Abstract
Higher stiffness of the Achilles tendon (AT) and gastrocnemius have been found to be risk factors associated with Achilles tendinitis. Static stretching (SS) is one intervention that has been investigated to improve the flexibility and therefore reduce injury risk. Previous studies have investigated the acute effect of SS on one region for AT and gastrocnemius morphology and stiffness; however, there is a lack of knowledge about the effect of SS on other regions of the AT and gastrocnemius (e.g., proximal vs. distal, within gastrocnemius). The aims of the present study were: (1) to investigate the acute effects of SS on the shear modulus of the medial gastrocnemius muscles (MG) and lateral gastrocnemius muscles (LG) and AT for different regions; (2) to examine the differences in range of motion (ROM) before and after SS; and (3) to investigate the change of thickness of AT and fascicle length of MG and LG before and after SS. The stiffness of AT and the gastrocnemius, fascicle length of the muscles, thickness of the AT, and maximal ankle joint dorsiflexion angle were measured in thirty healthy subjects (15 males, 15 females) before(pre) and immediately after (post) 5-minute SS. Stretching effects are not homogeneous among different regions. After SS administration, the proximal, middle, and distal regions of MG stiffness decreased by 34.12%, 22.45%, and 25.27%, respectively (p = 0.000), and LG stiffness decreased by 37.71%, 30.47%, and 22.13%, respectively (p = 0.000), whereas AT stiffness increased by 25.73%, 17.01%, and 19.53%, respectively (p= 0.000). ROM of ankle joint increased by 8.02% (p=0.00). Nevertheless, there were no changes in the thickness of AT and fascicle length of the gastrocnemius. These results suggest that non-uniform behaviour is consistently present within the gastrocnemius and AT, and the gastrocnemius heterogeneity is reduced after SS. The stretching maneuver could be effective to increase the flexibility.
Key points.
Stretching effects are not homogeneous among different regions of AT, MG, and LG. After SS administration, the proximal, middle, and distal regions of MG stiffness and LG stiffness were decreased, whereas AT stiffness were increased.
ROM of the ankle joint increased by 8.02%. Nevertheless, there were no changes in the thickness of AT and fascicle length of the gastrocnemius.
Non-uniform behaviour is consistently present within the gastrocnemius and AT, and the gastrocnemius inhomogeneity is reduced after SS.
Key words: Acute effect, muscle and tendon stiffness, flexibility, joint range of motion, ultrasound shear wave elastography
Introduction
The gastrocnemius-Achilles tendon (AT) complex is the largest and strongest muscle-tendon in the human body (O’Brien, 2005). The complex is subject to changes especially the mid-portion of AT depending to the tensile loads during its elongation or contraction, make it susceptible to overuse injuries. According to statistics, the incidence rate of Achilles tendinitis is 0.2% in the general population (Romero-Morales et al., 2019). Pre-exercise static stretching (SS) is commonly performed to reduce muscle stiffness to enhance functional range of motion (ROM) and avoid AT injuries (Rosario and Foletto, 2015). SS has also typically been used in clinical practice, especially in rehabilitation training (Santos et al., 2019). SS is a common method for decreasing the muscle-tendon unit (MTU) stiffness and passive torque to prevent or improve limited mobility (Nakamuraet al., 2011). Thus, stretching is a recommended intervention, whether in healthy people or patients, whether in daily exercise or in clinical rehabilitation training.
Understanding of the effect of SS on the architecture and mechanical properties of the gastrocnemius-AT complex has been a topic of interest among clinicians and researchers. This musculoskeletal system is composed of MTUs, whereas each MTU is divided into a passive component and an active component (muscle). Onefunction of the passive component of MTU is to store and release elastic energy (tendons—proximal and distal to the muscle), while the function of the active component is force generation (muscle) (Cenni et al., 2018). Thus, the capacity to contract muscle and the proper muscle force transmission and movement generation are influenced by the operating ratios between muscle and tendon (Cenni et al., 2018). Recently, the behaviours of the muscle-tendon complex were evaluated using ultrasound shear wave elastography (SWE). Our previous studies demonstrated that SWE is a valid and reliable tool to estimate the elastic properties of tendon (Zhang and Fu, 2013; Zhang et al., 2014) and muscle (Zhang et al., 2017). In addition, a positive significant correlation was found between the elastic modulus of muscle from SWE and the elastic modulus from a material testing system (Eby et al., 2013). Similarly, grey-scale ultrasound has the ability to estimate architectural parameters of muscles, such asfascicle lengths, and muscle thickness (Hodges et al., 2003). As described, accurately quantifying the morphology and stiffness of AT and gastrocnemius by SWE and grey-scale ultrasound before and after a SS may provide a more comprehensive understanding about the physiological characteristics of MTUs.
Previous studies estimated the passive behaviour of the gastrocnemius by measuring the stiffness of the proximal 30% or the middle region of the lower leg length of the MG and LG during passive dorsiflexion or stretching using SWE (Akagi and Takahashi, 2013; Cè et al., 2015; Hirata et al., 2016; Payne et al., 2018). as well as the passive behaviour of AT by measuring in the proximal or distal region of tendons (Kato and Fukunaga,2010; Nakamura et al.,2013; Cè et al., 2015; Chiu et al., 2016; Wren et al., 2003). Interestingly, Porta et al (2014) evaluated the proximal, middle, and distal portions of patellar tendons in healthy subjects by ultrasound. They found that the proximal portion of the patellar tendon was significantly stiffer than the distal portion. However, the acute effect of SS on passive stiffness among the different regions of gastrocnemius and AT remains unclear. Contrasting scenarios about the outcome of SS on the gastrocnemius muscle-AT complex stiffness have been reported, but the values of shear modulus of the complex were measured in only one muscle region or one tendon region in those reports. However, the local stiffness does not represent whole tissue stiffness. In terms of anatomy, the muscle fibre of the gastrocnemius has a complex multipennate arrangement (O’Brien, 2005), whereas the twisted structure of the AT rotates as they descend, but does not run parallel to each other (Edama et al., 2016). Also, tendon stiffness is expected to vary along the tendon length, whereas muscle stiffness varies along the muscle length. Thus, it is important to evaluate different regions within the same muscle and tendon to provide a better understanding of stiffness variations within the gastrocnemius-AT complex. Beyond a more in-depth description of the gastrocnemius-AT complex biomechanics, a better understanding about the intramuscle distribution and intra-tendon distribution of passive stiffness in vivo would allow the medical researcher and clinical worker to optimize treatment strategies by focusing attention specifically on the stiffer regions.
The objectives of this study were as follows: (1) to investigate the acute effects of SS on the shear modulus of the MG, LG and AT for different regionsby determining three proximal-distal regions for MG and LG (distal, mid, and proximal regions on the muscle) and three regions for the AT (0, 3, and 6cm above the calcaneal tuberosity); (2) to examine the changes on ROM before and after a SS;and (3) to investigate the change of thickness of the AT and fascicle length of the MG and LG before and after a SS.
Methods
Ethics statement
This study was approved by the Human Subjects Ethics committee of the Clinical Medical College of Acupuncture, Moxibustion and Rehabilitation (GZUCM2017-003-01). The study abided by the principles of the Declaration of Helsinki. Before the commencement of the study, all recruited subjects were fully informed of the study purposes, experimental procedures, rights of volunteers, and safety of SWE by an experimental statement, and all signed the informed consent.
Participants
Thirty healthy subjects [15 males and 15 females; males: age: 21.33±2.72 y; height: 1.73±0.07m; weight: 69.07±14.73 kg; body mass index (BMI): 22.99±4.96 kg/m2; females: age: 21.13±2.17 y; height: 1.62±0.05m; weight: 52.93±12.63 kg; body mass index (BMI): 20.19±4.13 kg/m2] were recruited for this study. Participants were not trained, recreationally active or sedentary. Each participant was asked to avoid longer than usual walking, standing, or running for a week prior to imaging.The location of the study was the Department of Ultrasound Imaging of Luoyang Orthopaedic Hospital of Henan Province.The inclusion criteria were that all subjects were healthy and couldfollowthe instructions of the operator.The exclusion criteria were as follows: neuromuscular disease, tendon rupture, musculoskeletal injury of lowerlimb, current use of corticosteroids.
Experimental setup and protocol
This experiment was an observational study. Before (PRE) and immediately after (POST) 5-minute SS for the AT and the gastrocnemius in the dominant leg, the shear elastic modules of AT and the gastrocnemius, fascicle length of the MG and LG, thickness of the AT, and ROM of the ankle joint were measured. The dominant leg of subjects was determined by kicking a ball.
Equipment and parameter settings
All ultrasound examinations were performed by the ultrasound SWE system (Aixplorer Supersonic Imagine, France) with a 50-mm linear-array transducer (SL15-4, Supersonic Imagine, France). The instrument used the default standard musculoskeletal (MSK) presets.The upper limit (800 kPa) of the system was adopted for measurement of the muscle-tendon elastic modulus. Other settings of the SWE systems were as follows:opacity was 85%, and depth of the B-scan ultrasound was 3.0 cm. The B-mode ultrasound was performed to assess the fascicle length in the middle regions of the MG and LG, and the thickness of the AT, whereas SWE was used to assess the stiffness of the MG, LG and the AT. In the SWE examination, the Q-box diameter of the AT was defined by the thickness of the AT (Zhang and Fu, 2013). The Q-box diameter of the MG and LG were set as 5 b 5 mm, and the size of the regions of interest (ROIs) was 10 10 mm (Saeki et al., 2017).
Stretching protocol
Before stretching, the subject was asked to wear loose-fitting short pants. In addition,the subject was explicitly asked to refrain from strenuous exercise for 48 hours before the experiment (Payne et al.,2018). To reduce experimental errors, the room temperature was maintained at 25°C throughout the experiment (Akagi and Takahashi, 2013). Five minutes of SS was administered to both legs of the subject. The subject was asked to stand on a 30-degree inclined platform with both legs vertical to the ground, and keep this posture for 5 minutes (Peltz et al., 2013). The subject was requested to relax throughout the SS. Immediately after the SS, an assessment was performed on the dominant leg using the aforementionedprotocol.
Ultrasound examination of the AT and gastrocnemius Procedures
The muscle-tendon shear modulus was measured on the dominant leg during the ankle was passively positioned at “relaxed”. The “relaxed” position is that subjects took what they perceived to be a “relaxed” foot position, and the angle of ankle was measured by a manual goniometer (Sammons Preston, Royan, Canada). After SS, the ankle joint was always passively fixed at the angle of previously measured using a customized and movable ankle foot orthosis (AFO). The fascicle length of the MG and LG, thickness of the AT were also measured at this angle position.
Measurements
During tests, the subject was asked to lay prone on the bed with the foot in a relaxed position. The hip and knee joints wereextended (Payne et al .,2018).According to the previous studies, the measurement site of the AT was defined as 0,3, and 6cm above the calcaneal tuberosity (Haen et al., 2017), whereas three regions of the MG and LG (distal, mid, and proximal regions on the muscle) were determined based on anatomical guidelines (Leet al., 2018).Images were obtained along the middle sagittal plane of the MG and LG, at the 25% (proximal region), 50% (middle region) and 75% (distal region)of muscle length (toward distal tendon insertion). Some previous studies demonstrated that the SWE had goodinter-day reliability for shear elastic modulus at all the locations used in this study (Payne et al., 2018; Le et al., 2017). The three regions of the MG and LG were identified by ultrasound before the experiment. All corresponding skin surfaces were marked with a black pen to allow repeated assessments from the same regions before and after SS. The B-mode ultrasound was performed to assess the fascicle length of the MG and LG and thickness of the AT. Enough ultrasound gel was applied on the dermal surface. For fascicle length of the MG and LG, the transducer thatoriented along the longitudinal section was placed at the middle region of the MG and LG, and positioned perpendicular to the skin. Then, the B-mode ultrasound was activated to display the appearance of the muscle under the longitudinal section. The grey-scale image was frozen until an image including both superficial and deep aponeuroses, and a number of fibres, were clearly visible. And fascicle length was calculated from the muscle thickness and pennation angle (Bouvier et al., 2017). For the AT, the transducer thatoriented along the transverse section was placed at the AT0cm, AT3cm and AT6cm. The thickness of the AT was the distance between the superior and inferior borders.After that,SWE was used to quantify the stiffness of the MG, LG and AT. The midpoint of the transducer was placed over the three regions of the MG and LG, or over the AT along the fascicle direction (Figure 1). The optimal probe location was determined for the grey- scale image to display several continuously visible fibres of the muscle or the superior-inferior borders of the tendon. In addition, the transducer was kept motionless for more than 5 seconds until the color in the ROI was uniform (Zhang and Fu, 2013). The images were then frozen and placed the Q-box to gain the shear elastic modules. Three values were recorded and averaged. Care was taken not topress and deform the skin surface throughout the scanning process.The order of scans was randomised across the MG, LG, and AT. Immediately after the stretching process, post-tests were performed with the same order of pre-tests.
Figure 1.
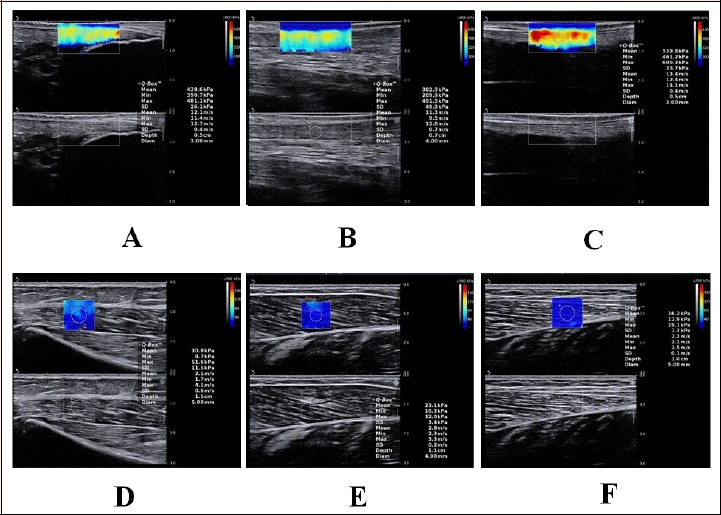
A longitudinal shear wave elastography scale sonogram of the AT and LG shows the measurement of the shear modulus at different regions (from A to F). The color-coded box presentation of muscle-tendon elasticity is shown in the upper images. The longitudinal grey-scale sonograms of muscle-tendon are shown in the bottom images. The Q-Box™ is shown on the right. A-C: the pre-stretching shear modulus values of AT0cm and AT6cm,respectively; D: the pre-stretching shear modulus values of proximal region of the LG; E: the pre-stretching shear modulus values of middle region of the MG; F:the pre-stretching shear modulus values of distal region of the LG.
ROM examination of ankle joint
The angle of ankle was measured by a manual goniometer (Sammons Preston, Royan, Canada). The ROM of the ankle joint was determined starting with the ankle at its neutral position (90-degrees), and then the subject was asked to slowly apply active dorsiflexion up to theirmaximum angle of dorsiflexion. The ROM was measured three times continuously, and at 5-second intervals each time. After the SS, the same procedure was followed starting from the neutral position each time. The mean was used for the follow-up data analysis.
Statistical analysis
All statistical analyses were performed using SPSS (version 19.0 Chicago, IL), and data were expressed as the mean ± standard deviation, however,the mean and the standard deviation reported are not representative of thestatistics due to the paired nature of the analyses. Therefore,the effect size was also calculated using Cohen’s d considering0.2, 0.5, and 0.8 as small, medium, and large effects,respectively. For the gastrocnemius-AT complex, shear modulus values, thickness of the AT, and fascicle length of the MG and LG were obtained and analysed. The Shapiro-Wilk test was used to analyse the normality of the data. Two-way analysis of variances (ANOVAs) were used to determine between-group difference in shear modulus at different measure regions (within subject factors: measure regions; between-subject factor: PRE-SS and POST-SS group). When significant interactions were found, independent t-test for comparisons of means for each dependent measure were used and post-hoc analysis was performed using Bonferroni tests to compare the differences between the groups (adjusted p values are reported). ROM, thickness, and fascicle length were compared by a one-way ANOVA. The post hoc analyses were carried out by means of Bonferroni’s correction. An α error of 0.05 (95% confidence interval) and a desired power of 80% (β error of 0.2) were used.The statistical significance was set at an alpha level of p < 0.05 (α = 0.05).
Results
Shear modulus
The mean shear modulus values of the AT, MG, and LG before and after SS are summarised in Table 1. There was a main effect of location (p < 0.01) for the shear modulus measured before and after SS. The pre-stretching shear modulus values of the MG and LG at the three regions were significantly higher than that of post-stretching (p =0.000), whereasthe pre-stretching shear modulus values of the AT were significantly lower than that of post-stretching (p =0.000). The different regions within the MG in the order of percentage change are as follows: proximal (34.12%±17.35%) >distal (25.27%±20.63%) > middle (22.45%±14.08%), LG was proximal (37.71%±19.61%) >middle (30.47%±16.80%) > distal (22.13%±11.38%), and AT was AT6cm (25.73%±20.72%) >AT0cm (19.53%±12.94%) > AT3cm (17.01%±13.01%).
Table 1.
Effect of static stretching on shear modulus values of gastrocnemius and AT.
| Measurement parts | Transducer location | Pre-stretching (kPa) |
Post-stretching (kPa) |
Percentage change (%) | Cohen’s d | P values |
|---|---|---|---|---|---|---|
| MG | Pro | 28.37±15.13 | 17.22±6.71 | 34.12±17.35 | 0.95 | 0.000 |
| Mid | 18.11±6.94 | 13.56±3.58 | 22.45±14.08 | 0.82 | 0.000 | |
| Dis | 25.67±17.54 | 16.92±6.98 | 25.27±20.63 | 0.66 | 0.000 | |
| LG | Pro | 32.94±13.69 | 19.46±9.33 | 37.71±19.61 | 1.15 | 0.000 |
| Mid | 23.72±8.69 | 15.77±5.51 | 30.47±16.80 | 1.09 | 0.000 | |
| Dis | 22.18±10.98 | 16.59±6.98 | 22.13±11.38 | 0.61 | 0.000 | |
| AT | 0cm | 430.56±53.25 | 512.15±64.14 | 19.53±12.94 | -1.38 | 0.000 |
| 3cm | 400.14±50.49 | 465.32±56.90 | 17.01±13.01 | -1.21 | 0.000 | |
| 6cm | 396.81±65.34 | 487.06±55.50 | 25.73±20.72 | -1.49 | 0.000 |
Pro: Proximal, Mid: middle, Dis: distal.
Changes in stiffness at the three regions
Changes in stiffness at different regions before and after SS are shown in Figure 2. Before stretching, significant differences were found among the three regions within the MG and LG (Figure 2, p < 0.01), with the highest value measured at the proximal region and the smallest in middle region.However,no significant differences were found after stretching (p = 0.05, p = 0.137, respectively). In addition, significant differences were found among the three regions within the AT before and after SS (Figure 2, p < 0.05), with the highest value of AT measured at the AT0cm.
Figure 2.
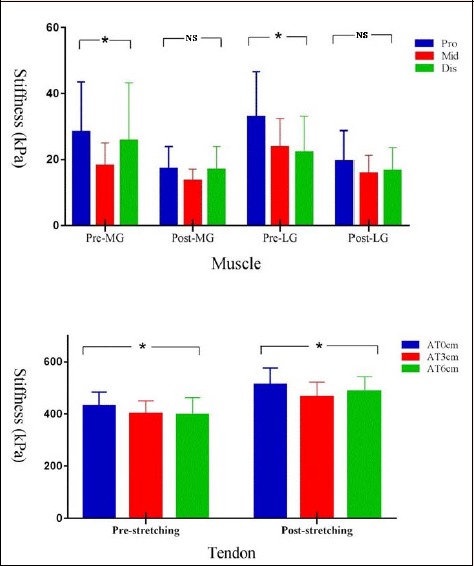
Histogram of mean shear values for the MG, LG, and AT before and after SS. Data are shown as mean values ± standard deviation. * p< 0.05, NS: non-significant at p <0.05. Pro: Proximal region, Mid: Middle region, Dis: Distal region, Pre: Pre-stretching, Post: Post-stretching.
Changes in ROM, thickness, and fascicle length
The mean ROM of the ankle joint, the mean thickness of the AT, and the mean fascicle length of the MG and LG before and after SS are summarized in Table 2. There was no significant difference in the fascicle length of the MG, LG and thickness of the AT before and after SS (p > 0.05). But, after 5 minutes of SS, the ROM of the ankle joint was significantly increased from 26.99±2.14 degrees to 29.11 ±1.95 degrees (ΔROM = 2.1 ± 0.95 deg) (p = 0.000).
Table 2.
Effect of static stretching on fascicle length of MG and LG, thickness of AT, and ROM of ankle joint.
| Thickness (cm) | Fascicle length (cm) | ROM (degrees) | ||||
|---|---|---|---|---|---|---|
| AT0cm | AT3cm | AT6cm | MG | LG | ||
| Pre-stretching | 0.40±0.05 | 0.45±0.06 | 0.29±0.07 | 4.84±0.72 | 5.21±0.77 | 26.99±2.14 |
| Post-stretching | 0.40±0.05 | 0.44±0.06 | 0.29±0.07 | 4.85±0.72 | 5.21±0.75 | 29.11±1.95 |
| P values | 0.61 | 0.36 | 0.19 | 0.36 | 0.67 | 0.00 |
| Percentage change (%) | 0.72±5.49 | 0.75±4.58 | 1.06±5.12 | 0.13±0.96 | 0.17±1.24 | 8.02±3.94 |
Discussion
The main findings of the present study were that (1) the immediate effect of a 5- minute SS was significant decrease in the stiffness of the MG and LG, on the contrary, significant increase in the stiffness of the AT; (2) passive stiffness differs among the different regions within each muscle and tendon.
Immediate effect of SS on MG and LG stiffness
The present findings show that 5 minutes of SS could decrease the stiffness of MG and LG, and the immediate effects of SS are not homogeneous among different regions of the MG and LG. These findings were consistent with the study of Bouvier et al (2017), in which the reduction of the middle region of MG was 19.30%. Moreover, in the study of Akagi and Takahashi (2013), the results showed that SS decreased MG and LG stiffness significantly. However, in the study of Hirata et al (2016), they found that the stiffness of passive muscle differs between the MG and LG, and the significant immediate effect of SS was observed only in stiff muscle (i.e., in MG). The possible reasons for the different experimental results were that in the study of Hirata et al. (2016), stretching was administered by dynamometer at sufficiently slow angular velocity to minimise or avoid thestretch reflex, whichcould increase the muscle stiffness. However, in the present study, the subject was asked to stand on a 30-degree inclined platform, which may lead to an increase in the stiffness of the LG during SS, which greatly decreased after SS.
Intramuscle differences in stiffness
The present study indicates that muscle stiffness differs among the three regions within each muscle (MG and LG). Before SS, significant differences were found among the three regions within the MG and LG, with the highest value measured at the proximal region, and the smallest in middle regions; but, no significant differences were found after stretching. Similar findings were found by Le Sant et al.(2017). They conducted two experiments to evaluate the passive behaviour of the lower leg muscles (including MG and LG) during passive dorsiflexion performed with the knee flexed at 90°or with the knee fully extended. The first experiment showed that the highest stiffness of the MG and LG were exhibited in the distal region, and was followed by the middle regions. The second experiment showed that the highest stiffness of the MG was in distal regions, but in the LG it was in proximal regions. Both experiments displayed regional differences of the MG and LG in stiffness during passive dorsiflexion, and the stiffness was heterogenous within the muscle. However, non-uniform behaviour is present within the MG and LG before SS in our study, and the MG and LG present more homogeneous after SS. In addition, the decrease amplitude of different regions of MG were proximal > distal > middle, whereas that of the LG were proximal > middle > distal. In terms of biomechanics, the possible explanation is that the triceps surae, which has a compliant and slack connection between muscle bellies, leaves a margin for a heterogeneous non-uniform behaviour during passive conditions or low levels of force production, but the tensing of muscle connections would lead to more uniform behaviour during more active conditions (Bogaerts et al., 2018). Therefore, the stiffness of the middle regions is the smallest, and there was a significant difference in muscle stiffness among the three regions before SS, but no significant difference after SS. Furthermore, we found that no matter before or after stretching, shear modulus values of the MG and LG were the greatest in the proximal regions, followed by the distal regions. Given the morphological characteristics of the MG and LG (O’Brien, 2005), the gastrocnemius fascicles of proximal portions insert at the femoral condyle level, which presents curvilinear directions, and the distal portions are directly attached to tendon (Edama et al., 2016). Moreover, the proximal and distal portions are near aponeuroses, which may result in an increased stiffness. Overall, the greatest stiffness of the MG and LG was in the proximal regions, and the smallest was in the middle regions.
Immediate effect of SS on AT stiffness
After SS, the stiffness of AT0cm, AT3cm, and AT6cm increased by 25.73%, 17.01%, and 19.53%, respectively. This finding is consistent with Chiu’s study (Chiu et al., 2016). The results indicated a significant increase in the stiffness value (21.0%±13.5%) after SS. Similarly, the same results were found in the study of Nakamura et al. (2011). The stiffness of the AT was significantly higher immediately after SS compared with pre-stretching. Interestingly, the change of tendon stiffness induced by stretching has been a matter of debate among researchers. On one hand, tendon stiffness decreases after SS were reported by Kato et al. (2010), Cè et al. (2015), and Burgess et al. (2009). On the other hand, some studies reported that stretching decreased muscle stiffness, whereas it had no effect on the tendon properties (Chiu et al., 2016; Morse et al., 2008; Kay and Blazevich, 2009). Besides, Chiu et al. (2016) demonstrated that tendon stiffness showed a significant increase in the non-dominant leg after SS, but not in the dominant leg. Similarly, Nakamura et al. (2013) found that 5 minutes of passive stretching increased tendon stiffness. The different methods used to determine measurement position of tendon (proximal vs. distal), the time of SS (5min vs. 3 min), and stretching modalities (isokinetic vs. manual, passive vs. active) might explain the discrepancies reported among studies. Therefore, the differences in the methodological issues may lead to the differences in measurement results.
Differences in stiffness within the AT
In this study, the stiffness of the AT was non-uniform among the different regions. Previous studies have shown that there are differences in mechanical behaviour among different layers of the AT. Slane et al. (2014) showed that the AT undergoes non-uniform displacement during both eccentric plantar flexor loading and passive, and the displacement of the mid and deep tendon were greater than that of the more superficial tendon when dorsiflexing the ankle. Similarly, Bogaerts et al. (2018) showed a significantly different displacement among superficial, middle, deep layers. The non-uniform deformation of the AT is consistently present, irrespective of knee angle and the level of force production. In addition, Wren et al. (2003) found that the strain distributions were different between the proximal and distal regions of tendons during loading. Furthermore, in our study, a significant difference was found among the three regions within the AT before and after SS, with the highest value of the AT measured at the AT0cm. In terms of anatomy, the thickness and CSA of the AT in different regions differed so that the intra-tendon micro-tearing also differed, leading to the ultimate uneven distribution of AT stiffness (Wang et al., 2012). Moreover, the AT consists of the gastrocnemius and soleus, and the different portions of the gastrocnemius and soleus feature different physiological CSA (Dalmau et al., 2014). Considering the rotatory anatomy and multi-muscles of the AT, it can be assumed that a difference in AT composition has an impact on the non-uniform behaviour of the different regions in the AT (Slane et al., 2014). Moreover, Porta et al. (2014) evaluated the proximal, middle, and distal portions of patellar tendons in healthy subjects by ultrasound. They found that the proximal portion of the patellar tendon was significantly stiffer than the distal portion. This may be because the proximal portion of the tendon has a more compliant endpoint (patella and quadriceps tendon) than the distal attachment (tibial tuberosity). Similarly, the proximal regions of the AT were significantly stiffer than the distal regions, as the distal regions of the AT (AT0cm) have a more incompliant endpoint (calcaneal tuberosity).
Immediate effect of SS on ROM, fascicle length and thickness of the AT
In this study, there was no significant difference in the fascicle length of the MG and the thickness of the AT before and after SS, but the ROM of the ankle joint was significantly increased from 26.99±2.14 degrees to 29.11±1.95 degrees (ΔROM = 2.1 ± 0.95 deg). These findings are consistent with the findings of previous studies. For example, Freitas et al. (2015) conducted a study about muscle and joint responses during and after SS performed at different intensities. They found that no significant changes were observed in MG fascicle length after the stretching. Another study evaluated the immediate effect of SS on normal AT morphology and stiffness (Chiu et al., 2016). The findings showed no significant change in the thickness of the AT after SS in both legs (Chiu et al., 2016). In addition, Akagi and Takahashi (2013) investigated the immediate effects of three periods of 2-minute SS on the stiffness of the MG and LG. The findings showed that SS increased the ROM from 28.9 ± 4.6 to 31.2 ± 5.8 degrees (ΔROM = 2.3 ± 2.0 deg), but did not change joint torque. Moreover, Nakamura et al. (2014) found after a 5-minute SS, dorsiflexion ROM of the ankle joint increased by 3.9 degrees. However, the measurements of ROM was influenced by several factors, such as aponeuroses, tendons, synergistic muscles, joint capsules, stretch tolerance, and ligaments (Maisetti et al., 2012). Thus, muscle-tendon stiffness, which reflected the shear elastic modulus, was recommended as an index for the passive property of the muscle-tendon complex. In this study, our results suggested that 5 minutes of SS can decrease muscle stiffness and increase the stiffness of the AT. Considering the stiffness-related changes in passive properties, an increase in ROM might be influenced by changes in muscle and tendon stiffness. However, it still cannot exclude the influence of ligament, stretch tolerance, and the joint capsule.
Limitations
The present study has some limitations. First, there was no limitation of ankle ROM in healthy young subjects, so in this study only the active ankle motion was measured. Further studies will compare active and passive joint mobility of patients. Second, in the study, stretching was not administered by dynamometer at sufficiently slow angular velocity to minimise or avoid the stretch reflex, which could increase the muscle stiffness. However, in the present study, the subject was asked to stand on a 30-degree inclined platform for 5 minutes, which may lead to minimise or avoid the stretch reflex. Third, EMG was not used during the tests to monitor the muscle activity for ensuring muscle without contraction. However, all participants were verbally instructed to stay relaxed, and no signs of muscle contraction were visible on the B-mode image. Further studies will be needed to investigate the immediate effects of SS on individuals with AT disorders and the delayed effect of SS on different regions of the MG, LG, and AT.
Conclusion
The stretching maneuver could be effective to increase flexibility. Non-uniform behaviour is consistently present within the MG, LG and AT, and the MG and LG appeared more homogeneous after SS. The muscle and tendon architecture was not related to alterations in muscle and tendon stiffness.
Acknowledgements
Part of this study were supported by the “Elite Youth Education Program” of the Guangzhou University of Chinese Medicine (No. QNYC20170107) and the Project of Science Research of Traditional Chinese Medicine of Henan Province of China (No. 2017ZY1004). The experiments comply with the current laws of the country in which they were performed. The authors declare no conflict of interest
Biographies

Jiping ZHOU
Employment
Clinical Medical College of Acupuncture, Moxibustion and Rehabilitation, Guangzhou University of Chinese Medicine, China
Degree
M.S. in Physical Therapy
Research interests
Stretching exercise and muscle flexibility.
E-mail:reha_jp@163.com

Chunlong LIU
Employment
Associate professor, Clinical Medical College of Acupuncture, Moxibustion and Rehabilitation, Guangzhou University of Chinese Medicine, China
Degree
M.S. in Physical Therapy
Research interests
Sports biomechanics; Research and Development of Rehabilitation Equipment
E-mail:polonmpt@163.com

Zhijie ZHANG
Employment
Vice-president, Associate professor, Luoyang Orthopedics Hospital of Henan Province, China
Degree
Ph.D. in Physical Therapy
Research interests
Exercise physiology, skeletal muscle biology, and mechanobiology; Identification, development, and optimisation of treatment and rehabilitation protocols for patients with musculoskeletal.
E-mail:sportspt@163.com
References
- Bogaerts S., De Brito Carvalho C., De Groef A., Suetens P., Peers K. (2018) Non-uniformity in pre-insertional Achilles tendon is not influenced by changing knee angle during isometric contractions. Scandinavian Journal of Medicine & Science in Sports 28(11), 2322-2329. [DOI] [PubMed] [Google Scholar]
- Burgess KE., Graham-Smith P., Pearson SJ. (2009) Effect of acute tensile loading on gender-specific tendon structural and mechanical properties. Journal of Orthopaedic Research. 27(4), 510-516. [DOI] [PubMed] [Google Scholar]
- Bouvier T., Opplert J., Cometti C., Babault N. (2017) Acute effects of static stretching on muscle-tendon mechanics of quadriceps and plantar flexor muscles. European Journal of Applied Physiology 117(7), 1309-1315. [DOI] [PubMed] [Google Scholar]
- Chiu T.C., Ngo H.C., Lau L.W., Leung K.W., Lo M.H, Yu H.F., Ying M. (2016) An Investigation of the Immediate Effect of Static Stretching on the Morphology and Stiffness of Achilles Tendon inDominant and Non-Dominant Legs. PLoS One 11(4), e0154443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cè E., Longo S., Rampichini S., Devoto M., Limonta E., Venturelli M., Esposito F. (2015) Stretch-induced changes in tension generation process and stiffness are not accompanied by alterations in muscle architecture of the middle and distal portions of the two gastrocnemii. Journal of Electromyography and Kinesiology 25(3), 469-478. [DOI] [PubMed] [Google Scholar]
- Cenni F., Schless SH., Bar-On L., Molenaers G., Van CA., Aertbeliën E., Bruyninckx H., Hanssen B., Desloovere K. (2018) Can in Vivo Medial Gastrocnemius Muscle-Tendon Unit Lengths be Reliably Estimated by Two Ultrasonography Methods? A Within-Session Analysis. Ultrasound in Medicine & Biology 44(1),110-118. [DOI] [PubMed] [Google Scholar]
- Dalmau-Pastor M., Fargues-Polo B., Casanova-Martínez D., Vega J., Golanó P. (2014) Anatomy of the triceps surae: a pictorial essay. Foot and Ankle Clinics 19(4), 603-635. [DOI] [PubMed] [Google Scholar]
- Eby SF., Song P., Chen S., Chen Q., Greenleaf J.F., An K.N. (2013) Validation of shear wave elastography in skeletal muscle. Journal of Biomechanics 46(14), 2381-2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edama M., Kubo M., Onishi H., Takabayashi T., Yokoyama E., Inai T., Watanabe H., Nashimoto S., Kageyama I. (2016) Structure of the Achilles tendon at the insertion on the calcaneal tuberosity. Journal of Anatomy 229(5), 610-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freitas S.R., Andrade R.J., Larcoupaille L., Mil-homens P., Nordez A. (2015) Muscle and joint responses during and after static stretching performed at different intensities. European Journal of Applied Physiology 115(6), 1263-1272. [DOI] [PubMed] [Google Scholar]
- Hirata K., Miyamoto-Mikami E., Kanehisa H., Miyamoto N. (2016) Muscle-specific acute changes in passive stiffness of human triceps surae after stretching. European Journal of Applied Physiology 116(5), 1-8. [DOI] [PubMed] [Google Scholar]
- Hodges P.W., Pengel L.H., Herbert R.D., Gandevia S.C. (2003) Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 27(6), 682-692. [DOI] [PubMed] [Google Scholar]
- Haen T.X., Roux A., Soubeyrand M., Laporte S. (2017) Shear waves elastography for assessment of human Achilles tendon’s biomechanical properties: an experimental study. Journal of the Mechanical Behavior of Biomedical Materials 69, 178-184. [DOI] [PubMed] [Google Scholar]
- Kato E., Fukunaga H.K. (2010) Changes in ankle joint stiffness due to stretching: The role of tendon elongation of the gastrocnemius muscle. European Journal of Sport Science 10(2), 111-119. [Google Scholar]
- Kay A.D., Blazevich A.J. (2009) Moderate-duration static stretch reduces active and passive plantar flexor moment but not Achilles tendon stiffness or active muscle length. Journal of Applied Physiology 106(4), 1249. [DOI] [PubMed] [Google Scholar]
- Le Sant G., Nordez A., Hug F., Andrade R., Lecharte T., McNair P.J., Gross R. (2019) Effects of stroke injury on the shear modulus of the lower leg muscle during passive dorsiflexion. Journal of Applied Physiology (1985) 126(1), 11-22. [DOI] [PubMed] [Google Scholar]
- Le Sant G., Nordez A., Andrade R., Le Sant G., Nordez A., Andrade R., Hug F., Freitas S., Gross R. (2017) Stiffness mapping of lower leg muscles during passive dorsiflexion. Journal of Anatomy 230(5), 639-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse CI., Degens H., Seynnes OR., Maganaris C.N., Jones D.A. (2008) The acute effect of stretching on the passive stiffness of the human gastrocnemius muscle tendon unit. The Journal of physiology 586(1), 97-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisetti O, Hug F., Bouillard K., Nordez A. (2012) Characterization of passive elastic properties of the human medial gastrocnemius muscle belly using supersonic shear imaging. Journal of Biomechanics 45, 978-984. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Takeno Y., Ichihashi N. (2011) Acute and prolonged effect of static stretching on the passive stiffness of the human gastrocnemius muscle tendon unit in vivo. Journal of Orthopaedic Research 29(11), 1759-1763. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Takeno Y., Ichihashi N. (2013) Time course of changes in passive properties of the gastrocnemius muscle-tendon unit during 5 min of static stretching. Manual Therapy, 211-215. [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Kobayashi T., Umegaki H., Takeno Y., Nishishita S., Ichihashi N. (2014) Acute effects of static stretching on muscle hardness of the medial gastrocnemius muscle belly in humans: an ultrasonic shear-wave elastography study. Ultrasound in Medicine & Biology 40(9), 1991-1997. [DOI] [PubMed] [Google Scholar]
- O’Brien M. (2005) The anatomy of the Achilles tendon. Foot and Ankle Clinics 10(2), 225-238. [DOI] [PubMed] [Google Scholar]
- Porta F., Damjanov N., Galluccio F., Iagnocco A., Matucci-Cerinic M. (2014) Ultrasound elastography is a reproducible and feasible tool for the evaluation of the patellar tendon in healthy subjects. International Journal of Rheumatic Diseases 17(7), 762-766. [DOI] [PubMed] [Google Scholar]
- Peltz C.D., Haladik J.A., Divine G., Siegal D., van Holsbeeck M., Bey M.J. (2013) ShearWaveelastography: repeatability for measurement of tendon stiffness. Skeletal Radiology 42(8), 1151-1156. [DOI] [PubMed] [Google Scholar]
- Payne C., Watt P., Cercignani M., Webborn N. (2018) Reproducibility of shear wave elastographymeasuresof the Achilles tendon. Skeletal Radiology 47(6), 779-784. [DOI] [PubMed] [Google Scholar]
- Romero-Morales C, Martín-Llantino PJ., Calvo-Lobo C., Palomo-López P., López-López D., Pareja-Galeano H., Rodríguez-Sanz D. (2019) Comparison of the sonographic features of the Achilles Tendon complex in patients with and without achilles tendinopathy: A?case-control study. Physical Therapy in Sport 35, 122-126. [DOI] [PubMed] [Google Scholar]
- Rosario J.L., Foletto Á. (2015) Comparative study of stretching modalities in healthy women: heating and application time. Journal of Bodywork and Movement Therapies 19, 3-7. [DOI] [PubMed] [Google Scholar]
- Saeki J., Ikezoe T., Nakamura M., Nishishita S., Ichihashi N. (2017) The reliability of shear elastic modulus measurement of the ankle plantar flexion muscles is higher at dorsiflexed position of the ankle. Journal of Foot and Ankle Research 10, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slane L.C., Thelen D.G. (2014) Non-uniform displacements within the Achilles tendon observed during passive and eccentric loading. Journal of Biomechanics 47(12), 2831-2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos C.X., Beltrão N.B., Pirauá A.L.T., Durigan J.L.Q., Behm D., de A., Rodrigo C. (2019) Static Stretching Intensity Does Not Influence Acute Range of Motion, Passive Torque, and Muscle Architecture. Journal of Sport Rehabilitation, 1-6. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Wang J.H., Guo Q., Li B. (2012) Tendon biomechanics and mechanobiology--a minireview of basic concepts and recent advancements. Journal of Hand Therapy 25(2), 133-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wren T.A., Lindsey D.P., Beaupré G.S., Carter D.R. (2003) Effects of creep and cyclic loading on the mechanical properties and failure of human Achilles tendons. Annals of Biomedical Engineering 31(6), 710-717. [DOI] [PubMed] [Google Scholar]
- Zhang Z.J., Fu S.N. (2013) Shear Elastic Modulus on Patellar Tendon Captured from Supersonic Shear Imaging: Correlation with Tangent Traction Modulus Computed from Material Testing System and Test-Retest Reliability. PLoS One 8(6), e68216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z.J., Ng G.Y., Lee W.C., Fu S.N. (2014) Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS One 9(10), e108337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZJ, Ng GYF, Lee WC, Fu SN. (2017) Increase in passive muscle tension of the quadriceps muscle heads in jumping athletes with patellar tendinopathy. Scandinavian Journal of Medicine Science in Sports 27(10), 1099-1104. [DOI] [PubMed] [Google Scholar]
- Akagi R., Takahashi H. (2013) Acute effect of static stretch-ing on hardness of the gastrocnemius muscle. Medicine and Science in Sports Exercise 45(7), 1348-1354. [DOI] [PubMed] [Google Scholar]


