Chang and Chaudhuri discuss basement membrane mechanics and how cells use both proteolytic and physical mechanisms to invade basement membranes during cancer progression.
Abstract
In epithelial cancers, cells must invade through basement membranes (BMs) to metastasize. The BM, a thin layer of extracellular matrix underlying epithelial and endothelial tissues, is primarily composed of laminin and collagen IV and serves as a structural barrier to cancer cell invasion, intravasation, and extravasation. BM invasion has been thought to require protease degradation since cells, which are typically on the order of 10 µm in size, are too large to squeeze through the nanometer-scale pores of the BM. However, recent studies point toward a more complex picture, with physical forces generated by cancer cells facilitating protease-independent BM invasion. Moreover, collective cell interactions, proliferation, cancer-associated fibroblasts, myoepithelial cells, and immune cells are all implicated in regulating BM invasion through physical forces. A comprehensive understanding of BM structure and mechanics and diverse modes of BM invasion may yield new strategies for blocking cancer progression and metastasis.
Introduction
The basement membrane (BM) is a thin, dense sheet of ECM that plays an important role in normal tissue development and function (Yurchenco, 2011). It separates epithelia, endothelia, fat, nerve, and cardiac cells from their underlying connective tissues. The origins of the BM trace back to the advent of multicellularity, and BM proteins are widely conserved across multicellular organisms (Fidler et al., 2017). Its two most abundant components are laminin, which provides cell signaling cues, and collagen IV, which is thought to function as the main structural backbone of the BM. Other components include nidogens, proteoglycans, and growth factors. Rich in biochemical and mechanical cues, the BM is crucial for cell signaling, structural integrity, and barrier protection against cells and very large molecules.
Abnormalities in the chemical and mechanical properties of the BM are implicated in diseases, particularly cancer. Aberrations in BM components during development result in diseases that are usually lethal before or shortly after birth (Wiradjaja et al., 2010). Mutations in laminin are involved in diseases associated with skin, muscle, and nerve (McGowan and Marinkovich, 2000). The BM plays a key role in epithelial cancers, or carcinomas. Epithelial BM serves as a physical barrier to carcinoma cell invasion into the surrounding stromal tissue, while endothelial BM hinders carcinoma cell invasion into (intravasation) and out of (extravasation) blood and lymphatic vessels during metastasis, which accounts for 90% of cancer-related deaths (Lambert et al., 2017; Fig. 1 A). In breast cancer, if carcinoma cells remain localized, the cancer is highly treatable, with a 99% 5-yr survival rate (Siegel et al., 2019). However, once cells have invaded through BMs into the surrounding region, the 5-yr survival rate decreases to 85%; the 5-yr survival rate for patients with distant, metastatic breast cancer drops further to 27% (Siegel et al., 2019). In some cases, carcinomas grow to centimeters in diameter without breaching the BM, while in other cases, BM invasion occurs when carcinoma growths are at the microscale. BM integrity is a key prognostic marker for breast (Gusterson et al., 1982), colorectal (Mylonas and Lazaris, 2014), oral (Wilson et al., 1999), prostate (Liu et al., 2009), and skin (Schmoeckel et al., 1989) cancer. Understanding strategies cells use to overcome the BM barrier may reveal new strategies to halt metastasis.
Figure 1.
BM composition, mechanics, and associated cell interactions. (A) During metastasis, tumor cells breach through the BM during primary tumor escape, intravasation, and extravasation. Inset corresponds to events described in B. (B) Cell integrin receptors bind to a laminin network, which binds to a collagen IV network via nidogen. Proteoglycans are also found within the BM, and collagen I is primarily found in the stromal matrix.
While the established view has been that BM invasion occurs primarily through chemical degradation of the BM with proteases, specifically matrix metalloproteinases (MMPs), emerging studies reveal that physical mechanisms of invasion may also contribute. Proteases were thought to be essential since the BM is a nanoporous barrier to the invasion of ∼10-µm-sized cells. However, a number of clinical trials using broad-spectrum or more specific MMP inhibitors failed to diminish mortality in clinical trials (Coussens et al., 2002; Fingleton, 2008). While there are a number of explanations for this failure, including severe side effects, subtherapeutic doses, inhibitor specificity, and the advanced stage of cancer of the patients that were treated, these results indicate the possibility that nonproteolytic mechanisms may play crucial roles during metastasis. Indeed, early in vitro studies indicated that nonproteolytic migration modes are adopted by tumor cells when proteases are inhibited (Friedl and Wolf, 2003; Sahai and Marshall, 2003). More recent work revealed that cells can invade through BMs independently of proteases in vivo and in vitro, challenging the established paradigm that proteases are always required for cancer invasion. Moreover, neighboring carcinoma and stromal cells in the tumor microenvironment can similarly exert forces to weaken the BM or promote invasion. In this review, we explore BM composition and mechanics and highlight (a) prior understanding of chemical modes as well as recent findings of physical modes of BM invasion during cancer, (b) the potential role of proliferation and collective migration on BM integrity, and (c) how neighboring stromal cells can facilitate BM invasion.
BM composition and mechanics
BM assembly and composition
The BM comprises laminins, type IV collagen, nidogens, and various proteoglycans. The BM attaches to the basal surface of epithelial and endothelial cells and surrounds muscle, fat, and Schwann cells (Hohenester and Yurchenco, 2013). In healthy tissue, the BM can be detected through histological staining of collagen IV (Wu et al., 2016) and laminin (Diaz et al., 2005). Cancerous tissues are often distinguished by the absence of both collagen IV and laminin (Diaz et al., 2005; Wu et al., 2016). While laminin directly binds to epithelial cells via integrin receptors, collagen IV interfaces the laminin network and surrounding connective tissue; nidogen cross-links the laminin and collagen IV networks, and proteoglycans are found throughout the BM (Fig. 1 B). Laminin, the most abundant component of the BM, is a biologically active glycoprotein heterotrimer formed by one α, one β, and one γ chain (Martin and Timpl, 1987); there have been five α, four β, and three γ subunits and at least 16 laminin isoforms identified (Yurchenco, 2011). Weak ternary binding interactions between the short arms of the α, β, and γ subunits in three adjacent laminins, along with homologous interactions between α and α or β and β subunits in adjacent laminins, generally drive laminin network formation, although variation exists among isoforms (Yurchenco and Cheng, 1993; Cheng et al., 1997; Odenthal et al., 2004). Each laminin isoform is cell and tissue specific, modulating cell adhesion, migration, and differentiation by binding to the integrin receptors on the cells (Patarroyo et al., 2002). α7β1, α6β4, α6β1, and α3β1 integrins bind exclusively to laminin (Humphries et al., 2006). Non-integrin laminin receptors include 37/67 laminin receptor, dystroglycan, and syndecan (Carulli et al., 2012; Cloutier et al., 2019). Laminin-111 is widely found in many tissues, including the parenchymal, renal proximal tubule, adrenal, salivary, and mammary gland BM. Laminin-332 is found in the epithelial and amnion BM (Simon and Bromberg, 2017). Laminin-511 has been implicated in cell migration, tumor growth, and metastasis, with higher levels of this isoform found in many breast, lung, thyroid, and prostate cancers (Chia et al., 2007; Pouliot and Kusuma, 2013).
The unique structural interactions found within the collagen IV network create a strong structural, but potentially malleable, framework of the BM. While collagen IV is typically arranged on the outer layer of the BM and does not directly interact with epithelial cells, cells can bind to collagen IV via integrins α1β1 and α2β1, which may be relevant as the BM breaks down (Kern et al., 1993; Khoshnoodi et al., 2008). The collagen IV network is observed to be arranged in a 3D, irregular polygonal architecture with pore sizes averaging ∼50 nm in amnion BM and ∼100 nm in reconstituted BM (rBM; Yurchenco and Ruben, 1987). However, it has been suggested that the collagen IV layer exhibits a more compact 3D configuration in its native state, in which pore size can increase when stretch is applied (Halfter et al., 2015). The maximum distance between two cross-linking sites is estimated to be 800 nm, the sum of two ∼400-nm collagen monomers (Timpl et al., 1981). Unlike fibrillar collagens, collagen IV is not proteolytically processed when secreted, so each collagen IV component is arranged head to head, rather than in parallel (Paulsson, 1992). These ends associate at the carboxy terminus, or the NC1 domain, through sulfilimine covalent bonds, as well as weaker hydrophobic and hydrophilic interactions (Timpl et al., 1981; Sundaramoorthy et al., 2002; Than et al., 2002; Vanacore et al., 2009). Further, disulfide bonds, lysine cross-links, and hydrophobic bonds link the amino terminus, or 7S domain, of four collagen IV molecules together into a tetramer (Timpl et al., 1981; Yurchenco and Furthmayr, 1984; Siebold et al., 1987; Khoshnoodi et al., 2008). Finally, weak noncovalent interactions link collagen IV molecules together laterally (Yurchenco and Furthmayr, 1984; Yurchenco and Ruben, 1987). The precise architectures and cross-linking interactions within the collagen IV networks in different BMs remain unclear.
Other important molecules in the BM include nidogen and proteoglycans. Nidogens-1 and -2, also known as entactins, are glycoproteins that noncovalently link the laminin and collagen IV networks, providing stabilization against mechanical stresses (Yurchenco, 2011). The three most well-characterized proteoglycans in the BM, collagen XVIII, perlecan, and agrin, play diverse biological roles, ranging from regulating growth factor activity to promoting angiogenesis (Iozzo, 2005). The BM also serves as a reservoir for growth factors, such as VEGF and PDGF, which tether to proteoglycans until release (Iozzo et al., 2009).
BM assembly is a multistep process regulated by laminin and collagen IV self-polymerization, intercomponent interactions, and cell-binding associations. BM assembly begins with the production and binding of laminin to cell surface receptors, such as β1 integrin or dystroglycan, to produce a high local concentration of laminins (Hohenester and Yurchenco, 2013; Glentis et al., 2014). Once in close proximity, laminins self-assemble with one another via α, β, and γ arms (McKee et al., 2007). During the second stage, collagen IV, nidogen, perlecan, and agrin are recruited onto the laminin scaffold, with collagen IV forming a network and nidogen linking the laminin and collagen IV networks. While the absence of collagen IV does not inhibit BM assembly during development, it prevents the formation of a structurally stable BM (Pöschl et al., 2004).
BM structure and mechanics
BM components are tightly arranged into a thin, nanoporous layer. The nanometer-sized pores of the BM restrict cell movement and diffusion of very large molecules, while permitting diffusion of smaller molecules. BM pore size is tissue specific, with the average pore size in corneal epithelial BM measured to be 32–112 nm (Abrams et al., 2000) and mammary epithelial BM measured to be ∼10 nm (Yurchenco and Ruben, 1987; Gaiko-Shcherbak et al., 2015). Using electron microscopy, BM thickness has been found to range from tens of nanometers to the order of microns, depending on the tissue (Kefalides and Borel, 2005; Halfter et al., 2013). Measurements of BM thickness using electron microscopy may underestimate the actual thickness, as this technique requires samples to be dehydrated; measurements using atomic force microscopy (AFM) estimate that BM thickness is twofold higher than the thickness reported from electron microscopy (Halfter et al., 2015). Even within the same tissue, BM thickness is not uniform. For example, at the milk-producing terminal end bud of the mammary gland, the BM of the bulbous tip is ∼100 nm thick, while the thickness at the ducts reaches 1.4 µm (Paine and Lewis, 2017).
Due to the challenges of isolating and handling the BM, there is limited knowledge of the mechanical properties of native, human BM. We review material mechanics and evidence of material descriptors that describe the BM in Box 2. It is assumed that although thin, the BM serves as structural support and barrier to cell invasion. Measurements of BM stiffness have been made on various tissues and using various mechanical testing techniques. The Young’s modulus, a material property related to stiffness, of BM derived from adult chick retina was measured to be as high as 4.07 MPa (Candiello et al., 2007), while the moduli of corneal BM ranged from 20 to 80 kPa (Last et al., 2009). Stiffness of BM from mouse mesentery was found to be ∼55 kPa (Glentis et al., 2017). Using a microcantilever tensional assay, BM stiffness ranged from 400 to 3,000 kPa in mice renal tubules (Bhave et al., 2017) and was ∼1,400 kPa in Drosophila melanogaster Malpighian tubules (Howard et al., 2019). AFM measurements found that the stiffness of BM that envelopes Drosophila eggs ranged up to 70 kPa (Crest et al., 2017) and up to 800 kPa (Chlasta et al., 2017). More recently, mechanical properties of BM isolated from human mammary epithelial acini grown in vitro were characterized, and the modulus was reported to be on the order of hundreds of pascals to several kilopascals (Fabris et al., 2018). In comparison, the Young’s moduli of epithelial cells range from 0.5 to 2.5 kPa and is largely governed by the actin cytoskeleton (Xu et al., 2012; Brückner and Janshoff, 2015). The moduli of soft tissues range from hundreds of pascals to tens of kilopascals, which is typically governed by a fibrillar collagen I network (Levental et al., 2007; Swift et al., 2013). The large variability in BM stiffness measurements likely depends on the type and composition of BM as well as the measurement technique. For example, AFM studies typically probe materials at high frequencies or over short time periods, and the measured elastic modulus of viscoelastic materials would be expected to increase with frequency. Stiffness measurements of human BM in vivo, especially those in the context of cancer invasion, are lacking, representing an important challenge for the field.
BM mechanics are particularly important to consider because of cell mechanotransduction, or the process by which cells sense and respond to mechanical cues. It is known that ECM stiffness impacts cell processes including cell spreading (Pelham and Wang, 1997), differentiation (Engler et al., 2006), malignancy (Paszek et al., 2005), migration (Lo et al., 2000), and proliferation (Kong et al., 2005). Known mechanisms of mechanotransduction involve actomyosin contractility (Paszek et al., 2005), integrin clustering (Kong et al., 2005; Paszek et al., 2005), nuclear deformation (Swift et al., 2013), talin unfolding (Goult et al., 2018), volume expansion (Lee et al., 2019a), and Yes-associated protein (YAP) activation (Dupont et al., 2011). However, most mechanotransduction studies are performed on collagen I, fibronectin, or RGD-presenting substrates and do not typically use substrates that present BM ligands. Thus, BM ligand–mediated mechanotransduction could involve distinct mechanisms. Indeed, increased stiffness in BM-like matrices induces a malignant phenotype in models of normal mammary epithelium 3D cultured within the matrices by inhibiting α6β4 integrin clustering into hemidesmosomes (Chaudhuri et al., 2014), independently of YAP activation (Lee et al., 2019b). Due to the thinness of the BM underlying epithelial tissues, a key question is whether cells can sense the stiffness of only the immediate BM or if they can also sense the stiffness of the stromal matrix beyond the BM. Studies show that cells can sense stiffness on the micron scale, so the effective stiffness sensed by cells in direct contact with the BM could be impacted by the mechanical properties of the surrounding stromal matrix (Sen et al., 2009; Buxboim et al., 2010; Lin et al., 2010; Mohammadi and McCulloch, 2014). This is supported by in vitro experiments in which mammary epithelial acini immediately surrounded by endogenous BM invade following increased stiffness of the matrix outside of the BM (Stowers et al., 2017). Thus, the stiffening of stromal tissue from ∼100 Pa to several kilopascals that occurs during breast cancer progression (Acerbi et al., 2015) is likely sensed by epithelial cells shielded from the stromal matrix by the BM. However, the degree to which changes in stromal matrix mechanics alters the effective stiffness of the BM sensed by cells remains unclear.
Chemical and physical modes of BM invasion
Protease-dependent BM degradation
Proteases, enzymes that can selectively degrade peptide bonds between amino acids, are used by cells to chemically degrade ECMs including BM. Early studies found that cancer cells can degrade collagen IV and that increased degradation correlated with greater metastatic potential (Liotta et al., 1980). Histological evidence shows that loss of BM can be detected at the site of transition from a benign ductal carcinoma in situ to an invasive ductal carcinoma (Carraro et al., 2014). Tumor cell migration through collagen I–rich stromal matrix with dense covalent cross-links requires the production of MMPs (Sabeh et al., 2004). BM degradation not only weakens its barrier function, but also enhances cell migration through signals induced by the cleaved product (Gilles et al., 2001; Udayakumar et al., 2003; Koshikawa et al., 2004). See Box 1 for a discussion of in vitro models of BM invasion.
Box 1. In vitro models of BM invasion
rBM
In vitro models of cancer invasion using rBM are powerful tools to elucidate the dynamics of BM invasion. Commercially available as Matrigel or Cultrex, rBM derived from the Engelbreth-Holm-Swarm (EHS) sarcoma is widely used to study BM invasion (Kleinman et al., 1982). The utility of EHS-derived rBM in culture was demonstrated by the Bissell group, who showed that healthy and cancerous mammary epithelial cells exhibited distinguishable phenotypes when cultured in rBM, but not on normal tissue culture plastic (Petersen et al., 1992). rBM, which gels at 37°C, contains on the order of 60% laminin, 30% collagen IV, 8% entactin, and 2% proteoglycans and/or growth factors, although the exact proportion can vary substantially between batches (Corning Incorporated, 2013). The average pore size of rBM matrix has been estimated to be 20–60 nm for rBM concentrations ranging from ∼4 mg/ml to 17 mg/ml (Chaudhuri et al., 2014). While the major components of rBM can be found in native BM, the only laminin isoform found in rBM is laminin-111 (Patarroyo et al., 2002). Furthermore, covalent cross-links found in native BM are not found in rBM, although methods to introduce covalent cross-links into rBM exist (Wisdom et al., 2019). For a thorough overview of in vivo BM invasion models, the reader is referred to an excellent recent review (Kelley et al., 2014).
rBM has been used in different approaches to study BM invasion in vitro. One method involves seeding cells onto rBM-coated Transwell inserts and counting the number of cells that migrate through the rBM and transwell pores (Kargozaran et al., 2007; Xie et al., 2009). Increased cell counts correspond to enhanced invasion capabilities. Addition of chemoattractant to the culture medium stimulates downward migration through the Transwell membrane. Alternatively, cells can be seeded on a layer of rBM with rBM-supplemented medium as 2.5D culture to capture horizontal cell movements, or embedded within rBM as 3D culture to capture multidirectional cell movements (Weaver et al., 1997; Leung and Brugge, 2012). However, one limitation is that the stiffness of pure, gelled EHS extract ranges from 100 Pa to 1 kPa, depending on density (Soofi et al., 2009; Chaudhuri et al., 2014), which may be low compared with native BMs. rBM stiffness can be tuned by incorporating a second material, such as collagen I (Paszek et al., 2005), polyethylene glycol (Beck et al., 2013), or alginate (Chaudhuri et al., 2014).
Native or cell-secreted BM
In addition to rBM-derived systems, native or cell-secreted BMs are used to model BM invasion in vitro. BM can be recovered from human peritoneum, stripped of overlying cells, mounted onto a holder, and seeded with cells (Hotary et al., 2006; Glentis et al., 2017). Alternatively, cells can also deposit BM in vitro. Endothelial cells that form microvessels deposit their own BM (Chen et al., 2016). Alveolar epithelial cells cultured on dense fibrillar collagen supplemented with rBM can secrete their own BM (Furuyama and Mochitate, 2000). When mammary epithelial cells are grown in rBM matrix, not only do they self-assemble into 3D, polarized acini structures, but they also secrete their own BM (Debnath et al., 2003). While the rBM contains laminin-111, this cell-secreted BM contains laminin-332. The rotational movement known as coherent angular motion of mammary epithelial cells during self-assembly into acini in 3D culture is critical to the production of endogenous BM (Tanner et al., 2012; Wang et al., 2013). Similarly, rotational movement plays an important role in BM polarization in Drosophila egg chamber formation (Cetera et al., 2014).
Collagen I versus BM models
While collagen I gels are often used to study cell migration, they are not ideal BM invasion models. Compared with the nanoporous, sheet-like nature of BM, collagen I gels are microporous and fibrillar (Wolf et al., 2013). Moreover, collagen I is a potent ligand for many receptors involved in adhesion, differentiation, migration, and proliferation (Boraschi-Diaz et al., 2017). Mammary epithelial cells do not polarize into 3D acini in collagen I gels (Gudjonsson et al., 2002), and human breast tumor organoids invade into the surrounding matrix when embedded in collagen I, but not in rBM (Nguyen-Ngoc et al., 2012). Thus, while collagen I matrices are useful for modeling cell migration through the stromal matrix, they may not capture key aspects of BM invasion.
While six classes of proteases—MMPs and cysteine, serine, threonine, glutamic acid, and aspartate proteases—may all be involved in cancer invasion to some degree, MMPs are thought to be especially important during BM invasion (Webber et al., 1995; Danø et al., 1999; Eatemadi et al., 2017). In particular, expression of MT1-MMP (MMP14), MMP15, or MMP16 was found to be necessary and sufficient for tumor cell invasion through ex vivo peritoneal BM or BM secreted by MDCK cells (Hotary et al., 2006). While MT1-MMP, MMP15, and MMP16 are membrane-bound MMPs that cleave many ECM substrates, MMP2 and MMP9 are secreted MMPs that selectively degrade collagen IV (Jacob and Prekeris, 2015). Beyond their function in degradation, MMPs also process cytokines and chemokines, thus playing important roles in physiological processes including inflammation, neovascularization, and differentiation (Nagase et al., 2006; Van Lint and Libert, 2007). Without MMPs, it was found that cancer cells can squeeze and migrate through rigid or elastic pores only when the pores are larger than ∼3 µm in diameter, with the deformability of the stiffer nucleus serving as the limiting factor (Wolf et al., 2013; Harada et al., 2014). Given that BMs are nanoporous, the thinking has been that cells must use proteases to biochemically degrade the BM or migrate through large defects in the BM.
Invadopodia are mechanosensitive actin-rich protrusions implicated in delivering proteases to the matrix. Marked by cortactin, Tks4, and Tks5, invadopodia cyclically protrude on the timescale of hours and are 0.5–2 µm wide and >2 µm long (Murphy and Courtneidge, 2011; Leong et al., 2014). Invadopodia use MMP2, MMP9, and MT1-MMP to degrade the BM (Clark et al., 2007; Poincloux et al., 2009). Application of mechanical strain onto the surrounding ECM enhances invadopodia maturation and cell invasion (Gasparski et al., 2017). Invadopodia activity is highest at moderate levels of cross-linking in collagen I matrices, compared with much lower or higher cross-linking (Pourfarhangi et al., 2018). Increased ECM stiffness on 2D surfaces promotes the invadopodia formation, thus increasing degradation (Alexander et al., 2008; Jerrell and Parekh, 2016). To quantify invadopodia activity, gelatin degradation assays are commonly used, since many of the same proteases that degrade the BM also degrade gelatin. In this assay, cells are seeded onto a layer of fluorescent gelatin, and a decrease in signal equates to degraded gelatin and, therefore, invadopodia activity (Díaz, 2013). However, gelatin assays may not permit complete invadopodia formation and maturation (Tolde et al., 2010). On 2D substrates, protrusions lengths are limited to <1 µm due to the thin layer of gelatin that is blocked by the underlying glass (Enderling et al., 2008). In 3D BM-like matrices, invadopodia lengths can reach as high as 20 µm (Wisdom et al., 2018). More rigorous studies to determine the effect of stiffness and other mechanical properties on invadopodia formation in 3D are needed.
Force-driven BM invasion
The role of protease-independent BM invasion has been controversial but has been implicated in immune cells and, more recently, carcinoma cells. Immune cells frequently traverse vascular BM to enter blood circulation during inflammation. Leukocytes, neutrophils, and monocytes all preferentially migrated through areas of venular BM that exhibited lower (<60%) protein deposition of laminin, collagen IV, and nidogen (Wang et al., 2006; Voisin et al., 2009). While monocytes were highly deformable and squeezed through existing openings in the BM, neutrophil migration led to remodeling and subsequent enlargement of these low-protein sites. Dendritic cells have been shown to migrate through preexisting openings in the lymphatic BM by widening these small gaps (Pflicke and Sixt, 2009). After being widened by cells, these gaps returned to a baseline slightly larger than the original gap size, indicative of mechanical plasticity of the BM (Box 2). Protease-independent BM invasion in immune cells suggested the possibility of a protease-independent strategy to BM invasion by carcinoma cells.
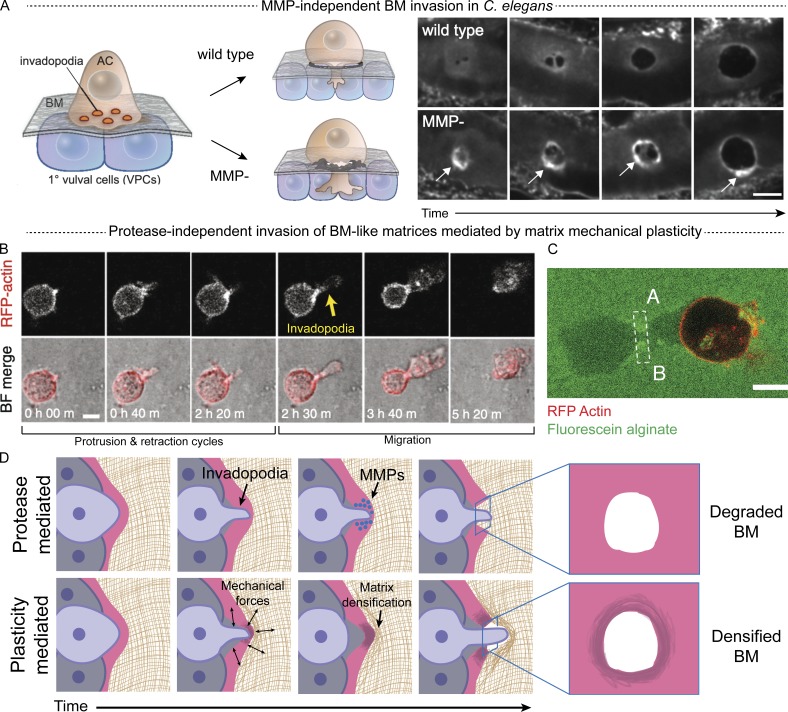
In a Caenorhabditis elegans model of BM invasion, cells could invade through the BM without proteases by applying force to deform the BM (Cáceres et al., 2018; Kelley et al., 2019). In C. elegans, an anchor cell, or specialized uterine cell, crosses the BM during a precise time during development, making it a useful in vivo model to study BM invasion. While anchor cells normally use proteases to degrade the BM, MMP-deficient anchor cells were still able to breach the BM by physically displacing the BM, evidenced by increased BM signal around the displaced hole (Fig. 2 A; Kelley et al., 2019). While wild-type animals used invadopodia to breach the BM, MMP-deficient animals formed protrusions that were approximately five times larger than normal invadopodia and enriched in actin, Arp2/3, mitochondria, and ATP (Kelley et al., 2019).
Figure 2.
Chemical and physical modes of BM invasion. (A) Anchor cell invasion in wild-type (top) and MMP-deficient (bottom) animals. Arrows point to increased fluorescence intensity of the BM at perimeter of cleared area. Scale bars, 5 µm. Image reproduced from Kelley et al. (2019) with permission from Elsevier. AC, anchor cell. (B) Cell extending and retracting invadopodia before migration in interpenetrating networks of rBM and alginate that exhibit sufficiently high matrix mechanical plasticity. Scale bars, 10 µm. Image reproduced from Wisdom et al. (2018) under a Creative Commons Attribution 4.0 International License. (C) Migrating cells in fluorescent alginate-rBM interpenetrating network leave lasting channels (region marked A to B) that cells can squeeze through. Scale bar, 10 µm. Image reproduced from Wisdom et al. (2018). (D) Cells can chemically degrade the BM using proteases (top) or physically break through the BM that exhibits mechanical plasticity using mechanical forces, which densifies the BM (bottom). Adapted from Wisdom et al. (2018) under a Creative Commons Attribution 4.0 International License.
Mechanistically, recent results indicate that matrix mechanical plasticity of the BM could permit protease-independent invasion in the absence of micron-sized defects. As with other soft tissues that are formed in part through weak bonds that link ECM proteins together, the BM likely exhibits some degree of mechanical plasticity (Box 2). A recent study examined the invasion and migration of cells through BM-like matrices with tunable mechanical plasticity. When the matrix exhibits sufficiently high mechanical plasticity, cells can widen nanosized pores within the BM-like matrices to create channels large enough for cells to invade through (Wisdom et al., 2018). Mechanistically, invadopodia exert both protrusive and contractile forces during repeated extension and retraction cycles to deform their surroundings and permanently open up micron-sized channels in the matrix (Fig. 2 B; Wisdom et al., 2018). While the primary function of invadopodia was thought to be BM degradation with proteases, these results highlight the role of invadopodia in generating force. Once micron-sized channels in the matrix were opened, cells then migrated through, exerting protrusive forces at the leading edge (Fig. 2 C). Increased covalent cross-linking of BM-like matrices diminishes matrix mechanical plasticity and restricts protrusions (Wisdom et al., 2019). One indication of plasticity-mediated invasion is matrix densification (Box 2). While holes in epithelial BM associated with initial invasion are difficult to capture, holes in lymphatic BM, including near metastases, have been observed (Pflicke and Sixt, 2009; Mayorca-Guiliani et al., 2017). These holes exhibit increased signal intensity at the border, suggesting matrix densification rather than degradation. This newly identified mechanism of protease-independent migration suggests that cells can circumvent protease-targeting drugs by engaging a physical migration mechanism (Fig. 2 D). In addition, the use of invadopodia in both protease-mediated and protease-independent invasion by carcinoma cells suggests the possibility that cells may use both modes synergistically during invasion in vivo.
Homotypic cell interactions on cancer cell invasion through the BM
Proliferation
Whether proliferation and invasion programs interact to overcome the BM barrier has been a question of great interest. Pathological studies found that above a threshold size, larger tumors are correlated with increased metastatic potential in renal and breast carcinoma, indicating a possible connection between proliferation and invasion (Thompson et al., 2009; Sopik and Narod, 2018). As cancer cells proliferate and ECM deposition increases, tumors grow and expand, while solid stress from the surrounding BM and stromal matrix resists this expansion. Experimental measurements combined with computational modeling indicate solid stresses of hundreds of pascals in brain tumors, ∼1 kPa in breast tumors, and ∼10 kPa in pancreatic tumors (Nia et al., 2016; Seano et al., 2019). Thus, the BM may be under a tensional prestress due to tumor expansion. One study found that mechanical compression of cancer cells on a 2D substrate with an agarose pad drives cancer cells toward an invasive phenotype, promoting leader cell activity (Tse et al., 2012). However, another study reported that a brief, transient compression applied to malignant breast cancer cells cultured in 3D BM-like matrices induced a phenotypic revision, with the cells establishing normal tissue architecture (Ricca et al., 2018).
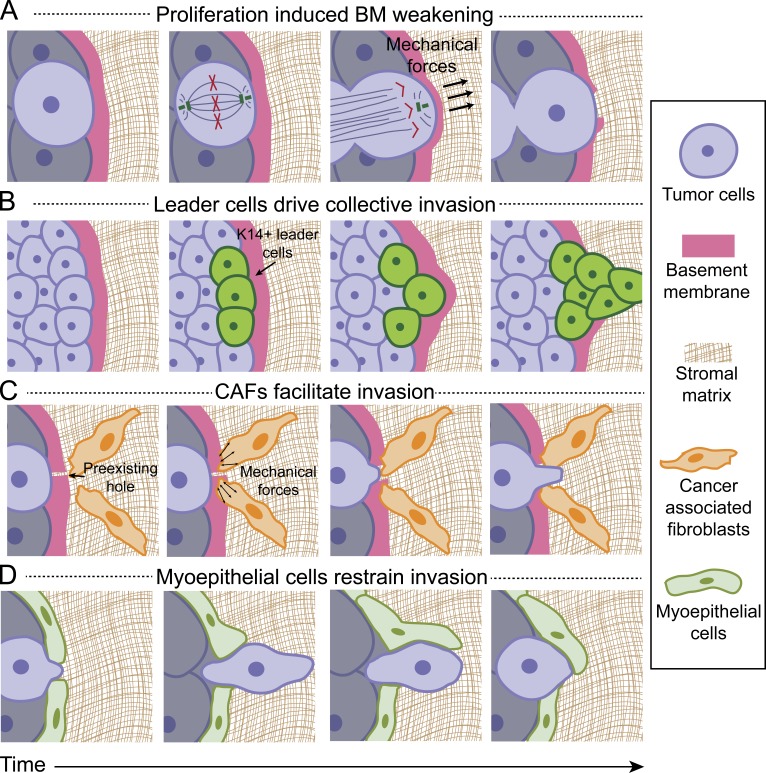
Recent work has implied the possibility that forces generated during cell division could directly weaken the BM, facilitating cancer invasion. Dividing cells generate extracellular protrusive stresses along the mitotic axis in the range of 1–2 kPa to allow mitotic elongation (Nam and Chaudhuri, 2018). Matrix deformation is greatest during anaphase and telophase/cytokinesis, due to forces generated by interpolar spindle elongation and cytokinetic ring contraction, which drives expansion along the mitotic axis due to volume conservation (Fig. 3 A). Although the maximum compression force that native human BM can withstand is unknown, these findings raise the possibility that forces generated during tumor proliferation alone can weaken or rupture the BM. Further, during the cell cycle leading up to mitosis, cells accumulate biomass and increase in volume, typically doubling in size, which may contribute to force exertion on the surrounding microenvironment (Son et al., 2015; Zlotek-Zlotkiewicz et al., 2015; Miettinen et al., 2019; Nam et al., 2019). Further studies are needed to dissect the impact of proliferation on invasion through cell signaling programs, as well as through direct and indirect mechanical action.
Figure 3.
Homotypic and heterotypic cell interactions associated with BM invasion. (A) Proposed representation of how dividing tumor cells may exert forces to breach the BM. Based on studies in Nam and Chaudhuri (2018). (B) Cytokeratin-14 is up-regulated in leader cells during collective invasion from tumors. Based on studies in Cheung et al. (2013). (C) CAFs physically weaken the BM, enabling tumor cells to escape from the primary tumor. Based on studies in Glentis et al. (2017). (D) Myoepithelial cells have been shown to restrain tumor cells from escaping and recapture disseminated tumor cells. Based on studies in Sirka et al. (2018).
Collective invasion and leader cells
While many previous studies have focused on single-cell invasion of the BM, collective invasion is likely more relevant to cancer invasion and metastasis. Histological evidence shows that cells invade collectively through the BM during initial invasion in cancer (Friedl et al., 2012). Moreover, circulating tumor cell (CTC) clusters, or groups of cells that have successfully escaped the primary tumor and entered blood circulation, are thought to account for >90% of metastases compared with single CTCs (Cheung et al., 2016). CTC clusters tend to derive from multicellular groupings of primary tumor cells rather than single cells (Aceto et al., 2014). Furthermore, multicellular CTCs have up to 100-fold greater metastatic potential than single-cell CTCs (Aceto et al., 2014; Cheung et al., 2016).
Within a cell cluster, a subpopulation of “leader cells” can emerge at the leading edge, trailed by follower cells. Leader cells are seen in wound healing, tracheal branching in Drosophila, and mammary cell morphogenesis (Khalil and Friedl, 2010; Yamaguchi et al., 2015). Rac, β1 integrin, and phosphatidylinositol 3-kinase have been shown to be up-regulated in leader cells (Yamaguchi et al., 2015). Moreover, leader cells have been shown to generate force to drag follower cells in a Rho-mediated mechanism (Reffay et al., 2014). However, other studies suggest that leader cells are not endowed with greater force-generating capabilities (Trepat et al., 2009). When breast cancer cells are seeded in collagen I matrices, leader cells up-regulated cytoskeletal protein keratin-14 (Cheung et al., 2013; Fig. 3 B). While no leader cell phenotypes were observed in rBM matrix, this may simply be because the acini remained noninvasive in the soft matrices. Thus, it will be important to determine whether this leader cell behavior with up-regulated keratin-14 is observed in stiff rBM matrices or other models of BM invasion. With the understanding that BM invasion is typically collective, it is critical to understand the unique features of collective invasion and the role of leader cells.
Heterotypic cell interactions during cancer cell invasion through the BM
Immune cells
Immune cells not only secrete signaling cues to promote tumor cell invasion, but also migrate through the BM themselves. Inflammation is frequently observed at tumor sites; immune cells are often found in tumor biopsies, and inflammatory diseases increase the risk for certain cancers (Mantovani et al., 2008). Macrophages also promote cancer cell intravasation (Condeelis and Pollard, 2006). Through paracrine signaling, cancer cells produce colony-stimulating factor-1 to stimulate migration in macrophages, and in return, macrophages produce EGF to stimulate migration in breast cancer cells (Wyckoff et al., 2004). Subsequent studies demonstrate that macrophages and cancer cells can interact to promote invasion through signaling pathways such as NF-κB and JNK, as well as through the release of cytokines such as TNF-α (Hagemann et al., 2005, 2006). Beyond cell signaling interactions, macrophages can use MMPs to degrade the BM (Tsuji et al., 2018). A recent study found that macrophages were required for cancer cell dissemination of very early stages of breast cancers, in which tumor metastases were identified despite the presence of only premalignant tumors (Linde et al., 2018). Macrophages can induce a malignant phenotype in a subpopulation of early disseminated cancer cells, which not only metastasize early but also interact with later-arriving tumor cells to facilitate growth of the metastasized cells. Despite the multitude of studies that have elucidated the role of immune cells in cancer, whether immune cells can facilitate cancer cell invasion via mechanical modification of the BM remains unclear.
Fibroblasts
Fibroblasts, which interact with neighboring cells through secretion of signaling molecules, were recently found to mechanically weaken the BM. Fibroblasts are mesenchymal cells that remodel ECM through degradation, mechanical remodeling, and secretion of ECM and growth factors (Kalluri and Zeisberg, 2006). Some of these growth factors stimulate laminin and collagen IV deposition by epithelial cells (El Ghalbzouri and Ponec, 2004). Moreover, fibroblast crosstalk with epithelial cells is necessary for proper BM formation (Smola et al., 1998; El Ghalbzouri et al., 2005). Cancer-associated fibroblasts (CAFs), a subpopulation of fibroblasts that are distinguished by α-smooth muscle actin expression, have been known to promote cancer invasion through paracrine signaling (Kalluri and Zeisberg, 2006) and ECM remodeling (Calvo et al., 2013). Recently, CAFs have been found to physically weaken the BM using contractile forces to expand preexisting gaps in the BM and facilitate cancer cell invasion through the gaps (Glentis et al., 2017; Fig. 3 C). In that study, CAFs were first seeded onto BM harvested from mouse mesentery to remodel the BM for several days. Compared to control BM with no CAF remodeling, CAF remodeled BM enhanced human colon cancer cell invasion. Moreover, cancer cells still invaded CAF-remodeled BM even in the presence of protease inhibitors. Thus, it was proposed that CAFs primarily weakened BM integrity, measured by decreased BM stiffness and increased cancer cell invasion, through contractile activity independent of protease degradation.
Myoepithelial cells
Myoepithelial cells are found between epithelial cells and the BM in some tissues and have been implicated in regulating invasion. In vivo, myoepithelial cells are found between epithelial cells and the BM, acting as an additional barrier to overcome during primary tumor escape. When co-cultured with healthy myoepithelial cells, epithelial cells form polarized acini and produce BM. However, when co-cultured with tumor-associated myoepithelial cells, epithelial cells failed to recapitulate the acini or produce BM (Gudjonsson et al., 2002). Tumor-associated myoepithelial cells promote an invasive phenotype in mammary epithelial cells through TGF-β signaling (Lo et al., 2017). Healthy myoepithelial cells typically surround luminal epithelial cells during noninvasive ductal carcinoma in situ, but diminish as cancer becomes invasive (Gudjonsson et al., 2005). In a 3D co-culture organoid collagen I assay of myoepithelial cells and tumor cells, myoepithelial cells not only acted as a passive physical barrier to epithelial cells, but also actively restrained and recaptured escaping epithelial cells (Fig. 3 D; Sirka et al., 2018). This myoepithelial barrier was compromised when α-smooth muscle actin or P-cadherin was depleted (Sirka et al., 2018). Since this study was performed in collagen I matrices, and myoepithelial cells are directly enclosed by the BM, future studies could elucidate whether an outer BM layer regulates myoepithelial cell action in restraining and recapturing invading cells.
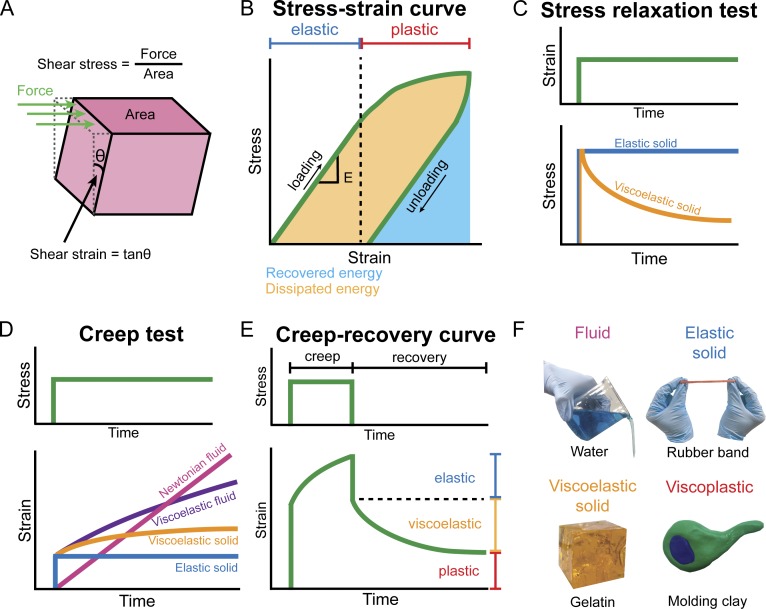
Box 2. Is the BM a viscous fluid, an elastic solid, viscoelastic, or viscoplastic?
Here we overview several categories of materials and consider which may serve as appropriate descriptors of the BM. Materials are often characterized by their response to the application and removal of an external force or deformation. Mechanical stress, which is force normalized by an area and can be normal or shear, is used to describe the local intensity of loading, while strain, which is a normalized measure of deformation, is used to describe the local intensity of deformation and can also be normal or shear. Materials are distinguished by relations between stress and strain or strain rate, storage versus loss of elastic energy, and reversible versus irreversible strain under loading. Biomaterial mechanical properties can be measured with a mechanical tester such as a rheometer, a device that applies shear stress or strain onto the sample and measures the resulting shear strain or stress, respectively (Fig. 4 A). A fluid exhibits continuously increasing strain, which can be measured as strain rate, in response to stress. In a Newtonian fluid, such as water, the strain rate is proportional to applied shear stress, and the constant of proportionality is the viscosity (η). Viscosity describes a fluid’s resistance to flow, and mechanical energy is dissipated in a fluid due to internal friction. In contrast, an elastic solid exhibits a constant time-independent strain in response to an applied stress. A perfectly elastic solid, often conceptualized as a spring, returns to its original shape when the applied stress is removed because energy is stored elastically and not dissipated. This can occur through reversible molecular deformations, such as the stretching of bonds between atoms, or through a reduction of entropy. At small strains, there is often a linear relationship between stress and strain in engineering materials, and the slope is defined as the elastic modulus (E), which relates to the concept of stiffness (Fig. 4 B). Many solid materials reach an elastic limit, beyond which the material starts experiencing irreversible, or plastic, deformation (Fig. 4 B).
Many biological materials are not purely viscous fluids or elastic solids and exhibit viscoelasticity and viscoplasticity, which both describe time-dependent material responses. Viscoelastic materials, such as gelatin or other hydrogels, exhibit properties of both viscous fluids and elastic solids, so the material response to an applied stress changes over time due to energy dissipation from the viscous component after an initial elastic response. Viscoelasticity can be characterized by the ratio between the loss modulus (G″), determined from the viscous response of a material in response to an oscillatory stress or strain, and the storage modulus (G′), determined from the elastic response. Viscoelasticity can also be characterized by stress relaxation, a decrease in stress under an applied constant strain (Fig. 4 C); creep, an increase in strain under an applied constant stress (Fig. 4 D); or hysteresis in the stress–strain curve during loading and unloading cycles (Fig. 4 B). Molecular events that dissipate energy, such as the unbinding of weak bonds or movement of fluid in a solid matrix, can give rise to viscoelasticity. Viscoelastic materials may also exhibit plasticity, or permanent deformation under load, and be viscoplastic, the property of time-dependent plasticity. Examples of viscoplastic materials include molding clay and silly putty. Viscoplasticity can be characterized through creep-recovery tests (Fig. 4 E). Many collagen-rich soft tissues and reconstituted ECMs exhibit viscoelastic and viscoplastic behaviors (Chaudhuri et al., 2016; Nam et al., 2016). Representative materials for these descriptors are shown in Fig. 4 F.
While direct tests of BM mechanical properties have been challenging, emerging biophysical evidence indicates that a viscoplastic description of the BM may be appropriate. Dehydrated BM exhibits a 10-fold decrease in thickness compared with normal, hydrated BM, illustrating the high water content of the BM, which would act to dissipate mechanical energy when deformed (Fabris et al., 2018). Weak bonds, such as those that link laminin together or those that laterally connect collagen IV molecules, can unbind under sufficient mechanical stress over time, dissipating energy and allowing matrix flow and opening up of the matrix pore structure (Nam et al., 2016). Rebinding of such weak bonds would make the deformation irreversible, leading to plasticity. In general, covalent cross-links, which can be viewed as permanent and irreversible connections, restrict matrix flow under stress and lead to a more solid-like matrix. Covalent cross-linking of the collagen IV network in BM could play a key role in impeding nonproteolytic mechanisms of BM invasion. The combination of covalent and weak cross-linking suggests that a viscoplastic description of the BM may be appropriate. Evidence of BM viscoplasticity include the findings that holes created in the BM are irreversible and remain open after invasion and, importantly, that BM density surrounding the holes increases in intensity, suggesting densification, rather than degradation, of BM (Pflicke and Sixt, 2009; Mayorca-Guiliani et al., 2017; Kelley et al., 2019; Fig. 2, A and D). While these are suggestive of a viscoplastic description, there is a critical need for measurements that definitively determine the mechanical character of the BM and the stresses, strains, and strain rates associated with cellular interactions with the BM during invasion.
Figure 4.
Mechanical testing of materials. (A) During mechanical testing, application of mechanical stress, or loading, results in an output mechanical strain, or deformation, or vice versa. (B) A material’s stress–strain curve can be separated into elastic and plastic regions, with reversible deformations occuring over the elastic region, and irreversible deformations occuring over the plastic region. Hysteresis between loading and unloading corresponds to dissipated energy. E, elastic modulus. (C) In a stress relaxation test, a constant strain is applied and stress is measured. (D) In a creep test, a constant stress is applied and strain is measured. (E) A creep–recovery curve, in which constant stress is applied during the creep and stress is removed during recovery, can be used to measure viscoelasticity and plastic deformation. (F) Material descriptors and their representative materials.
Concluding remarks
In this review, we have discussed the evidence that beyond using proteases, cells may use physical strategies to invade the BM, a key barrier to cancer cell invasion. In addition to its biological complexity, the BM exhibits unique mechanical characteristics that contribute to its robust barrier function that is particularly important in blocking cancer progression and metastasis. A deeper understanding of these mechanical properties illuminates previously unknown physical modes of BM invasion. These physical modes of invasion provide an alternative mechanism of invasion when proteases are inhibited and may act in concert with protease-dependent invasion mechanisms in the absence of treatment. Collectively, these findings suggest strategies for overcoming the failure of MMP inhibitors in clinical trials. In particular, targeting both modalities may be necessary for designing effective therapeutics for metastasis prevention.
Acknowledgments
We thank Professor Marc Levenston (Stanford University, Stanford, CA) and Professor Wei Cai (Stanford University, Stanford, CA) for helpful discussions.
We gratefully acknowledge a National Defense Science and Engineering Graduate fellowship for J. Chang, a National Science Foundation Graduate Research fellowship for J. Chang, and a National Institutes of Health National Cancer Institute grant (R37 CA214136) for O. Chaudhuri.
The authors declare no competing financial interests.
References
- Abrams G.A., Goodman S.L., Nealey P.F., Franco M., and Murphy C.J.. 2000. Nanoscale topography of the basement membrane underlying the corneal epithelium of the rhesus macaque. Cell Tissue Res. 299:39–46. 10.1007/s004410050004 [DOI] [PubMed] [Google Scholar]
- Acerbi I., Cassereau L., Dean I., Shi Q., Au A., Park C., Chen Y.Y., Liphardt J., Hwang E.S., and Weaver V.M.. 2015. Human breast cancer invasion and aggression correlates with ECM stiffening and immune cell infiltration. Integr. Biol. 7:1120–1134. 10.1039/c5ib00040h [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aceto N., Bardia A., Miyamoto D.T., Donaldson M.C., Wittner B.S., Spencer J.A., Yu M., Pely A., Engstrom A., Zhu H., et al. . 2014. Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell. 158:1110–1122. 10.1016/j.cell.2014.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander N.R., Branch K.M., Parekh A., Clark E.S., Iwueke I.C., Guelcher S.A., and Weaver A.M.. 2008. Extracellular matrix rigidity promotes invadopodia activity. Curr. Biol. 18:1295–1299. 10.1016/j.cub.2008.07.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck J.N., Singh A., Rothenberg A.R., Elisseeff J.H., and Ewald A.J.. 2013. The independent roles of mechanical, structural and adhesion characteristics of 3D hydrogels on the regulation of cancer invasion and dissemination. Biomaterials. 34:9486–9495. 10.1016/j.biomaterials.2013.08.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhave G., Colon S., and Ferrell N.. 2017. The sulfilimine cross-link of collagen IV contributes to kidney tubular basement membrane stiffness. Am. J. Physiol. Renal Physiol. 313:F596–F602. 10.1152/ajprenal.00096.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boraschi-Diaz I., Wang J., Mort J.S., and Komarova S.V.. 2017. Collagen Type I as a Ligand for Receptor-Mediated Signaling. Front. Phys. 5:12 10.3389/fphy.2017.00012 [DOI] [Google Scholar]
- Brückner B.R., and Janshoff A.. 2015. Elastic properties of epithelial cells probed by atomic force microscopy. Biochim. Biophys. Acta. 1853(11, 11 Pt B):3075–3082. 10.1016/j.bbamcr.2015.07.010 [DOI] [PubMed] [Google Scholar]
- Buxboim A., Rajagopal K., Brown A.E.X., and Discher D.E.. 2010. How deeply cells feel: methods for thin gels. J. Phys. Condens. Matter. 22:194116 10.1088/0953-8984/22/19/194116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cáceres R., Bojanala N., Kelley L.C., Dreier J., Manzi J., Di Federico F., Chi Q., Risler T., Testa I., Sherwood D.R., and Plastino J.. 2018. Forces drive basement membrane invasion in Caenorhabditis elegans. Proc. Natl. Acad. Sci. USA. 115:11537–11542. 10.1073/pnas.1808760115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvo F., Ege N., Grande-Garcia A., Hooper S., Jenkins R.P., Chaudhry S.I., Harrington K., Williamson P., Moeendarbary E., Charras G., and Sahai E.. 2013. Mechanotransduction and YAP-dependent matrix remodelling is required for the generation and maintenance of cancer-associated fibroblasts. Nat. Cell Biol. 15:637–646. 10.1038/ncb2756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candiello J., Balasubramani M., Schreiber E.M., Cole G.J., Mayer U., Halfter W., and Lin H.. 2007. Biomechanical properties of native basement membranes. FEBS J. 274:2897–2908. 10.1111/j.1742-4658.2007.05823.x [DOI] [PubMed] [Google Scholar]
- Carraro D.M., Elias E.V., and Andrade V.P.. 2014. Ductal carcinoma in situ of the breast: morphological and molecular features implicated in progression. Biosci. Rep. 34:19–28. 10.1042/BSR20130077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carulli S., Beck K., Dayan G., Boulesteix S., Lortat-Jacob H., and Rousselle P.. 2012. Cell surface proteoglycans syndecan-1 and -4 bind overlapping but distinct sites in laminin α3 LG45 protein domain. J. Biol. Chem. 287:12204–12216. 10.1074/jbc.M111.300061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cetera M., Ramirez-San Juan G.R., Oakes P.W., Lewellyn L., Fairchild M.J., Tanentzapf G., Gardel M.L., and Horne-Badovinac S.. 2014. Epithelial rotation promotes the global alignment of contractile actin bundles during Drosophila egg chamber elongation. Nat. Commun. 5:5511 10.1038/ncomms6511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri O., Koshy S.T., Branco da Cunha C., Shin J.-W., Verbeke C.S., Allison K.H., and Mooney D.J.. 2014. Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat. Mater. 13:970–978. 10.1038/nmat4009 [DOI] [PubMed] [Google Scholar]
- Chaudhuri O., Gu L., Klumpers D., Darnell M., Bencherif S.A., Weaver J.C., Huebsch N., Lee H.P., Lippens E., Duda G.N., and Mooney D.J.. 2016. Hydrogels with tunable stress relaxation regulate stem cell fate and activity. Nat. Mater. 15:326–334. 10.1038/nmat4489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.B., Lamar J.M., Li R., Hynes R.O., and Kamm R.D.. 2016. Elucidation of the Roles of Tumor Integrin β1 in the Extravasation Stage of the Metastasis Cascade. Cancer Res. 76:2513–2524. 10.1158/0008-5472.CAN-15-1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y.S., Champliaud M.F., Burgeson R.E., Marinkovich M.P., and Yurchenco P.D.. 1997. Self-assembly of laminin isoforms. J. Biol. Chem. 272:31525–31532. 10.1074/jbc.272.50.31525 [DOI] [PubMed] [Google Scholar]
- Cheung K.J., Gabrielson E., Werb Z., and Ewald A.J.. 2013. Collective invasion in breast cancer requires a conserved basal epithelial program. Cell. 155:1639–1651. 10.1016/j.cell.2013.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung K.J., Padmanaban V., Silvestri V., Schipper K., Cohen J.D., Fairchild A.N., Gorin M.A., Verdone J.E., Pienta K.J., Bader J.S., and Ewald A.J.. 2016. Polyclonal breast cancer metastases arise from collective dissemination of keratin 14-expressing tumor cell clusters. Proc. Natl. Acad. Sci. USA. 113:E854–E863. 10.1073/pnas.1508541113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia J., Kusuma N., Anderson R., Parker B., Bidwell B., Zamurs L., Nice E., and Pouliot N.. 2007. Evidence for a role of tumor-derived laminin-511 in the metastatic progression of breast cancer. Am. J. Pathol. 170:2135–2148. 10.2353/ajpath.2007.060709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chlasta J., Milani P., Runel G., Duteyrat J.-L., Arias L., Lamiré L.-A., Boudaoud A., and Grammont M.. 2017. Variations in basement membrane mechanics are linked to epithelial morphogenesis. Development. 144:4350–4362. 10.1242/dev.152652 [DOI] [PubMed] [Google Scholar]
- Clark E.S., Whigham A.S., Yarbrough W.G., and Weaver A.M.. 2007. Cortactin is an essential regulator of matrix metalloproteinase secretion and extracellular matrix degradation in invadopodia. Cancer Res. 67:4227–4235. 10.1158/0008-5472.CAN-06-3928 [DOI] [PubMed] [Google Scholar]
- Cloutier G., Sallenbach-Morrissette A., and Beaulieu J.-F.. 2019. Non-integrin laminin receptors in epithelia. Tissue Cell. 56:71–78. 10.1016/j.tice.2018.12.005 [DOI] [PubMed] [Google Scholar]
- Condeelis J., and Pollard J.W.. 2006. Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell. 124:263–266. 10.1016/j.cell.2006.01.007 [DOI] [PubMed] [Google Scholar]
- Corning Incorporated 2013. Corning® Matrigel® Matrix: Frequently Asked Questions. Available at: https://www.corning.com/catalog/cls/documents/faqs/faq_DL_026_Corning_Matrigel_Matrix.pdf (accessed February 2019).
- Coussens L.M., Fingleton B., and Matrisian L.M.. 2002. Matrix metalloproteinase inhibitors and cancer: trials and tribulations. Science. 295:2387–2392. 10.1126/science.1067100 [DOI] [PubMed] [Google Scholar]
- Crest J., Diz-Muñoz A., Chen D.-Y., Fletcher D.A., and Bilder D.. 2017. Organ sculpting by patterned extracellular matrix stiffness. eLife. 6:e24958 10.7554/eLife.24958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danø K., Rømer J., Nielsen B.S., Bjørn S., Pyke C., Rygaard J., and Lund L.R.. 1999. Cancer invasion and tissue remodeling--cooperation of protease systems and cell types. APMIS. 107:120–127. 10.1111/j.1699-0463.1999.tb01534.x [DOI] [PubMed] [Google Scholar]
- Debnath J., Muthuswamy S.K., and Brugge J.S.. 2003. Morphogenesis and oncogenesis of MCF-10A mammary epithelial acini grown in three-dimensional basement membrane cultures. Methods. 30:256–268. 10.1016/S1046-2023(03)00032-X [DOI] [PubMed] [Google Scholar]
- Diaz L.K., Cristofanilli M., Zhou X., Welch K.L., Smith T.L., Yang Y., Sneige N., Sahin A.A., and Gilcrease M.Z.. 2005. Beta4 integrin subunit gene expression correlates with tumor size and nuclear grade in early breast cancer. Mod. Pathol. 18:1165–1175. 10.1038/modpathol.3800411 [DOI] [PubMed] [Google Scholar]
- Díaz B. 2013. Invadopodia Detection and Gelatin Degradation Assay. Bio Protoc. 3:e997 10.21769/BioProtoc.997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupont S., Morsut L., Aragona M., Enzo E., Giulitti S., Cordenonsi M., Zanconato F., Le Digabel J., Forcato M., Bicciato S., et al. . 2011. Role of YAP/TAZ in mechanotransduction. Nature. 474:179–183. 10.1038/nature10137 [DOI] [PubMed] [Google Scholar]
- Eatemadi A., Aiyelabegan H.T., Negahdari B., Mazlomi M.A., Daraee H., Daraee N., Eatemadi R., and Sadroddiny E.. 2017. Role of protease and protease inhibitors in cancer pathogenesis and treatment. Biomed. Pharmacother. 86:221–231. 10.1016/j.biopha.2016.12.021 [DOI] [PubMed] [Google Scholar]
- El Ghalbzouri A., and Ponec M.. 2004. Diffusible factors released by fibroblasts support epidermal morphogenesis and deposition of basement membrane components. Wound Repair Regen. 12:359–367. 10.1111/j.1067-1927.2004.012306.x [DOI] [PubMed] [Google Scholar]
- El Ghalbzouri A., Jonkman M.F., Dijkman R., and Ponec M.. 2005. Basement membrane reconstruction in human skin equivalents is regulated by fibroblasts and/or exogenously activated keratinocytes. J. Invest. Dermatol. 124:79–86. 10.1111/j.0022-202X.2004.23549.x [DOI] [PubMed] [Google Scholar]
- Enderling H., Alexander N.R., Clark E.S., Branch K.M., Estrada L., Crooke C., Jourquin J., Lobdell N., Zaman M.H., Guelcher S.A., et al. . 2008. Dependence of invadopodia function on collagen fiber spacing and cross-linking: computational modeling and experimental evidence. Biophys. J. 95:2203–2218. 10.1529/biophysj.108.133199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engler A.J., Sen S., Sweeney H.L., and Discher D.E.. 2006. Matrix elasticity directs stem cell lineage specification. Cell. 126:677–689. 10.1016/j.cell.2006.06.044 [DOI] [PubMed] [Google Scholar]
- Fabris G., Lucantonio A., Hampe N., Noetzel E., Hoffmann B., DeSimone A., and Merkel R.. 2018. Nanoscale Topography and Poroelastic Properties of Model Tissue Breast Gland Basement Membranes. Biophys. J. 115:1770–1782. 10.1016/j.bpj.2018.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler A.L., Darris C.E., Chetyrkin S.V., Pedchenko V.K., Boudko S.P., Brown K.L., Gray Jerome W., Hudson J.K., Rokas A., and Hudson B.G.. 2017. Collagen IV and basement membrane at the evolutionary dawn of metazoan tissues. eLife. 6:e24176 10.7554/eLife.24176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingleton B. 2008. MMPs as therapeutic targets--still a viable option? Semin. Cell Dev. Biol. 19:61–68. 10.1016/j.semcdb.2007.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedl P., and Wolf K.. 2003. Tumour-cell invasion and migration: diversity and escape mechanisms. Nat. Rev. Cancer. 3:362–374. 10.1038/nrc1075 [DOI] [PubMed] [Google Scholar]
- Friedl P., Locker J., Sahai E., and Segall J.E.. 2012. Classifying collective cancer cell invasion. Nat. Cell Biol. 14:777–783. 10.1038/ncb2548 [DOI] [PubMed] [Google Scholar]
- Furuyama A., and Mochitate K.. 2000. Assembly of the exogenous extracellular matrix during basement membrane formation by alveolar epithelial cells in vitro. J. Cell Sci. 113:859–868. [DOI] [PubMed] [Google Scholar]
- Gaiko-Shcherbak A., Fabris G., Dreissen G., Merkel R., Hoffmann B., and Noetzel E.. 2015. The Acinar Cage: Basement Membranes Determine Molecule Exchange and Mechanical Stability of Human Breast Cell Acini. PLoS One. 10:e0145174 10.1371/journal.pone.0145174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparski A.N., Ozarkar S., and Beningo K.A.. 2017. Transient mechanical strain promotes the maturation of invadopodia and enhances cancer cell invasion in vitro. J. Cell Sci. 130:1965–1978. 10.1242/jcs.199760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilles C., Polette M., Coraux C., Tournier J.M., Meneguzzi G., Munaut C., Volders L., Rousselle P., Birembaut P., and Foidart J.M.. 2001. Contribution of MT1-MMP and of human laminin-5 gamma2 chain degradation to mammary epithelial cell migration. J. Cell Sci. 114:2967–2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glentis A., Gurchenkov V., and Matic Vignjevic D.. 2014. Assembly, heterogeneity, and breaching of the basement membranes. Cell Adhes. Migr. 8:236–245. 10.4161/cam.28733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glentis A., Oertle P., Mariani P., Chikina A., El Marjou F., Attieh Y., Zaccarini F., Lae M., Loew D., Dingli F., et al. . 2017. Cancer-associated fibroblasts induce metalloprotease-independent cancer cell invasion of the basement membrane. Nat. Commun. 8:924 10.1038/s41467-017-00985-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goult B.T., Yan J., and Schwartz M.A.. 2018. Talin as a mechanosensitive signaling hub. J. Cell Biol. 217:3776–3784. 10.1083/jcb.201808061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudjonsson T., Rønnov-Jessen L., Villadsen R., Rank F., Bissell M.J., and Petersen O.W.. 2002. Normal and tumor-derived myoepithelial cells differ in their ability to interact with luminal breast epithelial cells for polarity and basement membrane deposition. J. Cell Sci. 115:39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudjonsson T., Adriance M.C., Sternlicht M.D., Petersen O.W., and Bissell M.J.. 2005. Myoepithelial cells: their origin and function in breast morphogenesis and neoplasia. J. Mammary Gland Biol. Neoplasia. 10:261–272. 10.1007/s10911-005-9586-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gusterson B.A., Warburton M.J., Mitchell D., Ellison M., Neville A.M., and Rudland P.S.. 1982. Distribution of myoepithelial cells and basement membrane proteins in the normal breast and in benign and malignant breast diseases. Cancer Res. 42:4763–4770. [PubMed] [Google Scholar]
- Hagemann T., Wilson J., Kulbe H., Li N.F., Leinster D.A., Charles K., Klemm F., Pukrop T., Binder C., and Balkwill F.R.. 2005. Macrophages induce invasiveness of epithelial cancer cells via NF-kappa B and JNK. J. Immunol. 175:1197–1205. 10.4049/jimmunol.175.2.1197 [DOI] [PubMed] [Google Scholar]
- Hagemann T., Wilson J., Burke F., Kulbe H., Li N.F., Plüddemann A., Charles K., Gordon S., and Balkwill F.R.. 2006. Ovarian cancer cells polarize macrophages toward a tumor-associated phenotype. J. Immunol. 176:5023–5032. 10.4049/jimmunol.176.8.5023 [DOI] [PubMed] [Google Scholar]
- Halfter W., Candiello J., Hu H., Zhang P., Schreiber E., and Balasubramani M.. 2013. Protein composition and biomechanical properties of in vivo-derived basement membranes. Cell Adhes. Migr. 7:64–71. 10.4161/cam.22479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfter W., Oertle P., Monnier C.A., Camenzind L., Reyes-Lua M., Hu H., Candiello J., Labilloy A., Balasubramani M., Henrich P.B., and Plodinec M.. 2015. New concepts in basement membrane biology. FEBS J. 282:4466–4479. 10.1111/febs.13495 [DOI] [PubMed] [Google Scholar]
- Harada T., Swift J., Irianto J., Shin J.-W., Spinler K.R., Athirasala A., Diegmiller R., Dingal P.C.D.P., Ivanovska I.L., and Discher D.E.. 2014. Nuclear lamin stiffness is a barrier to 3D migration, but softness can limit survival. J. Cell Biol. 204:669–682. 10.1083/jcb.201308029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hohenester E., and Yurchenco P.D.. 2013. Laminins in basement membrane assembly. Cell Adhes. Migr. 7:56–63. 10.4161/cam.21831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotary K., Li X.-Y., Allen E., Stevens S.L., and Weiss S.J.. 2006. A cancer cell metalloprotease triad regulates the basement membrane transmigration program. Genes Dev. 20:2673–2686. 10.1101/gad.1451806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard A.M., LaFever K.S., Fenix A.M., Scurrah C.R., Lau K.S., Burnette D.T., Bhave G., Ferrell N., and Page-McCaw A.. 2019. DSS-induced damage to basement membranes is repaired by matrix replacement and crosslinking. J. Cell Sci. 132:jcs226860 10.1242/jcs.226860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphries J.D., Byron A., and Humphries M.J.. 2006. Integrin ligands at a glance. J. Cell Sci. 119:3901–3903. 10.1242/jcs.03098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iozzo R.V. 2005. Basement membrane proteoglycans: from cellar to ceiling. Nat. Rev. Mol. Cell Biol. 6:646–656. 10.1038/nrm1702 [DOI] [PubMed] [Google Scholar]
- Iozzo R.V., Zoeller J.J., and Nyström A.. 2009. Basement membrane proteoglycans: modulators Par Excellence of cancer growth and angiogenesis. Mol. Cells. 27:503–513. 10.1007/s10059-009-0069-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob A., and Prekeris R.. 2015. The regulation of MMP targeting to invadopodia during cancer metastasis. Front. Cell Dev. Biol. 3:4 10.3389/fcell.2015.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerrell R.J., and Parekh A.. 2016. Matrix rigidity differentially regulates invadopodia activity through ROCK1 and ROCK2. Biomaterials. 84:119–129. 10.1016/j.biomaterials.2016.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R., and Zeisberg M.. 2006. Fibroblasts in cancer. Nat. Rev. Cancer. 6:392–401. 10.1038/nrc1877 [DOI] [PubMed] [Google Scholar]
- Kargozaran H., Yuan S.Y., Breslin J.W., Watson K.D., Gaudreault N., Breen A., and Wu M.H.. 2007. A role for endothelial-derived matrix metalloproteinase-2 in breast cancer cell transmigration across the endothelial-basement membrane barrier. Clin. Exp. Metastasis. 24:495–502. 10.1007/s10585-007-9086-6 [DOI] [PubMed] [Google Scholar]
- Kefalides N., and Borel J.. 2005. Morphology and Ultrastructure of Basement Membranes. Curr. Top. Membr. 56:19–42. 10.1016/S1063-5823(05)56002-2 [DOI] [Google Scholar]
- Kelley L.C., Lohmer L.L., Hagedorn E.J., and Sherwood D.R.. 2014. Traversing the basement membrane in vivo: a diversity of strategies. J. Cell Biol. 204:291–302. 10.1083/jcb.201311112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley L.C., Chi Q., Cáceres R., Hastie E., Schindler A.J., Jiang Y., Matus D.Q., Plastino J., and Sherwood D.R.. 2019. Adaptive F-Actin Polymerization and Localized ATP Production Drive Basement Membrane Invasion in the Absence of MMPs. Dev. Cell. 48:313–328.e8. 10.1016/j.devcel.2018.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern A., Eble J., Golbik R., and Kühn K.. 1993. Interaction of type IV collagen with the isolated integrins alpha 1 beta 1 and alpha 2 beta 1. Eur. J. Biochem. 215:151–159. 10.1111/j.1432-1033.1993.tb18017.x [DOI] [PubMed] [Google Scholar]
- Khalil A.A., and Friedl P.. 2010. Determinants of leader cells in collective cell migration. Integr. Biol. 2:568–574. 10.1039/c0ib00052c [DOI] [PubMed] [Google Scholar]
- Khoshnoodi J., Pedchenko V., and Hudson B.G.. 2008. Mammalian collagen IV. Microsc. Res. Tech. 71:357–370. 10.1002/jemt.20564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman H.K., McGarvey M.L., Liotta L.A., Robey P.G., Tryggvason K., and Martin G.R.. 1982. Isolation and characterization of type IV procollagen, laminin, and heparan sulfate proteoglycan from the EHS sarcoma. Biochemistry. 21:6188–6193. 10.1021/bi00267a025 [DOI] [PubMed] [Google Scholar]
- Kong H.J., Liu J., Riddle K., Matsumoto T., Leach K., and Mooney D.J.. 2005. Non-viral gene delivery regulated by stiffness of cell adhesion substrates. Nat. Mater. 4:460–464. 10.1038/nmat1392 [DOI] [PubMed] [Google Scholar]
- Koshikawa N., Schenk S., Moeckel G., Sharabi A., Miyazaki K., Gardner H., Zent R., and Quaranta V.. 2004. Proteolytic processing of laminin-5 by MT1-MMP in tissues and its effects on epithelial cell morphology. FASEB J. 18:364–366. 10.1096/fj.03-0584fje [DOI] [PubMed] [Google Scholar]
- Lambert A.W., Pattabiraman D.R., and Weinberg R.A.. 2017. Emerging Biological Principles of Metastasis. Cell. 168:670–691. 10.1016/j.cell.2016.11.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Last J.A., Liliensiek S.J., Nealey P.F., and Murphy C.J.. 2009. Determining the mechanical properties of human corneal basement membranes with atomic force microscopy. J. Struct. Biol. 167:19–24. 10.1016/j.jsb.2009.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.P., Stowers R., and Chaudhuri O.. 2019a Volume expansion and TRPV4 activation regulate stem cell fate in three-dimensional microenvironments. Nat. Commun. 10:529 10.1038/s41467-019-08465-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.Y., Chang J.K., Dominguez A.A., Lee H.P., Nam S., Chang J., Varma S., Qi L.S., West R.B., and Chaudhuri O.. 2019b YAP-independent mechanotransduction drives breast cancer progression. Nat. Commun. 10:1848 10.1038/s41467-019-09755-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong H.S., Robertson A.E., Stoletov K., Leith S.J., Chin C.A., Chien A.E., Hague M.N., Ablack A., Carmine-Simmen K., McPherson V.A., et al. . 2014. Invadopodia are required for cancer cell extravasation and are a therapeutic target for metastasis. Cell Reports. 8:1558–1570. 10.1016/j.celrep.2014.07.050 [DOI] [PubMed] [Google Scholar]
- Leung C.T., and Brugge J.S.. 2012. Outgrowth of single oncogene-expressing cells from suppressive epithelial environments. Nature. 482:410–413. 10.1038/nature10826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levental I., Georges P.C., and Janmey P.A.. 2007. Soft biological materials and their impact on cell function. Soft Matter. 3:299–306. 10.1039/B610522J [DOI] [PubMed] [Google Scholar]
- Lin Y.-C., Tambe D.T., Park C.Y., Wasserman M.R., Trepat X., Krishnan R., Lenormand G., Fredberg J.J., and Butler J.P.. 2010. Mechanosensing of substrate thickness. Phys. Rev. E Stat. Nonlin. Soft Matter Phys. 82:041918 10.1103/PhysRevE.82.041918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde N., Casanova-Acebes M., Sosa M.S., Mortha A., Rahman A., Farias E., Harper K., Tardio E., Reyes Torres I., Jones J., et al. . 2018. Macrophages orchestrate breast cancer early dissemination and metastasis. Nat. Commun. 9:21 10.1038/s41467-017-02481-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liotta L.A., Tryggvason K., Garbisa S., Hart I., Foltz C.M., and Shafie S.. 1980. Metastatic potential correlates with enzymatic degradation of basement membrane collagen. Nature. 284:67–68. 10.1038/284067a0 [DOI] [PubMed] [Google Scholar]
- Liu A., Wei L., Gardner W.A., Deng C.-X., and Man Y.-G.. 2009. Correlated alterations in prostate basal cell layer and basement membrane. Int. J. Biol. Sci. 5:276–285. 10.7150/ijbs.5.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo C.M., Wang H.B., Dembo M., and Wang Y.L.. 2000. Cell movement is guided by the rigidity of the substrate. Biophys. J. 79:144–152. 10.1016/S0006-3495(00)76279-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo P.-K., Zhang Y., Yao Y., Wolfson B., Yu J., Han S.-Y., Duru N., and Zhou Q.. 2017. Tumor-associated myoepithelial cells promote the invasive progression of ductal carcinoma in situ through activation of TGFβ signaling. J. Biol. Chem. 292:11466–11484. 10.1074/jbc.M117.775080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A., Allavena P., Sica A., and Balkwill F.. 2008. Cancer-related inflammation. Nature. 454:436–444. 10.1038/nature07205 [DOI] [PubMed] [Google Scholar]
- Martin G.R., and Timpl R.. 1987. Laminin and other basement membrane components. Annu. Rev. Cell Biol. 3:57–85. 10.1146/annurev.cb.03.110187.000421 [DOI] [PubMed] [Google Scholar]
- Mayorca-Guiliani A.E., Madsen C.D., Cox T.R., Horton E.R., Venning F.A., and Erler J.T.. 2017. ISDoT: in situ decellularization of tissues for high-resolution imaging and proteomic analysis of native extracellular matrix. Nat. Med. 23:890–898. 10.1038/nm.4352 [DOI] [PubMed] [Google Scholar]
- McGowan K.A., and Marinkovich M.P.. 2000. Laminins and human disease. Microsc. Res. Tech. 51:262–279. [DOI] [PubMed] [Google Scholar]
- McKee K.K., Harrison D., Capizzi S., and Yurchenco P.D.. 2007. Role of laminin terminal globular domains in basement membrane assembly. J. Biol. Chem. 282:21437–21447. 10.1074/jbc.M702963200 [DOI] [PubMed] [Google Scholar]
- Miettinen T.P., Kang J.H., Yang L.F., and Manalis S.R.. 2019. Mammalian cell growth dynamics in mitosis. eLife. 8:e44700 10.7554/eLife.44700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammadi H., and McCulloch C.A.. 2014. Impact of elastic and inelastic substrate behaviors on mechanosensation. Soft Matter. 10:408–420. 10.1039/C3SM52729H [DOI] [PubMed] [Google Scholar]
- Murphy D.A., and Courtneidge S.A.. 2011. The ‘ins’ and ‘outs’ of podosomes and invadopodia: characteristics, formation and function. Nat. Rev. Mol. Cell Biol. 12:413–426. 10.1038/nrm3141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mylonas C.C., and Lazaris A.C.. 2014. Colorectal cancer and basement membranes: clinicopathological correlations. Gastroenterol. Res. Pract. 2014:580159 10.1155/2014/580159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagase H., Visse R., and Murphy G.. 2006. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res. 69:562–573. 10.1016/j.cardiores.2005.12.002 [DOI] [PubMed] [Google Scholar]
- Nam S., and Chaudhuri O.. 2018. Mitotic cells generate protrusive extracellular forces to divide in three-dimensional microenvironments. Nat. Phys. 14:621–628. 10.1038/s41567-018-0092-1 [DOI] [Google Scholar]
- Nam S., Lee J., Brownfield D.G., and Chaudhuri O.. 2016. Viscoplasticity Enables Mechanical Remodeling of Matrix by Cells. Biophys. J. 111:2296–2308. 10.1016/j.bpj.2016.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam S., Gupta V., Lee H., Lee J., Flaum E., Wisdom K., Varma S., Davis C., West R., and Chaudhuri O.. 2019. Cell cycle progression in confining microenvironments is regulated by a growth responsive TRPV4-PI3K/Akt-p27Kip1 signaling axis. Science Advances. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen-Ngoc K.-V., Cheung K.J., Brenot A., Shamir E.R., Gray R.S., Hines W.C., Yaswen P., Werb Z., and Ewald A.J.. 2012. ECM microenvironment regulates collective migration and local dissemination in normal and malignant mammary epithelium. Proc. Natl. Acad. Sci. USA. 109:E2595–E2604. 10.1073/pnas.1212834109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nia H.T., Liu H., Seano G., Datta M., Jones D., Rahbari N., Incio J., Chauhan V.P., Jung K., Martin J.D., et al. . 2016. Solid stress and elastic energy as measures of tumour mechanopathology. Nat. Biomed. Eng. 10.1038/s41551-016-0004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odenthal U., Haehn S., Tunggal P., Merkl B., Schomburg D., Frie C., Paulsson M., and Smyth N.. 2004. Molecular analysis of laminin N-terminal domains mediating self-interactions. J. Biol. Chem. 279:44504–44512. 10.1074/jbc.M402455200 [DOI] [PubMed] [Google Scholar]
- Paine I.S., and Lewis M.T.. 2017. The Terminal End Bud: the Little Engine that Could. J. Mammary Gland Biol. Neoplasia. 22:93–108. 10.1007/s10911-017-9372-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paszek M.J., Zahir N., Johnson K.R., Lakins J.N., Rozenberg G.I., Gefen A., Reinhart-King C.A., Margulies S.S., Dembo M., Boettiger D., et al. . 2005. Tensional homeostasis and the malignant phenotype. Cancer Cell. 8:241–254. 10.1016/j.ccr.2005.08.010 [DOI] [PubMed] [Google Scholar]
- Patarroyo M., Tryggvason K., and Virtanen I.. 2002. Laminin isoforms in tumor invasion, angiogenesis and metastasis. Semin. Cancer Biol. 12:197–207. 10.1016/S1044-579X(02)00023-8 [DOI] [PubMed] [Google Scholar]
- Paulsson M. 1992. Basement membrane proteins: structure, assembly, and cellular interactions. Crit. Rev. Biochem. Mol. Biol. 27:93–127. 10.3109/10409239209082560 [DOI] [PubMed] [Google Scholar]
- Pelham R.J. Jr., and Wang Y.. 1997. Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc. Natl. Acad. Sci. USA. 94:13661–13665. 10.1073/pnas.94.25.13661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen O.W., Rønnov-Jessen L., Howlett A.R., and Bissell M.J.. 1992. Interaction with basement membrane serves to rapidly distinguish growth and differentiation pattern of normal and malignant human breast epithelial cells. Proc. Natl. Acad. Sci. USA. 89:9064–9068. 10.1073/pnas.89.19.9064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pflicke H., and Sixt M.. 2009. Preformed portals facilitate dendritic cell entry into afferent lymphatic vessels. J. Exp. Med. 206:2925–2935. 10.1084/jem.20091739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poincloux R., Lizárraga F., and Chavrier P.. 2009. Matrix invasion by tumour cells: a focus on MT1-MMP trafficking to invadopodia. J. Cell Sci. 122:3015–3024. 10.1242/jcs.034561 [DOI] [PubMed] [Google Scholar]
- Pöschl E., Schlötzer-Schrehardt U., Brachvogel B., Saito K., Ninomiya Y., and Mayer U.. 2004. Collagen IV is essential for basement membrane stability but dispensable for initiation of its assembly during early development. Development. 131:1619–1628. 10.1242/dev.01037 [DOI] [PubMed] [Google Scholar]
- Pouliot N., and Kusuma N.. 2013. Laminin-511: a multi-functional adhesion protein regulating cell migration, tumor invasion and metastasis. Cell Adhes. Migr. 7:142–149. 10.4161/cam.22125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourfarhangi K.E., Bergman A., and Gligorijevic B.. 2018. ECM Cross-Linking Regulates Invadopodia Dynamics. Biophys. J. 114:1455–1466. 10.1016/j.bpj.2018.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reffay M., Parrini M.C., Cochet-Escartin O., Ladoux B., Buguin A., Coscoy S., Amblard F., Camonis J., and Silberzan P.. 2014. Interplay of RhoA and mechanical forces in collective cell migration driven by leader cells. Nat. Cell Biol. 16:217–223. [DOI] [PubMed] [Google Scholar]
- Ricca B.L., Venugopalan G., Furuta S., Tanner K., Orellana W.A., Reber C.D., Brownfield D.G., Bissell M.J., and Fletcher D.A.. 2018. Transient external force induces phenotypic reversion of malignant epithelial structures via nitric oxide signaling. eLife. 7:e26161 10.7554/eLife.26161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabeh F., Ota I., Holmbeck K., Birkedal-Hansen H., Soloway P., Balbin M., Lopez-Otin C., Shapiro S., Inada M., Krane S., et al. . 2004. Tumor cell traffic through the extracellular matrix is controlled by the membrane-anchored collagenase MT1-MMP. J. Cell Biol. 167:769–781. 10.1083/jcb.200408028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahai E., and Marshall C.J.. 2003. Differing modes of tumour cell invasion have distinct requirements for Rho/ROCK signalling and extracellular proteolysis. Nat. Cell Biol. 5:711–719. 10.1038/ncb1019 [DOI] [PubMed] [Google Scholar]
- Schmoeckel C., Stolz W., Sakai L.Y., Burgeson R.E., Timpl R., and Krieg T.. 1989. Structure of basement membranes in malignant melanoma and nevocytic nevi. J. Invest. Dermatol. 92:663–668. 10.1016/0022-202X(89)90179-6 [DOI] [PubMed] [Google Scholar]
- Seano G., Nia H.T., Emblem K.E., Datta M., Ren J., Krishnan S., Kloepper J., Pinho M.C., Ho W.W., Ghosh M., et al. . 2019. Solid stress in brain tumours causes neuronal loss and neurological dysfunction and can be reversed by lithium. Nat. Biomed. Eng. 3:230–245. 10.1038/s41551-018-0334-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen S., Engler A.J., and Discher D.E.. 2009. Matrix strains induced by cells: Computing how far cells can feel. Cell. Mol. Bioeng. 2:39–48. 10.1007/s12195-009-0052-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siebold B., Qian R.A., Glanville R.W., Hofmann H., Deutzmann R., and Kühn K.. 1987. Construction of a model for the aggregation and cross-linking region (7S domain) of type IV collagen based upon an evaluation of the primary structure of the alpha 1 and alpha 2 chains in this region. Eur. J. Biochem. 168:569–575. 10.1111/j.1432-1033.1987.tb13455.x [DOI] [PubMed] [Google Scholar]
- Siegel R.L., Miller K.D., and Jemal A.. 2019. Cancer statistics, 2019. CA Cancer J. Clin. 69:7–34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- Simon T., and Bromberg J.S.. 2017. Regulation of the Immune System by Laminins. Trends Immunol. 38:858–871. 10.1016/j.it.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirka O.K., Shamir E.R., and Ewald A.J.. 2018. Myoepithelial cells are a dynamic barrier to epithelial dissemination. J. Cell Biol. 217:3368–3381. 10.1083/jcb.201802144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smola H., Stark H.-J., Thiekötter G., Mirancea N., Krieg T., and Fusenig N.E.. 1998. Dynamics of basement membrane formation by keratinocyte-fibroblast interactions in organotypic skin culture. Exp. Cell Res. 239:399–410. 10.1006/excr.1997.3910 [DOI] [PubMed] [Google Scholar]
- Son S., Kang J.H., Oh S., Kirschner M.W., Mitchison T.J., and Manalis S.. 2015. Resonant microchannel volume and mass measurements show that suspended cells swell during mitosis. J. Cell Biol. 211:757–763. 10.1083/jcb.201505058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soofi S.S., Last J.A., Liliensiek S.J., Nealey P.F., and Murphy C.J.. 2009. The elastic modulus of Matrigel as determined by atomic force microscopy. J. Struct. Biol. 167:216–219. 10.1016/j.jsb.2009.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sopik V., and Narod S.A.. 2018. The relationship between tumour size, nodal status and distant metastases: on the origins of breast cancer. Breast Cancer Res. Treat. 170:647–656. 10.1007/s10549-018-4796-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowers R.S., Allen S.C., Sanchez K., Davis C.L., Ebelt N.D., Van Den Berg C., and Suggs L.J.. 2017. Extracellular Matrix Stiffening Induces a Malignant Phenotypic Transition in Breast Epithelial Cells. Cell. Mol. Bioeng. 10:114–123. 10.1007/s12195-016-0468-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundaramoorthy M., Meiyappan M., Todd P., and Hudson B.G.. 2002. Crystal structure of NC1 domains. Structural basis for type IV collagen assembly in basement membranes. J. Biol. Chem. 277:31142–31153. 10.1074/jbc.M201740200 [DOI] [PubMed] [Google Scholar]
- Swift J., Ivanovska I.L., Buxboim A., Harada T., Dingal P.C.D.P., Pinter J., Pajerowski J.D., Spinler K.R., Shin J.-W., Tewari M., et al. . 2013. Nuclear Lamin-A Scales with Tissue Stiffness and Enhances Matrix-Directed Differentiation. Science. 341:1240104 10.1126/science.1240104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner K., Mori H., Mroue R., Bruni-Cardoso A., and Bissell M.J.. 2012. Coherent angular motion in the establishment of multicellular architecture of glandular tissues. Proc. Natl. Acad. Sci. USA. 109:1973–1978. 10.1073/pnas.1119578109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Than M.E., Henrich S., Huber R., Ries A., Mann K., Kühn K., Timpl R., Bourenkov G.P., Bartunik H.D., and Bode W.. 2002. The 1.9-A crystal structure of the noncollagenous (NC1) domain of human placenta collagen IV shows stabilization via a novel type of covalent Met-Lys cross-link. Proc. Natl. Acad. Sci. USA. 99:6607–6612. 10.1073/pnas.062183499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R.H., Hill J.R., Babayev Y., Cronin A., Kaag M., Kundu S., Bernstein M., Coleman J., Dalbagni G., Touijer K., and Russo P.. 2009. Metastatic renal cell carcinoma risk according to tumor size. J. Urol. 182:41–45. 10.1016/j.juro.2009.02.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timpl R., Wiedemann H., van Delden V., Furthmayr H., and Kühn K.. 1981. A network model for the organization of type IV collagen molecules in basement membranes. Eur. J. Biochem. 120:203–211. 10.1111/j.1432-1033.1981.tb05690.x [DOI] [PubMed] [Google Scholar]
- Tolde O., Rösel D., Veselý P., Folk P., and Brábek J.. 2010. The structure of invadopodia in a complex 3D environment. Eur. J. Cell Biol. 89:674–680. 10.1016/j.ejcb.2010.04.003 [DOI] [PubMed] [Google Scholar]
- Trepat X., Wasserman M.R., Angelini T.E., Millet E., Weitz D.A., Butler J.P., and Fredberg J.J.. 2009. Physical forces during collective cell migration. Nat. Phys. 5:426–430. 10.1038/nphys1269 [DOI] [Google Scholar]
- Tse J.M., Cheng G., Tyrrell J.A., Wilcox-Adelman S.A., Boucher Y., Jain R.K., and Munn L.L.. 2012. Mechanical compression drives cancer cells toward invasive phenotype. Proc. Natl. Acad. Sci. USA. 109:911–916. 10.1073/pnas.1118910109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuji N., Matsuura T., Narama I., Yoshiki A., and Ozaki K.. 2018. Macrophage-Associated Gelatinase Degrades Basement Membrane at the Optic Fissure Margins During Normal Ocular Development in Mice. Invest. Ophthalmol. Vis. Sci. 59:1368–1373. 10.1167/iovs.17-21841 [DOI] [PubMed] [Google Scholar]
- Udayakumar T.S., Chen M.L., Bair E.L., Von Bredow D.C., Cress A.E., Nagle R.B., and Bowden G.T.. 2003. Membrane type-1-matrix metalloproteinase expressed by prostate carcinoma cells cleaves human laminin-5 beta3 chain and induces cell migration. Cancer Res. 63:2292–2299. [PubMed] [Google Scholar]
- Vanacore R., Ham A.-J.L., Voehler M., Sanders C.R., Conrads T.P., Veenstra T.D., Sharpless K.B., Dawson P.E., and Hudson B.G.. 2009. A sulfilimine bond identified in collagen IV. Science. 325:1230–1234. 10.1126/science.1176811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Lint P., and Libert C.. 2007. Chemokine and cytokine processing by matrix metalloproteinases and its effect on leukocyte migration and inflammation. J. Leukoc. Biol. 82:1375–1381. 10.1189/jlb.0607338 [DOI] [PubMed] [Google Scholar]
- Voisin M.-B., Woodfin A., and Nourshargh S.. 2009. Monocytes and neutrophils exhibit both distinct and common mechanisms in penetrating the vascular basement membrane in vivo. Arterioscler. Thromb. Vasc. Biol. 29:1193–1199. 10.1161/ATVBAHA.109.187450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Lacoche S., Huang L., Xue B., and Muthuswamy S.K.. 2013. Rotational motion during three-dimensional morphogenesis of mammary epithelial acini relates to laminin matrix assembly. Proc. Natl. Acad. Sci. USA. 110:163–168. 10.1073/pnas.1201141110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Voisin M.-B., Larbi K.Y., Dangerfield J., Scheiermann C., Tran M., Maxwell P.H., Sorokin L., and Nourshargh S.. 2006. Venular basement membranes contain specific matrix protein low expression regions that act as exit points for emigrating neutrophils. J. Exp. Med. 203:1519–1532. 10.1084/jem.20051210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver V.M., Petersen O.W., Wang F., Larabell C.A., Briand P., Damsky C., and Bissell M.J.. 1997. Reversion of the malignant phenotype of human breast cells in three-dimensional culture and in vivo by integrin blocking antibodies. J. Cell Biol. 137:231–245. 10.1083/jcb.137.1.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber M.M., Waghray A., and Bello D.. 1995. Prostate-specific antigen, a serine protease, facilitates human prostate cancer cell invasion. Clin. Cancer Res. 1:1089–1094. [PubMed] [Google Scholar]
- Wilson D.F., Jiang D.J., Pierce A.M., and Wiebkin O.W.. 1999. Oral cancer: role of the basement membrane in invasion. Aust. Dent. J. 44:93–97. 10.1111/j.1834-7819.1999.tb00207.x [DOI] [PubMed] [Google Scholar]
- Wiradjaja F., DiTommaso T., and Smyth I.. 2010. Basement membranes in development and disease. Birth Defects Res. C Embryo Today. 90:8–31. 10.1002/bdrc.20172 [DOI] [PubMed] [Google Scholar]
- Wisdom K.M., Adebowale K., Chang J., Lee J.Y., Nam S., Desai R., Rossen N.S., Rafat M., West R.B., Hodgson L., and Chaudhuri O.. 2018. Matrix mechanical plasticity regulates cancer cell migration through confining microenvironments. Nat. Commun. 9:4144 10.1038/s41467-018-06641-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisdom K.M., Indana D., Chou P.-E., Desai R., Kim T., and Chaudhuri O.. 2019. Covalent cross-linking of basement membrane-like matrices physically restricts invasive protrusions in breast cancer cells. Matrix Biol.:S0945-053X(19)30064-2 10.1016/J.MATBIO.2019.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf K., Te Lindert M., Krause M., Alexander S., Te Riet J., Willis A.L., Hoffman R.M., Figdor C.G., Weiss S.J., and Friedl P.. 2013. Physical limits of cell migration: control by ECM space and nuclear deformation and tuning by proteolysis and traction force. J. Cell Biol. 201:1069–1084. 10.1083/jcb.201210152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Chen G., Qiu J., Lu J., Zhu W., Chen J., Zhuo S., and Yan J.. 2016. Visualization of basement membranes in normal breast and breast cancer tissues using multiphoton microscopy. Oncol. Lett. 11:3785–3789. 10.3892/ol.2016.4472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyckoff J., Wang W., Lin E.Y., Wang Y., Pixley F., Stanley E.R., Graf T., Pollard J.W., Segall J., and Condeelis J.. 2004. A paracrine loop between tumor cells and macrophages is required for tumor cell migration in mammary tumors. Cancer Res. 64:7022–7029. 10.1158/0008-5472.CAN-04-1449 [DOI] [PubMed] [Google Scholar]
- Xie Y., Wolff D.W., Wei T., Wang B., Deng C., Kirui J.K., Jiang H., Qin J., Abel P.W., and Tu Y.. 2009. Breast cancer migration and invasion depend on proteasome degradation of regulator of G-protein signaling 4. Cancer Res. 69:5743–5751. 10.1158/0008-5472.CAN-08-3564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W., Mezencev R., Kim B., Wang L., McDonald J., and Sulchek T.. 2012. Cell stiffness is a biomarker of the metastatic potential of ovarian cancer cells. PLoS One. 7:e46609 10.1371/journal.pone.0046609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi N., Mizutani T., Kawabata K., and Haga H.. 2015. Leader cells regulate collective cell migration via Rac activation in the downstream signaling of integrin β1 and PI3K. Sci. Rep. 5:7656 10.1038/srep07656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurchenco P.D. 2011. Basement membranes: cell scaffoldings and signaling platforms. Cold Spring Harb. Perspect. Biol. 3:a004911 10.1101/cshperspect.a004911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurchenco P.D., and Cheng Y.S.. 1993. Self-assembly and calcium-binding sites in laminin. A three-arm interaction model. J. Biol. Chem. 268:17286–17299. [PubMed] [Google Scholar]
- Yurchenco P.D., and Furthmayr H.. 1984. Self-assembly of basement membrane collagen. Biochemistry. 23:1839–1850. 10.1021/bi00303a040 [DOI] [PubMed] [Google Scholar]
- Yurchenco P.D., and Ruben G.C.. 1987. Basement membrane structure in situ: evidence for lateral associations in the type IV collagen network. J. Cell Biol. 105:2559–2568. 10.1083/jcb.105.6.2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotek-Zlotkiewicz E., Monnier S., Cappello G., Le Berre M., and Piel M.. 2015. Optical volume and mass measurements show that mammalian cells swell during mitosis. J. Cell Biol. 211:765–774. 10.1083/jcb.201505056 [DOI] [PMC free article] [PubMed] [Google Scholar]