Abstract
Background:
Long-term exhaustion and chronic occupational stress often result in physician burnout, which can have adverse consequences for patients, physicians, their families, and society. We hypothesized that increased engagement with a wellness curriculum would reduce the level of burnout, as measured by the Maslach Burnout Inventory Human Services Survey (MBI-HSS).
Methods:
We created a yearlong multifaceted pilot wellness curriculum for anesthesia residents at our institution. All residents could experience the wellness curriculum regardless of enrollment in the study. Residents completed the MBI-HSS three times during the year and indicated the number of wellness events attended via web survey. We assessed the influence of different curriculum components and time on the trajectory of three MBI-HSS subscales: emotional exhaustion, depersonalization, and personal accomplishment.
Results:
Thirty-nine of 43 residents consented to participate in the study and completed at least one survey. Residents showed high levels of emotional exhaustion (mean 29.6; SD 11.14), depersonalization (12.8; 4.49), and personal accomplishment (45.0; 6.50) at baseline. Only personal accomplishment showed a significant increase over time (P < .036). Off-campus, wellness group sessions significantly decreased depersonalization (P = .001) and showed no difference in emotional exhaustion (P = .090). However, didactic workshops and wellness-related grand rounds failed to improve our measure of physician burnout, underscoring the need for alternative interventions to reduce this problem.
Conclusions:
A formal wellness curriculum that used classic didactic teaching methods was ineffective at decreasing resident burnout scores. Only wellness group meetings significantly reduced burnout measures. Our findings have important implications for planning future resident wellness interventions.
Keywords: Wellness, residents, anesthesia, curriculum
Introduction
Long-term exhaustion and chronic occupational stress often result in physician burn-out, which leads to adverse consequences for patients, physicians, their families, and society.1–3 Indeed, survey data show that nearly half of physicians report at least one symptom of burnout and are significantly more likely to have symptoms of burnout than adults with similar education levels working in other occupations.1,2 Additionally, many physicians lack insight into their experience of burnout.2,3 Burnout commonly begins in medical school, with the vast majority of medical students experiencing at least one form of distress.4 Burnout is associated with lower scores on measures of empathy and professionalism5,6 and has led the Accreditation Council of Graduate Medical Education (ACGME) in their Common Program Requirements to require that trainee education include topics in self-care and well-being.7
In addition to the ACGME requirements for education in well-being, the American Board of Anesthesiology (ABA) found that 50% of clinical anesthesia year CA-2 (PGY-3) residents and 41% of CA-1 (PGY-2) residents scored at high risk for burnout.8 Unfortunately, 25% of residents were unsure if adequate resources were available to address burnout and depression in their respective training programs.8
Sadaat et al.9 showed that instruction in the areas of active coping and social support help anesthesia residents maintain well-being in both their work and home environments, thus supporting the potential effectiveness of a wellness curriculum with this population. In this pilot study, we hypothesized that level of engagement with the wellness curriculum, as measured by number of wellness events attended, would have a dose-effect relationship with level of burnout, as measured by a web-based survey using the Maslach Burnout Inventory Human Services Survey (MBI-HSS).10
Materials and Methods
After obtaining IRB and participant consent, we created a yearlong (2015–2016) multifaceted pilot wellness curriculum for CA1–CA3 (PGY 2–PGY4) anesthesia residents. The study was presented to the residents in a large group to avoid coercion, emphasizing voluntary participation and with verbal and written reassurance that results would not be available to the program director or the department chair. We designed the curriculum based on a literature review of wellness curriculums (example: Saadat et al.)9, multiple facilitator training courses, and discussion with departmental leadership. It was offered to all residents regardless of study participation. The components of the curriculum included (1) five grand round presentations on topics of substance abuse avoidance, error disclosure, burnout, sexual harassment, and resiliency; (2) quarterly interactive sessions on mindfulness in medicine, which were held during protected didactic time; (3) a peer-mentoring program; (4) monthly e-mailed wellness education articles; (5) a laminated wellness reference card (Figure 1); (6) a confidential monitored wellness e-mail address; and (7) quarterly resident wellness group dinners. The wellness group dinners (funded by the Department of Anesthesiology) were hosted at an attending anesthesiologist's home. The general format of the wellness group dinners was dinner and social time, followed by a resilience exercise (such as guided meditation), led to resident-directed storytelling in an open forum discussion. Being hosted off campus provided a more relaxed, emotionally safe space to discuss resilience and burnout topics.
Figure 1.
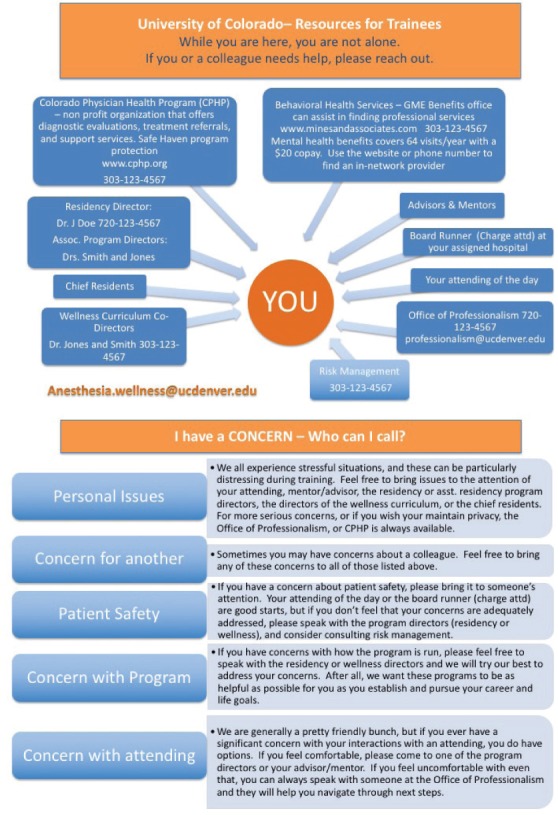
The University of Colorado Department of Anesthesiology's Resident Wellness Resource Card is shown. The wellness card is a laminated badge sized card with a front (a) and back (b), adapted from Amy Vinson, MD at Boston Children's Hospital and Karen Souter MB.BS, FRCA, MACM at University of Washington with permission. The front (a) has resources with accompanying telephone numbers and names and the back (b) has suggestions on who to call and when.
Levels of anesthesia resident burnout were measured in consented participants at three time points during the academic year: before the start of the wellness curriculum in July, midyear in February, and at the conclusion of the year in June. These surveys were done via an e-mail survey format with the MBI-HSS10 and number of wellness events attended. The MBI-HSS is a validated, widely used scale that is generally accepted as the “gold standard” measurement of burnout; it includes three subscales that measure emotional exhaustion (EE), de-personalization (DP), and personal accomplishment (PA). The EE subscale captures feelings of being emotionally overextended and drained. The score is divided into thirds, with increasing numbers correlating with higher burnout (low ≤18, average 19–26, high ≥27). The DP subscale evaluates the cynicism one has toward their patients with an increasing score correlating with higher burnout (low ≤5, average 6–9, high ≥10). The PA measures feelings toward one's own success and competence in work.
This subscale has an inverse relationship with burnout (low ≥40, average 39–34, high ≤28).10 Each subscale is calculated individually, and the survey generates three measures to evaluate burnout. At each time point, residents also reported which wellness events they had attended. All data were collected in REDCap (https://redcap.vanderbilt.edu) electronic data capture tools. All REDCap data were deidentified and exported to STATA 14.2 statistical software for analysis (StataCorp LLC, Stata Statistical Software, College Station, TX). The data were analyzed by descriptive statistics, paired t tests, and multilevel, mixed-effects models. The mixed-effects models allowed us to account for the repeated-measures study design with the resulting correlation between the measurements within each participant and the passing of time as an influence itself, as well as include data from all three measurements, even if some participants might have missing data for one of the measurements. A P value < .05 was considered statistically significant.
Results
Forty-three of 45 residents (96%) consented to participate in the study, of whom 39 (90.7%) responded to the first survey. Only residents who answered the first survey were subsequently evaluated with the MBIHSS. Of those 39, 16 (41%) completed all three surveys, 11 (28.2%) completed the first and third survey, and 12 (30.8%) completed only the first survey. The scores on the three subscales (EE, DP, and PA) from the first survey did not significantly predict attrition nor were they different across the three PGY levels (analyses not shown in detail). Paired t tests comparing the subscale scores of the 27 residents who completed the first and third survey did not show any significant differences between the mean scores on each of the three scales (Table 1). Descriptively, the MBI-HSS showed high levels of EE, DP, and PA at both time points since high levels on each subscale are defined by scores ≥27 (EE), ≥10 (DP), and ≥40 (PA).
Table 1.
Descriptive Statistics of Depersonalization, Emotional Exhaustion, and Personal Accomplishment Scores for Three Different Measurement Time Points and Results for Paired t Tests Between Scores from Surveys at Curriculum Beginning and End
| Curriculum Time Points, n; Mean (SD) | P Value | |||
|---|---|---|---|---|
| Beginning | Half-Time | End | ||
| Depersonalization | 38; 13.1 (4.94) | 16; 12.0 (3.76) | 28; 12.5 (3.53) | 0.718 |
| Emotional Exhaustion | 39; 29.8 (10.09) | 16; 29.6 (9.26) | 27; 28.6 (10.09) | 0.412 |
| Personal Accomplishment | 39; 45.6 (6.33) | 16; 45.9 (4.15) | 27; 45.3 (5.92) | 0.814 |
Three multilevel mixed effect models, each predicting the scores of one of the MBIHSS subscales, included the PGY level, the numbers of wellness groups, wellness grand rounds, and didactic sessions the residents had attended as well as a variable for time, including a nonlinear effect modifier as predictors (Table 2). Each model coefficient in Table 2 represents the average change in MBI-HSS subscale scores for the PGY level compared to PGY2, additional event attended or time passed. Although DP and EE showed no significant changes over time, PA increased significantly over time (P = .036). Among the different interventions, wellness group dinners were the only intervention that had a significant impact by decreasing DP scores on average by 2.40 for each additional wellness group dinner attended (P = .001).
Table 2.
Mixed Effects Models Coefficients: Dependent variables, horizontal. Independent variables, vertical
| Depersonalization | Emotional Exhaustion | Personal Accomplishment | |
|---|---|---|---|
| PGY level (comparison: PGY2) | |||
| PGY3 | −0.27 | 0.51 | −0.29 |
| PGY4 | 1.96 | −2.06 | −0.64 |
| Time | 2.56 | −7.93 | 11.08* |
| Time squared | −0.71 | 1.80 | −2.66* |
| Wellness groups attended | −2.40*** | −1.95 | 1.32 |
| Grand rounds attended | 0.62 | −0.003 | 1.33 |
| Workshops attended | −1.15 | 1.11 | 1.11 |
| Constant | 10.9** | 37.73*** | 34.77*** |
*P < .05;
***P < .01;
****P <.001.
Discussion
As reported in previous studies, we found high levels of EE and DP in anesthesia residents. We were unable to demonstrate a dose-effect relationship between number of wellness events residents attended and their EE or PA score. However, for each additional wellness dinner attended, their DP significantly declined by 2.40; further we did find that the PA of the MBI-HSS improved over the year. Of the many interventions instituted in our pilot wellness curriculum, the only intervention that made a difference was the group dinners. Both grand rounds and formal didactic sessions had no impact (Table 2). Our findings have important implications for planning future wellness interventions.
Both the ACGME and the ABA recognize the epidemic of physician burnout and have required that residency programs establish organized instruction in well-being.7,8 Unfortunately, this requirement was not accompanied with evidence-based instructions on how to accomplish this goal. We developed and tested a wellness curriculum that used classic university teaching methods, including grand rounds, didactic sessions, and so on, and found that they were ineffective as measured by the MBI-HSS. We speculate that these types of educational opportunities introduce material to combat burnout and improve well-being but do not allow any practice of new individual skills or change institutional practice. These findings highlight the need for alternative methods of resident engagement. Indeed, our finding that the resident wellness group dinners were quite effective may have significant implications for future curriculum development and design. Further, we speculate that attending these dinners decreased DP because they offered the opportunity to gather socially in an off-campus, comfortable, emotionally supportive environment, with facilitated discussion that included interactive practice of new resilience skills and the potential to effect culture change among residents. Presumably, wellness dinners may have had a protective effect, and lack of attendance would have increased DP. Discussions about sensitive topics like medical errors, hostile work environments, and challenging patient or staff interactions allowed for a normalization of experiences.
Anesthesia residents are unique in their training when compared to other medical and surgical residents because they rarely work with peers. Rather, they work alone and often interact only with an attending anesthesiologist. This structure decreases their peer-to-peer interactions and opportunities to build relationships of peer support. However, storytelling in trusted peer relationships as occurred in the wellness dinners appears to add to the resilience of our residents. On the other hand, our finding of an increase in PA over the year is a positive indicator that the residents are growing in their chosen field of medicine. It should be noted this increase might have occurred irrespective of our wellness intervention. As residents acquire more medical knowledge and improve their technical skills in the operating room, they will have more success over time (increased PA), but the gain decreases with each additional time point in our model indicating a nonlinear relationship (Table 2). Thus, our findings suggest that a wellness curriculum needs to include opportunities for residents to engage with peers in safe, supportive environments. The limitations of this pilot study include the following: small group of residents, one institution, the use of only one measure to assess the curriculum, and reliance on self-report. Based on our findings, we are currently studying a new curriculum that includes a weekend retreat that will provide residents with a unique opportunity to interact with each other, develop peer relationships, learn and practice resilience techniques, become familiar with resources available to them, and understand the commitment our department has to their education and well-being.
Conclusions
Burnout is a significant problem for anesthesia residents and requires novel intervention. Based on our pilot data, classic modalities of education are insufficient to teach wellness curricula. Alternative techniques may be more effective and are the target of our ongoing studies. As medical educators, we must open our minds to innovative techniques to support our residents.
Acknowledgments
We would like to thank Dr Myron Yaster and Claire F. Levine MS, ELS for their editorial assistance in preparing this manuscript.
Footnotes
Funding: Internal funding from Department of Anesthesiology at University of Colorado, NIH/NCRR Colorado CTSI Grant Number UL1 TR001082 (REDCap database).
References
- 1.Shanafelt TD, Boone S, Tan L et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 2.Shanafelt TD, Hasan O, Dyrbye LN et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–13. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 3.Peckham C. Medscape National Physician Burnout & Depression Report 2018. Art Science Code LLC; New York, New York: https://www.medscape.com/slideshow/2018-lifestyle-burnout-depression-6009235. [Google Scholar]
- 4.Dyrbye LN, Harper W, Durning SJ et al. Patterns of distress in US medical students. Med Teach. 2011;33(10):834–9. doi: 10.3109/0142159X.2010.531158. [DOI] [PubMed] [Google Scholar]
- 5.Brazeau CM, Schroeder R, Rovis S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(suppl 10):S33–6. doi: 10.1097/ACM.0b013e3181ed4c47. [DOI] [PubMed] [Google Scholar]
- 6.Dyrbye LN, Massie FS, Jr, Eacker A et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304(11):1173–80. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 7.The ACGME Common Program Requirements. Accreditation Council for Graduate Medical Education (ACGME); Jul, 2017. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The ABA Surveys CA-1 and CA-2 Residents. :8–9. http://www.theaba.org/PDFs/Newsletters/ABA-NEWS-2015.
- 9.Saadat H, Snow DL, Ottenheimer S et al. Wellness program for anesthesiology residents: a randomized controlled trial. Acta Anaesthesiol Scand. 2012;56(9):1130–8. doi: 10.1111/j.1399-6576.2012.02705.x. [DOI] [PubMed] [Google Scholar]
- 10.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Zalaquett CP, Wood RJ, editors. Evaluating Stress: A Book of Resources. 3rd ed. Scarecrow Education; Lanham, MD: 1997. pp. 191–218. (Eds.) [Google Scholar]


