Abstract
Introduction:
Atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS) of The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) has emerged as the most controversial category because of its heterogeneity and inconsistent reporting. There is a definite paucity in data available from the Indian subcontinent about the outcome of nodules carrying Bethesda category III or Bethesda category IV diagnoses.
Aims and Objectives:
The primary objective of our study was to determine the malignancy rate in Bethesda categories III and IV nodules. The secondary objectives were to determine predictive value of BRAFV600E mutation analysis on indeterminate thyroid nodules, predictive value of Thyroid image reporting and data system (TI-RADS) in malignancy prediction and to study the common histological variants in indeterminate nodules.
Materials and Methods:
This prospective study included 176 consecutive nodules of Bethesda categories III and IV, diagnosed over a period of 2 years from August 2015 to August 2017. A part of the fine needle aspirate was used to perform the BRAFV600E mutation analysis. The malignancy risk associated with these Fine needle aspiration Cytology categories were discussed with the patients. Those with Bethesda category IV diagnosis was advised surgery, whereas those with Bethesda category III were given the options of close follow-up with repeat FNA in 3 months or immediate surgery.
Results:
In our prospective study, there were 176 consecutive samples of categories III (140/79.5%) and IV (36/20.5%). Seventy-five (53.6%) category III nodules and 29 (80.6%) category IV nodules underwent immediate surgical excision. Fifty-five consecutive indeterminate cytology nodules were subjected for BRAFV600E. One of the samples was found to be positive for BRAF T1799A (V600E) mutation. The second sample harboured a missense mutation at position 1819 (TCC--GCC), wherein the codon 607 (TCC) coding for serine was substituted by alanine (GCC) which is a variant of unknown significance. In our study, the malignancy rate of Bethesda categories III and IV, which were triaged for immediate surgery were 54.6% and 72.4%, respectively.
Conclusion:
Malignancy rate in Category III at our center was much higher than that described by ATA and by other studies published from centers around the world, including the only two studies from India. In view of the strikingly high malignancy rate in these indeterminate nodules, strong consideration to surgery should be given to patients with FNA results suggesting these two categories. BRAFV600E mutation analysis in FNA specimen has limited utility in improving the preoperative diagnostic rate for malignancy.
Keywords: Atypia of undetermined significance, fine needle aspiration cytology, follicular lesion of undetermined significance, suspicious for follicular neoplasm, the bethesda system of reporting thyroid cytopathology
INTRODUCTION
Atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS) of The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) has emerged as the most controversial category because of its heterogeneity and inconsistent reporting.[1] The estimated risk of malignancy in Bethesda category III (AUS/FLUS) and Bethesda category IV, Follicular Neoplasm/Suspicious for Follicular Neoplasm (FN/SFN) nodules was described to be 5--15% and 15--30%, respectively, as per TBSRTC 2007.[1] The 2017 revision in TBSRTC was inspired by new data and new developments in the field of thyroid pathology. Consistent with data since 2010, the revised risk of malignancy in Bethesda III, as described in TBSRTC 2017, is 10--30% and that in Bethesda IV is 25--40% (when NIFTP- noninvasive follicular thyroid neoplasm with papillary-like nuclear features is included among carcinomas).[2]
The risk of malignancy for an indeterminate nodule, especially Bethesda III, is difficult to ascertain because only a minority of cases in this category undergo surgery.[1] Those that are resected represent a selected population of patients with repeatedly AUS/FLUS results or patients with worrisome clinical/sonographic findings.[1] The purpose of Bethesda category IV is to identify a nodule that might be a follicular carcinoma and triage it for excision. The term “suspicious for a follicular neoplasm” is preferred by some laboratories over “follicular neoplasm” for this category because a significant proportion (upto 35%) proves not to be neoplasm but a rather hyperplastic proliferation of follicular cells, most commonly those of multinodular goiter.
There is a definite paucity in data available from the Indian subcontinent about the outcome of nodules carrying Bethesda category III or Bethesda category IV diagnoses.
The primary objective of our study was to determine the malignancy rate in Bethesda categories III and IV nodules. The secondary objectives were to determine as follows:
Predictive value of BRAFV600E mutation analysis on indeterminate thyroid nodules
Predictive value of TIRADS in malignancy prediction
The common histological variants in indeterminate nodules.
MATERIALS AND METHODS
This was a prospective study from August 2015 to August 2017 at a tertiary center with the patient referral from all parts of the state of Kerala, India. The study was approved by the institutional review board and included 176 consecutive nodules of Bethesda categories III and IV, diagnosed during this period. A detailed clinical history, biochemical, and radiological investigations were recorded for each case. Subjects aged 15 years and more and those with Bethesda categories III and IV nodules were included in the study after signing an informed consent. Subjects with known thyroid cancer were excluded.
FNAC was performed using 24 gauge or 25 gauge French needle with 1--2 aspirates depending on the size of the swelling. A part of the fine needle aspirate was stored in microcentrifuge tubes at −20°C at the Department of Molecular Biology to perform the BRAFV6003 mutation analysis. DNA was extracted from the FNA samples using the QIAamp DNA extraction kit according to the manufacturer's protocol (Qiagen, Germany). For BRAFV600E mutation analysis, a 223 bp region flanking the T1799A mutation of the BRAF gene was PCR amplified using the primers B-Raf15F (5′TCATAATGCTTGCTCTGATAGGA- 3′) and B-Raf15R (5′-GGCCAAAAATTTAATCAGTGGA- 3′) in a 50 μl PCR reaction solution using 100 ng of the genomic DNA isolated from the tumor tissues as template and EmeraldAmp GT PCR Master Mix (Takara Bio Inc., Japan).
The malignancy risk associated with the FNA categories were discussed with the patients. Those with Bethesda category IV diagnosis was advised surgery, whereas those with Bethesda category III were given the options of close follow-up with repeat FNA in 3 months or immediate surgery.
Statistical analysis
Statistical analysis was done using SPSS software. For descriptive statistics, categorical variables were expressed as numbers and percentages. Continuous variables were summarized using mean and standard deviation in case of normal distribution of data. Percentage malignancy rate in categories III and IV thyroid nodules was computed. Percentage prevalence rate of BRAF mutation in indeterminate nodules was computed. To test the statistical significance of malignancy rate in Category III and IV nodules, Chi-square test was applied. A P value < 0.05 was considered statistically significant.
RESULTS
A total of 176 patients were followed up during the specified time period. Out of this sample size, 140 patients belonged to Bethesda Category III and 36 patients belonged to Bethesda Category IV. The mean age of presentation was 47 ± 14 years with a female preponderance [139/176 patients (79%)]. The mean nodule size was 21 ± 10 mm. Patients (104) underwent surgery and out of them 62 turned out to be malignant and 42 were benign. The malignancy rate in Bethesda category III was 54.7% and in Bethesda category IV was 72.4% with a P value of 0.098.
55 consecutive FNA samples were subjected to BRAF mutation analysis and one of the samples was found to be positive for BRAF T1799A (V600E) mutation. The second sample harboured a missense mutation at position 1819 (TCC--GCC), wherein the codon 607 (TCC) coding for serine was substituted by alanine (GCC) which is a variant of unknown significance.
The follow-up and outcome of the 176 Bethesda categories III and IV is mentioned in the Figure 1. 10% and 25% ofcategory III nodules were classified as TIRADS 4 and TIRADS categories less than 4, respectively. 11% and 22% category IV nodules were classified as TIRADS 4 and TIRADS categories less than 4, respectively. The malignancy rate of TIRADS 2,3,4 nodules was as per given in Table 1.
Figure 1.
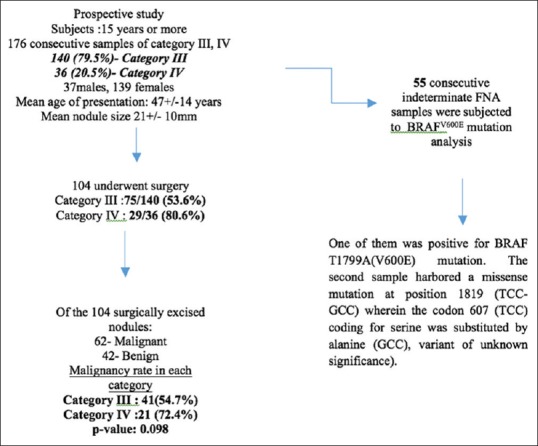
Flowchart of the study group
Table 1.
Malignancy rates based on TIRADS[15] classification
| TIRADS | Benign n | Malignant n |
|---|---|---|
| TIRADS 2 | 7 | 6 |
| TIRADS 3 | 28 | 44 |
| TIRADS 4 | 5 | 7 |
Malignancy in TIRADS 4 or more (58.8%) vs. <4 (58.3%), P=0.97
The most common malignant tumor type in either category was the follicular variant of PTC (FVPTC). The distribution of different tumor types in categories III and IV were as given in Table 2.
Table 2.
Different tumor types
| Malignant tumor type | n (%) Categories III & IV | n (%) Category III | n (%) Category IV |
|---|---|---|---|
| Classical Papillary thyroid carcinoma (PTC) | 16 (25.8%) | 14 (34.1%) | 2 (9.5%) |
| Follicular variant of PTC | 26 (42%) | 18 (44%) | 8 (38%) |
| Micropapillary carcinoma | 8 (12.9%) | 5 (12.2%) | 3 (14.3%) |
| Follicular carcinoma | 7 (11.3%) | 1 (2.4%) | 6 (28.6%) |
| Variants of PTC | 4 (6.4%) | Tall cell- 2 (4.9%) Solid variant- 1 (2.4%) | Poorly differentiated areas-1 (4.8%) |
| Anaplastic carcinoma | 1 (1.6%) | - | - |
Out of the 18 Bethesda category III nodules carrying the diagnosis of FVPTC, six were invasive FVPTC. Eight category IV nodules carried the diagnosis of FVPTC, out of which three were invasive.
Out of 140 category III nodules, 53.6%, 13.6%, 32.8% had cytological, focal architectural atypia and both, respectively. The malignancy rate in nodules with atypia was as given in Table 3.
Table 3.
Correlation of atypia with malignant and benign nodules
| Atypia | Benign n (%) | Malignant n (%) | Total | P value |
|---|---|---|---|---|
| No | 8 (27.6) | 21 (72.4) | 29 | |
| Yes | 34 (45.4) | 41 (54.6) | 75 | 0.098 |
DISCUSSION
The original TBSRTC recommended that an effort is made to limit the use of Bethesda category III to approximately 7% or fewer of all thyroid FNAs. In view of the practical difficulty faced by many laboratories, the 2017 TBSRTC has recommended 10% as a more realistic limit.[2] The 2017 TBSRTC has revised the risk of malignancy in AUS/FLUS and FN/SFN nodules to range from 10-30% and 25-40% respectively.[1] The usually recommended management as per 2007 TBSRTC was repeating FNA in 3 months in case of AUS/FLUS nodules. However, the 2017 TBSRTC recommends including molecular testing as part of the usual management.[2]
The malignancy rate of nodules carrying a diagnosis of Bethesda category III who underwent immediate surgery, as per Western studies, ranged from 20%, 25% to 28%.[3,4,5] Allen S Ho et al demonstrated a malignancy rate of 26.3% in nodules 8 with two consecutive AUS/FLUS diagnoses that underwent surgical resection.[6] Among the AUS/FLUS nodules triaged for immediate surgery, the malignancy rate was observed to be 37.8%. As per the only 2 available Indian studies, the malignancy rate in AUS/FLUS was as follows: in the study by Chandra S et al,[7] 49.2% of patients with an initial diagnosis of Bethesda category III underwent immediate surgery. In this group, the overall malignancy rate reported was 29%. In the study by Chakravarthy NS et al, out of 290 FNA specimens, 35(12%) were AUS. 44% of the 290 thyroid nodules underwent surgical excision and the malignancy rate in the 35 AUS nodules was found to be 69%.[8] S Doodi et al. demonstrated a malignancy rate of 81% in Bethesda Category IV nodules.[5] In his study, Bethesda category IV nodules constituted 1.7% of the total 621 nodules. In our study, the malignancy rate of Bethesda categories III and IV which were triaged for immediate surgery were 54.6%, and 72.4% respectively.
In a study by Park et al, the overall malignancy rate in Bethesda category III was 23.3%. The AUS-Nuclear atypia subcategory was associated with the highest risk of malignancy and the greatest frequency of BRAFV600E. They suggested that subcategorization of Bethesda category III by cytomorphology and BRAFV600E mutation status is important for predicting the risk of malignancy.[9] Tiffany et al. demonstrated a similar finding in their study. They demonstrated that malignancy rate for nodules that featured nuclear atypia was significantly higher at 36.8% than the rate for nodules that had only architectural atypia at 14.7%.[10] In our study cohort, subcategorization of Bethesda category III nodules into cytological and architectural atypia was of limited value in malignancy prediction.
The BRAFV600E mutation, which occurs in approximately 36-69% of Papillary thyroid cancer (PTC), is the most common mutation observed in PTC patients.[11] A prevalence of 51% and 49% of BRAFV600E in PTC has been documented in Indian and Korean cohorts respectively.[12,13] In a study conducted at our same institution, Nair CG et al. analyzed tissues which were histopathologically categorized as classical PTC and infiltrating FVPTC for the presence of BRAFV600E mutation.[12] These nodules carried FNA diagnoses of Bethesda categories V and VI. Of the 59 patients included in the study, 51% harbored BRAFV600E mutation, but the mutation status was not associated with aggressive tumor factors and adverse outcome.[12] Avik Chakraborty et al. studied the prevalence of BRAFV600E mutation in thyroid cancer among the Indian population.[14] The mutation analysis was done on tissue specimens categorized histopathologically as PTC. BRAF mutation at codon 600 was detected in 46 of 86 PTC patients (53.4%). They found a significant correlation between BRAF mutation status and extra-thyroidal invasion, lymph node metastasis, and tumor stage. Xing et al.[13] demonstrated that 49% of the tissue specimens histopathologically categorized as PTC were positive for BRAFV600E mutation. In our study, out of the 55 FNA samples analyzed for the presence of BRAFV600E mutation using Sanger sequencing, 4.one of the samples was found to be positive for BRAF T1799A (V600E) mutation. Another sample harbored a missense mutation at position 1819 (TCC- GCC) wherein the codon 607 (TCC) coding for serine was substituted by alanine (GCC). The clinical significance of this mutation, T1819G, has to be determined. Both the cases were confirmed to harbor classical papillary thyroid cancer on histopathology and were Bethesda category III.
Chandra S et al. observed that FVPTC was the most common malignancy diagnosed on histopathology in category III subjected to surgery.[7] In the study by Allen S Ho et al., the vast majority of malignant surgical specimens comprised papillary thyroid carcinoma, either classical or other subtypes (86.8%). Follicular variant of papillary thyroid carcinoma comprised 48.8% of the papillary thyroid cancers.[6]
TIRADS scores were of limited value in predicting malignancy in our cohort of patients but this could be explained by the relatively smaller sample size.
CONCLUSION
Malignancy rate in Category III at our center was much higher than that described by ATA and by other studies published from centers around the world including the only two studies from India. The rate at our center was 54.6%, which was strikingly higher than that from the above-mentioned studies which showed a rate of 20-28%. Malignancy rate in Category IV at our center was also much higher than described in the literature. In view of the strikingly high malignancy rate in these indeterminate nodules, strong consideration to surgery should be given to patients with FNA results suggesting these two categories. TIRADS scores were of limited value in predicting malignancy in our cohort of patients but this may be down to the small sample size. A BRAFV600E mutation analysis in FNA specimen has limited utility in improving the preoperative diagnostic rate for malignancy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cibas E, Ali S. The Bethesda System for Reporting Thyroid Cytopathology. Thyroid. 2009;19:1159–65. doi: 10.1089/thy.2009.0274. [DOI] [PubMed] [Google Scholar]
- 2.Cibas E, Ali S. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Journal of the American Society of Cytopathology. 2017;6:217–22. doi: 10.1016/j.jasc.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Layfield LJ, Morton MJ, Cramer HM, Hirschowitz S. Implications of the proposed thyroid fine needle aspiration category of “follicular lesion of undetermined significance”: A five-year multi-institutional analysis. Diagn Cytopathol. 2009;37:710–4. doi: 10.1002/dc.21093. [DOI] [PubMed] [Google Scholar]
- 4.Broome JT, Solorzano CC. The impact of atypia/follicular lesion of undetermined significance on the rate of malignancy in thyroid fine-needle aspiration: Evaluation of the bethesda system for reporting thyroid cytopathology. Surgery. 2011;150:1234–41. doi: 10.1016/j.surg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Doddi S, Chohda E, Maghsoudi S, Sheehan L, Sinha A, Chandak P, et al. The final outcome of indeterminate cytology of thyroid nodules in a District General Hospital. G Chir. 2015;36:122–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Ho A, Sarti E, Jain K, Wang H, Nixon I, Shaha A, et al. Malignancy rate in thyroid nodules classified as bethesda category III (AUS/FLUS) Thyroid. 2014;24:832–9. doi: 10.1089/thy.2013.0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandra S, Chandra H, Bisht S. Malignancy rate in thyroid nodules categorized as atypia of undetermined significance or follicular lesion of undetermined significance - An institutional experience. J Cytol. 2017;34:144–8. doi: 10.4103/JOC.JOC_234_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chakravarthy NS, Chandramohan A, Prabhu AJ, Gowri M, Mannam P, Shyamkumar NK, et al. Ultrasound-guided fine-needle aspiration cytology along with clinical and radiological features in predicting thyroid malignancy in nodules ≥1 cm. Indian J Endocr Metab. 2018;22:597–604. doi: 10.4103/ijem.IJEM_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park H, Moon J, Yom C, Kim K, Choi J, Choi S, et al. Thyroid “Atypia of undetermined significance” with nuclear atypia has high rates of malignancy and BRAF mutation. Cancer Cytopathol. 2014;122:512–20. doi: 10.1002/cncy.21411. [DOI] [PubMed] [Google Scholar]
- 10.Gan T, Nga M, Lum J, Wong W, Tan W, Parameswaran R, et al. Thyroid cytology-nuclear versus architectural atypia within the “Atypia of undetermined significance/follicular lesion of undetermined significance” Bethesda category have significantly different rates of malignancy. Cancer Cytopathol. 2017;125:245–56. doi: 10.1002/cncy.21823. [DOI] [PubMed] [Google Scholar]
- 11.Haugen B, Alexander E, Bible K, Doherty G, Mandel S, Nikiforov Y, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nair C, Babu M, Biswas L, Jacob P, Menon R, Revathy A, et al. Lack of association of B-type raf kinase V600E mutation with high-risk tumor features and adverse outcome in conventional and follicular variants of papillary thyroid carcinoma. Indian J Endocrinol Metab. 2017;21:329–33. doi: 10.4103/ijem.IJEM_353_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xing M, Westra WH, Tufano RP, Cohen Y, Rosenbaum E, Rhoden KJ, et al. BRAF mutation predicts a poorer clinical prognosis for papillary thyroid cancer. J Clin Endocrinol Metab. 2005;90:6373–9. doi: 10.1210/jc.2005-0987. [DOI] [PubMed] [Google Scholar]
- 14.Chakraborty A, Narkar A, Mukhopadhyaya R, Kane S, D’Cruz A, Rajan M. BRAF V600E Mutation in papillary thyroid carcinoma: Significant association with node metastases and extra thyroidal invasion. Endocr Pathol. 2011;23:83–93. doi: 10.1007/s12022-011-9184-5. [DOI] [PubMed] [Google Scholar]
- 15.Horvath E, Majlis S, Rossi R, Franco C, Niedmann J, Castro A, et al. An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J Clin Endocrinol Metab. 2009;94:1748–51. doi: 10.1210/jc.2008-1724. [DOI] [PubMed] [Google Scholar]


