Abstract
Background
To summarize the four recent sodium-glucose cotransporter 2 inhibitor (SGLT2i) trials: Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE), and explore the potential determinants for their cardiovascular, renal, and safety outcomes.
Results
The composite renal outcome event rates per 1000 patient-years for drug and placebo, as well as the corresponding relative risk reductions, were 3.7, 7.0, 47%; 5.5, 9.0, 40%; 6.3, 11.5, 46%; 43.2, 61.2, 30% for DECLARE-TIMI 58, CANVAS, EMPA–REG OUTCOME, and CREDENCE, respectively (event definitions varied across trials). The major adverse cardiovascular (CV) event rates per 1000 patient-years for drug and placebo, as well as the corresponding relative risk reductions, were 22.6, 24.2, 7%; 26.9, 31.5, 14%; 37.4, 43.9, 14%; 38.7, 48.7, 20% for DECLARE-TIMI 58, CANVAS, EMPA–REG OUTCOME, and CREDENCE, respectively. DECLARE-TIMI 58 had the fewest cardiorenal events and CREDENCE the most. These differences were presumably due to varying inclusion criteria resulting in DECLARE-TIMI 58 having the best baseline renal filtration function and CREDENCE the worst (mean estimated glomerular filtration rate 85.2, 76.5, 74, 56.2 mL/min/1.73 m2 for DECLARE-TIMI 58, CANVAS, EMPA–REG OUTCOME, and CREDENCE, respectively). Additionally, CREDENCE had considerably higher rates of albuminuria (median urinary albumin-creatinine ratios (UACR) were 927, 12.3, and 13.1 mg/g for CREDENCE, CANVAS, and DECLARE-TIMI 58, respectively; EMPA–REG OUTCOME had 59.4% UACR < 30, 28.6% UACR > 30–300, 11.0% UACR > 300 mg/g).
Conclusions
Dapagliflozin, empagliflozin, and canagliflozin have internally and externally consistent and biologically plausible class effects on cardiorenal outcomes. Baseline renal filtration function and degree of albuminuria are the most significant indicators of risk for both CV and renal events. Thus, these two factors also anticipate the greatest clinical benefit for SGLT2i.
Keywords: SGLT2 inhibitor, Empagliflozin, Canagliflozin, Dapagliflozin, CANVAS, EMPA–REG OUTCOME, DECLARE-TIMI 58, CREDENCE, Cardiovascular outcome trials, Heart failure hospitalization, Cardiovascular death, Albuminuria, Estimated glomerular filtration function, Chronic kidney disease, End-stage renal disease, Mortality
Background
Type 2 diabetes mellitus (T2DM) is significantly associated with cardiovascular disease (CVD) and is a risk factor for heart failure (HF); diabetic patients are hospitalized for HF approximately four times more frequently than nondiabetic patients [1–5]. T2DM is a risk factor for chronic kidney disease (CKD) and end-stage renal disease (ESRD) [6, 7]. T2DM is also associated with non-healing lower extremity wounds, deep tissue osteomyelitis, metabolic bone disease, anemia, pancreatitis, and diabetic ketoacidosis [8–10]. Further, T2DM medications often have deleterious side effects. Thiazolidinediones are linked to edema, HF hospitalization (HHF) and cardiovascular (CV) death in certain patient subsets [11–13]. Oral sulfonylureas are associated with hypoglycemia, myocardial infarction (MI), stroke, and CV death, although a recent intervention trial found that sulfonylureas had similar rates of CV events compared to pioglitazone (1.5/100 patient-years for both groups, hazard ratio (HR) = 0.96, 95% confidence interval (CI) 0.74–1.26, p = 0.79) [14–16].
The 2008 United States Food and Drug Administration (FDA) antidiabetic drug guidance required cardiovascular outcome trials (CVOTs) for novel antihyperglycemic medications to demonstrate that new drugs would not increase the risk for MI, stroke, or CV death [17]. The FDA has approved four sodium-glucose cotransporter 2 inhibitors (SGLT2i) based on these guidelines: canagliflozin (Invokana), dapagliflozin (Farxiga), empagliflozin (Jardiance), and ertugliflozin (Steglatro). A fifth SGLT2i, sotagliflozin (Zynquista), is in late clinical development. Multiple expert consensus decisions attest to the potential of SGLT2i as a promising new class for the treatment of patients with T2DM and established CVD [18, 19].
Three SGLT2i (canagliflozin, empagliflozin, dapagliflozin) have been studied in CVOTs; canagliflozin has also been studied in an additional randomized clinical trial involving patients with diabetic kidney disease [20–23]. This review will explore the design and results of each of the four key SGLT2i trials and discuss the potential determinants for their CV, renal, and safety outcomes.
Methods
We reviewed the relevant trials’ original methodology and results papers. The methodological details and outcomes of the trials will be reviewed in the Results section below. As some p-values were not provided in all trials, we calculated them from the HR and 95% CI [24]. We calculated the relative risk reduction percentages from the HR. Continuous variables are presented as mean ± standard deviation or median [quartile 1, quartile 3], if skewed. Categorical variables are presented as frequency (%).
Results
The EMPA–REG OUTCOME Trial
The first SGLT2i CVOT, the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose randomized double-blind controlled trial (EMPA–REG OUTCOME) assigned 7020 patients with T2DM and CVD to 10 mg or 25 mg of empagliflozin or placebo daily over a 3.1 year mean and median follow-up period [20, 25]. Study patients were required to have estimated glomerular filtration rate (eGFR) > 30 mL/min/1.73 m2 [calculated using the Modification of Diet in Renal Disease (MDRD) equation]; empagliflozin is indicated for T2DM patients with eGFR ≥ 45 mL/min/1.73 m2 [26].
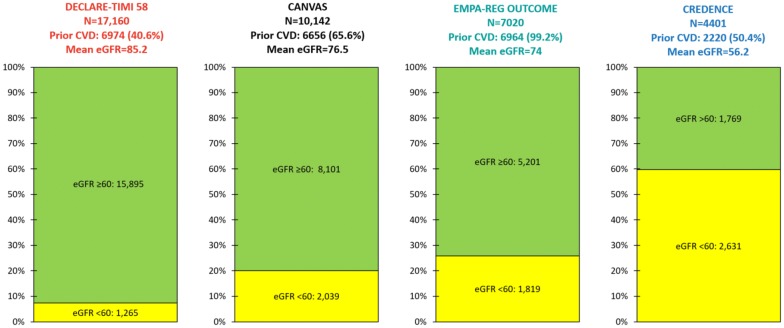
Nearly all [6964 (99.2%)] EMPA–REG OUTCOME patients had established CVD, most commonly stable coronary artery disease (Fig. 1). The mean eGFR was 74 ± 21 mL/min/1.73 m2, 1819 (25.9%) patients had eGFR < 60 mL/min/1.73 m2, and 5201 (74.1%) had eGFR > 60 mL/min/1.73 m2 [20, 27]. There were 4171 (59.4%) patients with urinary albumin-creatinine ratio (UACR) < 30 mg/g, 2013 (28.7%) with UACR > 30–300 mg/g, and 769 (11.0%) with UACR > 300 mg/g. Although angiotensin-converting-enzyme inhibitor (ACEi) or angiotensin-receptor blocker (ARB) use was not required, they were used in 5666 (80.7%) patients.
Fig. 1.
Baseline estimated glomerular filtration rates (eGFRs) and prior cardiovascular disease (CVD) rates in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Prior CVD displayed as incidence (percentage)
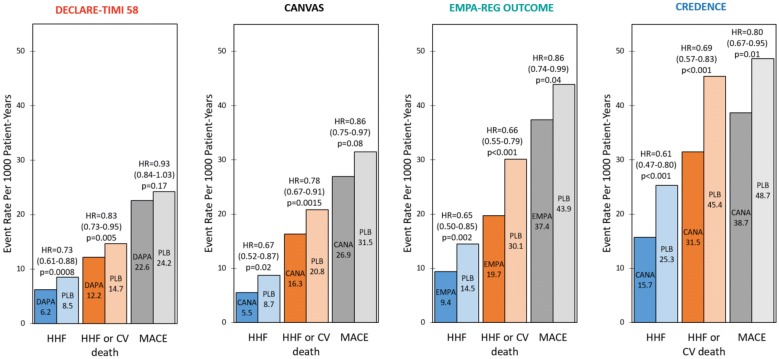
The primary composite CV endpoint (CV death, nonfatal MI, or nonfatal stroke) occurred in 10.5% of empagliflozin patients compared to 12.1% of placebo patients (rate per 1000 patient-years = 37.4 vs. 43.9, respectively; HR = 0.86, 95% CI 0.74–0.99, p = 0.04) (Fig. 2). With regard to secondary outcomes, HHF occurred in 2.7% of empagliflozin patients compared to 4.1% of placebo patients (rate per 1000 patient-years = 9.4 vs. 14.5, HR = 0.65, 95% CI 0.50–0.85, p = 0.002). HHF or CV death (excluding fatal stroke) occurred in 5.7% of empagliflozin patients compared to 8.5% of placebo patients (rate per 1000 patient-years = 19.7 vs. 30.1, HR = 0.66, 95% CI 0.55–0.79, p < 0.001). The composite renal outcome [doubling of serum creatinine level accompanied by an eGFR ≤ 45 mL/min/1.73 m2, initiation of renal-replacement therapy (RRT), or renal death] occurred in 1.7% of empagliflozin patients compared to 3.1% of placebo patients (rate per 1000 patient-years = 6.3 vs. 11.5, HR = 0.54, 95% CI 0.40–0.75, p < 0.001) (Fig. 3) [28].
Fig. 2.
Heart failure hospitalization (HHF), HHF and cardiovascular (CV) death, and major adverse cardiovascular event (MACE) event rates per 1000 patients in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Statistical outcomes displayed as hazard ratio, 95% confidence interval, p-value. HR hazard ratio, DAPA dapagliflozin, CANA canagliflozin, EMPA empagliflozin, PLB placebo
Fig. 3.
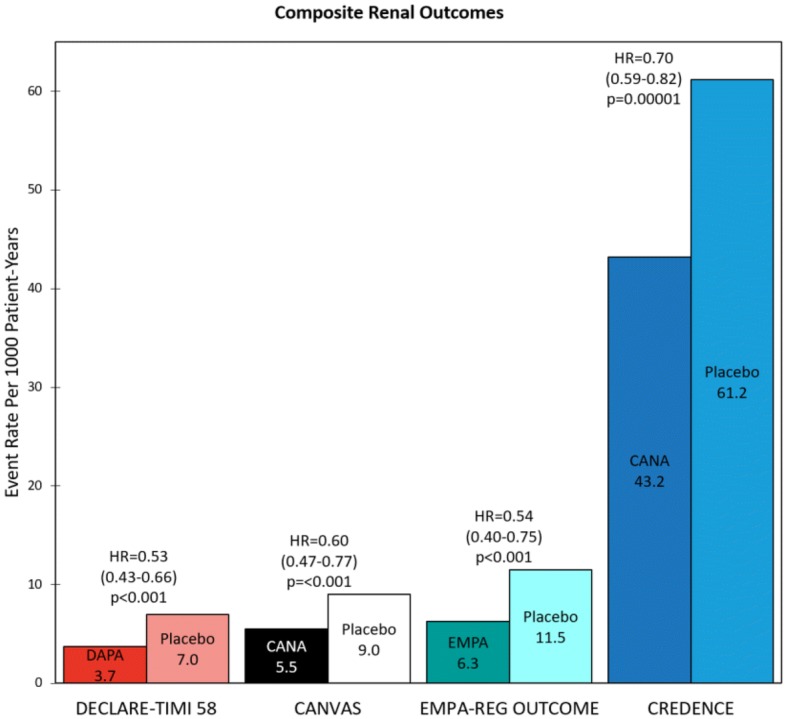
Composite renal outcome rates in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Statistical outcomes displayed as hazard ratio, 95% confidence interval, p-value. Composite renal outcomes defined as follows: DECLARE-TIMI 58: ≥ 40% reduction in estimated glomerular filtration rate (eGFR) to < 60, end-stage renal disease (ESRD) (dialysis ≥ 90 days, transplant or sustained eGFR < 15), or renal/cardiovascular (CV) death; CANVAS: ≥ 40% reduction in eGFR, renal-replacement therapy (RRT) (transplant, chronic dialysis, or sustained eGFR < 15), or renal death; EMPA–REG OUTCOME: doubling of serum creatinine (Cr) with eGFR ≤ 45, RRT, or renal death; CREDENCE: doubling of serum Cr, ESRD (eGFR < 15, dialysis, or renal transplant), renal/CV death. HR hazard ratio, DAPA dapagliflozin, CANA canagliflozin, EMPA empagliflozin
The CANVAS program
The second SGLT2i CVOT, the CANagliflozin CardioVascular Assessment Study (CANVAS) Program combined the CANVAS and CANVAS-Renal (CANVAS-R) study cohorts into a randomized double-blind controlled trial, assigning 10,142 T2DM patients to daily canagliflozin (100 mg with optional increase to 300 mg) or placebo over a 2.4 year median (188.2 week mean) follow-up period [21, 29]. Patients were required to be ≥ 30 years old with established CVD or ≥ 50 years with at least 2 CVD risk factors. Study patients were required to have eGFR > 30 mL/min/1.73 m2 (calculated using the MDRD equation); canagliflozin is indicated for T2DM patients with eGFR ≥ 45 mL/min/1.73 m2 and contraindicated for patients with eGFR < 30 mL/min/1.73 m2 [30].
A total of 6656 (65.6%) CANVAS Program patients had established CVD, most commonly stable coronary artery disease (Fig. 1). The mean eGFR was 76.5 ± 20.5 mL/min/1.73 m2, 2039 (20.1%) patients had eGFR < 60, and 8101 (79.9%) had eGFR > 60 mL/min/1.73 m2 [21, 31]. The median UACR was 12.3 [6.65, 42.1] mg/g; 7007 (69.8%) patients had UACR < 30 mg/g, 2266 (22.6%) had UACR > 30–300 mg/g, and 760 (7.6%) had UACR > 300 mg/g. Although antihypertensive agent use was not required, patients receiving these drugs were required to have a documented systolic blood pressure higher than 140 mm Hg. Renin-angiotensin-aldosterone system inhibitor (RAASi) use was not required; however, they were used in 8116 (80.0%) patients.
The primary composite CV endpoint (CV death, nonfatal MI, or nonfatal stroke) rate per 1000 patient-years was 26.9 for canagliflozin patients compared to 31.5 for placebo patients (HR = 0.86, 95% CI 0.75–0.97, p = 0.08) (Fig. 2). With regard to secondary outcomes, the HHF rate per 1000 patient-years was 5.5 for canagliflozin patients compared to 8.7 for placebo patients (HR = 0.67, 95% CI 0.52–0.87, p = 0.02). The HHF or CV death rate per 1000 patient-years was 16.3 for canagliflozin patients compared to 20.8 for placebo patients (HR = 0.78, 95% CI 0.67–0.91, p = 0.0015). The composite renal outcome [40% reduction in eGFR sustained for at least two consecutive measures, need for RRT (chronic dialysis, sustained eGFR < 15 mL/min/1.73 m2, or kidney transplantation), or renal death] rate per 1000 patient-years was 5.5 in empagliflozin patients compared to 9.0 in placebo patients (HR = 0.6, 95% CI 0.47–0.77, p < 0.001) (Fig. 3) [21].
The DECLARE-TIMI 58 trial
The third and most recent SGLT2i CVOT, the Dapagliflozin Effect on CardiovascuLAR Events randomized double-blind controlled trial (DECLARE-TIMI 58) assigned 17,160 T2DM patients to 10 mg of dapagliflozin daily or placebo over a median 4.2 [3.9, 4.4] year follow-up period [22]. Males ≥ 55 years or females ≥ 60 years with ≥ 1 CVD risk factor were included in the trial. Study patients were required to have creatinine clearance (CrCl) ≥ 60 mL/min with no specified minimum eGFR [32]. Dapagliflozin is indicated for T2DM patients with eGFR ≥ 45 mL/min/1.73 m2 (initially eGFR ≥ 60 but updated to 45 in March 2019) and contraindicated for patients with eGFR < 30 mL/min/1.73 m2 [33, 34]. Investigators used the Cockroft-Gault equation to calculate CrCl for the exclusion criteria and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation to calculate eGFR when reporting the composite renal outcomes.
In DECLARE-TIMI 58, 6974 (40.6%) patients had established CVD, most commonly stable coronary disease (Fig. 1). The mean eGFR was 85.2 mL/min/1.73 m2, 1265 (7.4%) patients had eGFR < 60, and 15,895 (92.6%) had eGFR > 60 mL/min/1.73 m2. The median UACR was 13.1 [6.0, 43.6] mg/g; 11,652 (67.9%) patients had UACR < 30 mg/g, 4023 (23.4%) had UACR > 30–300 mg/g, and 1169 (6.8%) had UACR > 300 mg/g. Although ACEi/ARB use was not required, they were used in 13,950 (81.3%) patients.
The primary composite CV endpoint (CV death, nonfatal MI, or nonfatal stroke) occurred in 8.8% of dapagliflozin patients compared to 9.4% of placebo patients (rate per 1000 patient-years = 22.6 vs. 24.2, HR = 0.93, 95% CI 0.84–1.03, p = 0.17) (Fig. 2). With regard to secondary outcomes, HHF occurred in 2.5% of dapagliflozin patients compared to 3.3% of placebo patients (rate per 1000 patient-years = 6.2 vs. 8.5, HR = 0.73, 95% CI 0.61–0.88, p = 0.0008). HHF or CV death occurred in 4.9% of dapagliflozin patients compared to 5.8% of placebo patients (rate per 1000 patient-years = 12.2 vs. 14.7, HR = 0.83, 95% CI 0.73–0.95, p = 0.005). The composite renal outcome [≥ 40% reduction in eGFR to a threshold < 60 mL/min/1.73 m2, ESRD (dialysis ≥ 90 days, sustained eGFR < 15 mL/min/1.73 m2, or kidney transplantation), or renal/CV death] occurred in 1.5% of dapagliflozin patients compared to 2.8% of placebo patients (rate per 1000 patient-years = 3.7 vs. 7, HR = 0.53, 95% CI 0.43–0.66, p < 0.001) (Fig. 3) [22].
The CREDENCE trial
The Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation randomized double-blind controlled trial (CREDENCE) assigned 4401 patients with T2DM and CKD to 100 mg of canagliflozin or placebo daily over a 2.62 year median follow-up period [23]. Study patients were required to have eGFR between 30 and 90 mL/min/1.73 m2 (calculated using the CKD-EPI equation) and investigators planned to include ~ 60% of patients with eGFR between 30 and 60 mL/min/1.73 m2. Additionally, patients were required to have albuminuria, defined as UACR > 300–5000 mg/g. Patients were not required to have prior CVD. Notably, the trial was stopped early as it met the pre-specified efficacy criteria for premature cessation.
In CREDENCE, 2220 (50.4%) patients had established CVD and ~ 16% had a baseline history of HF (Fig. 1). The mean eGFR was 56.2 ± 18.2 mL/min/1.73 m2, 2631 (59.8%) patients had eGFR < 60 mL/min/1.73 m2, and 1769 (40.2%) had eGFR > 60 mL/min/1.73 m2. In striking contrast to the three CVOT trials, the median UACR was 927 [463, 1833] mg/g; 31 (0.7%) patients had UACR < 30 mg/g, 496 (11.3%) had UACR > 30–300 mg/g, 3371 (76.6%) had UACR > 300–3000 mg/g, and 503 (11.4%) had UACR > 3000 mg/g. Stable ACEi/ARB use was required for ≥ 4 weeks prior to randomization and RAASi were used in 4395 (99.9%) patients.
The primary composite renal endpoint [doubling of serum creatinine from baseline (sustained for at least 30 days), ESRD (dialysis, renal transplantation, or sustained eGFR < 15 mL/min/1.73 m2), or renal/CV death] occurred in 11.1% of canagliflozin patients compared to 15.4% of placebo patients (rate per 1000 patient-years = 43.2 vs. 61.2, respectively; HR = 0.70, 95% CI 0.59–0.82, p = 0.00001) (Fig. 3). With regard to secondary outcomes, the composite CV outcome (CV death, nonfatal MI, or nonfatal stroke) occurred in 9.9% of canagliflozin patients compared to 12.2% of placebo patients (rate per 1000 patient-years = 38.7 vs. 48.7, HR = 0.80, 95% CI 0.67–0.95, p = 0.01) (Fig. 2). HHF occurred in 4.0% of canagliflozin patients compared to 6.4% of placebo patients (rate per 1000 patient-years = 15.7 vs. 25.3, HR = 0.61, 95% CI 0.47–0.80, p < 0.001). HHF or CV death occurred in 8.1% of canagliflozin patients compared to 11.5% of placebo patients (rate per 1000 patient-years = 31.5 vs. 45.4, HR = 0.69, 95% CI 0.57–0.83, p < 0.001).
Discussion
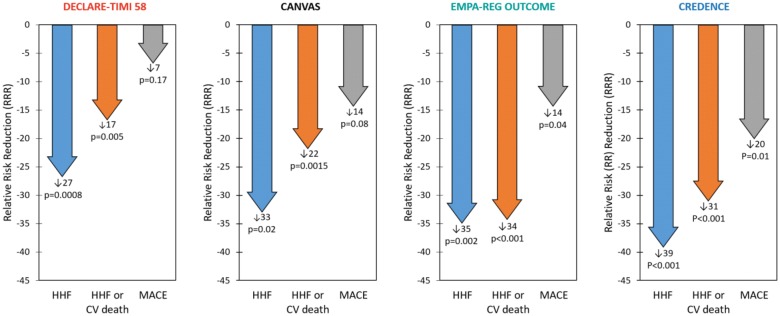
Cardiovascular and renal outcomes
When considering the four SGLT2i trials, we found that overall relative risk reductions for HHF and CV death were externally consistent among the clinical trials (Fig. 4). The relative reductions in HHF were considerably greater than those for ischemic events including nonfatal MI and ischemic stroke. Additionally, the absolute risks of CV events appeared to be more related to baseline renal filtration than the baseline CVD rate (largely comprised of stable coronary artery disease in the patient histories). Finally, when the trial criteria was designed to enroll patients with significant diabetic nephropathy with albuminuria, not only was a compelling reduction in the primary renal composite outcome observed, but the highest rate of CV events was observed as well.
Fig. 4.
Heart failure hospitalization (HHF), HHF and cardiovascular (CV) death, and major adverse cardiovascular event (MACE) relative risk reductions (RRRs) in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Statistical outcomes displayed as RRR, p-value. RRRs were calculated from hazard ratios
Of the four SGLT2i trials, CREDENCE had the highest CV event rates and DECLARE-TIMI 58 the lowest (Fig. 2). Relative risk reductions (RRRs) varied among the trials, but in general CREDENCE had the largest CV RRRs and DECLARE-TIMI 58 the smallest (Fig. 4). This is consistent with the superior baseline renal filtration function of DECLARE-TIMI 58 patients. CREDENCE had the highest composite renal event rates and DECLARE-TIMI 58 the lowest (Fig. 3). Despite these differences, the relative risk reductions in similar renal composite endpoints were externally consistent among the four trials (Fig. 5).
Fig. 5.
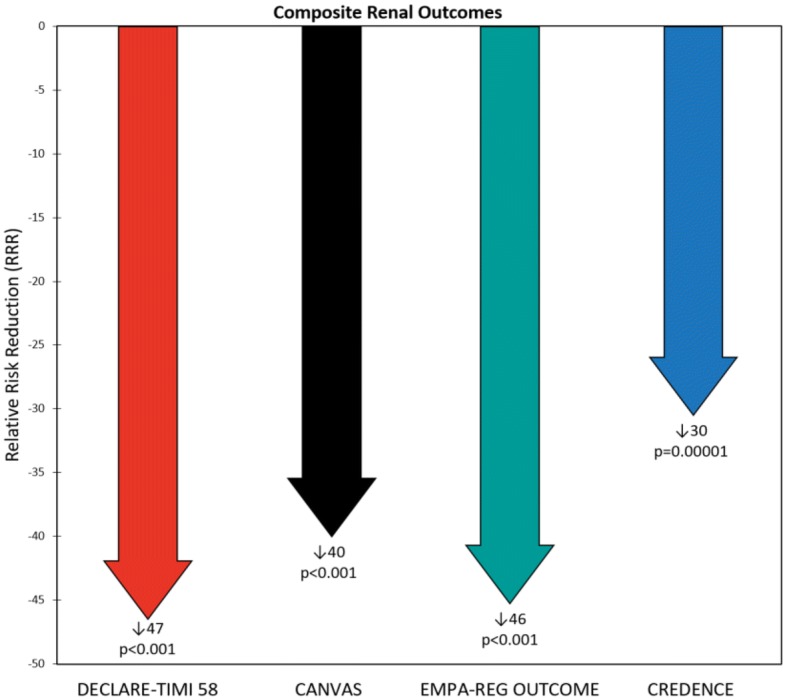
Composite renal outcome relative risk reductions (RRRs) in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Statistical outcomes displayed as RRR, p-value. RRRs were calculated from hazard ratios. Composite renal outcomes defined as follows: DECLARE-TIMI 58: ≥ 40% reduction in estimated glomerular filtration rate (eGFR) to < 60, end-stage renal disease (ESRD) (dialysis ≥ 90 days, transplant or sustained eGFR < 15), or renal/cardiovascular (CV) death; CANVAS: ≥ 40% reduction in eGFR, renal-replacement therapy (RRT) (transplant, chronic dialysis, or sustained eGFR < 15), or renal death; EMPA–REG OUTCOME: doubling of serum creatinine (Cr) with eGFR ≤ 45, RRT, or renal death; CREDENCE: doubling of serum Cr, ESRD (eGFR < 15, dialysis, or renal transplant), renal/CV death
We described the differences in CV and renal outcomes between the three CVOTs (CANVAS, DECLARE-TIMI 58, EMPA–REG OUTCOME) in a previous review [35]. We argued that the different results of the trials were at least partially attributable to non-standard inclusion criteria, renal filtration function equations, and event definitions rather than inherent differences among the medications. We suspect the same is true when comparing the three CVOTs to CREDENCE—its population had much higher baseline renal risk, and thus experienced more CV and renal outcomes. Specifically, CREDENCE had the lowest mean baseline eGFR (56.2 mL/min/1.73 m2) compared to DECLARE-TIMI 58, CANVAS, and EMPA–REG OUTCOME (85.2, 76.5, and 74 mL/min/1.73 m2, respectively) (Fig. 1). Most importantly, CREDENCE had the highest degree of albuminuria (median UACR = 927 [463, 1833] mg/g) compared to CANVAS (median UACR = 12.3 [6.65, 42.1] mg/g), DECLARE-TIMI 58 (median UACR = 13.1 [6.0, 43.6] mg/g), and EMPA–REG OUTCOME (median and quartiles 1 and 3 not supplied; 59.4% UACR < 30, 28.6% UACR > 30–300, 11.0% UACR > 300 mg/g). Together, these trials establish the UACR as a risk predictor not only for renal events but also CV outcomes. Figure 6 positions the four trials according to baseline UACR and eGFR; CREDENCE had the highest renal risk and DECLARE-TIMI 58 the lowest. This “heat map” was derived from the Chronic Kidney Disease Prognosis Consortium and the results we have summarized are consistent with the higher absolute renal and CV events observed in the four trials [36].
Fig. 6.
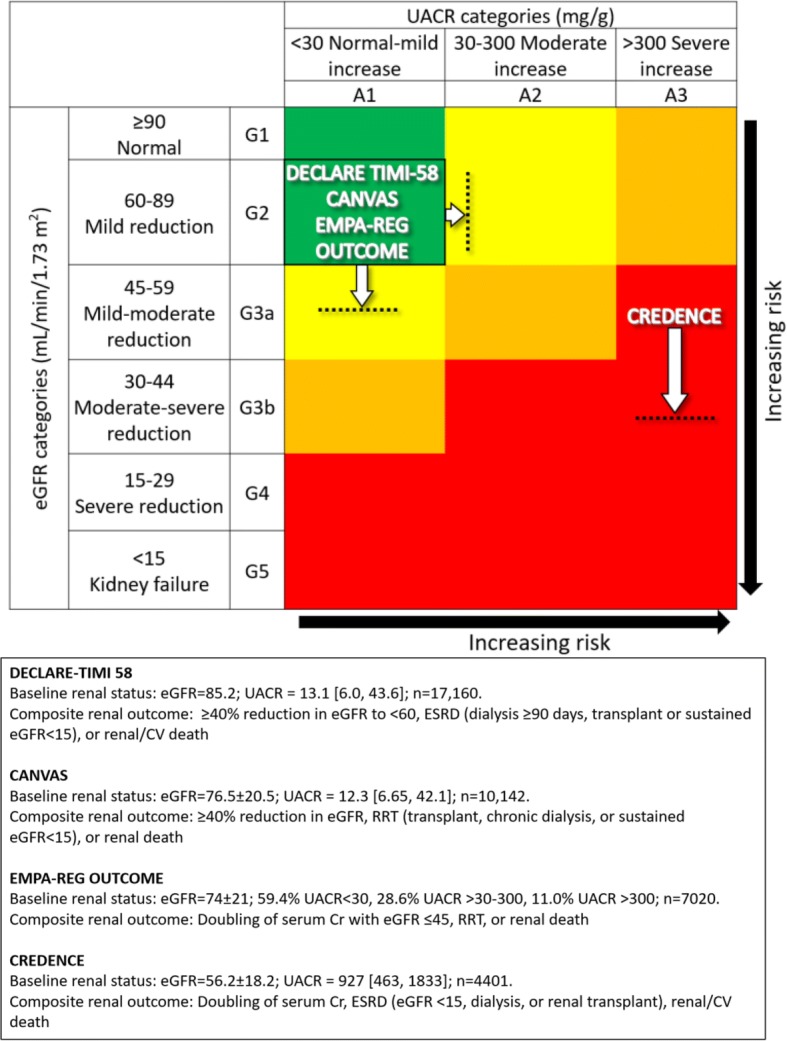
Baseline renal risk and composite renal outcome definitions in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials. Horizontal dotted lines and white arrows approximate trials averaged mean eGFRs minus 1 pooled standard deviation; vertical dotted lines and white arrows approximate trials’ quartile 3 of UACR. Data displayed as mean eGFR ± standard deviation (where available); median UACR [quartile 1, quartile 3] or percent of study population with UACR < 30, > 30–300, and > 300 (depending on trial). eGFR estimated glomerular filtration rate in mL/min/1.73 m2, UACR urinary albumin-creatinine ratio in mg/g
(Adapted from Ref. [60])
Note that eGFR is more likely to identify CKD in older patients whereas UACR/albuminuria is more likely to identify it in younger patients [37]. Additionally, albuminuria is an important predictor of CKD progression. We anticipate that some degree of the heterogeneity in cardiorenal outcomes between the trials is accountable to population differences in these two biomarkers.
Baseline renal filtration function appears to play a major role in predicting cardiorenal outcomes, perhaps more so than prior CVD. Even though CREDENCE was not planned as a CVOT and thus only 50.4% of its population had prior CVD (compared to 40.6%, 65.6%, and 99.2% for DECLARE-TIMI 58, CANVAS, and EMPA–REG OUTCOME, respectively), CREDENCE still had, for example, a two-fold increase in MACE compared to DECLARE-TIMI 58. This is supported by findings that SGLT2i decreased CV risk depending on baseline renal filtration function but not prior CVD status—lower function was associated with greater reductions in HHF [38].
Outcome definitions
We considered variance in trial methodologies as determinants for differences in results. Although the four trials had comparable CV event definitions due to FDA regulatory guidance, their composite renal outcome definitions varied according to sponsor choice (Table 1). For example, DECLARE-TIMI 58 and CREDENCE included CV death while CANVAS and EMPA–REG OUTCOME did not. There were also minor differences in the choice of renal filtration function estimation equation: DECLARE-TIMI 58 and CREDENCE used CKD-EPI to calculate eGFR while the other two trials used the MDRD equation. The CKD-EPI equation is slightly more accurate and precise and is more prognostic for mortality than MDRD [39–42]. We believe these relatively subtle differences in event definitions and estimation of renal filtration function did not play an appreciable role in the trials’ results or interpretation – the most significant factor still appears to be the position of the trials on the renal risk heat map (Fig. 6).
Table 1.
Renal drug guidelines, entry criteria, mean estimated glomerular filtration rate, and composite outcome definitions in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials
| Trial | FDA indicated guidelines | Study renal entry criteria | Results | |||
|---|---|---|---|---|---|---|
| Minimum recommended eGFR | eGFR minimum | eGFR equation | Additional renal criteria | Mean eGFR | Composite renal outcome | |
| DECLARE-TIMI 58 | 45 | N/A | CKD-EPI | CrCl 60 mL/min (Cockroft-Gault equation) | 85.2 | ≥ 40% reduction in eGFR to < 60, ESRD (dialysis ≥ 90 days, transplant or sustained eGFR < 15), or renal/CV death |
| CANVAS | 45 | 30 | MDRD | N/A | 76.5 | ≥ 40% reduction in eGFR, RRT (transplant, chronic dialysis, or sustained eGFR < 15), or renal death |
| EMPA–REG OUTCOME | 45 | 30 | MDRD | N/A | 74 | Doubling of serum Cr with eGFR ≤ 45, RRT, or renal death |
| CREDENCE | 45 | 30 | CKD-EPI | UACR 300–5000 | 56.2 | Doubling of serum Cr, ESRD (eGFR < 15, dialysis, or renal transplant), renal/CV death |
All eGFRs are in mL/min/1.73 m2
eGFR estimated glomerular filtration rate, MDRD modification of diet in renal disease, CKD-EPI chronic kidney disease epidemiology collaboration, RRT renal-replacement therapy, ESRD end-stage renal disease, CV cardiovascular, CrCl creatinine clearance, Cr creatinine, UACR urinary albumin-creatinine ratio in mg/g
Other notable trial results
Interestingly, the CREDENCE and EMPA–REG OUTCOME placebo groups had similar MACE incidence rates (48.7 and 43.9/1000 patient-years, respectively), despite different baseline UACR and eGFR. We expect this can be attributed to the balance of baseline CVD vs. renal risk: CREDENCE had significantly higher renal risk but only 50.4% prior CVD whereas EMPA–REG had nearly 100% prior CVD.
The composite renal outcome RRR is another intriguing result when comparing the four trials. In a reversal of the trend seen with the other outcomes, CREDENCE had the smallest RRR and DECLARE-TIMI 58 the largest (Fig. 5). We hypothesize that this effect may reflect differences in renal functional reserve (RFR) among the trial participants. RFR is defined as peak eGFR (induced via stress response) minus baseline eGFR and may result from recruiting inactive nephrons or increasing single nephron filtration [43, 44]. RFR has an inverse relationship with CKD stage, decreasing as CKD progresses [45]. Reducing renal hyperfiltration injury in patients with less severe CKD and thus more RFR (i.e., those in the three CVOTs) may yield more robust risk reduction or preventable fraction than in patients with advanced CKD and thus less RFR (i.e., those in CREDENCE). This hypothesis of varying opportunity for prevention of renal filtration function loss needs to be tested formally.
RAASi use
We considered other sources of confounding for differences among the trials. All four trials had substantial RAASi use: approximately 80% in the three CVOTs and 99.9% in CREDENCE. Thus, we do not believe differential rates of RAASi can explain the contrasts between the trials. Notably, the high rates of RAASi use indicate that the patients were well-treated at baseline. This should ease skepticism about the real-world therapeutic opportunity for SGLT2i, as any benefits due to the SGLT2i can be viewed as being additional to those from RAASi therapy.
Safety
We balanced our views on efficacy with the safety data. The four trials demonstrated several general safety trends (Tables 2 and 3). SGLT2i were found to be significantly safer than placebo regarding adverse events (AEs) and serious AEs. However, they were generally associated with increased risk of diabetic ketoacidosis and amputation and decreased risk of acute kidney injury. There were no clear trends regarding fractures or urinary tract infections. SGLT2i were significantly associated with increased risk of genital infections; however, this is expected due to the glucosuria promoted by the drugs. Recent research found that SGLT2i are associated with increased risk of Fournier’s gangrene [46, 47]. However, DECLARE-TIMI 58—the only trial of the four prospectively to study this AE—reported that Fournier’s gangrene occurred in 18 (0.2%) of dapagliflozin patients vs. 24 (0.3%) of placebo patients.
Table 2.
Adverse events in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials
| DECLARE-TIMI 58 | CANVAS | EMPA–REG OUTCOME | CREDENCE | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DAPA n (%) | Placebo n (%) | Riska | HR (95% CI) | p-value | CANA event rate | Placebo event rate | Riska | p-value | Pooled EMPA n (%) | Placebo n (%) | Riska | p-value | CANA n (%) | Placebo n (%) | CANA event rate | Placebo event rate | Riska | HR (95% CI) | |
| Male genital infectionb | 76 (0.9) | 9 (0.1) | +c | 8.36 (4.19–16.68)c | 0.001c | 34.9 | 10.8 | +c | < 0.001c | 166 (5.0) | 25 (1.5) | +c | < 0.001c | 28 (0.2) | 3 (0.0) | 8.4 | 0.9 | +c | 9.30 (2.83–30.60)c |
| Female genital infectionb | 68.8 | 17.5 | +c | < 0.001c | 135 (10.0) | 17 (2.6) | +c | < 0.001c | 22 (0.3) | 10 (0.0) | 12.6 | 6.1 | + | 2.10 (1.00–4.45) | |||||
| Any AE | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | 4230 (90.2) | 2139 (91.7) | −c | < 0.001c | 1784 (8.1) | 1860 (0.8) | 351.4 | 379.3 | −c | 0.87 (0.82–0.93)c |
| Serious AE | 2925 (34.1) | 3100 (36.2) | −c | 0.91 (0.87–0.96)c | < 0.001c | 104.3 | 120 | −c | 0.04c | 1789 (38.2) | 988 (42.3) | −c | < 0.001c | 737 (3.3) | 806 (0.4) | 145.2 | 164.4 | −c | 0.87 (0.79–0.97)c |
| AE leading to discontinuation | 693 (8.1) | 592 (6.9) | +c | 1.15 (1.03–1.28)c | 0.01c | 35.5 | 32.8 | + | 0.07 | 813 (17.3) | 453 (19.4) | −c | < 0.001c | N/A | N/A | N/A | N/A | N/A | N/A |
| Hypoglycemia | 58 (0.7) | 83 (1.0) | −c | 0.68 (0.49–0.95)c | 0.02c | 50 | 46.4 | + | 0.20 | 1303 (27.8) | 650 (27.9) | − | N/A | 225 (1.0) | 240 (0.1) | 44.3 | 48.9 | − | 0.92 (0.77–1.11) |
| UTI | 127 (1.5) | 133 (1.6) | − | 0.93 (0.73–1.18) | 0.54 | 40 | 37 | + | 0.38 | 842 (18.0) | 423 (18.1) | − | N/A | 245 (1.1) | 221 (0.1) | 48.3 | 45.1 | + | 1.08 (0.90–1.29) |
| Fracture | 457 (5.3) | 440 (5.1) | + | 1.04 (0.91–1.18) | 0.59 | 15.4 | 11.9 | +c | 0.02c | 179 (3.8) | 91 (3.9) | − | N/A | 67 (0.3) | 68 (0.0) | 11.8 | 12.1 | − | 0.98 (0.70–1.37) |
| Hyperkalemia | N/A | N/A | N/A | N/A | N/A | 6.9 | 4.4 | + | 0.10 | N/A | N/A | N/A | N/A | 151 | 181 | 29.7 | 36.9 | − | 0.80 |
| Amputation | 123 (1.4) | 113 (1.3) | + | 1.09 (0.84–1.40) | 0.53 | 6.3 | 3.4 | +c | < 0.001c | N/A | N/A | N/A | N/A | 70 (0.3) | 63 (0.0) | 12.3 | 11.2 | + | 1.11 (0.79–1.56) |
| AKI | 125 (1.5) | 113 (1.3) | −c | 0.69 (0.55–0.87)c | 0.002c | 3 | 4.1 | − | 0.33 | 45 (1.0) | 37 (1.6) | −c | < 0.05c | 86 (0.4) | 98 (0.0) | 16.9 | 20 | − | 0.85 (0.64–1.13) |
| Breast cancer | 36 (0.4) | 113 (1.3) | 0 | 1.02 (0.64–1.63) | 0.92 | 3.1 | 2.6 | + | 0.65 | N/A | N/A | N/A | N/A | 8 (0.1) | 3 (0.0) | 4.1 | 1.6 | + | 2.59 (0.69–9.76) |
| Bladder cancer | 26 (0.3) | 45 (0.5) | −c | 0.57 (0.35–0.93)c | 0.02c | 1 | 1.1 | − | 0.74 | N/A | N/A | N/A | N/A | 10 (0.0) | 9 (0.0) | 1.7 | 1.6 | + | 1.10 (0.45–2.72) |
| DKA | 27 (0.3) | 12 (0.1) | +c | 2.18 (1.10–4.30)c | 0.02c | 0.6 | 0.3 | + | 0.14 | 4 (0.1) | 1 (< 0.1) | + | N/A | 11 (0.0) | 1 (0.0) | 2.2 | 0.2 | +c | 10.80 (1.39–83.65)c |
DAPA dapagliflozin, CANA canagliflozin, EMPA empagliflozin, HR hazard ratio, CI confidence interval, AE adverse event, N/A not available, UTI urinary tract infection, AKI acute kidney injury, DKA diabetic ketoacidosis
aIndicates increased (“+”), decreased (“−”), or no difference in (“0”) risk associated with study drug compared to placebo.
bDECLARE-TIMI 58 did not differentiate genital infection by sex
cItalic indicates statistical significance at the α = 0.05 level
Table 3.
Risk associated with study drug compared to placebo for adverse events in the Dapagliflozin Effect on CardiovascuLAR Events (DECLARE-TIMI 58), CANagliflozin CardioVascular Assessment Study (CANVAS) Program, Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA–REG OUTCOME), and Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trials
| DECLARE-TIMI 58 | CANVAS | EMPA–REG OUTCOME | CREDENCE | |
|---|---|---|---|---|
| Male genital infectiona | +b | +b | +b | +b |
| Female genital infectiona | +b | +b | + | |
| Any AE | N/A | N/A | −b | −b |
| Serious AE | −b | −b | −b | −b |
| AE causing discontinuation | +b | + | −b | N/A |
| Hypoglycemia | −b | + | − | − |
| UTI | − | + | − | + |
| Fracture | + | +b | − | − |
| Hyperkalemia | N/A | + | N/A | − |
| Amputation | + | +b | N/A | + |
| AKI | −b | − | −b | − |
| Breast cancer | 0 | + | N/A | + |
| Bladder cancer | −b | − | N/A | + |
| DKA | +b | + | + | +b |
AE adverse event, N/A not available, UTI urinary tract infection, AKI acute kidney injury, DKA diabetic ketoacidosis
aDECLARE-TIMI 58 did not differentiate genital infection by sex
bindicates statistical significance at the α = 0.05 level. “+” = increased risk, “−” = decreased risk, “0” = no difference in risk
Future potential benefits of SGLT2i
SGLT2i have demonstrated a host of positive effects of interest for future research. In animal models of T2DM female mice, empagliflozin ameliorated kidney injury by promoting glycosuria, and possibly by reducing systemic and renal artery stiffness; canagliflozin attenuated the progression of atherosclerosis, reducing hyperlipidemia, hyperglycemia, and inflammation by lowering the expression of some inflammatory molecules [48, 49]. Of note, the hyperexpressed SGLT1 in cardiomyocytes may represent a potential pharmacological target for cardioprotection [50]. In human studies of T2DM patients, both dapagliflozin and canagliflozin demonstrated beneficial effects on left ventricular diastolic functional parameters [51, 52]. With regard to SGLT2i versus other antihyperglycemic agents, SGLT2i were associated with a reduced risk of HHF compared to dipeptidyl peptidase 4 inhibitors (DPP4i) and canagliflozin was associated with a reduced risk of HHF and a similar risk of MI or stroke compared to DPP4i, glucagon-like peptide-1 agonists, and sulfonylureas [53, 54]. Finally, the EMPA–REG OUTCOME results may be applicable to T2DM patients with a broader CV risk profile, including patients at low risk of CVD [55].
Class effects
Giugliano et al. [56] studied the three SGLT2i CVOTs and suggested a class effect with regard to HF risk reduction. After reviewing the CVOTs and CREDENCE, we believe this class effect can be expanded to include CV and renal outcomes in general. Note that there is no universal definition of class effect; the closest approximation is the term “class labeling” used by the FDA, which “assumes that all products within a class are closely related in chemical structure, pharmacology, therapeutic activity, and adverse reactions” [57]. With this in mind, we believe there is sufficient evidence of a class effect. Firstly, the SGLT2i have similar molecular structures. Also, though much of their pharmacological methods of action are unknown, we believe one plausible explanation is off-target inhibition of the sodium-proton antiporter/exchanger—a membrane-bound family of channels present in both the heart and kidneys [58, 59]. The four trials are internally consistent, with no particular subgroup benefitting over another and no treatment interactions within any of the trials. The trials are externally consistent with each other, showing reliable cardiorenal benefit (according to baseline risk) and comparable adverse effects. Lastly, the SGLT2i studied have similar known mechanisms of action resulting in losses of glucose and sodium in the urine and reductions in blood pressure and body weight [58]. This proposed pharmacologic class effect would apply more to HHF, CV death, and renal composite events than to the MACE composite outcome, which was not significantly reduced in DECLARE-TIMI 58. Additionally, this class effect is limited to the three SGLT2i we have reviewed in this paper: canagliflozin, dapagliflozin, and empagliflozin. It remains to be seen if it will extend to ertugliflozin, sotagliflozin, and/or other similar agents.
Conclusions
Dapagliflozin, empagliflozin, and canagliflozin have internally and externally consistent class effects on cardiorenal outcomes and similar safety profiles. Baseline renal filtration function and degree of albuminuria are the most significant indicators of risk for both CV and renal events. Thus, these two factors also anticipate the greatest clinical benefit for SGLT2i.
Acknowledgements
None.
Abbreviations
- ACEi
angiotensin-converting-enzyme inhibitor
- AE
adverse event
- ARB
angiotensin-receptor blocker
- CANVAS
CANagliflozin CardioVascular Assessment Study
- CANVAS-R
CANVAS-Renal
- CI
confidence interval
- CKD
chronic kidney disease
- CKD-EPI
chronic kidney disease epidemiology collaboration
- CrCl
creatinine clearance
- CREDENCE
canagliflozin and renal events in diabetes with established nephropathy clinical evaluation
- CV
cardiovascular
- CVD
cardiovascular disease
- CVOT
cardiovascular outcomes trial
- DECLARE-TIMI 58
Dapagliflozin Effect on CardiovascuLAR Events
- DPP4i
dipeptidyl peptidase 4 inhibitor(s)
- eGFR
estimated glomerular filtration rate
- EMPA–REG OUTCOME
Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose
- ESRD
end-stage renal disease
- FDA
United States Food and Drug Administration
- HF
heart failure
- HHF
heart failure hospitalization
- HR
hazard ratio
- MDRD
modification of diet in renal disease
- MI
myocardial infarction
- RAASi
renin–angiotensin–aldosterone system inhibitor
- RRR
relative risk reduction
- RRT
renal-replacement therapy
- SGLT2i
sodium-glucose cotransporter 2 inhibitor(s)
- T2DM
type 2 diabetes mellitus
- UACR
urinary albumin-creatinine ratio
Authors’ contributions
AYK and PMC wrote the first draft of the paper. All other authors provided editing assistance. All authors read and approved the final manuscript.
Funding
This work was partially funded by the Baylor Health Care System Foundation.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the american heart association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Fitchett DH, Udell JA, Inzucchi SE. Heart failure outcomes in clinical trials of glucose-lowering agents in patients with diabetes. Eur J Heart Fail. 2017;19:43–53. doi: 10.1002/ejhf.633. [DOI] [PubMed] [Google Scholar]
- 3.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.CIR.0000039105.49749.6F. [DOI] [PubMed] [Google Scholar]
- 4.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 5.Zelniker TA, Braunwald E. Cardiac and renal effects of sodium-glucose co-transporter 2 inhibitors in diabetes: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72(15):1845–1855. doi: 10.1016/j.jacc.2018.06.040. [DOI] [PubMed] [Google Scholar]
- 6.Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, Saran R, Wang AY, Yang CW. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382(9888):260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 7.Kastarinen M, Juutilainen A, Kastarinen H, Salomaa V, Karhapää P, Tuomilehto J, et al. Risk factors for end-stage renal disease in a community-based population: 26-year follow-up of 25,821 men and women in eastern Finland. J Intern Med. 2010;267(6):612–620. doi: 10.1111/j.1365-2796.2009.02197.x. [DOI] [PubMed] [Google Scholar]
- 8.Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–2375. doi: 10.1056/NEJMra1615439. [DOI] [PubMed] [Google Scholar]
- 9.Gilbert MP, Pratley RE. The impact of diabetes and diabetes medications on bone health. Endocr Rev. 2015;36(2):194–213. doi: 10.1210/er.2012-1042. [DOI] [PubMed] [Google Scholar]
- 10.Thomas MC, Tsalamandris C, MacIsaac RJ, Jerums G. The epidemiology of hemoglobin levels in patients with type 2 diabetes. Am J Kidney Dis. 2006;48(4):537–545. doi: 10.1053/j.ajkd.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Kaul S, Bolger AF, Herrington D, Giugliano RP, Eckel RH, American Heart Association; American College Of Cardiology Foundation Thiazolidinedione drugs and cardiovascular risks: a science advisory from the American Heart Association and American College Of Cardiology Foundation. J Am Coll Cardiol. 2010;55(17):1885–1894. doi: 10.1016/j.jacc.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 12.Home PD, Pocock SJ, Beck-Nielsen H, Curtis PS, Gomis R, Hanefeld M, Jones NP, Komajda M, McMurray JJ. Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trial. Lancet. 2009;373:2125–2135. doi: 10.1016/S0140-6736(09)60953-3. [DOI] [PubMed] [Google Scholar]
- 13.Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298:1180–1188. doi: 10.1001/jama.298.10.1180. [DOI] [PubMed] [Google Scholar]
- 14.Douros A, Dell’Aniello S, Yu OHY, Filion KB, Azoulay L, Suissa S. Sulfonylureas as second line drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: population based cohort study. BMJ. 2018;362:k2693. doi: 10.1136/bmj.k2693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell WR, Christiansen CL, Miller DR. Meta-analysis of sulfonylurea therapy on long-term risk of mortality and cardiovascular events compared to other oral glucose-lowering treatments. Diabetes Ther. 2018;9(4):1431–1440. doi: 10.1007/s13300-018-0443-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vaccaro O, Masulli M, Nicolucci A, Bonora E, Del Prato S, Maggioni AP, et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin (TOSCA.IT): a randomised, multicentre trial. Lancet Diabetes Endocrinol. 2017;5(11):887–897. doi: 10.1016/s2213-8587(17)30317-0. [DOI] [PubMed] [Google Scholar]
- 17.Zannad F, Stough WG, Lipicky RJ, Tamargo J, Bakris GL, Borer JS, et al. Assessment of cardiovascular risk of new drugs for the treatment of diabetes mellitus: risk assessment vs. risk aversion. Eur Heart J Cardiovasc Pharmacother. 2016;2(3):200–205. doi: 10.1093/ehjcvp/pvw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Das SR, Everett BM, Birtcher KK, Brown JM, Cefalu WT, Januzzi JL, Jr, Kalyani RR, Kosiborod M, Magwire ML, Morris PB, Sperling LS. 2018 ACC expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a report of the American college of cardiology task force on expert consensus decision pathways. J Am Coll Cardiol. 2018;72(24):3200–3223. doi: 10.1016/j.jacc.2018.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scheen AJ, Paquot N. Management of hyperglycaemia of type 2 diabetes. Paradigm change according to the ADA-EASD consensus report 2018. Rev Med Liege. 2018;73(12):629–633. [PubMed] [Google Scholar]
- 20.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE, EMPA–REG OUTCOME Investigators Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. doi: 10.1056/nejmoa1504720. [DOI] [PubMed] [Google Scholar]
- 21.Neal B, Perkovic V, Mahaffey KW, Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR, CANVAS Program Collaborative Group Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. doi: 10.1056/nejmoa1611925. [DOI] [PubMed] [Google Scholar]
- 22.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS, DECLARE–TIMI 58 Investigators Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. doi: 10.1056/nejmoa1812389. [DOI] [PubMed] [Google Scholar]
- 23.Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu PL, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H, Zinman B, Meininger G, Brenner BM, Mahaffey KW, CREDENCE Trial Investigators Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;1:1. doi: 10.1056/nejmoa1811744. [DOI] [Google Scholar]
- 24.Altman DG, Bland JM. How to obtain the P value from a confidence interval. BMJ. 2011;343:d2304. doi: 10.1136/bmj.d2304. [DOI] [PubMed] [Google Scholar]
- 25.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 26.Jardiance. Drugs website. 2019. https://www.drugs.com/pro/jardiance.html. Accessed 22 Apr 2019.
- 27.Zinman B, Inzucchi SE, Lachin JM, Wanner C, Ferrari R, Fitchett D, Bluhmki E, Hantel S, Kempthorne-Rawson J, Newman J, Johansen OE, Woerle HJ, Broedl UC. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA–REG OUTCOME™) Cardiovasc Diabetol. 2014;19(13):102. doi: 10.1186/1475-2840-13-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wanner C, Inzucchi SE, Lachin JM, Fitchett D, Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B, EMPA–REG OUTCOME Investigators Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–334. doi: 10.1056/nejmoa1515920. [DOI] [PubMed] [Google Scholar]
- 29.Neal B, Perkovic V, Zeeuw D, Mahaffey KW, Fulcher G, Stein P, Desai M, Shaw W, Jiang J, Vercruysse F. Rationale, design, and baseline characteristics of the canagliflozin cardiovascular assessment study (CANVAS)—a randomized placebo-controlled trial. Am Heart J. 2013;166:217–223. doi: 10.1016/j.ahj.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Invokana. Drugs website. 2018. https://www.drugs.com/pro/invokana.html. Accessed 22 Apr 2019.
- 31.Neuen BL, Ohkuma T, Neal B, Matthews DR, de Zeeuw D, Mahaffey KW, Fulcher G, Desai M, Li Q, Deng H, Rosenthal N, Jardine MJ, Bakris G, Perkovic V. Cardiovascular and renal outcomes with canagliflozin according to baseline kidney function. Circulation. 2018;138(15):1537–1550. doi: 10.1161/CIRCULATIONAHA.118.035901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Bansilal S, Bhatt DL, Leiter LA, McGuire DK, Wilding JP, Gause-Nilsson IA, Langkilde AM, Johansson PA, Sabatine MS. The design and rationale for the dapagliflozin effect on cardiovascular events (DECLARE)-TIMI 58 trial. Am Heart J. 2018;200:83–89. doi: 10.1016/j.ahj.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 33.Farxiga. Drugs website. 2019. https://www.drugs.com/pro/farxiga.html. Accessed 22 Apr 2019.
- 34.Blair G. New FDA Extension for Farxiga and Xigduo XR. Diabetes in Control website. 2019. http://www.diabetesincontrol.com/new-fda-extension-for-farxiga-and-xigduo-xr/. Accessed 10 May 2019.
- 35.Kluger AY, Tecson KM, Barbin CM, Lee AY, Lerma EV, Rosol ZP, Rangaswami J, Lepor NE, Cobble ME, McCullough PA. Cardiorenal outcomes in the CANVAS, DECLARE-TIMI 58, and EMPA–REG OUTCOME trials: a systematic review. Rev Cardiovasc Med. 2018;19(2):41–49. doi: 10.31083/j.rcm.2018.02.907. [DOI] [PubMed] [Google Scholar]
- 36.Chronic Kidney Disease Prognosis Consortium. Matsushita K, Velde M, Astor BC, Woodward M, Levey AS, Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–2081. doi: 10.1016/s0140-6736(10)60674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCullough PA, Li S, Jurkovitz CT, Stevens LA, Wang C, Collins AJ, Chen SC, Norris KC, McFarlane SI, Johnson B, Shlipak MG, Obialo CI, Brown WW, Vassalotti JA, Whaley-Connell AT, Kidney Early Evaluation Program Investigators CKD and cardiovascular disease in screened high-risk volunteer and general populations: the Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 Suppl 2):38–45. doi: 10.1053/j.ajkd.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 38.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31–39. doi: 10.1016/S0140-6736(18)32590-X. [DOI] [PubMed] [Google Scholar]
- 39.Stevens LA, Li S, Kurella Tamura M, Chen SC, Vassalotti JA, Norris KC, Whaley-Connell AT, Bakris GL, McCullough PA. Comparison of the CKD Epidemiology Collaboration (CKD-EPI) and modification of diet in renal disease (MDRD) study equations: risk factors for and complications of CKD and mortality in the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2011;57(3 Suppl 2):S9–S16. doi: 10.1053/j.ajkd.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCullough PA, Patanker G, Stoler RC. Estimating renal filtration, drug dosing, and clinical outcomes. J Am Coll Cardiol. 2015;65(25):2724–2725. doi: 10.1016/j.jacc.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 41.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Becker BN, Vassalotti JA. A software upgrade: CKD testing in 2010. Am J Kidney Dis. 2010;55:8–10. doi: 10.1053/j.ajkd.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 43.Palsson R, Waikar SS. Renal functional reserve revisited. Adv Chronic Kidney Dis. 2018;25(3):e1–e8. doi: 10.1053/j.ackd.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Ronco C, Chawla LS. Glomerular and tubular kidney stress test: new tools for a deeper evaluation of kidney function. Nephron. 2016;134(3):191–194. doi: 10.1159/000449235. [DOI] [PubMed] [Google Scholar]
- 45.Barai S, Gambhir S, Prasad N, Sharma RK, Ora M. Functional renal reserve capacity in different stages of chronic kidney disease. Nephrology (Carlton). 2010;15(3):350–353. doi: 10.1111/j.1440-1797.2010.01291.x. [DOI] [PubMed] [Google Scholar]
- 46.Bersoff-Matcha SJ, Chamberlain C, Cao C, Kortepeter C, Chong WH. Fournier gangrene associated with sodium-glucose cotransporter-2 inhibitors: a review of spontaneous postmarketing cases. Ann Intern Med. 2019 doi: 10.7326/m19-0085. [DOI] [PubMed] [Google Scholar]
- 47.Scheen AJ. An update on the safety of SGLT2 inhibitors. Exp Opin Drug Saf. 2019;18(4):295–311. doi: 10.1080/14740338.2019.1602116. [DOI] [PubMed] [Google Scholar]
- 48.Aroor, et al. Glycemic control by the SGLT2 inhibitor empagliflozin decreases aortic stiffness, renal resistivity index and kidney injury. Cardiovasc Diabetol. 2018;17:108. doi: 10.1186/s12933-018-0750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nasiri-Ansari, et al. Canagliflozin attenuates the progression of atherosclerosis and inflammation process in APOE knockout mice. Cardiovasc Diabetol. 2018;17:106. doi: 10.1186/s12933-018-0749-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franco Di, et al. Sodium-dependent glucose transporters (SGLT) in human ischemic heart: a new potential pharmacological target. Int J Cardiol. 2017;243:86–90. doi: 10.1016/j.ijcard.2017.05.032. [DOI] [PubMed] [Google Scholar]
- 51.Soga, et al. Impact of dapagliflozin on left ventricular diastolic function of patients with type 2 diabetic mellitus with chronic heart failure. Cardiovasc Diabetol. 2018;17:132. doi: 10.1186/s12933-018-0775-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matsutani, et al. Effect of canagliflozin on left ventricular diastolic function in patients with type 2 diabetes. Cardiovasc Diabetol. 2018;17:73. doi: 10.1186/s12933-018-0717-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim, et al. Association between sodium glucose co-transporter 2 inhibitors and a reduced risk of heart failure in patients with type 2 diabetes mellitus: a real-world nationwide population-based cohort study. Cardiovasc Diabetol. 2018;17:91. doi: 10.1186/s12933-018-0737-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patorno E, Goldfine AB, Schneeweiss S, Everett BM, Glynn RJ, Liu J, Kim SC. Cardiovascular outcomes associated with canagliflozin versus other non-gliflozin antidiabetic drugs: population based cohort study. BMJ. 2018;6(360):k119. doi: 10.1136/bmj.k119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gallwitz B. The cardiovascular benefits associated with the use of sodium-glucose cotransporter 2 inhibitors—real-world data. Eur Endocrinol. 2018;14:17–23. doi: 10.17925/EE.2018.14.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Giugliano D, Meier JJ, Esposito K. Heart failure and type 2 diabetes: from cardiovascular outcome trials, with hope. Diabetes Obes Metab. 2019;21(5):1081–1087. doi: 10.1111/dom.13629. [DOI] [PubMed] [Google Scholar]
- 57.Furberg CD. Class effects and evidence-based medicine. Clin Cardiol. 2000;23(7 Suppl 4):IV15–19. doi: 10.1002/clc.4960230705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McCullough PA, Kluger AY, Tecson KM, Barbin CM, Lee AY, Lerma EV, Rosol ZP, Kluger SL, Rangaswami J. Inhibition of the sodium–proton antiporter (Exchanger) is a plausible mechanism of potential benefit and harm for drugs designed to block sodium glucose co-transporter 2. Rev Cardiovasc Med. 2018;19(2):51–63. doi: 10.31083/j.rcm.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 59.Kaplan A, Abidi E, El-Yazbi A, Eid A, Booz GW, Zouein FA. Direct cardiovascular impact of SGLT2 inhibitors: mechanisms and effects. Heart Fail Rev. 2018;23(3):419–437. doi: 10.1007/s10741-017-9665-9. [DOI] [PubMed] [Google Scholar]
- 60.Eckardt KU, Bansal N, Coresh J, Evans M, Grams ME, Herzog CA, James MT, Heerspink HJL, Pollock CA, Stevens PE, Tamura MK, Tonelli MA, Wheeler DC, Winkelmayer WC, Cheung M, Hemmelgarn BR, Conference Participants Improving the prognosis of patients with severely decreased glomerular filtration rate (CKDG4+): conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int. 2018;93(6):1281–1292. doi: 10.1016/j.kint.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.