Abstract
Purpose:
Few population-level surveys have explored patient-centered priorities for improving colorectal cancer survivors’ care. Working with patients, we designed a survey to identify care improvement and survivorship priorities.
Methods:
We surveyed a random sample of 4,000 patients from a retrospective, population-based cohort of colorectal cancer survivors diagnosed during 2010–2014. The survey included two multiple response questions: “What would you have changed about your cancer diagnosis and treatment experience?” and “What are your biggest health or lifestyle concerns (other than having cancer) since being diagnosed?” Multivariable regression identified characteristics associated with endorsement of health care experience and survivorship concerns.
Results:
Survey response rate was 50.2% (2,000/3,986). 53% reported at least one unmet need, most commonly for more information about life after treatment (26.7%). Survivors of rectal cancer reported more needs than respondents with colon cancer; persons of color reported more needs than non-Hispanic whites; individuals without high school diplomas reported more needs than individuals with more education. Fear of recurrence was the most common health/lifestyle concern (58.9%). Respondents under age 65 reported nearly all health/lifestyle concerns more often than respondents over age 74. Rectal cancer survivors reported more concerns about activity limitation, changes and body function and appearance than colon cancer survivors. Persons of color were more likely to report financial concerns than non-Hispanic whites.
Conclusions:
The greatest needs for intervention are among survivors of rectal cancer, survivors of minority racial/ethnic background, and survivors of younger age. Survivors with low educational attainment, and those with higher stage disease could also benefit.
Keywords: Colorectal cancer, cancer survivors, health disparities, care improvement, survey
Introduction
Few population-level surveys in the United States have elicited patient-reported experiences of care[1]. Cancer survivors report considerable unmet informational needs relating to health and health care, pointing to the need for interventions to empower patients to be well-informed during cancer treatment and survivorship[2]. A 2008 study of survivors of many cancer types, surveyed 2–5 years after diagnosis, found prevalent unmet information needs relating to tests and treatments, health promotion, side effects and symptoms, personal relationships, and emotional issues. Younger age, non-White race/ethnicity, a greater number of health problems, and reported problems with the quality of cancer care were associated with more unmet informational needs[3]. A follow-up study found that informational needs among cancer patients persist years after cancer diagnosis, with concerning disparities among minorities and patients diagnosed at a younger age[4].
A national survey of US cancer survivors found that 19% of colorectal cancer (CRC) survivors reported unmet needs relating to education and information and 17% reported unmet needs relating to systems of care[5]. In a UK survey of CRC survivors, negative experiences of care most often related to lack of post-treatment care and insufficient information concerning self-management (11% and 8% of negative experiences, respectively)[6].
Previous surveys have been limited by sparse information about respondents’ cancer site, stage at diagnosis, and other characteristics that would help identify groups who would most benefit from interventions. The purpose of this study was to identify health care improvement and survivorship priorities among a large, diverse and well-characterized cohort of CRC survivors in the US and to identify subgroups who could benefit most from intervention.
Materials & Methods
Study setting and population
The study population was derived from the Patient Outcomes Research to Advance Learning (PORTAL) Network, funded by the Patient Centered Outcomes Research Institute. PORTAL includes 6 health systems and 9 research centers affiliated with those systems. Together, PORTAL health systems provide care for approximately 13 million members, or 1 of every 25 people in the United States[7,8]. This study was approved by the Institutional Review Board (IRB) of Kaiser Permanente Colorado (KPCO). After review and approval, all other participating health plans ceded oversight to the KPCO IRB.
A retrospective cohort of CRC survivors was developed from the population and included all cases diagnosed between 1/1/2010 and 12/31/2014 at one of 6 health care systems: Group Health Cooperative in Seattle, WA (now Kaiser Permanente Washington); HealthPartners in Minneapolis, MN; and Kaiser Permanente (KP) health plans in Colorado, Southern California, Northern California, and Oregon/southwest Washington. A random sample of 4,000 people from the cohort were invited to complete a survey, administered by multiple modalities including paper, online, and interactive voice response. Details of the cohort and sampling frame are provided elsewhere[9].
Patient engagement
Survey administration modalities, questions, and response categories were developed in partnership with patient advisors, and a representative from PORTAL’s CRC nonprofit advocacy partner, Fight Colorectal Cancer (fightcolorectalcancer.org). Patient partners reviewed preliminary results, participated in the interpretation of survey results, and have co-authored this manuscript (AD, RH, FK, CA).
Measures
Administrative data:
Tumor, clinical, and demographic characteristics were drawn from the Health Care Systems Research Network’s Virtual Data Warehouse (VDW), which includes standardized variables derived from electronic health records and administrative databases at each participating health care system[10–13]. We used tumor registry tables to define CRC (ICD-O-3 codes: C180, C182-C189, C199, C209) and to obtain information about cancer stage at diagnosis, and first course of cancer treatment (surgery, chemotherapy, radiotherapy). Vital status, birthdate, race/ethnicity, gender, and language preference (English or Spanish) were extracted from other tables in the VDW.
Patient-reported data:
The 17-item survey included 2 questions about unmet needs and priorities. The first asked about health care experience: “If you could, what would you have changed about your cancer diagnosis and treatment experience?” Respondents were instructed to select all categories that applied to them, from a list including: better information or understanding about 1) treatment options; 2) treatment side effects; 3) recovery time; 4) life after treatment; or 5) would not have changed anything. Participants could also select “other” and were given space to include a comment. The second question asked: “What are your biggest health or lifestyle concerns (other than having cancer) since being diagnosed?” Respondents were instructed to select all categories that applied to them, from a list including: 1) limitations on activity; 2) inability to sleep/lack of sleep; 3) changes to weight; changes to diet; 4) changes to my body functions, such as in frequency of bowel movements; 5) changes from surgery that I can see, such as a colostomy, scars, etc.; 6) financial issues; and 7) possibility of cancer recurrence. This question also offered an “other” category, followed by a space for comments. Patients were asked to report their highest education level.
Analysis
We analyzed the relationship between endorsement (yes/no) of each unmet health care need or health/lifestyle concern and 6 demographic and clinical characteristics (age, gender, race/ethnicity, education, cancer site, cancer stage). We explored subgroup differences in satisfaction with cancer care experiences further by using a series of multivariable logistic regression models, with each cancer care experience as the outcome and the participant characteristics as predictors. To quantify the extent of unmet needs relating to health care experience, we created a count variable by summing the number of concerns reported (range: 0–4) and conducted linear regression analysis to identify demographic and clinical predictors of that variable. All models were adjusted for health plan, although we did not consider health plan as a predictor. Because very few responses included open-ended comments, we did not include these in the current analysis.
Results
The response rate was 50.2% (2,000/3,986). We excluded 53 respondents who either denied a prior diagnosis of CRC (n=33) or because their tumor site (as coded by tumor registries) was not in the colon, rectosigmoid junction, or rectum (n=20). The average age of participants was 68.6 years (range = 17.0 to 99.2 years), 51.1% were male, 69.1% were non-Hispanic white, and 69.1% had at least some college education (Table 1). Colon cancer survivors were older than rectosigmoid or rectal cancer survivors (p<0.001). Rectal cancer survivors were more likely male than female (p<0.001). Respondents with colon, rectosigmoid, and rectal cancer did not differ by stage at diagnosis, and most respondents (84.5%) were diagnosed with cancer at stages 1–3.
Table 1.
Characteristics of survey respondents, by cancer site
| Characteristics | Cancer Site | p-value | |||
|---|---|---|---|---|---|
| Overall (N=1947) |
Colon (N=1418) |
Rectosigmoid (N=101) |
Rectal (N=428) |
||
| Demographic characteristics | |||||
| Age at survey, in years | |||||
| <50 | 124 (6.4%) | 79 (5.6%) | 4 (4.0%) | 41 (9.6%) | <0.001 |
| 50–64 | 589 (30.3%) | 370 (26.1%) | 45 (45.6%) | 174 (40.7%) | |
| 65–74 | 611 (31.4%) | 437 (30.8%) | 31 (30.7%) | 143 (33.4%) | |
| ≥75 | 623 (32.0%) | 532 (37.5%) | 21 (20.8%) | 70 (16.4%) | |
| Male | 995 (51.1%) | 689 (48.6%) | 44 (43.6%) | 262 (61.2%) | <0.001 |
| Race/Ethnicity | |||||
| Hispanic (any race) | 267 (13.7%) | 179 (12.6%) | 17 (16.8%) | 71 (16.6%) | 0.07 |
| White (non-Hispanic) | 1345 (69.1%) | 984 (69.4%) | 69 (68.3%) | 292 (68.2%) | |
| Black (non-Hispanic) | 149 (7.7%) | 122 (8.6%) | 3 (3.0%) | 24 (5.6%) | |
| Asian (non-Hispanic) | 170 (8.7%) | 122 (8.6%) | 8 (7.9%) | 40 (9.4%) | |
| Multiple / Other / Unknown | 16 (0.8%) | 11 (0.78%) | 4 (4.0%) | 1 (0.23%) | |
| Highest level of education | |||||
| Some high school | 170 (8.7%) | 119 (8.4%) | 14 (13.9%) | 37 (8.6%) | 0.34 |
| High school graduate or GED | 345 (17.7%) | 255 (18.0%) | 19 (18.8%) | 71 (16.6%) | |
| Some college or 2-year degree | 657 (33.7%) | 469 (33.1%) | 34 (33.7%) | 154 (36.0%) | |
| College graduate | 305 (15.7%) | 232 (16.4%) | 8 (7.9%) | 65 (15.2%) | |
| More than a college degree | 384 (19.7%) | 281 (19.8%) | 19 (18.8%) | 84 (19.6%) | |
| Clinical characteristics | |||||
| Years since diagnosis, mean (SD) | 3.3 (1.11) | 3.3 (1.1) | 3.3 (1.1) | 3.3 (1.1) | 0.96 |
| Years since surgery, mean (SD) | 3.2 (1.12) | 3.3 (1.1) | 3.2 (1.1) | 3.2 (1.2) | 0.51 |
| Stage at diagnosis | |||||
| 0 | 194 (10.0%) | 130 (9.2%) | 9 (8.9%) | 55 (12.9%) | 0.13 |
| 1 | 631 (32.4%) | 456 (32.2%) | 37 (36.6%) | 138 (32.2%) | |
| 2 | 509 (26.1%) | 397 (28.0%) | 20 (19.8%) | 92 (21.5%) | |
| 3 | 506 (26.0%) | 357 (25.2%) | 28 (27.7%) | 121 (28.3%) | |
| 4 | 86 (4.4%) | 64 (4.5%) | 6 (5.9%) | 16 (3.7%) | |
| Unknown | 21 (1.1%) | 14 (1%) | 1 (1%) | 6 (1.4%) | |
| Received chemotherapy (%) | 716 (36.8%) | 430 (30.3%) | 44 (43.6%) | 242 (56.5%) | <0.001 |
| Received radiotherapy (%) | 151 (7.8%) | 4 (.28%) | 13 (12.9%) | 134 (31.3%) | <0.001 |
Opportunities for improving the cancer care experience
More than half (53%) of respondents were dissatisfied with at least one aspect of their cancer care, with 26.7% noting they would have liked to receive better information or understanding about life after treatment, 23.7% noting a lack of information about treatment side effects, 19.6% noting lack of information about recovery time, and 18.4% noting lack of information about treatment options. To better understand the prevalence of these concerns, Table 2 presents the unadjusted percentages of individuals endorsing each unmet need. Table 3 shows the results of the logistic regression analysis. All models were significant with Wald χ2 (DF=20, N=1825) ranging from 56.4 to 94.1 (all p < 0.001).
Table 2:
Number and proportion of reported unmet needs relating to cancer care experience (n=1947)
| Treatment options | Side effects | Recovery time | Life after treatment | |
|---|---|---|---|---|
| Age at survey, in years | ||||
| <50 | 26 (20.0%) | 36 (29.0%) | 23 (18.6%) | 40 (32.3%) |
| 50–64 | 128 (21.7%) | 168 (28.5%) | 148 (25.1%) | 203 (34.5%) |
| 65–74 | 111 (18.2%) | 144 (23.6%) | 114 (18.7%) | 153 (25.0%) |
| ≥75 | 94 (15.1%) | 113 (18.1%) | 97 (15.6%) | 124 (19.9%) |
| Gender | ||||
| Female | 171 (18.0%) | 227 (23.8%) | 189 (19.9%) | 261 (27.4%) |
| Male | 188 (18.9%) | 234 (23.5%) | 193 (19.4%) | 259 (26.0%) |
| Race/Ethnicity | ||||
| White, non-Hispanic | 252 (15.7%) | 364 (22.7%) | 288 (17.9%) | 401 (24.9%) |
| Other | 105 (32.2%) | 95 (29.1%) | 89 (27.3%) | 112 (34.3%) |
| Education | ||||
| Some high school | 52 (30.6%) | 58 (34.1%) | 41 (24.1%) | 51 (30.0%) |
| High school graduate | 52 (15.1%) | 68 (19.7%) | 56 (16.2%) | 81 (23.5%) |
| Some college | 123 (18.7%) | 151 (23.0%) | 136 (20.7%) | 190 (28.9%) |
| College graduate | 61 (20.0%) | 84 (27.5%) | 62 (20.3%) | 78 (25.6%) |
| Graduate school | 59 (15.4%) | 89 (23.2%) | 76 (19.8%) | 106 (27.6%) |
| Cancer site | ||||
| Colon | 242 (17.1%) | 295 (20.8%) | 258 (18.2%) | 338 (23.8%) |
| Rectosigmoid | 19 (18.8%) | 22.8 (23%) | 15 (14.9%) | 23 (22.8%) |
| Rectum | 98 (22.9%) | 143 (33.4%) | 109 (25.5%) | 159 (37.2%) |
| Stage at diagnosis | ||||
| 0 | 37 (19.1%) | 40 (20.6%) | 30 (15.5%) | 40 (20.6%) |
| 1 | 96 (15.2%) | 117 (18.5%) | 121 (19.2%) | 147 (23.3%) |
| 2 | 85 (16.7%) | 114 (22.4%) | 99 (19.5%) | 140 (27.5%) |
| 3 | 112 (22.1%) | 152 (30.0%) | 104 (20.6%) | 160 (31.6%) |
| 4 | 24 (27.9%) | 29 (33.7%) | 24 (27.9%) | 26 (30.2%) |
Table 3.
Multivariable logistic regression models predicting unmet needs relating to cancer care experience
| Characteristic | Odds ratio (95% confidence interval) and p value | ||||
|---|---|---|---|---|---|
| Better information or understanding about treatment options | Better information or understanding about treatment side effects | Better information or understanding about recovery time | Better information or understanding about life after treatment | ||
| Age | |||||
| <50 | 1.17, (0.68, 2.01) p=0.58 | 1.44 (0.89, 2.33) p=0.14 | 1.09 (0.64, 1.89) p=0.75 | 1.63 (1.03, 2.60) p=0.04 | |
| 50–64 | 1.41 (1.02, 1.95) p=0.04 | 1.64 (1.22, 2.21) p=0.001 | 1.82 (1.33, 2.48) p<0.001 | 2.03 (1.53, 2.69) p<0.001 | |
| 65–74 | 1.17 (0.84, 1.62) p=0.35 | 1.37 (1.02, 1.84) p=0.04 | 1.19 (0.87, 1.63) p=0.29 | 1.26 (0.95, 1.68) p=0.11 | |
| ≥75 | - ref - | - ref - | - ref - | - ref - | |
| Gender | |||||
| Female | 0.90 (0.71, 1.16) p=0.42 | 1.05 (0.84, 1.32) p=0.67 | 1.01 (0.80, 1.28) p=0.94 | 1.07 (0.86, 1.33) p=0.55 | |
| Male | - ref - | - ref - | - ref - | - ref - | |
| Race/Ethnicity | |||||
| Minority race/ethnicity | 2.66 (1.99, 3.55) p<0.001 | 1.44 (1.09, 1.92) p=0.01 | 1.79 (1.34, 2.39) p<0.001 | 1.63 (1.24, 2.15) p<0.001 | |
| White and/or Non-Hispanic | - ref - | - ref - | - ref - | - ref - | |
| Education | |||||
| Some high school but did not graduate | - ref - | - ref - | - ref - | - ref - | |
| High school graduate or GED | 0.38 (0.24, 0.61) p<0.001 | 0.46 (0.30, 0.71) p<0.001 | 0.61 (0.39, 0.98) p=0.039 | 0.71 (0.46, 1.08) p=0.11 | |
| Some college or 2 year degree | 0.48 (0.33, 0.72) p<0.001 | 0.55 (0.38, 0.81) p<0.001 | 0.75 (0.50, 1.13) p=0.17 | 0.87 (0.59, 1.28) p=0.49 | |
| College graduate | 0.46 (0.30, 0.73) p<0.001 | 0.67 (0.44, 1.02) p=0.06 | 0.70 (0.44, 1.11) p=0.13 | 0.70 (0.45, 1.08) p=0.11 | |
| More than a college degree | 0.38 (0.24, 0.59) p<0.001 | 0.55 (0.37, 0.84) p=0.005 | 0.72 (0.46, 1.13) p=0.16 | 0.82 (0.54, 1.24) p=0.35 | |
| Cancer site | |||||
| Rectosigmoid | 1.18 (0.67, 2.06) p=0.57 | 1.13 (0.67, 1.88) p=0.65 | 0.72 (0.40, 1.32) p=0.29 | 0.80 (0.47, 1.36) p=0.41 | |
| Rectal | 1.43 (1.07, 1.91) p=0.02 | 1.85 (1.43, 2.40) p<0.001 | 1.46 (1.11, 1.92) p=0.007 | 1.83 (1.43, 2.35) p<0.001 | |
| Colon | - ref - | - ref - | - ref - | - ref - | |
| Stage at diagnosis | |||||
| 0 | 1.43 (.92, 2.22) p=0.11 | 1.24 (0.82, 1.88) p=0.32 | 0.8 (0.51, 1.26) p=0.33 | 0.89 (0.59, 1.34) p=0.56 | |
| 1 | - ref - | - ref - | - ref - | - ref - | |
| 2 | 1.23 (0.88, 1.72) p=0.23 | 1.41 (1.04, 1.91) p=0.03 | 1.12 (0.82, 1.52) p=0.47 | 1.39 (1.05, 1.85) p=0.02 | |
| 3 | 1.59 (1.16, 2.20) p=0.004 | 1.9 (1.42, 2.54) p<0.001 | 1.08 (0.80, 1.47) p=0.61 | 1.5 (1.14, 1.99) p=0.004 | |
| 4 | 2.07 (1.18, 3.65) p=0.01 | 2.17 (1.29, 3.65) p=0.004 | 1.43 (0.82, 2.48) p=0.21 | 1.22 (0.71, 2.09) p=0.47 | |
Note: All models are adjusted for health plan
Age was associated with more need for information about treatment side effects (Wald χ2 10.94, p=0.01), recovery time (Wald χ2 16.84, p<0.001) and life after treatment (Wald χ2 26.4, p<0.001). Compared to survivors ≥75, those aged 50–64 were significantly more likely to report these needs (OR 1.64, 95% CI: 1.22, 2.21 for side effects; OR 1.82, 95% CI 1.33, 2.48 for recovery time; OR 2.03, 95% CI: 1.53, 2.69 for life after treatment). Gender was not a significant predictor in any of the models.
Respondents from minority race/ethnic groups were more likely than white and/or non-Hispanic respondents to report the need for more information or understanding about all aspects of care (OR 2.66, 95% CI: 2.00, 3.55 for treatment options; OR 1.44, 95% CI: 1.09, 1.92 for side effects; OR 1.79, 95% CI: 1.34, 2.39 for recovery time; and OR 1.63, 95% CI 1.24, 2.15 for life after treatment). Education level was a significant predictor of the need for information and understanding about treatment options (Wald χ2 22.4, p<0.001) and side effects (Wald χ2 14.6, p=0.006), and most of this difference was driven by the high level of need in our reference group, which included respondents with “some high school,” the lowest level of education (see Table 2).
Cancer site was a significant predictor of all of the unmet informational needs (treatment options Wald χ2 6.0, p=0.05; side effects Wald χ2 22.2, p<0.001; recovery time Wald χ2 9.3, p=0.01 and life after treatment Wald χ2 24.8, p<0.001). Compared to colon cancer survivors, survivors of rectal tumors were 1.43 to 1.85 times more likely to report unmet informational needs relating to all aspects of the cancer care experience. There was not a difference between survivors of colon and rectosigmoid cancer in the odds of endorsing unmet needs.
The odds of survivors reporting each type of unmet need generally increased by stage at diagnosis and the variable was a significant predictor of three of the four outcomes (treatment options Wald χ2 11.6, p=0.02; side effects Wald χ2 22.1, p<0.001; and life after treatment Wald χ2 12.7, p=0.01). Compared to survivors diagnosed at stage 1, survivors diagnosed at stage 3 were 1.5 to 1.9 times more likely to report these unmet needs. Survivors diagnosed at stage 4 were twice as likely to report unmet needs for better understanding of treatment options and side effects, compared to survivors diagnosed at stage 1. Survivors diagnosed at stage 4 did not differ from those diagnosed at stage 1 regarding information on life after treatment.
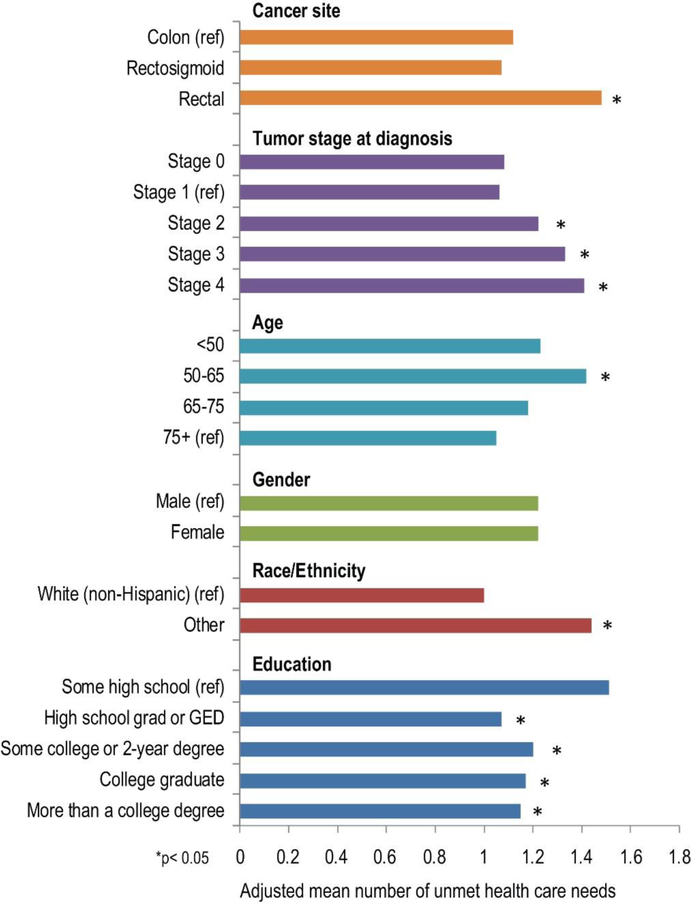
Figure 1 shows the adjusted mean number of unmet needs by patient characteristics. The overall model was significant and accounted for 6.8% of the variance (F=6.6, p<0.001). Five of the independent variables contributed significantly to the prediction of number of unmet information needs. After accounting for the variance explained by the other variables, respondents ages 50–65 reported significantly more unmet needs than those ≥75 (t=4.74, p<0.001). Participants who were Hispanic and/or from racial groups other than white reported more unmet needs than non-Hispanic whites (t=5.52, p<0.001); and individuals who had not graduated high school reported a greater number of unmet needs than individuals with more education (all t scores <−2.83, all p<0.005). Respondents diagnosed with stage 2 (t=2.13, p=0.033), 3 (t=3.54, p<0.001), and 4 (t=2.34, p=0.019) cancer all had more needs than respondents diagnosed at stage 1. Respondents who were survivors of rectal cancer reported more unmet needs than respondents with colon cancer (t=4.97, p<0.001).
Figure 1.
Adjusted mean number of unmet health care needs by demographic and clinical characteristics (N=1,825)
Health and lifestyle concerns during survivorship
The most common health and lifestyle concerns were fear of recurrence (58.9%) and changes in body or bowel function (40.9%). Other concerns were much less frequently endorsed (activity limitations, 26.8%; weight changes, 24.0%; sleep problems, 21.3%; visible changes from surgery, 16.6%; financial issues, 13.6%). Table 4 shows the unadjusted percentages of respondents who endorsed each health and lifestyle concern by subgroup.
Table 4:
Number and proportion of reported health and lifestyle concerns (other than having cancer) (n=1947)
| Activity limitation | Sleep | Weight changes | Diet changes | Changes to body function | Visible changes from surgery | Financial issues | Cancer recurrence | |
|---|---|---|---|---|---|---|---|---|
| Age at survey | ||||||||
| <50 | 40 (32%) | 30 (24%) | 47 (38%) | 44 (36%) | 49 (40%) | 34 (27%) | 30 (24%) | 85 (69%) |
| 50–64 | 164 (28%) | 147 (25%) | 141 (24%) | 148 (25%) | 281 (48%) | 119 (20%) | 114 (19%) | 392 (66%) |
| 65–74 | 155 (25%) | 114 (19%) | 136 (23%) | 108 (18%) | 241 (39%) | 100 (16%) | 77 (13%) | 349 (57%) |
| ≥75 | 162 (26%) | 123 (20%) | 144 (23%) | 102 (16%) | 226 (36%) | 70 (11%) | 44 (7%) | 320 (51%) |
| Gender | ||||||||
| Female | 254 (27%) | 219 (23%) | 268 (28%) | 205 (22%) | 376 (40%) | 162 (17%) | 137 (14%) | 562 (59%) |
| Male | 267 (27%) | 195 (20%) | 200 (20%) | 197 (20%) | 421 (42%) | 161 (16%) | 128 (13%) | 584 (59%) |
| Race/Ethnicity | ||||||||
| Non-Hispanic White | 427 (27%) | 332 (21%) | 377 (24%) | 316 (20%) | 659 (41%) | 258 (16%) | 198 (12%) | 956 (60%) |
| Other | 91 (28%) | 79 (24%) | 88 (27%) | 84 (26%) | 132 (41%) | 65 (20%) | 65 (20%) | 181 (55%) |
| Education | ||||||||
| Some high school | 58 (34%) | 38 (22%) | 40 (23%) | 44 (26%) | 52 (31%) | 36 (21%) | 27 (16%) | 97 (57%) |
| High school graduate | 87 (25%) | 70 (20%) | 91 (26%) | 69 (20%) | 142 (41%) | 67 (19%) | 50 (14%) | 200 (58%) |
| Some college | 185 (28%) | 169 (26%) | 177 (27%) | 147 (22%) | 292 (44%) | 121 (18%) | 108 (16%) | 431 (66%) |
| College graduate | 87 (28%) | 68 (23%) | 73 (24%) | 61 (20%) | 139 (46%) | 47 (15%) | 30 (10%) | 180 (60%) |
| Graduate school | 98 (25%) | 60 (15%) | 75 (19%) | 75 (19%) | 159 (41%) | 48 (12%) | 44 (11%) | 217 (56%) |
| Cancer site | ||||||||
| Colon | 342 (24%) | 308 (22%) | 347 (24%) | 274 (19%) | 505 (36%) | 182 (13%) | 180 (13%) | 842 (59%) |
| Rectosigmoid | 21 (21%) | 13 (13%) | 16 (16%) | 22 (22%) | 53 (52%) | 14 (14%) | 17 (17%) | 56 (55%) |
| Rectum | 158 (37%) | 93 (22%) | 105 (24%) | 106 (25%) | 239 (56%) | 127 (30%) | 68 (16%) | 248 (58%) |
| Stage at diagnosis | ||||||||
| 0 | 35 (18%) | 34 (17%) | 43 (22%) | 28 (14%) | 53 (27%) | 19 (10%) | 18 (9%) | 107 (55%) |
| 1 | 140 (22%) | 118 (19%) | 141 (22%) | 123 (19%) | 260 (41%) | 93 (15%) | 75 (12%) | 360 (57%) |
| 2 | 136 (27%) | 111 (22%) | 128 (25%) | 109 (21%) | 237 (47%) | 100 (20%) | 55 (11%) | 288 (57%) |
| 3 | 165 (32%) | 114 (22%) | 128 (25%) | 116 (23%) | 207 (41%) | 85 (17%) | 86 (17%) | 329 (65%) |
| 4 | 39 (45%) | 32 (37%) | 24 (28%) | 20 (23%) | 32 (37%) | 21 (24%) | 28 (33%) | 52 (60%) |
We also examined the characteristics associated with each health and lifestyle concern using multivariable logistic regression (Table 5). All models were significant with Wald χ2 (DF=20, N=1825) ranging from 46.3 to 113.4 (all p < 0.001). Age was a significant predictor of all these concerns except limitations on activity (Wald χ2 ranging from 46.3 to 113.4 (all p < 0.001). Compared to survivors ages 75 and older, younger survivors (age <65 years) were more than twice as likely to report concerns about recurrence (OR=2.42, 95% CI: 1.53–3.83 for age < 50 and OR=2.19, 95% CI: 1.70–2.84 for ages 50–64). They were also more than three times as likely to report concerns about financial issues (OR=4.36, 95% CI: 2.51–7.57 for age < 50 and OR=3.13, 95% CI: 2.11–4.65 for ages 50–64). Compared to survivors ages 75 and above, the youngest survivors (under age 50) were more than twice as likely to report concerns about changes in their weight (OR=2.40, 95% CI 1.55–3.73) and diet (OR=2.95, 95% CI=1.86–4.66). We found no association with gender, with the exception of women having more concern with changes in weight than men (OR=1.53, 95% CI: 1.22–1.90). Survivors who were Hispanic and/or from a racial group other than white had nearly double the financial concerns of non-Hispanic whites (OR=1.85, 95% CI: 1.33–2.58).
Table 5.
Multivariable logistic regression models predicting endorsement of health and lifestyle concerns
| Characteristic | Odds ratio (95% confidence interval) and p value | |||||||
|---|---|---|---|---|---|---|---|---|
| Limitations on activity | Inability to sleep or lack of sleep | Changes to weight | Changes to diet | Changes to my body functions | Changes from surgery that I can see | Financial issues | Possibility of cancer recurrence | |
| Age | ||||||||
| <50 | 1.04 (0.66, 1.63) p=0.88 |
1.35 (0.83, 2.20) p=0.23 | 2.40 (1.55, 3.73) p<0.001 | 2.95 (1.86, 4.66) p<0.001 | 1.06 (0.69, 1.64) p=0.78 | 3.12 (1.88, 5.18) p<0.001 | 4.36 (2.51, 7.57) p<0.001 | 2.42 (1.53, 3.83) p=0.001 |
| 50–64 | 0.97 (0.74, 1.28) p=0.83 |
1.43 (1.07, 1.92) p=0.02 | 1.10 (0.83, 1.47) p=0.51 | 1.76 (1.30, 2.38) p<0.001 | 1.54 (1.20, 1.99) p<0.001 | 1.87 (1.32, 2.65) p<0.001 | 3.13 (2.11, 4.65) p<0.001 | 2.19 (1.70, 2.84) p<0.001 |
| 65–74 | 0.91 (0.69, 1.20) p=0.50 |
0.97 (0.72, 1.30) p=0.82 | 1.00 (0.76, 1.33) p=0.97 | 1.08 (0.79, 1.48) p=0.62 | 1.08 (0.84, 1.39) p=0.53 | 1.50 (1.06, 2.13) p=0.02 | 1.84 (1.22, 2.77) p=0.004 | 1.31 (1.03, 1.67) p=0.03 |
| ≥ 75 | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| Gender | ||||||||
| Female | 1.00 (0.81, 1.23) p=0.98 |
1.18 (0.94, 1.49) p=0.15 | 1.53 (1.22, 1.90) p<0.001 | 1.09 (0.86, 1.37) p=0.48 | 0.90 (0.74, 1.09) p=0.29 | 1.13 (0.87, 1.46) p=0.36 | 1.04 (0.79, 1.38) p=0.77 | 0.93 (0.76, 1.13) p=0.45 |
| Male | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| Race/Ethnicity | ||||||||
| Minority race/ethnicity | 1.13 (0.85, 1.50) P=0.40 |
1.21 (0.90, 1.62) p=0.22 | 1.14 (0.86, 1.52) p=0.37 | 1.42 (1.06, 1.91) p=0.02 | 1.01 (0.78, 1.31) p=0.95 | 1.36 (0.98, 1.88) p=0.07 | 1.85 (1.33, 2.58) p<0.001 | 0.78 (0.60, 1.01) p=0.06 |
| White and/or Non-Hispanic | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| Education | ||||||||
| Some high school | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| High school graduate or GED | 0.65 (0.43, 0.99) p=0.04 | 0.87 (0.55, 1.37) p=0.55 | 1.13 (0.73, 1.75) p=0.59 | 0.79 (0.51, 1.24) p=0.31 | 1.78 (1.18, 2.68) p=0.006 | 0.90 (0.56, 1.45) p=0.65 | 0.90 (0.53, 1.54) p=0.71 | 1.07 (0.73, 1.58) p=0.72 |
| Some college or 2 year degree | 0.74 (0.51, 1.07) p=0.11 | 1.14 (0.76, 1.72) p=0.54 | 1.15 (0.76, 1.71) p=0.51 | 0.82 (0.55, 1.22) p=0.32 | 1.89 (1.30, 2.76) p<0.001 | 0.78 (0.50, 1.21) p=0.26 | 0.95 (0.58, 1.53) p=0.82 | 1.35 (0.95, 1.93) p=0.09 |
| College graduate | 0.75 (0.49, 1.13) p=0.17 | 0.91 (0.57, 1.44) p=0.68 | 0.97 (0.61, 1.52) p=0.88 | 0.67 (0.42, 1.05) p=0.08 | 2.09 (1.38, 3.17) p<0.001 | 0.63 (0.38, 1.04) p=0.07 | 0.45 (0.25, 0.81) p=0.008 | 1.03 (0.69, 1.52) p=0.90 |
| More than a college degree | 0.65 (0.43, 0.97) p=0.04 | 0.62 (0.39, 0.98) p=0.04 | 0.74 (0.47, 1.15) p=0.18 | 0.72 (0.47, 1.13) p=0.15 | 1.69 (1.13, 2.53) p=0.01 | 0.48 (0.29, 0.79) p=0.004 | 0.58 (0.34, 1.01) p=0.05 | 0.92 (0.63, 1.34) p=0.66 |
| Cancer site | ||||||||
| Colon | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| Rectosigmoid | 0.82 (0.48, 1.38) p=0.45 | 0.47 (0.25, 0.89) p=0.021 | 0.63 (0.36, 1.10) p=0.11 | 1.19 (0.71, 1.98) p=0.52 | 2.47 (1.58, 3.88) p<0.001 | 1.10 (0.60, 2.01) p=0.76 | 1.18 (0.65, 2.13) p=0.59 | 0.72 (0.46, 1.13) p=0.16 |
| Rectal | 1.96 (1.53, 2.51) p<0.001 | 0.95 (0.72, 1.26) p=0.71 | 1.01 (0.77, 1.33) p=0.92 | 1.19 (0.91, 1.58) p=0.21 | 2.36 (1.86, 2.99) p<0.001 | 2.78 (2.10, 3.68) p=<0.001 | 1.05 (0.75, 1.46) p=0.78 | 0.78 (0.61, 0.99) p=0.04 |
| Cancer stage | ||||||||
| 0 | 0.78 (0.51, 1.19) p=0.25 | 1.02 (0.66, 1.57) p=0.93 | 1.09 (0.73, 1.63) p=0.69 | 0.72 (0.46, 1.15) p=0.17 | 0.57 (0.39, 0.82) p=0.003 | 0.60 (0.35, 1.03) p=0.07 | 0.84 (0.48, 1.47) p=0.54 | 1.09 (0.77, 1.56) p=0.62 |
| 1 | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- | -ref- |
| 2 | 1.30 (0.98, 1.71) p=0.070 | 1.22 (0.90, 1.64) p=0.20 | 1.20 (0.90, 1.59) p=0.22 | 1.21 (0.90, 1.63) p=0.21 | 1.38 (1.07, 1.77) p=0.01 | 1.57 (1.13, 2.18) p=0.007 | 1.00 (0.68, 1.47) p=1.0 | 1.00 (0.78, 1.28) p=0.97 |
| 3 | 1.66 (1.26, 2.19) p<0.001 | 1.17 (0.86, 1.57) p=0.32 | 1.08 (0.81, 1.44) p=0.60 | 1.09 (0.81, 1.48) p=0.56 | 0.96 (0.75, 1.24) p=0.76 | 1.07 (0.77, 1.51) p=0.68 | 1.43 (1.01, 2.04) p=0.05 | 1.36 (1.05, 1.76) p=0.02 |
| 4 | 2.70 (1.66, 4.41) p<0.001 | 2.23 (1.34, 3.73) p=0.002 | 1.04 (0.60, 1.80) p=0.88 | 1.05 (0.60, 1.85) p=0.87 | 0.78 (0.47, 1.28) p=0.33 | 1.52 (0.84, 2.73) p=0.16 | 3.29 (1.90, 5.72) p<0.001 | 1.05 (0.64, 1.71) p=0.86 |
Note: All models are adjusted for health plan
Education level was a significant predictor of concern regarding sleep (Wald χ2 13.32, p=0.01), changes in body function (Wald χ2 13.48, p=0.009), visible changes caused by the surgery (Wald χ2 12.45, p=0.01), financial issues (Wald χ2 15.52, p=0.004), and recurrence (Wald χ2 9.64, p=0.05). Higher education was generally associated with fewer concerns about sleep, changes from surgery, and financial issues, but with more concerns about changes in body functions and cancer recurrence.
Cancer site was significantly related to limitations on activities (Wald χ2 30.5, p<0.001), changes in body function (Wald χ2 58.94, p<0.001), and visible changes from the surgery (Wald χ2 52.35, p<0.001). Compared to survivors with colon cancer, survivors with rectal cancer were almost two times more likely to have significant concerns about limitations on activity (OR=1.96, 95% CI:1.52– 2.51) and almost three times more likely to be concerned about visible changes from surgery (OR=2.78, 95% CI: 2.10–3.68). Survivors of rectal and rectosigmoid cancer were more than twice as likely to express concern about changes in body functions compared to survivors of colon cancer (OR=2.36, 95% CI: 1.86–2.99).
Cancer stage was a significant predictor of concerns regarding limitations on activities (Wald χ2 29.93, p<0.001), sleep problems (Wald χ2 10.11, p=0.04), changes in body function (Wald χ2 23.24, p<0.001), visible changes caused by the surgery (Wald χ2 16.27, p=0.003), and financial issues (Wald χ2 23.56, p<0.001). Those diagnosed at stage 4 were significantly more likely to have concerns about limitations on activity (OR=2.70, 95% CI: 1.66–4.41), problems with sleep (OR=2.23, 95% CI: 1.34–3.73), and financial concerns (OR=3.29, 95% CI:1.90 −5.72) compared to those diagnosed at stage 1.
Discussion & Conclusion
Most survivors endorsed opportunities to improve care during treatment. The most frequently identified priority was better communication about what to expect during life after cancer treatment. In this well-insured population, survivors with minority racial/ethnic background were consistently more likely than non-Hispanic whites to report unmet needs relating to their cancer care and to report financial concerns in survivorship. This suggests that, at least for CRC survivors, disparities in unmet informational needs[3,4] are not driven only by access to care. Culturally appropriate and tailored communication interventions to address diverse groups of survivors, which have shown promise in CRC screening[14], may also be effective in improving CRC treatment and survivorship care. It is worth noting that we are using standard categories for describing racial and ethnic subgroups the US population, which we do not consider a reflection of underlying biological differences.
Fear of recurrence has been reported as a major concern of cancer survivors[15], and our results confirm this. Recurrence was the most frequently noted survivorship concern in our cohort and was reported by a majority of respondents. Only age was shown to be a predictor of variability in this concern, with younger respondents expressing the concern most frequently.
Our results also highlight that rectal and colon cancer survivors have very different experiences of care and priorities for survivorship, and that rectosigmoid cancer patients’ rating of priorities generally falls in between the two groups. This is likely due to the complexity of rectal cancer treatment and the lasting effects of surgery and radiation therapy on bowel function, whether or not patients have a permanent ostomy[16].
Other subgroups that could benefit from care improvement and survivorship interventions include: patients younger than 65, and to some extent, patients with later stage disease. For those under 50, the differences compared to those over 75 are particularly noteworthy with respect to concerns about changes in diet, visible changes from surgery, and financial issues. The salience of financial issues is also high for individuals under 65. Factors that are likely driving these changes include the impact of bowel dysfunction on daily life when working outside the home, as well as lack of Medicare insurance, and loss of wages among younger survivors.
Two findings warrant further discussion. First, individuals who reported not having graduated from high school were significantly less likely to state that body function changes were a survivorship priority (30.6%) when compared to other groups with increasing levels of education (41.2%, 44.4%, 45.6% and 41.4%). This may be due to differences in expectations, priorities and resources by educational status, or the vague wording of the response category “changes to body function.” Second, patients diagnosed with stage 0 disease reported relatively high unmet needs relating to treatment options (19%) and side effects (20.6%). Adjusted analyses showed these rates did not significantly differ in comparison to stage 1 patients (15.2% and 18.5%, respectively) whose care is more complex. This may be explained by the fact that stage 0 patients, who may be treated solely by removal of a small cancer in a polyp during a colonoscopy, receive relatively little information about their cancer, recurrence risk, and follow-up care in comparison to those who see a surgeon or oncologist in addition to a gastroenterologist.
Because potential survey participants were identified through the PORTAL infrastructure, we were able to recruit a population-based random sample of survivors and we were able to link responses to clinical and demographic data. The results of this multi-center study have broad generalizability to recent U.S. CRC survivors with health insurance. They may not extend to those without insurance, or to disadvantaged groups, among whom our response rates were quite low[9]. Particularly among those under age 65, further research is warranted to explore priorities and unmet needs among survivors who are under-insured, uninsured, or who receive care outside of integrated delivery systems. We did not collect data that could have helped to determine whether unmet needs and survivorship concerns are influenced by educational interventions, type of insurance coverage, or incidence of treatment-related complications. These are opportunities for further research.
Our main goal was to identify subgroup differences in priorities and concerns. Survivors who could most benefit from care improvement and survivorship interventions include: rectal cancer survivors, individuals of racial-ethnic minority background, and younger survivors (particularly under 65). Individuals with later stage disease and those with lower educational attainment could also benefit. Further research should seek to identify interventions that reduce these quality gaps in high risk groups.
Acknowledgements:
This study used the infrastructure developed by the PORTAL (Patient Outcomes Research to Advance Learning) Network, a consortium of three integrated delivery systems (Kaiser Permanente, HealthPartners, and Denver Health) and their affiliated research centers. Research reported in this article was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (CDRN-1306–04681 Phase II). The PORTAL infrastructure builds upon data structures that receive ongoing support from the National Cancer Institute Cancer (NCI) Research Network (Grant No. U24 CA171524, awarded to Dr. Lawrence H. Kushi, PI) and the Kaiser Permanente Center for Effectiveness and Safety Research. The statements in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Funding: This work was support by Contract No. CDRN-1306–04681 from the Patient Outcomes Research Institute (Awarded to Drs. Elizabeth M. McGlynn and Tracy Lieu). The work builds upon data structures that receive ongoing support from the National Cancer Institute Cancer (NCI) Research Network (Grant No. U24 CA171524, awarded to Dr. Lawrence H Kushi, PI) and the Kaiser Permanente Center for Effectiveness and Safety Research.
References:
- 1.Black N (2013) Patient reported outcome measures could help transform healthcare. Bmj 346:f167. doi: 10.1136/bmj.f167 [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine, National Research Council (2006) From Cancer Patient to Cancer Survivor: Lost in Transition. The National Academies Press, Washington, DC. doi:doi: 10.17226/11468 [DOI] [Google Scholar]
- 3.Beckjord EB, Arora NK, McLaughlin W, Oakley-Girvan I, Hamilton AS, Hesse BW (2008) Health-related information needs in a large and diverse sample of adult cancer survivors: implications for cancer care. J Cancer Surviv 2 (3):179–189. doi: 10.1007/s11764-008-0055-0 [DOI] [PubMed] [Google Scholar]
- 4.Kent EE, Arora NK, Rowland JH, Bellizzi KM, Forsythe LP, Hamilton AS, Oakley-Girvan I, Beckjord EB, Aziz NM (2012) Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Educ Couns 89 (2):345–352. doi: 10.1016/j.pec.2012.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burg MA, Adorno G, Lopez ED, Loerzel V, Stein K, Wallace C, Sharma DK (2015) Current unmet needs of cancer survivors: Analysis of open-ended responses to the American Cancer Society Study of Cancer Survivors II. Cancer 121 (4):623–630. doi: 10.1002/cncr.28951 [DOI] [PubMed] [Google Scholar]
- 6.Corner J, Wagland R, Glaser A, Richards SM (2013) Qualitative analysis of patients’ feedback from a PROMs survey of cancer patients in England. BMJ open 3 (4). doi: 10.1136/bmjopen-2012-002316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corley DA, Feigelson HS, Lieu TA, McGlynn EA (2015) Building Data Infrastructure to Evaluate and Improve Quality: PCORnet. Journal of oncology practice 11 (3):204–206. doi: 10.1200/jop.2014.003194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGlynn EA, Lieu TA, Durham ML, Bauck A, Laws R, Go AS, Chen J, Feigelson HS, Corley DA, Young DR, Nelson AF, Davidson AJ, Morales LS, Kahn MG (2014) Developing a data infrastructure for a learning health system: the PORTAL network. J Am Med Inform Assoc 21 (4):596–601. doi: 10.1136/amiajnl-2014-002746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feigelson HS, McMullen CK, Madrid S, Sterrett AT, Powers JD, Blum-Barnett E, Pawloski PA, Ziegenfuss JY, Quinn VP, Arterburn DE, Corley DA (2017) Optimizing patient-reported outcome and risk factor reporting from cancer survivors: a randomized trial of four different survey methods among colorectal cancer survivors. J Cancer Surviv 11 (3):393–400. doi: 10.1007/s11764-017-0596-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner EH, Greene SM, Hart G, Field TS, Fletcher S, Geiger AM, Herrinton LJ, Hornbrook MC, Johnson CC, Mouchawar J, Rolnick SJ, Stevens VJ, Taplin SH, Tolsma D, Vogt TM (2005) Building a research consortium of large health systems: the Cancer Research Network. J Natl Cancer Inst Monogr (35):3–11. doi: 10.1093/jncimonographs/lgi032 [DOI] [PubMed] [Google Scholar]
- 11.Ritzwoller DP, Carroll N, Delate T, O’Keeffe-Rossetti M, Fishman PA, Loggers ET, Aiello Bowles EJ, Elston-Lafata J, Hornbrook MC (2013) Validation of electronic data on chemotherapy and hormone therapy use in HMOs. Med Care 51 (10):e67–73. doi: 10.1097/MLR.0b013e31824def85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ross TR, Ng D, Brown JS, Pardee R, Hornbrook MC, Hart G, Steiner JF (2014) The HMO Research Network Virtual Data Warehouse: A Public Data Model to Support Collaboration. EGEMS (Washington, DC) 2 (1):1049. doi: 10.13063/2327-9214.1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hornbrook MC, Hart G, Ellis JL, Bachman DJ, Ansell G, Greene SM, Wagner EH, Pardee R, Schmidt MM, Geiger A, Butani AL, Field T, Fouayzi H, Miroshnik I, Liu L, Diseker R, Wells K, Krajenta R, Lamerato L, Neslund Dudas C (2005) Building a virtual cancer research organization. J Natl Cancer Inst Monogr (35):12–25. doi: 10.1093/jncimonographs/lgi033 [DOI] [PubMed] [Google Scholar]
- 14.Naylor K, Ward J, Polite BN (2012) Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med 27 (8):1033–1046. doi: 10.1007/s11606-012-2044-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, Ozakinci G (2013) Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv 7 (3):300–322. doi: 10.1007/s11764-013-0272-z [DOI] [PubMed] [Google Scholar]
- 16.McMullen CK, Bulkley JE, Altschuler A, Wendel CS, Grant M, Hornbrook MC, Sun V, Krouse RS (2016) Greatest Challenges of Rectal Cancer Survivors: Results of a Population-Based Survey. Dis Colon Rectum 59 (11):1019–1027. doi: 10.1097/dcr.0000000000000695 [DOI] [PMC free article] [PubMed] [Google Scholar]