [Google Scholar]
- Tomoyasu Y, Nakamura M, Ueno N. Role of dpp signalling in prepattern formation of the dorsocentral mechanosensory organ in Drosophila melanogaster. Development. 1998;125:4215–4224. doi: 10.1242/dev.125.21.4215. [DOI] [PubMed] [Google Scholar]
- Tong J, Huang C, Bi F, Wu Q, Huang B, Liu X, Li F, Zhou H, Xia XG. Expression of ALS-linked TDP-43 mutant in astrocytes causes non-cell-autonomous motor neuron death in rats. The EMBO Journal. 2013;32:1917–1926. doi: 10.1038/emboj.2013.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai PI, Wang M, Kao HH, Cheng YJ, Lin YJ, Chen RH, Chien CT. Activity-dependent retrograde laminin A signaling regulates synapse growth at Drosophila neuromuscular junctions. PNAS. 2012;109:17699–17704. doi: 10.1073/pnas.1206416109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Bosch L, Van Damme P, Bogaert E, Robberecht W. The role of excitotoxicity in the pathogenesis of amyotrophic lateral sclerosis. Biochimica Et Biophysica Acta (BBA) - Molecular Basis of Disease. 2006;1762:1068–1082. doi: 10.1016/j.bbadis.2006.05.002. [DOI] [PubMed] [Google Scholar]
- Vandenberg RJ, Ryan RM. Mechanisms of glutamate transport. Physiological Reviews. 2013;93:1621–1657. doi: 10.1152/physrev.00007.2013. [DOI] [PubMed] [Google Scholar]
- Verstreken P, Koh TW, Schulze KL, Zhai RG, Hiesinger PR, Zhou Y, Mehta SQ, Cao Y, Roos J, Bellen HJ. Synaptojanin is recruited by endophilin to promote synaptic vesicle uncoating. Neuron. 2003;40:733–748. doi: 10.1016/S0896-6273(03)00644-5. [DOI] [PubMed] [Google Scholar]
- Wang X, Wang W, Li L, Perry G, Lee H-gon, Zhu X. Oxidative stress and mitochondrial dysfunction in Alzheimer's disease. Biochimica Et Biophysica Acta (BBA) - Molecular Basis of Disease. 2014;1842:1240–1247. doi: 10.1016/j.bbadis.2013.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson MR, Lagow RD, Xu K, Zhang B, Bonini NM. A Drosophila model for amyotrophic lateral sclerosis reveals motor neuron damage by human SOD1. Journal of Biological Chemistry. 2008;283:24972–24981. doi: 10.1074/jbc.M804817200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West RJ, Lu Y, Marie B, Gao FB, Sweeney ST. Rab8, POSH, and TAK1 regulate synaptic growth in a Drosophila model of frontotemporal dementia. The Journal of Cell Biology. 2015;208:931–947. doi: 10.1083/jcb.201404066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wishart TM, Parson SH, Gillingwater TH. Synaptic vulnerability in neurodegenerative disease. Journal of Neuropathology & Experimental Neurology. 2006;65:733–739. doi: 10.1097/01.jnen.0000228202.35163.c4. [DOI] [PubMed] [Google Scholar]
- Xu KY, Zweier JL, Becker LC. Hydroxyl radical inhibits sarcoplasmic reticulum ca(2+)-ATPase function by direct attack on the ATP binding site. Circulation Research. 1997;80:76–81. doi: 10.1161/01.res.80.1.76. [DOI] [PubMed] [Google Scholar]
- Yamada T, Mishima T, Sakamoto M, Sugiyama M, Matsunaga S, Wada M. Oxidation of myosin heavy chain and reduction in force production in hyperthyroid rat soleus. Journal of Applied Physiology. 2006;100:1520–1526. doi: 10.1152/japplphysiol.01456.2005. [DOI] [PubMed] [Google Scholar]
- Yao CK, Lin YQ, Ly CV, Ohyama T, Haueter CM, Moiseenkova-Bell VY, Wensel TG, Bellen HJ. A synaptic vesicle-associated Ca2+ channel promotes endocytosis and couples exocytosis to endocytosis. Cell. 2009;138:947–960. doi: 10.1016/j.cell.2009.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh E, Gustafson K, Boulianne GL. Green fluorescent protein as a vital marker and reporter of gene expression in Drosophila. PNAS. 1995;92:7036–7040. doi: 10.1073/pnas.92.15.7036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeeshan HM, Lee GH, Kim HR, Chae HJ. Endoplasmic reticulum stress and associated ROS. International Journal of Molecular Sciences. 2016;17:327. doi: 10.3390/ijms17030327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Wang X, Vikash V, Ye Q, Wu D, Liu Y, Dong W. ROS and ROS-Mediated cellular signaling. Oxidative Medicine and Cellular Longevity. 2016;2016:1–18. doi: 10.1155/2016/4350965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Zhao B. Oxidative stress and the pathogenesis of alzheimer's disease. Oxidative Medicine and Cellular Longevity. 2013;2013:1–10. doi: 10.1155/2013/316523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zima AV, Blatter LA. Redox regulation of cardiac calcium channels and transporters. Cardiovascular Research. 2006;71:310–321. doi: 10.1016/j.cardiores.2006.02.019. [DOI] [PubMed] [Google Scholar]