Abstract
Objective:
It is still debatable whether diagnostic coronary angiography (CA) or percutaneous coronary interventions (PCIs) increase radiation exposure when performed via radial approach as compared to femoral approach. This question was investigated in this study by comparison of dose-area product (DAP), reference air kerma (RAK), and fluoroscopy time (FT) among radial and femoral approaches.
Methods:
All coronary procedures between November 2015 and November 2017 were assessed; and 4215 coronary procedures were enrolled in the study. Patients with bifurcation, chronic total occlusion, cardiogenic shock, or prior coronary artery bypass surgery were excluded. These 4215 procedures were evaluated for three different categories: diagnostic CA (Group I), PCI in patients with stable angina (Group II), and PCI in patients with ACS (Group III).
Results:
Age was significantly higher in the femoral arm of all groups. Among patients in the radial arm of Groups I and II, males were over-represented. Therefore, a multiple linear regression analysis with stepwise method was performed. After adjusting these clinical confounders, there was no significant difference with regard to DAP, RAK, and FT between femoral and radial access in Group I. In contrast, PCI via radial access was significantly associated with increased DAP, RAK, and FT in Groups II and III.
Conclusion:
In spite of an increased experience with trans-radial approach, PCI of coronary lesions via radial route was associated with a relatively small but significant radiation exposure in our study. Compared to femoral access, diagnostic CA via radial access was not related to an increased radiation exposure.
Keywords: coronary angiography, femoral artery, percutaneous coronary intervention, radial artery, radiation exposure
Introduction
In recent years, radial access has become a more frequently used access site during coronary interventions. It is recommended over femoral access in contemporary cardiology guidelines because of diminished vascular access site complications, enhanced patient comfort, earlier discharge, diminished costs, and decreased morbidity and cardiac mortality, particularly in patients with acute coronary syndrome (ACS) (1-4). However, it is still a matter of debate as to whether diagnostic coronary angiography (CA) or percutaneous coronary interventions (PCIs) increase radiation exposure when performed via radial approach as compared to femoral approach. As medical exposure to ionizing radiation is associated with stochastic risks (carcinogenic and genetic effects) and deterministic effects (radiation-induced skin injury and cataract), it is a crucial issue for interventional cardiologists (5-8). Therefore, it is also important to apply the practical ways to reduce radiation exposure as fluoroscopy system customization, workflow adaptations, and effective use of shielding equipment (9).
This study was designed to assess whether there was a difference between radial and femoral access sites with regard to the parameters of ionizing radiation as measured by dose-area product (DAP) (which demonstrates the stochastic risk), reference air kerma (RAK) (which demonstrates the deterministic effect), and fluoroscopy time (FT).
Methods
Study design and patient population
The SAKARYA study is a single-center, observational, and retrospective study; and 5707 consecutive coronary procedures performed between November 2015 and November 2017 were evaluated. Radiation parameters were not available in 843 procedures, and they were therefore excluded from the study. Patients with chronic total occlusion (CTO), bifurcation lesion, prior coronary artery bypass grafting (CABG), or cardiogenic shock were excluded from the study (194,103, 222, and 41 procedures, respectively). This was because a femoral approach was preferred in all patients with CTO, bifurcation lesion, cardiogenic shock, and in almost all of the patients with prior CABG. Moreover, 89 patients who had conversions from one access to another (trans-radial to trans-femoral, due to puncture failure or vice-versa due to bilateral iliac or femoral artery occlusion) were also excluded from the study because the total amount of radiation exposure was increased because of two attempts. Thus, 4215 procedures were enrolled in this study. A flowchart of the study is shown in Figure 1.
Figure 1.
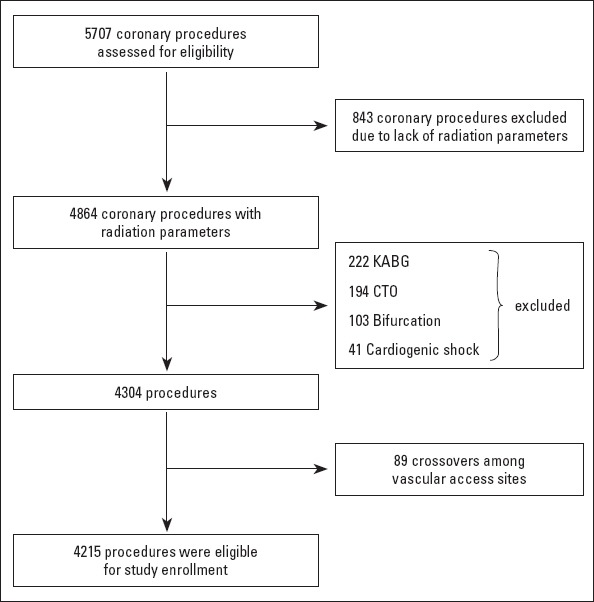
The flowchart of procedure selection
These 4215 procedures were classified as diagnostic CA (Group I), PCI in patients with stable angina (elective PCI) (Group II), and PCI in patients with ACS (Group III). PCI was subclassified into two different categories, stable angina and ACS, based on the different nature of coronary lesions, which may possibly change the difficulties during PCI. This may cause a difference in radiation exposure, and this issue has not yet been evaluated.
In our institution, more than 1000 diagnostic CAs and more than 1500 PCIs are performed each year in two catheter laboratories by 10 interventional cardiologists. Fifty percent of all these procedures are performed via radial access, of which the right radial artery constitutes 99%. In addition, radial operators in our institution have a lifetime radial access experience of at least 1000 cases.
Standard Judkins coronary catheters were initially used for CA via femoral access, whereas a radial TIG catheter (Terumo, NJ, USA) was initially used for CA via radial access. Left ventriculography was not routinely performed during diagnostic CAs, and it occurred far less than 1% of the time in this study. In addition, if there was more than one lesion, the second lesion underwent angioplasty in another session in either the same or the next hospitalization in our institution. This study complies with the Declaration of Helsinki, and the research protocol was approved by the Local Ethics Committee.
Dose metrics and angiographic equipment
In this study, the radiation parameters registered were DAP (expressed in cGY*cm2), RAK (expressed in mGy), and FT (expressed in min). All of these parameters were provided by built-in software of the angiography system, which was periodically calibrated by a technician.
DAP is the integral of radiation dose across the entire X-ray beam emitted from the x-ray tube. Briefly, it is the total amount of energy delivered to the patient. RAK is the air kerma accumulated at a specific point in space, which is the patient entrance reference point relative to the fluoroscopic gantry for a procedure. Air kerma is the energy released in a small volume of air when an X-ray beam irradiates it (10). DAP is strongly related to the long-term stochastic risk (carcinogenic and genetic effects) of cancer. In contrast, DAP is a poor indicator of the deterministic effects that are the tissue reactions as radiation-induced skin injury and cataract. However, as compared to DAP, RAK is a more accurate indicator to demonstrate the deterministic effects.
All cardiovascular procedures were performed using Toshiba Infinix 8000V and Toshiba Infinix 8000G5 (Toshiba Medical Systems, Nasushiobara, Japan). The number of frames was set at 7.5 s-1 frame rate for both fluoroscopy and cineangiography.
Statistical analysis
Statistical analyses were performed using the SPSS software version 24 (SPSS Inc, Chicago IL, USA). Variables were investigated using visual and analytical methods (Kolmogorov-Smirnov test) to determine whether they were normally distributed. As the variables [DAP, RAK, FT, age, and body mass index (BMI)] were not normally distributed and gender was a categorical variable, a Mann-Whitney U test was used to compare these variables between the femoral and radial access groups. The variables affecting DAP, RAK, and FT were investigated using the Spearman correlation. A multiple linear regression analysis with stepwise method was performed, and vascular access site and the other variables that were distributed differently between radial and femoral arms were included in the models to identify the independent predictors of DAP, RAK, and FT. A p-value of less than 0.05 was considered as statistically significant.
Results
A total of 4215 coronary procedures were eligible for the study. Baseline characteristics of patients are shown in Table 1. Those procedures were classified as diagnostic CA (Group I), PCI to patients with stable angina (Group II), and PCI to patients with ACS (Group III) (Table 2).
Table 1.
Comparison of baseline characteristics of patient groups according to radial vs. femoral access sites
| Diagnostic CA (Group I) | P value | PCI of stable angina (Group II) | P value | PCI of ACS (Group III) | P value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| Femoral | 61 (22-89) | <0.001 | 62 (34-88) | 0.017 | 62 (29-100) | <0.001 |
| Radial | 58 (18-100) | 60 (31-86) | 59 (30-100) | |||
| Male Gender | ||||||
| Femoral | 56.2% | 0.011 | 69.5% | 0.003 | 76.7% | 0.095 |
| Radial | 61.7% | 79.3% | 80.7% | |||
| BMI | ||||||
| Femoral | 27.2 (18.0-37.1) | 0.064 | 27.2 (19.2-38.7) | 0.941 | 27.3 (21.6-41.3) | 0.872 |
| Radial | 27.2 (17.6-42.3) | 27.3 (20.9-40.1) | 27.2 (24.1-37.8) | |||
ACS - acute coronary syndrome, BMI - body mass index, CA - coronary angiography, PCI - percutaneous coronary intervention
Table 2.
The distribution of patient groups according to vascular access sites
| Diagnostic CA (Group I) (n, %) | PCI of stable angina (Group II) (n, %) | PCI of ACS (Group III) (n, %) | |
|---|---|---|---|
| Femoral | 856 (41.4%) | 407 (57.2%) | 989 (69%) |
| Radial | 1213 (58.6%) | 305 (42.8%) | 445 (31%) |
| Total | 2069 (100%) | 712 (100%) | 1434 (100%) |
ACS - acute coronary syndrome, CA - coronary angiography, n - number, PCI - percutaneous coronary intervention
Results of Group I
Diagnostic CAs were performed in 2069 patients, 1213 (58.6%) of whom were executed by means of a radial approach. There was no statistical difference regarding the DAP value, RAK, and FT between radial and femoral arms (Table 3). However, median age was higher in the femoral arm of Group I, and the ratio of male gender was higher in the radial arm of Group I (p<0.001 and p=0.011, respectively). There was no statistical difference regarding BMI between radial and femoral arms (p=0.064). In a univariate analysis, older age was associated with higher DAP, RAK, and FT (p<0.001, p=0.001, and p<0.001, respectively). Moreover, male gender was associated with higher DAP and RAK, whereas male gender was not associated with FT (p=0.003, p=0.002, and p=0.489, respectively). Age, gender, and vascular access site were included in multiple linear regression analysis with the stepwise method to determine the independent predictors of DAP, RAK, and FT. Age was an independent predictor of DAP, RAK, and FT; and gender was an independent predictor of DAP and RAK; whereas vascular access site had no impact on DAP, RAK, and FT (Table 4). These results also mean that there was still no statistical difference between femoral and radial arms in terms of DAP, RAK, and FT after adjusting for age and gender.
Table 3.
Radiation exposure parameters according to patient groups
| Diagnostic CA (Group I) | P value | PCI of stable angina (Group II) | P value | PCI of ACS (Group III) | P value | |
|---|---|---|---|---|---|---|
| DAP (cGy*cm2) | ||||||
| Femoral | 798.70 (126.78-5907.71) | 0.580 | 3006.31 (428.72-14546.20) | <0.001 | 3492.88 (563.07-20854.49) | 0.006 |
| Radial | 721.88 (129.54-4767.13) | 3241.47 (625.00-12787.69) | 3686.68 (510.50-23311.97) | |||
| RAK (mGy) | ||||||
| Femoral | 64.75 (8.84-768.60) | 0.802 | 259.24 (39.77-1824.92) | <0.001 | 323.27 (38.96-3938.50) | 0.001 |
| Radial | 61.94 (7.49-789.56) | 284.39 (37.30-1636.80) | 349.27 (33.18-4189.03) | |||
| FT (minute) | ||||||
| Femoral | 1.9 (0.3-27.8) | 0.156 | 7.3 (1.1-36.7) | <0.001 | 7.8 (0.5-48.9) | 0.003 |
| Radial | 1.6 (0.5-18.1) | 7.9 (2.2-39.6) | 8.1 (2-54.1) | |||
ACS - acute coronary syndrome, CA - coronary angiography, DAP - dose-are product, FT - fluoroscopy time, NoE - number of exposures, PCI - percutaneous coronary intervention, RAK - reference air kerma
Table 4.
Multiple linear regression analysis with stepwise method for DAP, RAK, and FT
| Group I P value | Group II P value | Group III P value | |
|---|---|---|---|
| DAP | |||
| Age | 0.001 | * | <0.001 |
| Male gender | <0.001 | * | * |
| Vascular access site | * | <0.001 | 0.022 |
| RAK | |||
| Age | 0.002 | * | 0.002 |
| Male gender | <0.001 | * | * |
| Vascular access site | * | <0.001 | 0.014 |
| FT | |||
| Age | <0.001 | * | <0.001 |
| Male gender | * | * | * |
| Vascular access site | * | 0.021 | 0.009 |
The factors that were not included in the final model formed by stepwise method.
DAP - dose-are product, FT - fluoroscopy time, RAK - reference air kerma
Results of Group II
PCI in patients with stable angina was performed in 712 procedures; and the DAP value, RAK, and FT were all significantly higher in the radial arm (305 procedures, 42.8%) (Table 3). However, median age was higher in the femoral arm of Group II, and the ratio of male gender was higher in the radial arm of Group II (p=0.017, and p=0.003, respectively). There was no statistical difference with regard to BMI between radial and femoral arms of Group II (p=0.941). In a univariate analysis, age and gender were not found to be correlated with DAP, RAK, and FT (p=0.704, p=0.770, and p=0.058, respectively for age; and p=0.516, p=0.392, and p=0.203, respectively for gender). Age, gender, and vascular access site were included in multiple linear regression analysis with the stepwise method to determine the independent predictors of DAP, RAK, and FT. Vascular access site was an independent predictor of DAP, RAK, and FT. These results suggest that radial approach is associated with higher radiation exposure in patients with stable angina who have undergone PCI after adjusting for age and gender. The average increase was 7.3% in DAP, 8.8% in RAK, and 7.6% in FT as shown in Figure 2.
Figure 2.
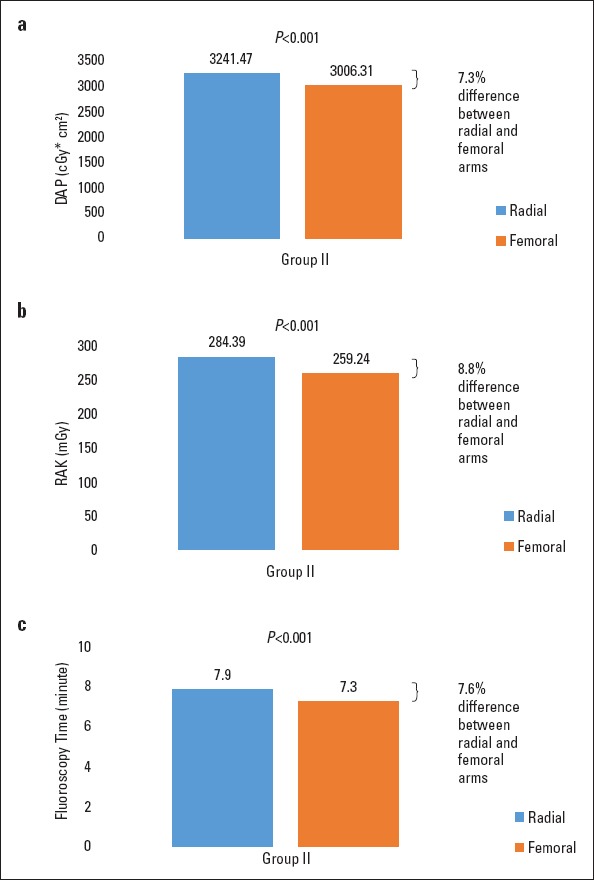
The difference of dose-area product (a), reference air kerma (b), and fluoroscopy time (c) between radial and femoral arms in Group II.
DAP - dose-are product, RAK - reference air kerma
Results of Group III
The DAP value, RAK, and FT were again significantly higher in the radial arm of patients with ACS who underwent PCI (445 procedures, 31%) (Table 3). There was no statistical difference with regard to the BMI and gender of Group III patients who had undergone PCI involving either the radial or femoral arms (p=0.872, and p=0.095, respectively). However, median age was higher in the femoral arm of Group III (p<0.001). In a univariate analysis, older age was found to be correlated with higher DAP, RAK, and FT (p<0.001, p=0.002, and p<0.001, respectively). Age and vascular access site were included in multiple linear regression analysis with the stepwise method to determine the independent predictors of DAP, RAK, and FT (Table 4). Age and vascular access site were independent predictors of DAP, RAK, and FT. Therefore, radial access was associated with higher radiation exposure in patients with ACS who underwent PCI as compared to femoral access after adjusting for age. The average increase was 5.3% in DAP, 7.4% in RAK, and 3.7% in FT as shown in Figure 3.
Figure 3.
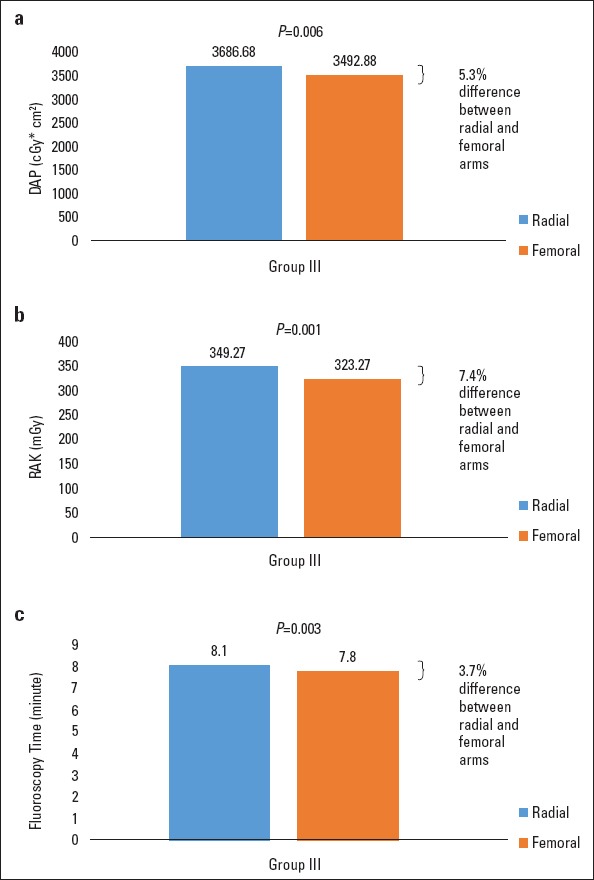
The difference of dose-area product (a), reference air kerma (b), and fluoroscopy time (c) between radial and femoral arms in Group III.
DAP - dose-are product, RAK - reference air kerma
Discussion
It is still debatable whether radial approach leads to prolonged procedures and increased radiation exposure during coronary procedures. As the results of published studies are contradictory, new studies are needed to find an answer to this tough question.
This study demonstrated that there was a similar radiation exposure in both radial and femoral arms during diagnostic CAs when performed by experienced operators. The DAP value, RAK, and FT were similar in both groups, irrespective of the entry site. Therefore, we stated that the stochastic risk and the deterministic effects of radiation exposure were not increased in patients who underwent diagnostic CA via radial approach. There are only a few studies which have focused on radiation exposure of patients who only underwent diagnostic CA, whereas most studies have analyzed radiation exposure involving both diagnostic CA and PCI arms. In parallel with our result, Kuipers et al. (11) demonstrated similar radiation exposure between trans-radial and trans-femoral groups in the diagnostic CA arm of the study. Moreover, Gray et al. (12) have found similar radiation exposure for both femoral and radial approaches in patients who underwent diagnostic CA. Furthermore, the REVERE trial noted that radiation exposure to patients was similar during diagnostic CA, irrespective of the vascular access site (13). However, Mercuri et al. (14) have stated that radial approach was a predictor of increased radiation exposure during diagnostic CA. Farman et al. (15) emphasized that radial approach during diagnostic CA was related to prolonged FT, even when performed by experienced operators. Shah et al. (16) stated that trans-radial approach performed by experienced operators was associated with higher radiation exposure in the diagnostic CA arm. A meta-analysis by Plourde et al. (17) also demonstrated an increased radiation exposure in the diagnostic CA arm of the study (17). On the other hand, Georges et al. (18, 19) have stated that radial approach during diagnostic CA was associated with lower radiation exposure than femoral approach in high-radial-volume centers. A possible explanation for the similar radiation exposure observed in the diagnostic CA arm of this study (as compared to other studies that demonstrated a higher radiation exposure during diagnostic CA) is that a radial TIG catheter was used, instead of standard Judkins left-and-right catheters. Thus, only a single effort was needed to reach the aortic root and to visualize both left and right coronary arteries via an easy manipulation of the TIG catheter to disengage the left main coronary artery and to engage the right coronary artery. Here, it should be emphasized that TIG catheter cannot be purchased and found in every catheter laboratory; thus, two different diagnostic catheters are used during diagnostic CA, which may potentially increase the radiation exposure.
In the PCI arm of this study, PCIs were classified into two separate groups as “PCI in patients with stable angina” and ”PCI in patients with ACS”. These groups were evaluated as distinct groups based on the different nature of coronary lesions: stable angina and ACS (which may possibly change the difficulties encountered during PCI). No study addressed this issue in the literature. This study demonstrated an increased radiation exposure during PCI to patients with stable angina and PCI to patients with ACS when a radial approach was chosen. In both groups, the DAP, RAK, and FT were all higher in the radial access arm. Thus, the PCI groups produced similar results in this study and the trans-radial approach was associated with an increased radiation exposure irrespective of the nature of the coronary lesions (either stable or unstable). The average increase in radiation exposure in the radial arm ranged between 3.7% and 8.8% in Groups II and III according to DAP, RAK, and FT. The difference in radiation exposure between the radial and femoral arms was relatively small but significant. This finding is similar to the results of the meta-analysis by Plourde et al. (17) with regard to the patients who underwent PCI. Plourde et al. (17) also concluded that there was a small but significant increase in radiation exposure in patients who underwent PCI via a radial approach. Because of this study, we suggested that PCI of stable or unstable coronary lesions via radial approach may prolong the procedure time and may lead to increased DAP and RAK. Thus, PCI via trans-radial approach may increase the stochastic risk and the deterministic effects of radiation exposure in patients who have undergone PCI.
The published studies, which investigated whether a difference was present in radiation exposure with regard to the vascular access site in patients who have undergone PCI, assessed PCI as a whole without subclassification. In parallel with our results, Shah et al. (16) demonstrated that PCI via radial approach and performed by experienced operators was associated with higher radiation exposure. Moreover, Sciahbasi et al. (20) concluded that radial approach was associated with higher operator and patient radiation exposure when performed by expert operators in patients with ACSs. In contrast, Georges et al. (18, 19) stated that PCI via radial approach was associated with lower radiation exposure compared to femoral approach in high-radial-volume centers. They emphasized the importance of experience with regard to trans-radial angiography. In addition, Hetherington et al. (21) compared the radial approach and femoral approaches in patients with ST elevation myocardial infarction with regard to factors such as major and minor vascular complications, in-hospital mortality, contrast volume used, radiation dose absorbed. They concluded that radial approach was associated with lower radiation exposure as compared to femoral approach (21). Kuipers et al. (11) and Gray et al. (12) revealed similar radiation exposures for both femoral and radial approaches in patients who underwent PCI. Rigattieri et al. (22) found similar results. They concluded that after adjusting for clinical and procedural confounders, trans-radial approach was not associated with increased radiation exposure as compared to trans-femoral approach.
The main argument of the articles asserting a lower or similar radiation exposure with the radial approach was that increased radiation exposure was due to inadequate experience typical of operators carrying out a radial approach. The experience of radial operators and the coronary procedure volume in our institution was mentioned in the material and methods section. Moreover, a study including more than 10,000 patients who underwent diagnostic CA or PCI via radial approach was previously published by our institution (23). Therefore, higher radiation exposure due to trans-radial approach in Groups II and III cannot be explained by lower operator experience with the radial approach. A possible explanation for increased radiation exposure in the PCI arm of this study is that PCI via radial approach may be more technically arduous if the following conditions exist: i) brachiocephalic-aortic axis or subclavian-aortic axis is tortuous and ii) if several attempts to crossover this tortuous axis may be needed during PCI.
Hence, this study suggests that patients who underwent diagnostic CA were exposed to similar levels of radiation in both radial and femoral arms, whereas they were exposed to relatively small-but significantly higher-levels of ionizing radiation during PCI via radial approach. This study could not give an exact idea regarding radiation exposure of operators, because radiation exposure of operators should be selectively measured and assessed with dosimeters for the thorax, wrist, and eye, rather than with assessment of procedural DAP, RAK, and FT. However, increased FT, DAP, and RAK may indirectly reveal an increased risk of radiation exposure for operators. This could be argued because a similar result for patients and operators with regard to radiation exposure was demonstrated in the RAD-Matrix trial (20). Moreover, a strong correlation between procedural DAP and reference personal dosimeter dose was demonstrated by Sailer et al. (24). Furthermore, Brasselet et al. (25) and Kuipers et al. (26) revealed strong correlations between patient and operator exposure. Therefore, it might be reasonable to deem that higher radiation exposure in patients may correlate with increased radiation exposure in operators as well. However, further trials addressing the radiation exposure of both patients and operators are needed.
Study limitations
Our study has several limitations. Firstly, it was not designed as a prospective study. Therefore, this may result in unmeasured confounding variables. Moreover, the data for this study belong to one institution. Thus, it is a retrospective and single-center study. Furthermore, the coronary lesion characteristics were not obtained and classified. Therefore, even the patient volume was high, this might act as a confounding variable. Finally, DAP, RAK, and FT mainly demonstrate the radiation exposure of patients. However, special dosimeters for the thorax, wrist, and eye are needed for more exact measurements of radiation exposure of operators.
Conclusion
This study demonstrated that radial approach was not associated with increased radiation exposure during diagnostic CAs. On the other hand, radial approach increased the radiation exposure during PCI of stable lesions and PCI of ACS lesions. Although radial approach during PCI decreases complications as compared to femoral approach, it may increase the possible stochastic risk and deterministic effects when performed even by experienced operators. Therefore, additional stringent precautions should be taken not only for the benefit of patients but also for the benefit of operators in order to reduce radiation exposure during coronary interventions via radial access, as thousands of coronary interventions are performed by an operator during his/her professional career.
Acknowledgements
We would like to thank to Işın Üreyen, MD for her contribution to the statistical analysis of this study. This study was presented at the 34th Turkish Cardiology Congress with international participation as an oral presentation in Belek/Antalya on October 23, 2018, with a presentation number of SB-147.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – Ç.M.Ü., K.C., M.G.V., S.E.Ş.; Design – Ç.M.Ü., M.T.A., E.T., H.G., R.A.; Supervision – M.G.V., M.T.A., E.T., H.G., R.A.; Fundings – None; Materials – None; Data collection &/or processing – Ç.M.Ü., S.E.Ş., İ.K., M.T.P., M.N.M.A.; Analysis &/or interpretation – Ç.M.Ü., K.C., İ.K., M.T.P., M.N.M.A.; Literature search – Ç.M.Ü., S.E.Ş., M.T.A.; Writing – Ç.M.Ü.; Critical review – Ç.M.Ü., K.C., M.G.V., S.E.Ş., İ.K., M.T.P., M.N.M.A., M.T.A., E.T., H.G., R.A.
References
- 1.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome:the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60:2481–9. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Valgimigli M, Gagnor A, Calabro P, Frigoli E, Leonardi S, Zaro T, et al. Radial versus femoral access in patients with acute coronary syndromes undergoing invasive management:a randomised multicentre trial. Lancet. 2015;385:2465–76. doi: 10.1016/S0140-6736(15)60292-6. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell MD, Hong JA, Lee BY, Umscheid CA, Bartsch SM, Don CW. Systematic review and cost-benefit analysis of radial artery access for coronary angiography and intervention. Circ Cardiovasc Qual Outcomes. 2012;5:454–62. doi: 10.1161/CIRCOUTCOMES.112.965269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bertrand OF, Belisle P, Joyal D, Costerousse O, Rao SV, Jolly SS, et al. Comparison of transradial and femoral approaches for percutaneous coronary interventions:a systematic review and hierarchical Bayesian meta-analysis. Am Heart J. 2012;163:632–48. doi: 10.1016/j.ahj.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Roguin A, Goldstein J, Bar O, Goldstein JA. Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol. 2013;111:1368–72. doi: 10.1016/j.amjcard.2012.12.060. [DOI] [PubMed] [Google Scholar]
- 6.Buchanan GL, Chieffo A, Mehilli J, Mikhail GW, Mauri F, Presbitero P, et al. The occupational effects of interventional cardiology:results from the WIN for Safety survey. EuroIntervention. 2012;8:658–63. doi: 10.4244/EIJV8I6A103. [DOI] [PubMed] [Google Scholar]
- 7.Marinskis G, Bongiorni MG, Dagres N, Lewalter T, Pison L, Blomstrom-Lundqvist C Scientific Initiative Committee, European Heart Rhythm Association. X-ray exposure hazards for physicians performing ablation procedures and device implantation:results of the European Heart Rhythm Association survey. Europace. 2013;15:444–6. doi: 10.1093/europace/eut022. [DOI] [PubMed] [Google Scholar]
- 8.Karatasakis A, Brilakis HS, Danek BA, Karacsonyi J, Martinez-Parachini JR, Nguyen-Trong PJ, et al. Radiation-associated lens changes in the cardiac catheterization laboratory:Results from the IC-CATARACT (CATaracts Attributed to RAdiation in the CaTh lab) study. Catheter Cardiovasc Interv. 2018;91:647–54. doi: 10.1002/ccd.27173. [DOI] [PubMed] [Google Scholar]
- 9.Heidbuchel H, Wittkampf FH, Vano E, Ernst S, Schilling R, Picano E, et al. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014;16:946–64. doi: 10.1093/europace/eut409. [DOI] [PubMed] [Google Scholar]
- 10.Miller DL, Balter S, Cole PE, Lu HT, Schueler BA, Geisinger M, et al. RAD-IR study. Radiation doses in interventional radiology procedures:The RAD-IR study Part I. Overall measures of dose. J Vasc Interv Radiol. 2003;14:711–27. doi: 10.1097/01.rvi.0000079980.80153.4b. [DOI] [PubMed] [Google Scholar]
- 11.Kuipers G, Delewi R, Velders XL, Vis MM, van der Schaaf RJ, Koch KT, et al. Radiation exposure during percutaneous coronary interventions and coronary angiograms performed by the radial compared with the femoral route. JACC Cardiovasc Interv. 2012;5:752–7. doi: 10.1016/j.jcin.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Gray B, Klimis H, Inam S, Ariyathna N, Kumar S, Bailey B, et al. Radiation exposure during cardiac catheterisation is similar for both femoral and radial approaches. Heart Lung Circ. 2015;24:264–9. doi: 10.1016/j.hlc.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 13.Pancholy SB, Joshi P, Shah S, Rao SV, Bertrand OF, Patel TM. Effect of vascular access site choice on radiation exposure during coronary angiography:The REVERE trial (Randomized Evaluation of Vascular Entry Site and Radiation Exposure) JACC Cardiovasc Interv. 2015;8:1189–96. doi: 10.1016/j.jcin.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 14.Mercuri M, Mehta S, Xie C, Valettas N, Velianou JL, Natarajan MK. Radial artery access as a predictor of increased radiation exposure during a diagnostic cardiac catheterization procedure. JACC Cardiovasc Interv. 2011;4:347–52. doi: 10.1016/j.jcin.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Farman MT, Khan NU, Sial JA, Saqhir T, Rizvi SN, Zaman KS. Comparison of fluoroscopy time during coronary angiography and interventions by radial and femoral routes- can we decrease the fluoroscopy time with increased experience? An observational study. Anadolu Kardiyol Derg. 2011;11:607–12. doi: 10.5152/akd.2011.163. [DOI] [PubMed] [Google Scholar]
- 16.Shah B, Bangalore S, Feit F, Fernandez G, Coppola J, Attubato MJ, et al. Radiation exposure during coronary angiography via transradial or transfemoral approaches when performed by experienced operators. Am Heart J. 2013;165:286–92. doi: 10.1016/j.ahj.2012.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Plourde G, Pancholy SB, Nolan J, Jolly S, Rao SV, Amhed I, et al. Radiation exposure in relation to the arterial access site used for diagnostic coronary angiography and percutaneous coronary intervention:a systematic review and meta-analysis. Lancet. 2015;386:2192–203. doi: 10.1016/S0140-6736(15)00305-0. [DOI] [PubMed] [Google Scholar]
- 18.Georges JL, Belle L, Ricard C, Cattan S, Albert F, Hirsch JL, et al. Patient exposure to x-rays during coronary angiography and percutaneous transluminal coronary intervention:Results of a multicenter national survey. Catheter Cardiovasc Interv. 2014;83:729–38. doi: 10.1002/ccd.25327. [DOI] [PubMed] [Google Scholar]
- 19.Georges JL, Belle L, Meunier L, Dechery T, Khalife K, Pecheux M, et al. Radial versus femoral access for coronary angiography and intervention is associated with lower patient radiation exposure in high-radial-volume centres:Insights from the RAY'ACT-1 study. Arch Cardiovasc Dis. 2017;110:179–87. doi: 10.1016/j.acvd.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Sciahbasi A, Frigoli E, Sarandrea A, Rothenbühler M, Calabro P, Lupi A, et al. Radiation Exposure and Vascular Access in Acute Coronary Syndromes:The RAD-Matrix Trial. J Am Coll Cardiol. 2017;69:2530–7. doi: 10.1016/j.jacc.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 21.Hetherington SL, Adam Z, Morley R, de Belder MA, Hall JA, Muir DF, et al. Primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction:changing patterns of vascular access, radial versus femoral artery. Heart. 2009;95:1612–8. doi: 10.1136/hrt.2009.170233. [DOI] [PubMed] [Google Scholar]
- 22.Rigattieri S, Sciahbasi A, Drefahl S, Mussino E, Cera M, Di Russo C, et al. Transradial access and radiation exposure in diagnostic and interventional coronary procedures. J Invasive Cardiol. 2014;26:469–74. [PubMed] [Google Scholar]
- 23.Tatli E, Buturak A, Cakar A, Vatan BM, Degirmencioglu A, Agac TM, et al. Unusual vascular complications associated with transradial coronary procedures among 10,324 patients:Case-based experience and treatment options. J Interv Cardiol. 2015;28:305–12. doi: 10.1111/joic.12206. [DOI] [PubMed] [Google Scholar]
- 24.Sailer AM, Paulis L, Vergoossen L, Kovac AO, Wijnhoven G, Schurink GW, et al. Real-Time Patient and Staff Radiation Dose Monitoring in IR Practice. Cardiovasc Intervent Radiol. 2017;40:421–9. doi: 10.1007/s00270-016-1526-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brasselet C, Blanpain T, Tassan-Mangina S, Deschildre A, Duval S, Vitry F, et al. Comparison of operator radiation exposure with optimized radiation protection devices during coronary angiograms and ad hoc percutaneous coronary interventions by radial and femoral routes. Eur Heart J. 2008;29:63–70. doi: 10.1093/eurheartj/ehm508. [DOI] [PubMed] [Google Scholar]
- 26.Kuipers G, Velders XL, Piek JJ. Exposure of cardiologists from interventional procedures. Radiat Prot Dosimetry. 2010;140:259–65. doi: 10.1093/rpd/ncq113. [DOI] [PubMed] [Google Scholar]


