Abstract
STUDY QUESTION
Do sense of meaning and acceptance mediate the relationships between gratitude and infertility-related stress among women undergoing IVF?
SUMMARY ANSWER
Among women undergoing IVF, the negative relationships between gratitude and infertility-related stress are explained by a general sense of meaningfulness and acceptance of life.
WHAT IS KNOWN ALREADY
Infertility experts increasingly call for a re-balancing of the deficit-based view of psychosocial adjustment in IVF, which has been heavily dominated by studies of risk factors and psychological distress. Attention has been given to strength-based perspectives that emphasize character strengths and personal growth. Gratitude has been found to be a potent protective factor in coping with life stressors; however, its salutary effects and protective processes for infertile women undergoing IVF are yet to be explored.
STUDY DESIGN, SIZE, DURATION
This study utilized baseline data of a randomized controlled trial for mind–body interventions with 357 Hong Kong Chinese women. Data collection was conducted between January 2015 and December 2017.
PARTICIPANTS/MATERIALS, SETTINGS, METHODS
Eligible women were approached by a research assistant immediately after their first medical consultation at an ART centre of a major university-affiliated hospital. Participants were asked to complete a battery of questionnaires, including the Gratitude Questionnaire-6, the Fertility Problem Inventory, and the Holistic Well-Being Scale. Mediation analyses were conducted with bootstrapped samples.
MAIN RESULTS AND THE ROLE OF CHANCE
Of the 494 women who were approached, 357 (72.3%) provided informed consent and participated in the study. Results show that gratitude was negatively associated with all infertility-related stress domains (rs = −0.19 to −0.36), and these relationships are mediated by acceptance and loss of sense of meaning. Further, the link between gratitude and relationship concerns is mediated by loss of sense of meaning in women with a definable cause of infertility (95% CI = [−0.31, −0.08]), but by acceptance among those with unexplained infertility (95% CI = [−0.33, −0.01]).
LIMITATIONS, REASONS FOR CAUTION
The cross-sectional nature of the study precluded inferences of causality. Self-selection and self-report biases could be present. Our findings may not be readily generalizable to women who do not intend to undergo psychosocial intervention for their infertility or ART.
WIDER IMPLICATIONS OF THE FINDINGS
Our findings support the salutary effects of gratitude in coping with IVF and highlight the role of unexplained infertility in the coping process. These findings offer preliminary support to the use of psychosocial interventions in promoting gratitude, acceptance, and meaning reconstruction for reducing infertility-related stress in women undergoing IVF.
STUDY FUNDING/COMPETING INTEREST(S)
This study was funded by the Hong Kong University Grant Council—General Research Fund (HKU27400414). All authors declare no competing interests.
TRIAL REGISTRATION NUMBER
HKUCTR-1984.
Keywords: IVF, infertility, gratitude, reproduction, coping, psychotherapy, Chinese, personality, counselling, stress
WHAT DOES THIS MEAN FOR PATIENTS?
This study looks at whether having a grateful disposition is related to stress for women in IVF treatment, and whether acceptance and sense of meaning play any part in this relationship.
IVF is a physically and mentally stressful procedure. While many studies have investigated how people cope with treatment distress, very few have looked at the protective factors that shield people from negative emotions. We know that grateful people tend to be more appreciative towards other people and events, and are better able to accept the ups and downs in life. Therefore, in a sample of women who are about to begin an IVF cycle, we test whether those who perceive themselves to be grateful experience lower levels of infertility-related stress, and whether this relationship can be explained by women’s ability to accept and let go of negative events, as well as their ability to find meaning in life.
We found that women who score higher on a gratitude questionnaire also report lower levels of fertility-related stress. We suggest this may be because grateful personalities direct people’s attention towards the positive aspects and away from the negative aspects of life, thus making them more able to accept what comes in their way and protecting them from losing hope and meaning for life. The findings are encouraging as they suggest it is possible to relieve treatment distress through cultivating gratitude and acceptance through interventions, and provide a basis for future intervention studies.
However, we should bear in mind that the present observations are made at a single point in time, meaning we cannot be certain whether it is being grateful that reduces stress or having low stress that makes a person more able to be appreciative. Further, the findings only apply to women in IVF, thus leaving the coping strategies of men in IVF an open question.
Introduction
Research has revealed the rates of psychological distress experienced by women undergoing IVF as comparable to those of the general public (Verhaak et al., 2006). Elevated distress is often transient, but peaks at moments of medical procedures (e.g. oocyte retrieval, embryo transfer), during the waiting period prior to a pregnancy test, and upon learning of treatment failure (Mahajan et al., 2010; Gameiro et al., 2015). The majority of women starting IVF report only slight differences in levels of psychological distress compared to their healthy counterparts (Verhaak et al., 2006). To understand how women cope with IVF, researchers have advocated adopting a strength-based orientation that acknowledges personal strengths for attaining quality of life, gains, and growth, in place of the long-established deficit-based view that emphasizes risk factors and defines well-being as the absence of ill-being (Herrmann et al., 2011; Rockliff et al., 2014; Raque-Bogdan and Hoffman, 2015). So far, only a handful of studies have investigated what these strengths are and how they facilitate coping with stress related to infertility and its treatment. Existing studies have examined associations between attributes such as resilience (Herrmann et al., 2011; Yu et al., 2014), self-compassion (Galhardo et al., 2013; Raque-Bogdan and Hoffman, 2015) and optimism (Lancastle and Boivin, 2005), and psychosocial adjustment among infertile women.
According to McCullough et al. (2002, 2004), gratitude can be conceptualized as an affective trait, meaning that people with higher levels of this trait tend to exhibit grateful emotions in relation to a wider array of things, in more diverse circumstances, more frequently, and of greater intensity in each episode. A rich corpus of studies has demonstrated a robust positive association between gratitude and subjective well-being (McCullough et al., 2002), and a negative association with psychological distress (DeWall et al., 2012; Lambert et al., 2012), among diverse populations dealing with health concerns, including women with breast cancer (Ruini and Vescovelli, 2013) and caregivers of persons with dementia (Lau and Cheng, 2017). Previous studies have demonstrated that couples identify gains, such as a closer relationship with spouse and other family members, greater understanding of life’s mission and priorities, and enhanced mastery, knowledge, and problem-solving, resulting from their IVF experiences (Schmidt et al., 2005; Lee et al., 2009; Ying et al., 2015; Habroe et al., 2007). Gratitude may facilitate the identification of these gains and promote adjustment among infertile women undergoing IVF.
Grateful individuals tend to attribute the good things that exist or happen in their lives to a benevolent other, be it a higher power, a supportive spouse, friend, or family member. Instead of taking these benefits for granted, grateful individuals perceive the benefits as an altruistic gift and the benefits as more valuable (Wood et al., 2008). The find-remind-and-bind theory (Algoe, 2012) also suggests that gratitude amplifies the benefits a person experiences and the kindness of the benefactor in one’s account of an experience. In turn, this may neutralize an apparently negative experience, such as infertility, with positive episodes, making the total experience more palatable. Hence, grateful individuals have an easier time accepting the peaks and troughs in life or are better at using ‘letting go’ coping (Rapoport-Hubschman et al., 2009) (i.e. ‘acceptance pathway’). In addition, gratitude may enhance adaptation to infertility and its treatment through fostering a sense of meaning and circumventing feelings of disorientation (i.e. ‘the meaning pathway’; (Liao and Weng, 2018). In this regard, the current study expanded investigation of the salutary effects of gratitude to the context of infertility by testing the hypotheses that gratitude negatively relates to multidimensional infertility-related stress, and that the links between gratitude and infertility-related stress are mediated by the acceptance and the meaning pathways among infertile women undergoing IVF (Fig. 1).
Figure 1.
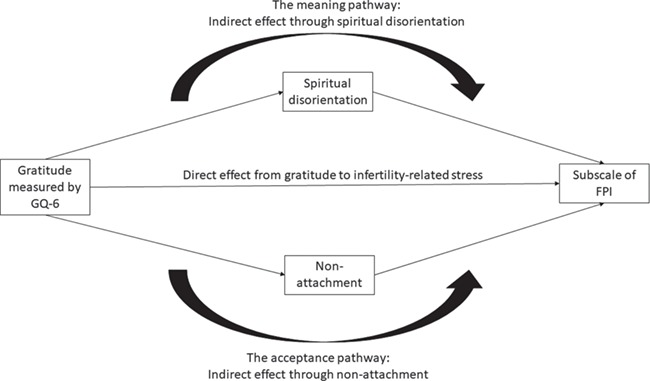
Proposed mediation pathways between gratitude and domains of infertility-related stress. GQ-6: Gratitude Questionnaire-6, FPI: Fertility Problem Inventory.
About 30% of infertile couples worldwide are diagnosed with unexplained infertility (Sadeghi, 2015), meaning that the woman experiences infertility in spite of ovulating normally, having patent fallopian tubes, and a normal semen analysis of her partner. The impact of a known cause of infertility on the psychosocial adjustment of infertile individuals has been documented, but remains inconclusive. Chan et al. (2015) showed that women facing unexplained infertility reported greatest physical distress but not psychological and spiritual distress compared to those facing infertility with a known cause. Lee et al. (2001) found that women facing female factor infertility experienced greater distress than those facing infertility due to male-, mixed- or unknown factors. Newton et al. (1999), however, showed that women facing idiopathic infertility reported lower levels of distress than those facing male factor infertility, but higher levels of distress than those with female factor infertility. Romano et al. (2012) found that compared to women with explained infertility, women facing unexplained infertility exhibit maladaptive coping and defence mechanisms.
Assigning personal and interpersonal meanings to their infertility could be particularly difficult for individuals who do not know the medical reason behind their infertility and who are thus unable to identify who and what are responsible for it. This ‘sense of utter mystery’ (Paul et al., 2009) may predispose individuals to relentless rumination about the cause of their infertility. Accepting or ‘letting go’, rather than becoming enmeshed in the pursuit of a meaning, could therefore be more adaptive in the case of unexplained infertility. To date, the impact of unexplained infertility on adaptation to infertility and its treatment has not received sufficient attention. Hence, this study also explored whether unexplained infertility is associated with infertility-related stress and whether it moderates the mediating pathways between gratitude and infertility-related stress.
Materials and Methods
Ethical Approval
The study was approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 14-252) and Human Research Ethics Committee of The University of Hong Kong (EA 1511002), and is registered on the HKU Clinical Trial Registry (HKUCTR-1984). Written informed consent has been obtained from the participants before the beginning of data collection.
Design
This study analysed the data collected as a part of a randomized controlled trial on self-administered mind–body interventions for infertile women undergoing IVF. The trial compared the efficacy of a mind–body intervention, a spiritual intervention and a health education control condition on relieving anxiety and improving fertility-related quality of life among infertile women during the 2-week waiting period between embryo transfer and pregnancy test. The current baseline data were collected after the first medical appointment and before embryo transfer. The data were collected before the beginning of the psychosocial intervention and before participants were aware of their group allocation.
Participants and setting
Participants were recruited from patients attending the Centre of Assisted Reproduction and Embryology, The University of Hong Kong—Queen Mary Hospital. In Hong Kong, women below the age of 40 years at the time of treatment who do not have living children are entitled to three government-subsidized IVF treatments using fresh embryos at a public hospital such as the Queen Mary Hospital. Infertile women who were about to undergo an IVF cycle were approached. Exclusion criteria included women who were not Chinese, who had a known history of severe psychiatric illness (e.g. psychosis, schizophrenia), or who did not possess internet or mobile phone access.
Procedure
Eligible women were approached by a research assistant immediately after their first medical consultation. The research assistant explained the study, and women who were willing to participate were given a cover letter and asked to sign an informed consent form. Regardless of their group allocation, participants were then scheduled to attend an introductory session where they would complete the baseline survey. Data were collected between January 2015 and December 2017.
Measures
Gratitude was measured by the Gratitude Questionnaire-6 (GQ-6) (McCullough et al., 2002). Participants rated six statements, such as ‘I have so much in life to be thankful for’ and ‘If I had to list everything that I felt grateful for, it would be a very long list’ on a scale of 1–7 to indicate their day-to-day gratitude levels, 1 (‘totally disagree’) and 7 (‘totally agree’). Responses on opposite direction items were reverse-coded, and scores on the six items were averaged to provide the scale score. Higher scale scores indicate greater gratitude. Reliability was satisfactory (α = 0.83).
The non-attachment and spiritual disorientation subscales of the Holistic Well-Being cale (Chan et al., 2014b) were used to measure acceptance and loss of sense of meaning. The non-attachment subscale encompasses five items describing acceptance and being at peace with the vicissitudes life, such as ‘I can let go if I so desire’ and ‘I can accept the ups and downs in life as they come’. The spiritual disorientation subscale contains four items describing the lack of meaning, value, and direction in life, such as ‘My whole life seems to be meaningless’ and ‘I have lost my direction in life’. Both subscales have been used among several local populations, including adults with depression syndrome seeking treatment at Chinese medicine clinics (Chan et al., 2014b), adults with sleep problems (Ji et al., 2017), and patients with lung cancer and their caregivers (Lau et al., 2018), with satisfactory psychometric properties. Participants rated the extent to which each item represented a suitable description of themselves on a 10-point Likert scale from 1 (‘totally unsuitable’) to 10 (‘totally suitable’). Scale scores were derived by reverse-coding opposite direction items and averaging the responses across the items. Higher scale scores indicate a greater display of each characteristic. Reliability was satisfactory for both scales (αs = 0.74 and 0.89).
Infertility-related stress was assessed by the Fertility Problem Inventory (FPI; Newton et al., 1999). The 46-item scale encompasses five subscales (social concerns, e.g. ‘I find it hard to spend time with friends who have young children’, sexual concerns, e.g. ‘I feel like I’ve failed at sex’, relationship concerns, e.g. ‘My partner doesn’t understand the way the fertility problem affects me’, need for parenthood, e.g. ‘For me, being a parent is a more important goal than having a satisfying career’, rejection of a childfree lifestyle, e.g. ‘Couples without a child are as just as happy as those with children’ [reverse-coded]) and a composite global stress scale. Participants responded to the item using a 6-point Likert scale ranging from 1 (‘strongly disagree’) to 6 (‘strongly agree’). Scale scores were derived by reverse-coding opposite direction items and adding up responses to constituent items, such that higher scores indicate greater infertility-related stress. The global stress score was derived from the sum of the five subscale scores. Reliabilitiy was satisfactory (αs = 0.65 and 0.83).
Participants provided demographic information (e.g. age of the woman, her husband education level, and religious affiliation), history of infertility and related treatment (e.g. choice of current treatment, number of previous ART cycles, years, and type of infertility). Medical records were checked and information about the cause of infertility was extracted. Cases with a definable cause (female-, male-, or mixed-factor) were grouped together for the purpose of comparison against unexplained infertility cases.
Statistical analysis
Descriptive statistics were used to indicate the levels of gratitude, loss of sense of meaning, acceptance, and infertility-related stress. Bivariate correlations were deployed to assess correlations among key variables. Associations of infertility-related stress with unexplained infertility (0 = with definable cause, 1 = unexplained) were explored by an adjusted multivariate analysis of variance (MANOVA). A mediation analysis, followed by a moderated mediation analysis with unexplained infertility as moderator, was conducted with each FPI scale using the PROCESS macro developed by Hayes (2012) (Fig. 1). In each analysis, 5000 bootstrapped samples were used to generate upper and lower CIs for direct and indirect effects. As suggested by Baron and Kenny (1986), direct effect refers to the effect between the predictor and the outcome, net the effect of the mediator(s) in a model. Thus, direct effect refers to the association between gratitude and the subscale of FPI, controlling for the effects of spiritual disorientation and non-attachment. Indirect effect is the reduction of the effect from the predictor to the outcome after the influence of the mediator(s) is considered; in other words, how much of the association between the predictor and the outcome is explained by the mediator(s) in the model. Thus, indirect effect indicates the strength of the mediation. In this study, the indirect effect from spiritual disorientation indicates the extent to which the association between gratitude and the subscale of infertility-related stress is explained by the meaning pathway; while the indirect effect from non-attachment indicates the strength of the acceptance pathway. Complete mediation suggests that the mediator(s) in the model fully explain the association between the predictor (gratitude) and the outcome (FPI subscale). Incomplete mediation suggests that variables other than the proposed mediator(s) may explain the relationship between the predictor and the outcome, rendering the direct effect remains significant. A pair of 95% CIs which excludes zero indicates statistical significance at P-value of less than 0.05. Complete mediation is indicated by significant indirect effects and a non-significant direct effect, while partial mediation is indicated by significant indirect and direct effects. To reduce the risk of conceptual overlapping among predictors, women’s age, education, presence of religious affiliation, choice of current treatment (fresh embryo transfer or frozen embryo transfer), and frequencies of previous ART cycles were chosen as control variables in the MANOVA and all mediation analyses, including the moderated models. All analyses were based on complete cases, and cases with missing data were excluded from the analysis. All data were analysed by SPSS (version 26 for Windows; Chicago, IL, USA).
Results
A total of 808 eligible women were identified during the screening process, 314 of whom were excluded either as a duplicate case, meaning that the patient record system included duplicate records for the patient, or on one or more exclusion criteria. Of the 494 women who were approached, 357 (72.3%) provided informed consent and participated in the study.
Participants’ demographic and clinical characteristics are presented in Table I. The mean age of the women was 35.6 years. The mean age of their husbands was 40.2 years and the couples had been married for an average of 7 years. A total of 53.5% were suffering from primary infertility for an average duration of 4 years. Unexplained, female, male, and mixed causes were endorsed by 15.1%, 19.9%, 31.9%, and 10.4% of participants respectively. In total, 36.1% had previously undergone assisted reproduction treatment; the average duration from when participants received their first IVF cycle is 37 months.
Table I.
Demographic and clinical characteristics of participants (N = 357).
| Characteristics | n | % |
|---|---|---|
| Age of woman (years) | ||
| Mean/SD (range) | 35.6/2.9 (28–44) | |
| 30 or below | 19 | 5.3 |
| 31–35 | 146 | 40.9 |
| 36–40 | 177 | 49.6 |
| 40+ | 15 | 4.2 |
| Education | ||
| Secondary education or below | 143 | 40.1 |
| Tertiary education | 206 | 57.7 |
| Not available | 8 | 2.2 |
| Employment | ||
| Employed (Part-time) | 21 | 5.9 |
| Employed (Full-time) | 270 | 75.6 |
| Unemployed | 50 | 14.0 |
| Others | 7 | 2.0 |
| Not available | 9 | 2.5 |
| Religious affiliation | ||
| Yes | 136 | 38.1 |
| No | 195 | 54.6 |
| Not available | 26 | 7.3 |
| Age of husband (years) | ||
| Mean/SD (range) | 40.2/5.4 (30–72) | |
| 30–35 | 66 | 18.5 |
| 36–40 | 144 | 40.3 |
| 41–45 | 98 | 27.5 |
| 45+ | 49 | 13.7 |
| Duration of marriage (years) | ||
| Mean/SD (range) | 7.1/3.3 (0–19) | |
| 5 or below | 113 | 31.7 |
| 6–10 | 192 | 53.8 |
| 10+ | 52 | 14.6 |
| Duration of infertility (years) | ||
| Mean/SD (range) | 4.2/2.7 (0–25) | |
| Not available | 100 | 27.2 |
| Type of infertility | ||
| Primary | 191 | 53.5 |
| Secondary | 89 | 24.9 |
| Not available | 77 | 21.6 |
| No. of live births | ||
| 0 | 353 | 98.9 |
| 1 or more | 4 | 1.1 |
| Causes of infertility | ||
| Unexplained cause | 54 | 15.1 |
| Male factor | 114 | 31.9 |
| Female factor | 71 | 19.9 |
| Mixed factors | 37 | 10.4 |
| Not available | 81 | 22.7 |
| Duration of assisted reproduction (months) | ||
| Mean/SD (range) | 37.5/26.0 (0–120) | |
| Not available | 65 | 18.2 |
| No. of previous assisted reproduction cycles | ||
| Mean/SD (range) | 0.7/1.2 (0–8) | |
| 0 | 228 | 63.9 |
| 1 | 61 | 17.1 |
| 2 | 37 | 10.4 |
| 3 or more | 31 | 8.7 |
| Current treatment | ||
| Frozen-thawed embryo transfer | 73 | 20.4 |
| Fresh embryo transfer | 201 | 56.3 |
| Not available | 83 | 23.3 |
Descriptive statistics and correlations of key variables are presented in Table II. Gratitude was negatively correlated with loss of sense of meaning and all types of infertility-related stress, and positively related to acceptance. The magnitude of associations ranged from small to moderate. Loss of sense of meaning was negatively associated with acceptance, and positively with all FPI subscales. Similarly, acceptance was negatively associated with all FPI subscales. The results of MANCOVA showed that the presence of unexplained infertility was not associated with infertility-related stress, after controlling for age, education, presence of religious affiliation, current treatment, and previous ART, F(5, 214) = 1.505, P = 0.189. Using the same MANCOVA model, male factor infertility, which made up around one-third of the cases, was also not associated with infertility-related stress, F(5, 223) = 0.751, P = 0.586.
Table II.
Descriptive statistics and correlations of key variables.
| Variables | Mean | SD | Reliability (Cronbach\
 ) ) |
Correlations | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | ||||
| (1) Gratitude | 5.55 | 0.85 | 0.83 | −0.44 | 0.27 | −0.32 | −0.19 | −0.36 | −0.27 | −0.20 | −0.36 |
| (2) Loss of a sense of meaning | 3.20 | 1.66 | 0.74 | −0.56 | 0.56 | 0.35 | 0.36 | 0.28 | 0.43 | 0.54 | |
| (3) Acceptance | 5.95 | 1.80 | 0.89 | −0.55 | −0.38 | −0.22 | −0.29 | −0.38 | −0.50 | ||
| (4) Social concern | 29.65 | 7.99 | 0.80 | 0.51 | 0.43 | 0.45 | 0.56 | 0.81 | |||
| (5) Sexual concern | 22.10 | 7.07 | 0.82 | 0.45 | 0.28 | 0.44 | 0.73 | ||||
| (6) Relationship concern | 29.74 | 6.50 | 0.65 | 0.26 | 0.35 | 0.66 | |||||
| (7) Rejection of childfree lifestyle | 25.20 | 6.11 | 0.81 | 0.61 | 0.69 | ||||||
| (8) Need for parenthood | 36.50 | 8.00 | 0.82 | 0.81 | |||||||
| (9) Global stress | 142.93 | 27.01 | 0.83 | ||||||||
All correlations were significant at P < 0.05 (N = 343).
Table III indicates the direct and indirect effects of the mediation analyses. The acceptance and meaning pathways completely explained the link between gratitude and need for parenthood, social concerns, and sexual concerns. The meaning pathway, but not the acceptance pathway, mediated the link with relationship concerns, while the acceptance pathway, but not the meaning pathway, mediated the association with rejection of a childfree lifestyle. The relationships with global stress were mediated by both the acceptance and meaning pathways. Partial mediation was found for relationship concerns, rejection of a childfree lifestyle, and global stress as the direct effects remained significant.
Table III.
Results of mediation models (N = 250).
| Outcomes | Direct effects | Indirect effects via loss of a sense of meaning | Indirect effects via acceptance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | B | SE | LLCI | ULCI | |
| Social concern | −0.92 | 0.54 | −1.97 | 0.14 | −1.57 | 0.35 | −2.37 | −0.97 | −0.66 | 0.24 | −1.23 | −0.28 |
| Sexual concern | −0.38 | 0.53 | −1.42 | 0.67 | −0.95 | 0.31 | −1.64 | −0.42 | −0.53 | 0.23 | −1.09 | −0.17 |
| Relationship concern | −1.94 | 0.52 | −2.96 | −0.91 | −0.65 | 0.28 | −1.24 | −0.12 | −0.02 | 0.18 | −0.38 | 0.33 |
| Rejection of childfree lifestyle | −1.29 | 0.49 | −2.25 | −0.33 | −0.24 | 0.23 | −0.71 | 0.19 | −0.33 | 0.17 | −0.76 | −0.08 |
| Need for parenthood | −0.12 | 0.61 | −1.09 | 1.32 | −1.32 | 0.35 | −2.07 | −0.68 | −0.39 | 0.22 | −0.94 | −0.07 |
| Global stress | −4.40 | 1.82 | −7.99 | −0.82 | −4.73 | 1.11 | −7.23 | −2.84 | −1.93 | 0.76 | −3.77 | −0.70 |
B = unstandardized coefficient; LLCI = lower limit of 95% CI; ULCI = upper limit of 95% CI. A pair of 95% CIs which does not include a zero indicates statistical significance at P < 0.05 for the corresponding effect.
Lastly, we examined the moderation effects of unexplained infertility on the relationships between mediators (loss of sense of meaning and acceptance) and outcomes (infertility-related stress). The interaction effects with unexplained infertility were only found in the model with relationship concerns, but not with other subscales of infertility-related stress. Table IV presents the results of the model with relationship concerns. While the association of gratitude with relationship concerns remained negative and significant, unexplained infertility and loss of meaning were positively related to relationship concerns. Both interaction effects (unexplained infertility × loss of meaning, unexplained infertility × acceptance) were significant. According to the 95% CIs of the indirect effects, the meaning pathway significantly explained the links between gratitude and relationship concerns only among women who were not facing unexplained infertility. Among women who had unexplained infertility, only acceptance significantly mediated the relationships between gratitude and relationship concerns.
Table IV.
Unstandardized coefficients in the moderated mediation model with relationship concern as the outcome (N = 225).
| DV: Loss of a sense of meaning | DV: Acceptance | DV: Relationship concern | |
|---|---|---|---|
| Gratitude | −0.52 (0.07)*** | 0.46 (0.11)*** | −0.35 (0.09)*** |
| Age of woman | 0.08 (0.13) | −0.00 (0.20) | −0.06 (0.14) |
| Education | −0.51 (0.71) | −1.55 (1.08) | 0.00 (0.77) |
| Religious affiliation | −0.97 (0.76) | −0.31 (1.16) | 2.00 (0.82)* |
| Current treatment | −1.01 (0.96) | −0.72 (1.46) | 1.30 (1.03) |
| Frequency of previous assisted reproduction cycles | 0.76 (0.32)* | −0.37 (0.48) | −0.67 (0.34) |
| Unexplained infertility | 22.76 (6.62)*** | ||
| Loss of meaning | 0.35 (0.09)*** | ||
| Acceptance | 0.06 (0.06) | ||
| Unexplained infertility x loss of meaning | −0.75 (0.25)** | ||
| Unexplained infertility x acceptance | −0.37 (0.15) * | ||
| R2 | 0.28 | 0.09 | 0.25 |
| Bootstrapped 95% CIs | B (SE) [LLCI, ULCI] | ||
| Indirect effect of loss of meaning with unexplained infertility | 0.21 (0.15) [−0.07, 0.49] | ||
| Indirect effect of loss of meaning without unexplained infertility | −0.18 (0.06) [−0.31, −0.08] | ||
| Indirect effect of acceptance with unexplained infertility | −0.14 (0.08) [−0.33, −0.01] | ||
| Indirect effect of acceptance without unexplained infertility | 0.03 (0.03) [−0.03, 0.10] | ||
* P < 0.05, **P < 0.01, ***P < 0.001. B = unstandardized coefficient; A pair of 95% CIs which does not include a zero indicates statistical significance at P < 0.05 for the corresponding effect. SEs are in parentheses. DV: dependent variable.
Discussion
In view of the scarcity of studies on the role of personal strengths in coping with infertility, this study investigated the mechanisms by which gratitude reduces infertility-related stress and the moderating role of unexplained infertility among infertile women undergoing IVF. The associations between gratitude and lower need for parenthood, rejection of a childfree lifestyle, sexual, and social concerns were explained by participants’ acceptance of the life’s peaks and troughs. Greater sensitivity to the positive aspects of their life among women with high levels of gratitude may help them tolerate the status quo, perceive fewer flaws in their childfree life, establish new life goals, and experience lower levels of infertility-related stress (Thompson et al., 2011). Notably, heightened acceptance explained the negative relationship between gratitude and all subscales of FPI, except for relationship concerns, which reflects the well-being of the couple rather than of the participant alone. Pasch et al. (2002) found that wives perceived infertility as less harmful and experienced higher quality marital communications when their husbands showed greater willingness to discuss infertility-related issues. It is possible that a person’s acceptance of the status quo may not be sufficient to relieve their partner’s stress (Berghuis and Stanton, 2002), thereby subjecting them to relational repercussions brought about by infertility.
However, the meaning pathway explained the associations between gratitude and all FPI subscales but rejection of a childfree lifestyle. That is, individuals with greater gratitude have greater immunity from a lack of meaning, and therefore perceive their infertility as less stressful. Previous studies found that relational growth, refreshed views about parenthood and priorities in life, and enhanced confidence in handling social pressures often featured in couples’ accounts of their experience of infertility (Lee et al., 2009; Ying et al., 2015). Gratitude may provide an impetus to personal growth and encourage women to construct meanings from their experience of infertility. These, in turn, may relieve stress arising from relational, social, and life priorities domains (e.g. social, relationship, and sexual concerns, and need for parenthood). Apprehension about a certain way of living may not be readily resolved through attaining meaning for one’s failure to attain the desired lifestyle. Instead, it could be more closely related to whether one can accept the status quo, regardless of whether there is meaning to it. This may explain why loss of a sense of meaning did not mediate the effect on rejection of a childfree lifestyle.
Infertility-related stress was found to be comparable among both women with a definable cause of infertility and those with unexplained infertility. The extent to which acceptance and meaning explains the association between gratitude and relationship concerns, however, depended on the presence of a definable cause of infertility. Among women with unexplained infertility, the relationship between gratitude and relationship concerns was explained by the acceptance pathway. Among women with a definable cause for infertility, the relationship was explained by the meaning pathway. When a definable cause is present (female-, male-, or combined factor), the couple can attribute the cause of infertility to someone, interpret the situation from that vantage point, and begin to construct meaning out of this interpretation in order to handle relational conflicts. However, in the absence of a definable cause, interpretation of the situation becomes difficult, and there is often no way of determining any one attribution as ‘correct’. In fact, discrepancy in attributions among couples may even give rise to relational conflicts (Peterson et al., 2003). Accepting the uncertainty and ambiguity of their infertility is the only way for the couple to move forward and attain personal and relational growth in their shared trauma. In contrast with coping with other domains of infertility-related stress, relationship concerns may be more sensitive to how the cause of infertility is attributed. The attribution of responsibility directly influences how and for what the spouse is appreciated or blamed. In studies on male infertility, many husbands who were interviewed were appreciative of the sacrifices made by their wife in undergoing invasive medical treatment to fulfil their shared dreams. At the same time, these husbands felt helpless seeing their wife suffering during treatment because of their physiological problems (Johansson et al., 2011; Schick et al., 2016). In negotiating relational issues, couples facing unexplained infertility cannot take advantage of the additional information about who is biologically responsible for their infertility to resolve conflicts or induce appreciation; all they can rely on, instead, is to embrace the unexplainable.
Implications
The systematic review by Rockliff et al. (2014) highlighted the imbalance in understanding the risk versus protective factors of psychological distress in infertility and fertility treatment, with many more studies on the former than the latter. Increasingly, studies have found interventions based on enhancing character strengths (e.g. gratitude intervention, forgiveness intervention, personal growth, instilling hope, and a combination of intervention components) efficacious in fostering psychosocial adjustment among infertile women undergoing IVF (e.g. Chan et al., 2012; Domar et al., 2015). Many of these interventions can be easily adapted into self-administered format in order to facilitate patient convenience, especially during treatment and the waiting period before a pregnancy test. For instance, Domar et al. (2015) combined the Positive Reappraisal Coping Invention (PRCI) model with a mind–body exercise programme to construct a multicomponent self-help intervention for women undergoing IVF (Domar et al., 2015). While the PRCI utilizes instructions to induce positive reframing in its users, the element of acceptance and ‘letting go’ is less obvious. Peterson and Eifert (2011) have shown that cultivating non-judgmental acceptance may assist couples adapt to long-term infertility.
Gratitude, despite being a disposition, is amenable to change through interventions and daily practise (Emmons and Stern, 2013). Our findings suggest that gratitude intervention may foster meaning construction and acceptance for maximizing the benefits for women undergoing IVF. Gratitude interventions commonly take the form of daily or weekly gratitude journaling, gratitude letter (and visit), journaling about something good that happened or will happen, or gratitude journaling coupled with mental imagery. Most of these interventions involve brief activities performed several times a week. In a seminal article about gratitude intervention, Emmons and McCullough (2003) asked participants to list up to five things for which they were grateful, and found that compared to control groups (listing hassles and neutral events), the gratitude-outlook group experienced more positive mood, fewer physical symptoms, more health-enhancing behaviours, and prosocial behaviours as well as more optimistic appraisals of life. Lambert et al. (2009) found that daily prayer for 4 weeks increased their participants’ gratitude. Emmons and Stern (2013) also discussed the potential of focusing and mindfulness techniques in enhancing attention to various positive things in life, and therefore training a grateful mindset.
Requiring merely several minutes daily for practise, gratitude interventions can be recommended to patients even early on when they are still considering treatment or have just begun their treatment. The short duration required for practise could render gratitude intervention a feasible and attractive means of preparing individuals psychologically for the upcoming ART. Gratitude interventions may facilitate psychological resource building by enhancing individuals’ sense of meaning and perceived social support and prepare them for the psychologically demanding treatment. With limited logistical requirements, gratitude interventions can be easily adapted to a self-help format and facilitate adjustments among women while waiting for a pregnancy test following embryo transfer. Deriving meaning and acceptance from a failed IVF experience has been shown to facilitate adjustment in couples (Lee et al., 2009). Thus, gratitude interventions may also be used for enhancing meaning reconstruction and acceptance of a failed cycle. Future interventions may consider supplementing the well-validated psychological interventions with practises of gratitude and acceptance to reduce multiple dimensions of infertility stress, and compare the efficacy of gratitude interventions at different stages of IVF treatment.
Gratitude has been lauded as a well-being enhancing and prosocial virtue in a number of major philosophical-religious traditions (Emmons and Crumpler, 2000). Its effect on psychological well-being has been replicated in a wide range of socio-cultural contexts. Sense of meaning and acceptance have also been found to facilitate adjustment in infertility in a number of socio-cultural backgrounds (Lee et al., 2009; Peterson and Eifert, 2011). With almost no research on cross-cultural comparisons of the role of gratitude in infertility, it is difficult to quantify the role of Chinese-specific factors in the current findings. Instead, we take a more conservative stance and call for future studies to investigate the role of gratitude and other character strengths in adapting to infertility using cross-cultural methodologies.
Paul et al. (2009) found that post-traumatic growth is less likely among couples confronting unexplained infertility and remarked that these couples may experience greater alienation and confusion compared to their counterparts with a ‘viable’ cause of infertility. Our findings highlight the intricate differences in the coping process among women facing unexplained infertility compared to those with a diagnosed cause, although the two groups did not differ on the severity of their infertility-related stress. We also found that the differences in coping appeared to be specific to dealing with relationship concerns. Although the associations between infertility diagnosis and well-being outcomes remain inconclusive, healthcare professionals should be sensitive to the possible impact of the absence of a diagnosed cause on the couple’s distress and be mindful of whether this factor complicates their relationship issues.
Limitations
The findings of this study should be considered with the following limitations. First, this is a cross-sectional dataset, which may preclude the inferences of direction of causality. Second, our participants were enrolled in a randomized controlled trial for a self-help mind–body intervention aiming to relieve anxiety during the waiting period between embryo transfer and a pregnancy test. Thus, the study findings may not be readily generalizable to women with no intention or interest in receiving psychosocial support. Caution should also be taken in generalizing our findings to infertile women who are not receiving or have no intention to undergo ART, as both the source and magnitude of their infertility-related stress could be different. We examined only the coping process among infertile women. Future studies may take a dyadic approach to explore the interactions of character strength, coping styles and outcomes in infertile couples.
Conclusion
In response to the call for balancing the deficit-based view with a strength-based orientation in understanding how women cope with infertility and fertility treatment, our study investigated the role of gratitude in relieving multidimensional infertility-related stress. We found that gratitude was negatively associated with all dimensions of infertility-related stress, and the relationships were mediated by acceptance and loss of a sense of meaning. Further, we found the mediation pathways between gratitude and relationship concerns differed for women with a definable cause of their infertility and those with unexplained infertility.
Authors’ roles
MYJT, EHYN, CLWC and CHYC designed the study. MYJT, SYH, and BHPL conducted the data collection and data analysis. The first draft of the manuscript was written up by BHPL and SYH. All authors contributed critically to the subsequent drafts and approved its submission.
Funding
Hong Kong University Grant Council—General Research Fund (HKU27400414).
Conflict of interest
None to declare.
References
- Algoe SB. Find, remind, and bind: the functions of gratitude in everyday relationships. Soc Pers Psychol Compass 2012;6:455–469. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- Berghuis JP, Stanton AL. Adjustment to a dyadic stressor: a longitudinal study of coping and depressive symptoms in infertile couples over an insemination attempt. J Consult Clin Psychol 2002;70:433–438. [DOI] [PubMed] [Google Scholar]
- Chan CHY, Chan THY, Chan CLW. Translating Daoist concepts into integrative social work practice: an empowerment program for persons with depressive symptoms. J Relig Spiritual Soc Work. 2014a;33:61–72. [Google Scholar]
- Chan CHY, Chan THY, Chan CLW, Ng EHY, Ho PC. Diagnostic ambiguity and psychosocial distress among Chinese women with idiopathic and non-idiopathic infertility. Illn Crisis Loss 2015;23:45–58. [Google Scholar]
- Chan CHY, Chan THY, Leung PPY, Brenner MJ, Wong VPY, Leung EKT, Wang X, Lee MY, Chan JSM, Chan CLW. Rethinking well-being in terms of affliction and equanimity: development of a Holistic Well-Being Scale. J Ethn Cult Divers Soc Work 2014b;23:289–308. [Google Scholar]
- Chan CHY, Chan CLW, Ng EHY, Ho PC, Chan THY, Lee GL, Hui WHC. Incorporating spirituality in psychosocial group intervention for women undergoing in vitro fertilization: a prospective randomized controlled study. Psychol Psychother 2012;85:356–373. [DOI] [PubMed] [Google Scholar]
- DeWall CN, Lambert NM, Pond RS Jr, Kashdan TB, Fincham FD. A grateful heart is a nonviolent heart: cross-sectional, experience sampling, longitudinal, and experimental evidence. Soc Psychol Personal Sci 2012;3:232–240. [Google Scholar]
- Domar AD, Gross J, Rooney K, Boivin J. Exploratory randomized trial on the effect of a brief psychological intervention on emotions, quality of life, discontinuation, and pregnancy rates in in vitro fertilization patients. Fertil Steril 2015;104:440–451. [DOI] [PubMed] [Google Scholar]
- Emmons RA, Crumpler CA. Gratitude as a human strength: appraising the evidence. J Soc Clin Psychol 2000;19:56–69. [Google Scholar]
- Emmons RA, McCullough ME. Counting blessings versus burdens: an experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol 2003;84:377–389. [DOI] [PubMed] [Google Scholar]
- Emmons RA, Stern R. Gratitude as psychotherapeutic intervention. J Clin Psychol 2013;69:846–855. [DOI] [PubMed] [Google Scholar]
- Galhardo A, Cunha M, Pinto-Gouveia J, Matos M. The mediator role of emotion regulation processes on infertility-related stress. J Clin Psychol Med Settings 2013;20:497–507. [DOI] [PubMed] [Google Scholar]
- Gameiro S, Boivin J, Dancet E, de Klerk C, Emery M, Lewis-Jones C, Thorn P, Van den Broeck U, Venetis C, Verhaak CM et al. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction—a guide for fertility staff. Hum Reprod 2015;30:2476–2485. [DOI] [PubMed] [Google Scholar]
- Habroe M, Schmidt L, Evald Holstein B. Does childbirth after fertility treatment influence sense of coherence? A longitudinal study of 1,934 men and women. Acta Obstet Gynecol Scand 2007;86:1215–1221. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. University of Kansas, Kansas2012.
- Herrmann D, Scherg H, Verres R, von Hagens C, Strowitzki T, Wischmann T. Resilience in infertile couples acts as a protective factor against infertility-specific distress and impaired quality of life. J Assist Reprod Genet 2011;28:1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji XW, Chan CHY, Lau BHP, Chan JSM, Chan CLW, Chung KF. The interrelationship between sleep and depression: a secondary analysis of a randomized controlled trial on integrative mind-body-spirit intervention. Sleep Med 2017;2:41–46. [DOI] [PubMed] [Google Scholar]
- Johansson M, Hellstrom A-L, Berg M. Severe male infertility after failed ICSI treatment—a phemenological study of men’s experiences. Reprod Health 2011;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert NM, Fincham FD, Braithwaite SR, Graham SM, Beach SR. Can prayer increase gratitude. Psycholog Relig Sipritual 2009;1:139. [Google Scholar]
- Lambert NM, Fincham FD, Stillman TF. Gratitude and depressive symptoms: the role of positive reframing and positive emotion. Cogn Emot 2012;26:615–633. [DOI] [PubMed] [Google Scholar]
- Lancastle D, Boivin J. Dispositional optimism, trait anxiety, and coping: unique or shared effects on biological response to fertility treatment. Health Psychol 2005;24:171–178. [DOI] [PubMed] [Google Scholar]
- Lau BHP, Cheng C. Gratitude and coping among familial caregivers of persons with dementia. Aging Ment Health 2017;21:445–453. [DOI] [PubMed] [Google Scholar]
- Lau BHP, Chow AYM, Wong DFK, Chan JSM, Chan CHY, Ho RTH, So TH, Lam TC, Lee VHF, Lee AWM et al. Study protocol of a randomized controlled trial comparing integrative body-mind-spirit intervention and cognitive behavioural therapy in fostering quality of life of patients with lung Cancer and their family caregivers. J Evid Inf Soc Work 2018;15:258–276. [DOI] [PubMed] [Google Scholar]
- Lee GL, Hui Choi WH, Chan CHY, Chan CLW, Ng EHY. Life after unsuccessful IVF treatment in an assisted reproduction unit: a qualitative analysis of gains through loss among Chinese persons in Hong Kong. Hum Reprod 2009;24:1920–1929. [DOI] [PubMed] [Google Scholar]
- Lee T-Y, Sun G-H, Chao S-C. The effect of an infertility diagnosis on the distress, marital and sexual satisfaction between husbands and wives in Taiwan. Hum Reprod 2001;16:1762–1767. [DOI] [PubMed] [Google Scholar]
- Liao KYH, Weng CY. Gratefulness and subjective well-being: social connectedness and presence of meaning as mediators. J Couns Psychol 2018;65:383–393. [DOI] [PubMed] [Google Scholar]
- Mahajan NN, Turnbull DA, Davies MJ, Jindal UN, Briggs NE, Taplin JE. Changes in affect and state anxiety across an in vitro fertilization/intracytoplasmic sperm injection cycle. Fertil Steril 2010;93:517–526. [DOI] [PubMed] [Google Scholar]
- McCullough ME, Emmons RA, Tsang J-A. The grateful disposition: a conceptual and empirical topography. J Pers Soc Psychol 2002;82:112–127. [DOI] [PubMed] [Google Scholar]
- McCullough ME, Tsang J-A, Emmons RA. Gratitude in intermediate affective terrain: links of grateful moods to individual differences and daily emotional experience. J Pers Soc Psychol 2004;86:295–309. [DOI] [PubMed] [Google Scholar]
- Newton CR, Sherrard W, Glavac I. The fertility problem inventory: measuring perceived infertility-related stress. Fertil Steril 1999;72:54–62. [DOI] [PubMed] [Google Scholar]
- Pasch LA, Dunkel-Schetter C, Christensen A. Differences between husbands’ and wives’ approach to infertility affect marital communication and adjustment. Fertil Steril 2002;77:1241–1247. [DOI] [PubMed] [Google Scholar]
- Paul MS, Berger R, Berlow N, Rovner-Ferguson H, Figlerski L, Gardner S, Malave AF. Posttraumatic growth and social support in individuals with infertility. Hum Reprod 2009;25:133–141. [DOI] [PubMed] [Google Scholar]
- Peterson BD, Eifert GH. Using acceptance and commitment therapy to treat infertility stress. Cogn Behav Pract 2011;18:577–587. [Google Scholar]
- Peterson BD, Newton CR, Rosen KH. Examining congruence between partners' perceived infertility-related stress and its relationship to marital adjustment and depression in infertile couples. Fam Process 2003;42:59–71. [DOI] [PubMed] [Google Scholar]
- Rapoport-Hubschman N, Gidron Y, Reicher-Atir R, Sapir O, Fisch B. “Letting go” coping is associated with successful IVF treatment outcome. Fertil Steril 2009;92:1384–1388. [DOI] [PubMed] [Google Scholar]
- Raque-Bogdan TL, Hoffman MA. The relationship among infertility, self-compassion, and well-being for women with primary or secondary infertility. Psychol Women Q 2015;39:484–496. [Google Scholar]
- Rockliff HE, Lightman SL, Rhidian E, Buchanan H, Gordon U, Vedhara K. A systematic review of psychosocial factors associated with emotional adjustment in in vitro fertilization patients. Hum Reprod Update 2014;20:594–613. [DOI] [PubMed] [Google Scholar]
- Romano GA, Ravid H, Zaig I, Schreiber S, Azem F, Shachar I, Bloch M. The psychological profile and affective response of women diagnosed with unexplained infertility undergoing in vitro fertilization. Arch Womens Ment Health 2012;15:403–411. [DOI] [PubMed] [Google Scholar]
- Ruini C, Vescovelli F. The role of gratitude in breast cancer: its relationships with post-traumatic growth, psychological well-being and distress. J Happiness Stud 2013;14:263–274. [Google Scholar]
- Sadeghi MR. Unexplained infertility, the controversial matter in management of infertile couples. J Reprod Infertil 2015;16:1–2. [PMC free article] [PubMed] [Google Scholar]
- Schick M, Rosner S, Toth B, Strowitzki T, Wischmann T. Exploring involuntary childlessness in men—a qualitative study assessing quality of life, role aspects, and control beliefs in men’s perception of the fertility treatment process. Hum Fertil 2016;19:32–42. [DOI] [PubMed] [Google Scholar]
- Schmidt L, Holstein B, Christensen U, Boivin J. Does infertility cause marital benefit? An epidemiological study of 2250 women and men in fertility treatment. Patient Educ Couns 2005;59:244–251. [DOI] [PubMed] [Google Scholar]
- Thompson EH, Woodward JT, Stanton AL. Moving forward during major goal blockage: situational goal adjustment in women facing infertility. J Behav Med 2011;34:275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhaak CM, Smeenk J, Evers A, Kremer JA, Kraaimaat F, Braat D. Women’s emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update 2006;13:27–36. [DOI] [PubMed] [Google Scholar]
- Wood AM, Maltby J, Stewart N, Linley PA, Joseph S. A social-cognitive model of trait and state levels of gratitude. Emotion 2008;8:281–290. [DOI] [PubMed] [Google Scholar]
- Ying LY, Wu LH, Loke AY. The experience of Chinese couples undergoing in vitro fertilization treatment: perception of the treatment process and partner support. PloS One 2015;10:e0139691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y, Peng L, Chen L, Long L, He W, Li M, Wang T. Resilience and social support promote posttraumatic growth of women with infertility: the mediating role of positive coping. Psychiatry Res 2014;215:401–405. [DOI] [PubMed] [Google Scholar]


