Abstract
The purpose of the study was to examine whether a higher aerobic fitness in 9-10 year old children is related to superior macro and microvascular health and cardiovascular disease (CVD) risk. Ninety-six 9-10 year olds (53 boys) completed the study. Body composition was assessed from air displacement plethysmography and magnetic resonance imaging. Peak oxygen uptake (V̇O2) was assessed from a ramp-incremental cycling exercise test. Macrovascular outcomes were assessed from pulse wave analysis and pulse wave velocity (PWV) using applanation tonometry. Microvascular function was assessed from the functional microvascular reserve and skin erythrocyte flux after iontophoretic application of skin vasodilators. Assessment of CVD risk was assessed via body mass index, total body fat percentage and visceral adipose tissue, glucose, triglyceride, total cholesterol, HDL cholesterol and LDL cholesterol, while insulin resistance was calculated using Homeostatic model assessment. Aerobic fitness groups (higher vs lower) were calculated from V̇O2 peak scaled for body mass (mL·kg-0.61·min-1) and fat free mass (mL·FFM-1·min-1). Children with a higher V̇O2 peak scaled for body mass had a greater carotid to ankle PWV compared to those with lower aerobic fitness (mean ± SD: 6.08 ± 0.47 vs. 5.87 ± 0.43 m·s-1; p = 0.039), although this became non-significant when scaled for FFM (p = 0.56). No other mean differences in vascular or CVD risk health markers were present between higher and lower groups of aerobic fitness when scaled for body mass or FFM. Conclusion: Directly assessed aerobic fitness is not related to macro and microvascular health outcomes or CVD risk markers in 9-10 year olds.
Key points.
Children with a greater aerobic fitness had a higher carotid to ankle PWV compared to the lower fitness group when scaled for body mass, but not when adjusted for FFM.
When split into higher and lower groups for aerobic fitness and adjusted for TBF%, no differences in CVD risk factors were observed.
Higher levels of aerobic fitness, irrespective of normalisation for body mass or FFM, was not associated with improved vascular or CVD risk health outcomes in 9-10 year old children.
Key words: Peak oxygen uptake, heart disease, youth, blood vessel
Introduction
Cardiovascular diseases (CVD) are the leading causes of non-communicable deaths worldwide (WHO, 2018). Although the consequences of CVD, such as a myocardial infarction or stroke, do not manifest until adulthood, the pathobiology of CVD begins in childhood (Juonala et al., 2005). The atherosclerotic process is progressive and is associated with the development of CVD risk factors during childhood as well as early deterioration in vascular function (Aggoun et al., 2005). Promoting cardiovascular health in childhood and identifying those with elevated risk is therefore important for the prevention of CVD outcomes in adulthood (Urbina et al., 2009).
Aerobic fitness is a strong predictor of cardiovascular health with low aerobic fitness being associated with elevated CVD risk in children and adolescents (Barker et al., 2018; Ekelund et al., 2007; Steele et al., 2008). Conversely, a high level of aerobic fitness has been associated with lower blood pressure (Nielsen and Andersen, 2003), improved lipid profiles (Hager et al., 1995), lower levels of inflammatory markers (Isasi et al., 2003), lower rates of obesity (Janz et al., 2002) and enhanced insulin sensitivity (Lee et al., 2006) in children and adolescents. More recently, aerobic fitness during adolescence has also been found to relate to myocardial infarction (Högström et al., 2014) and mortality (Högström et al., 2016) in adult life. These data suggest a possible protective effect of attaining high levels of aerobic fitness within youth upon CVD risk factors and vascular and haemodynamic function.
Exercise training has been shown to enhance both macro and microvascular function in adults (Green et al., 2011) and adolescents (Bond et al., 2015). Data in healthy children are sparse, but an association between aerobic fitness and macrovascular function has been shown in 6 to 11 year old children (Agbaje et al., 2019; Hopkins et al., 2009; Reed et al., 2005; Veijalainen et al., 2016). Sakuragi and colleagues (2009) also reported a negative association between aerobic fitness and arterial stiffness in 573 10-year olds, although the association became weaker after adjusting for adiposity. Aerobic fitness was assessed indirectly using the 20 m shuttle run test, which although correlates with a direct measurement of peak oxygen uptake (V̇O2 peak) in children (Castro-Pinero et al., 2010), the explained variance can be less than 50% (Mayorga-Vega et al., 2015). Furthermore, the test is strongly influenced by adiposity (Olds and Dollman, 2004) and has been criticised for being a measure of performance and thereby its use as a prediction for estimating peak V̇O2 has been questioned (Armstrong, 2018). Thus, the recommended ‘gold-standard’ measurement of aerobic fitness requires gas analysis during maximal exercise to directly measure V̇O2 peak (Barker et al., 2013) with adjustment for body size and composition (Loftin et al., 2016). Nadeau and colleagues (2010) directly measured V̇O2 peak and reported a positive correlation with forearm blood flow in healthy adolescents and adolescents with type I diabetes. Although the group directly measured V̇O2 peak, it was expressed as a ratio-standard for body mass (mL.kg-1.min-1) which may not adequately control for body size (Welsman and Armstrong, 2000). Allometric scaling methods are recommended to control for the influence of body size on aerobic capacity and have been shown to reduce the size of the relationship between aerobic fitness and markers of CVD risk in children when compared to the ratio standard method and after accounting for body composition (Agbaje et al., 2019).
Microvascular dysfunction is an important predictor of early atherosclerosis (Wilkins et al., 2012) and provides additional valuable information on vascular risk. However, our understanding of the relationship with fitness and microvascular function in paediatric groups is limited. There is evidence to suggest more physically active children have better retinal arteriolar caliber (Gopinath et al., 2011) but not microvascular function (Radtke et al., 2013). Reed and colleagues (2005) identified that healthy children with higher levels of aerobic fitness had improved small vessel function, although only arterial stiffness was assessed and V̇O2 peak was estimated from the 20 m shuttle run test. Paediatric analyses of microvascular function have typically included overweight or obese children (representing > 50% of the sample) (Bastos da Cunha et al., 2017; Hedvall Kallerman et al., 2014) or those with type I diabetes (Roche et al., 2008). Furthermore, studies that have focused on the association between microcirculatory function and aerobic fitness typically use a single measure of vascular function (Reed et al., 2005) or quantify aerobic fitness using the ratio standard expression for V̇O2 peak without appropriate statistical justification (Roche et al., 2008).
The aim of this study was to examine differences in macro and microvascular function between 9-10 year old children stratified for ‘higher’ and ‘lower’ directly assessed aerobic fitness (i.e. V̇O2 peak) with appropriate adjustment for body size and composition. We also explored differences in CVD risk factors and blood markers including insulin resistance between levels of aerobic fitness. We hypothesised that: 1) children with higher aerobic fitness will have superior macro and microvascular function in comparison to those with lower aerobic fitness, even after adjusting for adiposity and 2) children with lower aerobic fitness will have a poorer CVD risk factor profile including increased insulin resistance compared to those with higher aerobic fitness.
Methods
Participants
Children from three state primary schools in the South West of England were invited to participate in the study and 100 children (53 males, 47 females) aged nine and 10 years volunteered. One girl withdrew following her initial visit and three girls were removed from the study due to use of vasoactive medication leaving a total sample of 96 children (53 males, 43 females). Written informed assent and consent was obtained from the child and their parents/guardians respectively. A medical screening questionnaire was completed and signed by the parents/guardians. The Local Medical Research Ethics Committee provided ethical approval for the study.
The children visited the University laboratories on three occasions over a 1-month period where practical. During the first visit anthropometric measures and body composition were assessed. During the second visit a maximal exercise test was completed and during the third visit vascular function and blood markers were assessed.
Anthropometry
Measurements were performed while the child was wearing either a lightweight t-shirt and shorts or a swimming costume with no footwear. Stature was measured using a stadiometer to the nearest 0.01 m. Body mass was assessed with a balance beam scale and recorded to the nearest 0.1 kg. Body mass index (BMI) was calculated. Children were classified as lean, overweight or obese using age and sex-specific BMI cut-offs (Cole et al., 2000).
Total body fat percentage (TBF%) was calculated following air displacement plethysmography (BOD POD 2000A). Body volume was adjusted for lung volume using tidal volume estimates. TBF% was calculated from body density using Lohman’s child adjusted Siri equation (Lohman, 1989). TBF% was obtained in 86 of the participants and subsequently used to estimate fat free mass (FFM).
Visceral adipose tissue (VAT) was assessed using magnetic resonance imaging. Examinations were performed using a 1.5 Tesla superconducting magnetic resonance scanner (Gyroscan Intera, Philips). Interleaved transverse slices (8 mm thick, with a 1 mm gap between them) were acquired from lumbar region (L)1 to L5 with a typical voxel size of 2.5 x 3.5 x 8.0 mm. Scanning was performed with the participant performing a ~ 20 s breath hold to minimize movement artifacts. Data are reported for 86 children for whom successful scans were obtained. The estimated volumes for VAT and the total cavity from L1 to L5 in cm3 were determined.
Aerobic fitness
Peak V̇O2 was determined during a ramp exercise test to volitional exhaustion on an electro-magnetically braked cycle ergometer (Excaliber Sport; Lode). Heart rate (HR) was measured continuously using HR telemetry (Polar Vantage NV, Polar Electro Oy). Gas exchange variables (e.g. V̇O2), were measured continuously using an online breath-by-breath metabolic cart (Cortex Metalyzer 3B; Cortex Medical) which was calibrated prior to each test. The test began with a 5-minute warm up at 20 watts (W), followed by a 10 W increment per minute protocol until voluntary exhaustion, despite strong verbal encouragement. Participants were asked to maintain a pedal cadence of ~ 70 rpm throughout the test. Peak V̇O2 was taken as the highest 10 s average V̇O2 during the test, which in our laboratory results in the measurement of a true maximal V̇O2 in ~ 90% of cases (Barker et al., 2011; Sansum et al., 2019). Absolute peak V̇O2 (L·min-1) was initially ratio scaled to body mass (mL·kg-1·min-1) and FFM (mL·kg FFM-1·min-1). Preliminary analyses revealed a significant residual size correlation for ratio scaling of body mass (r = -0.40; p < 0.001), demonstrating the invalidity of this method. Therefore, a log-linear allometric model controlling for sex (Welsman and Armstrong, 2000), was used to identify a scaling exponent (b = 0.61) for body mass. This exponent was subsequently used for both sexes to allometrically scale peak V̇O2 via the power function ratio (mL·kg-0.61·min-1), which no longer correlated with body mass (r = -0.06; p = 0.58). In contrast, as ratio scaling of peak V̇O2 with FFM satisfied the statistical assumptions underlying ratio scaling (Welsman and Armstrong, 2019), allometric scaling was not required in this case.
Vascular function
Vascular function was assessed in the morning following an overnight fast and conducted in a quiet, temperature-controlled room (22.0 ± 0.5 °C) with the child lying in the supine position following an acclimatisation period of 30 minutes.
Pulse wave analysis
Applanation tonometry of the radial pulse of the right arm enabled analysis of the peripheral waveforms. A high-fidelity micromanometer (SphygmoCor®; AtCor Medical Pty. Ltd., Sydney, Australia) was used to flatten, but not occlude, the radial artery using gentle pressure. The waveforms were visually displayed on a portable microcomputer using online recording software (SphygmoCor® version 7.01; AtCor Medical Pty. Ltd., Sydney, Australia). A three-lead electrocardiogram (ECG) incorporated within the SphygmoCor® software displayed ECG waveforms alongside peripheral waveforms simultaneously and enabled the R wave peak to be used as a reference point. After two sequential screens of clear waveforms (using all complete and satisfactory complexes within a 10 second period), the averaged peripheral and corresponding central arterial waveform were recorded. Measures were taken in triplicate and the mean value used. The resulting augmentation index (AI) was assessed as the size of the reflected peak with respect to the primary peak. Since the transformation of pulse wave analysis using central pressures has not been validated in children under the age of 17 years (Khan et al., 2006), the peripheral non-transformed index (PAI) was used. The intra-individual coefficient of variation (CV) of PAI in our laboratory is 8.5%.
Pulse wave velocity (PWV)
To determine PWV, pressure waveforms were recorded at two sites sequentially: carotid to radial for brachial PWV and carotid to posterior tibial (ankle) for aortic PWV. We chose to use the posterior tibial rather than the femoral artery because of potential embarrassment for the participants, leading to measurement refusal. Although less commonly used than the femoral site, the tibial site has previously been used in the assessment of PWV in pre-school aged children (Currie et al., 2010). Distances between the radial and carotid artery, carotid artery and sternal notch (to represent the top of the aortic arch) and sternal notch and posterior tibial artery, were measured as straight lines between those points on the body surface using an anthropometric tape measure. The pulse wave transit time was calculated using the R wave of the simultaneously recorded ECG as the point of cardiac ejection, and the arrival of the systolic pulse at the distal site, using the tonometer. The time taken between cardiac ejection and pulse arrival represented the pulse wave transit time. After manual entry of distances the software calculated PWV (m.s-1) as distance (m) divided by pulse wave transit time (s) (O'Rourke et al., 2002). Measures were taken in triplicate at the different sites and the mean recorded. The intra-individual CV for the PWV measurement in our laboratory is 3.6 % for brachial (carotid to radial) PWV and 6.0 % for aortic (carotid to ankle) PWV.
Functional Microvascular Reserve (FMR)
The maximal hyperemic response to a local heat stimulus was determined using a single point laser Doppler flow meter probe (Pf2; Perimed) in accordance with previous studies in our laboratory (Middlebrooke et al., 2005; Middlebrooke et al., 2006) and is described in detail elsewhere (Rayman et al., 1986). In brief, a thermocouple was attached to the dorsal site of the foot immediately adjacent to the heating site. The foot was then gently warmed to 36°C before being heated to 42°C using a small brass heater (Shore et al., 1991). In order to reduce the burden on the participants the typical heating phase of 30 minutes was reduced by 10 minutes. A 20 minute heating period has been shown to be sufficient in inducing maximum hyperaemia (Gooding et al., 1999) and has previously been used to determine maximal hyperaemia in young participants (Goh et al., 2001). With the heater remaining in situ, erythrocyte flux was measured at eight adjacent sites within the heated area, for 30 seconds at each site. The final value was calculated as the mean of the eight sites, measured in volts and used for later analysis in line with previous work (Middlebrooke et al., 2005; Middlebrooke et al., 2006). The mean intra-individual CV for FMR was 11.1 %.
Iontophoresis of acetylcholine (ACh) and sodium nitroprusside (SNP)
Iontophoresis was used in combination with laser Doppler perfusion imaging in order to investigate the vasodilatory response of the microcirculation to endothelial dependent (ACh) and independent (SNP) stimuli. The protocol outlined below has been described previously in detail (Middlebrooke et al., 2005; Middlebrooke et al., 2006; Stone et al., 2009) and has been developed within our laboratories over a number of years in order to elicit maximal drug delivery.
Prior to iontophoresis assessment, the volar aspect of the right forearm of the participant was thoroughly cleaned. The iontophoresis chambers (Moor Instruments Ltd., Devon, UK), consisting of a Perspex® ring with an internal diameter of 10 mm, were firmly secured to an area of forearm free from hair (where possible), freckles and broken skin using a double-sided adhesive ring. A conductive hydro-gel pad (Moor Instruments Ltd., Devon, UK) was attached to the right wrist, which served as a reference or ‘indifferent’ electrode, in order to complete the electrical circuit. Both the chamber and the indifferent electrode were connected to an iontophoresis controller (DRT4; Moor Instruments Ltd, Axminster, UK).
For each test, solution was administered into the centre of the appropriate chamber with a glass cover slip placed on top. A laser Doppler imager (PIM II LDI; Lisca Development AB, Linköping, Sweden) was used to assess erythrocyte flux (in response to the iontophoretically introduced substance) at a distance of 130 mm from the region of interest on the skin surface. A non-reflective cloth was placed over the laser head and test site in order to reduce the interference of external light on the measurements.
Prior to the assessment of drug perfusion a vehicle response was obtained for each drug with 3% mannitol (RD&E Hospital, Devon, UK) and 0.45% saline (Fresenius Kabi Ltd., Warrington, UK). Following assessment of vehicle responses, a solution of 1% ACh (20 mg acetylcholine chloride and 60 mg mannitol in 2 mL of distilled deionised water; Novartis Pharmaceuticals UK Ltd., Surrey, UK) was delivered using a anodal (positive) charge with five doses (100 μA) for 20 seconds with a 60 second interval between each dose, resulting in a total charge of 10 mC over the skin. Forearm skin erythrocyte flux was recorded immediately prior to the first charge (baseline), at the onset of each charge, and then 20 seconds after the end of each charge period resulting in a total of 12 scans.
SNP (0.25%; Mayne Pharma Plc., Warwickshire, UK) was delivered using a cathodal (negative) charge with one dose (200 μA) for 60 seconds, followed by five minutes of zero charge resulting in a total charge of 12 mC over the skin. Forearm skin erythrocyte flux was measured by a single perfusion image immediately prior to the first charge (baseline) and then every 60 seconds for six minutes, resulting in a total of seven scans.
Data were expressed as the forearm skin red blood cell flux over an area of 0.78 cm2. A typical response to the iontophoresis delivery of ACh and SNP in two different participants is illustrated in Figure 1, both demonstrating a plateau in flux representative of a maximal vasodilatory response. The responses to ACh and SNP were expressed as peak response and area under the curve (AUC) respectively, measures which we have previously shown to represent endothelial dependent and independent function (Middlebrooke et al., 2005; Middlebrooke et al., 2006; Stone et al., 2009). The mean intra-individual CV for the peak response and AUC in our laboratory is 15.0 % and 18.5 % for ACh and 13.1 % and 25.9 % for SNP respectively, and compare favorably with previous work of ours (Middlebrooke et al., 2006; Morris et al., 1995) and that of others (Puissant et al., 2013).
Figure 1.
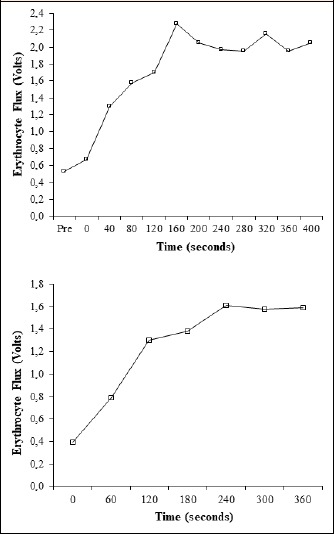
Typical erythrocyte response to ACh (top graph) and SNP (bottom graph).
Blood markers of CVD risk
A trained clinician drew fasting venous blood samples after all vascular measurements had been completed. Sixteen children did not give blood samples since two refused assent at recruitment and an adequate sample could not be obtained from the remaining 14. Enzymatic assays were performed using a Roche modular analyser (Roche Diagnostics, Lewes, UK) in order to obtain measures of plasma glucose, total cholesterol, triglyceride (TG) and high density lipoprotein cholesterol (HDL-C), while low density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald formula (Friedewald et al., 1972). Insulin was measured using a specific immunoenzymometric assay calibrated against International Reference Preparation 66/304 and with no detectable cross-reactivity with intact proinsulin or 32-33 split proinsulin. An Excel version of the homeostatic model assessment (HOMA) calculator (version 2.2) was used to calculate β-cell function, insulin sensitivity (HOMA-IS) and insulin resistance (HOMA-IR) (OCDEM, 2004). The CV for glucose is 1.8 %, for total cholesterol 2.3 %, for TG 2.9 %, for HDL-C 2.2 %, while the interassay CV for specific insulin is less than 10 % over the range 95 to 1038 pmol·L-1.
Statistical analyses
Statistical analyses were performed using SPSS for Windows (version 21; SPSS, Chicago, IL, US). Data are expressed as mean ± standard deviation unless stated otherwise. Data that were not normally distributed were log-transformed (visceral fat volume/total volume ratio, carotid-radial PWV, carotid-ankle PWV, total cholesterol, LDL-C, TG, specific insulin, β cell function, HOMA-IS and HOMA-IR) for analyses, but non-transformed descriptive data are presented for ease of interpretation. Sex differences in body composition, blood markers, peak V̇O2 and micro and macrovascular function were assessed using independent sample Student t tests. Pearson’s correlation coefficient was used to examine the association between measures of body composition (i.e. BMI, TBF%, VAT) and vascular and blood markers for the whole group and boys and girls separately. Pearson’s correlations were also used to investigate the relationship between peak V̇O2 (ratio scaled to FFM and allometrically scaled to body mass) and measures of macro and microvascular function. Sex-specific quartiles for peak V̇O2 allometrically scaled for body mass (mL.kg-0.61.min-1) and ratio scaled for FFM (mL.FFM-1.min-1) were calculated to form ‘higher’ and ‘lower’ aerobic fitness groups using a median split (i.e. quartile 1&2 vs quartile 3&4). Univariate analyses of variance (ANOVAs) compared mean differences in the vascular and blood outcomes between the aerobic fitness groups after adjusting for body composition if required. Specifically, where a significant correlation between a measure of body composition and the vascular or blood markers were identified, this was entered as a covariate into the ANOVA model. Statistical significance was set at an alpha level of 0.05.
Results
The physical and aerobic fitness characteristics of the 96 children are displayed in Table 1. There were no differences between girls and boys for age, stature, body mass, BMI, VAT or VAT:total volume ratio. TBF% was greater in girls compared to boys. Of the 96 children, four were classified as obese (three girls) and nine classified as overweight (seven girls). Boys had a higher peak V̇O2 compared to girls when expressed in absolute terms and when scaled for body mass (mL·kg-0.61·min-1) and FFM (mL.FFM-1·min-1).
Table 1.
Anthropometric and exercise test characteristics. Values are mean ± SD
| Whole Group (n=96) | Boys (n=53) | Girls (n=43) | P-value | |
|---|---|---|---|---|
| Age (y) | 9.9 ± 0.4 | 9.9 ± 0.3 | 9.9 ± 0.4 | 0.66 |
| Stature (m) | 1.39 ±0.08 | 1.38 ±0.06 | 1.39 ±0.09 | 0.70 |
| Body mass (kg) | 33.4 ±6.9 | 32.9 ± 5.0 | 34.1 ±8.8 | 0.42 |
| BMI (kg·m-2) | 17.2 ±2.4 | 17.1±1.9 | 17.4± 2.9 | 0.73 |
| TBF% | 17.9 ± 8.4 (n=86) | 15.7 ± 8.2 (n=50) | 21.0 ± 7.9 (n=36) | 0.003 |
| VAT (cm3) | 120.2 ± 75.9 (n=86) | 117.6 ± 69.0 (n=49) | 123.6 ± 85.0 (n=37) | 0.72 |
| VAT as a % of total volume | 4.70 ± 1.84 (n=86) | 4.64 ± 1.75 (n=49) | 4.78 ± 1.98 (n=37) | 0.73 |
| Peak oxygen uptake (L·min-1) | 1.37 ± 0.28 | 1.45 ± 0.25 | 1.27 ± 0.29 | 0.001 |
| Peak oxygen uptake (mL·kg-0.61.min-1) | 160.6 ± 28.5 | 171.7 ± 26.5 | 147.1 ± 25.1 | <0.001 |
| Peak oxygen uptake (mL·FFM-1.min-1) | 50.7 ± 8.2 (n=86) | 52.5 ± 8.4 (n=49) | 48.2 ± 7.3 (n=37) | 0.015 |
Sample size (n=) is provided when different from the whole group. Significant p values are highlighted in bold. BMI - body mass index; TBF% - total body fat percentage; VAT - visceral adipose tissue; FFM – fat free mass.
The vascular and blood outcomes are displayed in Table 2. There were no significant sex-differences for the vascular and blood outcomes.
Table 2.
Vascular and blood characteristics. Values are mean ± standard deviation.
| Whole Group | Boys | Girls | ||
|---|---|---|---|---|
| Macrovascular | PAI (%) | 49.3 ± 9.9 (n=93) | 48.2 ± 9.6 (n=50) | 50.5 ± 10.2 (n=43) |
| Carotid to ankle PWV (m.s-1) | 5.97 ± 0.46 (n=90) | 5.94 ± 0.46 (n=50) | 6.02 ± 0.47 (n=40) | |
| Carotid to radial PWV (m.s-1) | 6.64 ± 0.74 (n=94) | 6.59 ± 0.66 (n=52) | 6.70 ± 0.83 (n=42) | |
| Microvascular | FMR (V) | 1.78 ± 0.37 (n=96) | 1.78 ± 0.32 (n=53) | 1.79 ± 0.44(n=43) |
| Peak ACh response (V) | 1.96 ± 0.42 (n=93) | 1.97 ± 0.46 (n=51) | 1.95 ± 0.37 (n=42) | |
| ACh AUC (V x time) | 479.6 ± 132.1 (n=92) | 488.5 ± 140.2 (n=50) | 469.1 ± 122.5 (n=42) | |
| Peak SNP response (V) | 1.62 ± 0.49 (n=69) | 1.65 ± 0.48 (n=38) | 1.59 ± 0.51 (n=31) | |
| SNP AUC (V x time) | 285.9 ± 113.6 (n=69) | 291.6 ± 112.8 (n=38) | 278.9 ± 115.9 (n=31) | |
| Blood | Total cholesterol (mmol.L-1) | 4.50 ± 0.46 (n=79) | 4.53 ± 0.66 (n=49) | 4.47 ± 0.47 (n=30) |
| HDL-C (mmol.L-1) | 1.86 ± 0.42 (n=78) | 1.89 ± 0.44 (n=49) | 1.80 ± 0.39 (n=29) | |
| LDL-C (mmol.L-1) | 2.29 ± 0.59 (n=78) | 2.28 ± 0.55 (n=49) | 2.30 ± 0.66 (n=29) | |
| TG (mmol.L-1) | 0.80 ± 0.29 (n=79) | 0.77 ± 0.29 (n=49) | 0.84 ± 0.30 (n=30) | |
| Glucose (mmol.L-1) | 4.33 ± 0.42 (n=80) | 4.32 ± 0.40 (n=49) | 4.35 ± 0.36 (n=31) | |
| Specific insulin (pmol.L-1) | 48.0 ± 25.0 (n=77) | 44.2 ± 24.1 (n=46) | 53.6 ± 25.6 (n=31) | |
| β-cell function (%) | 124.5 ± 45.6 (n=77) | 117.4 ± 45.7 (n=46) | 135.0 ± 44.1 (n=31) | |
| HOMA-IS (%) | 141.2 ± 87.1 (n=77) | 153.0 ± 90.1 (n=46) | 123.7 ± 80.6 (n=31) | |
| HOMA-IR | 0.98 ± 0.51 (n=77) | 0.90 ± 0.48 (n=46) | 1.09 ± 0.52 (n=31) | |
Values are mean ± standard deviation. Sample size (n=) is provided for each outcome. PAI - peripheral non-transformed augmentation index; PWV - pulse wave velocity; FMR - functional microvascular reserve; ACh - acetylcholine; AUC - area under the curve; SNP - sodium nitroprusside; HDL-C - high density lipoprotein cholesterol; LDL-C – low density lipoprotein cholesterol; TG -Triglyceride; HOMA – Homeostatic model assessment; IS – Insulin sensitivity; IR – Insulin resistance.
Body composition and vascular outcomes
When assessed as a whole group and in both boys and girls separately there was a negative correlation between BMI and carotid to ankle PWV in the whole group (r = -0.24; p = 0.020) and boys (r = -0.30; p = 0.038) but not girls (r = -0.24; p = 0.13). Positive correlations were observed between TBF% and both peak SNP response (r = 0.33; p = 0.008) and SNP AUC (r = 0.332; p = 0.008) for the whole group, which remained in boys (r = 0.36; p = 0.028 and r = 0.34; p = 0.038) and girls (r = 0.40; p = 0.045 and r = 0.045; p = 0.022) respectively, when analysed separately. There were no other significant correlations between indices of body composition and vascular function in the group.
There was a significant negative relationship between the volume of VAT and FMR (r = -0.23; p = 0.031) for the whole group, but not when split by sex. There were no other significant correlations between the volume of VAT and the vascular outcomes.
Body composition and blood outcomes
Correlations between BMI and LDL-C (r = 0.26; p = 0.020), TG (r = 0.31; p = 0.005), glucose (r = 0.23; p = 0.040), specific insulin (r = 0.24; p = 0.039), HOMA-IS (r = -0.25; p = 0.032) and HOMA-IR (r = 0.25; p = 0.026) were apparent in the whole group. In boys, BMI was correlated with LDL-C (r = 0.35; p = 0.013). In girls, BMI was correlated with TG (r = 0.44; p = 0.014), specific insulin (r = 0.42; p = 0.018), HOMA-IS (r = -0.41; p = 0.022) and HOMA-IR (r = 0.421; p = 0.018).
TBF% correlated with specific insulin (r = 0.41; p < 0.001), beta cell function (r = 0.37; p = 0.002), HOMA-IS (r = -0.42; p < 0.001) and HOMA-IR (r = 0.41; p < 0.001) for the whole group. In boys, TBF% was correlated with LDL-C (r = 0.29; p = 0.048); specific insulin (r = 0.440; p < 0.001), beta cell function (0.42; p = 0.005), HOMA-IS (r = -0.45; p = 0.003) and HOMA-IR (r = 0.45; p = 0.003). No significant correlations were observed between TBF% and the blood outcomes in girls.
The volume of VAT was not related to any of the blood outcomes apart from a significant positive association with TG in girls only (r = 0.47, p = 0.014).
Aerobic fitness and vascular outcomes
There were no significant correlations between the expressions of aerobic fitness and any of the macro and microvascular outcomes. Likewise, when split into higher and lower groups of aerobic fitness, no significant differences were found for the majority of the vascular outcomes (Table 3). However, the group with a higher peak V̇O2 scaled for body mass did have a higher (p < 0.05) carotid to ankle PWV, although this became non-significant when peak V̇O2 was scaled for FFM.
Table 3.
Macro and micro-vascular function by higher and lower aerobic fitness groups. Mean ± standard deviation.
| Peak oxygen uptake (mL·kg-0.61.min-1) |
Peak oxygen uptake (mL·FFM-1.min-1) |
||||
|---|---|---|---|---|---|
| Lower | Higher | Lower | Higher | ||
| Macrovascular | PAI (%) | 51.1±9.5 (n=46) | 47.5±10.1 (n=47) | 49.1±10.6 (n=41) | 49.4±9.5 (n=52) |
| Carotid to ankle PWV (m·s-1) | 5.87±0.43 (n=45) | 6.08±0.47* (n=45) | 5.93±0.43 (n=40) | 6.02±0.49 (n=50) | |
| Carotid to radial PWV (m·s-1) | 6.62±0.72 (n=48) | 6.66±0.78 (n=46) | 6.58±0.63 (n=42) | 6.68±0.83 (n=52) | |
| Microvascular | FMR (V) | 1.77±0.36 (n=48) | 1.80±0.39 (n=48) | 1.76±0.35 (n=43) | 1.81±0.40 (n=53) |
| Peak ACh response (V) | 1.95±0.45 (n=48) | 1.97±0.40 (n=45) | 1.88±0.46 (n=40) | 2.02±0.38 (n=53) | |
| ACh AUC (V x time) | 478.3±141.3 (n=44) | 480.8±124.5 (n=48) | 458.4±130.5 (n=39) | 495.2±132.3 (n=53) | |
| Peak SNP response (V) | 1.64±0.49 (n=35) | 1.57±0.50 (n=28) | 1.54±0.46 (n=34) | 1.69±0.53 (n=29) | |
| SNP AUC (V x time) | 289.4±116.9 (n=35) | 274.5±111.9 (n=28) | 264.6±116.0 (n=34) | 304.1±109.9 (n=29) | |
Sample size (n=) is provided for each outcome. PAI - peripheral non-transformed augmentation index; PWV - pulse wave velocity. FMR - functional microvascular reserve; ACh - acetylcholine; AUC - area under the curve; SNP - sodium nitroprusside. Body mass index was entered as a covariate for carotid to ankle PWV. TBF% was added as a covariate for the SNP peak and AUC variables.
* p < 0.05.
Aerobic fitness and markers of CVD risk
There were no significant relationships for aerobic fitness and blood outcomes for the whole group and females. However, significant (p < 0.05) relationships were found for peak V̇O2 normalised for FFM (mL·FFM-1.min-1) and insulin markers [specific insulin (r = 0.34), β-cell function (r = 0.38), HOMA-IS (r = - 0.32) and HOMA-IR (r = 0.31)] of metabolic health in boys only. In addition, significant negative relationships were found for peak V̇O2 and TBF% for the whole group (r = 0.34; p = 0.001) and girls (r = 0.34; p = 0.044, but these disappeared when peak V̇O2 was normalised for FFM. ANOVA analyses did not reveal any mean differences between aerobic fitness groups for any of the markers of CVD risk (see Table 4), with TBF% entered as a covariate for the specific insulin, beta cell function, HOMA-IS and HOMA-IR models.
Table 4.
Cardiovascular disease risk outcomes by higher and lower aerobic fitness groups. Mean ± standard deviation.
| Peak oxygen uptake (mL·kg-0.61.min-1) |
Peak oxygen uptake (mL·FFM-1.min-1) |
|||
|---|---|---|---|---|
| Lower | Higher | Lower | Higher | |
| BMI (kg·m-2) | 17.8 ± 2.9 (n=48) | 16.8 ± 1.6 (n=48) | 17.4 ± 2.38 (n=43) | 17.1 ± 2.43 (n=53) |
| TBF% | 19.5 ± 9.6 (n=43) | 16.2 ± 6.7 (n=43) | 16.2 ± 8.7 (n=43) | 19.6 ± 7.8 (n=43) |
| VAT (cm3) | 131.1 ± 86.4 (n=42) | 109.8 ± 63.6 (n=44) | 118.0 ± 60.2 (n=38) | 121.9 ± 86.9 (n=48) |
| Total cholesterol (mmol·L-1) | 4.57 ± 0.66 (n=38) | 4.45 ± 0.73 (n=41) | 4.39 ± 0.63 (n=37) | 4.61 ± 0.74 (n=42) |
| HDL-C (mmol·L-1) | 1.86 ± 0.44 (n=38) | 1.86 ± 0.41 (n=40) | 1.79 ± 0.40 (n=37) | 1.92 ± 0.44 (n=41) |
| LDL-C (mmol·L-1) | 2.34 ± 0.59 (n=38) | 2.24 ± 0.60 (n=40) | 2.24 ± 0.55 (n=37) | 2.33 ± 0.63 (n=41) |
| TG (mmol·L-1) | 0.81 ± 0.31 (n=38) | 0.79 ± 0.28 (n=40) | 0.78 ± 0.32 (n=37) | 0.81 ± 0.28 (n=41) |
| Glucose (mmol.L-1) | 4.38 ± 0.33 (n=38) | 4.29 ± 0.42 (n=42) | 4.37 ± 0.38 (n=37) | 4.30 ± 0.39 (n=43) |
| Specific insulin (pmol·L-1) | 45.1 ± 24.3 (n=35) | 51.0 ± 25.7 (n=34) | 43.4 ± 21.9 (n=36) | 53.1 ± 27.5 (n=33) |
| β-cell function (%) | 118.1 ± 44.7 (n=35) | 130.4 ± 47.5 (n=34) | 113.2 ± 35.2 (n=36) | 136.2 ± 53.8 (n=33) |
| HOMA-IS (%) | 153.7 ± 98.9 (n=35) | 127.0 ± 71.9 (n=34) | 157.3 ± 101.3 (n=36) | 122.4 ± 65.0 (n=33) |
| HOMA-IR | 0.92 ± 0.49 (n=35) | 1.04 ± 0.51 (n=34) | 0.89 ± 0.45 (n=36) | 1.07 ± 0.55 (n=33) |
Sample size (n=) is provided for each outcome. BMI - body mass index; TBF% - total body fat percentage; VAT - visceral adipose tissue; HDL-C - high density lipoprotein cholesterol; LDL-C – low density lipoprotein cholesterol; TG -Triglyceride; HOMA – Homeostatic model assessment; IS – Insulin sensitivity; IR – Insulin resistance. TBF% was entered as a covariate for the specific insulin, β-cell function, HOMA-IS and HOMA-IR outcomes.
Discussion
The aim of the current study was to investigate whether a higher level of aerobic fitness, after appropriate adjustment for body size and composition, is related to improved macro and microvascular health and CVD risk in children. Our key finding was that higher levels of aerobic fitness, irrespective of normalisation for body mass or FFM, was not associated with improved vascular or CVD risk health outcomes in our sample of 9-10 year old children.
In contrast to our primary hypothesis, there was no consistent evidence for differences in macrovascular outcomes between the higher and lower aerobic fitness groups. However, children who had a higher aerobic fitness when allometrically scaled for body mass exhibited a higher carotid to ankle PWV compared to the lower fitness group. These observations are contrary to previous work which has shown that aerobic fitness exerts a positive effect on large artery compliance in children (Agbaje et al., 2019; Reed et al., 2005; Veijalainen et al., 2016), adolescents (Haapala et al., 2018) and young adults (Boreham et al., 2004). Interestingly, Meyer and colleagues (2017) reported a similar finding to the current paper in that brachial artery PWV was associated with higher aerobic fitness in 646 children and adolescents. They acknowledged the inverse relationship between aerobic fitness and arterial stiffness in older subjects but commented that much of the literature reporting the same association in young children is controversial since results are mediated by fat intake, stature, blood pressure and most notably body fat. Our findings that BMI and TBF% correlated with carotid to ankle PWV and (endothelial independent) SNP responses respectively, support an influence of body composition on vascular function in young subjects. Of note is that the difference in carotid to ankle PWV between the higher and lower fitness groups in the current study was no longer significant when aerobic fitness was adjusted for FFM, thus providing further evidence for an affect of body composition on macrovascular outcomes.
Previous studies have suggested that the beneficial effects of aerobic exercise may begin further down the vascular tree with greater aerobic fitness associated with improved microcirculatory function (Reed et al., 2005). However, the results of the current study do not support this suggestion since no associations were apparent between microvascular function and aerobic fitness, which is in agreement with a previous report in adolescents (Radtke et al., 2013). Thus our hypothesis that reduced aerobic fitness will be associated with a more impaired microvascular function cannot be supported, and these observations were consistent regardless of the scaling method employed to normalise peak V̇O2 for body size and composition. As associations between aerobic fitness and microvascular function have been shown in children and adolescents with type I diabetes (Roche et al., 2008), who have reduced aerobic fitness (Komatsu et al., 2005) and endothelial dysfunction, it may be that in our healthy cohort of young children the microcirculation in those with lower levels of aerobic fitness is not impaired. Alternatively, there may be other mediating factors such as maturity status, diet or levels of physical activity that could impact on vascular health and need to be taken into consideration in further studies in children.
A second hypothesis of this study was to test whether those with a higher aerobic fitness would present reduced CVD risk. We found a negative association between TBF% and peak V̇O2 normalised for body mass in the whole group and girls, which disappeared when peak V̇O2 was scaled for FFM. In addition, in boys only, we found significant associations between specific insulin, β-cell function, insulin sensitivity and peak V̇O2 scaled for FFM. However, when the whole group was split into higher and lower groups for aerobic fitness and adjustment made for TBF%, no differences in insulin health outcomes were observed. Thus, the present study found no consistent evidence for superior CVD risk factor status in children with higher aerobic fitness. Evidence supporting a direct association between aerobic fitness and CVD risk in children and adolescence within the literature is inconclusive. While some groups have reported associations between increased aerobic fitness and lower individual and clustered CVD risk (Ekelund et al., 2007; Latt et al., 2016) and increased insulin sensitivity (Lee et al., 2006; Ruiz et al., 2007), the relationships are either mediated or confounded by adiposity. Indeed, a recent meta-analysis of longitudinal studies investigating the relationship between aerobic fitness in youth and future CVD risk concluded that the relationships were unconvincing and stressed the importance of accounting for adiposity during analyses (Mintjens et al., 2018). The results of the current investigation further support the need to correctly adjust for adiposity in future work of aerobic fitness and CVD risk in youth.
A major strength of this study is thus the direct determination of aerobic fitness (peak V̇O2) and normalisation for body size and composition using scaling procedures that resulted in a size-free expression of aerobic fitness. Many prior studies have used predictions of peak V̇O2 from performance measures (e.g. 20 m shuttle test), which are crude surrogate measures of aerobic fitness and have a residual relationship with body size/fatness. Even studies that have directly assessed peak V̇O2 have expressed peak V̇O2 as a ratio standard to body mass. Ratio scaling is known to 'overscale' and this method still holds a strong negative relationship with body size (Armstrong and McManus, 2017). A further strength of this study is the direct assessment of visceral adiposity, a gold standard measure of body fat percentage and the inclusion of a number of vascular (macro and micro) measures.
Although 96 children completed the study it was challenging to acquire some of the microvascular measures in this population meaning the final data set was reduced to 69 for the peak SNP response and SNP AUC. Data for 24 children were lost to technical error, two due to a poor laser signal and one child requested to stop the test early because of discomfort. We did however make every effort to ensure the rigor of the methods used in this study and have provided laboratory specific values for measurement variability for all our vascular measures. Furthermore, we did not measure physical activity in the current study which is known to be related to vascular health outcomes in youth independent of fitness (Radtke et al., 2013). We also did not undertake a formal measurement of pubertal status (i.e. pubertal stages) and the participants were referred to as nine to 10 year old children throughout the current paper.
Conclusion
The results of the current study revealed that higher levels of aerobic fitness, whether scaled for body mass or FFM, is not related to macro and microvascular health outcomes and CVD risk factors in 9-10 year old children. We hypothesise that this lack of an association between fitness and vascular and CVD risk health outcomes is due to the low exposure to the deleterious effect of lifestyle factors on altering the vasculature in children within the first decade of life. Thus, tracking of individuals from childhood to adulthood would be necessary to identify changes in large and small vessel outcomes and CVD risk with aerobic fitness over time.
Acknowledgements
The authors would like to thank the staff and Year 5 pupils from Stoke Hill Junior School, St. Sidwell’s Primary School and St. Nicholas Primary School (Exeter, UK) for participating in the project. The authors also thank Mr David Childs and Mrs Sue Vooght at the Children’s Health and Exercise Research Centre (Exeter, UK) for their technical assistance and Professor Angela Shore, Dr Kim Gooding and Dr Jackie Whatmore at the Diabetes and Vascular Research Centre (Exeter, UK) for their technical and intellectual input in the project. The authors have no conflicts of interest and the project received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. All work and experiments undertaken for the current paper comply with UK law.
Biographies

Colin FARR
Employment
Research Assistant, Medical Research Council Epidemiology Unit, University of Cambridge, UK
Degrees
BSc, MSc, PhD
Research interests
Cardiovascular risk and prevention in childhood and adulthood
E-mail: colin.farr@mrc-epid.cam.ac.uk

Andrew R. MIDDLEBROOKE
Employment
Director of Exercise Science Consulting Limited, Woodbury, Devon, UK
Degrees
BSc, PhD
Research interests
The research and application of exercise and sports science principles to optimise human performance
E-mail:andymiddlebrooke@gmail.com
Neil ARMSTRONG
Employment
Professor of Paediatric Physiology and Founding Director of Children’s Health and Exercise Research Centre, University of Exeter, UK
Degrees
BEd, MSc, PhD, DSc, LLD(hc), ScD(hc)
Research interests
Children’s sport and exercise science and medicine
E-mail: N.Armstrong@exeter.ac.uk

Alan R. BARKER
Employment
Senior Lecturer in Paediatric Exercise and Health, University of Exeter, UK
Degrees
BSc, MSc, PhD
Research interests
Paediatric exercise medicine, paediatric exercise physiology, sport performance and training adaptations in youth
E-mail: A.R.Barker@exeter.ac.uk
Jon FULFORD
Employment
Senior Research Fellow, NIHR Exeter Clinical Research Facility, University of Exeter Medical School, Exeter, UK
Degrees
BSc, MSc, MSc, PhD
Research interests
Employment of MRI techniques to assess modifications in physiological parameters, as a result of interventions or associations with certain clinical conditions
E-mail: J.Fulford@exeter.ac.uk

David M. MAWSON
Employment
Laboratory Technical Manager, Diabetes and Vascular Medicine, NIHR Exeter Clinical Research Facility, University of Exeter Medical School, RD&E (Wonford), Barrack Road, Exeter, UK
Degrees
BSc
Research interests
Design and use of laboratory techniques to investigate endothelial and vascular function
E-mail: D.M.Mawson@exeter.ac.uk

Ali M. MCMANUS
Employment
Professor, School of Health and Exercise Sciences, University of British Columbia, Canada
Degrees
BA(Ed), MMEDSci, PhD
Research interests
Understanding the impact of exercise and prolonged sitting upon cardiopulmonary and vascular function in children
E-mail: ali.mcmanus@ubc.ca
References
- Agbaje A. O., Haapala E. A., Lintu N., Viitasalo A., Barker A. R., Takken T., Tompuri T., Lindi V., Lakka T. A. (2019) Peak oxygen uptake cut-points to identify children at increased cardiometabolic risk - The PANIC Study. Scandinavian Journal of Medicine and Science in Sports 29(1), 16-24. [DOI] [PubMed] [Google Scholar]
- Agbaje A. O., Haapala E. A., Lintu N., Viitasalo A., Vaisto J., Khan S., Veijalainen A., Tompuri T., Laitinen T., Lakka T. A. (2019) Associations of Cardiorespiratory Fitness and Adiposity With Arterial Stiffness and Arterial Dilatation Capacity in Response to a Bout of Exercise in Children. Pediatric Exercise Science 31(2), 238-247. [DOI] [PubMed] [Google Scholar]
- Aggoun Y., Szezepanski I., Bonnet D. (2005) Noninvasive assessment of arterial stiffness and risk of atherosclerotic events in children. Pediatric Research 58(2), 173-178. [DOI] [PubMed] [Google Scholar]
- Armstrong N. (2018) Commentary on the Assessment and Interpretation of Pediatric Aerobic Fitness-The Year That Was 2017. Pediatric Exercise Science 30(1), 12-18. [DOI] [PubMed] [Google Scholar]
- Armstrong N., McManus A. M. (2017) Chapter 12: Aerobic fitness. Oxford textbook of children's sport and exercise medicine. 3rd Edition Eds: Armstrong N., Van Mechelen W. Oxford, Oxford University Press; 161-180. [Google Scholar]
- Barker A. R., Gracia-Marco L., Ruiz J. R., Castillo M. J., Aparicio-Ugarriza R., Gonzalez-Gross M., Kafatos A., Androutsos O., Polito A., Molnar D., Widhalm K., Moreno L. A. (2018) Physical activity, sedentary time, TV viewing, physical fitness and cardiovascular disease risk in adolescents: The HELENA study. International Journal of Cardiology 254, 303-309. [DOI] [PubMed] [Google Scholar]
- Barker A. R., Williams C. A., Jones A. M., Armstrong N. (2011) Establishing maximal oxygen uptake in young people during a ramp cycle test to exhaustion. British Journal of Sports Medicine 45, 498-503. [DOI] [PubMed] [Google Scholar]
- Barker A. R., Williams C. A., Tolfrey K., Fawkner S. G., Sandercock G. (2013) The BASES Expert Statement on Measurement and Interpretation of Aerobic Fitness in Young People. The Sport and Exercise Scientist Autumn 2013(37), 10-11. [Google Scholar]
- Bastos da Cunha C., Sicuro F., Maranhao P. A., Borges M. A., Cyrino F. Z., Gazolla F. M., Madeira I. R., Bordallo M. A. N., Bouskela E., Kraemer-Aguiar L. G. (2017) Microcirculation, Adiposity, and Traditional and Emerging Cardiovascular Risk Factors in Prepubertal Children. Journal of the Endocrine Society 1(7), 908-917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond B., Cockcroft E. J., Williams C. A., Harris S., Gates P. E., Jackman S. R., Armstrong N., Barker A. R. (2015) Two weeks of high-intensity interval training improves novel but not traditional cardiovascular disease risk factors in adolescents. American Journal of Physiology Heart and Circulatory Physiology 309(6), H1039-1047. [DOI] [PubMed] [Google Scholar]
- Boreham C. A., Ferreira I., Twisk J. W., Gallagher A. M., Savage M. J., Murray L. J. (2004) Cardiorespiratory fitness, physical activity, and arterial stiffness: the Northern Ireland Young Hearts Project. Hypertension 44(5), 721-726. [DOI] [PubMed] [Google Scholar]
- Castro-Pinero J., Artero E. G., Espana-Romero V., Ortega F. B., Sjostrom M., Suni J., Ruiz J. R. (2010) Criterion-related validity of field-based fitness tests in youth: a systematic review. British Journal of Sports Medicine 44(13), 934-943. [DOI] [PubMed] [Google Scholar]
- Cole T. J., Bellizzi M. C., Flegal K. M., Dietz W. H. (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244), 1240-1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie K. D., Proudfoot N. A., Timmons B. W., MacDonald M. J. (2010) Noninvasive measures of vascular health are reliable in preschool-aged children. Applied Physiology, Nutrition and Metabolism 35(4), 512-517. [DOI] [PubMed] [Google Scholar]
- Ekelund U., Anderssen S. A., Froberg K., Sardinha L. B., Andersen L. B., Brage S. (2007) Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: the European youth heart study. Diabetologia 50(9), 1832-1840. [DOI] [PubMed] [Google Scholar]
- Friedewald W. T., Levy R. I., Fredrickson D. S. (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry 18(6), 499-502. [PubMed] [Google Scholar]
- Goh K. L., Shore A. C., Quinn M., Tooke J. E. (2001) Impaired Microvascular Vasodilatory Function in 3-Month-Old Infants of Low Birth Weight. Diabetes Care 24(6), 1102-1107. [DOI] [PubMed] [Google Scholar]
- Gooding K. M., Tooke J. E., Shore A. C. (1999) The Time Course of the Skin Hyperaemic Response during Local Heating. Journal of Vascular Research 36 (4), 332. [Google Scholar]
- Gopinath B., Baur L. A., Wang J. J., Hardy L. L., Teber E., Kifley A., Wong T. Y., Mitchell P. (2011) Influence of physical activity and screen time on the retinal microvasculature in young children. Arteriosclerosis, Thrombosis and Vascular Biology 31(5), 1233-1239. [DOI] [PubMed] [Google Scholar]
- Green D. J., Spence A., Halliwill J. R., Cable N. T., Thijssen D. H. (2011) Exercise and vascular adaptation in asymptomatic humans. Experimental Physiology 96(2), 57-70. [DOI] [PubMed] [Google Scholar]
- Haapala E. A., Laukkanen J. A., Takken T., Kujala U. M., Finni T. (2018) Peak oxygen uptake, ventilatory threshold, and arterial stiffness in adolescents. European Journal of Applied Physiology 118(11), 2367-2376. [DOI] [PubMed] [Google Scholar]
- Hager R. L., Tucker L. A., Seljaas G. T. (1995) Aerobic fitness, blood lipids, and body fat in children. American Journal of Public Health 85(12), 1702-1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedvall Kallerman P., Hagman E., Edstedt Bonamy A. K., Zemack H., Marcus C., Norman M., Westerstahl M. (2014) Obese children without comorbidities have impaired microvascular endothelial function. Acta Paediatrica 103(4), 411-417. [DOI] [PubMed] [Google Scholar]
- Högström G., Nordström A., Nordström P. (2014) High aerobic fitness in late adolescence is associated with a reduced risk of myocardial infarction later in life: a nationwide cohort study in men. European Heart Journal 35(44), 3133-3140. [DOI] [PubMed] [Google Scholar]
- Högström G., Nordström A., Nordström P. (2016) Aerobic fitness in late adolescence and the risk of early death: a prospective cohort study of 1.3 million Swedish men. International Journal of Epidemiology 45(4), 1159-1168. [DOI] [PubMed] [Google Scholar]
- Hopkins N. D., Stratton G., Tinken T. M., McWhannell N., Ridgers N. D., Graves L. E., George K., Cable N. T., Green D. J. (2009) Relationships between measures of fitness, physical activity, body composition and vascular function in children. Atherosclerosis 204(1), 244-249. [DOI] [PubMed] [Google Scholar]
- Isasi C. R., Deckelbaum R. J., Tracy R. P., Starc T. J., Berglund L., Shea S. (2003) Physical fitness and C-reactive protein level in children and young adults: the Columbia University BioMarkers Study. Pediatrics 111(2), 332-338. [DOI] [PubMed] [Google Scholar]
- Janz K. F., Dawson J. D., Mahoney L. T. (2002) Increases in physical fitness during childhood improve cardiovascular health during adolescence: the Muscatine Study. International Journal of Sports Medicine 23(Supplement 1), S15-21. [DOI] [PubMed] [Google Scholar]
- Juonala M., Jarvisalo M.J., Maki-Torkko N., Kahonen M., Viikari J.S., Raitakari O.T. (2005) Risk factors identified in childhood and decreased carotid artery elasticity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 112(10), 1486-1493. [DOI] [PubMed] [Google Scholar]
- Khan F., Kerr H., Ross R.A., Newton D. J., Belch J.J. (2006) Effects of poor glucose handling on arterial stiffness and left ventricular mass in normal children. International Angiology 25(3), 268-273. [PubMed] [Google Scholar]
- Komatsu W. R., Gabbay M. A., Castro M. L., Saraiva G. L., Chacra A. R., de Barros Neto T. L., Dib S. A. (2005) Aerobic exercise capacity in normal adolescents and those with type 1 diabetes mellitus. Pediatric Diabetes 6(3), 145-149. [DOI] [PubMed] [Google Scholar]
- Latt E., Maestu J., Raask T., Jurimae T., Jurimae J. (2016) Cardiovascular fitness, physical activity, and metabolic syndrome risk factors among adolescent estonian boys: A longitudinal study. American Journal of Human Biology 28(6), 782-788. [DOI] [PubMed] [Google Scholar]
- Lee S., Bacha F., Gungor N., Arslanian S. A. (2006) Cardiorespiratory fitness in youth: relationship to insulin sensitivity and beta-cell function. Obesity (Silver Spring) 14(9), 1579-1585. [DOI] [PubMed] [Google Scholar]
- Loftin M., Sothern M., Abe T., Bonis M. (2016) Expression of V̇O2peak in Children and Youth, with Special Reference to Allometric Scaling. Sports Medicine 46(10), 1451-1460. [DOI] [PubMed] [Google Scholar]
- Lohman T. (1989) Assessment of body composition in children. Pediatric Exercise Science 1, 19-30. [DOI] [PubMed] [Google Scholar]
- Mayorga-Vega D., Aguilar-Soto P., Viciana J. (2015) Criterion-Related Validity of the 20-M Shuttle Run Test for Estimating Cardiorespiratory Fitness: A Meta-Analysis. Journal of Sports Science and Medicine 14(3), 536-547. [PMC free article] [PubMed] [Google Scholar]
- Meyer J., Elmenhorst J., Giegerich T., Oberhoffer R., Muller J. (2017) Controversies in the association of cardiorespiratory fitness and arterial stiffness in children and adolescents. Hypertension Research 40(7), 675-678. [DOI] [PubMed] [Google Scholar]
- Middlebrooke A. R., Armstrong N., Welsman J. R., Shore A. C., Clark P., MacLeod K. M. (2005) Does aerobic fitness influence microvascular function in healthy adults at risk of developing Type 2 diabetes? Diabetic Medicine 22(4), 483-489. [DOI] [PubMed] [Google Scholar]
- Middlebrooke A. R., Elston L. M., Macleod K. M., Mawson D. M., Ball C. I., Shore A. C., Tooke J. E. (2006) Six months of aerobic exercise does not improve microvascular function in type 2 diabetes mellitus. Diabetologia 49(10), 2263-2271. [DOI] [PubMed] [Google Scholar]
- Mintjens S., Menting M. D., Daams J. G., van Poppel M. N. M., Roseboom T. J., Gemke R. (2018) Cardiorespiratory Fitness in Childhood and Adolescence Affects Future Cardiovascular Risk Factors: A Systematic Review of Longitudinal Studies. Sports Medicine 48(11), 2577-2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris S. J., Shore A. C., Tooke J. E. (1995) Responses of the skin microcirculation to acetylcholine and sodium nitroprusside in patients with NIDDM. Diabetologia 38(11), 1337-1344. [DOI] [PubMed] [Google Scholar]
- Nadeau K. J., Regensteiner J. G., Bauer T. A., Brown M. S., Dorosz J. L., Hull A., Zeitler P., Draznin B., Reusch J. E. (2010) Insulin resistance in adolescents with type 1 diabetes and its relationship to cardiovascular function. Journal of Clinical Endocrinology and Metabolism 95(2), 513-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen G. A., Andersen L. B. (2003) The association between high blood pressure, physical fitness, and body mass index in adolescents. Preventive Medicine 36(2), 229-234. [DOI] [PubMed] [Google Scholar]
- O'Rourke M. F., Staessen J. A., Vlachopoulos C., Duprez D., Plante G. E. (2002) Clinical applications of arterial stiffness; definitions and reference values. American Journal of Hypertension 15(5), 426-444. [DOI] [PubMed] [Google Scholar]
- OCDEM. (2004) HOMA calculator v2.2. Oxford Centre for Diabetes, Endocrinology and Metabolism, (1 screen), June. Available from URL: http://www.dtu.ox.ac.uk/homa
- Olds T. S., Dollman J. (2004) Are changes in distance-run performance of Australian children between 1985 and 1997 explained by changes in fatness. Pediatric Exercise Science 16, 201-209. [Google Scholar]
- Puissant C., Abraham P., Durand S., Humeau-Heurtier A., Faure S., Leftheriotis G., Rousseau P., Mahe G. (2013). Reproducibility of non-invasive assessment of skin endothelial function using laser Doppler flowmetry and laser speckle contrast imaging. PLoS One 8(4), e61320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radtke T., Kriemler S., Eser P., Saner H., Wilhelm M. (2013). Physical activity intensity and surrogate markers for cardiovascular health in adolescents. European Journal of Applied Physiology 113(5), 1213-1222. [DOI] [PubMed] [Google Scholar]
- Rayman G., Williams S. A., Spencer P. D., Smaje L. H., Wise P. H., Tooke J. E. (1986). Impaired microvascular hyperaemic response to minor skin trauma in type I diabetes. BMJ (Clinical Research Edition) 292(6531), 1295-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed K. E., Warburton D. E., Lewanczuk R. Z., Haykowsky M. J., Scott J. M., Whitney C. L., McGavock J. M., McKay H. A. (2005). Arterial compliance in young children: the role of aerobic fitness. European Journal of Cardiovascular Prevention and Rehabilitation 12(5), 492-497. [DOI] [PubMed] [Google Scholar]
- Roche D. M., Edmunds S., Cable T., Didi M., Stratton G. (2008). Skin microvascular reactivity in children and adolescents with type 1 diabetes in relation to levels of physical activity and aerobic fitness. Pediatric Exercise Science 20(4), 426-438. [DOI] [PubMed] [Google Scholar]
- Ruiz J. R., Rizzo N. S., Ortega F. B., Loit H. M., Veidebaum T., Sjostrom M. (2007). Markers of insulin resistance are associated with fatness and fitness in school-aged children: the European Youth Heart Study. Diabetologia 50(7), 1401-1408. [DOI] [PubMed] [Google Scholar]
- Sakuragi S., Abhayaratna K., Gravenmaker K. J., O'Reilly C., Srikusalanukul W., Budge M. M., Telford R. D., Abhayaratna W. P. (2009). Influence of adiposity and physical activity on arterial stiffness in healthy children: the lifestyle of our kids study. Hypertension 53(4), 611-616. [DOI] [PubMed] [Google Scholar]
- Sansum K. M., Weston M. E., Bond B., Cockcroft E. J., O'Connor A., Tomlinson O. W., Williams C. A., Barker A. R. (2019) Validity of the Supramaximal Test to Verify Maximal Oxygen Uptake in Children and Adolescents. Pediatric Exercise Science 31(2), 213-222. [DOI] [PubMed] [Google Scholar]
- Shore A. C., Price K. J., Sandeman D. D., Green E. M., Tripp J. H., Tooke J. E. (1991) Impaired microvascular hyperaemic response in children with diabetes mellitus. Diabetic Medicine 8(7), 619-623. [DOI] [PubMed] [Google Scholar]
- Steele R. M., Brage S., Corder K., Wareham N. J., Ekelund U. (2008) Physical activity, cardiorespiratory fitness, and the metabolic syndrome in youth. Journal of Applied Physiology 105(1), 342-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone M. R., Rowlands A. V., Middlebrooke A. R., Jawis M. N., Eston R. G. (2009) The pattern of physical activity in relation to health outcomes in boys. International Journal of Pediatric Obesity 4(4), 306-315. [DOI] [PubMed] [Google Scholar]
- Urbina E. M., Williams R. V., Alpert B. S., Collins R. T., Daniels S. R., Hayman L., Jacobson M., Mahoney L., Mietus-Snyder M., Rocchini A., Steinberger J., McCrindle B., American Heart Association Atherosclerosis, H. and Obesity in Youth Committee of the Council on Cardiovascular Disease in the, Y (2009) Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension 54(5), 919-950. [DOI] [PubMed] [Google Scholar]
- Veijalainen A., Tompuri T., Haapala E. A., Viitasalo A., Lintu N., Vaisto J., Laitinen T., Lindi V., Lakka T. A. (2016) Associations of cardiorespiratory fitness, physical activity, and adiposity with arterial stiffness in children. Scandinavian Journal of Medicine and Science in Sports 26(8), 943-950. [DOI] [PubMed] [Google Scholar]
- Welsman J., Armstrong N. (2019) Interpreting Aerobic Fitness in Youth: The Fallacy of Ratio Scaling. Pediatric Exercise Science 31(2), 184-190. [DOI] [PubMed] [Google Scholar]
- Welsman J. R., Armstrong N. (2000) Statistical techniques for interpreting body size-related exercise performance during growth. Pediatric Exercise Science 12, 112-127. [Google Scholar]
- WHO. (2018) Noncommunicable diseases. World Health Organisation online webpage, (1 screen), June. Available from URL: http://www.who.int/en/news-room/fact-sheets/detail/noncommunicable-diseases
- Wilkins J. T., McDermott M. M., Liu K., Chan C., Criqui M. H., Lloyd-Jones D. M. (2012). Associations of noninvasive measures of arterial compliance and ankle-brachial index: the Multi-Ethnic Study of Atherosclerosis (MESA). American Journal of Hypertension 25(5), 535-541. [DOI] [PMC free article] [PubMed] [Google Scholar]


